Abstract
Purpose:
The aim of this study was to determine the frequency and various types of ophthalmic manifestation of patients with COVID-19.
Methods:
This is a prospective observational study conducted on patients with SARS-Co-V-2 infection, at a dedicated tertiary COVID-19 hospital in South India from April 1 to July 31, 2020. At the time of their admission to the COVID hospital, demographic data such as name, age, sex was recorded. A thorough history regarding the onset, duration, progression, nature of symptoms and its associated factors, medication history, treatment history were elicited and documented. Ocular examination was performed under torchlight by an ophthalmologist posted for COVID duty. Further investigations including imaging were sought for, depending on clinical indications. Serial follow-up examinations of all patients were carried out every 72 hours or when patients complained of any ocular symptoms whichever earlier, until discharge. All relevant data were compiled and statistically analyzed.
Results:
A total of 2742 patients were examined. Of them, 1461 (53.28%) were males and 1281 (46.72%) were females. The mean age (±SD) was 39.46 ± 17.63 years. None of the patients in our study had any ocular symptoms or signs as the presenting complaint at the time of their admission. On subsequent follow-up, only 20 (0.72%) developed ocular manifestations, of which 19 (95%) had features suggestive of Bilateral viral conjunctivitis. However, 1 (5%) patient had orbital cellulitis secondary to pansinusitis.
Conclusion:
Ophthalmic manifestations in the clinical spectrum of COVID-19 infection are uncommon and unlikely to be the presenting clinical impression. However, it has broadened our view to a wider spectrum of COVID-19 presentations enhancing our clinical acumen for staunch detection of COVID-19 suspects in our daily practice, augmenting early diagnosis and management and also break the chain of transmission for the greater good of humanity.
Keywords: Conjunctivitis, ophthalmic manifestations, orbital cellulitis, SARS-Co-V-2
The COVID-19 pandemic has taken over the healthcare system since its first case in December 2019 and altered the clinical approach to patient examination and management all over the world. The pathogen in this Novel Coronavirus Disease 2019 (COVID-19) is SARS CoV-2, an enveloped, positive-stranded RNA virus, belonging to the genus Betacoronavirus of the family Coronaviridae.[1] It has human-to human transmission via various routes namely aerosol, respiratory droplets, and fomites.[2] The SARS CoV-2 infection has varied symptomatology and presentations, with majority of hosts being asymptomatic or pauci-symptomatic with mild to moderate disease, and a proportion of individuals can have severe to critical disease and may succumb to it.[3] Fatal outcomes were mainly reported among elderly over 60 years of age and individuals with other comorbidities, such as chronic liver disease, myocarditis, renal dysfunction and cardiovascular disease.[1,4] Early diagnosis and treatment has been a key measure is lessening the morbidity and mortality risk.[5] This has prompted researchers all over the world to intensively study the various clinical presentations with more stress on the initial symptoms and signs.[6] There have been various case reports and series of COVID-19 keratoconjunctivitis.[7,8] As ophthalmologists, we too may encounter asymptomatic or paucisymptomatic patients with COVID-19 during our clinical practice presenting with ophthalmic complaints who may not be diagnosed with the infection until they reach us. So, a better understanding of the various ophthalmic manifestations and presentations of COVID-19 infection will be helpful in prompt detection of COVID-19 suspects presenting to the ophthalmology clinic and also offer a deeper understanding of the overall clinical picture of the COVID-19 infection.
Methods
This is a prospective observational study conducted at a dedicated tertiary COVID-19 hospital in South India from April 1 to July 31, 2020.
Following approval and clearance from the institutional ethics committee, the participants were enrolled for the study after applying inclusion and exclusion criteria. Patients with SARS-CoV-2 infection, confirmed by real-time RT-PCR test of nasopharyngeal swab, conforming to the case definition of WHO standards with or without ocular symptoms were included in the study.[9] Patients who did not give consent for participation and suspects without confirmatory test reports were excluded.
