Abstract
Purpose:
To evaluate the impact of the COVID-19 pandemic and the national lockdown on the demographic and clinical profile of patients presenting with ocular trauma.
Methods:
In this retrospective, hospital-based, comparative analysis, patients presenting to the emergency department with ocular trauma in the following COVID-19 period (March 25, 2020 to July 31, 2020) were compared with patients in the pre-COVID-19 period (March 25, 2019 to July 31, 2019).
Results:
Overall, 242 patients (COVID-19 period: 71 and pre-COVID-19 period: 171) presented with ocular trauma. The mean age of the patients in COVID-19 and pre-COVID-19 periods were 26.7 ± 17.3 and 34.1 ± 20.3 years, respectively (P = 0.008). A majority of patients (68.6%) in both groups were from the rural background. Home-related injuries were common in the COVID-19 period (78.8%) as compared to pre-COVID-19 period (36.4%) (P < 0.0001). Iron particles (29.5%) were the common inflicting agents in the COVID-19 period while it was plant leaves (25.5%) in the pre-COVID-19 period. The most common ocular diagnosis was open globe injury (40.8%) in the COVID-19 period and microbial keratitis (47.9%) in the pre-COVID-19 period. Surgical intervention was required in 46.4% of patients in the COVID-19 period and 32.1% of patients in the pre-COVID-19 period (P = 0.034).
Conclusion:
During the COVID-19 period, there was a significant decline in the number of patients presenting with ocular trauma. In this period, a majority of patients sustained ocular trauma in home-settings. About half the patients required surgical intervention which was most commonly rendered in the form of primary wound repair.
Keywords: Closed globe injury, COVID-19, national lockdown, ocular trauma, open globe injury, pandemic
The World Health Organization declared the outbreak of a pandemic caused by Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) on March 11, 2020.[1] The first case had been reported in Wuhan, Hubei province in China in late 2019 and within the next two months, it had spread to 113 countries including India.[2,3,4] This virus is highly contagious and manifests as mild-to-moderate respiratory tract infection, but in selected groups it may lead to acute respiratory distress syndrome, cytokine storm, disseminated intravascular coagulation, and multi-organ failure. Unavailability of an effective vaccine and therapeutic agents against this novel virus has increased the virulence of the disease attack. Hence, the Indian Government was one of the few governments across the globe to implement early and strict nationwide lockdown that began on March 25, 2020. The first two phases of complete lockdown extended from March 25, 2020 to May 3, 2020.[5,6,7,8] Barring emergency services, all other services were suspended. This was followed by gradual relaxations in phases over the next few months.
Ocular trauma is an important and preventable cause of visual impairment in both developing and developed countries.[9] Work-related trauma and road traffic accident remain the important causes of ocular injuries.[9,10,11] Due to the implementation of lockdown, the fear of getting infected with COVID-19, and in keeping with social distancing measures, people remained confined to their homes. This probably had a significant impact on the risk and pattern of ocular trauma during this period. Secondly, routine out-patient departments across hospitals and clinics in India were shut down initially during the lockdown.[7,12] Due to lack of guidelines in the initial phase of the lockdown, most of the ophthalmologists were clueless as how to keep their hospitals functional. Hence, they ceased their clinical services at their respective locations. In a survey involving 1260 ophthalmologists to study the impact of the lockdown on ophthalmic practices, 72.5% of the respondents were not seeing any patients during the lockdown period.[7] This, in turn, led to limited accessibility of health care systems to patients. Hence, this study was conducted to evaluate the impact of the COVID-19 pandemic and the national lockdown on ocular trauma at a tertiary eye care institute.
