Abstract
To evaluate the association between general self-efficacy and depression/anxiety among newly HIV-diagnosed Chinese men who have sex with men (MSM) in Beijing, our study evaluated the baseline survey data of MSM taking part in a clinical trial among Chinese MSM in Beijing. The baseline survey of the trial was conducted between March 2013 and March 2014. General self-efficacy and depression/anxiety were measured using standard scales. Logistic regression and cumulative logistic regression were used to evaluate the associations between general self-efficacy and depression/anxiety. A total of 367 newly HIV-diagnosed Chinese MSM in Beijing were recruited. There were negative associations between general self-efficacy and depression/anxiety among the study population. As general self-efficacy increased by one unit, the odds of “likely” or “borderline” depression versus normal, or “likely” depression versus “borderline” depression or normal decreased by 12% [adjusted odds ratio (AOR): 0.88, 95% confidence interval (CI): 0.85–0.92] after adjusting for potential confounders. Similarly, general self-efficacy was negatively associated with anxiety (AOR: 0.89, 95% CI: 0.86–0.93). A higher level of general self-efficacy was associated with lower levels of depression and anxiety among newly HIV-diagnosed Chinese MSM. Interventions promoting overall health and wellness should address self-efficacy, depression and anxiety.
Keywords: General self-efficacy, anxiety, depression, men who have sex with men, HIV
1. Introduction
Human immunodeficiency virus (HIV) continues to pose a significant health threat to men who have sex with men (MSM) in China and many parts of the world (Cui et al., 2016; Joint United Nations Programme on HIV/AIDS, 2017; Lou et al., 2014). MSM living with HIV face dual HIV- and homosexuality-related stigmas, which may impact mental and physical health through exacerbating symptoms of depression and anxiety (Hylton et al., 2017; Tao, Wang, et al., 2017). In China, the lifetime prevalence of depression and anxiety has been found to be four times higher among MSM in comparison to the general male population (depression: 11.7% vs. 3.5%; anxiety: 18.6% vs. 3.7%) (Yu et al., 2013). Depression and anxiety are not uncommon among people living with HIV in other parts of the world as well; a study in the United States reported 36% HIV-infected people met criteria for major depression and 15.8% had generalized anxiety disorder (Bing et al., 2001). Other work in this area has found that the prevalence of depression and anxiety was relatively high among HIV-infected MSM, 58.1% and 38.2% respectively (Berg, Mimiaga, & Safren, 2004). Depression has also been found to associate with HIV risk behaviors and disease progression (Chen & Raymond, 2017; Leserman, 2008). A recent study also suggested that depression and anxiety may be associated with poorer adherence to HIV antiretroviral therapy (ART) among newly HIV-diagnosed Chinese MSM (Tao, Qian, et al., 2017). Health care programs for MSM living with HIV may be well advised to address depression and anxiety.
General self-efficacy is the belief in one’s capabilities to organize and execute the courses of action required to manage prospective situations (Bandura, 1995). A strong sense of general self-efficacy can help people be resilient to setbacks and disappointments (Bandura, 1994) and has been associate with optimism and lower stress (Zhao, Lei, He, Gu, & Li, 2015). Research has supported an association between levels of general self-efficacy and risk reduction behaviors among HIV-negative women (Somlai et al., 2000) and people living with HIV (Kalichman & Nachimson, 1999).
General self-efficacy has been found to relate to depression (Maciejewski, Prigerson, & Mazure, 2000), and interventions focused on increasing self-efficacy have reduced depression and anxiety, as well as risky sexual and injection drug use (Murphy, Stein, Schlenger, & Maibach, 2001). The negative correlation of general self-efficacy and depression and anxiety has been reported in various populations (John, Meyer, Rumpf, & Hapke, 2004; Schwarzer & Aristi, 1997), but if and how these important mental health factors influence newly HIV-diagnosed Chinese MSM is presently unknown. To address this gap, we evaluated the relationship between general self-efficacy and depression and anxiety among newly HIV-diagnosed Chinese MSM.
