ABSTRACT
During Sierra Leone’s 2014–2015 Ebola virus disease (EVD) epidemic, early reports warned of health system collapse and potential effects on other-cause mortality. These same warnings are reverberating during the COVID-19 pandemic. Consideration of the impacts of EVD on maternal and child health services from facility data can be instructive during COVID-19. We surveyed all peripheral healthcare units (PHUs) in Sierra Leone in October 2014 and March 2015 to assess closures, staffing, amenities, medicines, supplies, and service utilization during May 2014–January 2015 and October 2013–January 2014. We report PHU characteristics and service utilization changes for equivalent 4-month periods during the epidemic and the prior year. We present utilization changes by district and service type, and model excess child mortality. PHU closures (−8%) and staff attrition (−3%) were limited, but many facilities lacked amenities, medicines, and supplies. Utilization of preventive and scheduled services fell more than individualized, clinical care interventions, aside from malaria treatment which declined significantly. Ebola virus disease intensity in districts was weakly associated with utilization, aside from two districts that were severely affected. Modeling suggests utilization declines resulted in 6,782 excess under-five deaths (an increase of 21%) between 2014 and 2015. Ebola virus disease negatively affected service provision, but utilization declined relatively more, particularly for preventive and scheduled interventions. Although these findings are specific to Sierra Leone’s EVD epidemic, they illustrate the magnitude of possible effects in other settings due to COVID-19–induced service disruptions, where collateral impacts on child mortality from other preventable causes may far outweigh COVID-19 mortality.
INTRODUCTION
The ongoing COVID-19 epidemic and the mitigation measures used raise fears of disruptions in health service provision and utilization for maternal and child health (MCH) services, which could increase child mortality from causes other than COVID-19.1,2 To assess the potential magnitude, we review actual service readiness and service utilization data during Sierra Leone’s Ebola virus disease (EVD) epidemic, model resulting in child deaths, and discuss implications for the COVID-19 healthcare response.
Sierra Leone’s devastating EVD epidemic began in May 2014. By the end of the epidemic in March 2016, Sierra Leone had 14,124 confirmed EVD cases.3 Although the epidemic affected all districts, the timing of the epidemic’s onset, intensity, and duration varied across districts. In 2013, before EVD, Sierra Leone’s maternal mortality ratio and under-five mortality rate were among the highest in the world: 1,100/100,000 live births4 and 133/1,000,5 respectively. Ten years of civil war, concluding in 2002, wracked the country’s infrastructure, workforce, and social capital. Despite efforts to rebuild the health system, including the 2010 Free Health-Care Initiative for pregnant women, breastfeeding mothers, and children,6 systems remained severely under-capacitated.7,8 Early reports during the EVD epidemic warned of health system collapse9,10 and the potential indirect effect of EVD on other-cause mortality11,12 because of limited availability of health services and fear, affecting both care-seeking and health worker attendance.13
Amid uncertainty about health system performance, Sierra Leone’s Ministry of Health and Sanitation (MoHS), with support from UNICEF and partners, conducted two rapid health facility assessments (HFAs) of all peripheral healthcare units (PHUs) in October 2014 and March 2015. PHUs include all non-tertiary facilities and account for 95% of all health facilities. Using HFA data, this article reports on PHU characteristics and examines MCH service utilization changes at national and district levels during a period of high EVD transmission, compared with a similar period 1 year prior. We explore the relationship between the intensity of EVD transmission and changes in MCH service utilization by type of service. We estimate other-cause mortality among children younger than 5 years attributable to the observed MCH service utilization changes. Finally, we discuss the implications of our findings in the context of the current COVID-19 pandemic in low- and middle-income countries.
MATERIALS AND METHODS
Setting.
Sierra Leone is a small West African nation that had about seven million people and a female adult literacy rate of 35.5% in 2013.14 Although very high, under-five child mortality was declining before EVD15 and coverage of key MCH services (antenatal care [ANC], institutional delivery, the third dose of DPT vaccine, and seeking treatment for fever) ranged from 55% to 99.5% across districts (Table 1). Ebola virus disease was first detected in Sierra Leone in May 2014 in Kailahun district. By October 2014, it spread to all districts with nearly 2000 reported cases per month in November 2014 (Table 2). The epidemic subsided rapidly thereafter but was not declared over until March 2016. District cumulative EVD incidence rates over the period May 2014–January 2015 ranged from 12.5/100,000 in Pujehun to 205.9/100,000 in Western Area (Table 2).
Table 1.