Methods
In this retrospective, hospital-based, comparative study, we included all the patients presenting with ocular trauma to the emergency department of our tertiary eye care institute from March 25, 2020 to July 31, 2020 and compared them with those from the same period of the previous year, i.e., March 25, 2019 to July 31, 2019. We excluded patients with inadequate data on the injury and patients with symptoms of COVID-19 as they were referred to the other centre with a COVID-19 facility. Since ours is primarily an eye care institute patients with polytrauma having orbital injuries requiring a multidisciplinary approach were referred to nearby multispeciality hospital and hence they were not included in this study. The Institutional Ethics Committee approved the study and it was conducted in full accord with the tenets of the Declaration of Helsinki. It is a routine practise to obtain a written informed consent from all patients presenting to our institute for participation in research, which also includes consent for the protection of electronic data privacy. No identifiable variables of the patient were used during the analysis of data. Records of all the patients were retrieved from the Electronic Medical Record (EMR) system. Data retrieved included age, sex, residence (rural/urban), mode of injury, place of injury (home/work/road traffic accident), prior intervention, time interval between injury to presentation, clinical presentation, ocular diagnosis and treatment modalities.
During the COVID-19 period, our institute constituted a task force team for COVID-19 to formulate a standard operating procedure for functioning of the institute based on guidelines issued by the Ministry of Health and Family Welfare, Government of India and the All India Ophthalmological Society (AIOS), which is a professional body of Ophthalmology in India.[8] These included reduction of the workforce, adequate personal protective equipment (PPE) for all on-duty staff, regular sanitization of instruments and furniture, and adequate social distancing norms in waiting halls. In our institute, we divided our clinical and non-clinical support staff into three teams that rotated twice a week and continued to provide care to all patients presenting to the hospital during the lockdown period. All the patients were asked if they had any symptoms of COVID-19 and temperature was recorded with an electronic thermometer at the hospital entry. Patients were categorized into emergency or routine patients based on operational guidelines formulated by the All India Ophthalmological society guidelines.[8] We strictly followed a policy of one patient with one attendant in one room.
All patients underwent a comprehensive eye evaluation at presentation. We classified ocular injuries into open globe injuries and closed globe injuries.[13] In patients with open globe injuries, we planned primary repair under general anesthesia on an emergency basis. Patients presenting with infectious keratitis underwent corneal scraping at presentation. Smears were examined for Gram's, Giemsa, and 10% potassium hydroxide mounts. The remaining sample was inoculated on blood agar (5% sheep blood) and incubated at the appropriate temperature and atmospheric conditions.
Statistical analysis
Data were collected and stored in a spreadsheet using Microsoft Excel software. Data management and coding was done in Excel. Data were analyzed using Version SPSS 16.0 (IBM Inc., Chicago, IL, USA). Descriptive analysis was primarily carried out, where categorical variables were presented in the form of frequencies and percentages and continuous variables in the form of mean ± standard deviation. A Pearson's Chi-square test was used to analyze the difference between the groups. A value of P < 0.05 was considered statistically significant.
Results
During the study period, a total of 242 patients (pre-COVID-19: 171 and COVID-19: 71) presented with a history of ocular trauma to the emergency department of our institute. The mean age of the study population was significantly lower in the COVID-19 period (26.7 ± 17.3 years) as compared to the pre-COVID-19 period (34.1 ± 20.3 years) (P = 0.008) [Table 1]. Seven (9.8%) patients were >50 years in the COVID-19 period while 40 (23.4%) patients were >50 years in the pre-COVID-19 period (P = 0.015). The distribution of gender and area of residence was comparable in both the groups. The time interval between sustaining an injury and presentation to our institute was higher in the COVID-19 period (10.2 ± 18.6 days) as compared to the pre-COVID-19 period (8.4 ± 22.9 days). However, this difference was statistically not significant (P = 0.31). A proportion of patients presenting with prior consultation, medical management and surgical management done elsewhere, were comparable in both the groups.
Table 1.
