Abstract
Background
COVID-19 has created barriers to the delivery of health care services, including dental care. This study sought to quantify the change in dental visits in 2020 compared with 2019.
Methods
This retrospective, observational study examined the percentage change in weekly visits to dental offices by state (inclusive of the District of Columbia), nationally, and by county-level COVID-19 incidence using geographic information from the mobile applications of 45 million smartphones during 2019 and 2020.
Results
From March through August 2020, weekly visits to dental offices were 33% lower, on average, than in 2019. Weekly visits were 34% lower, on average, in counties with the highest COVID-19 rates. The greatest decline was observed during the week of April 12, 2020, when there were 66% fewer weekly visits to dental offices. The 5 states (inclusive of the District of Columbia) with the greatest declines in weekly visits from 2019 through 2020, ranging from declines of 38% through 53%, were California, Connecticut, District of Columbia, Massachusetts, and New Jersey.
Conclusions
Weekly visits to US dental offices declined drastically during the early phases of the COVID-19 pandemic. Although rates of weekly visits rebounded substantially by June 2020, rates remain about 20% lower than the prior year as of August 2020. These findings highlight the economic challenges faced by dentists owing to the pandemic.
Practical Implications
States exhibited widespread variation in rates of declining visits during the pandemic, suggesting that dental practices may need to consider different approaches to reopening and encouraging patients to return depending on location.
Key Words: Access to care, dental offices, dental health services, utilization of care
Abbreviation Key: ADA, American Dental Association; NAICS, North American Industry Classification System
The COVID-19 pandemic has resulted in substantial changes to the delivery of health care services. Studies have already documented declines in use of outpatient and emergency medical services in the United States owing to the pandemic.1 , 2 Dentistry faces challenges in the delivery of care because common dental procedures generate droplets and aerosols, which likely contribute to the transmission of COVID-19.3 , 4 Little, however, is known about how the pandemic has affected delivery of dental care in the United States.
Many dental offices closed or offered only emergency care during the spring of 2020 owing to the risk of experiencing virus transmission. In the United States, all states (inclusive of the District of Columbia (DC)) restricted dental visits in some way, generally limiting services to only emergency care.5 In a survey conducted by the American Dental Association (ADA) Health Policy Institute, 97% of responding dentists indicated that their offices were seeing emergency patients only or not seeing any patients during the week of April 6, 2020.6 By the week of September 7, 2020, about 99% of responding dentists reported being open, with 50% reporting lower patient volumes than usual.7 In addition, a nationally representative survey of adults conducted at the end of May 2020 reported that about 75% of US adults reported delaying dental care due to the pandemic.8 However, all of these studies relied on self-reported information from surveys, which may have limitations owing to social desirability and nonresponse biases, and most report data from only a single point in time. Thus additional data and analysis are needed to determine the impact of the COVID-19 pandemic on US dental care utilization.
Using aggregated geographic data obtained from smartphones, the aims of this study were to compare the volume of visits in dental offices between 2019 and 2020 and examine how visit volume varied by COVID-19 incidence. We hypothesized that visits to dental offices would be lower in 2020 owing to the pandemic and that the decline in visits over time would be greater in communities with higher rates of COVID-19.
Methods
Data and variables
We used data from SafeGraph, a company that collects aggregate geographic information from the mobile applications of 45 million smartphones in all 50 states and the District of Columbia.9 These data consist of Global Positioning System “pings” from smartphones, which are assigned a unique anonymous identifier for each smartphone, and the time, date, latitude, and longitude of the ping. Typical sources for these data include weather and shopping applications,10 and users of these applications voluntarily agree to share geographic information. The applications providing data are not disclosed by SafeGraph. SafeGraph data have been used by others to examine consumer preferences for restaurants and examine community mobility, social distancing, and COVID-19 transmission.11, 12, 13 For this study, we used SafeGraph’s Core Places and Patterns files providing data for 34 weeks in 2019 and 2020 for the dates of January 6, 2019 through August 31, 2019 and January 5, 2020, through August 29, 2020. The Core Places file and Patterns file include approximately 5 through 6 million business establishments identified by North American Industry Classification System (NAICS) codes, which is a large share of the estimated 7 through 10 million establishments nationally.14 All places in the data are assigned 1 NAICS code, and we identified dental offices using NAICS code 6212. Among the 140,749 unique places identified by NAICS code 6212 in our data set, we excluded 2,230 places (1.6% of the total sample) that, on the basis of a name and Google search, appeared unlikely to be dental offices. By linking the Core Places and Patterns files, we were able to examine visits to dental offices.