At the time of their admission to the dedicated COVID hospital, written informed consent was obtained from each patient. Demographic data such as name, age, sex were recorded. A thorough history regarding the onset, duration, progression, nature of symptoms and its associated factors, medication history, treatment history were elicited and documented. Ophthalmic clinical examination was performed under torchlight by an ophthalmologist posted for COVID duty. Detailed examination of lids and adnexa for signs of inflammation, conjunctiva for any follicles/congestion, cornea for any infiltrates/punctate keratitis, AC for depth, iris for any nodules/synechiae/other signs of uveitis, pupils for RAPD, and reaction to both direct and consensual light and lens grading were done. Bedside visual acuity testing was also performed using Snellen acuity chart. Further investigations including imaging were sought for, depending on clinical indications. Serial follow-up examinations of all patients were carried out every 72 hours or whenever patients complained of any ocular symptoms whichever earlier, since the time of their admission until discharge. Appropriate Infection Prevention and Control measures including safe Personal Protection Equipment (PPE) practices as per the guidelines of the Ministry of Health and Family Welfare of the Republic of India were followed throughout the doctor–patient interaction.[10]
Statistics
Data was compiled and entered into Microsoft Excel sheet and analyzed using software SPSS version 20.0. Data was analyzed using descriptive statistics (frequencies, mean, standard deviation, and percentages). For association data, Chi-square test was used. Data is presented in the form of tables and graphs wherever necessary.
Results
A total of 2742 patients were examined. Of them, 1461 (53.28%) were males and 1281 (46.72%) were females. The mean age (±SD) was 39.46 ± 17.63 years. Patients as young as 3 days old and as old as 99 years were included in the study. None of the patients in our study had any ocular symptoms or signs as the presenting complaint at the time of their admission. On subsequent follow-up, only 20 (0.72%) developed ocular manifestations, of which 19 had features suggestive of Bilateral conjunctivitis [Fig. 1a and b] and were managed conservatively with supportive therapy of lubricants and prophylactic antibiotics topically.
Figure 1.
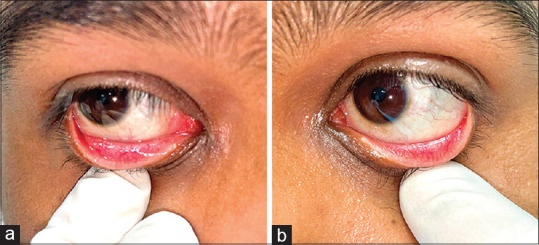
(a) Follicular conjunctivitis. (b) Follicular conjuctivitis
Among the 20 (0.72%), ocular features included diffuse conjunctival congestion and increased lacrimation seen in 19 patients (95%), chemosis in 5 patients (20%), around 9 patients (0.45%) had visible follicular response classic of viral conjunctivitis. However, 1 patient (5%) had features suggestive of orbital cellulitis [Fig. 2] such as proptosis, blurring of vision, painful restriction of movements, and diplopia, for which the patient was subjected to Non-Contrast CT scan of orbits, paranasal sinuses, and brain, imaging confirmed orbital cellulitis secondary to pansinusitis. Among the 20 patients with ocular manifestations, COVID-19 systemic disease severity was mild among 5 patients (25%), moderate among 9 (45%), severe in 4 (20%), and critical in 2 patients (10%).
Figure 2.
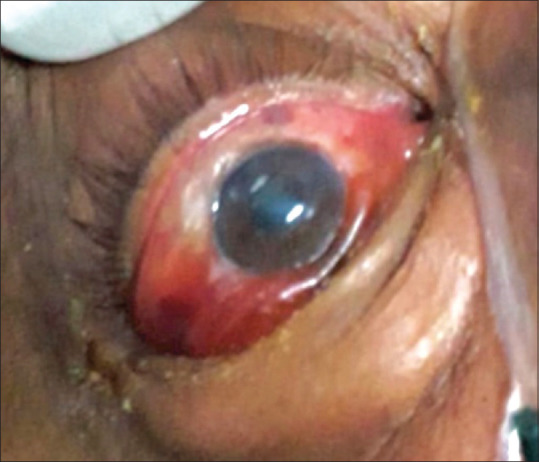
Case of orbital cellulitis showing lid edema, chemosis
Discussion
A study by Guan at al outlined that fever was the most common presentation followed by cough, nausea or vomiting, diarrhea, and only 9 (0.8%) out of 1,099 patients were reported to have conjunctival congestion.[11,12] Uniformly, none of the patients in our study had any presenting ocular manifestation at the time of admission at our institution, and the ones who had ocular features developed it later during their stay at the hospital as the disease progressed.
