Abstract
Objectives
Caring for individuals with intellectual disabilities (ID) or autism spectrum disorder (ASD) can be gratifying as well as stressful. Professional staff employed as caregivers often report compromised mental and physical wellbeing due to the stressful nature of working with clients who exhibit aggressive and destructive behaviors. Prolonged work-related stress results in diminished quality of life for the caregivers. The aim of the present study was to evaluate the comparative effects of three programs—mindfulness program, psychoeducational program, and inservice training-as-usual—on the quality of life of professional caregivers who provide services to adolescent and adult clients with ID and ASD
Methods
Professional caregivers (N = 216) were randomized into three experimental conditions, and trained in mindfulness, psychoeducation, and inservice training-as-usual. The effects of the training on the caregivers’ quality of life were assessed in terms of perceived stress, compassion satisfaction, compassion fatigue (i.e. burnout, secondary traumatic stress), and symptoms of depression at the end of 32 weeks of implementation.
Results
Perceived stress, burnout, and secondary traumatic stress decreased significantly in the mindfulness condition, followed by psychoeducation, but not in the inservice training-as-usual condition. Compassion satisfaction increased significantly in the mindfulness condition, followed by psychoeducation, but not in the inservice training-as-usual condition. Symptoms of depression, which were rated in the borderline clinical range prior to intervention, decreased significantly to within normal levels in the mindfulness condition, decreased minimally in the psychoeducation condition, and showed no change in the training-as usual condition.
Conclusions
A 3-day training in mindfulness meditations and associated contemplative practices provides a better basis for enhancing caregivers’ quality of life than psychoeducation or inservice training-as-usual.
Keywords: Developmental disabilities, caregivers, MBPBS, mindfulness, psychoeducation, inservice training, stress, burnout
Many caregivers gain much gratification in providing care to people with disabilities, especially those in pain and suffering (Beighton and Wills 2019; Hastings and Horne 2004). In the fields of intellectual disabilities (ID) and autism spectrum disorder (ASD), parents and other family members often provide the caregiving, but individuals with ID and ASD who reside in institutions and community group homes rely on professionals employed specifically to support and take care of their needs. Regardless of whether parents and family members or professional staff provide the caregiving, being constantly exposed to challenging behaviors, pain, and suffering of their care recipients can be emotionally draining, often leading to stress, compassion fatigue, and decreased quality of life (Hensel et al. 2012, Mutkins et al. 2011). In this context, quality of life refers to the positive and negative effects of working under stressful conditions in human services. Although there are multiple pathways that affect caregiver quality of life, including the personal attributes of the caregivers, the key issues appear to be severity of the individuals’ disability, their behavioral challenges (e.g. aggressive and destructive behaviors), limited organizational support, and inadequate training to address these issues (Korsitas et al. 2010, Rose et al. 2010).
Several programs have been developed to provide support and training to caregivers of individuals with ID and ASD. The majority of research evaluating this effort has been with parents and family caregivers (Iadarola et al. 2018, Smith and Iadarola 2015), mostly with mothers of children with ASD. A meta-analysis of 41 studies focusing on parental caregivers of individuals with ASD reported the effectiveness of a number of different programs, including social support, positive psychotherapy, written emotional disclosure, multicomponent interventions, psychoeducational programs, Acceptance and Commitment Therapy (ACT), and mindfulness-based programs (Yu et al. 2019). While all interventions were somewhat effective, ACT, mindfulness programs, and cognitive behavioral interventions (CBT) were more effective than the others in terms of psychosocial outcomes for the caregivers.
