Abstract
Purpose:
There is limited information in literature about the scope and usability of Smartphone Applications (Apps) in ophthalmology. Eye care professionals are therefore skeptical about the benefits of smartphone Apps and are reluctant to adopt it in their day to day practice. The purpose of this study was to provide an updated overview of all Apps exclusive to ophthalmology.
Methods:
This study was a quantitative analysis of Smartphone Apps exclusively designed for ophthalmic care. The Apple iPhone and Google play store were searched for eye care themed Apps. Any App related to eye treatment and management such as visual acuity screening, eye education, calculators, eBooks, Low Vision Aids were included in the study. Data on the purpose of the Apps, target end-users, validation, App usage, user ratings, and App developer qualifications were documented.
Results:
As of March 2020, a total of 131 Apps exclusively dedicated for eye care were identified. 53% (69/131) were available in iPhones, 44% (58/131) in Android smartphones, and 3% in both. 32% (41/131) Apps were designed for visual acuity (VA) screening, 13% (17/131) for eye relaxation exercises, 12% (15/131) for professional education, and the remaining for Apps detecting color blindness, low vision aids, and assistance and patient education. Among the 131 Apps, 6 (4.5%) Apps are claimed by the developers as validated.
Conclusion:
This study unveils a wide range of smartphone Apps exclusive to ophthalmology and suggests guidelines to choose an appropriate App. The study also highlights the importance of interdisciplinary collaboration in the design, development, and validation of such Apps.
Keywords: Apps in Ophthalmology, eye care apps, ophthalmic apps, smartphone applications
Mobile-based technology is likely to be the future of telemedicine. Outreach activities would be centered around the home than it is now.[1,2,3] Visual acuity (VA) and visual field screening Apps available in the App market are capable of detecting visual degradation even before they present to a healthcare professional (HCP). Apps could also make the patient feel more engaged and improve their compliance with treatment. In this regard, smartphone Applications (Apps) are capable of improving disease outcomes.
Globally, there is an increasing trend in the usage of smartphones. In 2010, the ASCRS (American Society of Cataract and Refractive Surgeons) survey showed that approximately 83% of members use smartphones to accomplish their professional responsibilities.[4] It was predicted that by 2022, 36% of mobile phone users in India would use a smartphone.[5] Therefore, widespread use of smartphones could enhance the potential of mhealth in early diagnosis and treatment of ophthalmic diseases. Several Apps were released in the last decade. However, ophthalmologists still find it difficult to adopt a good App into their day to day practice.[6]
It has been over a decade since Apps were designed exclusively for the ophthalmic purpose. Since then several studies have showed the potential scope of Apps in the near future.[1,2,3,4,5] Many studies have given a qualitative analysis of randomly selected Apps.[4,6,7] Little is discussed about the validity and usability of these Apps. HCPs are skeptical about the benefits of these Apps and may be reluctant to adopt it in their day to day practice. Additionally, there an increasing number of ophthalmic Apps dedicated to general public and non-eyecare professionals.[8,9,10,11,12,13,14,15,16,17,18] Therefore, it is also the responsibility of HCPs to guide patients to choose a suitable App. The purpose of this study was to provide an updated overview of all Apps exclusive to ophthalmology available in the market as of March 2020. In addition, the study explores the current trend in the usability and validation of these Apps.
Methods
This study was a quantitative analysis of Smartphone Applications exclusively designed for ophthalmic care.
Search methods: The Apple iPhone and Google play store were searched from Jan 2020 to March 2020 for eye care themed Apps. Keywords such as “eye”, “vision”, “vision screening” “visual acuity”, “sight”, “ophthalmology” and “optics” were used. Apps were also manually searched semantically by tracking similar Apps, developers, and healthcare products. All the Apps were manually analyzed by a single researcher and data was collected from the App description provided by its developers in the App store.