In a 2003 Singaporean study, Loon et al. sampled tears from 36 suspects of having SARS over a period of 12 days, of which 3 patients had positive results early in their course of infection. Moreover, Tear samples were used to confirm SARS in the female patient, who was positive only from her tears.[13] In a similar study pertaining to the SARS CoV-2, among a series of 30 patients, one patient's tear and conjunctival secretions yielded positive RT-PCR results.[14] The fact that virus could be isolated from tears and conjunctival secretion, propels the proposition of localized ocular infection and thereby ocular manifestation in the pathogenesis of the SARS CoV-2 virus disease spectrum.
In previous case reports, other coronaviruses have been implicated in human conjunctivitis.[15] There has also been a case report of relapsing viral keratoconjunctivitis in a COVID-19 patient.[7] In our study, only 20 (0.7%) had ocular manifestations, among them19 had findings consistent with conjunctivitis bilaterally, similar to the findings of Guan et al.[12] Contrary to our findings, Wu Ping et al. in their case series of 38, reported ocular manifestations in almost one-third of patients that was consistent with conjunctivitis.[8]
However, amongst our 20 patients, Orbital cellulitis was observed in a case of 60-year-old male with severe COVID-19 pneumonia with uncontrolled type 2 Diabetes mellitus. Possibility of various differential diagnosis were considered, including mucormycosis, but Non-Contrast CT showed no evidence of fungal sinusitis. As the patient had severe COVID-19 pneumonia, patient was on systemic steroids and anticoagulants as per the standard treatment guidelines followed at the dedicated COVID hospital. It has been noted that Sino-nasal cavity may be a major site of infection by SARS-CoV-2, with high expression of susceptibility genes required for infection.[16] Although venous thromboembolism has been well documented in cases of Covid-19, there was no such finding on plain CT as opined by a radiologist.[17] Contrast-enhanced CT would be the preferred modality to assess thrombosis of superior ophthalmic vein, it was deferred in view of deranged renal function parameters; however, demise of the patient due to COVID-related Acute respiratory distress syndrome limited us from observing the further clinical course.
Among the patients with ocular manifestations, COVID-19 disease severity was mild among 5 patients (25%), moderate among 9 (45%), severe in 4 (20%), and critical in 2 patients (10%). Our findings indicate that ocular manifestation is seen in patients with varying severity of COVID-19 disease spectrum and hence severity of systemic symptoms was not relevant for ocular manifestation.
With the knowledge recruited from our findings, one can deduce that ophthalmic manifestations are uncommon and unlikely to be the presenting clinical picture, but are one among the many manifestations in the clinical spectrum of COVID-19 infection. This low frequency of ophthalmic manifestations can be attributed to the phylogenetic tropism of the virus, as coronaviruses are known to cause acute and chronic respiratory, enteric, and central nervous system diseases in many species of animals, including humans.[18] Hence, may not be deemed primary ocular surface pathogens, in spite of there being ample evidence for the presence of the angiotensin-converting enzyme – 2 (ACE-2) receptors in the eye namely in the Retinal pigmented epithelium (RPE),[19] Choroid[19] and Conjunctiva[20] that has been indicated to serve as the SARS-CoV-2 receptor correlating with the state of cell differentiation and ACE2 expression and localization.[21]
However, Marvi Cheema et al. reported a case of COVID-19 with an initial presentation of keratoconjunctivitis, the patient's primary symptom was red eye with watery discharge and has been the first such case reported in North America.[22] Likewise, in our study diffuse conjunctival congestion, increased lacrimation, chemosis, and follicular response classic of viral conjunctivitis was observed.
