Abstract
Objective
The COVID-19 epidemic has spread worldwide since December 2019. To contain it, preventive measures including social distancing, economic shutdown, and school closures were introduced, carrying the risk of mental health burden in adults and children. Although the knowledge base regarding children's response to trauma and adverse events in general has broadened, descriptions of their mental health during epidemics remain scarce. In particular, the role of family socioeconomic characteristics and parental mental health are poorly understood.
Methods
We assessed the correlates of children’s emotional difficulties and symptoms of hyperactivity/inattention during the COVID-19 lockdown in a French community-based sample. Data came from 432 community-based parents (27–46 years, TEMPO cohort) and their children (mean age 6.8 ± 4.1) interviewed online. Children’s symptoms of emotional difficulties and hyperactivity/inattention were assessed using the parent-reported Strengths and Difficulties Questionnaire during the 5th week of home confinement. Family socioeconomic characteristics and parental mental health and substance use were assessed weekly during the first 5 weeks of home confinement. Data were analyzed using logistic regression models.
Results
7.1% of children presented symptoms of emotional difficulties and 24.7% symptoms of hyperactivity/inattention. Family financial difficulties and parental symptoms of anxiety and depression, as well as children’s sleeping difficulties and screen time, were associated with the presence of psychological difficulties.
Conclusion
Children's emotional and behavioural difficulties are associated with parental mental health and socioeconomic difficulties. In the unprecedented situation of the COVID-19 epidemic, parents and professionals involved in caring for children should pay special attention to their mental health needs.
Keywords: Children’s mental health, Self-report, Epidemiology, Community survey: COVID-19
Introduction
As the coronavirus (COVID-19) epidemic progresses worldwide, on March 17, 2020, the French Government ordered a nationwide lockdown, with strict social restrictions and limitations of individuals’ movements. Families were confined to their homes, with the risk of job loss, salary reduction or closure of regular activities such as schools. According to UNESCO, as of April 1st 2020, the infection has caused 194 countrywide closures around the world, thus affecting 1,598,099,000 students, knowing that school closures have been shown to have an impact on children psychological difficulties [1–3], school closure may also cause disruptions in physical activity, social interactions, and mental health of children and adolescents.
Prior studies on the health impact of a quarantine [1, 4, 5] have shown that when children are out of school, they are physically less active, have longer screen time and irregular sleep patterns, resulting in weight gain and loss of cardiorespiratory fitness, which can all subsequently impact their psychological well-being.
There is evidence that in some special populations, such as children of health workers [6], children with a chronic disease [7] as well as those suffering from ADHD before the epidemic [8, 9], the COVID-19 outbreak and the accompanying disease containment measures introduced had an impact on psychological well-being. However, though research highlights children’s mental health risks associated with anxiety, lack of peer contacts, reduced opportunities for stress regulation or parental mental illness [10–12], and several reports [1, 13, 14] call for further research, to date there is little epidemiological data on the mental health of children drawn from the community in face of the COVID-19 epidemic.
Given the well-known associations between family characteristics such as parental mental health [15–17], low socioeconomic position [17],18] and offspring high risk of poor mental health [15, 16], we chose to specifically examine the role of these factors.
The current study
The aim of our study was to assess family and individual correlates of children’s symptoms of emotional difficulties and hyperactivity/inattention in a community-based sample in France.
We assumed that children's characteristics such as sleeping difficulties, elevated screen time use, as well as the family’s circumstances including parents’ marital situation (single vs living together), financial difficulties, low income and unstable work situation during lockdown, parents' symptoms of anxiety and depression or substance use, and parents’ experience of COVID-19 symptoms were correlated to children's psychological difficulties and studied these characteristics.
Methods
Setting and study design
Data for this study come from a longitudinal survey of a cohort of parents who took part in the 2020 online assessment of the TEMPO (Trajectoires EpidéMiologiques en Population) COVID-19 study (www.tempo.inserm.fr).
Sample characteristics
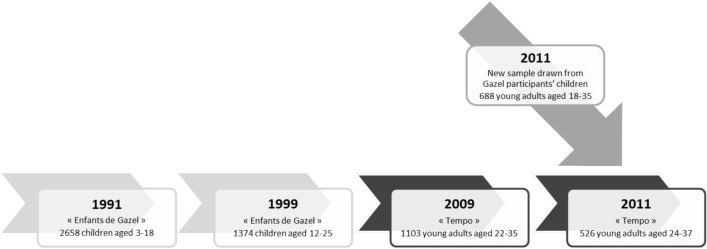
The TEMPO study was set up in 2009 to examine associations between life circumstances and substance use and mental health in young adults. All TEMPO participants have a parent who took part in the GAZEL cohort study [19, 20]. TEMPO study participants were recruited in 1991 when 2585 children aged 4–16 were selected to take part in a survey of their mental health. In 2009, all 1991 study participants (aged 22–35 at the time) were invited to participate again: 1103 agreed, of whom 752 agreed to a longitudinal follow-up [21]. In 2011, we conducted a new wave of data collection and the study sample was expanded to all GAZEL participants’ offspring aged 18–37 years [22] (Fig. 1). The TEMPO study received approval from France’s national committees for data protection (CCTIRS: Comité Consultatif sur le Traitement des Informations pour la Recherche en Santé: CNIL: Commission Nationale Informatique et Liberté).
Fig. 1.
Design of the cohort study using both TEMPO participants' and GAZEL participants'
Sample
On March 17, 2020, 7730 cases of COVID-19 were reported by France’s public health authorities, among them 2759 were hospitalized and 700 were in intensive care [23], pushing the French government to order a nationwide lockdown. From March 24th to April 28th 2020, TEMPO participants were invited by email to complete a weekly online questionnaire. The four initial questionnaires focused on sociodemographics, work characteristics, COVID-19 infection, general and mental health, as well as substance use. During the 5th week of lockdown, the questionnaire assessed participants’ children’s mental health and was completed by 432 participants. Participants who had more than one child were asked to complete the questionnaire in reference to their youngest child. Sample characteristics are described in Table 1. In total, 432 participants, including 276 women (65%) and 148 men (34.9%), completed the study questionnaire about their children: 31 (7.2%) children had signs of emotional difficulties and 107 (24.8%) of symptoms of hyperactivity/inattention.
Table 1.