2. Methods
2.1. Study design and population
The present study used data from the Multi-component HIV Intervention Packages for Chinese MSM (China MP3 Project), which consisted of two phases. Of 3760 MSM who were invited to participate in the Phase I cross-sectional survey, 3588 undertook HIV tests and 455 men were HIV positive. Of these newly diagnosed participants, 367 were eventually enrolled to the Phase II randomized intervention clinical trial (RCT). The details of this trial have been described elsewhere (Liu et al., 2018). The study protocol was approved by the institutional review boards of Vanderbilt University (IRB# 111144) and the National Center for AIDS/STD Control and Prevention of Chinese Center for Disease Control and Prevention (No. X120331206).
2.2. Data collection
Sociodemographic information was collected via interviewer-administered surveys in the Phase I study, including age, ethnicity, marital status, education, employment, healthcare, monthly income, place of birth, Beijing household (or Hukou) and duration of living in Beijing. Behavioral and psychological information were gathered in the baseline survey for Phase II RCT, including drug and alcohol use, general self-efficacy, and current status of depression and anxiety.
2.3. Measurement
2.3.1. General self-efficacy
Self-efficacy was measured using the General Self-Efficacy Scale (GSES) (Schwarzer & Jerusalem, 1995), a 10-item scale in which participants are asked to rate 10 questions using one of four responses: 1 (not at all true), 2 (hardly true), 3 (moderately true) or 4 (exactly true). A higher score suggests a higher level of general self-efficacy. The scale has been used widely in Chinese populations (Wang, Liu, Shi, & Wang, 2016; Yang, Liu, Wang, Wang, & Wang, 2014), and the Chinese version of this scale had good reliability and validity (Chiu & Tsang, 2004; Wang CaiKang, 2000).
2.3.2. Depression and anxiety
Current levels of depression and anxiety were measured by the Hospital Anxiety and Depression Scale (HADS) (Zigmond & Snaith, 1983), which has been validated in previous studies (Chan, Tsang, Lau, & Chung, 2017; Watrowski & Rohde, 2014). The HADS is a 14-item scale, including 7 items related to anxiety and 7 related to depression. Items ask about feelings and emotions during the past week. Each item is scored from 0 to 3. The total possible scores for both depression and anxiety range from 0 to 21. Scores between 11 and 21 are defined as “suspected” or “likely” depression or anxiety, 8–10 defined as “borderline” depression or anxiety, and 0–7 considered “normal” or none. Categorization may be clinically meaningful, but it assumes that any score with the same category has the same effects. This assumption may not be true. Hence, we used both categorical and continuous formats of depression and anxiety scores to assess their associations with general self-efficacy.
2.4. Statistical analysis
The primary dependent variables were depression and anxiety. The variables were classified into three categories as described above, and as dichotomous – high if ≥mean score and low if <mean score. The main predictor of depression/anxiety was general self-efficacy, which was used as both continuous and dichotomous. Simple descriptive statistics (mean, standard deviation [SD], proportion and so on) for the main outcome variables and predictors were calculated. Simple logistic regression and simple cumulative logistic regression models were used to evaluate the associations between depression/anxiety and general self-efficacy. In addition, multiple logistic regression modeling and multiple cumulative logistic regression modeling were performed to assess the associations between depression/anxiety and general self-efficacy while adjusting for potential confounders: age, ethnicity, marital status, education, occupation, health care, place of birth, drug and alcohol use. For all cumulative logistic regression models in the analyses, the proportional odds assumption is satisfied since none of the score tests of the assumption is found to be significant at alpha = 0.05 level. Furthermore, predicted probabilities of depression and anxiety across the spectrum (10–40) of the GSES scores were calculated. Statistical analysis was performed using SAS (SAS 9.4; SAS Institute, Inc., Cary, NC).
3. Results
3.1. Demographic and behavioral characteristics
Of 367 newly HIV-diagnosed Chinese MSM participants, median age was 28 years (interquartile range [IQR]: 25–32). The majority were of Han ethnicity (93.2%), were single (83.9%), attended college (76.8%), had less than 5000 yuan (~750 USD) monthly income (60.0%) and had health insurance (55.3%). The prevalence of alcohol use and drug use in the last 3 months was 55.0% and 33.0%, respectively (Table 1).
Table 1.