Demographic profile of the study population (Numbers in brackets indicate percentage)
| Parameters | PRE-COVID (n=171) | COVID (n=71) | P | |
|---|---|---|---|---|
| Mean Age (years) | 34.1±20.3 | 26.7±17.3 | 0.008 | |
| Age-groups (years) | 0-16 | 38 (22.2) | 19 (26.7) | 0.44 |
| >16-50 | 93 (54.3) | 45 (63.3) | 0.19 | |
| >50 | 40 (23.4) | 7 (9.8) | 0.015 | |
| Gender | Male | 117 (68.4) | 53 (74.6) | 0.69 |
| Female | 54 (31.6) | 18 (25.4) | ||
| Residence | Urban | 57 (33.3) | 21 (29.5) | 0.56 |
| Rural | 114 (66.7) | 50 (70.5) | ||
| Laterality | Right Eye | 77 (45) | 27 (38) | 0.22 |
| Left Eye | 86 (50.3) | 43 (60.6) | ||
| Bilateral | 8 (4.7) | 1 (1.4) | ||
| Time Interval between injury & presentation (days) | 8.4±22.9 | 10.2±18.6 | 0.316 | |
| Prior to presentation | Consultation Taken | 127 (74.2) | 48 (67.6) | 0.29 |
| Medical Management | 120 (70) | 45 (63.3) | 0.3 | |
| Surgical Management | 7 (4) | 3 (4.2) | 0.96 | |
Monthly variation
After announcement of the lockdown, no patient presented to the emergency department in the initial 1 week period [Table 2]. However, there was a gradual increase in the number of patients on a monthly basis with 63.3% (n = 55) patients presenting in the months of June and July 2020 [Fig. 1]. The difference in the number of patients between both the groups was statistically significant for the months of March (P = 0.015), April (P = 0.012) and July (P = 0.0008).
Table 2.
Distribution of patients with trauma according to months and place of injury
| Month | Period | Home | Work | Road Traffic Accidents | Total |
|---|---|---|---|---|---|
| March | pre-COVID | 8 (36.3) | 13 (59) | 1 (4.5) | 22 (12.8) |
| COVID | 0 (0) | 0 (0) | 0 (0) | 0 | |
| April | pre-COVID | 16 (32) | 30 (60) | 4 (8) | 50 (29.2) |
| COVID | 10 (100) | 0 (0) | 0 (0) | 10 (14.1) | |
| May | pre-COVID | 17 (43.5) | 19 (48.7) | 3 (7.6) | 39 (22.8) |
| COVID | 12 (75) | 3 (18.7) | 1 (6.2) | 16 (22.5) | |
| June | pre-COVID | 11 (35.4) | 17 (54.8) | 3 (9.6) | 31 (18.1) |
| COVID | 12 (75) | 4 (25) | 0 (0) | 16 (22.5) | |
| July | pre-COVID | 10 (34.4) | 14 (48.2) | 5 (17.2) | 29 (16.9) |
| COVID | 22 (75.8) | 5 (17.2) | 2 (6.8) | 29 (40.8) |
Numbers in brackets indicates percentages
Figure 1.
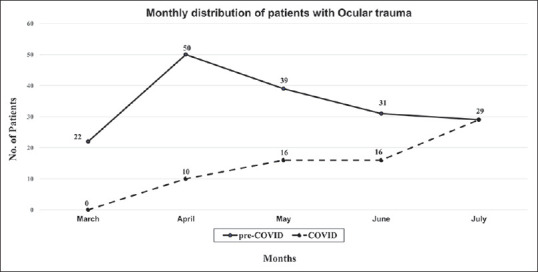
Monthly variation in the patient presentation with Ocular trauma in pre-COVID and COVID era
Place and mode of injury
During the COVID-19 period, 56 (78.8%) patients sustained ocular trauma at home as compared to 62 (36.4%) patients in the pre-COVID-19 period (P < 0.0001). On the contrary, in the COVID-19 period, 12 (16.9%) patients suffered ocular trauma at the workplace as compared to 93 (54.7%) patients in pre-COVID-19 period (P < 0.0001). Only 3 patient had ocular trauma due to road traffic accidents in COVID-19 period as compared to 16 patient in pre-COVID-19 period (P = 0.17). Two of three patient in COVID-19 period had road traffic accident in month of July when unlocking process started. The most common inflicting agent of injury in the COVID-19 period was iron particles (29.5% patients), while in the pre-COVID-19 period, it was plant leaves (25.5% patients). Details of various trauma inflicting agents are listed in Table 3.