Inclusion criteria: Any App intended to perform preliminary ophthalmic assessments such as visual acuity screening, color vision screening, and support management such as eye education, calculators, eBooks, LVAs were included in the study.
Exclusion criteria: General medical and non-English Apps (translation unavailable) were excluded. Apps such as eye chart remotes, blue light filters, eye protectors, eye video games, eye color changers, eye product advertisements were also excluded from the study. General healthcare Apps that could be used in ophthalmology but not exclusively to ophthalmology such as torchlight, camera, voice recorders, and voice to text dictation Apps were also excluded. Apps that require specialized equipment such as slit lamp adaptors as add-ons were also excluded.
Data collection and Analysis: Data collection included year of publication, the purpose of App, target audience, whether the App was available for free or not, estimated number of downloads, average user ratings, reports on validation, and documented involvement of qualified professionals. A descriptive quantitative analysis was conducted and depicted as pie charts, bar, and line diagrams.
Results
Our initial search identified more than 700 Apps (both android and iPhone) with eye care themed search terms. As of March 2020, 259 Apps were selected after applying the inclusion and exclusion criteria mentioned in the methodology. Following this, 131 Apps were selected by the researcher to be relevant exclusively for ophthalmic practice after removing general healthcare Apps and Apps that require specialized equipment.
Target audience
32% (42/131) of the Apps were designed exclusively for Eye Care Professionals (ECP), that is, ophthalmologists and optometrists. 60% (78/131) of the Apps were developed for non-Eye Care Professionals (non-ECPs). Non-ECPs include eye-care health workers, and HCPs who may not be eyecare professionals, community healthcare outreach workers, volunteers, or the general public. In short non-ECPs are those who do not have any professional training in ophthalmology but could have obtained part-time training in using a particular App. For example, Portable Eye Examination Kit (PEEK) Acuity App can be used by either community outreach workers or individuals for self- assessment of visual acuity. Most of the Color blindness testing Apps are designed for self-assessment of color vision by taxi and truck drivers. Eight % (11/131) of the Apps are dedicated for both ECPs and non-ECPs.
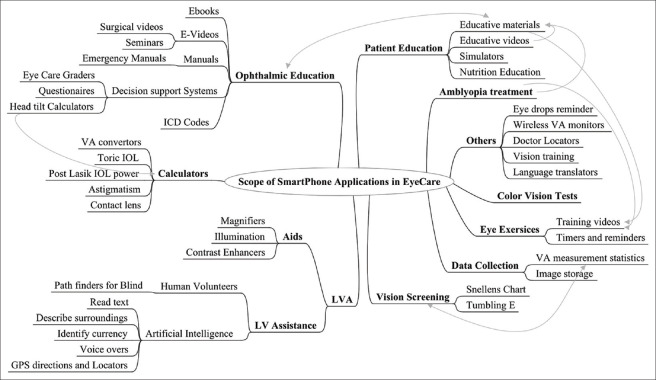
Distribution of Apps as per Operating system and utility [Figs. 1 and 2]
Figure 1.
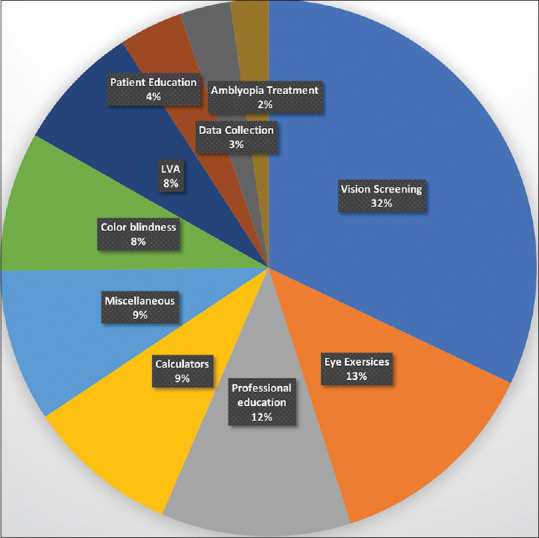
Distribution of Apps as per Utility
Figure 2.