There is emerging research on interventions with professional caregivers with the earliest studies using psychoeducation and CBT for self-management of work-related stress (Gardner et al. 2005, Innstrand et al. 2004, Rose et al. 1998). Other studies have used ACT or ACT-based interventions or mindfulness-based programs. For example, in two related studies, Noone and Hastings (2009, 2010) provided an ACT-based intervention training called Promotion of Acceptance in Carers and Teachers (PACT) to support staff in intellectual disabilities. Results showed a reduction in psychological distress following training on PACT even when the support staff perceived no change in the level of their work stress. In a pilot study, Bethay et al. (2013) assessed the effects of an ACT intervention combined with instruction in applied behavior analysis (ABA) against instruction in ABA alone on staff members’ general distress and burnout. While there was no overall difference between the two interventions in terms of outcomes for the participants, subsidiary analyses indicated that those with greater psychological distress at the outset of the study showed larger reductions in psychological distress in the ACT plus ABA intervention condition than those in the ABA alone condition. Similar findings were reported for indicators of burnout in the ACT plus ABA participants when compared to participants in the ABA alone condition. Outcomes were mixed, however, when ACT interventions were evaluated in two randomized controlled trials (RCT). One study reported significant reductions in perceived stress (Biglan et al. 2013) while the other reported increased stress following training in ACT (McConachie et al. 2014). Psychological distress, which was measured only in the McConachie et al. (2014) study, significantly decreased following an ACT intervention thus supporting the findings of Noone and Hastings (2010).
Mindfulness-based programs (MBPs) have been used for enhancing the wellbeing of professional caregivers of people with ID and ASD (Hwang and Singh 2016, Myers et al. 2014). Brooker et al. (2013) reported mixed findings in a study that evaluated the effects of a customized “occupational mindfulness” program with staff in disability services. Staff reported increased positive affect, no change in intrinsic job satisfaction, but significant decrease in extrinsic job satisfaction. In addition, there were significant increases in negative affect, perceived stress, anxiety, and negative emotional symptoms. However, the staff also reported enhanced awareness of signs and sources of stress, and positive changes in self-care attitudes and interactions with clients. A series of studies evaluated the effects of Mindfulness-Based Positive Behavior Support (MBPBS) on client and staff outcomes. Singh et al. (2015) reported significant reductions in staff use of verbal redirection, elimination of use of physical restraints, reduction in staff stress, and zero staff turnover as a result of staff caregiver training in MBPBS. These findings were replicated and extended in a proof-of-concept study (Singh, Lancioni, Karazsia, and Myers 2016), and an RCT (Singh, Lancioni, Karazsia, and Chan, et al. 2016), suggesting the findings are reliable and robust. In a further RCT that compared the effects of MBPBS to PBS alone, Singh, Lancioni, Medvedev, et al. (2020) reported that while both conditions were effective in significantly decreasing staff perceived stress, burnout, and secondary traumatic stress, and increasing compassion satisfaction, the MBPBS program was significantly more effective than PBS alone.
MBPBS is the braiding of two evidence-based programs—mindfulness and positive behavior support (Singh, Lancioni, Chan, et al. 2020). Given the superiority of MBPBS over PBS alone, it stands to reason that the mindfulness program may be the key ingredient of MBPBS that makes a significant difference in the quality of life of professional caregivers who provide services to people with ID and ASD, but this proposition has not been experimentally evaluated. Thus, the aim of the present study was to assess the effects of the mindfulness component of the MBPBS program in a randomized controlled trial against an active treatment condition (i.e. psychoeducation) and a control condition (i.e. inservice training-as-usual). Specifically, we tested the hypothesis that professional caregivers’ quality of life outcomes (i.e. perceived stress, compassion satisfaction, burnout, secondary traumatic stress, and symptoms of depression) would be significantly enhanced in the mindfulness program, followed by the psychoeducation training, and least in the inservice training-as-usual condition.
Method
Participants
The participants were professional caregivers in group homes for adolescents and adults with ID and ASD, and employed by a single agency. As part of the agency’s professional development plan for enhancing the health and wellness of caregivers, all direct caregiver staff were invited by the agency to participate in one of three programs for enhancing self-care and quality of life. Of the 249 caregivers available for the training, 33 did not meet the inclusion criteria (i.e. fulltime employment, availability during the scheduled training). The remaining 216 caregivers who consented to participate were randomized into a mindfulness program, a psychoeducation program, or a control group program (i.e. inservice training-as-usual). The agency informed all staff that the three programs were effective, included evidence-based components, and could be equally beneficial. They were also informed that the comparative outcomes of the three programs would be evaluated to inform future planning of the agency’s health and wellness programs.
