Abstract
Purpose:
The aim of this study was to describe the experience of teleconsultations addressed at our hospital in India during the ongoing coronavirus (COVID-19) lockdown.
Methods:
This cross-sectional hospital-based study included 977 teleconsultations presenting between April 1st and May 31, 2020. A two-level protocol was implemented to triage the calls.
Results:
Overall, 977 teleconsultation were addressed. Of the 621 teleconsultation addressed the most common queries were related to redness/pain/ watering/blurred vision/itching/irritation (52.49%), followed by queries related to medications (28.01%), appointments (18.84%) & 0.64% cited an emergency need to visit the hospital due to sudden loss of vision. The majority of the queries were directed to the department of cornea (58.93%) followed by retina (16.26%), cataract (13.04%), glaucoma (10.14%) & pediatric ophthalmology (1.61%). The most common advice given to the patient was related to medications (47.66%) followed by appointment-related queries (31.72%) & fixing of surgical appointment (20.61%). Among the 356 preterm babies that were screened, 57 (16.01%) were diagnosed with retinopathy of prematurity (ROP). Of them 3 required laser and 3 were given injection.
Conclusion:
Teleconsultation is here to stay beyond the pandemic. WhatsApp was the preferred modality of communication for us. Teleophthalmology has given us insights to use this evolving technology to reach out to the population at large to provide eye care services. We believe that this mode of teleophthalmology has helped us in providing feasible eye care to the patients.
Keywords: COVID-19, impact, lockdown, South India, teleophthalmology
The COVID-19 pandemic has affected the healthcare sector worldwide. The world is grappling with the challenges posed by the coronavirus (COVID-19) which has spread rapidly across different geographies. The rapid spread of the virus lead to nationwide lockdown, thus promoting social distancing in the population with the hope to flatten the curve. Since all focus shifted to the management of the pandemic, patients with diseases other than COVID-19 began to suffer due to lack of health access.
India went into a lockdown from March 23, 2020 posing unexpected challenges for institutions providing eye care. Clinical care was reduced to the provision of emergency services. In a high volume setting, the lack of information about the status of next visit or the need to clarify any query may result in stress to the patients in this time of crisis. This has resulted in a rise in the need for telemedicine platforms.
During this period, we have received messages, audio and video calls from patients seeking advice. These are all informal ways of care with no records of interactions with the patient, which is preferable for emergencies.
The Ministry of Health and Family Welfare, Government of India had released a set of telemedicine guidelines once the lockdown period was initiated.[1] Video consultation is better as we can see the patient directly, look for eye signs, and can enquire to determine if the patient has been exposed to COVID-19. This helps us to establish a provisional diagnosis, advise the patient on management, and counsel them to adhere to therapy.[1] A teleconsultation may be initiated by the patient or the doctor as and when deemed necessary.
The basic necessity for such consultations have been suggested by the All India Ophthalmological Society.[2] These include verification of identity, consent, documentation of any available investigation, documentation of findings, and prescription in the approved format. A very important fact to note is that teleconsultation does not grant immunity from medico-legal liabilities. Primarily teleconsultation is to determine whether a physical visit is required and to offer advice in the meantime. In this current scenario we wish to present the experience of addressing clinical queries of a cohort of patients through teleconsultations at a tertiary eye care center, in Tirunelveli, Tamil Nadu during the unique scenario of the ongoing COVID-19 lockdown.
Methods
This cross-sectional observational hospital-based study included teleconsultations of patients addressed between 1st of April to 31st of May 2020 at a tertiary eye care center, Tirunelveli, Tamil Nadu. The patient or the parents or guardians of the patient called the designated teleconsultation number of the hospital [Fig. 1]. All research adhered to the tenets of the Declaration of Helsinki and was approved by the Institutional Ethics Committee. Institutional review board exemption for this study was obtained from institutional ethics committee. We have obtained all appropriate patient consent forms. In the form the patients have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published.
Figure 1.
Teleconsultation contact number
Teleconsultation protocol
A total of 977 teleconsultations were addressed at our center during the study period. The phone calls as per protocol were divided into two levels.[3] Level 1 involved resolution of the call by the general ophthalmologist itself; Level 2 involved taking the patient query to the ophthalmologist of that speciality department for further evaluation and follow-up. The prescription of medicines adhered to the telemedicine practice guidelines of India.[4] and the patients were advised to continue their previous medications where relevant. All the teleconsultation were provided free of cost. Some of the frequent questions asked by the patients and answered by the ophthalmologist are listed in Table 1. Some common scenarios that can be managed on teleconsultation like sudden diminution of vision and headache are shown in Figs. 2 and 3 respectively.