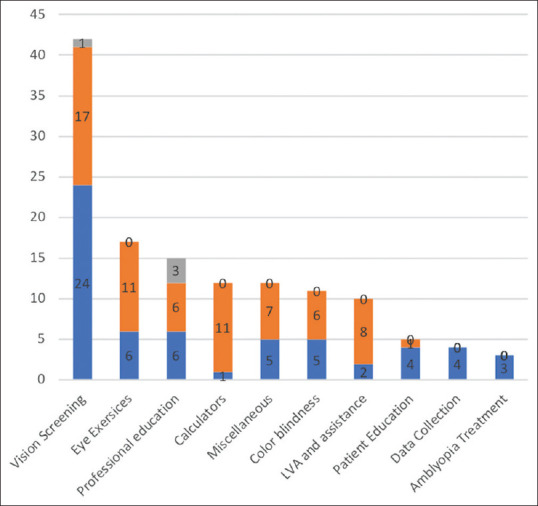
Distribution of Apps as per Operating System and Utility. Orange bars indicate iPhone and Blue bars indicate android operating system
53% (69/131) of the Apps were available on iPhones, 44% (58/131) in android smartphones, and 3% in both. 32% (42/131) were designed for Visual Acuity (VA) screening alone. Of the 42 Apps designed for VA screening, 7 Apps, additionally included other comprehensive eye exam tests also and 5 Apps were designed exclusively for near vision to detect Age-Related Macular Degeneration (AMD) and Diabetic Retinopathy (DR). 4 Apps documented VA measurement statistics also.
13% (17/131) of Apps were designed for eye relaxation exercises. About 12% (15/131) of the Apps were dedicated to professional education. These include eBooks, videos, and emergency manuals. Nine % (12/131) designed for eyecare decision support such as Intra Ocular Lens (IOL) power and Contact Lens (CL) calculators. Apps detecting color blindness, Low Vision Aids& Assistance, and Patient education includes 8%, 8%, and 4% each respectively.
Availability
76% (100/131) of the Apps are available for free. About 22% (30/131) need a monthly or annual payment ranging from 5-22 $ per month. Of the 30 Apps that required a payment, 23 belonged to iPhone, 5 to Android phones and 2 in both. In about 2% of Apps, developers provide a free trial of about 2 weeks.
The 10-year trend of Apps [Fig. 3]
Figure 3.
MindMap of Scope of Smartphone Applications in Eye Care
About 4 Apps dedicated to ophthalmology were first published in 2009. Since then the scope of Apps on ophthalmology has expanded from vision screening to data collection, amblyopia treatment, and low vision assistance. In 2018, 23 Apps were released for public use and further 19 were added in 2019.
Download rates
Download history was readily available in android phones. 45/131 Apps (34%) were downloaded over 10,000 times. Of these 3 Apps, Eye Exam App, Eye Care Plus App and Eye Test App, crossed 1 million downloads. All the three Apps were dedicated for general public. Of the 42 Apps developed exclusively for ECPs, three Apps crossed 100 thousand downloads. These include the Eye Hand Book (EHB), Color Blindness Test: Eye Color Vision App and Daltonism Test: Color Blindness Test App.
Reviewer rating
13 Apps had more than 500 reviewers. all of which were designed for non-ECPs. The Eye test App, designed for general public, received largest number of reviewers' ratings. Of the 42 Apps designed for ECPs, 30 Apps had less than 50 review rating. The App with maximum reviewer rating is Smart optometry App. The App had 50,000 downloads, of which 680 reviewers had rated the App.
Validation
Four % (6/131) Apps are claimed by the developers to have undergone some validation tests. 28% (37/131) of these Apps claim to have involved an ECP in the making of the App. Three Apps were designed by ECPs without developer involvement. About 10 Apps were endorsed by ECPs and healthcare institutions. My Vision Tracker (mVT) is the first ophthalmic App to be FDA approved in 2014. The features of these Apps are tabulated in Table 1.