We obtained ZIP code−level data from the 2019 novel coronavirus visual dashboard operated by the Johns Hopkins University Center for Systems Science and Engineering to examine variation in visits by local severity of the pandemic as of August 29, 2020.15 We constructed county-level counts of COVID-19 cases per 100,000 population using population estimates from the American Community Survey.16
Analysis
First, we examined the percentage change in weekly visits to dental offices nationally and by state (inclusive of DC). We calculated the percentage difference in weekly visits to dental offices identified in SafeGraph data from the week of January 5, through the week of August 23, 2020, relative to the week of January 6, through the week of August 25, 2019. To illustrate the state-level findings, we stratified states (inclusive of DC) into quartiles on the basis of the percentage difference in visits from 2019 through 2020.
Second, we examined if visit volume varied by COVID-19 incidence. To do so, we used information on the county location of dental offices and then constructed terciles to stratify counties by COVID-19 incidence per 100,000 residents as of August 29, 2020. We constructed these terciles owing to the distribution of the data and for ease of interpretation of results. We plotted the change in weekly visits to dental offices over time. We then estimated a linear regression model to examine if the percentage change in weekly visits from 2020 through 2019 was significantly different in counties by tercile of the county-level COVID-19 incidence rate during the pandemic. The dependent variable was the percentage change in weekly visits from 2020 to 2019 in the weeks of March 8, 2020 and after being compared with the same period in 2019. The key explanatory variable was the tercile of county level-COVID-19 incidence (reference group = counties in lowest tercile of COVID-19 incidence). The model was estimated with robust standard errors.
All analyses were conducted using Stata/MP Version 16.1 (StataCorp). This study was deemed exempt by our institutional review board. No patient consent was required for this research, as the data were anonymous without personal identifiers or contact information.
Results
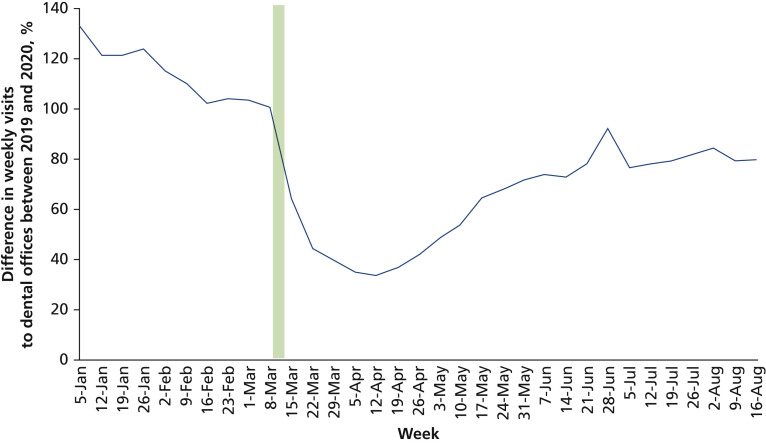
The analytic data set included 43,328,712 total visits to dental offices from January 5 through August 29, 2020, and 55,398,871 total dental visits during the same period in 2019. The largest number of visits during both 2019 and 2020 were observed in Texas, California, and New York. On March 13, 2020, the COVID-19 pandemic was declared a national emergency in the United States.17 Nationally, weekly visits to dental offices were 15% higher, on average, in the weeks before the declaration of a national emergency (January 5-March 7, 2020) than in the corresponding weeks during 2019 (Figure 1 ). From the week of March 8 through the week of August 23, 2020, weekly visits to dental offices were 34% lower, on average, than in the corresponding weeks during 2019. The greatest decline in weekly visits compared with 2019 was observed during the week of April 12, 2020, when there were 66% fewer weekly visits to dental offices.
Figure 1.