Sierra Leone district-level population (2015) and literacy and coverage of select maternal and child health interventions (2013)
| District | Population, 2015 | % Literate, women aged 15–49 years | Under-five mortality per 1,000 live births | % Receiving antenatal care from a skilled provider | % Delivering in a health facility | % Vaccinated with the third dose of DPT vaccine | % Of children younger than 5 years with fever for whom advice or treatment was sought from a health facility or provider |
|---|---|---|---|---|---|---|---|
| Western Area rural | 444,270 | 51 | 176 | 98.6 | 56.7 | 71.6 | 71.4 |
| Western Area urban | 1,055,964 | 65 | 152 | 97.4 | 61.6 | 68.5 | 51.4 |
| Port Loko | 615,376 | 28 | 175 | 97.1 | 39.2 | 74 | 61.9 |
| Bombali | 606,544 | 39 | 113 | 95.5 | 41.4 | 84.2 | 83.5 |
| Kailahun | 526,379 | 29 | 186 | 98.7 | 84.3 | 89 | 81.8 |
| Tonkolili | 531,435 | 28 | 190 | 97.6 | 35.2 | 69.5 | 63.5 |
| Kono | 506,100 | 31 | 171 | 97.6 | 52.7 | 80 | 72.9 |
| Kenema | 609,891 | 31 | 224 | 98.4 | 77.3 | 83.3 | 72.6 |
| Moyamba | 318,588 | 24 | 199 | 97.2 | 32.7 | 78.7 | 63.7 |
| Bo | 575,478 | 36 | 173 | 99.5 | 71.9 | 93.4 | 66.2 |
| Kambia | 345,474 | 20 | 131 | 93.1 | 33.9 | 61.1 | 59.5 |
| Koinadugu | 409,772 | 18 | 202 | 90.1 | 32.8 | 69.9 | 55 |
| Bonthe | 200,781 | 25 | 77 | 96.2 | 74 | 80.9 | 81.1 |
| Pujehun | 346,461 | 23 | 217 | 98.5 | 62.1 | 87.1 | 65.8 |
| National | 7,092,513 | 36 | 156 | 97.1 | 54.4 | 77.9 | 65.6 |
| Median | 516,240 | 28 | 176 | 97.5 | 54.7 | 79.4 | 66 |
| SD | 202,633 | 6 | 44 | 2.7 | 19.7 | 9.2 | 9.4 |
| 25th percentile | 346,461 | 24 | 152 | 96.2 | 35.2 | 69.9 | 61.9 |
| 75th percentile | 606,544 | 36 | 199 | 98.5 | 71.9 | 84.2 | 72.9 |
| Interquartile range | 260,083 | 12 | 47 | 2.3 | 36.7 | 14.3 | 11 |
EVD = Ebola virus disease; ICF = International Community Foundation; Sources: Statistics Sierra Leone. Population and Housing Census 2015, Statistics Sierra Leone and ICF International 2014, Sierra Leone Demographic and Health Survey 2013. Freetown, Sierra Leone, and Rockville, MA: Statistics Sierra Leone and ICF International.
Table 2.
Monthly number of confirmed EVD cases by district, May 2014–January 2015
| District | May | June | July | August | September | October | November | December | January | Total | Ebola Virus Disease Cumulative Incidence Rate (per 100,000 population) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Kailahun | 8 | 98 | 122 | 140 | 73 | 25 | 8 | 3 | 0 | 477 | 90.6 |
| Kenema | 0 | 24 | 108 | 150 | 71 | 62 | 1 | 2 | 8 | 426 | 69.8 |
| Bo | 0 | 1 | 5 | 35 | 51 | 80 | 74 | 47 | 14 | 307 | 53.3 |
| Bombali | 0 | 0 | 4 | 35 | 183 | 333 | 229 | 136 | 20 | 940 | 155.0 |
| Port Loko | 0 | 0 | 4 | 57 | 225 | 235 | 326 | 309 | 123 | 1,279 | 207.8 |
| Western Area | 0 | 0 | 4 | 71 | 320 | 718 | 943 | 754 | 278 | 3,088 | 205.8 |
| Tonkolili | 0 | 0 | 1 | 15 | 62 | 132 | 160 | 57 | 18 | 445 | 83.7 |
| Kono | 0 | 0 | 1 | 3 | 17 | 19 | 55 | 110 | 40 | 245 | 48.4 |
| Moyamba | 0 | 0 | 0 | 5 | 47 | 39 | 49 | 25 | 17 | 182 | 57.1 |
| Kambia | 0 | 2 | 0 | 0 | 17 | 21 | 39 | 35 | 39 | 153 | 44.3 |
| Koinadugu | 0 | 0 | 0 | 0 | 0 | 15 | 74 | 18 | 4 | 111 | 27.1 |
| Pujehun | 0 | 0 | 0 | 6 | 12 | 9 | 19 | 0 | 1 | 47 | 13.6 |
| Bonthe | 0 | 0 | 0 | 0 | 0 | 31 | 19 | 2 | 0 | 52 | 25.9 |
| National | 8 | 125 | 249 | 517 | 1,078 | 1719 | 1996 | 1,498 | 562 | 7,752 | 109.3 |
Data accessed on April 2015 (Sierra Leone Ministry of Health and Sanitation): 1–50 cases, 51–100 cases, 101–200 cases, 201–500 cases, and 500+ cases.
Study design and data collection.
Two HFAs of all PHUs in Sierra Leone were conducted in October 2014 and March 2015. The first aimed to understand PHU operational status and service utilization during the epidemic. The second expanded on the first, to help plan for health system recovery. Both HFAs documented PHU closure, the availability of human resources, and monthly service visits for 10 essential MCH services: family planning, ANC, prevention of mother-to-child transmission of HIV, institutional delivery, postnatal care, pediatric HIV treatment, pentavalent vaccination (third dose), pediatric malaria treatment, growth monitoring, and treatment for severe acute malnutrition in children. The March 2015 HFA also collected information on the availability of medicines, supplies, and amenities (water, sanitation, and electricity). During the March 2015 HFA, service visit data were abstracted from facility records for two comparable 4-month periods before and during the epidemic: October 2013–January 2014 (period 1, before EVD) and October 2014–January 2015 (period 2, during EVD). Because seasonal variation can affect service utilization patterns, in this article, we only assess changes in service uptake for these two periods and do not include service utilization data collected during the October 2014 HFA. In addition, we reviewed EVD incidence over the period May 2014–January 2015.