Table 3.
Various Trauma inflicting agents
| Trauma Inflicting Agent | Pre-COVID (n=171) | COVID (n=71) | ||||
|---|---|---|---|---|---|---|
| Home | Work Place | RTA | Home | Work Place | RTA | |
| Metallic (Iron) | 12 | 16 | 6 | 10 | 9 | 2 |
| Plant Leaf | 15 | 24 | 4 | - | - | - |
| Wooden Stick | 6 | 10 | 1 | 12 | - | - |
| Construction Site Related (Brick, Stone, Soil) | 5 | 15 | 4 | 2 | 2 | - |
| Chemical Injuries (Lime, Cement, Color) | 7 | 8 | - | 5 | 1 | 1 |
| Sharps & Daily Use (Pen, Glass, Rubber, Plastic, Leather, Fan) | 8 | 6 | - | 7 | - | - |
| Sports Injury (Tip-cat, Tennis Ball, Shuttle Cock) | 3 | - | 10 | - | - | |
| Human Inflicted (Hand, Finger Nail, Fist, Self-Fall) | 3 | 6 | 1 | 3 | - | - |
| Animal Related (Cow Horn, Insect, Cow Tail) | - | 7 | - | 3 | - | - |
| Blast Injuries (Battery Blast, Cracker, Cooker Blast) | 4 | - | - | 4 | - | - |
RTA: Road Traffic Accident
Ocular diagnosis
In the COVID-19 period, 29 (40.8%) patients sustained open globe injuries, 24 (33.8%) sustained closed globe injuries and 9 (12.7%) patients sustained chemical injuries and microbial keratitis each. However, in the pre-COVID-19 period, 82 (47.9%) patients had microbial keratitis following trauma, 47 (27.5%) patients had open globe injuries, 29 (16.9%) had closed globe injuries and 13 (7.7%) patients had chemical injuries. The number of patients presenting with microbial keratitis was higher in the pre-COVID-19 period as compared to the COVID-19 period (P = 0.0001). Contrarily, the number of patients presenting with closed globe injuries was higher in the COVID-19 period as compared to the pre-COVID-19 period (P = 0.003). Traumatic endophthalmitis was diagnosed in 8 (4.6%) eyes and 7 (9.8%) eyes in pre-COVID-19 and COVID-19 periods, respectively. Retained intraocular foreign bodies were present in 2 (1.1%) eyes and 1 (1.4%) eye in the pre-COVID-19 and COVID-19 periods, respectively.
Management
Thirty-three (46.4%) patients in the COVID-19 period and 115 (67.2%) patients in the pre-COVID-19 period were treated conservatively with medication. In the COVID-19 period, surgical intervention was carried out on 33 (46.4%) patients, whereas in the pre-COVID-19 period, a total of 55 (32.1%) patients underwent surgical intervention as the management for ocular trauma (P = 0.034). In both the groups, primary wound repair was the most common type of surgical intervention carried out in 24 (72.7%) and 46 (83.6%) patients respectively. Details pertaining to various surgical interventions are listed in Table 4. Additionally, two patients underwent foreign body removal during pre-COVID period while one patient in COVID period refused for any surgical intervention.
Table 4.