Sociodemographic characteristics of newly HIV-diagnosed MSM in Beijing, China (N = 367).
| Covariate | Mean(SD) or N (%) | General self-efficacy (mean (SD)) | P |
|---|---|---|---|
| Age (year) | 29.6 (7.4) | 31.5 (6.3) | NA |
| Ethnicity | |||
| Han | 342 (93.2) | 31.5 (6.2) | |
| Other | 25 (6.8) | 31.5 (6.9) | 0.96 |
| Marital status | |||
| Single | 308 (83.9) | 31.6 (6.0) | |
| Currently married | 44 (12.0) | 31.2 (7.6) | |
| Divorced or separated or widowed or other | 15 (4.1) | 30.4 (7.9) | 0.70 |
| Currently living with | |||
| Others | 288 (78.5) | 31.4 (6.4) | |
| Male sexual partner | 79 (21.5) | 32.2 (5.7) | 0.28 |
| Education | |||
| Junior middle school or lower | 50 (13.6) | 28.0 (8.8) | |
| Senior high school | 35 (9.5) | 31.3 (6.1) | |
| College and above | 282 (76.8) | 32.2 (5.5) | <0.01 |
| Employment | |||
| Employed | 304 (82.8) | 31.8 (6.1) | |
| Unemployed/retired | 25 (6.8) | 27.6 (7.5) | |
| Student | 24 (6.5) | 32.0 (5.1) | |
| Other | 14 (3.8) | 31.6 (7.4) | 0.01 |
| Monthly income (Chinese yuan) | |||
| <5000 | 220 (60.0) | 31.0 (6.4) | |
| ≥5000 | 147 (40.1) | 32.5 (5.9) | 0.02 |
| Health care | |||
| Yes | 203 (55.3) | 32.0 (6.1) | |
| No | 164 (44.7) | 31.0 (6.5) | 0.11 |
| Place of birth | |||
| Large city | 92 (25.1) | 31.7 (5.4) | |
| Medium city | 89 (24.3) | 32.4 (6.2) | |
| Small city | 78 (21.3) | 31.6 (6.4) | |
| Township/countryside | 108 (29.4) | 30.6 (6.9) | 0.24 |
| Legal Beijing Residency | |||
| Yes | 66 (18.0) | 32.3 (5.7) | |
| No | 301 (82.0) | 31.4 (6.4) | 0.30 |
| Years of living in Beijing | |||
| <5 | 182 (49.6) | 31.1 (6.5) | |
| ≥5 | 185 (50.4) | 32.0 (6.1) | 0.19 |
| Alcohol use in the past 3 months | 202 (55.0) | 31.7 (5.7) | 0.54 |
| Drug use in the past 3 months | 121 (33.0) | 32.6 (5.4) | 0.03 |
Newly HIV-diagnosed Chinese MSM with lower general self-efficacy scores were more likely to have junior middle school or lower education, be unemployed, and have a monthly income less than 5000 yuan (Table 1).
3.2. Distributions of general self-efficacy, depression and anxiety
The mean score of general self-efficacy among the study population (measured by GSES with the Cronbach’s alpha 0.93) was 31.5 (SD: 6.3) on a scale of 10–40. Of 367 Chinese MSM, 70 (19.1%) were classified as “likely” depressed with the mean score of general self-efficacy scale 27.7 (SD: 8.0), 53 (14.4%) as “borderline” depression (mean: 30.3, SD: 5.7) and 244 (66.5%) as “normal” (mean 32.9, SD: 5.3). In terms of anxiety, 100 (27.3%) were classified as “likely” anxiety with mean score 28.7 (SD: 7.4), 69 (18.8%) as “borderline” anxiety (mean: 31.0, SD: 5.1) and 198 (54.0%) as “normal” (mean: 33.2, SD: 5.5) according to the HADS (Cronbach’s alpha = 0.89 for depression and anxiety) (Table 2).
Table 2.