Assessments were approved and managed by the MoHS and UNICEF. They comprised close-ended questionnaires administered to senior onsite health workers, direct observation of amenities and stocks, and abstraction of data for 10 MCH service indicators from facility-based monthly health management information system (HMIS) reports. Data were collected by trained teams of two using paper-based questionnaires (October 2014) and tablets with KoBo Toolbox (version 1.4.3 [1,039]; Harvard Humanitarian Initiative, Cambridge, MA) open-source software (March 2015). Quality control measures included field-based supervision and review, back-up paper questionnaires in the event of tablet malfunction, and centralized review of values. Ministry of Health and Sanitation confirmed EVD case data were used to assess EVD intensity by district.
Data analysis.
We report descriptive PHU characteristics, including closures and availability of staff, amenities, medicines, and supplies. We used MCH Aides (junior nurses), which according to our survey were the largest cadre of health workers, to gauge attrition of clinical health workers during the EVD epidemic. We calculate the percent change in median cumulative MCH service visits between period 1 and period 2 by district for five tracer services: pentavalent three vaccine administration, malaria treatment (artemisinin-based combination therapy) for children younger than 5 years, four ANC visits (ANC 4), institutional deliveries, and growth monitoring. We use median as the central tendency measure because data are not normally distributed with high skewness and kurtosis, likely because of data quality issues common to routinely collected health data. Where data were missing for 1 month in a series, the 3-month average was imputed for the missing value. Where data were missing for more than 1 month, the PHU record was dropped for analysis of that intervention. Dropped values account for less than 3% of PHUs. We also excluded extreme outliers, which accounted for 3–5% of PHUs (Supplemental Webappendix 1).
We evaluate whether changes in service utilization between periods 1 and 2 are statistically significant at P < 0.05 using the Wilcoxon signed-rank test (Supplemental Webappendix 2). We also assess whether changes in service use differed across districts using pairwise nonparametric Bonferoni-adjusted Dunn tests (Supplemental Webappendix 3). To determine if some interventions were more affected than others, we compared median percentage change in cumulative visits by intervention type and applied the Wilcoxon matched-pairs signed-rank test. To assess the relationship between service utilization and EVD intensity, we examine the correlation between the cumulative EVD incidence rate using MoHS confirmed case data from May 2014 to January 2015 and changes in service utilization across districts. Statistical analyses were conducted in STATA (STATA IC 12·1, StataCorp., College Station, TX).
Last, we used the Lives Saved Tool (LiST) within spectrum analyzer (version 5.07; Avenir Health, Glastonbury, CT)16 to model excess under-five mortality attributable to the observed reductions in MCH service uptake during a 12-month period during 2014 and 2015. Lives Saved Tool is designed to estimate the impact of changes in health intervention coverage on mortality. We used annual country data available from the LiST website and incorporated additional data for 2013 and 2014 (Supplemental Webappendix 4). We created a baseline projection that assumed 2014 coverage estimates continued along the 2013 trajectory. We then developed a second projection that used the HFA-detected percent change in service utilization for 10 interventions to adjust annual MCH intervention coverage levels. Because the HFA did not collect data on all interventions included in LiST, we assumed the same change in coverage for interventions that are similar or operate on the same platform. For instance, changes in institutional deliveries were applied to newborn care services. Where no related data were obtained, we did not adjust 2014 coverage levels unless new estimates were published. Because much of the underlying data used in LiST are based on annual estimates, we are unable to present a more detailed estimate than expected excess mortality over a 12-month time period within 2014 and 2015.
Role of the funding source.
UNICEF and the Sierra Leone MoHS supported the cost of the HFAs. UNICEF and MoHS staff conducted this analysis and wrote the manuscript. The authors had access to all data reported in this article and have final responsibility for the decision to publish. Ethics approval was not required/sought.
RESULTS
In October 2014, 1,175 PHUs were assessed. In March 2015, 10 additional PHUs were found and one PHU was missed, resulting in 1,184 PHUs assessed (Table 3). Only a small percentage (8%) of facilities were closed or reported a period of closure during the preceding 4 months at the time of either assessment. In March 2015, the majority of closures (66%) were for less than 1 month and 44% were among the lowest level PHUs typically staffed by 1–2 personnel. Maternal and child health Aides with 1–2 years of nursing training constituted half of the clinical workforce in April 2014 (n = 2,038). We found limited attrition of MCH Aides (−3% between October 2014 and March 2015). During this period, 124 PHU personnel died of EVD and 215 abandoned posts. In March 2015, 93% of facilities reported having at least two people trained in infection prevention and control (IPC), and 98% reported having triage stations in place. Although preparedness improved, in March 2015, 67% of health workers reported fear of stigmatization from the community (down from 90% in October 2014), suggesting that fear of health centers was still pervasive. The majority of health workers were still wary of being infected with EVD (74%) in March 2015. Although PHUs mostly remained open and staffed, the March 2015 assessment revealed severe deficits in basic amenities and supplies.
Table 3.