Details of management in both the groups
| Management | Pre-COVID (n=171) | COVID (n=71) | P |
|---|---|---|---|
| A) Conservative (Medical) | 115 (67.2) | 33 (46.5) | 0.002 |
| B) Surgical | 55 (32.1) | 33 (46.5) | 0.034 |
| 1) Primary Wound Repair (Total) | 46 (26.9) | 24 (33.8) | 0.28 |
| i) Corneal Tear Repair | 36 (21) | 18 (25.3) | 0.46 |
| ii) Scleral Tear Repair | 5 (2.9) | 4 (5.6) | 0.31 |
| iii) Eyelid Tear Repair | 5 (2.9) | 2 (2.8) | 0.96 |
| 2) Pars Plana Vitrectomy | 8 (4.6) | 11 (15.5) | 0.004 |
| 3) Pars Plana Lensectomy/Lens Aspiration | 9 (5.2) | 10 (14) | 0.02 |
Numbers in brackets indicates percentages
Among patients with microbial keratitis, fungus was the causative agent in 37 (45.1%) patients, bacteria in 26 (31%) patients, while no organism was identified in 19 (23.2%) patients on microbiological workup in the pre-COVID-19 period. In the COVID-19 period, fungus was isolated in 4 (44.4%) patients, bacteria in 2 (22.2%) patients and no organism was detected in 3 (33.3%) patients. Most of the patients diagnosed with microbial keratitis were managed with medical treatment in both the study groups. In the pre-COVID-19 period, 5 (6.1%) patients needed therapeutic penetrating keratoplasty (TPK) and they successfully underwent surgery. However, in the COVID-19 period, 3 (33%) patients needed TPK but none of these patients could undergo the surgery due to lack of availability of donor corneal tissue. Six patients (COVID-19: 5, pre-COVID-19: 1) did not consent for surgery and were lost to follow-up. All of these patients were diagnosed with open globe injury and planned for primary wound repair.
Discussion
The corona virus pandemic has not only affected routine ophthalmic practices in multiple ways, but has also posed challenges in patients seeking ophthalmic care.[7,8,9,10,11,12,14,15] Patients presenting with routine ophthalmic check-up have reduced significantly. However, patients with ocular trauma requiring emergency ophthalmic attention were still being attended by ophthalmologists at tertiary eye care and government institutes.[7] To the best of our knowledge, this is the largest reported series of patients presenting to emergency departments with ocular trauma in the COVID-19 period from India. During the COVID-19 period, we witnessed a significant decline in the total number of ocular trauma cases, a change in the setting where injury was sustained, delayed time of presentation, and a higher number of patients requiring surgical intervention, in comparison with the pre-COVID-19 period.
A majority of the patients (67.7%) included in this study were from a rural background. Since farming is the main source of income, injury with plant leaves was commonly reported in the pre-COVID 19 period. However, during the COVID-19 period, strangely, none of the patients presented with plant leaf injury. This could be due to fear of the pandemic and the strict lockdown measures that were imposed compelling people to stay at home. In this study, we also observed that patients with ocular trauma in the COVID-19 period had delayed presentation. In a survey conducted during the COVID-19 period, of 1260 ophthalmologists who participated, only 287 (22.7%) ophthalmologists were managing emergencies and most of them were based in government and municipal hospitals or ophthalmic institutes.[7] Hence, patients had difficulty in accessing health care services. The mean age of the patients in the COVID-19 period was less than that of the patients in the pre-COVID-19 period because people more than 50 years of age presenting with ocular trauma were significantly fewer in the COVID-19 period. People belonging to the older age group are more vulnerable to COVID-19 infection with high morbidity and mortality related to the disease. Hence, people belonging to this age group probably took extreme precautions even during the unlock period, restricting themselves to their home environment.
During the period of complete lockdown that extended from March 25, 2020 to May 3, 2020, only 10 patients presented with ocular trauma and all these injuries were sustained at home. Injuries sustained at home were significantly higher than workplace injuries in the COVID-19 period. Similar rise in ocular trauma sustained at home settings were reported in studies from United States and United Kingdom as well.[16,17] Since most of the people indulged in sports activity for recreation during COVID period there was corresponding increase in sports related injuries.[18] In this period, barring emergency services, all other non-essential services and commercial activities were completely shut down. All public transport facilities by air, railways and road were stopped, borders were sealed and a curfew-like situation was created. This had a significant negative impact on the Indian economy. In order to revive the sinking economy, the central and state governments gradually started the unlock process in a phased manner from the month of May. Industries and factories were operational with movement of people away from home. In the months of May, June and July, the number of patients presenting with ocular trauma in the emergency gradually increased. Workplace injuries also showed an upward trend during this period and in July it constituted around 41% of total workplace injuries reported.