Mean and standard deviation for general self-efficacy scores among 367 newly HIV-diagnosed Chinese MSM stratified by depression and anxiety status.
| Covariate | N (%) | General self-efficacy (mean (SD)) |
|---|---|---|
| Depression status | ||
| Normal (0–7) | 244 (66.5) | 32.9 (5.3) |
| Borderline depression (8–10) | 53 (14.4) | 30.3 (5.7) |
| Likely depression (11–21) | 70 (19.1) | 27.7 (8.0) |
| Anxiety status | ||
| Normal (0–7) | 198 (54.0) | 33.2 (5.5) |
| Borderline anxiety (8–10) | 69 (18.8) | 31.0 (5.1) |
| Likely anxiety (11–21) | 100 (27.3) | 28.7 (7.4) |
3.3. Association between general self-efficacy and depression
The simple cumulative logistic regression analysis showed that general self-efficacy was negatively associated with depression (odds ratio [OR]: 0.90, 95% confidence interval [CI]: 0.86–0.93). Specifically, the odds of being classified as being “likely” or “borderline” depressed decreased by 10% compared to being classified as “normal” with a one unit increase in the general self-efficacy score. After adjusting for potential confounders: age, ethnicity, marital status, education, occupation, health care, place of birth, drug and alcohol use, the odds of being “likely” or “borderline” depressed decreased by 12% as general self-efficacy score increased one unit (adjusted OR [AOR]: 0.88, 95% CI: 0.85–0.92). If general self-efficacy was categorized as high and low by mean score, the negative association remained significant both in the simple cumulative logistic regression model (OR: 0.36, 95% CI: 0.23–0.56) and multiple cumulative logistic regression model (AOR: 0.32, 95% CI: 0.20–0.51) (Table 3).
Table 3.
Association between depression/anxiety and self-efficacy among 367 newly HIV-diagnosed MSM in Beijing, China, using logistic regression analysis.
| Depression |
Anxiety |
|||
|---|---|---|---|---|
| Covariate | OR (CI) | AOR (CI) | OR (CI) | AOR (CI) |
| Self-efficacy | ||||
| <32 | 1.0 | 1.0 | 1.0 | 1.0 |
| ≥32 A | 0.36 (0.23–0.56)* | 0.32 (0.20–0.51)* | 0.40 (0.27–0.59)* | 0.38 (0.25–0.57)* |
| B | 0.33 (0.21–0.50)* | 0.30 (0.19–0.48)* | 0.38 (0.25–0.59)* | 0.35 (0.23–0.55)* |
| Self-efficacy (continuous) | ||||
| A | 0.90 (0.86–0.93)* | 0.88 (0.85–0.92)* | 0.90 (0.87–0.93)* | 0.89 (0.86–0.93)* |
| B | 0.89 (0.85–0.92)* | 0.87 (0.84–0.91)* | 0.90 (0.87–0.94)* | 0.89 (0.86–0.93)* |
Note: OR, crude odds ratio; AOR, odds ratio adjusted by age, ethnic, marital status, education, occupation, health care, place of birth, drug and alcohol use; CI, 95% confidence interval; A, Depression and anxiety were divided into three types (suspected, borderline depression/anxiety and normal), the normal status was used as the reference category; B, Depression and anxiety were divided into two categories: high if ≥mean score versus low if <mean score.
Significant with P < 0.0001.
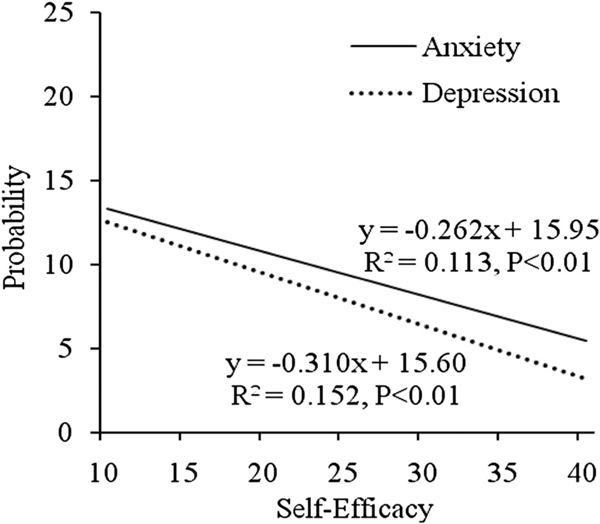
If depression was dichotomized as high or low by mean score, the negative association was also significant both in the simple logistic regression modeling (OR: 0.89, 95% CI: 0.85–0.92 for continuous measurement of GSES; OR: 0.33, 95% CI: 0.21–0.50 for dichotomous measurement) and multiple logistic regression modeling (AOR: 0.87, 95% CI: 0.84–0.91 for continuous measurement; AOR: 0.30, 95% CI: 0.19–0.48 for dichotomous measurement) (Table 3). As GSES score increased, the probability of depression decreased significantly (Figure 1).