Peripheral health care unit (PHU) characteristics, October 2014 and March 2015
| Indicator | October 2014, N (%) | March 2015, N (%) | |
|---|---|---|---|
| PHU type | |||
| PHUs surveyed | 1,175 | 1,184 | |
| PHU operational status | |||
| PHUs closed at time of survey or experiencing some period of closure in the last 4 months | 94 (8) | 94 (8) | |
| PHUs closed at time of survey | 47 (4) | 24 (2) | |
| PHUs open at time of survey, but reporting temporarily closure during the past 4 months | 47 (4) | 70 (6) | |
| PHUs closed at time of survey in October and still closed in March | Not asked | 5 (0.4) | |
| PHUs closed during the last 4 months (March N = 94) | |||
| PHUs closed for less than 1 month | Not asked | 62 (66) | |
| October 2014 (N) | March 2015 (N) | Percent change | |
| Availability of healthcare workers (October N = 1,174, March N = 1,160) | |||
| State registered nurses (SRNs) and midwives | 239 | 228 | −5 |
| Community health officers (CHOs) and community health assistants (CHAs) | 501 | 477 | −5 |
| State enrolled community health nurses | 1,083 | 1,095 | 1 |
| Maternal and child health aides | 2,038 | 1,978 | −3 |
| Laboratory personnel | 225 | 213 | −5 |
| Non-technical personnel | 3,746 | 3,812 | 2 |
| Community health workers | 10,899 | 12,674 | 16 |
| Status of facility-based healthcare workers (October N = 1,174, March N = 1,160) | |||
| Healthcare workers trained in IPC | 4,052 | 10,596 | – |
| Healthcare workers reported deceased from EVD since October 2014 | – | 124 | – |
| Health care workers abandoned post since October 2014 | – | 215 | – |
| Availability of facility amenities (All open PHUs, March N = 1,160) | – | March 2015, N (%) | |
| Electricity | 391 (34) | ||
| Consistent electricity available from main or auxiliary source during the last 7 days | 249 (21) | ||
| Water always available | 827 (71) | ||
| Water never available | 157 (14) | ||
| Water onsite | 678 (58) | ||
| Running water in the delivery room (N = 1,143) | – | 129 (11) | |
| Functional incinerator and/or burn pit | 1,148 (97) | ||
| At least two latrines (standard) | 480 (41) | ||
| At least one latrine | 1,094 (92) | ||
| Functional refrigerator for vaccines | – | 467 (39) | |
| Availability of essential medicines and supplies - all open PHUs (N = 1,160) | |||
| Artemisinin-based combination therapy and amoxicillin/cotrimoxazole | 778 (67) | ||
| Folic acid and albendazole | – | 307 (26) | |
| Oxytocin, magnesium sulfate, and injectable benzylpenicillin | 28 (2) | ||
| HIV test kits | 554 (48) | ||
| Delivery bed and complete delivery kit (N = 1,143) | 250 (22) | ||
| BEmONC facilities: Availability of amenities, medicines, and supplies (N = 64) | |||
| Running water in the delivery room | – | 26 (41) | |
| pcOxytocin, magnesium sulfate and injectable benzylpenicillin | – | 28 (44) | |
| Standard delivery bed and complete delivery kit | 42 (66) | ||
| Availability of IPC inputs (N = 1,160) | |||
| At least two people trained in IPC | – | 1,079 (93) | |
| Triage stations in place | – | 1,131 (98) | |
| Chlorine/disinfectant | – | 1,138 (98) | |
| Latex gloves | – | 1,140 (98) | |
| Ebola Virus Disease challenges and concerns reported by staff at PHUs | |||
| % Of PHUs reporting “fear of being stigmatised by community” | 1,057 (90%) | 780 (67) | |
| % Of PHUs reporting “fear of being infected by patient” | Not asked | 853 (74) | |
EVD= Ebola virus disease; IPC = infection prevention and control; PHU = peripheral health care unit.
Table 4 presents the change in median service utilization between period 1 (October 2013–January 2014, pre-Ebola) and period 2 (October 2014–January 2015, during Ebola). We find sizeable and statistically significant national declines in service utilization for all tracer MCH services. Reductions were largest for child malaria treatment and growth monitoring (−33% and −32%), with lower but statistically significant declines in the third dose of pentavalent immunization (−17%), ANC 4 (−16%), and institutional deliveries (−7%). District-level results exhibit a wide range of reduction patterns across services. We evaluated rates of decline for each intervention as compared with declines in the other interventions to assess whether certain intervention types were more heavily affected by changing use patterns. These differences were statistically significant, except between malaria treatment and growth monitoring (Supplemental Webappendix 2).
Table 4.
Ebola cumulative incidence rate (May 2014–January 2015) and percent change in median cumulative service utilization between the 4-month periods October 2013–January 2014 and October 2014–January 2015
| Ebola cum I.R. (per 100,000) May 2014–January 2015 | Pentavalent 3, % | Antenatal care 4, % | Deliveries, % | Malaria treatment (artemisinin-based combination therapy) for children younger than 5 years, % | Growth monitoring, % | |
|---|---|---|---|---|---|---|
| WA | 205.8 | −32* | −24* | −22* | −57* | −33* |
| Port Loko | 207.8 | −39* | −33* | −25* | −55* | −61* |
| Bombali | 155.0 | −18* | −20 | −12* | −30* | −32* |
| Kailahun | 90.6 | −4 | −11 | −10* | −15 | −30* |
| Tonkolili | 83.7 | −27* | −8* | −2 | −32* | −39* |
| Kono | 48.4 | −19* | −23* | −13* | −29* | −48* |
| Moyamba | 57.1 | −19* | −11 | −2 | −16* | −21* |
| Kenema | 69.8 | −11 | −13† | −4 | −29* | −29* |
| Bo | 53.3 | −8* | 2 | −1 | −24* | −25* |
| Kambia | 44.3 | −13* | −10† | −1 | −47* | −34* |
| Koinadugu | 27.1 | −10 | −24 | 3 | −27* | −20* |
| Bonthe | 25.9 | −21* | −26† | −16* | −22 | −27* |
| Pujehun | 13.6 | −6 | −9 | 6 | −16* | −19* |
| National | 109.3 | −17* | −16* | −7* | −33* | −32* |
| Median | −18 | −13 | −4 | −29 | −30 | |
| p25 | −21 | −24 | −13 | −32 | −34 | |
| P75 | −10 | −10 | −1 | −22 | −25 | |
| Median district | Bombali | Kenema | Kenema | Kenema | Kailahun | |
Statistically significant at P ≤ 0.01 level.