Descriptive characteristics of children of TEMPO 2020 study participants during the COVID-19 lockdown in France (n = 432)
| Variable | Frequency (%) |
|---|---|
| SDQ scores in the children | |
| High emotional difficulties | |
| Yes | 31 (7.2) |
| No | 401 (92.8) |
| High hyperactivity/inattention | |
| Yes | 107 (24.8) |
| No | 325 (75.2) |
| Children’s characteristics | |
| Age | |
| ≤ 6 years | 172 (51.5) |
| >6 years | 162 (48.5) |
| Sex | |
| Female | 164 (48.9) |
| Male | 171 (51.0) |
| Sleeping difficulties | |
| Yes | 69 (21.2) |
| No | 256 (78.8) |
| Screen time (per day) | |
| < 1 h | 88 (26.8) |
| > 1 h | 240 (73.1) |
| Family sociodemographic characteristics | |
| Parental situation during COVID-19 lockdown | |
| Single/biological parents not living together | 152 (40.2) |
| Parental couple living together | 226 (59.8) |
| Sex of the responding participant | |
| Female (Yes) | 276 (65.0) |
| Male | 148 (34.9) |
| Number of children in the family | |
| ≤2 | 185 (80.8) |
| >2 | 44 (19.2) |
| Financial difficulties | |
| No | 382 (89.9) |
| Yes | 43 (10.1) |
| Average Family Income (/month) | |
| ≤2500 euros (Ref) | 148 (34.3) |
| >2500 euros | 284 (65.7) |
| Job situation | |
| Normal/distance working | 289 (76.0) |
| Unemployment/job loss during confinement/sick leave | 119 (29.1) |
| Parental characteristics | |
| COVID-19 symptoms | |
| Yes | 28 (6.5) |
| No | 404 (93.5) |
| Parental mental health difficulties during lockdown | |
| Symptoms of anxiety-depression | |
| Yes | 118 (27.3) |
| No | 314 (72.7) |
| Substance use | |
| Tobacco smoker | |
| Yes | 49 (16.8) |
| No | 243 (83.2) |
| Problematic alcohol use | |
| Yes | 31 (10.9) |
| No | 254 (89.1) |
SDQ strength and difficulties questionnaire. Note 1: Frequency and percentages for categorical variables. Note 2: Owing to missing values, the frequencies of some categorical variables do not add up to 432
Ethical section
The TEMPO study received approval from France’s national committees for data protection (CCTIRS: Comité Consultatif sur le Traitement des Informations pour la Recherche en Santé: CNIL: Commission Nationale Informatique et Liberté).
Measures
Children
We used the SDQ to ascertain symptoms of emotional difficulties and hyperactivity/inattention.
Emotional and hyperactivity/inattention symptoms
Children’s symptoms of emotional difficulties as well as hyperactivity/inattention were reported by parents using the Strengths and Difficulties Questionnaire (SDQ) during the 5th week (from 20 to 26th of April 2020) of home confinement. The SDQ is a brief, 25-item, measure of behavioral and emotional difficulties that can be used in children and young people aged 4–17 years [24–26]. In this study, we used two subscales: “emotional difficulties” and symptoms of “hyperactivity/inattention”, with five items each. Each item was scored on a 3 points ordinal Likert scale (0 “not true”; 1 "somewhat true"; 2 "certainly true"). A cut-off of >3 out of 10 was used to detect high symptom levels on emotional difficulties scale and of >5 out of 10 to detect high symptoms levels on hyperactivity/inattention scale. The internal consistency of the subscales was acceptable (Cronbach’s α of 0.62 for emotional difficulties and 0.74 for symptoms of hyperactivity/inattention).
Risk factors of children’s psychological difficulties
Risk factors studied in this investigation included children’s age, sleep and screen time use, family sociodemographic characteristics, parents’ mental health and substance use, and parents’ experience of COVID-19 symptoms.
Children’s characteristics (sociodemographics, sleeping difficulties, screen time)
The child’s sociodemographic characteristics included sex (female vs. male), age (> or ≤6 years old).
Sleeping difficulties were assessed by the following questions: "During the preceding 7 days, did your child have difficulties sleeping that: appeared or increased or decreased or disappeared or stayed stable or no difficulties." We created the following categories "Sleeping difficulties (including "sleeping difficulties that "appeared" or "increased” or “stayed stable") vs. "No sleeping difficulties” (including "no difficulties”, or “difficulties disappeared" or "difficulties decreased").
Screen time was assessed by the following questions: "During the preceding 7 days, how much time has your child spent in front of a screen (TV, tablet, computer, smartphone..) per day. We created the two following categories: "Less than 1 h", vs. "More than 1 h", based on the American Academy of Pediatrics new Recommendations for Children's Media Use [27].
Parents
Family sociodemographic characteristics
Sociodemographic characteristics studied include: family situation (single vs couple), financial difficulties in the preceding 5 weeks (yes vs no), household monthly income (2500 euro or less vs >2500 euro) (in reference to the average income in France) [28] and work situation during lockdown (normal /distance working vs job loss/unemployment vs sick leave).
Parents’ mental health
To assess parents’ symptoms of anxiety and depression during the first 5 weeks of lockdown, we used weekly repeated measures of the subscale assessing anxious-depressed symptoms in the Adult Self Report Scale (ASR) [29], creating a dichotomized T-score with a cut-off based on +1 standard deviation from the mean. Additionally, using an assessment of ASR-based anxious-depressed symptoms obtained in the TEMPO study in 2018, we also identified parents’ symptoms of anxiety and depression before lockdown, which were studied in additional analyses.
Parents’ substance use
Participants reported levels of substance use and abuse during the first 5 weeks of lockdown in weekly questionnaires.
Tobacco smoking status was assessed using the following question in week 1: “Are you a regular or occasional smoker?” coded yes vs. no.
Alcohol use was assessed using the French version of the Alcohol Use Disorders Identification Test (AUDIT-C) [30, 31]. This brief three-item alcohol screening tool developed by the WHO focuses on the frequency and quantity of alcohol consumption [32], matches DSM IV criteria for alcohol abuse and dependence and is validated against clinical diagnosis. Audit-C test scores of 3 or more for women and 4 or more for men were considered to indicate a heightened risk for hazardous drinking/alcohol use disorder [32, 33].
COVID-19 symptoms of the parents
Parents’ COVID-19 symptoms during the first 5 weeks were ascertained weekly by the following question: "Did you present symptoms of COVID-19 infection (fever, cough, loss of taste or smell)”? Based on participants’ weekly repeated responses (“yes” vs “no"), we created a variable indicating the presence of symptoms prior to the measure of children’s psychological difficulties.