In the COVID-19 period, only 9 (12.7%) patients presented with corneal ulcer secondary to trauma, while in the pre-COVID-19 period, 82 (47.9%) patients had corneal ulcers. Thirty-three percent patients (3 of 9 patients) with infectious keratitis presented with large corneal ulcers, requiring TPK, in the COVID-19 period. However, in the pre-COVID-19 period, only 6.1% patients with keratitis had large corneal ulcers. Delayed presentation during the COVID-19 period resulted in progression of corneal ulcers that could have possibly been managed medically if they had presented in the initial stages. Secondly, none of the patients in the COVID-19 period could undergo TPK, while all the patients in the pre-COVID-19 period underwent TPK. Non-availability of donor tissues due to suspension of all eye banking activities were the reasons for shortage of graft during the COVID-19 period. In India, the most popular storage medium used by eye banks for preservation of donor corneal tissues is the McCarey-Kaufmann Medium or the Cornisol® Medium, both of which allow short to medium-term storage of donor grafts. It would be prudent in future to place all donor corneal tissues preserved in the above two mediums which are not used during the recommended time period in glycerol for long-term storage. Additionally, availability of artificial corneas may play a significant role during such health emergencies, but these are still in the research stage.[19]
Considering the potentially long time frame of the COVID 19 pandemic with several new restriction periods, the need to maintain strict social distancing and sanitary precautions during next few months, smart phone based teleophthalmology is an easy and effective solution to maintain health care access and regulate access to ophthalmologic emergency centers.[15] Teleophthalmology has so far been utilized for screening Diabetic Retinopathy, diagnosis of glaucoma and monitoring Age Related Macular Degeneration. But, it can also play an important role in assisting primary care physicians to better triage patients with acute ocular complaints and promptly referring those requiring urgent attention to an eye specialist. Additionally, non-emergency patients can avoid hospital visits and instead sought consultation via teleophthalmology avoiding crowding at hospitals.
The limitations and possible biases in the present study are that it was performed in a single institution, and was retrospective in nature. We did not explore the barriers to accessing eye care services in patients visiting the hospital. Nevertheless, this is the first study from India that reported the pattern of ocular trauma in the COVID-19 period and compared it with the pre-COVID-19 period.
Conclusion
In conclusion, the enforcement of a nationwide lockdown due to the COVID-19 pandemic resulted in a significant decline in the number of patients presenting with ocular trauma to the emergency department. Although injury sustained in the home setting was common in the COVID-19 period, workplace injury showed a steady increase during the unlock period.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1. [Last accessed on 2020 Aug 31]. Available from: https://www.who.int/emergencies/diseases/novelcoronavirus-2019 .
- 2.Wang C, Horby PW, Hayden FG, Gao GF. A novel coronavirus outbreak of global health concern. Lancet. 2020;395:470–3. doi: 10.1016/S0140-6736(20)30185-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Xia J, Tong J, Liu M, Shen Y, Guo D. Evaluation of coronavirus in tears and conjunctival secretions of patients with SARS-CoV-2 infection. J Med Virol. 2020;92:589–94. doi: 10.1002/jmv.25725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Khanna RC, Honavar SG. All eyes on Coronavirus — What do we need to know as ophthalmologists. Indian J Ophthalmol. 2020;68:549–53. doi: 10.4103/ijo.IJO_516_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. [Last accessed on 2020 Sep 04]. Available from: https://www.pmindia.gov.in/en/news_updates/pm-calls-for-complete-lockdown-of-entire-nation-for-21-days/?comment=disable .