P ≤ 0.05 level, otherwise non-statistically significant (Wilcoxon sign-rank test).
District-specific analysis revealed large and statistically significant reductions in services in most districts across all services. Port Loko and Western Area, districts with the highest EVD cumulative incidence rates, register the largest declines in service use across nearly all tracer services, and these reductions were often statistically significantly larger than changes in other districts (Figure 1). More detail on changes by district for each tracer service is included in Supplemental Webappendix 3.
Figure 1.
Correlation between district-level changes in service utilization levels and district-level Ebola virus disease (EVD) cumulative incidence rate (May 2014–January 2015). This figure appears in color at www.ajtmh.org.
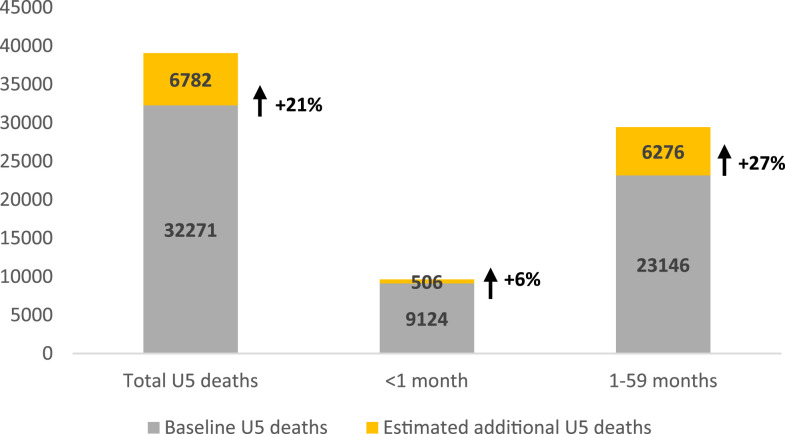
Based on these coverage changes, our modeled estimates of excess mortality suggest that an additional 6,782 deaths (506 neonatal and 6,276 children aged 1–59 months), representing an increase of 21%, occurred in Sierra Leone during a 12-month period of the epidemic during 2014 and 2015 (Figures 2 and 3).
Figure 2.
Additional (non-Ebola virus disease) child deaths estimated in Sierra Leone during a 12-month period (2014–2015) as a result of reduced health service utilization.
Figure 3.
Estimated additional (non-Ebola virus disease ) deaths among children younger than 5 years during a 12-month period (2014–2015), by cause of death, Sierra Leone.
We estimate the top three causes of excess death to be diarrheal disease (43%), malaria (21%), and pneumonia (20%).
DISCUSSION
This study, using health service statistics from all PHUs in Sierra Leone during the height of the Ebola emergency, suggests that there were significant declines in MCH service use. Although initially PHUs were not well equipped to manage EVD, IPC improvements were made during the emergency, and the vast majority of PHUs remained open and staffed during the height of the epidemic.17 Nonetheless, reductions in service use occurred throughout the country even where EVD transmission was modest, suggesting that demand-side factors played an important role. This finding is similar to that of a study in Guinea that reported declines in malaria treatment both in highly EVD-affected prefectures and in prefectures with no EVD.18 Several variables may have influenced service use, including limited trust in the health system, difficulties accessing facilities,19 economic factors,20 fear of nosocomial transmission,21 and other sociocultural factors.22
Preventive and schedulable tracer services, such as ANC, immunization and growth monitoring, declined more than individualized, clinical care services, such as deliveries, and therefore it is possible that the population felt these services could be delayed. This concurs with another study that reported large (−22%) declines in ANC coverage during the epidemic,23 although it conflicts with a meta-analysis that found higher declines among inpatient services versus outpatient services.24 One individualized, clinical care intervention we examined (child malaria treatment) showed heavy declines and defied the pattern of more moderate declines that were otherwise observed. This may be because of a combination of factors. First, Sierra Leone conducted a national distribution of 3.6 million bednets in May 2014, with reported child use at 90% in July 2014.25 Mass drug administration of malaria treatment also took place in December 2014 and January 2015.26 Malaria and EVD are both indicated by fever; individuals with fever were instructed to go to EVD units for screening, where they were often treated presumptively for malaria. General fear of exhibiting EVD symptoms and attending EVD units may have discouraged treatment seeking, as both healthcare workers and healthcare facilities were seen as potential sources of infection, particularly at the start of the epidemic.27 This view was supported by evidence that the risk of infection was 21–32 times higher in health workers in the region than in non–health workers.28 Health seeking for malaria treatment could be similar during COVID-19, if people with fever are afraid to present at facilities, are unable to travel because of restrictions on movement, or believe they should isolate at home.