Percentage differences in weekly visits to dental offices between 2019 and 2020. Number of weekly visits to dental offices was tracked using smartphone location data. The percentage changes were centered at 100 for ease of interpretation. The green bar illustrates that the COVID-19 pandemic was declared a national emergency in the United States on March 13, 2020.
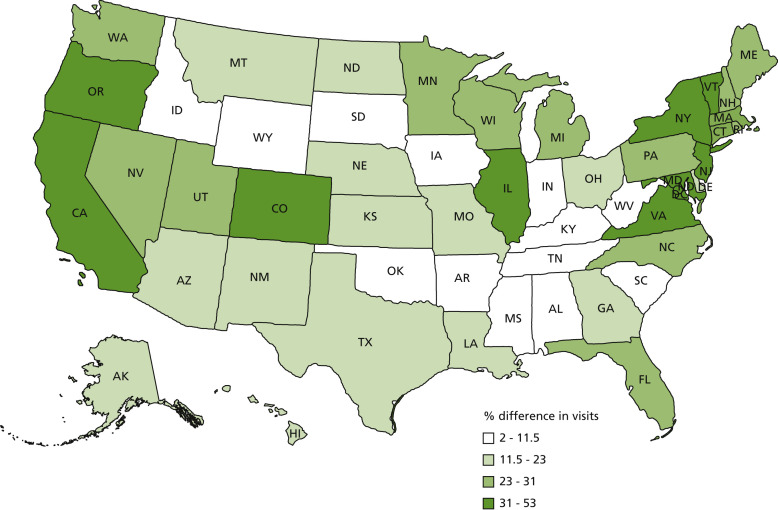
At the state-level, among the 13 states (inclusive of DC) (that is, top quartile) experiencing the greatest declines in weekly visits to dental offices after the declaration of a national emergency, most were located in the Northeast (n = 5) and South (n = 4) US Census regions (Figure 2 ). The 5 states with the greatest declines in weekly visits from 2019 through 2020, ranging from declines of 38% through 53%, were California, Connecticut, Washington, DC, Massachusetts, and New Jersey. The greatest decline was observed in Washington, DC, which experienced a 53% decline in weekly visits. Among the states in the bottom quartile experiencing the smallest declines in weekly visits to dental offices after the declaration of a national emergency, most were located in the South (n = 8) US Census region.
Figure 2.
State-level percentage differences in weekly visits to dental offices from March through August between 2019 and 2020. Map reflects the state-level (inclusive of District of Columbia) unadjusted differences in weekly visits to dental offices from March 8 through the week of August 23, 2020, compared with the same weeks in 2019. Weekly visits to dental offices were tracked using smartphone location data.
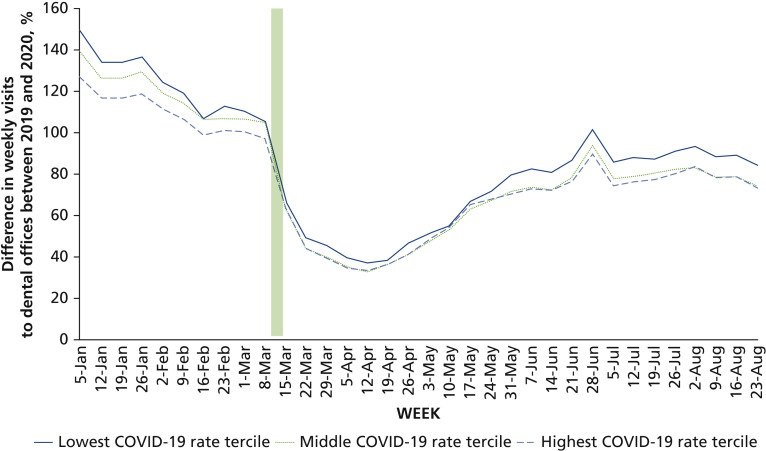
When examined by county level−COVID-19 incidence, the decline in weekly visits was slightly higher in those counties most affected by COVID-19 (Figure 3 ). From the week of March 8 through the week of August 23, 2020, weekly visits to dental offices were 35% lower, on average, than in the corresponding weeks during 2019 in counties with the highest COVID-19 rates. During this same period, weekly visits were 27% lower, on average, than in the corresponding weeks during 2019 in counties with the lowest COVID-19 rates. Results from the regression model allow us to compare the difference in visits between 2019 and 2020 in counties after the declaration of a national emergency (eTable, available at the end of this article). As indicated by the intercept in the regression model, weekly visits declined by 0.8% on average during the pandemic for counties with the lowest COVID-19 incidence. The average decline in weekly visits during the pandemic was 5.7% greater in counties with the highest COVID-19 incidence than in counties with the lowest COVID-19 incidence (95% CI = −7.8 to −3.7; P < .001). The average decline in weekly visits during the pandemic was 8.3% greater in counties in the middle tercile COVID-19 incidence than in counties in the lowest tercile of COVID-19 incidence (95% CI = −10.1 to −6.5; P < .001).