Seventy-two participants were assigned to each experimental condition, clustered by group homes to avoid contamination of training across the three experimental conditions. Each group home had 6 caregivers and thus 12 clusters of group homes were assigned to each experimental condition. Those who participated in the mindfulness condition had an average age of 40.68 years (range = 19 to 61), an average service years of 15.11 (range = 1 to 37), and included 42 females. Those in the psychoeducational condition had an average age of 37.89 years (range = 19 to 61), an average service years of 13.76 (range = 1 to 35), and included 38 females. The participants in the control condition had an average age of 39.61 years (range = 19 to 61), an average service years of 15.17 (range = 1 to 39), and included 39 females. There were no statistically significant differences in age, service years, and sex distribution across the three groups (p > 0.05).
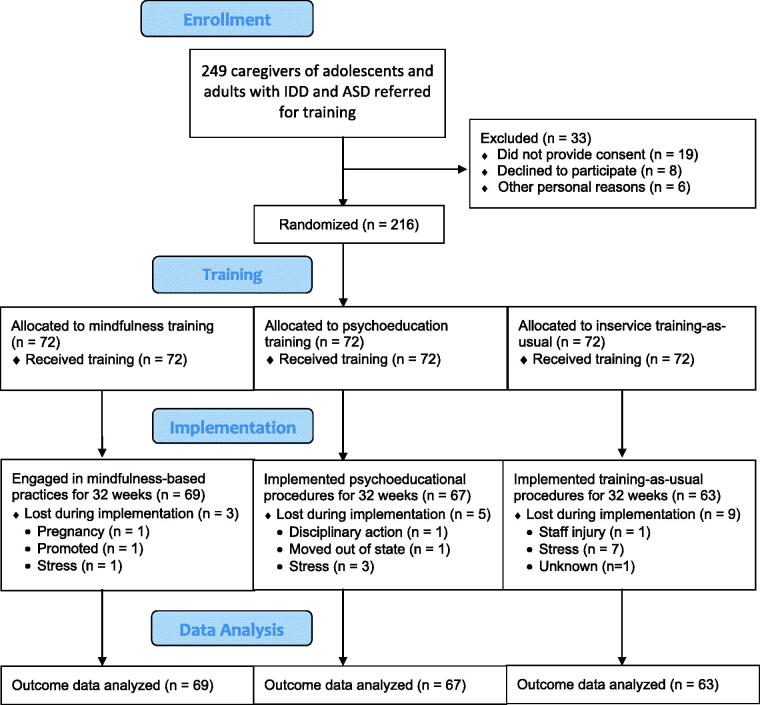
Some participants in each experimental condition were lost during implementation, i.e. 3, 5, and 9 in the mindfulness, psychoeducation, and inservice training-as-usual conditions, respectively. Figure 1 presents a CONSORT participant flow diagram.
Figure 1.
Consort flow diagram.
Procedure
Experimental design
A three-arm cluster randomized controlled trial design was used, with two active conditions and a control condition: a mindfulness program; a psychoeducation program; and an inservice training-as-usual program. The caregivers in each cluster of group homes were assigned to the same training condition to minimize diffusion of instructions across clusters and experimental conditions. Furthermore, the group home agency directed the participants not to share their training and training materials with participants from other group homes. To control for non-specific factors that may affect outcomes across the three conditions, the following were programmed: (a) training time in each condition was 8 h each day for 3 consecutive days; (b) training was presented in a group format; (c) the trainers were matched across the three experimental conditions as much as possible for professional qualification, content expertise, and training experience; and (d) the agency director explicitly stated to the participants that: (i) regardless of the experimental condition, the training would be beneficial for the caregivers, (ii) attendance was required, (iii) home practice was required, (iv) full implementation of the program was required for 32 weeks following condition-specific training, and (v) full participation in the evaluation of outcomes was required.