Ebola virus disease exposed preexisting vulnerabilities of Sierra Leone’s health system, including deficits in basic amenities, supplies, and medicines. Challenges due to an understaffed and overworked health workforce have been documented.29 These gaps are long-standing, limit quality of care, and reduce community trust.30 Although our results confirm weaknesses in the system, the relatively low levels of health worker attrition and PHU closure suggest some resilience and ability to maintain health system function during an emergency. These results provide hope that MCH services provided in countries with weak health system infrastructures need not collapse or be shut down completely during the COVID-19 pandemic of 2020. Managing the current COVID-19 epidemic and preparing for future pandemics require building on features of the health system that proved resilient during the EVD epidemic while also making critical choices and investments to prioritize the maintenance of essential health services during and following health emergencies.
Healthcare workers at facility and community levels are the backbone of health systems. The WHO states that health worker protection is key to the capability of health systems to respond to health emergencies and meet routine healthcare needs.31 Sierra Leone’s installation of infection, prevention, and control measures (including personal protective equipment [PPE], handwashing stations, and thermometers), as well as incentives for health workers to stay in their posts (“risk allowances”),32 were a morale boost33 and likely contributed to continued staffing in most facilities. Unfortunately, IPC measures have not been fully sustained in Sierra Leone.34,35 In July 2020, during the COVID-19 epidemic, news outlets reported a strike among doctors because of a shortage of PPE.36 This is a critical enabler of health system resilience that is proving challenging across many countries and demonstrates the imperative of sustained investments in IPC and health worker safety as part of health emergency preparedness.
Community health workers and other community-level actors also played important roles during the Ebola outbreak by adapting emergency response measures to ensure community acceptability and providing feedback on community priorities.37 Their engagement in emergency preparedness and response plans during COVID-19 may strengthen communication efforts and service delivery at both community and facility levels. Furthermore, regular two-way communication between the health system and the community that is fact based, timely, and accurate will instill trust in the system and enhance the capacity of health workers to continue to provide primary health care.
Our findings indicate that the indirect impact of Ebola on child mortality (6,782 deaths over 12 months) far exceeded the death toll from EVD (3,956) for all age-groups in Sierra Leone. This suggests that the impact of an epidemic should not be measured by the mortality directly attributed to a specific pathogen alone, such as Ebola or SARS-CoV-2, but overall excess mortality, which includes the indirect effect of the health emergency. Assessing the impact of a health emergency in this way, while challenging in real time, can prompt more nuanced consideration of emergency response priorities and strategies. During COVID-19, many governments in the African region were quick to use restrictive social measures to prevent the spread of COVID-19. Although these measures may be reducing the spread of COVID-19, they have other social, economic, and health consequences that must be carefully weighed. In settings with high child and adult mortality from infectious diseases and other preventable conditions such as diarrheal disease, pneumonia, malaria, malnutrition, and neonatal sepsis, it is critical to consider the relative risks of mortality due to these other causes when making decisions about the redistribution of health system resources, restrictions on movement, and public health messaging. Policy adjustments to balance COVID-19 mitigation measures with the need for continued attention to ongoing, more routine but still devastating health risks are necessary and urgent.
Good monitoring of routine health system performance and the continuity of essential health services both on the supply and demand side is essential in determining whether emergency response measures or population sentiment across subnational locations are influencing health service delivery patterns over the course of the pandemic and prompt remedial action. Although Sierra Leone relied on two national facility surveys administered in-person because of reservations concerning the completeness of the HMIS, strong health information systems enabled by digital reporting of routine health statistics, surveillance of notifiable disease and death, and rapid surveys can be instrumental in providing national and subnational government decision-makers with the information required to ensure timely, adaptive management of protracted crises like Ebola or COVID-19. These data should be complemented by the perspectives of community members and health workers to better understand why disruptions occur and how they might be quickly resolved to save lives. Unfortunately, in many contexts, routine information systems are still weak, resulting in a limited understanding of the full effects of COVID-19, which affects response efforts and has led to an overreliance on models.
There are several limitations to our findings. First, the HFA was a census of PHUs and did not include hospitals or EVD case management facilities. Hospitals account for approximately 4.6% of health facilities. Our analysis assumes that facility choice did not change during EVD. Second, our results may be limited by completeness and accuracy errors that commonly affect routine health service statistics. We assume that data quality is comparable across periods. However, it is possible that data quality declined during period 2 because of fewer staff, less supervision, and changing priorities. Third, LiST modeling relied on several assumptions: 1) changes at PHUs are representative of national utilization patterns, 2) changes are representative of a 12-month period, and 3) similar interventions experienced the same changes seen among the tracer interventions reviewed. Lives Saved Tool estimates are also limited to deaths attributed to declines in health service uptake alone. The relationship between service utilization and mortality is complex and difficult to estimate accurately. Lives Saved Tool estimates should therefore be interpreted with caution.
As the COVID-19 pandemic continues to unfold across the world and challenge health systems, including the best endowed, it is urgent to heed the lessons learned from Sierra Leone by ensuring investments in both health emergency preparedness and primary healthcare systems are both significant and sustained. One without the other is insufficient. In the African region, given the pressures of population growth, climate change, and urbanization, there is no time to waste.
