Abstract
Purpose:
The aim of this study was to evaluate tumor control of OSSN with topical IFNα2b alone based on tumor configuration (flat versus (vs.) dome-shaped).
Methods:
Retrospective, nonrandomized, interventional cohort study on 64 consecutive tumors in 63 patients with OSSN treated with topical IFNα2b. Topical IFNα2b (1 million international units/cc) was compounded and provided by the Thomas Jefferson University Hospital Pharmacy to be refrigerated and applied 4 times daily until biomicroscopic evidence of tumor resolution was observed.
Results:
The tumor configuration was flat (n = 15, 23%) or dome-shaped (n = 49, 77%). A comparison (flat vs. dome-shaped) revealed dome-shaped with older mean patient age at presentation (62 vs. 70 years, P = 0.04), greater patient history of smoking (13% vs. 42%, P = 0.04), greater corneal involvement (7% vs. 82%, P < 0.001), larger mean basal diameter (5.5 vs. 12.4 mm, P = 0.001) and mean thickness (1.9 vs. 4.3, P = 0.002), and longer mean duration IFNα2b therapy (3.7 vs. 6.3 months, P = 0.002). There was no difference in mean follow-up time (22.2 vs 23.1 months) or time to complete response (5.0 vs. 6.1 months). There was no difference in achievement of complete tumor control with IFNα2b alone (93% vs. 96%). There were no cases with metastasis or death.
Conclusion:
Topical IFNα2b alone shows excellent overall tumor control of 95% with no difference in efficacy based on tumor configuration.
Keywords: Configuration, conjunctiva, dome-shaped, flat, interferon alpha-2b, ocular surface squamous neoplasia, squamous cell carcinoma, treatment
Ocular surface squamous neoplasia (OSSN) is an umbrella term referring to the spectrum of squamous epithelial malignancy that can occur on the ocular surface, from in situ mild dysplasia to invasive epithelial malignant tumors. Based on the National Institutes of Health (NIH) American Association of Retired Persons (AARP) Diet and Health Study of 566,401 individuals aged 50-71 years, the incidence of OSSN was 8.4 per million persons, and found to be greater incidence in males (10.3 per million) and age >60 years (10.0 per million).[1] The management of this malignancy involves surgical and non-surgical alternatives, using topical or injection chemotherapy or immunotherapy. Several publications have explored the role of topical interferon alpha 2-B (IFNα2b) for tumor management.[1,2,3] A matched comparative analysis (IFNα2b (topical and injections) versus (vs.) surgery) for OSSN therapy revealed no difference in the recurrence rate (3% vs. 5%)[4] and non-significant equivalent cost for the full course of the two alternatives ($2831 vs $3528 US dollars (Medicare allowable charges)).[5] Thus, topical and injection IFNα2b for OSSN remains an important therapeutic alternative to surgery for affected patients.
Herein, we specifically focus on the role of topical IFNα2b monotherapy in the management of OSSN. In this analysis, we explore tumor control with topical IFNα2b based on tumor configuration (flat versus (vs.) dome-shaped). Many clinicians using topical therapies apply the medications based on classic tumor features and without the need for tumor biopsy, to spare the patient surgical intervention. Thus, tumor grouping by the American Joint Committee on Cancer (AJCC) Classification is not possible, as histopathology evaluation of tumor depth (in situ vs. deeper) is not available. However, one might speculate that tumor configuration as flat could serve as a surrogate for Tis and configuration as dome-shaped could represent T1, T2, T3, or T4 based on tumor basal dimension and adjacent tissue involvement as proposed by the AJCC.[6] Herein, we explore outcomes of topical IFNα2b based on practical tumor configuration, whether the tumor is thin (flat) or thick (dome-shaped).