Experimental conditions
Mindfulness program
In the mindfulness condition, the 3-day stepped care mindfulness program from the full MBPBS program was used to teach basic meditations and related contemplative practices. The mindfulness program included the following standard Buddhist meditation practices: (1) Samatha, walking, and insight meditations; (2) five hindrances (i.e. sensory desire, ill will, sloth and torpor, restlessness and remorse, and doubt); (3) the four Immeasurables (i.e. lovingkindness; compassion; empathetic joy, and equanimity (equipoise); (4) the three poisons (i.e. attachment, anger, and ignorance (doubt); (5) beginner’s mind; (6) informal mindfulness practices; and (7) practicing ethical precepts (e.g. refrain from harming anyone, taking that which is not given, and incorrect or false speech). Following instructions in the meditation practices, the caregivers were encouraged to develop a daily formal meditation practice for about 20 min that involved focused meditation and different combinations of the other meditations.
Psychoeducational program
A psychoeducational program was developed specifically for this condition. The program had two key functions. First, it was designed to teach caregivers key aspects of workplace stress, how to recognize it, and how to reduce it. Second, it was designed to educate caregivers how to meet the needs of individuals with ID and ASD. This included information on positive methods of responding to the behavioral excesses and deficits of the individuals, and their social and instructional relationship with the individuals. The program emphasized the following: (1) how to relate skillfully with the individuals (i.e. effective communication that is positive, attentive, and nonjudgmental); (2) accepting of the individual especially when they are engaged in challenging behaviors (i.e. reducing automatic negative responses, no use of aversive or punishing consequences, responding in a calm manner that shows the caregiver understands the behavioral functions of the challenging behaviors, as well as the role of emotion dysregulation in their behavior); and (3) using evidence-based and practice-based evidence for the treatment of individuals with ID and ASD.
Inservice training-as-Usual program
The agency responsible for the group homes provided their standard inservice training on care and management of individuals with ID and ASD, as well as booster sessions to supplement the new employee training. The yearly updated training curriculum included: (1) behavior management; (2) crisis intervention plans; (3) 1-on-1 interventions; (4) emergency medications for severe aggressive behavior to self, peers, and staff; (5) physical restraints; (6) aversive contingencies and punishment strategies; and (7) skills training.
Implementation
Following the three days of training, caregivers in each condition were required to implement the substance of their training with the clients. The formal implementation period (i.e. for the study) was for 32 weeks, and no additional training was provided during this period. However, the instructor for each experimental condition was available as a resource to the agency during this period.
Training adherence and home meditation practice
Participant attendance in each of the three training programs was documented. The participants were provided a Daily Meditation Log for documenting their daily meditation practice. Even though meditation practice was an integral part of only the mindfulness program, it was deemed advisable to request all participants to collect such data because meditation instruction is increasingly available in the community and could be a part of the lifestyle of participants in the other two experimental conditions.
Training format
In each experimental condition, training was provided in small groups of up to 25 caregivers at one of the residential group homes. The training included didactic instruction, experiential practicum, demonstration, modeling, videos, and meditation practices. While these six training formats cover the universe of training techniques used across the three experimental conditions, they were used singly or in combination with each component of the training, as appropriate. For example, in the mindfulness training condition, the five hindrances are usually taught via didactic instruction and experiential practice.
Trainers
The mindfulness teacher was an experienced meditation teacher, with a long-standing personal practice of meditation, and a PhD in psychology. The psychoeducation instructor was an experienced behavioral psychologist at the PhD level. The two inservice instructors at the PhD level were agency staff who provided regular training to new employees as well as periodic inservice training to all staff.