Supplemental webappendices
ACKNOWLEDGMENTS
We thank UNICEF Sierra Leone, Ministry of Health and Sanitation, and FOCUS 1000 colleagues for their support of the design and management of the health facility surveys: Faraja Chiwile, Nathalie Daries, Shane O’Connor, Yaron Wolman, Hamjatu Khazali, Moses Cowan, Joseph Nganga Njau, Miatta Koroma, John Baimba, and Mohamed Jalloh, Paul Sengeh, and MoHS colleagues. We would also like to thank UNICEF Sierra Leone, UNICEF West and Central Africa Office, and UNICEF New York Headquarters colleagues for technical inputs: Augustin Kabano, Ngozi Kennedy, Patrick Okoth, Nathalie Diaries, Vandana Joshi, Edmund Makiu, Sylvia Lee, Abdulai Jalloh, Prabhat Kumar, Remy Mwamba, Jerome Pfaffmann, Richard Kumapley, Kumanan Rasanathan, Theresa Diaz, David Hipgrave, and Stefan Peterson. We are also thankful to the reviewers of our initial manuscript for their thoughtful comments.
Note: Supplemental webappendices appear at www.ajtmh.org.
REFERENCES
- 1.Nelson R, 2020. COVID-19 disrupts vaccine delivery. Lancet Infect Dis 20: P546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Roberton T, Carter ED, Chou VB, Stegmuller A, Jackson BD, Tam Y, Sawadogo-Lewis T, Walker N, 2020. Early estimates of the indirect effects of the Coronavirus pandemic on maternal and child mortality in low- and middle-income countries. Lancet 8: E901–E908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shoman H, Karafillakis E, Rawaf S, 2017. The link between the west African Ebola outbreak and health systems in Guinea, Liberia and Sierra Leone: a systematic review. Glob Health 13: 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.WHO, UNICEF, UNFPA, World Bank, United Nations Population Division , 2014. Trends in Maternal Mortality: 1990–2013. Geneva, Switzerland: World Health Organization. Available at: https://www.who.int/reproductivehealth/publications/monitoring/maternal-mortality-2013/en/. Accessed April 26, 2020. [Google Scholar]
- 5.UN Interagency Group for Child Mortality Estimation , 2014. Levels and Trends in Child Mortality. Available at: https://www.who.int/maternal_child_adolescent/documents/levels_trends_child_mortality_2014/en/. Accessed April 26, 2020. [Google Scholar]
- 6.Donnelly J, 2011. How did Sierra Leone provide free health care? Special Report. Lancet 377: 1393–1396. [DOI] [PubMed] [Google Scholar]
- 7.World Health Organization , 2012. Sierra Leone Service Availability and Readiness Assessment. Geneva, Switzerland: WHO. Available at: https://apps.who.int/healthinfo/systems/datacatalog/index.php/catalog/27/reports. Accessed April 26, 2020. [Google Scholar]
- 8.Witter S, Wurie H, Bertone MP, 2016. The free health care initiative: how has it affected health workers in Sierra Leone? Health Pol Plan 31: 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Blanchet K, Nam S, 2014. Warnings over collapse of health system in the wake of Ebola in Sierra Leone. NewStatesman. Available at: http://www.newstatesman.com/health/2014/12/warnings-over-collapse-health-system-wake-ebola-sierra-leone. Accessed April 26, 2020. [Google Scholar]
- 10.Lako S, 2015. The Impact of Ebola in Sierra Leone. Br Med J Blog. Available at: http://blogs.bmj.com/bmj/2015/01/14/sandra-lako-the-impact-of-ebola-in-sierra-leone/. Accessed April 26, 2020. [Google Scholar]
- 11.Walker PG, White MT, Griffin JT, Reynolds A, Ferguson NM, Ghani AC, 2015. Malaria morbidity and mortality in Ebola-affected countries caused by decreased health-care capacity, and the potential effect on mitigation strategies: a modelling analysis. Lancet Infect Dis 15: 825–832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Helleringer S, Noymer A, 2015. Magnitude of Ebola relative to other causes of death in Liberia, Guinea and Sierra Leone. Lancet 3: PE255–PE256. [DOI] [PubMed] [Google Scholar]
- 13.Dynes MM, Miller L, Sam T, Vandi MA, Tomczyk B, 2015. Perceptions of the risk for Ebola and health facility use among health workers and pregnant and lactating women – Kenema district, Sierra Leone, September 2014. MMWR 63: 1226–1227. [PubMed] [Google Scholar]
- 14.Statistics Sierra Leone (SSL) and ICF International , 2014. Sierra Leone Demographic and Health Survey 2013. Freetown, Sierra Leone and Rockville, MA: SSL and ICF International. [Google Scholar]
- 15.United Nations Children’s Fund , 2014. Committing to Child Survival: A Promise Renewed. Progress Report 2014. New York, NY: UNICEF. [Google Scholar]
- 16.Johns Hopkins Bloomberg School of Public Health , 2020. The Lives Saved Tool (LiST). Available at: https://www.jhsph.edu/research/centers-and-institutes/institute-for-international-programs/current-projects/lives-saved-tool/. Accessed April 26, 2020. [Google Scholar]