Table 1.
Validated/Endorsed Apps with their Features
| Name of APP | Operating System | Target Audience | Purpose | Cost of the App |
| PEEK Acuity | Android | Mixed Users | VA screening | free |
| Kay iSight Test Professional | iPhone | ECP | VA screening in children | free |
| Community Eye | Android+iPhone | ECP | ECP education | free |
| Eye Hand Book | Android | ECP | Multi-purpose | free |
| Smart Optometry - Eye Tests for Professionals | Android+iPhone | ECP | VA screening | free |
| My Vision Tracker (mVT) | iPhone | ARMD and DR Patients | Home vision screening | 8.95$/month |
PEEK Acuity App
PEEK Acuity App has undergone several validation tests under different circumstances. Peek acuity App was developed by the International Centre for Eye Health, Department of Clinical Research in London. The same team compared test–retest variability (TRV) and measurement time, with that of the Snellen and ETDRS-based tumbling E Log MAR chart in private clinics and rural houses in Kenya. The study concluded that the PEEK Acuity smartphone test is capable of accurate and repeatable acuity measurements in either set in the elderly population.[8] Few other studies, including a cluster randomized controlled Kenya, found that the App is an efficient tool for school screening purposes also.[9,10,11,12] The App was showed promising results when used by non-ophthalmic staff in emergency department.[13] Similarly, PEEK App was also tested amidst the Chinese and Australian population revealing promising results.[14]
Kay ISight Test Professional App
This App measures near and distant visual acuity by using the LogMAR chart. It provides various distances from 33 cm to 6 m, depending on which the size of the chart could be altered. Kay's picture optotypes are used for young children and those with a learning disability. The App has undergone a couple of validation tests in the UK and is suggested to be a reliable tool to assess vision in pre-school children.[15,16] Another study concluded that LogMAR crowded Kay picture test is a useful tool in clinical practice.[17,18]
Community Eye Care App
The App provides free online and offline access to peer-reviewed articles in community eye health. The App aims to improve standardization and enable easy access to eye care knowledge for all categories of eye care beginning from ophthalmology, optometry, eye nursing, and eye care delivery. The App is supported by several well-known NGOs such as the Conrad Hilton Foundation, Sightsavers, Orbis, and Seva Foundation.[19,20]
Eye Hand Book (EHB) App
EHB is both a diagnostic and treatment reference App. EHB serves as a one-stop-shop for multiple needs of ophthalmic practice. It offers a dozen features to both ophthalmologists and eye care workers such as educational videos (for both patients and professionals), calculators, testing tools, practice efficiency tools, coding tools, journal portals, treatment reference manuals, discussion boards, etc. The EHB is one of the most popular Apps amidst ECPs with over half a million downloads and 25 thousand active users.[21] Several studies have mentioned and endorsed the use of EHB.[7,22]
Smart Optometry- Eye Tests for Professionals App
This App incorporates various vision screening tests including color vision, near vision, amblyopia, Worth four dot test, Hirschberg, Amsler grid, etc. The App is available in 11 languages in both android and iPhone. Developers of the App claim it to be fast, easy to use with results that are accurate, reliable, and clinically validated. It is one of the most downloaded App by healthcare professionals with over 50,000 downloads.[23]
mVT (My Vision Track) App
mVT App can easily convert the Apple smartphones into a medical device that can track the progression of vision damaging diseases such as age-related macular degeneration and diabetic retinopathy. Patient test data are automatically uploaded to a Physician's Portal where licensed eye-care professionals can monitor all patient test results. It has been validated as a remote monitoring tool at home to track treatment effects and to detect disease condition changes.[24] Alleye is another App which also FDA approved for monitoring maculopathy. Both are available in iPhone bd cost about 9 $/month.[25]
Professional Education and Decision Support Apps
26 out of 131 (20%) Apps were dedicated to ophthalmic education and decision support in the form of calculators. None of the Apps were validated by any HCP groups. Three were endorsed, all of which were designed by institutions. A majority of HCPs did not provide any reviewer rating. The maximum reviewer participation was 121 for Ophthalmology and Optometry Guide App which had a download rate of 10000. Eye-hand Book (EHB) is one of the most popular eyecare educational App with maximum of 1 million downloads. The App has an average reviewer rating of 3.8 stars in Android phones and four stars in iPhone.