Table 1.
Protocol followed by ophthalmologist to address the queries of the patients
| Patient Query | Ophthalmologist Answer |
|---|---|
| I have an appointment, what can I do now? | Due to coronavirus situation we are dealing with emergencies only. We are noting down your medical record number and will reschedule your appointment, when the situation stabilizes. |
| I was scheduled to have surgery? What can be done now? | Due to coronavirus situation we are dealing with emergencies only. We are noting down your medical record number and will reschedule your surgery and contact you, when the situation stabilizes. |
| I am having a problem in my and eye and I need help for the eye and I need help for the same. (New Patient) | Please let me know your problem and I will help you out with the same. |
| I am already being treated at your hospital & now am having a problem in my eye. (Review patient) | Please hold on as we retrieve your case sheet & the treating ophthalmologist of that particular department will clear your query. |
| Can I continue my treatment till my next appointment? | Kindly hold on as we retrieve your case sheet and discuss with the ophthalmologist of the concerned speciality and clear your query. |
| When will the Hospital open again? | We are not sure at this point in time and will make a formal announcement when the situation stabilizes based on the government guidelines. |
Figure 2.
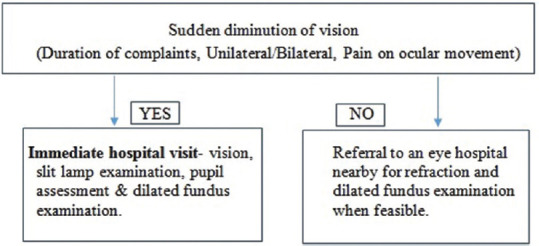
Flow chart followed for sudden diminution of vision
Figure 3.
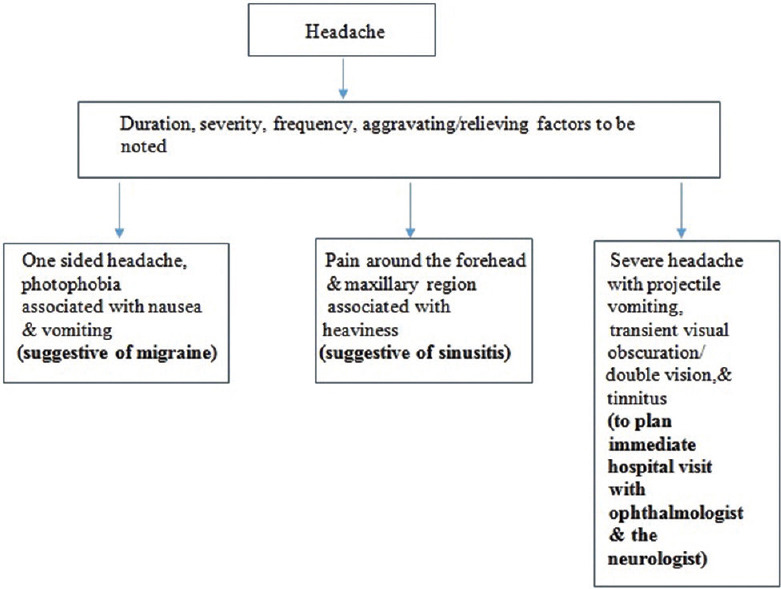
Flow chart followed for headache
RetCam screening
With the help of our RetCam [RetCam Shuttle (Clarity Medical Systems, Pleasanton, California, USA)] the trained mid-level ophthalmic professionals (MLOP) used to travel to hospitals in Tirunelveli and nearby districts [Kanyakumari, Thoothukudi]. All the preterm infants were screened for Retinopathy of prematurity. The images that were taken with the help of RetCam were sent to the base hospital using the ADRES (Aravind diabetic retinopathy screening) software. All of the images were gradable. At the base hospital the retina specialist will make the diagnosis and decide on further management.
Results
Demographics
Among the 977 patients who were addressed, 621 were addressed by teleconsultation and 356 were preterm babies which were screened with the help of RetCam. Among the 621 patients, 436 (70.2%) were follow up patients and 185 (29.79%) were new patients and of the 356 preterm babies, 202 (56.74%) were new patients and 154 (43.25%) were review patients.
Patient queries
Of the 621 patients, 326 (52.49%) were related to symptoms of redness/pain/watering/blurred vision/itching/irritation; 174 (28.01%) were medication related queries; 117 (18.84%) were appointment related; 4 (0.64%) cited an emergency need to visit the hospital due to sudden loss of vision. The 356 preterm babies were screened using RetCam in hospitals of various nearby districts and graded by our retina consultants at the base hospital.