Methods
The medical records of all patients with clinically-evident OSSN diagnosed and managed on the Ocular Oncology Service at Wills Eye Hospital, Philadelphia USA, between October 4, 2005, and January 28, 2019 were retrospectively reviewed. Patients were included if primary treatment for OSSN consisted only of topical IFNα2b monotherapy. Patients who received treatment prior to referral, or those who received subconjunctival injection of IFNα2b or were treated with prophylactic IFNα2b were excluded. The treatment protocol included use of IFNα2b (Intron-A, Schering-Plough, London UK) in a topical formulation of 1 million international units (IU)/mL compounded by Thomas Jefferson University Hospital Pharmacy, Philadelphia USA, and stored in refrigeration, avoiding disturbance or shaking of the bottle. The eye drops were administered 4 times daily until 1 month beyond clinical evidence of complete tumor resolution or until the time a secondary treatment was deemed necessary due to poor response. The response to treatment was monitored every 3 to 6 months and the duration of treatment was modified on the basis of tumor response. This study was approved by the Institutional Review Board of Wills Eye Hospital, Philadelphia USA and adhered to the tenets of the Declaration of Helsinki. Informed consent was obtained from all patients.
All patients were examined by a trained ocular oncologist (CLS, SEL) with slit-lamp biomicroscopy, documentation on detailed, large conjunctival drawings, and with photographic documentation. The demographic data included age, race, sex, and Fitzpatrick skin type. Past medical history included risk factors of smoking status, autoimmune condition, chronic use (>6 months) of topical or systemic corticosteroids or other immunosuppressive medications, organ transplant, corneal graft, human papillomavirus (HPV) infection, human immunodeficiency virus infection, and cutaneous or mucous membrane squamous cell carcinoma. Clinical findings at presentation included best-corrected visual acuity), tumor laterality, tumor multiplicity, tissues involved (bulbar conjunctiva, forniceal conjunctiva, tarsal conjunctiva, plica semilunaris, caruncle, cornea, eyelid, and orbit), quadrant or location involved (superior, temporal, inferior, nasal, diffuse), largest tumor basal diameter, number of clock hours involved, tumor configuraton (flat, dome-shaped), lesion color, feeder and intrinsic vessels, leukoplakia, and internal pigment. The tumor configuration was considered flat if there was a flat surface of ≤1 mm thickness, whereas the tumors were considered dome-shaped if the mass gradually increased in thickness from the margin to a central apex and were >1 mm thickness centrally.
The number of months of topical IFNα2b therapy were recorded. At each follow-up examination, features were recorded regarding best-corrected visual acuity, tumor basal diameter, tissue involvement, and interferon-induced toxicity. Treatment outcomes included tumor control (complete, partial, or no response), recurrence, treatment for recurrence, metastasis, and death. Complete response was defined as complete tumor regression with total disappearance of tumor. Partial response was defined as tumor regression of less than 100%. No response was defined as no visible change following therapy. Recurrence was defined as reappearance of tumor at the primary tumor location after complete resolution following topical IFNα2b. Additional treatment required for tumor control after primary topical IFNα2b was noted. Spread to regional lymph nodes was assessed by history and palpation of preauricular, submental, submandibular, and cervical lymph nodes at each visit. Distant metastasis and death per the general medical physician were recorded.
Demographics, clinical features, and outcomes were compared by tumor configuration (flat vs. dome-shaped) using Fisher's exact test, Chi-squared test, and Mann Whitney U test. A P value <0.05 was considered significant.
Results
Of the 236 consecutive patients with clinically evident OSSN evaluated and managed on the Ocular Oncology Service, Wills Eye Hospital, during this time period, there were 64 tumors in 63 eyes of 63 patients that met inclusion criteria for this study. Tumors were classified according to surface configuration (flat (thin) (n = 15, 23%) vs. dome-shaped (thick) (n = 49, 77%)).
The patient demographic features are listed in Table 1. A comparison (flat vs. dome-shaped) revealed dome-shaped tumors with older mean patient age (62 vs. 70 years, P = 0.04) and greater frequency of smoking (13% vs. 42%, P = 0.04). There was no difference regarding patient race, sex, or Fitzpatrick Skin Type, autoimmune disease, immunosuppression, medical history of squamous neoplasia elsewhere, and tumor laterality and multiplicity.