Figure 1.
Predicted probability of depression and anxiety score by general self-efficacy among newly HIV-diagnosed Chinese MSM (N = 367).
3.4. Association between general self-efficacy and anxiety
The simple cumulative logistic regression analysis showed that general self-efficacy was negatively associated with anxiety (OR: 0.90, 95% CI: 0.87–0.93). Specifically, the odds of being “likely” or “borderline” anxiety decreased by 10% as general self-efficacy score increased one unit. After adjusting for potential confounders: age, ethnicity, marital status, education, occupation, health care, place of birth, drug and alcohol use, the odds of being “likely” or “borderline” anxiety decreased by 11% as general self-efficacy score increased one unit (AOR: 0.89, 95% CI: 0.86–0.93). If general self-efficacy was dichotomized as high or low using a mean split, the negative association remained significant both in the simple cumulative logistic regression modeling (OR: 0.40, 95% CI: 0.27–0.59) and multiple cumulative logistic regression modeling (AOR: 0.38, 95% CI: 0.25–0.57) (Table 3).
The mean split for dichotomized anxiety was negatively associated with GSES measured continuously (OR: 0.90, 95% CI: 0.87–0.94) and dichotomously (OR: 0.38, 95% CI: 0.25–0.59) in simple logistic regression models. Similarly, multiple logistic regression modeling was significant for continuous (AOR: 0.89, 95% CI: 0.86–0.93) and dichotomous measurements of GSES (AOR: 0.35, 95% CI: 0.23–0.55) (Table 3). As GSES score increased, the probability of anxiety decreased significantly (Figure 1).
4. Discussion
The mean score for general self-efficacy was 31.5 (SD: 6.3) in this study population. It was lower than those for condom use (mean: 35.2, SD: 6.0) and negotiation for safer sex (mean: 33.6, SD: 6.6) among MSM living with HIV (Brown, Serovich, Kimberly, & Umasabor-Bubu, 2015). In the newly HIV-diagnosed MSM in Beijing, there were significant associations between lower general self-efficacy score and depression or anxiety. Previous studies have reported that general self-efficacy was negatively associated with depression in Chinese transgender women (Yang et al., 2015) and unemployed individuals (Wang et al., 2014), and a negative association between general self-efficacy and anxiety among cancer patients (Mystakidou et al., 2013). In our work, newly HIV-diagnosed Chinese MSM with lower scores were significantly more likely to report symptoms of depression and anxiety.
Among 367 newly HIV-diagnosed Chinese MSM participants, about one-third (33.5%) had “likely” or “borderline” depression (19.1% “likely” and 14.4% “borderline”). It was lower than that among HIVinfected MSM in the United States (58%) (Berg et al., 2004), but was higher than 11.7% among Chinese MSM with unknown HIV status (Yu et al., 2013). Forty-six percent of participants had “likely” or “borderline” anxiety (27.3% “likely” and 18.8% “borderline”), which was higher than 38.2% previously reported in a sample of MSM living with HIV in the United States (Berg et al., 2004) and much higher than 3.7% among Chinese MSM in general (Yu et al., 2013).
To our knowledge, this study was the first one to assess the association between general self-efficacy and depression and anxiety among newly HIV-diagnosed Chinese MSM. The strengths of our research include working with MSM recently diagnosed with HIV and using a well-validated general self-efficacy and anxiety and depression scales (Chan et al., 2017; Zhang, 1995).
Limitations include the cross-sectional data that cannot be used to evaluate a temporal relationship between general self-efficacy and depression and anxiety. We could not exclude the possibility of residual confounding, for example, we did not measure other potential confounding variables such as social support.