Statistical analyses
First, descriptive statistics including frequencies and percentages were used to characterize the study population (Table 1). We tested bivariate associations between potential individuals and family risk factors, and children’s symptoms of emotional difficulties or hyperactivity/inattention using the Chi-square test (Tables 2 and 3).
Table 2.
Parental characteristics and children’s psychological emotional difficulties during COVID-19 lockdown in France (TEMPO COVID-19 Questionnaire 2020, age- and sex-adjusted odds ratios, multivariate model, Chi Square tests)
| Emotional symptoms | |||||||
|---|---|---|---|---|---|---|---|
| Characteristicsa | Yes | No | Chi2 test | Age- and sex-adjusted OR | 95% Wald CI | Multivariate model ORc | 95% Wald CI |
| Children’s characteristics | |||||||
| Age | 0.3 | 1.5 | 0.7–3.2 | 1.1 | 0.4–2.6 | ||
| ≤ 6 years old | 13 (41.9) | 159 (52.4) | |||||
| >6 years old | 18 (58.0) | 144 (47.5) | |||||
| Sex | 0.2 | 1.0 | 0.9–1.1 | 1.8 | 0.7–4.1 | ||
| Female | 18 (58.0) | 146 (48.0) | |||||
| Male (Ref) | 13 (41.9) | 158 (51.9) | |||||
| Sleeping difficulties | < 0.05 | 2.6b | 1.2–5.7 | 2.0 | 0.8–4.8 | ||
| No (Ref) | 19 (61.3) | 237 (80.6) | |||||
| Yes | 12 (38.7) | 57 (19.3) | |||||
| Screen time per day | < 0.05 | 6.8b | 1.5–30.9 | 6.2b | 1.4-28.0 | ||
| < 1 h (Ref) | 2 (6.4) | 86 (28.9) | |||||
| >1 h | 29 (93.5) | 211 (71.0) | |||||
| Family sociodemographic characteristics during lockdown | |||||||
| Family situation | 0.8 | 1.2 | 0.6–2.7 | 0.7 | 0.3–1.9 | ||
| Single/biological parents not living together | 12 (41.4) | 140 (40.1) | |||||
| Couple | 17 (58.6) | 209 (59.9) | |||||
| Sex of the responding parent during the 5 week | < 0.05 | 2.5 | 0.9–6.8 | 1.7 | 0.6–6.1 | ||
| Female | 26 (83.9) | 250 (63.6) | |||||
| Male (Ref) | 5 (16.1) | 140 (36.4) | |||||
| Number of children in the family | 0.8 | 1.0 | 0.3–3.2 | 0.9 | 0.3–3.1 | ||
| ≤ 2 | 18 (81.8) | 167 (80.7) | |||||
| > 2 | 4 (18.1) | 40 (19.3) | |||||
| Financial difficulties | < 0.05 | 4.2b | 1.6–11.0 | 2.3 | 0.8–6.2 | ||
| No (Ref) | 22 (73.3) | 360 (91.4) | |||||
| Yes | 8 (26.7) | 355 (8.9) | |||||
| Income | 0.8 | 1.1 | 0.5–2.4 | 0.9 | 0.4–2.1 | ||
| 2500 euros or less (Ref) | 30 (28.0) | 118 (36.3) | |||||
| > 2500 euros | 77 (71.9) | 207 (63.7) | |||||
| Job situation | 0.2 | 1.6 | 0.7–3.5 | 1.3 | 0.5–3.2 | ||
| Normal activity/teleworking | 17 (68) | 272 (76.6) | |||||
| Unemployment/job loss during confinement/Sick leave | 11 (39.2) | 108 (28.4) | |||||
| Parental characteristics during lockdown | |||||||
| COVID-19 symptoms (during lockdown) | 0.3 | 1.7 | 0.5–5.3 | 2.2 | 0.6–10.0 | ||
| Yes | 4 (11.4) | 27 (6.9) | |||||
| No | 31 (88.6) | 369 (93.1) | |||||
| Parental mental health | |||||||
| Symptoms of anxiety-depression during lockdown | < 0.05 | 8.1b | 2.4–26.8 | 5.7b | 2.4–5.1 | ||
| No (Ref) | 8 (50) | 133 (84.1) | |||||
| Yes | 8 (50) | 25 (15.8) | |||||
| Parents’ substance use | |||||||
| Tobacco (regular smoker > 10/day) | 0.06 | 2.3 | 0.8–6.6 | 1.4 | 0.4–5.4 | ||
| Yes | 10 (58.8) | 73 (36.3) | |||||
| No | 7 (41.2) | 128 (63.7) | |||||
| Problematic consumption of alcohol | 0.8 | 0.7 | 0.1–3.8 | 0.4 | 0.07–2.8 | ||
| Yes | 2 (9.5) | 29 (11) | |||||
| No | 19 (90.5) | 235 (89.0) | |||||
Note. TEMPO Trajectoires Epidémiologiques en Population; CI confidence interval; OR odds ratio
aOwing to missing values, the frequencies of some categorical variables do not add up to 432
bStatistically significant (P < 0.05)
cMultivariate model: age- and sex-adjusted analysis, additionally adjusted on all variables that were significant in bivariate analysis (P < 0.05): sleeping difficulties, screen time, sex of the responding parent, financial difficulties, symptoms of anxiety-depression during lockdown
Table 3.