Figure 3.
Percentage differences in weekly visits to dental offices between 2019 and 2020, by cumulative county-level COVID-19 incidence rate per 100,000 population tercile. Number of weekly visits to dental offices was tracked using smartphone location data. The percentage changes were centered at 100 for ease of interpretation. County-level COVID-19 incidence rates per 100,000 population were estimated using data from the Johns Hopkins University Center for Systems Science and Engineering as of August 29, 2020. The green bar illustrates that the COVID-19 pandemic was declared a national emergency in the United States on March 13, 2020.
Discussion
From March through August 2020, there was a large decline in the number of weekly visits to dental offices compared with the corresponding period in 2019. The largest decline was observed during April, a time when many states were encouraging social distancing to avoid the spread of the virus. Visits to dental offices increased through early July but declined again and were 20% lower than the prior year’s rates of weekly visits at the end of August. Although surveys of providers and patients have indicated that the COVID-19 pandemic led to fewer dental visits,6 , 8 this is the first study, to our knowledge, to directly compare the volume of visits in 2019 and 2020 and to use objective data unaffected by self-reporting biases.
Visits to dental offices may have declined during the spring and summer of 2020 for several reasons. First, many dental offices closed during this time in response to mandates and recommendations issued by states and state dental societies that dental offices provide only urgent care.5 Second, even when offices were open, patients may have cancelled or delayed visits owing to fear about contracting COVID-19, a fear that has been documented by media outlets.18 , 19 A survey of US dentists, however, reported that less than 1% of dentists had COVID-19 within the past month, nearly all dentists had implemented enhanced infection control efforts, and 73% of dentists reported using personal protective equipment, as recommended by the Centers for Disease Control and Prevention.20 Finally, even before the pandemic, 13% of nonelderly adults reported financial barriers to receiving dental care, which was higher than any other type of health care,21 and pandemic-related economic uncertainty may further encourage patients to avoid or delay dental care due to cost.
The ADA recommended postponing elective procedures as of March 16, 2020, and all states and DC had some level of closure or reduced services, primarily in March and April.5 , 22 We found declines in visits to dental offices after the declaration of a national emergency across all terciles of COVID-19 incidence per 100,000 county population. Although all communities were likely affected by reductions in dental services regardless of the severity of the pandemic, we observed larger declines in counties with higher COVID-19 rates than in counties with the lowest COVID-19 rates. These findings may be driven by closures of dental offices in areas most affected by the pandemic or patient choices to delay care due to fear of COVID-19. There may also be other characteristics of the communities most affected in the early months of the pandemic that explain this difference. Future studies should examine the impact of the COVID-19 pandemic over a longer period on dental services, as well as how prepandemic levels of access to dentists are associated with declines in dental visits during the pandemic, as well as other factors such as socioeconomic status and the percentage of routine users of dental care in a community.
Furthermore, the pandemic has disproportionally hurt racial and ethnic minority and low-income populations23—populations that are also disproportionally affected by caries and have low rates of dental visits.24 , 25 A survey of US adults conducted in May 2020 reported no difference in delayed dental care due to the pandemic by race and ethnicity8; however, the survey sample was small and did not allow for stratification. The data used in our study lack information on individual characteristics, preventing us from examining this important issue. Further research is needed to understand if historically disadvantaged populations are differentially affected by declines in visits to dental offices, and those studies can potentially use information on the distribution of racial and ethnic groups at the community level. In the interim, efforts to monitor and facilitate dental care access for historically disadvantaged populations during and after the pandemic are needed.