- 17.Kanu H, Wilson K, Sesay-Kamara N, Bennett S, Mehtar S, Storr J, Allegranzi B, Benya H, Park B, Kolwaite A, 2019. Creation of a national infection prevention and control programme in Sierra Leone, 2015. BMJ Glob Health 4: e001504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Plucinski MM, et al. 2015. Effect of Ebola-virus-disease epidemic on malaria case management in Guinea, 2014: a cross-sectional survey of health facilities. Lancet Infect Dis 15: 1017–1023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Brolin Ribacke KJ, van Duinen AJ, Nordenstedt H, Höijer J, Molnes R, Froseth TW, Koroma AP, Darj E, Bolkan HA, Ekström AM, 2016. The impact of the west Africa Ebola outbreak on obstetric health care in Sierra Leone. PLoS One 11: e0150080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Huber C, Finelli L, Stevens W, 2018. The economic and social burden of the 2014 Ebola outbreak in west Africa. J Infect Dis 218: S698–S704. [DOI] [PubMed] [Google Scholar]
- 21.Pruyt E, Auping WL, Kwakkel JH, 2015. Ebola in west Africa: model-based exploration of social psychological effects and interventions. Syst Res Behav Sci 32: 2–14. [Google Scholar]
- 22.Sharareh N, Sabounchi NS, Sayama H, MacDonald R, 2016. The Ebola crisis and the corresponding public behaviour: a system dynamics approach. PLoS Curr 8. 10.1371/currents.outbreaks.23badd9821870a002fa86bef6893c01d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sochas L, Channon AA, Nam S, 2017. Counting indirect crisis-related deaths in the context of a low-resilience health system: the case of maternal and neonatal health during the Ebola epidemic in Sierra Leone. Health Pol Plan 32: iii32–ii39. [DOI] [PubMed] [Google Scholar]
- 24.Wilhelm JA, Helleringer S, 2019. Utilization of non-Ebola health care services during Ebola outbreaks: a systematic review and meta-analysis. J Glob Health 9: 010406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ministry of Health and Sanitation, Irish Aid and UNICEF , 2014. Sierra Leone National Nutrition Survey 2014. Freetown, Sierra Leone: UNICEF. [Google Scholar]
- 26.Aregawi M, Smith SJ, Sillah-Kanu M, Seppeh J, Kamara ARY, Williams RO, Aponte JJ, Bosman A, Alonso P, 2016. Impact of the Mass drug administration for malaria in response to the Ebola outbreak in Sierra Leone. Malar J 15: 480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Nuriddin A, et al. 2018. Trust, fear, stigma and disruptions: community perceptions and experiences during periods of low but ongoing transmission of Ebola virus disease in Sierra Leone, 2015. BMJ Glob Health 3: e000410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.World Health Organization , 2015. Health Worker Ebola Infections in Guinea, Liberia and Sierra Leone. A Preliminary Report 21 May 2015. Geneva, Switzerland: WHO. Available at: https://www.who.int/hrh/documents/21may2015_web_final.pdf. Accessed May 7, 2020. [Google Scholar]
- 29.Wurie H, Witter S, 2014. Serving through and after conflict: life histories of health workers in Sierra Leone. Report for ReBUILD. Available at: http://www.rebuildconsortium.com/resources/research-reports/serving-through-and-after-conflict-life-historiesof-health-workers-in-sierra-leone/. Accessed May 7, 2020. [Google Scholar]
- 30.Boozary AS, 2014. The Ebola outbreak, fragile health systems, and quality as a cure. JAMA 312: 1859–1860. [DOI] [PubMed] [Google Scholar]
- 31.World Health Organization , 2015. Health Worker Ebola Infections in Guinea, Liberia and Sierra Leone. Preliminary Report 21 May 2015. Available at: https://apps.who.int/iris/bitstream/handle/10665/171823/WHO_EVD_SDS_REPORT_2015.1_eng.pdf?sequence=1&isAllowed=y. Accessed May 7, 2020. [Google Scholar]
- 32.Raven J, Wurie H, Witter S, 2018. Health workers’ experiences of coping with the Ebola epidemic in Sierra Leone’s health system: a qualitative study. BMC Health Serv Res 18: 251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ratnayake R, Ho LS, Ansumana R, Brown H, Borchert M, Miller L, Kratz T, McMahon SA, Sahr F, 2016. Improving Ebola infection prevention and control in primary healthcare facilities in Sierra Leone: a single-group pretest post-test, mixed-methods study. BMJ Glob Health 1: e000103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mandoh S, Gogra AB, Mandoh IV, Kangbai JB, 2017. Level of IPC knowledge and practice in hospitals still low in Sierra Leone after the 2014–2015 Ebola outbreak. Integr J Glob Health 1: 14. [Google Scholar]
- 35.Nuclear Threat Initiative , 2019. Global Health Security Index. Building Collective Action and Accountability. Available at: https://www.ghsindex.org/wp-content/uploads/2019/10/2019-Global-Health-Security-Index.pdf. Accessed May 7, 2020. [Google Scholar]
- 36.Inveen C, 2020. Sierra Leone doctors’ strike leaves COVID-19 patients stranded. Health News. Reuters. Available at: https://www.reuters.com/article/us-health-coronavirus-leone/sierra-leone-doctors-strike-leaves-covid-19-patients-stranded-idUSKBN2432NU. Accessed May 7, 2020. [Google Scholar]
- 37.Miller NP, et al. 2018. Community health workers during the Ebola outbreak in Guinea, Liberia, and Sierra Leone. J Glob Health 8: 020601. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.