Parental characteristics and children’s symptoms of hyperactivity/inattention during the COVID-19 lockdown in France (TEMPO Covi19 Questionnaire 202O, age- and sex-adjusted odds ratios, multivariate model, Chi Square tests)
| Hyperactivity/inattention symptoms | |||||||
|---|---|---|---|---|---|---|---|
| Characteristicsa | Yes | No | Chi2 test P-value | Age and sex-adjusted OR | 95% Wald CI | Multivariate model ORc | 95% Wald CI |
| Children characteristics | |||||||
| Age | 0.4 | 0.9 | 0.9–1.0 | 1.1 | 0.6–1.9 | ||
| ≤6 years old (Ref) | 51 (48.1) | 121 (53.1) | |||||
| > 6 years old | 55 (51.9) | 107 (46.9) | |||||
| Sex | 0.7 | 0.4–1.1 | 0.7 | 0.4–1.1 | |||
| Female | 46 (42.9) | 118 (51.7) | 0.7 | ||||
| Male (Ref) | 61 (57.1) | 110 (48.2) | |||||
| Sleeping difficulties | < 0.05 | 2.0b | 1.1–3.3 | 1.7 | 0.9–3.0 | ||
| No (Ref) | 75 (70.7) | 181 (82.6) | |||||
| Yes | 31 (29.2) | 38 (17.3) | |||||
| Screen time per day | 0.07 | 1.3 | 0.9–1.9 | 1.5 | 0.8–2.8 | ||
| <1 h (Ref) | 22 (20.5) | 66 (29.8) | |||||
| >1 h | 85 (79.4) | 155 (70.1) | |||||
| Family sociodemographic characteristics during lockdown | |||||||
| Family situation | 0.6 | 1.4 | 0.9–2.3 | 1.3 | 0.7–2.1 | ||
| Single/biological parents not living together | 42 (42.4) | 110 (39.4) | |||||
| Couple (Ref) | 57 (57.6) | 169 (60.6) | |||||
| Sex of the responding parent | 0.8 | 0.7 | 0.4–1.2 | 0.6 | 0.3–0.9 | ||
| Female (Ref) | 68 (64.1) | 208 (65.4) | |||||
| Male | 38 (35.8) | 110 (34.6) | |||||
| Number of children in the family | 0.3 | 0.6 | 0.3–1.5 | 0.6 | 0.2–1.4 | ||
| ≤2 | 57 (85.0) | 128 (79.0) | |||||
| > 2 | 10 (14.9) | 34 (20.9) | |||||
| Financial difficulties | < 0.05 | 2.3b | 1.1–4.6 | 4.3b | 1.1–17.9 | ||
| No (Ref) | 86 (81.9) | 296 (92.5) | |||||
| Yes | 19 (18.1) | 24 (7.5) | |||||
| Income | 0.1 | 1.0 | 0.6–1.7 | 1.0 | 0.6–1.8 | ||
| 2500 euros or less (Ref) | 30 (28.0) | 118 (36.3) | |||||
| >2500 euros | 77 (71.9) | 207 (63.7) | |||||
| Job situation | 0.1 | 1.8b | 1.1–3.3 | 1.7 | 1.0–2.9 | ||
| Normal activity/teleworking | 67 (64.4) | 222 (73.0) | |||||
| Unemployment/job loss during confinement/sick leave | 37 (35.6) | 82 (26.9) | |||||
| Parental characteristics during lockdown | |||||||
| COVID symptoms for parents | 0.8 | 0.9 | 0.4–2.1 | 0.9 | 0.3–2.4 | ||
| Yes | 9 (8.5) | 26 (8.0) | |||||
| No | 97 (91.5) | 299 (92.0) | |||||
| Parental mental health | |||||||
| Anxious-depressive symptoms during the first 5 weeks of lockdown | 0.1 | 2.6b | 1.0–7.1 | 2.5b | 1.4–4.2 | ||
| No (Ref) | 35 (74.5) | 106 (83.5) | |||||
| Yes | 12 (25.5) | 21 (16.5) | |||||
| Drugs consumption for the parents | |||||||
| Tobacco (regular smoker > 10 /day) | 0.9 | 0.8 | 0.4–1.6 | 1.6 | 0.6–3.6 | ||
| Yes | 19 (38) | 64 (38.1) | |||||
| No (Ref) | 31 (62) | 104 (61.9) | |||||
| Problematic consumption of alcohol since beginning of home confinement | 0.06 | 1.2 | 0.7–1.9 | 0.8 | 0.3–2.1 | ||
| Yes | 21 (23.3) | 50 (18.2) | |||||
| No (Ref) | 69 (76.7) | 224 (81.7) | |||||
Note. TEMPO Trajectoires Epidémiologiques en Population; CI confidence interval; OR odds ratio
aOwing to missing values, the frequencies of some categorical variables do not add up to 432
bStatistically significant (P < 0.05)
cMultivariate model: age- and sex-adjusted analysis, additionally adjusted on all variables that were significant in bivariate analysis (P < 0.05): sleeping difficulties, financial difficulties, job situation, symptoms of anxiety-depression during lockdown
Second, to identify factors associated with children’s emotional difficulties and symptoms of hyperactivity/inattention, we used logistic regression with the alpha value set at P < 0.05. We built one model, adjusting for the child’s age and sex, and an additional multivariate model adjusting for all variables that were significantly associated with the study outcomes in bivariate analyses.
Additional analyses
We tested for statistical interactions between children’s age and sex on one hand and parents’ mental health and financial difficulties on the other. None of these statistical interactions were statistically significant.
All statistical analyses were conducted using STATA 16.1 (StataCorp, College Station, Texas, USA).
Results
Sample characteristics (Table 1)
Sample characteristics are described in Table 1. In total, 432 participants, including 276 women (65%) and 148 men (34.9%), completed the study questionnaire about their children: 31 (7.2%) children had signs of emotional difficulties and 107 (24.8%) of symptoms of hyperactivity/inattention.
Tables 2 and 3 show factors associated with children’s emotional difficulties and symptoms of hyperactivity/inattention.
Risk factors of children’s emotional difficulties and symptoms of hyperactivity/inattention (Tables 2, 3)
Emotional symptoms
Age- and sex-adjusted logistic regression analyses (Table 2) showed that the odds of children’s high levels of emotional difficulties were elevated among those who had sleeping difficulties (OR 2.6, 95% CI 1.2–5.7), whose screen time was more than 1 h per day (OR 6.8, 95% CI 1.5–30.9), whose parents had symptoms of anxiety-depression during lockdown (OR 8.1, 95% CI 2.4–26.8), or who had financial difficulties (OR 4.2, 95% CI 1.6–11.0).
Family situation (OR 1.2, 95% 0.6–2.7), the number of children in the family (OR 1.0, 95% 0.3–3.2), income (OR 1.1, 95% 0.5–2.4), job situation (OR 1.6, 95% 0.7–3.5), COVID-19 symptoms (OR 1.7, 95% 0.5–5.3), and parents' substance use, such as tobacco consumption (OR 2.3, 95% 0.8–6.6) and problematic alcohol consumption (OR 0.7, 95% 0.1–3.8) were not associated with children's high levels of emotional difficulties.
These associations did not change in a multivariate regression models, except for sleep difficulties and financial difficulties, which were no longer associated with children’s emotional symptoms.
Symptoms of hyperactivity/inattention
Age- and sex-adjusted logistic regression analyses (Table 3) showed that the odds of children’s symptoms of hyperactivity/inattention were elevated among children who had sleeping difficulties (OR 2.0, 95% CI 1.1–3.3), had parents with symptoms of anxiety or depression (OR 2.6, 95% CI 1.1–1.2), financial difficulties (OR 2.3, 95% CI 1.1–4.6), or who were unemployed (OR 1.8, 95% CI 1.1–3.3).