Eye Exercise And Training Plan Apps
13% of the Apps are dedicated to general public for eye exercises and eye training plans. All these Apps are available for free. But, they are yet to be validated or endorsed. Eye Exercises & Eye Training Plans - Eye Care Plus App contains more than 50 exercises, 12 eye tests to track vision improvement and a training calendar. The App has over two million downloads with a reviewer rating of 4.6 among 27000 reviews.
Apps as Low Vision Aids (LVA) and Low Vision Assistance (LVAsst)
About 10 Apps (8%) are dedicated to LVA and LVAsst, 5 in each [Table 2]. All are available in iPhone alone and none have been validated. The App “BE My Eyes” functions based on Audi-Visual interaction between visually impaired and a global community of volunteers who provide remote assistance via a live video. Although not validated, the App has received several awards such as 2020 Dubai Expo Global Innovator, 2018 Winner of Google Play Awards - Best Accessibility Experience and 2018 Winner of AbilityNet Accessibility Award at the Tech4 Good Awards.[26,27]
Table 2.
Author’s Picks: Some interesting Apps (not yet validated)
| Name of APP | Operating System | Purpose | Interesting Features |
|---|---|---|---|
| Exclusively For ECPs | |||
| Eye Emergency Manual | Android | e-Book + Clinical Decision support (CDS) | Quick and simple guide to manage eye emergencies |
| Eye Grader | Android | e-Book + (CDS) | Instant access to all Grading scales |
| Optiexpert™ | Android | CDS for Contact lens (CL) prescription | Calculators for Toric and multifocal CL prescription |
| ViaOpta Simulator | Android | Patient Education | Simulates vision loss in different diseases |
| Eye Pro | iPhone | CDS | Toric IOL power Calculator |
| VA Converter | iPhone | CDS | Auto calculates VA in different scales |
| Astigmaster | iPhone | CDS | Surgery Induced Astigmatism Calculator |
| Eye Diagnosis | Android | Data Collection | Support visualization and organization of eye photos by name, date and laterality. |
| For General public | |||
| Eye Exam Pro | Android | Home vision Screening | Also provides VA measurement statistics like history, charts and trends (one time cost Rs. 183 per download) |
| Eyeque Insight | iPhone | Patient Education | Patented technology |
| Lazy Eye Exercises | Android | Amblyopia Management | Send reminders and treats amblyopia via games |
| Magnifying Glass with Light | iPhone | LVA | Digital magnifier |
| Sullivan+ | Android | LVA | Magnifier + uses Artificial Intelligence (AI) to recognize Text, face and images |
| Be My Eyes | iPhone | LVA + LVAssistance | Also connects to support groups |
| Eye-D | iPhone | LVA + LVA Assistance | AI, both aid and assistance, available Indian language also |
| Color Blind Eye Exam Test | iPhone | Color Blindness Screening | Self-screening by truck drivers and taxi cab drivers |
Discussion
Purpose of the study is to give a comprehensive overview of all Apps currently available, their uses in eye care and their complex interconnections. Apps exclusive to eye care were first released in 2009. By 2013, around 340 Apps were released in both Android and iPhone using eye care themed concepts.[28] Few studies have been published in literature regarding Apps exclusive to ophthalmology.[6,7,22,23,29,30] Attempts were made to broadly categorize the Apps based on user needs and qualitatively describe selected Apps in ophthalmic practice from a clinicians' perspective. A study by Akkara and Kuriakose has qualitatively analyzed smartphone applications specifically for LVA.[30] Two studies have quantitatively analyzed smartphone Apps in ophthalmology.[6,13] The first comprehensive quantitative analysis of Apps in ophthalmology was published in 2015. This study identified about 182 Apps from the iPhone alone.[6] The second was focused on using such Apps in emergency conditions.[13]