Ocular subspecialty
Of the 621 patients, 366 (58.93%) were related to Cornea and anterior segment; 101 (16.26%) were addressed by the subspecialty of Retina; 81 (13.04%) were Cataract related; 63 (10.14%) were Glaucoma clinic related; 10 (1.61%) were associated with Pediatric Ophthalmology. The 356 preterm babies screening was taken care by the retina department.
Diagnosis
Of the 326 patients who had called up for symptoms related to redness/pain/watering/itching/irritation: 128 of them had allergic conjunctivitis, 52 had acute conjunctivitis, and the remaining 146 of them had nonspecific complaints like watering, foreign body sensation etc. 4 of the patients who had cited an emergency visit to the hospital due to sudden loss of vision, among them 2 were diagnosed with retinal detachment, 1 had subconjunctival hemorrhage post trauma with a stick and 1 had corneal tear post blunt injury with a stone.
Ophthalmologist advice
Of the 621 patients, 296 (47.66%) were medication related. Of the 296 patients, 25.12% (156) were asked to continue/taper the medication, 13.52% (84) were asked to stop medications and 9.01% (56) were prescribed an alternative brand of medication, mostly an antiglaucoma medication which were unavailable in their area. 197 (31.72%) were appointment related which were rescheduled for a later date. 128 (20.61%) were related to fixing a surgical appointment. 258 new prescriptions were given. Of the 356 preterm babies seen with the help of RetCam, 57 (16.01%) were diagnosed to have retinopathy of prematurity, of which 3 required laser and 3 were given injection bevacizumab. The 6 preterm babies requiring treatment had turned up for their treatment.
Follow up (post op)
Of the 621 patients who had called us, we had 112 postop patients requiring follow up. Among the 112 post op patients, 28 was from the retina department, 62 belonged to the cataract department, 10 from the department of cornea and 12 post ops were from the glaucoma department.
Discussion
The ongoing COVID-19 pandemic has changed the pattern of healthcare with prime importance being given to telemedicine, which has taken a center stage. Due to the ongoing pandemic, routine out-patient department and elective surgeries have been suspended and in-patient care only for emergency situations are being provided.[5] Tele ophthalmology which has been just a bystander for over a decade, became the need of the hour. Not only does it lessen the need for the patient and clinician to be in the same place but also protects both the patient and the doctor by reducing the time of patient exposure for the doctor, and the patient by limiting visit to the hospital only in case of a dire emergency.[6] It has served as a lifeline for nearly 2 months when routine services had come to a complete standstill.
Taking into account all these aspects and rooting for community wellness, we at our tertiary eye care center started teleconsultation during the lockdown. The findings of our study showed that majority of the patient queries were related to symptoms of redness/pain/watering/irritation/itching/blurred vision of the eyes. The most common advice given was medication related. Majority of the patients came under the subspecialty of cornea and anterior segment followed by retina, cataract, glaucoma and pediatric ophthalmology respectively.
Our study reports the use of teleconsultation as a means of management of patients to ensure continuity of care during the period of lockdown. All teleconsultations were given free of cost. WhatsApp messages made it very convenient for us to receive and analyze images which helped to overcome the limitation of verbal communication. One of the unique difficulty faced by us was to get an e-pass for our RetCam shuttle to travel to other districts for ROP screening and the same difficulty was faced by the patients for coming to our hospital from other districts. A child with congenital glaucoma had undergone left eye trabeculectomy with trabeculotomy just before lockdown. The parents were worried that the opacity in the left eye was increasing post-surgery. A referral letter for e-pass was mailed to the parents using which they had come to the hospital for follow up. The child was advised to undergo evaluation under anesthesia (EUA) in both eyes and an antiglaucoma medication was prescribed for both eyes. Parents were not willing for EUA. Another patient had redness in the right eye post trauma with a stick. The patient was mailed a referral letter for e-pass. The patient had visited our hospital after 2 days. The redness was nothing more than a subconjunctival hemorrhage and there were no other significant finding on examination. The patient was treated for the same [Fig. 4].
Figure 4.

Case scenarios during lockdown. (a) Congenital glaucoma, (b) Subconjunctival haemorrhage due to stick injury, (c) Aggressive posterior retinopathy of prematurity pre injection, (d) Aggressive posterior retinopathy of prematurity post injection
Despite the lockdown, using a RetCam shuttle we were able to screen 356 preterm babies in hospitals from multiple nearby districts and treat the patients accordingly. This definitely has helped in diagnosing aggressive posterior retinopathy of prematurity (APROP) and timely intervening, which will prevent the child from losing their vision permanently [Fig. 4].