The child’s screen time (OR 1.3, 95% CI 0.9–1.9), the responding parent’s sex (OR 0.7, 95% CI 0.4–1.2), the family situation (OR 1.4, 95% CI 0.9–2.3), the number of children in the family (OR 0.6, 95% CI 0.3–1.5), parents’ substance use such as tobacco consumption (OR 0.8, 95% 0.4–1.6) and problematic alcohol consumption (OR 1.2, 95% 0.7–1.9), COVID symptoms (OR 0.9, 95% CI 0.4–2.1), or income (OR 1.0, 95% CI 0.6–1.7) were not associated with children's elevated levels of symptoms of hyperactivity/inattention.
These associations did not change in a multivariate regression model, except for sleeping difficulties and parental work situation, which were no longer associated with children’s symptoms of hyperactivity/inattention.
Discussion
Main findings
Ours is one of the first studies to explore children’s psychological symptoms and their correlates during the COVID-19 epidemic and associated lockdown. Overall, when adjusting on age and sex, children’s emotional difficulties and symptoms of hyperactivity/inattention were significantly associated with their sleeping difficulties and screen time exposure, their parents’ symptoms of anxiety or depression and financial difficulties. Parental employment situation was associated with children’s symptoms of hyperactivity/inattention only, in an age- and sex-adjusted model. Overall, children’s symptoms of frequent psychological difficulties are associated with known risk factors of youth mental health problems. Children of parents who have psychological difficulties or who experience socioeconomic difficulties should benefit from special attention from primary and mental health practitioners.
Interpretation of study findings
We discuss our findings on the role of parents’ mental health and socioeconomic characteristics on the one side, and children’s sleep disorders and screen time use on the other side.
Parents’ characteristics
In accordance with previous research [34–36], parents’ symptoms of anxiety or depression during lockdown, as well as parents’ pre-existing mental health difficulties, were associated with a higher level of children’s emotional difficulties and symptoms of hyperactivity/inattention.
In a stressful period such as the COVID-19 epidemic and resulting disruptions of daily life, parents are the best resource for children to seek help from. Good parenting skills are hence crucial when children are confined at home [1]. In general, children with a mentally ill parent more frequently experience negative emotions, including anger, fear, and sadness. They also show higher levels of disturbed attachment and difficulties in emotional regulation [37]. Consequently, they are at elevated risk of internalizing problems, such as depression and anxiety [15, 16].
Concerning children's symptoms of hyperactivity/inattention, the study of Zhang [9] showed that they were related to parent's mood during the COVID-19 outbreak in China. Additionally, parents of children with ADHD experience high levels of daily child-rearing stressors [38, 39], therefore, this association may also be bidirectional. The special combination of school closures and children staying at home might bring elevated difficulties and stress for both children and their parents. Our results have significant clinical implications concerning the importance of assessing parents' negative mood when evaluating children’s well-being. During periods of lockdown, when assessing a child, mental health practitioners should pay further attention to the mental health status of the parents, especially looking for depression or anxiety symptoms.
Similarly, independently of home confinement, previous research has reported that children of parents with substance use disorders, [40–42], have an elevated likelihood of additional mental disorders. However, we found no relationship between parental consumption of tobacco or alcohol and offspring psychological difficulties. This may reflect low rates of tobacco and alcohol use among TEMPO cohort participants [43].
In our study, having a parent who presented with symptoms of COVID-19 was not associated with a higher score of emotional difficulties or hyperactivity/inattention. In a recent Chinese study [34], having relatives or acquaintances infected with COVID-19 was an independent risk factor of anxiety among college students, probably due to the high contagiousness of the illness [44]. It is important to note that parental COVID-19 symptoms were self-reported since biological testing was hardly available during the lockdown. It may also be that individuals who were too ill were not able to respond to TEMPO study questionnaires.
Parental financial difficulties and work situation were associated with children’s emotional difficulties and symptoms of hyperactivity/inattention. Stability of family income has been found to be significantly associated with youth anxiety during the COVID 19 crisis, due to links with psychological and economic pressure [34, 45].
Our findings indicate an increased risk of psychological difficulties in children whose family had psychological or financial difficulties during lockdown. This result is consistent with previous studies, which demonstrated that parents with financial difficulties are at higher risk of mental health difficulties such as anxiety. Economic decline [46] is associated with increased mental health problems for youths that may be affected by its consequences on adult unemployment and mental health, such as depression [14, 47].
Children’s characteristics
Children’s elevated levels of emotional difficulties and symptoms of hyperactivity/inattention were associated with sleeping difficulties. Because both were measured simultaneously, it is possible that these relationships are bidirectional. Children who are anxious or experience symptoms of depression frequently have sleeping problems, which sometimes appear as a key symptom of distress [18, 48]. Symptoms of hyperactivity and inattention are core symptoms of ADHD. Similarly, ADHD may disrupt sleep by increasing the probability of bedtime struggles or resistance, limit-setting sleep problems, inadequate sleep hygiene, and insufficient sleep disorder or poor sleep quality. In turn, sleep problems may result in ADHD-like day-time behaviors [49].
In the specific context of COVID-19, Zhang et al. [9] showed that children who have ADHD and experience low overall mood are most likely to see their symptoms of ADHD, including sleep patterns, worsen. Another study [13] found that poor sleep, including nightmares, is among the most frequently reported children’s conditions during the COVID-19 outbreak.
In our study, children with emotional difficulties or symptoms of hyperactivity/inattention spent more time in front of a screen during the COVID-19 outbreak than children without such symptoms, which is line with previous studies showing that increased screen time may exacerbate risk for depression, anxiety, suicide, and inattention among children and adolescents [50]. Excessive screen time may also be associated with health risks including poor sleep and sedentarity, which further exacerbate risk of children’s psychological difficulties [51, 52]. It is, however, important to note that our study being cross-sectional, screen use may also be a consequence of children’s psychological difficulties, both potentially reinforcing one another. Kiraly et al. [53] made some practical guidance to prevent children’s problematic Internet use and emphasize that monitoring and regulating screen time is crucial and can be implemented by involving young people in rule-making [54].
Paradoxically, during the COVID-19 pandemic, many mental health educational resources and support services were offered via online platforms, which required screen use. Obviously, screen time may become over-present during periods of school closure [51], and existing guidelines need to be adequately updated to remain relevant. A recent literature review emphasized that not all screen time is equal—e.g. doing online lessons for school is different from social media use, which is different from video games [55].