This study portrays in-depth quantitative analysis of all Apps currently designed exclusively for ophthalmic practice. Several search words resembling ophthalmological themes but not intended for healthcare purposes were excluded from the study to avoid cluttering. The 131 Apps thus identified in the study were categorized into 10 categories based on their scope of practice in ophthalmology. Each category is further divided into subcategories based on its intended use. Every App understudy was designed to cater one or more application each of which are interrelated to each other. Apps like EHB caters a wide variety of ECP needs beginning from vison screening tools, IOL power calculators, and educative materials to support evidence based decision making. Therefore the authors have designed a MindMap instead of a multilevel list or table to illustrate complex interrelations via linking arrows between various categories and sub categories [Fig. 4].
The study also adds light to the feasibility and reliability of using such Apps including cost, validity tests, and download rates. The study exposes the fact that less than a quarter of the Apps exclusively designed for Eye care involves an ECP in the design.
Download rates and reviewer rating provide information about the readiness of the ECPs to use the Apps. Download rates are an indirect indication of awareness of end-users about the existence of an App and an opportunity to try using the APP. Despite hundreds of Apps created, the usage of Apps in day to day practice as seen by download rates is very low, especially among HCPs. One of the main reasons for this is the lack of awareness among HCPs regarding the benefits of Apps. Many others are confused about choosing the right App. HCPs are also doubtful about the reliability of such Apps.[2,6] Reviewer rating is one of the ways to judge the usability of an App. The quality of an App is measured in terms of ratings provided. Poor review ratings may be attributed to a lack of validity tests and usability tests on these Apps. So far only 2 Apps has been FDA approved in ophthalmic practice.[24,25]
This study elaborates on the scope of mHealth Applications in ophthalmology and provides an updated version of its uses [Table 2]. It identifies lacunae in designing, validating, and adoption of mhealth in day to day practice. Most of the Apps were developed without professional ophthalmologist or a professional App designer. The study reveals opportunities to HCPs and institutions in promoting mHealth. It unfolds reasons ECPs' reluctance to choose and adopt Apps such as lack of validation, endorsement, or peer review. This is further enhanced by poor participation from ECPs in the making, reviewing, validation, and endorsement of Apps.
The study could not provide a qualitative analysis of each App as describing and evaluating each App is a study by itself. However, the authors plan to conduct and recommend evaluation of individual Apps in the future. The study has excluded general Apps that could also be used in ophthalmic practice as it is beyond the scope of this paper. Apps designed for LVA and LV Assistance, amblyopia management, eyedrops reminders, vision simulators etc., are a domain by themselves that needs special attention.
The researchers recommend active participation from individuals (ECPs and general public) by sharing their experience with the App via review ratings and comments. Current validation methods are inadequate as it needs validation of scientific concepts used in the App and usability factors. Healthcare institutions must promote strong interdisciplinary collaboration between eye care professionals and software developers in the designing, validation, and updating of an App. Frequent workshops could educate and train ECPs to adopt mhealth technology into their routine practice. The study also aims to provide guidelines to ECPs to choose the apt App and encourage them to evaluate the usability of Apps. A well trained ECP can, in turn, educate patients, stay connected, and suggest suitable Apps that could empower patients in managing their disease condition or even diagnose it in their neighborhood.