Our study highlights the economic challenges of the pandemic for dentists, as declines in visits correspond to lost revenue. The ADA Health Policy Institute estimates that dental care spending may have declined by up to 38% in 2020, which aligns with our finding that weekly visits to dental offices declined by an average of 33% during March 8 through August 23, 2020.26 Lost revenue may have immediate effects, as more than one-half of dental practices are solo practices.27 Federal funding has been made available to dental practices experiencing economic challenges due to the pandemic, including Paycheck Protection Program loans, Economic Injury Disaster Loans, and grants via the Provider Relief Fund for eligible providers who participate in Medicaid and the Children’s Health Insurance Program.28 , 29 Whether this funding will be sufficient to sustain dental practices remains unclear.
Our study results should be interpreted in the context of its limitations. SafeGraph data provide information on a large national sample of people, representing about 10% through 15% of smartphones in the United States, but do not represent people without smartphones.30 SafeGraph acquires mobile location data through voluntary user opt-ins. Research indicates willingness to opt-in to disclose personal information typically declines with age, so these results may be more representative of younger populations.31 In addition, the smartphones included in the data set may change over time as users install and remove applications; thus our findings are likely suggestive of societal trends rather than the behavior of specific people. Furthermore, we used pings from smartphone visits to dental offices, identified using NAICS code 6212. These pings were used as proxies for dental visits, and we were unable to distinguish between visits made by staff members and patients. We cannot determine what type of treatments patients may have received during visits. If dental offices were underrepresented in these data, we may undercount dental visits. However, as this would affect both 2019 and 2020, we would not expect this to affect the percentage change in weekly visits to dental offices over time. Furthermore, although we took care to exclude places identified by NAICS code 6212 that were unlikely to provide dental care (for example, laboratories making dental materials), this code may be an imprecise identifier of dental offices. We also lacked information on county-level COVID-19 rates for some counties in Utah and Massachusetts and instead used rates aggregated across counties. Finally, we did not account for state (inclusive of Washington, DC)-specific stay-at-home orders or regulations and recommendations for the closure and safe practice of dentistry during the pandemic. As we noted earlier, state-level and ADA guidance encouraged some level of closure or reduced services in dental offices during March and April 2020,5 , 22 indicating all states and DC were affected by closures.
Conclusions
Our study provides important information about declines in weekly visits to US dental offices in 2020. Although rates of weekly visits were 66% lower in April 2020 than in April 2019, by early August 2020, rates had rebounded somewhat and were about 20% lower than in 2019. States exhibited widespread variation in declining visits, suggesting that dental practices may need to consider different approaches to reopening and encouraging patients to return depending on location.
Biographies
Dr. Kranz is a policy researcher at the RAND Corporation, Arlington, VA.
Dr. Chen is an assistant policy researcher at the RAND Corporation, Santa Monica, CA and a PhD student, Pardee RAND Graduate School, Santa Monica, CA.
Ms. Gahlon is a research assistant at RAND Corporation, Arlington, VA.
Dr. Stein is a senior physician policy researcher at the RAND Corporation, Pittsburgh, PA.
Footnotes
Disclosure. None of the authors reported any disclosures.
This research was funded by grants R01 DE026136-03 and R01 DE028530-01A1 from the National Institute of Dental and Craniofacial Research. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Dental and Craniofacial Research or the National Institutes of Health. The funding source had no involvement in study design; collection, analysis, and interpretation of data; writing of the report; or decision to submit the article for publication.
Supplemental data related to this article can be found at https://doi.org/10.1016/j.adaj.2021.02.016.
Supplemental Data
eTable.
Results of regression model examining percent change in weekly visits to dental offices between 2019 and 2020.∗
| TERCILE OF COUNTY-LEVEL COVID-19 INCIDENCE RATE | COEFFICIENT | 95% CONFIDENCE INTERVAL | P VALUE |
|---|---|---|---|
| Lowest [Reference] | |||
| Middle | −8.9 | −10.7 to −7.1 | < .001 |
| Highest | −5.6 | −7.7 to −3.5 | < .001 |
| Intercept† | −0.6 | −2.1 to 0.9 | .435 |
Data are from a linear regression model with robust standard errors, using the county-week as the unit of observation (N = 66,817), examining the percentage change in weekly visits to dental offices during the pandemic (weeks of March 8, 2020, and later) compared with the same period in 2019.