In spite of the low rate of virus isolation from tears sampling, the ocular route seems to be an important mode for SARS CoV-2 transmission, as Lu et al. noted a case being infected by SARS CoV-2 despite wearing an N95 mask but without any eye protection and had complained of redness of the eyes several days before the onset of pneumonia.[23]
Though these case reports seem anecdotal, eye protection is an important barrier to curb the chain of transmission, as Li et al. emphasized that Ophthalmologists should take particular care when examining patients, because of both the proximity to patients' nose and mouth, and the potential exposure to tears which may contain the virus.[24]
Besides the aforementioned, there may be a few factors that may confound our findings and hence alter the conjecture. These include ocular morbidities independent of COVID-19 infection associated with critically ill patients, who may develop exposure keratopathy, chemosis, and microbial keratitis.[25,26] Mela et al. observed that microbial ocular surface colonization was associated with longer period of ICU hospitalization, use of sedation, and mechanical respiratory support, thereby most patients (85%) showed ocular surface bacterial colonization within the first seven days of sedation and intubation.[27]
Nonetheless, treatment of COVID-19 itself can pose significant adverse effects on the eye, such as hydroxychloroquine (HCQ) is known to cause photoreceptor destruction and thereby bull's eye maculopathy. Raumviboonsuk et al. addressed that the major risk factor with HCQ use while treating COVID-19 patients was the higher than generally recommended dosage, although over a relatively short period of time, that is for about a week; however, there has not yet been a report on retinal toxicity associated with this kind of treatment.[28]
Also, some anti-viral medications have reportedly been associated with drug-induced uveitis.[29,30] Although there has been no such evidence so far, in the case of the newer antiviral like Faviparavir and Remdesivir that have been used at our institution.[31,32] But, there has a been case report of Oseltamivir induced transient myopia and bilateral acute angle-closure glaucoma secondary to ciliochoroidal effusion due to its dopaminergic effect.[33]
Our study is limited by the absence of slit-lamp biomicroscopic examination and fundus evaluation due to the potential compromise of health care worker safety and the significant technical difficulties of performing while having donned full PPE. Other limitations include lack of conjunctival swab evidence from the symptomatic cases and presence of the said confounding factors.
A thorough understanding of the various ophthalmic manifestations and presentations in COVID-19 infection may help ophthalmologists detect COVID-19 suspects in their clinical practice, thereby enhance early diagnosis for the benefit of the patient's better prognosis and limit the chain of transmission further. Moreover, this will guide clinicians to make better-informed decisions while dealing with potential COVID-19 suspects whether to defer a certain procedure due to its contact or proximity risk or aerosol generation. As Kuo and O'Brien rightly pointed out that Ophthalmologists face an increased occupational risk of contracting nosocomial COVID-19 infection due to the proximity of examination and various contact procedures and without adequate protective measures, this could prove potentially lethal as in the case of Dr. Li Wenliang.[34,35]
Conclusion
Thus, ophthalmic manifestations in the clinical spectrum of COVID-19 infection are uncommon and unlikely to be the presenting clinical impression, yet, an important conundrum in clinical practice that shall catapult regulations and standard operative protocols prompting the eye care team to be vigilant about their own safety while caring for patients. It has also broadened our view to a wider palate of COVID-19 presentations enhancing our clinical acumen for staunch detection of COVID-19 suspects in our daily practice, augmenting early diagnosis and management, thereby help in curbing the associated morbidity and mortality amongst our patients and also break the chain of transmission for the greater good of humanity.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Chen Y, Liu Q, Guo D. Emerging coronaviruses: Genome structure, replication, and pathogenesis. J Med Virol. 2020;92:418–23. doi: 10.1002/jmv.25681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Transmission of SARS-CoV-2: Implications for infection prevention precautions [Internet] Last cited on 2020 Jul 27. Available from: https://www.who.int/news-room/commentaries/detail/transmission-of-sars-cov-2-implications-for-infection-prevention-precautions .