Concerning professional educational Apps such as EHB and Eye Emergency Manual App, institutions, and/or individuals could endorse and make suggestions. Like research papers, Apps dedicated to professional use must also be peer-reviewed. Further studies are needed to understand the readiness and concerns of ECPs in adopting mhealth.
Conclusion
Our study unveils a wide range of smartphone Apps exclusive to ophthalmology. Guidelines to choose an appropriate App are suggested. We also emphasize on the importance of interdisciplinary collaboration in the design, development, and validation of such Apps.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Rahme RJ, Fishman AJ, Hunt BH, Bendok BR. The future is now: Smartphones to join scalpels and stethoscopes? Neurosurgery. 2012;70:N19–20. doi: 10.1227/01.neu.0000413224.88090.66. [DOI] [PubMed] [Google Scholar]
- 2.Istepanian R, Philip N, Wang XH, Laxminarayan S. Non-telephone healthcare: The role of 4G and emerging mobile systems for future m-health systems. Stud Health Technol Inform. 2004;103:465–70. [PubMed] [Google Scholar]
- 3.Low DK, Pittaway AP. The 'iPhone' induction - A novel use for the Apple iPhone. Paediatr Anaesth. 2008;18:573–4. doi: 10.1111/j.1460-9592.2008.02498.x. [DOI] [PubMed] [Google Scholar]
- 4.Davis EA, Hovanesian JA, Katz JA, Kraff MC, Trattler WB. Professional life and the smartphone. Cataract Refract Surg Today. 2010:21–2. [Google Scholar]
- 5.Statista.com [Internet]. Smartphone users in India - Penetration rate as share of mobile phone users 2014-2022. [[Updated 2019 Oct 24; cited 2020 Apr 09]]. Available from: https://www.statista.com/statistics/257048/smartphone-user-penetration-in-india/
- 6.Cheng NM, Chakrabarti R, Kam JK. iPhone applications for eye care professionals: A review of current capabilities and concerns. Telemed J E Health. 2014;20:385–7. doi: 10.1089/tmj.2013.0173. [DOI] [PubMed] [Google Scholar]
- 7.Moradian S, Safi S. Application of mobile phones in ophthalmology. J ophthalmic Vis Res. 2015;10:200–5. doi: 10.4103/2008-322X.163775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bastawrous A, Rono HK, Livingstone IA, Weiss HA, Jordan S, Kuper H. Development and validation of a smartphone-based visual acuity test (peek acuity) for clinical practice and community-based fieldwork. JAMA Ophthalmol. 2015;133:930–7. doi: 10.1001/jamaophthalmol.2015.1468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Brady CJ, Eghrari AO, Labrique AB. Smartphone-based visual acuity measurement for screening and clinical assessment. JAMA. 2015;314:2682–3. doi: 10.1001/jama.2015.15855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dhanesha U, Polack S, Bastawrous A, Banks LM. Prevalence and causes of visual impairment among school children in Mekelle, Ethiopia. Cogent Med. 2018;5:1554832. [Google Scholar]
- 11.Zhao L, Stinnett SS, Prakalapakorn SG. Visual acuity assessment and vision screening using a novel smartphone application. J Pediatr. 2019;213:203–10. doi: 10.1016/j.jpeds.2019.06.021. [DOI] [PubMed] [Google Scholar]
- 12.Rono HK, Bastawrous A, Macleod D, Wanjala E, Di Tanna GL, Weiss HA, et al. Smartphone-based screening for visual impairment in Kenyan school children: A cluster randomized controlled trial. Lancet Glob Health. 2018;6:e924–32. doi: 10.1016/S2214-109X(18)30244-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pathipati AS, Wood EH, Lam CK, Sáles CS, Moshfeghi DM. Visual acuity measured with a smartphone app is more accurate than Snellen testing by emergency department providers. Graefe's Arch Clin Exp Ophthalmol. 2016;254:1175–80. doi: 10.1007/s00417-016-3291-4. [DOI] [PubMed] [Google Scholar]
- 14.Han X, Scheetz J, Keel S, Liao C, Liu C, Jiang Y, et al. Development and validation of a smartphone-based visual acuity test (vision at home) Transl Vis Sci Technol. 2019;8:27. doi: 10.1167/tvst.8.4.27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dawkins A, Bjerre A. Do the near computerised and non-computerised crowded Kay picture tests produce the same measure of visual acuity? Br Ir Orthopt J. 2016;13:22–8. [Google Scholar]
- 16.Kay HA. New method of assessing visual acuity with pictures. Br J Ophthalmol. 1983;67:131–3. doi: 10.1136/bjo.67.2.131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Northway N, Panesar G, McCulloch D, McKay R. A validation of iSight app in pre-school vision screening Presented at the XIV Biennial Meeting of the Child Vision Research Society, 17–19 June 2013, Ontario, Canada. [[Last accessed 2013 Sep 08]]. Available from: http://cvrsoc.org/docs/CVRS2013-web.pdf pg 34 .