Fidelity of training
Two aspects of fidelity were assessed in each of the three experimental conditions, structural fidelity (i.e. what is being taught) and process fidelity (i.e. how the contents are being taught) (Feagans Gould et al. 2016). An additional experienced instructor for each condition was present during training in each of the three experimental conditions and performed the fidelity ratings. The fidelity data collectors did not deliver any of the instructions in this study. The four commonly accepted facets of fidelity of implementation (Dane and Schneider 1998, Dusenbury et al. 2003) were adapted for monitoring the fidelity of training in each experimental condition. These facets included: adherence (i.e. extent to which the core training components of each program were taught); dosage (i.e. the number of training sessions delivered); quality (i.e. extent to which the trainer delivered the program components and contents as intended); and responsiveness (i.e. extent to which the trainer was responsive and skillfully engaged with the training participants). The structural and process fidelity were assessed at 100% for all three experimental conditions.
Measures
Training attendance
Agency staff provided records of staff attendance during the 3-day training for each of the three experimental conditions.
Meditation practice
Participants in each experimental condition were required to keep a daily log of the number of minutes they meditated throughout the study.
Outcome variables
Participants in all three experimental conditions completed three self-reported rating scales at two timepoints: immediately prior to the first day of training and during the last week of the 32-week study. On average, the caregivers took about 30 min to complete the rating scales.
Perceived psychological stress
The Perceived Stress Scale (PSS-10; Cohen et al. 1983) is a 10-item rating scale that measures each participant’s perception of current psychological stress caused by different situations and events in their lives in the preceding month. It provides a subjective evaluation of lack of control, unpredictability, and overload in a person’s daily life (Cohen and Williamson 1988). The items are rated on a 5-point Likert scale that ranges from 0 (never) to 4 (very often), with four items (i.e. Items #: 4, 5, 7, and 8) being reversed scored. Higher total scores indicate greater stress. PSS-10 has adequate psychometric properties, with Cronbach’s alpha of 0.78 (Cohen and Williamson 1988) and 0.82 for the present study.
Professional quality of life
The Professional Quality of Life (ProQOL) is a 30-item rating scale for measuring how a caregiver feels in relation to their work. ProQOL has a positive (Compassion Satisfaction—the pleasure derived from being able to do one’s work well) and a negative (Compassion Fatigue—work-related, secondary exposure to extremely or traumatically stressful events) component, with Compassion Fatigue including: (1) Burnout—exhaustion, frustration, anger, and depression; and (2) Secondary Traumatic Stress—negative feeling driven by fear and work-related trauma (Stamm 2010). The items are rated on a 5-point Likert scale that ranges from 1 (never) to 5 (very often), with five items (i.e. Items: 1, 4, 15, 17 and 29) being reversed scored. The items are summed by subscale and the raw score is converted to a t-score. ProQOL has adequate psychometric properties, with Cronbach’s alpha of 0.88 for compassion satisfaction (0.87 for the present study), 0.75 for burnout (0.80 for the present study), and 0.81 for secondary traumatic stress (0.83 for the present study). A score of 43 or less is low, between 43-56 is average, and above 57 is high on each of the three scales. High scores indicate greater compassion satisfaction, burnout, and secondary traumatic stress.
Symptoms of depression
The Beck Depression Inventory-II (BDI-II; Beck et al. 1996) is a 21-item rating scale that measures symptoms and severity of depression in individuals aged 13 years and older. The scale can be used as a baseline measure of severity of symptoms of depression and responsiveness to treatment. Its items measure cognitive, affective, somatic, and vegetative symptoms of depression during the preceding 2 weeks. The items are rated on a 4-point Likert scale that ranges from 0 (not at all) to 3 (greatest severity of each symptom). The total score is obtained by adding the ratings for all 21 items. Higher scores are indicative of greater severity. For those diagnosed with depression, the scores can be interpreted as: minimal range = 0–9, mild depression = 10–16, moderate depression = 17–29, and severe depression = 30–63. For non-clinical populations (as in the present study), a score of 1-10 = normal ups and downs of life, 11-16 = mild mood disturbance, 17-20 = borderline clinical depression, 21-30 =moderate depression, 31-40 = severe depression, and over 40 = extreme depression. The BDI-II has adequate psychometric properties, with Cronbach’s alpha of 0.81 in a psychiatric sample (Beck, Steer, and Carbin 1988) and 0.85 for the present study.