- 3.Cascella M, Rajnik M, Cuomo A, Dulebohn SC, Di Napoli R. StatPearls. Treasure Island (FL): StatPearls Publishing; 2020. Features, Evaluation and Treatment Coronavirus (COVID-19) [Internet] Last cited on 2020 Aug 03. Available from: http://www.ncbi.nlm.nih.gov/books/NBK554776/ [PubMed] [Google Scholar]
- 4.Fu L, Wang B, Yuan T, Chen X, Ao Y, Fitzpatrick T, et al. Clinical characteristics of coronavirus disease 2019 (COVID-19) in China: A systematic review and meta-analysis. J Infect. 2020;80:656–65. doi: 10.1016/j.jinf.2020.03.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Million M, Lagier J-C, Gautret P, Colson P, Fournier P-E, Amrane S, et al. Early treatment of COVID-19 patients with hydroxychloroquine and azithromycin: A retrospective analysis of 1061 cases in Marseille, France. Travel Med Infect Dis. 2020;35:101738. doi: 10.1016/j.tmaid.2020.101738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sharma R, Agarwal M, Gupta M, Somendra S, Saxena SK. Clinical Characteristics and Differential Clinical Diagnosis of Novel Coronavirus Disease 2019 (COVID-19) Coronavirus Disease 2019 (COVID-19) 2020:55–70. Published 2020 Apr 30. doi:10.1007/978-981-15-4814-7_6. [Google Scholar]
- 7.Guo D, Xia J, Wang Y, Zhang X, Shen Y, Tong J-P. Relapsing viral keratoconjunctivitis in COVID-19: A case report. Virol J. 2020;17:97. doi: 10.1186/s12985-020-01370-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wu P, Duan F, Luo C, Liu Q, Qu X, Liang L, et al. Characteristics of ocular findings of patients with coronavirus disease 2019 (COVID-19) in Hubei Province, China. JAMA Ophthalmol. 2020;138:575–8. doi: 10.1001/jamaophthalmol.2020.1291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.WHO | Case Definitions for Surveillance of Severe Acute Respiratory Syndrome (SARS) [Internet]. WHO. Last cited on 2020 Aug 02. Available from: https://www.who.int/csr/sars/casedefinition/en/
- 10.Guidelines on rational use of Personal Protective Equipment. pdf [Internet] Last cited on 2020 Jul 28. Available from: https://www.mohfw.gov.in/pdf/GuidelinesonrationaluseofPersonalProtectiveEquipment.pdf .
- 11.Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: Summary of a report of 72 314 cases from the Chinese Center for disease control and prevention. JAMA. 2020;323:1239–42. doi: 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]
- 12.Guan W, Ni Z, Hu Y, Liang W, Ou C, He J, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382:1708–20. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Loon S-C, Teoh SCB, Oon LLE, Se-Thoe S-Y, Ling A-E, Leo Y-S, et al. The severe acute respiratory syndrome coronavirus in tears. Br J Ophthalmol. 2004;88:861–3. doi: 10.1136/bjo.2003.035931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Xia J, Tong J, Liu M, Shen Y, Guo D. Evaluation of coronavirus in tears and conjunctival secretions of patients with SARS-CoV-2 infection. J Med Virol. 2020;92:589–94. doi: 10.1002/jmv.25725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.van der Hoek L, Pyrc K, Jebbink MF, Vermeulen-Oost W, Berkhout RJM, Wolthers KC, et al. Identification of a new human coronavirus. Nat Med. 2004;10:368–73. doi: 10.1038/nm1024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gengler I, Wang JC, Speth MM, Sedaghat AR. Sinonasal pathophysiology of SARS-CoV-2 and COVID-19: A systematic review of the current evidence. Laryngoscope Investig Otolaryngol [Internet] 2020. cited 2021 Feb 3. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7262250 . [DOI] [PMC free article] [PubMed]
- 17.Khan IH, Savarimuthu S, Leung MST, Harky A. The need to manage the risk of thromboembolism in COVID-19 patients. J Vasc Surg. 2020;72:799–804. doi: 10.1016/j.jvs.2020.05.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.McIntosh K. Coronaviruses: A comparative review. In: Arber W, Haas R, Henle W, Hofschneider PH, Jerne NK, Koldovský P, et al., editors. Current Topics in Microbiology and Immunology/Ergebnisse der Mikrobiologie und Immunitätsforschung. Berlin, Heidelberg: Springer; 1974. pp. 85–129. [Google Scholar]