William AM et al. published a study that reported video calls as a useful modality for triage and taking care of lowrisk cases.[7] Video call does provide a facility of realtime interaction with the patient but needs a good quality connection at both ends. We had very limited use of video calls since a large proportion of our patients were from rural area where network connectivity is poor. A survey done by Nair AG et al. reported telephonic consultation (54.9%) as the most preferred mode of interaction, followed by social media apps like WhatsApp while video calls were minimally used.[8] Majority of our interaction was via WhatsApp calls and messages with very few video calls.
Our study suggests that teleconsultation is definitely a feasible option in delivering day to day eye care services. In this age of technology and widespread availability of mobile phones and social media applications, establishing patientdoctor interaction even in times of lockdown has made teleconsultation a life saver. Teleconsultation helped us in providing treatment to many patients for mild conditions like redness/pain/watering/irritation/itching, thus minimizing the need for their travel and possible risk of transmission of infections in a crowded hospital environment. Majority of the followup cases were managed with a detailed history and photographic evaluation where necessary.
Teleophthalmology definitely has its own limitations. The virtual technology cannot replace in-person clinical examination. There is always a risk of making an error in diagnosis, which could lead to medicolegal implications. The data security and confidentiality are some issues that needs to be looked into. It is imperative for us to make innovations and come up with some form of technology that will help us to cater even to the lower socioeconomic strata. It does not have much role in glaucoma patients where we cannot actually measure the IOP, PDR patients with vitreous hemorrhage, etc. Nevertheless, the usefulness of this modality during this global pandemic crisis cannot be overlooked.
The financial consideration has to be evaluated against several variables such as equipment and annual maintenance, transmission/software, evolution and growth of field, cost of technology, and return on investment. Even the European law, for instance, states that telemedicine is a “health and an information service” which should be provided “for a fee” at a distance.[9]
There are other aspects that need to be considered before deciding on the fee to be levied such as the nature of the disease being treated online. Teleophthalmology is being used extensively especially for diabetic retinopathy (DR) screening. Evidence has shown that teleophthalmology is very useful to deliver cost-effective as well as accessible screening for DR.[10,11,12] Certain factors influencing the cost effectiveness were age of onset of diabetes, glycemic control and compliance rate of the patient.[10] Similarly even for glaucoma it was found to be cost effective compared to in person examination.[13] Even in case of retinopathy of prematurity (ROP) screening it was found that telemedicine screening for ROP was an economically feasible option depending on the place and the number of infants being screened routinely.[14] Few other factors which need to be taken into account that influence the cost-effectiveness are the age of the patient,[15] full utilization of the equipment[16] and the frequency of screening.[17]
We have to wait and observe the demand for telemedicine once the restrictions due to ongoing pandemic are lifted and also the behavior and response of the patients which will dictate the growth of teleconsultation in ophthalmology. It is best to charge a fee per session. It should be integrated into hospital's payment portals thus maximizing digital payments. This definitely is a viable option in the future, especially for those living in distant and remote places with limited healthcare facilities, seeking urgent advice.
A limitation of our study was the lack of electronic medical record in our institution which resulted in our dependence on patient in providing report via email or WhatsApp. During the period of lockdown our vision centers were closed as it was under the red zone, hence any sort of consultation or sharing of clinical pictures for ophthalmologist opinion was not possible. This affected our outreach to the lower socioeconomic strata of people. Another limitation was the skill of our respondents that ranged from junior residents to experienced consultants. Also active participation of the patient and the family is required and they should have a basic technical knowledge for sharing images. No amount of photograph/video call can replace the information that is gained by slit-lamp examination. Certain important tests such as intraocular pressure measurement are definitely not possible.
Other issues such as informed consent of the patient, medicolegal liabilities for the doctor and giving a prescription for medications are some of the issues that cannot be overlooked.
Conclusion
In conclusion, this study aimed to describe our experience of teleconsultation. Teleconsultation is here to stay beyond the pandemic and we may have to modify our practices accordingly. Our experience with regards to patient care using teleconsultation has been a very enriching one. WhatsApp was the preferred modality of communication for us. For patients who may not be able to travel at all, a teleconsultation is better than no consultation at all and does serve as a reasonable form of triage. It has a significant use especially in cases of follow up patients. Teleconsultation not only helps in providing primary eye care for most of the eye conditions but also as a forward triage for rest of the other conditions. Teleophthalmology has given us insights to use this evolving technology to reach out to the population at large to provide eye care services. We believe that this mode of teleophthalmology has helped us in providing feasible eye care to the patients.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1. Available from: https://www.mohfw.gov.in/pdf/Telemedicine.pdf .