The intercept is interpreted as the average change in weekly visits between 2019 and 2020 during the pandemic among counties with the lowest COVID-19 incidence.
References
- 1.Hartnett K., Kite-Powell A., DeVies J. National Syndromic Surveillance Program Community of Practice: impact of the COVID-19 pandemic on emergency department visits—United States, January 1, 2019–May 30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(23):699–704. doi: 10.15585/mmwr.mm6923e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mehrotra A., Chernew M., Linetsky D., Hatch H., Cutler D., Schneider E.C. The Commonwealth Fund; New York, NY: 2020. The impact of the COVID-19 pandemic on outpatient care: visits return to prepandemic levels, but not for all providers and patients. [Google Scholar]
- 3.Izzetti R., Nisi M., Gabriele M., Graziani F. COVID-19 transmission in dental practice: brief review of preventive measures in Italy. J Dent Res. 2020;99(9):1030–1038. doi: 10.1177/0022034520920580. [DOI] [PubMed] [Google Scholar]
- 4.Meng L., Hua F., Bian Z. Coronavirus disease 2019 (COVID-19): emerging and future challenges for dental and oral medicine. J Dent Res. 2020;99(5):481–487. doi: 10.1177/0022034520914246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.American Dental Association. COVID-19 state mandates and recommendations. Accessed October 15, 2020. https://success.ada.org/en/practice-management/patients/covid-19-state-mandates-and-recommendations.
- 6.ADA Health Policy Institute. COVID-19: Economic impact on dental practices, week of June 1 results. Accessed July 10, 2020. https://surveys.ada.org/reports/RC/public/YWRhc3VydmV5cy01ZWQ2NjRiNzBhNzI3MTAwMGVkMDY2ZTQtVVJfNWlJWDFFU01IdmNDUlVO.
- 7.ADA Health Policy Institute. COVID-19: Economic impact on dental practices, week of September 7 results. Accessed October 21, 2020. https://iad1.qualtrics.com/reports/RC/public/YWRhc3VydmV5cy01ZjU3OWI5NzkzZDE2YTAwMTYzMjBmZWUtVVJfM3BaeGhzWm12TnNMdjB4
- 8.Kranz A.M., Gahlon G., Dick A.W., Stein B.D. Characteristics of US adults delaying dental care due to the COVID-19 pandemic. JDR Clin Trans Res. 2021;6(1):8–14. doi: 10.1177/2380084420962778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.SafeGraph . SafeGraph; San Francisco, CA: 2020. Determining point-of-interest visits from location data: a technical guide to visit attribution. [Google Scholar]
- 10.Andersen M., Bryan S., Slusky D. COVID-19 surgical abortion restriction did not reduce visits to abortion clinics. NBER Working Paper 2020;(28058) https://www.nber.org/papers/w28058 Accessed January 7, 2021.
- 11.Athey S, Blei D, Donnelly R, Ruiz F, Schmidt T. Estimating heterogeneous consumer preferences for restaurants and travel time using mobile location data. AEA Papers Proceed. 108:64-67.
- 12.Lasry A., Kidder D., Hast M., CDC Public Health Law Program, New York City Department of Health and Mental Hygiene, Louisiana Department of Health, Public Health–Seattle & King County, San Francisco COVID-19 Response Team, Alameda County Public Health Department, San Mateo County Health Department, Marin County Division of Public Health Timing of community mitigation and changes in reported COVID-19 and community mobility: four US metropolitan areas, February 26–April 1, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(15) doi: 10.15585/mmwr.mm6915e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Narayanan R.P., Nordlund J., Pace R.K., Ratnadiwakara D. Demographic, jurisdictional, and spatial effects on social distancing in the United States during the COVID-19 pandemic. PLoS One. 2020;15(9) doi: 10.1371/journal.pone.0239572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Crane L.D., Decker R.A., Flaaen A., Hamins-Puertolas A., Kurz C. Board of Governors of the Federal Reserve System; 2020. Business exit during the COVID-19 pandemic: non-traditional measures in historical context. Finance and Economics Discussion Series 2020-089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.COVID-19 data repository by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University. Johns Hopkins University; 2020. [Google Scholar]
- 16.U.S. Census Bureau. American Community Survey 2014-2018 5-year estimates now available. Accessed October 6, 2020. https://www.census.gov/newsroom/press-releases/2019/acs-5-year.html.