The study findings on the negative relationship between general self-efficacy and depression and anxiety may help guide health promotion among newly HIV-diagnosed Chinese MSM. Depression and anxiety are risk factors of morbidity and mortality (Antoni et al., 2006; Ironson et al., 2005). Effective support and treatment for depression and anxiety may also improve medication adherence (Chesney et al., 2000) and self-care more generally. Our study suggests that elevated general self-efficacy does relate to lower depression and anxiety. Interventions, including cognitive–behavioral stress management and psychopharmacology should be considered as potential important parts of programs aiming to assist MSM in China adjusting to a new HIV diagnosis (Jones et al., 2010; Murphy et al., 2001). Considering the high prevalence of depression and anxiety and low level of general self-efficacy among our study population, further studies are needed to increase general self-efficacy and reduce depression and anxiety.
Acknowledgements
The funder had no role in study design, data collection and analysis, decision to publish or preparation of the manuscript.
Funding
This work was supported by the National Institute of Allergy and Infectious Diseases of the National Institutes of Health [Grant Numbers R01AI094562, R34AI091446] and National Natural Science Foundation of China [Grant number 81760616].
Footnotes
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Antoni MH, Carrico AW, Duran RE, Spitzer S, Penedo F, Ironson G, … Schneiderman N. (2006). Randomized clinical trial of cognitive behavioral stress management on human immunodeficiency virus viral load in gay men treated with highly active antiretroviral therapy. Psychosomatic Medicine, 68(1), 143–151. doi: 10.1097/01.psy.0000195749.60049.63 [DOI] [PubMed] [Google Scholar]
- Bandura A. (1994). Self-efficacy. Encyclopedia of Human Behavior, 4, 71–81. [Google Scholar]
- Bandura A. (1995). Self-efficacy in changing societies. New York: Cambridge University Press. [Google Scholar]
- Berg MB, Mimiaga MJ, & Safren SA (2004). Mental health concerns of HIV-infected gay and bisexual men seeking mental health services: An observational study [Research Support, U.S. Gov’t, P.H.S. Review]. AIDS Patient Care STDS, 18(11), 635–643. doi: 10.1089/apc.2004.18.635 [DOI] [PubMed] [Google Scholar]
- Bing EG, Burnam MA, Longshore D, Fleishman JA, Sherbourne CD, London AS, … Shapiro M. (2001). Psychiatric disorders and drug use among human immunodeficiency virus-infected adults in the United States. Archives of General Psychiatry, 58(8), 721–728. [DOI] [PubMed] [Google Scholar]
- Brown MJ, Serovich JM, Kimberly JA, & Umasabor-Bubu O. (2015). Disclosure and self-efficacy among HIV-positive men who have sex with men: A comparison between older and younger adults. AIDS Patient Care and STDs, 29(11), 625–633. doi: 10.1089/apc.2015.0133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang CaiKang LY (2000). Correlations among general self-efficacy, trait anxiety, state anxiety and test anxiety. Chinese Journal of Clinical Psychology, 8, 229–230. [Google Scholar]
- Chan CYY, Tsang HHL, Lau CS, & Chung HY (2017). Prevalence of depressive and anxiety disorders and validation of the Hospital Anxiety and Depression Scale as a screening tool in axial spondyloarthritis patients. International Journal of Rheumatic Diseases, 20(3), 317–325. doi: 10.1111/1756-185X.12456 [DOI] [PubMed] [Google Scholar]
- Chen YH, & Raymond HF (2017). Associations between depressive syndromes and HIV risk behaviors among San Francisco men who have sex with men. AIDS Care, 29(12), 1538–1542. doi: 10.1080/09540121.2017.1307925 [DOI] [PubMed] [Google Scholar]
- Chesney MA, Ickovics JR, Chambers DB, Gifford AL, Neidig J, Zwickl B, & Wu AW (2000). Self-reported adherence to antiretroviral medications among participants in HIV clinical trials: The AACTG adherence instruments Patient Care Committee & Adherence Working Group of the Outcomes Committee of the Adult AIDS Clinical Trials Group (AACTG). AIDS Care, 12(3), 255–266. doi: 10.1080/09540120050042891 [DOI] [PubMed] [Google Scholar]
