Abstract
With increasing experience, it has been suggested that the SARS-CoV-2 virus has a neurotropic effect. Here, we present a case of a tonic pupil who developed after COVID-19 infection. A 36-year-old woman presented with progressive photophobia and blurred vision. On neurological examination, loss of deep tendon reflexes accompanying a tonic pupil was detected and brain MR imaging was normal. With this case, we aimed to describe a rare pattern of neurological involvement caused by the possible SARS-CoV-2 virus.
Keywords: Adiefs tonic pupil, anisocoria, COVID-19, nervous system, neurological symptom
Coronavirus disease-2019 (COVID-19) is caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) which was first detected in the human population in late December 2019. It is a viral infection with a wide spectrum of severity and prognosis. Although the most common and important presentation is with respiratory disease, reports of neurological manifestations are increasing. To date, encephalitis, cerebrovascular diseases, myelitis, and peripheral neuropathy have been reported as neurological syndromes that may be associated with SARS-CoV-2.[1] Most recently, pupillary involvement associated with this virus has been reported.[2,3,4] Here, we report a further case of a possible COVID-19-related tonic pupil manifested by blurred vision.
Case Report
A 36-year-old previously healthy female patient admitted to the hospital with a 3-week history of left eye photophobia and blurred vision. She noticed that her left pupil appeared dilated during this time. In her medical history, two months ago she was admitted to the hospital with the complaints of cough and difficulty breathing. It was learned that, although nasopharyngeal swab PCR test for SARS-CoV -2 was negative, she was treated with the diagnosis of COVID-19 due to the presence of viral pneumonia findings on thorax computerized tomography (CT). In the neurological examination, visual acuity (20/20), visual field, intraocular pressure (15 mmHg), and fundoscopy were normal without refractive error in both eyes. There were no gaze abnormalities or nystagmus. Pupillary examination showed an enlarged left pupil unreactive to the light; near response was also impaired [Fig. 1a-c]. Slit-lamp examination of the anterior segment was within normal limits in both eyes. Pharmacological testing with dilute pilocarpine 0.1% resulted in constriction of the left pupil but no change in the right pupil, demonstrating cholinergic hypersensitivity [Fig. 1d]. In addition, deep tendon reflexes were absent both in the upper and lower limbs. The rest of the examination was normal.
Figure 1.
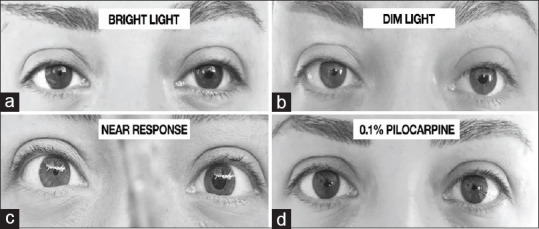
Parasympathetic denervation of the iris sphincter muscle in Adie syndrome results in an enlarged tonic right pupil reacting poorly to light (a and b). Near response was also impaired (c). It is supersensitive to cholinergic agents (pilocarpine 0.1%) (d)
Routine laboratory investigations included hemogram, biochemistry, thyroid function tests, ferritin, folate, vitamin B12, hepatitis markers, syphilis markers, anti-HIV, chest x-ray, were within the normal range. Autoimmune panels and tumor markers were all negative. Cerebrospinal fluid (CSF) analysis showed normal protein concentration and a normal white cell count of 2/mm3. Subsequent standard CSF virology PCR (herpes simplex virus 1 and 2, varicella zoster virus, adenovirus, cytomegalovirus, Epstein-Barr virus) and SARS-CoV-2 PCR were negative. Magnetic resonance imaging (MRI) of the brain, orbita and spinal cord was unremarkable [Fig. 2]. No signs of malignancy were detected in thorax CT, abdominal CT, and breast ultrasonography.
Figure 2.
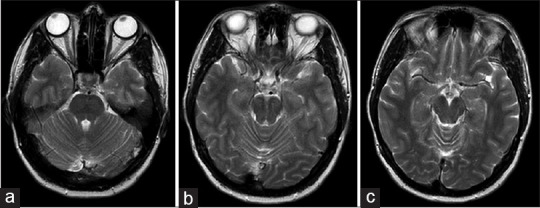
Patient's MRI: Normal midbrain and oculomotor pathway (a-c)
After a detailed clinical investigation and differential diagnosis, our patient was diagnosed with Holmes-Adie syndrome. Dilute pilocarpine 0.1% was tried for symptomatic treatment. There was not achieved significant improvement in the visual complaints with pilocarpine. Intravenous methylprednisolone treatment was recommended to the patient, but she did not accept the treatment.