- 18.Elliot MC, Firth AY. The logMAR Kay picture test and the logMAR acuity test: A comparative study. Eye. 2009;23:85–8. doi: 10.1038/sj.eye.6702990. [DOI] [PubMed] [Google Scholar]
- 19.Wolvaardt E. The community eye health journal in your pocket. Community Eye Health. 2019;32:61. [PMC free article] [PubMed] [Google Scholar]
- 20.International Agency For Prevention of Blindness (IAPB). org [Internet]. England: The Community Eye Health Journal is now available via App. [[updated 2019 November 13; cited 2020 Apr 14]]. Available from: https://www.iapb.org/news/the-community-eye-health-journal-is-now-available-via-app/
- 21.Lord K, Shah VA, Krishna R. The Eye Handbook: A mobile app in ophthalmic medicine. Mo Med. 2013;110:49–51. [PMC free article] [PubMed] [Google Scholar]
- 22.Chhablani J, Kaja S, Shah VA. Smartphones in ophthalmology. Indian J Ophthalmol. 2012;60:127–31. doi: 10.4103/0301-4738.94054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Charlesworth JM, Davidson MA. Undermining a common language: Smartphone applications for eye emergencies. Med Devices (Auckl) 2019;12:21–40. doi: 10.2147/MDER.S186529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wang YZ, He YG, Csaky KG, Mitzel G, Hernandez K, Zhang S, et al. Diabetic retinopathy and the my vision track® App (DRAMA) study. Invest Ophthalmol Vis Sci. 2015;56:516. [Google Scholar]
- 25.International Agency For Prevention of Blindness (IAPB). org [Internet] England: The Community Eye Health Journal is now available via App; [[updated 2019 November 13; cited 2020 Apr 14]]. Available from: https://www.iapb.org/news/the-community-eye-health-journal-is-now-available-via-app/ [Google Scholar]
- 26.Wiberg JH. Be My Eyes. Lend your eyes to the blind. Retrieved September. 2016;15:2016. [Google Scholar]
- 27.Avila M, Wolf K, Brock A, Henze N. Remote assistance for blind users in daily life: A survey about be my eyes. In Proceedings of the 9th ACM International Conference on PErvasive Technologies Related to Assistive Environments. 2016 Jun 29;:1–2. [Google Scholar]
- 28.Tahiri RJ, El MS, Dupont-Monod S, Baudouin C. Smartphones in ophthalmology. Journal Fr Ophtalmol. 2013;36:499–525. doi: 10.1016/j.jfo.2013.02.002. [DOI] [PubMed] [Google Scholar]
- 29.Akkara JD, Kuriakose A. Innovative smartphone apps for ophthalmologists. Kerala J Ophthalmol. 2018;30:138–44. [Google Scholar]
- 30.Akkara JD, Kuriakose A. Smartphone apps for visually impaired persons. Kerala J Ophthalmol. 2019;31:242–8. [Google Scholar]