- Chiu FP, & Tsang HW (2004). Validation of the Chinese general self-efficacy scale among individuals with schizophrenia in Hong Kong. International Journal of Rehabilitation Research, 27(2), 159–161. [DOI] [PubMed] [Google Scholar]
- Cui Y, Guo W, Li D, Wang L, Shi CX, Brookmeyer R, Wu Z. (2016). Estimating HIV incidence among key affected populations in China from serial cross-sectional surveys in 2010–2014. Journal of The international Aids Society, 19(1), 20609. doi: 10.7448/IAS.19.1.20609 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hylton E, Wirtz AL, Zelaya CE, Latkin C, Peryshkina A, Mogilnyi V, … Beyrer C. (2017). Sexual identity, stigma, and depression: The role of the “Anti-gay Propaganda Law” in mental health among men who have sex with men in Moscow, Russia. Journal of Urban Health, 94(3), 319–329. doi: 10.1007/s11524-017-0133-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ironson G, Weiss S, Lydston D, Ishii M, Jones D, Asthana D, … Antoni M. (2005). The impact of improved self-efficacy on HIV viral load and distress in culturally diverse women living with AIDS: The SMART/EST Women’s Project [Clinical Trial Randomized Controlled Trial Research Support, N.I.H., Extramural Research Support, U.S. Gov’t, P.H.S.]. AIDS Care, 17(2), 222–236. doi: 10.1080/09540120512331326365 [DOI] [PubMed] [Google Scholar]
- John U, Meyer C, Rumpf HJ, & Hapke U. (2004). Self-efficacy to refrain from smoking predicted by major depression and nicotine dependence [Research Support, Non-U.S. Gov’t]. Addictive Behaviors, 29(5), 857–866. doi: 10.1016/j.addbeh.2004.02.053 [DOI] [PubMed] [Google Scholar]
- Joint United Nations Programme on HIV/AIDS. (2017). The Global AIDS Update 2017. Retrieved from http://www.unaids.org/sites/default/files/media_asset/20170720_Data_book_2017_en.pdf [Google Scholar]
- Jones DL, Ishii Owens M, Lydston D, Tobin JN, Brondolo E, & Weiss SM (2010). Self-efficacy and distress in women with AIDS: The SMART/EST women’s project. AIDS Care, 22(12), 1499–1508. doi: 10.1080/09540121.2010.484454 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalichman SC, & Nachimson D. (1999). Self-efficacy and disclosure of HIV-positive serostatus to sex partners [Research Support, U.S. Gov’t, P.H.S.]. Health Psychology, 18(3), 281–287. [DOI] [PubMed] [Google Scholar]
- Leserman J. (2008). Role of depression, stress, and trauma in HIV disease progression [Research Support, N.I.H., Extramural Review]. Psychosomatic Medicine, 70(5), 539–545. doi: 10.1097/PSY.0b013e3181777a5f [DOI] [PubMed] [Google Scholar]
- Liu Y, Vermund SH, Ruan Y, Liu H, Rivet Amico K, Simoni JM, … Qian H. (2018). Peer counselling versus standard-of-care on reducing high-risk behaviours among newly diagnosed HIV-positive men who have sex with men in Beijing, China: A randomized intervention study. Journal of the International Aids Society, 21(2). doi: 10.1002/jia2.25079 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lou J, Blevins M, Ruan Y, Vermund SH, Tang S, Webb GF, … Qian HZ (2014). Modeling the impact on HIV incidence of combination prevention strategies among men who have sex with men in Beijing, China [Research Support, N.I.H., Extramural Research Support, Non-U.S. Gov’t]. PLoS One, 9(3), e90985. doi: 10.1371/journal.pone.0090985 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maciejewski PK, Prigerson HG, & Mazure CM (2000). Self-efficacy as a mediator between stressful life events and depressive symptoms. Differences based on history of prior depression. British Journal of Psychiatry, 176, 373–378. [DOI] [PubMed] [Google Scholar]
- Murphy DA, Stein JA, Schlenger W, & Maibach E. (2001). Conceptualizing the multidimensional nature of self-efficacy: Assessment of situational context and level of behavioral challenge to maintain safer sex National Institute of Mental Health Multisite HIV Prevention Trial Group [Research Support, U.S. Gov’t, P.H.S.]. Health Psychology, 20(4), 281–290. [PubMed] [Google Scholar]