Table 1.
Primary Treatment of Ocular Surface Squamous Neoplasia with Topical Interferon Alpha-2b in 64 Cases of 63 Patients. Demographic features
| Demographic Features | Flat [Tis] (n=15 patients) [n (%)] | Dome-shaped [T3] (n=48 patients) [n (%)] | P | Total (n=63 patients) [n (%)] |
|---|---|---|---|---|
| Age (years) | ||||
| Mean (median, range) | 62 (61, 45-85) | 70 (68, 30-97) | 0.04 | 68 (64, 30-97) |
| Race | ||||
| Caucasian | 14 (93) | 45 (94) | 0.67 | 59 (94) |
| African American | 1 (7) | 1 (2) | 2 (3) | |
| Hispanic | 0 (0) | 1 (2) | 1 (2) | |
| Asian | 0 (0) | 1 (2) | 1 (2) | |
| Sex | ||||
| Male | 8 (53) | 27 (56) | 0.84 | 35 (56) |
| Female | 7 (47) | 21 (44) | 28 (44) | |
| Fitzpatrick Skin Type | ||||
| I | 4 (27) | 17 (35) | 0.73 | 21 (33) |
| II | 9 (60) | 23 (48) | 32 (51) | |
| III | 1 (7) | 5 (10) | 6 (10) | |
| IV | 0 (0) | 2 (4) | 2 (3) | |
| V | 0 (0) | 0 (0) | 0 (0) | |
| VI | 1 (7) | 1 (2) | 2 (3) | |
| Smoking History | ||||
| Yes | 2 (13) | 20 (42) | 0.04 | 22 (34) |
| No | 13 (87) | 28 (58) | 42 (66) | |
| Medical History - Autoimmune | ||||
| Celiac | 0 (0) | 1 (2) | 0.77 | 1 (2) |
| Ocular cicatricial pemphigoid | 0 (0) | 1 (2) | 0.77 | 1 (2) |
| Psoriatic arthritis | 1 (7) | 0 (0) | 0.23 | 1 (2) |
| Rheumatoid arthritis* | 0 (0) | 1 (2) | 0.77 | 1 (2) |
| Sjögren’s syndrome* | 0 (0) | 1 (2) | 0.77 | 1 (2) |
| Thyroiditis | 0 (0) | 1 (2) | 0.77 | 1 (2) |
| Medical History - Immunosuppression | ||||
| Chronic systemic corticosteroids | 1 (7) | 2 (4) | 0.56 | 3 (5) |
| Chronic systemic immunosuppressants | 1 (7) | 2 (4) | 0.56 | 3 (5) |
| Chronic topical corticosteroids | 0 (0) | 1 (2) | 0.99 | 1 (2) |
| Organ transplant | 0 (0) | 1 (2) | 0.99 | 1 (2) |
| Corneal graft | 0 (0) | 2 (4) | 0.99 | 2 (3) |
| HPV history | 1 (7) | 1 (2) | 0.42 | 2 (3) |
| Medical History - SCC History | ||||
| Skin SCC | 2 (13) | 6 (13) | 0.93 | 8 (13) |
| Mucosal SCC** | 0 (0) | 2 (4) | 0.99 | 2 (3) |
| Laterality | ||||
| Right | 4 (27) | 25 (52) | 0.40 | 29 (46) |
| Left | 11 (73) | 23 (48) | 34 (54) | |
| Multiplicity of tumors | ||||
| Single | 15 (100) | 47 (98) | 0.99 | 62 (98) |
| Multiple | 0 (0) | 1 (2) | 1 (2) |
HPV=Human papilloma virus, SCC=squamous cell carcinoma. Bold values indicate significant P. * There was one patient diagnosed with both rheumatoid arthritis and Sjögren’s syndrome. **There was one case of oropharyngeal SCC and one case of rectal SCC
The tumor features are listed in Table 2. At presentation, there was no evidence of lymph node or distant metastatic disease. A comparison (flat vs. dome-shaped) revealed dome-shaped tumors with greater corneal involvement (7%% vs. 82%, P < 0.001), greater mean basal diameter (5.5 vs. 12.4 mm, P = 0.001) and greater mean clock hour involvement (1.9 vs. 4.1, P = 0.002). There was no difference in tumor quadrant, growth pattern, color, vascularity, or additional features.