Strengths and limitations
Our study’s main strengths are that it was conducted in the community and started prior to the COVID-19 epidemic, making it possible to control for pre-existing risk factors. However, it also has some limitations that need to be highlighted. First, all measures were based on self-reports, including the children’s SDQ scores, which could have been influenced by parental emotional state [56]. Still, parental evaluations are appropriate given the young mean age of surveyed children (i.e. 6 years). Importantly, the performance and validity of the parent-reported SDQ in French [26] suggests that it is a good approximation of a psychiatric interview, in studies of population representative samples [57–59]. Second, we did not assess children’s emotional difficulties and hyperactivity/inattention before the COVID-19 epidemic, so we have no information concerning pre-existing vulnerabilities. Children who experienced psychological difficulties prior to the pandemic or had pre-existing mental health problems are at high risk of having symptoms of anxiety [60]. Third, though some variables were assessed longitudinally on a weekly basis during lockdown, the causal relationship between children’s and parents’ characteristics and children’s emotional difficulties or symptoms of hyperactivity/inattention cannot be confirmed as children’s symptoms were assessed only once. A recent study [61] outlined the need for longitudinal mental health research with children during and after lockdown. Fourth, the relatively small sample of the study limited the statistical power of some analyses. This suggests that a larger sample may show evidence of other risk factors of children’s psychological difficulties. Fifth, participants were more likely to live with a partner, have higher education and hold a managerial position than middle-aged adults of the same age in France. Reassuringly, we observed a similar rate of lifetime unemployment compared to the general population [17, 62]. Overall, associations between parental mental health and socioeconomic characteristics, as well as children’s sleep and screen use, may actually be stronger than we report. Sixth, children’s age range was limited, as the study did not include many very young or adolescent children. However, a focus on pre-teenagers made it possible for us to study a coherent demographic group. Seventh, our measure of children’s emotional and behavioural difficulties was dichotomized, which may have limited the statistical power of our analyses, however, we used a validated cut-off, and were thus able to identify children with potentially clinically relevant psychological difficulties.
Implications
The aim of our study was to assess family and individual risk factors of children’s symptoms of emotional difficulties and hyperactivity/inattention in a community-based sample in France.
While the COVID-19 pandemic is spreading all over the world, attention is mostly focused on adults, hiding the public mental health burden in children. Our results underline the necessity to consider long-term mental health effects on this worldwide situation on children, who account for 42% of the world's population [63].
Risk factors of children’s mental health difficulties identified in our study, which have previously been reported, may require special monitoring during the time of the pandemic. For instance, paying attention to sleep difficulties and nightmares, and suggesting sleep hygiene and relaxation methods, could be especially worthwhile during the epidemic [13]. Moreover, screen time guidelines need to updated, as many children and adolescents will not attend school.
Further longitudinal studies should be conducted to test prospective risk factors of children’s mental health difficulties. Indeed, even as restrictions are lifted and schools re-open, the psychological impact of the pandemic will last. Increased awareness of the risk factors of mental health difficulties in children in this unprecedented event is needed to prevent them in the short and long terms.
Acknowledgements
We thank TEMPO and GAZEL study participants who provided data for this project.
Funding
The TEMPO cohort received funding from the French National Research Agency (ANR) including the Flash COVID-19 funding scheme; the French Institute for Public Health Research-IReSP (TGIR Cohortes); the French Inter-departmental Mission for the Fight against Drugs and Drug Addiction (MILDeCA); the French Institute of Cancer (INCa); and the Pfizer Foundation.
Availability of data and materials
Upon request.
Code availability
STATA 16.1 (StataCorp, College Station, Texas, USA).
Declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethics approval
The TEMPO study received approval from France’s national committees for data protection (CCTIRS: Comité Consultatif sur le Traitement des Informations pour la Recherche en Santé: CNIL: Commission Nationale Informatique et Liberté).
Footnotes
Cédric Galéra and Maria Melchior co-last author contributed equally.
References
- 1.Wang G, Zhang Y, Zhao J, et al. Mitigate the effects of home confinement on children during the COVID-19 outbreak. Lancet. 2020;395:945–947. doi: 10.1016/S0140-6736(20)30547-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tang S, Xiang M, Cheung T, Xiang Y-T. Mental health and its correlates among children and adolescents during COVID-19 school closure: the importance of parent-child discussion. J Affect Disord. 2021;279:353–360. doi: 10.1016/j.jad.2020.10.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Viner RM, Russell SJ, Croker H, et al. School closure and management practices during coronavirus outbreaks including COVID-19: a rapid systematic review. Lancet Child Adolesc Health. 2020;4:397–404. doi: 10.1016/S2352-4642(20)30095-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Brazendale K, Beets MW, Weaver RG, et al. Understanding differences between summer vs school obesogenic behaviors of children: the structured days hypothesis. Int J Behav Nutr Phys Act. 2017;14:100. doi: 10.1186/s12966-017-0555-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mahajan C, Kapoor I, Prabhakar H. Psychological effects of corona virus disease (COVID 19) on children of health care workers. Anesth Analg. 2020 doi: 10.1213/ANE.0000000000005034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Brooks SK, Webster RK, Smith LE, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395:912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Martinelli M, Strisciuglio C, Fedele F, et al. Clinical and psychological issues in children with inflammatory bowel disease during COVID-19 pandemic. Inflamm Bowel Dis. 2020 doi: 10.1093/ibd/izaa136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bobo E, Lin L, Acquaviva E, et al. How do children and adolescents with attention deficit hyperactivity disorder (ADHD) experience lockdown during the COVID-19 outbreak? Encephale. 