- 2. Available from: https://aios.org/pdf/AIOS-Telemedicine-Practice-Guidelines.pdf .
- 3.Das AV, Rani PK, Vaddavalli PK. Teleconsultations and electronic medical records driven remote patient care: Responding to the COVID-19 lockdown in India. Indian J Ophthalmol. 2020;68(6):1007–12. doi: 10.4103/ijo.IJO_1089_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ministry of Health and Family Welfare, Government of India [Internet] Telemedicine Practice Guidelines. c2020. Available from: https://www.mohfw.gov.in/pdf/Telemedicine.pdf .
- 5.Recommendations for urgent and nonurgent patient care [Internet] American Academy of Ophthalmology. 2020. Available from: https://www.aao.org/headline/new-recommendation-surgentnonurgent-patient-care .
- 6.Sim D, Thomas P, Canning C. Tackling COVID-19 with telemedicine [Internet] The Ophthalmologist. 2020. Available from: https://theophthalmologist.com/subspecialties/tackling-COVID-19-with-telemedicine . cited on 2020 May 23.
- 7.Williams AM, Kalra G, Commiskey PW, Bowers EMR, Rudolph BR, Pitcher MD, et al. Ophthalmology practice during the coronavirus disease 2019 pandemic: The University of Pittsburgh experience in promoting clinic safety and embracing video visits. Ophthalmol Ther. 2020;6:1–9. doi: 10.1007/s40123-020-00255-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nair AG, Gandhi RA, Natarajan S. Effect of COVID-19 related lockdown on ophthalmic practice and patient care in India: Results of a survey. Indian J Ophthalmol. 2020;68:725–30. doi: 10.4103/ijo.IJO_797_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Directive 95/46/EC of the European Parliament and of the Council of 24 October 1995 on the protection of individuals with regard to the processing of personal data and on the free movement of such data. Off J. 1995;281:31–50. Available from: https://eur-lex.europa.eu/legalcontent/en/TXT/?uri=CELEX%3A31995L0046 . [Google Scholar]
- 10.Jones S, Edwards RT. Diabetic retinopathy screening: A systematic review of the economic evidence. Diabet Med. 2010;27:249–56. doi: 10.1111/j.1464-5491.2009.02870.x. [DOI] [PubMed] [Google Scholar]
- 11.Au A, Gupta O. The economics of telemedicine for vitreoretinal diseases. Curr Opin Ophthalmol. 2011;22:194–8. doi: 10.1097/ICU.0b013e3283459508. [DOI] [PubMed] [Google Scholar]
- 12.De la Torre-Díez I, López-Coronado M, Vaca C, Aguado JS, de Castro C. Cost-utility and cost-effectiveness studies of telemedicine, electronic, and mobile health systems in the literature: A systematic review. Telemed J E Health. 2015;21:81–5. doi: 10.1089/tmj.2014.0053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Thomas S, Hodge W, Malvankar-Mehta M. The cost-effectiveness analysis of teleglaucoma screening device. PLoS One. 2015;10:e0137913. doi: 10.1371/journal.pone.0137913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Isaac M, Isaranuwatchai W, Tehrani N. Cost analysis of remote telemedicine screening for retinopathy of prematurity. Can J Ophthalmol. 2018;53:162–7. doi: 10.1016/j.jcjo.2017.08.018. [DOI] [PubMed] [Google Scholar]
- 15.Kirkizlar E, Serban N, Sisson JA, Swann JL, Barnes CS, Williams MD. Evaluation of telemedicine for screening of diabetic retinopathy in the Veterans Health Administration. Ophthalmology. 2013;120:2604–10. doi: 10.1016/j.ophtha.2013.06.029. [DOI] [PubMed] [Google Scholar]
- 16.Phan AD, Koczman JJ, Yung CW, Pernic AA, Doerr ED, Kaehr MM. Cost analysis of teleretinal screening for diabetic retinopathy in a county hospital population. Diabetes Care. 2014;37:e252–3. doi: 10.2337/dc14-0929. [DOI] [PubMed] [Google Scholar]
- 17.Rachapelle S, Legood R, Alavi Y, Lindfield R, Sharma T, Kuper H, et al. The cost-utility of telemedicine to screen for diabetic retinopathy in India. Ophthalmology. 2013;120:566–73. doi: 10.1016/j.ophtha.2012.09.002. [DOI] [PubMed] [Google Scholar]