Table 2.
Primary Treatment of Ocular Surface Squamous Neoplasia with Topical Interferon Alpha-2b in 64 Cases: Tumor characteristics
| Tumor Characteristics | Flat [Tis] (n=15 tumors) [n (%)] | Dome-shaped [T3] (n=49 tumors) [n (%)] | P | Total (n=64 tumors) [n (%)] |
|---|---|---|---|---|
| Tissue involved | ||||
| Bulbar | 13 (87) | 41 (84) | 0.78 | 54 (84) |
| Fornix | 0 (0) | 9 (18) | 0.07 | 9 (14) |
| Tarsus | 2 (13) | 6 (12) | 0.91 | 8 (13) |
| Plica semilunaris | 0 (0) | 1 (2) | 0.99 | 1 (2) |
| Caruncle | 0 (0) | 2 (4) | 0.99 | 2 (3) |
| Cornea | 1 (7%) | 40 (82) | <0.001 | 41 (64) |
| Eyelid | 0 (0) | 2 (4) | 0.99 | 2 (3) |
| Orbit | 0 (0) | 0 (0) | NA | 0 (0) |
| Quadrant involved | ||||
| Superior | 1 (7) | 4 (8) | 0.97 | 5 (8) |
| Temporal | 3 (20) | 10 (20) | 13 (20) | |
| Inferior | 2 (13) | 9 (18) | 11 (17) | |
| Nasal | 9 (60) | 25 (51) | 34 (53) | |
| Diffuse | 0 (0) | 1 (2) | 1 (2) | |
| Tumor Size | ||||
| Largest basal diameter (mm) Mean (median, range) | 5.5 (5.0, 1.0-12.0) | 12.4 (10.0, 1.5-60.0) | 0.001 | 10.8 (8.2, 1.0-60.0) |
| Number of clock hours involved Mean (median, range) | 1.9 (2.0, 1.0-5.0) | 4.1 (3.0, 1.0-12.0) | 0.002 | 3.6 (3.0, 1.0-12.0) |
| Tumor Color | ||||
| Pink | 2 (13) | 6 (12) | 0.99 | 8 (12) |
| Yellow | 10 (67) | 34 (69) | 44 (69) | |
| White | 3 (20) | 9 (18) | 12 (19) | |
| Tumor Vascularity | ||||
| Intrinsic vessels | 8 (53) | 28 (57) | 0.80 | 36 (56) |
| Feeder vessels | 6 (40) | 18 (37) | 0.82 | 24 (37) |
| Additional features | ||||
| Leukoplakia | 5 (33) | 8 (16) | 0.15 | 13 (20) |
| Internal cysts | 1 (7) | 0 (0) | 0.23 | 1 (2) |
| Internal pigment | 0 (0) | 0 (0) | NA | 0 (0) |
Bold values indicate significant P
Topical IFNα2b at a dose of 1 million IU/mL administered 4 times daily was used as primary monotherapy for all patients. The tumor response is listed in Table 3. There was no difference in percentage of patients lost to follow-up (7% vs. 2%, P = 0.42) or mean follow-up time (22.2 vs. 23.1 months, P = 0.87). A comparison (flat vs. dome-shaped) revealed dome-shaped tumors with longer mean duration of IFNα2b monotherapy for tumor control (3.7 vs. 6.3 months, P = 0.002). There was no difference in complete tumor response (93% vs. 96%, (P = 0.65), partial response (7% vs. 2%), or no response (0% vs. 2%) (P = 0.54) [Fig. 1]. The single patient with no response had prior corneal graft and received topical IFNα2b with no improvement, and later required subconjunctival IFNα2b injection. There was no difference regarding mean time to complete response (5.0 vs. 6.1 months, P = 0.25). Following initial response, there was no difference in tumor recurrence (7% vs. 2%, P = 0.41). Regarding local treatment side effects, flat tumors had more frequent follicular reaction (20% vs. 2%, P = 0.04). There was no difference in ocular surface irritation or corneal epithelial defect. There were no patients who developed metastatic disease or death.