2020 doi: 10.1016/j.encep.2020.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhang J, Shuai L, Yu H, et al. Acute stress, behavioural symptoms and mood states among school-age children with attention-deficit/hyperactive disorder during the COVID-19 outbreak. Asian J Psychiatr. 2020;51:102077. doi: 10.1016/j.ajp.2020.102077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fegert JM, Vitiello B, Plener PL, Clemens V. Challenges and burden of the coronavirus 2019 (COVID-19) pandemic for child and adolescent mental health: a narrative review to highlight clinical and research needs in the acute phase and the long return to normality. Child Adolesc Psychiatry Ment Health. 2020;14:20. doi: 10.1186/s13034-020-00329-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Xie X, Xue Q, Zhou Y et al (2020) Mental health status among children in home confinement during the coronavirus disease 2019 outbreak in Hubei Province, China. JAMA Pediatr. 10.1001/jamapediatrics.2020.1619 [DOI] [PMC free article] [PubMed]
- 12.Liang L, Ren H, Cao R, et al. The effect of COVID-19 on youth mental health. Psychiatr Q. 2020;91:841–852. doi: 10.1007/s11126-020-09744-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jiao WY, Wang LN, Liu J, et al. Behavioral and emotional disorders in children during the COVID-19 epidemic. J Pediatr. 2020;221:264–266.e1. doi: 10.1016/j.jpeds.2020.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Golberstein E, Wen H, Miller BF. Coronavirus disease 2019 (COVID-19) and mental health for children and adolescents. JAMA Pediatr. 2020 doi: 10.1001/jamapediatrics.2020.1456. [DOI] [PubMed] [Google Scholar]
- 15.Merikangas KR, Dierker LC, Szatmari P. Psychopathology among offspring of parents with substance abuse and/or anxiety disorders: a high-risk study. J Child Psychol Psychiatry. 1998;39:711–720. [PubMed] [Google Scholar]
- 16.Weissman MM, Wickramaratne P, Gameroff MJ, et al. Offspring of depressed parents: 30 years later. Am J Psychiatry. 2016;173:1024–1032. doi: 10.1176/appi.ajp.2016.15101327. [DOI] [PubMed] [Google Scholar]
- 17.Melchior M, Chastang J-F, Walburg V, et al. Family income and youths' symptoms of depression and anxiety: a longitudinal study of the French GAZEL Youth cohort. Depress Anxiety. 2010;27:1095–1103. doi: 10.1002/da.20761. [DOI] [PubMed] [Google Scholar]
- 18.Yap MBH, Jorm AF. Parental factors associated with childhood anxiety, depression, and internalizing problems: a systematic review and meta-analysis. J Affect Disord. 2015;175:424–440. doi: 10.1016/j.jad.2015.01.050. [DOI] [PubMed] [Google Scholar]
- 19.Redonnet B, Chollet A, Fombonne E, et al. Tobacco, alcohol, cannabis and other illegal drug use among young adults: the socioeconomic context. Drug Alcohol Depend. 2012;121:231–239. doi: 10.1016/j.drugalcdep.2011.09.002. [DOI] [PubMed] [Google Scholar]
- 20.Lemogne C, Consoli SM, Geoffroy-Perez B, et al. Personality and the risk of cancer: a 16-year follow-up study of the GAZEL cohort. Psychosom Med. 2013;75:262–271. doi: 10.1097/PSY.0b013e31828b5366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fombonne E, Vermeersch S (1997) Les enfants de la cohorte GAZEL: I-Prévalence des contacts avec le système médico-éducatif pour des motifs psychologiques, et facteurs associés. Revue d'épidémiologie et de santé [PubMed]
- 22.Melchior M, Chollet A, Elidemir G, et al. Unemployment and substance use in young adults: does educational attainment modify the association? Eur Addict Res. 2015;21:115–123. doi: 10.1159/000365887. [DOI] [PubMed] [Google Scholar]
- 23.Agence nationale de santé publique". www.santepubliquefrance.fr
- 24.Goodman R. Psychometric properties of the strengths and difficulties questionnaire. J Am Acad Child Adolesc Psychiatry. 2001;40:1337–1345. doi: 10.1097/00004583-200111000-00015. [DOI] [PubMed] [Google Scholar]
- 25.Goodman A, Goodman R. Strengths and difficulties questionnaire as a dimensional measure of child mental health. J Am Acad Child Adolesc Psychiatry. 2009;48:400–403. doi: 10.1097/CHI.0b013e3181985068. [DOI] [PubMed] [Google Scholar]
- 26.Shojaei T, Wazana A, Pitrou I, Kovess V. The strengths and difficulties questionnaire: validation study in French school-aged children and cross-cultural comparisons. Soc Psychiatry Psychiatr Epidemiol. 2009;44:740–747. doi: 10.1007/s00127-008-0489-8. [DOI] [PubMed] [Google Scholar]
- 27.American Academy of Pediatrics Announces New Recommendations for Children's Media Use. APA.org
- 28.INSEE: Revenu disponible par ménage (moyenne et médiane). http://www.insee.fr/fr/themes/tableauasp?reg_id=0&ref_id=NATSOS04202
- 29.Kessler RC, Adler L, Ames M, et al. The World Health Organization adult ADHD self-report scale (ASRS): a short screening scale for use in the general population. Psychol Med. 2005;35:245–256. doi: 10.1017/S0033291704002892. [DOI] [PubMed] [Google Scholar]
- 30.Reinert DF, Allen JP. The Alcohol Use Disorders Identification Test (AUDIT): A review of recent research. Alcoholism: Clinical and Experimental Research. 2002;26:272–279. doi: 10.1111/j.1530-0277.2002.tb02534.x. [DOI] [PubMed] [Google Scholar]
- 31.Gache P, Michaud P, Landry U, et al. The alcohol use disorders identification test (AUDIT) as a screening tool for excessive drinking in primary care: reliability and validity of a French version. Alcohol Clin Exp Res. 2005;29:2001–2007. doi: 10.1097/01.alc.0000187034.58955.64. [DOI] [PubMed] [Google Scholar]
- 32.Bohn MJ, Babor TF, Kranzler HR. The alcohol-use disorders identification test (audit)—validation of a screening instrument for use in medical settings. J Stud Alcohol. 1995;56:423–432. doi: 10.15288/jsa.1995.56.423. [DOI] [PubMed] [Google Scholar]
- 33.(2002) The alcohol use disorders identification test, pp 1–41
- 34.Cao W, Fang Z, Hou G, et al. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res. 2020;287:112934. doi: 10.1016/j.psychres.2020.112934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Woodgate RL, Tailor K, Tennent P, et al. The experience of the self in Canadian youth living with anxiety: a qualitative study. PLoS ONE. 2020;15:e0228193. doi: 10.1371/journal.pone.0228193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gentili D, Bardin A, Ros E, et al. Impact of communication measures implemented during a school tuberculosis outbreak on risk perception among parents and school staff, Italy, 2019. Int J Environ Res Public Health. 2020 doi: 10.3390/ijerph17030911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Schechter DS, Willheim E. Disturbances of attachment and parental psychopathology in early childhood. Child Adolesc Psychiatr Clin N Am. 2009;18:665–686. doi: 10.1016/j.chc.2009.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Pelham WE, Lang AR. Can your children drive you to drink? Stress and parenting in adults interacting with children with ADHD. Alcohol Res Health. 1999;23:292–298. [PMC free article] [PubMed] [Google Scholar]