- Mystakidou K, Tsilika E, Parpa E, Gogou P, Panagiotou I, Vassiliou I, & Gouliamos A. (2013). Relationship of general self-efficacy with anxiety, symptom severity and quality of life in cancer patients before and after radiotherapy treatment. Psycho-oncology, 22(5), 1089–1095. doi: 10.1002/pon.3106 [DOI] [PubMed] [Google Scholar]
- Schwarzer R, & Aristi B. (1997). Optimistic self-beliefs: Assessment of general perceived self-efficacy in thirteen cultures. Word Psychology, 3(1–2), 177–190. [Google Scholar]
- Schwarzer R, & Jerusalem M. (1995). Generalized Self-Efficacy scale. In Weinman J, Wright S, & Johnston M, Measures in health psychology: A user’s portfolio. Causal and control beliefs (pp. 35–37). Windsor, UK: NFERNELSON. [Google Scholar]
- Somlai AM, Kelly JA, Heckman TG, Hackl K, Runge L, & Wright C. (2000). Life optimism, substance use, and AIDS-specific attitudes associated with HIV risk behavior among disadvantaged innercity women [Research Support, Non-U.S. Gov’t Research Support, U.S. Gov’t, P.H.S.]. Journal of Women’s Health & Gender Based Medicine, 9(10), 1101–1111. doi: 10.1089/152460900446018 [DOI] [PubMed] [Google Scholar]
- Tao J, Qian HZ, Kipp AM, Ruan Y, Shepherd BE, Amico KR, … Vermund SH (2017). Effects of depression and anxiety on antiretroviral therapy adherence among newly diagnosed HIV-infected Chinese MSM. AIDS, 31(3), 401–406. doi: 10.1097/QAD.0000000000001287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tao J, Wang L, Kipp AM, Qian HZ, Yin L, Ruan Y, … Vermund SH (2017). Relationship of stigma and depression among newly HIV-diagnosed Chinese men who have sex with men. AIDS and Behavior, 21(1), 292–299. doi: 10.1007/s10461-016-1477-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang ZY, Liu L, Shi M, & Wang L. (2016). Exploring correlations between positive psychological resources and symptoms of psychological distress among hematological cancer patients: A cross-sectional study. Psychology, Health & Medicine, 21(5), 571–582. doi: 10.1080/13548506.2015.1127396 [DOI] [PubMed] [Google Scholar]
- Wang Y, Yao L, Liu L, Yang X, Wu H, Wang J, & Wang L. (2014). The mediating role of self-efficacy in the relationship between Big five personality and depressive symptoms among Chinese unemployed population: A cross-sectional study. BMC Psychiatry, 14, 61. doi: 10.1186/1471-244x-14-61 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watrowski R, & Rohde A. (2014). Validation of the Polish version of the Hospital Anxiety and Depression Scale in three populations of gynecologic patients. Archives of Medical Science, 10(3), 517–524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang YL, Liu L, Wang XX, Wang Y, & Wang L. (2014). Prevalence and associated positive psychological variables of depression and anxiety among Chinese cervical cancer patients: A cross-sectional study. PLoS One, 9(4), e94804. doi: 10.1371/journal.pone.0094804 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang X, Wang L, Hao C, Gu Y, Song W, Wang J, … Zhao Q. (2015). Sex partnership and self-efficacy influence depression in Chinese transgender women: A cross-sectional study. PLoS One, 10(9). doi: 10.1371/journal.pone.0136975 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu L, Jiang C, Na J, Li N, Diao W, Gu Y, … Pan G. (2013). Elevated 12-month and lifetime prevalence and comorbidity rates of mood, anxiety, and alcohol use disorders in Chinese men who have sex with men [Research Support, Non-U.S. Gov’t]. PLoS One, 8(4), e50762. doi: 10.1371/journal.pone.0050762 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang JX SR (1995). Measuring optimistic self-beliefs: A Chinese adaptation of the General Self-Efficacy Scale. Psychologia, 38, 174–181. [Google Scholar]
- Zhao FF, Lei XL, He W, Gu YH, & Li DW (2015). The study of perceived stress, coping strategy and selfefficacy of Chinese undergraduate nursing students in clinical practice. International Journal of Nursing Practice, 21(4), 401–409. [DOI] [PubMed] [Google Scholar]
- Zigmond AS, & Snaith RP (1983). The hospital anxiety and depression scale. Acta Psychiatrica Scandinavica, 67 (6), 361–370. [DOI] [PubMed] [Google Scholar]