Table 3.
Primary Treatment of Ocular Surface Squamous Neoplasia with Topical Interferon Alpha-2b in 64 Cases: Outcomes
| Outcomes | Flat [Tis] (n=15 tumors) [n (%)] | Dome-shaped [T3] (n=49 tumors) [n (%)] | P | Total (n=64 tumors) [n (%)] |
|---|---|---|---|---|
| No follow-up | 1 (7) | 1 (2) | 0.42 | 2 (3) |
| Tumor response | n=14 | n=48 | n=62 | |
| Complete | 13 (93) | 46 (96) | 0.54 | 59 (95) |
| Partial | 1 (7)* | 1 (2)** | 2 (3) | |
| No response | 0 (0) | 1 (2)*** | 1 (2) | |
| n=14 | n=47 | n=61 | ||
| Recurrence after initial response | 1 (7) | 1 (2) | 0.41 | 2 (3) |
| Additional treatment needed for complete response | 1 (7) | 6 (13) | 0.68 | 7 (11) |
| Topical mitomycin C | 0 (0) | 1 (2) | 0.99 | 1 (2) |
| Surgical excision | 1 (7) | 5 (9) | 0.99 | 6 (10) |
| Local treatment side effects | ||||
| Follicular reaction | 3 (20) | 1 (2) | 0.04 | 4 (6) |
| Irritation | 0 (0) | 1 (2) | 0.99 | 1 (2) |
| Corneal epithelial defect | 0 (0) | 1 (2) | 0.99 | 2 (3) |
| Systemic outcomes | ||||
| Metastasis | 0 (0) | 0 (0) | NA | 0 (0) |
| Death | 0 (0) | 0 (0) | NA | 0 (0) |
| Total duration of interferon alpha-2b therapy (months) | ||||
| Mean (median, range) | 3.7 (3.0, 0.5-7.0) | 6.3 (6.0, 1.0-13.0) | 0.002 | 5.7 (5.0, 0.5-13.0) |
| Time to complete response (months) | ||||
| Mean (median, range) | 5.0 (3.8, 1.0-11.5) | 6.1 (5.4, 1.3-17.8) | 0.25 | 5.8 (5.0, 1.0-17.8) |
| Follow-up time (months) | n=14 | n=48 | n=62 | |
| Mean (median, range) | 22.2 (14.3, 2.9-63.1) | 23.1 (13.9, 1.3-114.6) | 0.87 | 23.0 (14.4, 1.3-114.6) |
Bold values indicate significant P. * Patient lost to follow-up after 7 months of therapy due to liver transplant. ** Patient stopped interferon alpha-2b after 1 month due to ocular surface discomfort and was lost to follow-up. *** Patient elected not to continue treatment after secondary treatment was advised
Figure 1.
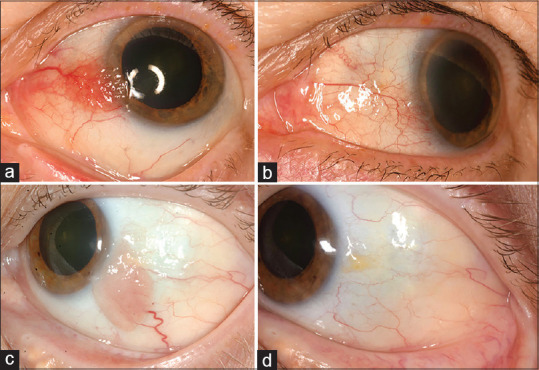
Treatment of ocular surface squamous neoplasia (OSSN) using topical interferon alpha-2b (IFNa2b) monotherapy. Flat vascular OSSN in a 76-year-old female (a) before and (b) after 4 months of IFNa2b monotherapy. Dome-shaped OSSN in a 57-year-old female (c) before and (d) after 8 months of IFNa2b monotherapy
Discussion
A recent report of 5002 conjunctival tumors from an ocular oncology center revealed that premalignant/malignant squamous neoplasia (OSSN) represented 729 (15%) of all cases, mostly with diagnoses of conjunctival intraepithelial neoplasia (CIN) (n = 275 tumors) or squamous cell carcinoma (SCC) (n = 440 tumors).[7] In that analysis, CIN or SCC was most often noted at the corneoscleral limbus (575/715, 80%), located nasally (269/715, 38%) or temporally (285/715, 40%), and appearing as a lump/swelling to the patient (434/715, 61%).