- 17.White House. Message to the Congress on declaring a national emergency concerning the novel coronavirus disease (COVID-19) outbreak. Accessed October 23, 2020. https://www.whitehouse.gov/briefings-statements/message-congress-declaring-national-emergency-concerning-novel-coronavirus-disease-covid-19-outbreak/
- 18.Kritz F. The dentist will see you now. But should you go? Washington, DC: National Public Radio; 2020. https://www.npr.org/sections/health-shots/2020/07/06/886456835/the-dentist-will-see-you-now-but-should-you-go Accessed October 15, 2020.
- 19.Cramer M. Is it safe to go back to the dentist? New York Times. Accessed October 15, 2020. https://www.nytimes.com/2020/06/25/health/dentist-coronavirus-safe.html
- 20.Estrich C.G., Mikkelsen M., Morrissey R. Estimating COVID-19 prevalence and infection control practices among US dentists. JADA. 2020;151(11):815–824. doi: 10.1016/j.adaj.2020.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Vujicic M., Buchmueller T., Klein R. Dental care presents the highest level of financial barriers, compared to other types of health care services. Health Aff. 2016;35(12):2176–2182. doi: 10.1377/hlthaff.2016.0800. [DOI] [PubMed] [Google Scholar]
- 22.Burger D. ADA recommending dentists postpone elective procedures. https://www.ada.org/en/publications/ada-news/2020-archive/march/ada-recommending-dentists-postpone-elective-procedures Accessed October 20, 2020.
- 23.Moore J.T., Ricaldi J.N., Rose C.E., COVID-19 State, Tribal, Local, and Territorial Response Team Disparities in incidence of COVID-19 among underrepresented racial/ethnic groups in counties identified as hotspots during June 5–18, 2020: 22 states, February–June 2020. MMWR Morb Mortal Wkly Rep. 2020;69(33):1122–1126. doi: 10.15585/mmwr.mm6933e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lin M., Griffin S.O., Gooch B.F. Centers for Disease Control and Prevention; Atlanta, GA: 2019. Oral health surveillance report: trends in dental caries and sealants, tooth retention, and edentulism, United States: 1999–2004 to 2011–2016. [Google Scholar]
- 25.Zhang Y. Racial/ethnic disparity in utilization of general dental care services among US adults: Medical Expenditure Panel Survey; 2012. J Racial Ethn Health Disparities. 2016;3(4):565–572. doi: 10.1007/s40615-015-0175-y. [DOI] [PubMed] [Google Scholar]
- 26.Nasseh K., Vujicic M. American Dental Association; 2020. Modeling the impact of COVID-19 on US dental spending: June 2020 update. [Google Scholar]
- 27.ADA Health Policy Institute. How many dentists are in solo practice? Accessed October 15, 2020. https://www.ada.org/∼/media/ADA/Science%20and%20Research/HPI/Files/HPIgraphic_1018_1.pdf?la=en.
- 28.American Dental Association. Fact Sheet: Small Business Administration loans for dentists. Accessed October 16, 2020. https://www.ada.org/∼/media/CPS/Files/COVID/ADA_ADCPA_SBA_Loan.pdf.
- 29.HHS Assistant Secretary for Public Affairs. CARES Act Provider Relief Fund: general information. Accessed October 16, 2020. https://www.hhs.gov/coronavirus/cares-act-provider-relief-fund/general-information/index.html.
- 30.Squire R.F. SafeGraph; 2019. What about bias in the SafeGraph dataset? [Google Scholar]
- 31.Goldfarb A., Tucker C. Shifts in privacy concerns. Am Econ Rev. 2012;102(3):349–353. [Google Scholar]