Discussion
A tonic pupil is also known as Adie's pupil is a dilated pupil with preserved near response despite poor light reaction and hypersensitivity to cholinergic drugs. It occurs due to aberrant regeneration of parasympathetic nerve fibers after ciliary ganglion injury. The reason for light-near dissociation is that the ciliary body has a much denser neuronal innervation than the iris sphincter. In the minority of patients whose near response is affected, as in our patient, the main clinic may be compatible with blurred vision and mimic optic neuritis. Pupillary involvement may remain isolated or accompanied by generalized areflexia, which is called Holmes-Adie syndrome. Although the tonic pupil is mostly idiopathic, ocular infection and inflammation, peripheral and autonomic neuropathies, paraneoplastic syndromes, tumors, and trauma are associated conditions.[5] This case was accepted as a possible COVID-19-related tonic pupil based on the history of COVID-19 disease just prior to ophthalmologic complaints, after excluding all possible causes. Despite the negative SARS-CoV-2 result on the nasopharyngeal swab, in the presence of respiratory symptoms and signs of viral pneumonia on thoracic CT, it is considered to be 'possible COVID-19' disease as in our patient and false negativity should be questioned.[6]
Neuro-ophthalmologic manifestations associated with SARS-CoV-2 have also been identified. Koh et al. described dysautonomic syndrome as a new finding due to COVID-19, including Adie's tonic pupil, in their study.[2] Later than, Ordás et al. reported SARS-CoV-2 related unilateral tonic pupil accompanying cranial neuropathy, 3 weeks after COVID-19 infection.[3] Most recently, Seller et al. reported SARS-CoV-2 related inflammatory chorioretinopathy and bilateral Adie's syndrome two days after the onset of respiratory symptoms.[4] In our patient, the onset of neurological involvement in the subacute period after respiratory complaints and the results of CSF suggest post-infection processes rather than direct viral entry into the CNS.
Although Adie's tonic pupil usually does not require treatment, dilute pilocarpine 0.1% can be considered as a therapy in patients with blurred vision. In our patient, a significant improvement in the visual complaints was not achieved with pilocarpine. Steroids may be an option in cases where autoimmunity has been considered. Taper prednisolone was also chosen in Adie's pupil due to COVID-19, which was considered as a delayed immune response, and a regression in neurological complaints was observed.[3]
Conclusion
In this case, a rare pattern of neurological involvement caused by possibly SARS-CoV-2 has been discussed. Careful clinical, diagnostic, and epidemiological studies are needed to help define the manifestations and burden of neurological disease caused by SARS-CoV-2. The possibility of an immune-mediated process and its therapeutic implications also warrants greater study.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Ellul MA, Benjamin L, Singh B, Lant S, Michael BD, Easton A, et al. Neurological associations of COVID-19. Lancet Neurol. 2020;19:767–83. doi: 10.1016/S1474-4422(20)30221-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Koh JS, De Silva DA, Quek AML, Chiew HJ, Tu TM, Seet CYH, et al. Neurology of COVID-19 in Singapore. J Neurol Sci. 2020;418:117118. doi: 10.1016/j.jns.2020.117118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ordás CM, Villacieros-Álvarez J, Pastor-Vivas AI, Corrales-Benítez Á. Concurrent tonic pupil and trochlear nerve palsy in COVID-19. J Neurovirol. 2020;26:970–2. doi: 10.1007/s13365-020-00909-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ortiz-Seller A, Martínez Costa L, Hernández-Pons A, Valls Pascual E, Solves Alemany A, Albert-Fort M. Ophthalmic and neuro-ophthalmic manifestations of coronavirus disease 2019 (COVID-19) Ocul Immunol Inflamm. 2020;28:1285–9. doi: 10.1080/09273948.2020.1817497. [DOI] [PubMed] [Google Scholar]
- 5.Moeller JJ, Maxner CE. The dilated pupil: An update. Curr Neurol Neurosci Rep. 2007;7:417–22. doi: 10.1007/s11910-007-0064-9. [DOI] [PubMed] [Google Scholar]
- 6.WHO. Coronavirus Disease 2019 (COVID-19): Situation Report, 61. Geneva: World Health Organization; 2020. [Google Scholar]