In 2012, Shah et al. reported the results of topical v for OSSN in 23 cases based on the 7th edition AJCC classification and noted that complete control was achieved in 83% of cases, specifically 67% of those labeled as Tis and 85% of the T3 group.[8] In that analysis there were no patients with T1, T2, or T4, as found in our current study. Further investigation of topical or injection IFNα2b for OSSN revealed applications for immunoreduction of giant OSSN, and immunoprevention in immunosuppressed patients, especially those with human immunodeficiency virus (HIV) or organ transplant who are at risk to have numerous and multifocal OSSN.[9,10] Galor et al. compared the topical dose of 1 million IU/ml to 3 million IU/mL IFNα2b and found no difference in tumor response, treatment duration, recurrence, or adverse effects.[11]
Since the above publications, the AJCC has been updated to the 8th edition. However, classification requires tumor biopsy and histopathologic analysis, but in this current era of topical therapies, clinicians often avoid biopsy when starting topical therapies if the diagnosis is clinical evident. Thus, AJCC classification is not possible for clinicians using purely topical therapies. In this report, we accommodate AJCC 8th edition classification by inferring that flat tumor configuration with no corneal component might serve as a surrogate for Tis and dome-shaped as T1, T2, T3, or T4.
In this analysis, we were able to provide a comparative analysis of tumor control with topical IFNα2b monotherapy without the need for biopsy. We found important differences in clinical features in that dome-shaped tumors occurred in older mean patient age (62 vs. 70 years, P = 0.04), with greater patient history of smoking (13% vs. 42%, P = 0.04), greater corneal involvement (0% vs. 84%, P < 0.001), larger mean basal diameter (5.5 vs. 12.4 mm, P = 0.001) and mean clock hour extent (1.9 vs. 4.3, P = 0.002). To achieve control with topical IFNα2b, dome-shaped tumors tumors required greater mean duration IFNα2b therapy (3.7 vs. 6.3 months, P = 0.002) for equivalent complete tumor control (93% vs. 96%, P = 0.65).
There are limitations to this study that should be considered. The data was a retrospective collection with inherent biases and drawbacks. Additionally, the cohort size was relatively small at 64 cases, resulting in limited statistical power, but due to the rarity of this malignancy and strict inclusion criteria of primary treatment with topical IFNα2b monotherapy only, our data represents pure data with few conflicting events. We recognize that precise AJCC classification could not be performed without histopathologic anaylsis, and microscopic invasion of the basement membrane in the case of flat tumor could have been missed. Nevertheless, with excellent tumor control for both flat and dome-shaped tumor, biopsy would not likely have changed our main study conclusion. Perhaps further studies could evaluate outcomes based on clinical imaging such as anterior segment optical coherence tomography or ultrasound biomicroscopy. Lastly, further follow-up with larger cohort in the future could potentially verify our observations.
Most previous studies on this topic have included pretreatment biopsy for diagnostic and staging confirmation, but that interferes with the ability to promptly employ some topical therapies and adds a confounding factor of the amount of tumor surgically excised versus the remnant of tumor left for treatment with topical therapy. Hence, we chose to avoid biopsy as this is consistent with how most clinicians currently approach clinically-evident OSSN, especially when starting topical therapy. Thus our results reflect the impact of topical IFNα2b monotherapy for the entire OSSN without the need for biopsy.