- 39.Yousefia S, Far AS, Abdolahian E. Parenting stress and parenting styles in mothers of ADHD with mothers of normal children. Proc Social Behav Sci. 2011;30:1666–1671. doi: 10.1016/j.sbspro.2011.10.323. [DOI] [Google Scholar]
- 40.Riley AW, Valdez CR, Barrueco S, et al. Development of a family-based program to reduce risk and promote resilience among families affected by maternal depression: theoretical basis and program description. Clin Child Fam Psychol Rev. 2008;11:12–29. doi: 10.1007/s10567-008-0030-3. [DOI] [PubMed] [Google Scholar]
- 41.Bosanac P, Buist A, Burrows G. Motherhood and schizophrenic illnesses: a review of the literature. Aust N Z J Psychiatry. 2003;37:24–30. doi: 10.1046/j.1440-1614.2003.01104.x. [DOI] [PubMed] [Google Scholar]
- 42.Rasic D, Hajek T, Alda M, Uher R. Risk of mental illness in offspring of parents with schizophrenia, bipolar disorder, and major depressive disorder: a meta-analysis of family high-risk studies. Schizophr Bull. 2014;40:28–38. doi: 10.1093/schbul/sbt114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Galéra C, Pingault J-B, Fombonne E, et al. Attention problems in childhood and adult substance use. J Pediatr. 2013;163:1677–1683.e1. doi: 10.1016/j.jpeds.2013.07.008. [DOI] [PubMed] [Google Scholar]
- 44.Song Z, Xu Y, Bao L et al (2019) From SARS to MERS, thrusting coronaviruses into the spotlight. Viruses. 10.3390/v11010059 [DOI] [PMC free article] [PubMed]
- 45.Liu JJ, Bao Y, Huang X, et al. Mental health considerations for children quarantined because of COVID-19. Lancet Child Adolesc Health. 2020;4:347–349. doi: 10.1016/S2352-4642(20)30096-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Catalano R, Goldman-Mellor S, Saxton K, et al. The health effects of economic decline. Annu Rev Public Health. 2011;32:431–450. doi: 10.1146/annurev-publhealth-031210-101146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Golberstein E, Gonzales G, Meara E. How do economic downturns affect the mental health of children? Evidence from the National Health Interview Survey. Health Econ. 2019;28:955–970. doi: 10.1002/hec.3885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Alfano CA, Zakem AH, Costa NM, et al. Sleep problems and their relation to cognitive factors, anxiety, and depressive symptoms in children and adolescents. Depress Anxiety. 2009;26:503–512. doi: 10.1002/da.20443. [DOI] [PubMed] [Google Scholar]
- 49.Yurumez E, Kilic BG. Relationship between sleep problems and quality of life in children With ADHD. J Atten Disord. 2016;20:34–40. doi: 10.1177/1087054713479666. [DOI] [PubMed] [Google Scholar]
- 50.Maras D, Flament MF, Murray M, et al. Screen time is associated with depression and anxiety in Canadian youth. Prev Med. 2015;73:133–138. doi: 10.1016/j.ypmed.2015.01.029. [DOI] [PubMed] [Google Scholar]
- 51.Nagata JM, Abdel Magid HS, Gabriel KP. Screen time for children and adolescents during the COVID-19 pandemic. Obesity (Silver Spring) 2020 doi: 10.1002/oby.22917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Lissak G. Adverse physiological and psychological effects of screen time on children and adolescents: literature review and case study. Environ Res. 2018;164:149–157. doi: 10.1016/j.envres.2018.01.015. [DOI] [PubMed] [Google Scholar]
- 53.Király O, Potenza MN, Stein DJ, et al. Preventing problematic internet use during the COVID-19 pandemic: consensus guidance. Compr Psychiatry. 2020;100:152180. doi: 10.1016/j.comppsych.2020.152180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Bjelland M, Soenens B, Bere E, et al. Associations between parental rules, style of communication and children's screen time. BMC Public Health. 2015 doi: 10.1186/s12889-015-2337-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Orben A. Teenagers, screens and social media: a narrative review of reviews and key studies. Soc Psychiatry Psychiatr Epidemiol. 2020;55:407–414. doi: 10.1007/s00127-019-01825-4. [DOI] [PubMed] [Google Scholar]
- 56.Neugebauer R, Ng S. Differential recall as a source of bias in epidemiologic research. J Clin Epidemiol. 1990;43:1337–1341. doi: 10.1016/0895-4356(90)90100-4. [DOI] [PubMed] [Google Scholar]
- 57.Mathai J, Anderson P, Bourne A. Comparing psychiatric diagnoses generated by the strengths and difficulties questionnaire with diagnoses made by clinicians. Aust N Z J Psychiatry. 2004;38:639–643. doi: 10.1080/j.1440-1614.2004.01428.x. [DOI] [PubMed] [Google Scholar]
- 58.Costello EJ, Foley DL, Angold A. 10-year research update review: the epidemiology of child and adolescent psychiatric disorders: II. Developmental epidemiology. J Am Acad Child Adolesc Psychiatry. 2006;45:8–25. doi: 10.1097/01.chi.0000184929.41423.c0. [DOI] [PubMed] [Google Scholar]
- 59.Goodman R, Ford T, Simmons H, et al. Using the strengths and difficulties questionnaire (SDQ) to screen for child psychiatric disorders in a community sample. Br J Psychiatry. 2000;177:534–539. doi: 10.1192/bjp.177.6.534. [DOI] [PubMed] [Google Scholar]
- 60.Duffy KA, McLaughlin KA, Green PA. Early life adversity and health-risk behaviors: proposed psychological and neural mechanisms. Ann N Y Acad Sci. 2018;1428:151–169. doi: 10.1111/nyas.13928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Wade M, Prime H, Browne DT. Why we need longitudinal mental health research with children and youth during (and after) the COVID-19 pandemic. Psychiatry Res. 2020;290:113143. doi: 10.1016/j.psychres.2020.113143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Aljandaleh H, Bolze C, El-Khoury Lesueur F, et al. Factors associated with electronic cigarette use among young adults: the French “Trajectoires Epidé Miologiques en Population” (TEMPO) cohort study. Subst Use Misuse. 2020;55:964–972. doi: 10.1080/10826084.2020.1717534. [DOI] [PubMed] [Google Scholar]
- 63.Dalton L, Rapa E, Stein A. Protecting the psychological health of children through effective communication about COVID-19. Lancet Child Adolesc Health. 2020;4:346–347. doi: 10.1016/S2352-4642(20)30097-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Upon request.
STATA 16.1 (StataCorp, College Station, Texas, USA).