- 6. [Last accessed on 2020 Sep 07]. Available from: https://www.pmindia.gov.in/en/news_updates/pms-address-to-the-nation-4/?comment=disable .
- 7.Nair AG, Gandhi RA, Natarajan S. Effect of COVID-19 related lockdown on ophthalmic practice and patient care in India: Results of a survey. Indian J Ophthalmol. 2020;68:725–30. doi: 10.4103/ijo.IJO_797_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sengupta S, Honavar SG, Sachdev MS, Sharma N, Kumar A, Ram J, et al. All India Ophthalmological Society-Indian Journal of Ophthalmology consensus statement on preferred practices during the COVID-19 pandemic. Indian J Ophthalmol. 2020;68:711–24. doi: 10.4103/ijo.IJO_871_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mir TA, Canner JK, Zafar S, Srikumaran D, Friedman DS, Woreta FA. Characteristics of open globe injuries in the United States From 2006 to 2014. JAMA Ophthalmol. 2020;138:268–75. doi: 10.1001/jamaophthalmol.2019.5823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Low L, Hodson J, Morris D, Desai P, MacEwen C. Socioeconomic deprivation and serious ocular trauma in Scotland: A national prospective study. Br J Ophthalmol. 2017;101:1395–8. doi: 10.1136/bjophthalmol-2016-309875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kanoff JM, Turalba AV, Andreoli MT, Andreoli CM. Characteristics and outcomes of work-related open globe injuries. Am J Ophthalmol. 2010;150:265–9.e2. doi: 10.1016/j.ajo.2010.02.015. [DOI] [PubMed] [Google Scholar]
- 12.Sanjay S, Garg A, Shetty R, Shetty N, Shetty BK. Impact of COVID-19 on a tertiary eye hospital. Indian J Ophthalmol. 2020;68:1485–6. doi: 10.4103/ijo.IJO_921_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kuhn F, Morris R, Witherspoon CD, Heimann K, Jeffers JB, Treister G. A standardized classification of ocular trauma. Ophthalmology. 1996;103:240–3. doi: 10.1016/s0161-6420(96)30710-0. [DOI] [PubMed] [Google Scholar]
- 14.Das AV, Narayanan R. Demographics and clinical presentation of patients with ocular disorders during the COVID-19 lockdown in India: A report. Indian J Ophthalmol. 2020;68:1393–9. doi: 10.4103/ijo.IJO_1171_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Babu N, Kohli P, Mishra C, Sen S, Arthur D, Chhablani D, et al. To evaluate the effect of COVID-19 pandemic and national lockdown on patient care at a tertiary-care ophthalmology institute. Indian J Ophthalmol. 2020;68:1540–4. doi: 10.4103/ijo.IJO_1673_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wu C, Patel SN, Jenkins TL, Obeid A, Ho AC, Yonekawa Y. Ocular trauma during COVID-19 stay-at-home orders: A comparative cohort study. Curr Opin Ophthalmol. 2020;31:423–6. doi: 10.1097/ICU.0000000000000687. [DOI] [PubMed] [Google Scholar]
- 17.Hamroush A, Qureshi M, Shah S. Increased risk of ocular injury seen during lockdown due to COVID-19. Cont Lens Anterior Eye. 2020;43:216. doi: 10.1016/j.clae.2020.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bapaye MM, Nair AG, Mangulkar PP, Bapaye CM, Bapaye MM. Resurgence of “bow and arrow” related ocular trauma: Collateral damage arising from COVID-19 lockdown in India? Indian J Ophthalmol. 2020;68:1222–3. doi: 10.4103/ijo.IJO_901_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zhang B, Xue Q, Li J, Ma L, Yao Y, Ye H, et al. 3D bioprinting for artificial cornea. Challenges and perspectives. Med Eng Phys. 2019;71:68–78. doi: 10.1016/j.medengphy.2019.05.002. [DOI] [PubMed] [Google Scholar]