Conclusion
In conclusion, based on tumor configuration of OSSN, overall tumor control is 95% and does not differ when comparing flat to dome-shaped tumors. In addition, dome-shaped tumors required longer duration of therapy and demonstrated no greater recurrence upon discontinuation of the medication. We conclude that topical IFNα2b monotherapy is highly effective for the treatment of conjunctival OSSN, whether or not the tumor is flat or dome-shaped.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Emmanuel B, Ruder E, Lin SW, Abnet C, Hollenbeck A, Mbulaiteye S. Incidence of squamous-cell carcinoma of the conjunctiva and other eye cancers in the NIH-AARP Diet and Health Study. Ecancermedicalscience. 2012;6:254. doi: 10.3332/ecancer.2012.254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sayed-Ahmed IO, Palioura S, Galor A, Karp CL. Diagnosis and medical management of ocular surface squamous neoplasia. Expert Rev Ophthalmol. 2017;12:11–9. doi: 10.1080/17469899.2017.1263567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cincinelli MV, Marchese A, Bandello F, Modorati G. Clinical management of ocular surface squamous neoplasia: A review of the current evidence. Ophthalmol Ther. 2018;7:247–62. doi: 10.1007/s40123-018-0140-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nanji AA, Moon CS, Galor A, Sein J, Oellers P, Karp CL. Surgical versus medical treatment of ocular surface squamous neoplasia: A comparison of recurrences and complications. Ophthalmology. 2014;121:994–1000. doi: 10.1016/j.ophtha.2013.11.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Moon CS, Nanji AA, Galor A, McCollister KE, Karp CL. Surgical versus medical treatment of ocular surface squamous neoplasia: A cost comparison. Ophthalmology. 2016;123:497–504. doi: 10.1016/j.ophtha.2015.10.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Conway RM, Graue GF, Pelayes . Conjunctival carcinoma. In: Amin MB, Edge SB, Greene FL, editors. AJCC Cancer Staging Manual. (8th edition) Springer International Publishing; 2017. pp. 787–93. [Google Scholar]
- 7.Shields CL, Alset AE, Boal NS, Casey MG, Knapp AN, Sugarman JA, et al. Conjunctival tumors in 5002 cases. Comparative analysis of benign versus malignant counterparts. The 2016 James D. Allen lecture. Am J Ophthalmol. 2016;173:106–33. doi: 10.1016/j.ajo.2016.09.034. [DOI] [PubMed] [Google Scholar]
- 8.Shah SU, Kaliki S, Kim HJ, Lally SE, Shields JA, Shields CL. Topical interferon alfa-2b for management of ocular surface squamous neoplasia in 23 cases: Outcomes based on the American Joint Committee on Cancer classification. Arch Ophthalmol. 2102;130:159–64. doi: 10.1001/archophthalmol.2011.385. [DOI] [PubMed] [Google Scholar]
- 9.Shields CL, Kaliki S, Kim HJ, Al-Dahmash S, Shah SU, Lally SE, et al. Interferon for ocular surface squamous neoplasia in 81 cases: Outcomes based on the American Joint Committee on Cancer classification. Cornea. 2013;32:248–56. doi: 10.1097/ICO.0b013e3182523f61. [DOI] [PubMed] [Google Scholar]
- 10.Kim HJ, Shields CL, Shah SU, Kaliki S, Lally SE, Shields JA. Giant ocular surface squamous neoplasia managed with interferon alpha-2b as immunotherapy or immunoreduction. Ophthalmology. 2012;119:938–44. doi: 10.1016/j.ophtha.2011.11.035. [DOI] [PubMed] [Google Scholar]
- 11.Galor A, Karp CL, Chhabra S, Barnes S, Alfonso EC. Topical interferon alpha 2b eyedrops for treatment of ocular surface squamous neoplasia: A dose comparison study. Br J Ophthalmol. 2010;94:551–4. doi: 10.1136/bjo.2008.153197. [DOI] [PubMed] [Google Scholar]