- 19.Wagner J, Danser AHJ, Derkx FH, de Jong TV, Paul M, Mullins JJ, et al. Demonstration of renin mRNA, angiotensinogen mRNA, and angiotensin converting enzyme mRNA expression in the human eye: Evidence for an intraocular renin-angiotensin system. Br J Ophthalmol. 1996;80:159–63. doi: 10.1136/bjo.80.2.159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lange C, Wolf J, Auw-Haedrich C, Schlecht A, Boneva S, Lapp T, et al. Expression of the COVID-19 receptor ACE2 in the human conjunctiva. J Med Virol. 2020;92:2081–6. doi: 10.1002/jmv.25981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jia HP, Look DC, Shi L, Hickey M, Pewe L, Netland J, et al. ACE2 receptor expression and severe acute respiratory syndrome coronavirus infection depend on differentiation of human airway epithelia. J Virol. 2005;79:14614–21. doi: 10.1128/JVI.79.23.14614-14621.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Keratoconjunctivitis as the initial medical presentation of the novel coronavirus disease 2019 (COVID-19) [Internet] Last cited on 2020 Aug 05. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7124283/ [DOI] [PMC free article] [PubMed]
- 23.Lu C, Liu X, Jia Z. 2019-nCoV transmission through the ocular surface must not be ignored. Lancet. 2020;395(10224):e39. doi: 10.1016/S0140-6736(20)30313-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Li J-PO, Lam DSC, Chen Y, Ting DSW. Novel coronavirus disease 2019 (COVID-19): The importance of recognising possible early ocular manifestation and using protective eyewear. Br J Ophthalmol. 2020;104:297–8. doi: 10.1136/bjophthalmol-2020-315994. [DOI] [PubMed] [Google Scholar]
- 25.Grixti A, Sadri M, Datta AV. Uncommon ophthalmologic disorders in intensive care unit patients. J Crit Care. 2012;27:746.e9–22. doi: 10.1016/j.jcrc.2012.07.013. [DOI] [PubMed] [Google Scholar]
- 26.Alansari MA, Hijazi MH, Maghrabi KA. Making a Difference in Eye Care of the Critically Ill Patients. J Intensive Care Med. 2015;30(6):311–7. doi: 10.1177/0885066613510674. [DOI] [PubMed] [Google Scholar]
- 27.Mela EK, Drimtzias EG, Christofidou MK, Filos KS, Anastassiou ED, Gartaganis SP. Ocular surface bacterial colonisation in sedated intensive care unit patients. Anaesth Intensive Care. 2010;38:190–3. doi: 10.1177/0310057X1003800129. [DOI] [PubMed] [Google Scholar]
- 28.Ruamviboonsuk P, Lai TYY, Chang A, Lai C-C, Mieler WF, Lam DSC, et al. Chloroquine and hydroxychloroquine retinal toxicity consideration in the treatment of COVID-19. Asia Pac J Ophthalmol. 2020;9:85–7. doi: 10.1097/APO.0000000000000289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Moorthy RS, Moorthy MS, Cunningham ET. Drug-induced uveitis. Curr Opin Ophthalmol. 2018;29:588–603. doi: 10.1097/ICU.0000000000000530. [DOI] [PubMed] [Google Scholar]
- 30.Fraunfelder FW, Rosenbaum JT. Drug-induced uveitis.Incidence, prevention and treatment. Drug Saf. 1997;17:197–207. doi: 10.2165/00002018-199717030-00005. [DOI] [PubMed] [Google Scholar]
- 31.Wang Y, Zhang D, Du G, Du R, Zhao J, Jin Y, et al. Remdesivir in adults with severe COVID-19: A randomised, double-blind, placebo-controlled, multicentre trial. Lancet. 2020;395:1569–78. doi: 10.1016/S0140-6736(20)31022-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Chen C, Zhang Y, Huang J, Yin P, Cheng Z, Wu J, et al. Favipiravir versus Arbidol for COVID-19: A randomized clinical trial [Internet]. Infectious Diseases (except HIV/AIDS) 2020. Last cited on 2020 Aug 07. Available from: http://medrxiv.org/lookup/doi/100.1101/2020.03.17.20037432 .
- 33.Lee JW, Lee JE, Choi HY, Lee JS. Oseltamivir (Tamiflu)-induced bilateral acute angle closure glaucoma and transient myopia. Indian J Ophthalmol. 2014;62:1165–7. doi: 10.4103/0301-4738.109531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kuo, Irene C, Terrence P O'Brien. “COVID-19 and ophthalmology: an underappreciated occupational hazard.” Infection control and hospital epidemiology vol. 41, 10 (2020) :1207–1208. doi: 10.1017/ice.2020.238. doi:10.1017/ice.2020.238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Li Wenliang: Ophthalmologist hero [Internet] Ophthalmol. Times. Last cited on 2020 Aug 05. Available from: https://www.ophthalmologytimes.com/view/li-wenliang-ophthalmologist-hero .