Data analyses
Data from all rating scales were distributed close to normal with acceptable values of skewness ranging from −0.50 to 0.32 and kurtosis ranging from −1.22 to 0.19 (Muthén and Kaplan 1985).
Outcome variables were analyzed using mixed model ANOVA (3 × 2) with three groups (mindfulness, psychoeducation, and control) as between-subject factors and pre-intervention (baseline) and post-intervention as within-subject factors. Post-hoc tests were used to determine statistical significance of differences between groups and within groups if the relevant significant effects were indicated by the omnibus ANOVA. Differences between groups at baseline were tested using independent t-tests Bonferroni adjusted for the number of comparisons to reduce possibility of Type I error. Statistical significance was determined based on the conventional cut-off point of p-value < .05 throughout.
Results
Attendance was 100% because it was a requirement by the agency that all staff must attend their assigned training following randomization. The mean daily meditation time during the 32-week implementation was 21.0 min (range = 12 to 34 min) for participants in the mindfulness program condition, 2.0 min (range = 0 to 5 min) in the psychoeducation condition, and 0 min in the inservice training-as-usual control condition.
Figure 2 shows that caregivers’ perceived stress was at the same baseline level with no significant differences identified among the three groups. At post-intervention the largest decrease in perceived stress was evident in the mindfulness group, followed by a noticeable decrease in the psychoeducation group. There was no change in the control group. Mixed ANOVA indicated significant large effects of time (F(1, 196) = 1173.81, p<.001, η2 = .86), group (F(2, 196) = 164.94, p<.001, η2 = .63) and time-group interaction (F(2, 196) = 495.28, p<.001, η2 = .84) on caregivers’ perceived stress, reflecting significant changes in stress levels across groups over time. Differences among all three groups were statistically significant at post-intervention as indicated by post-hoc tests (all p-values <.001).
Figure 2.
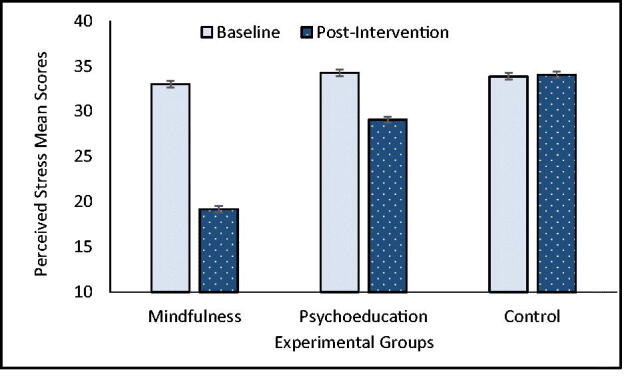
Perceived stress mean scores (PSS-10) for mindfulness, psychoeducation, and control groups self-rated at baseline and post-intervention. Error bars indicate standard error of the mean.
There were no significant differences among the three groups in compassion-satisfaction levels at baseline. Figure 3 shows a large increase in caregivers’ compassion satisfaction in the mindfulness group at post-intervention followed by a lower but substantial increase in the psychoeducation group and a minor decrease in the control group. Mixed ANOVA indicated strong significant effects of time (F(1, 196) = 869.23, p<.001, η2 = .82) and time-group interaction (F(2, 196) = 355.54, p<.001, η2 = .78), and a moderate effect of group (F(2, 196) = 28.23, p<.001, η2 = .23) on caregivers’ compassion satisfaction. Differences among all three groups were statistically significant at post-intervention as indicated by post-hoc tests (all p-values <.01).
Figure 3.
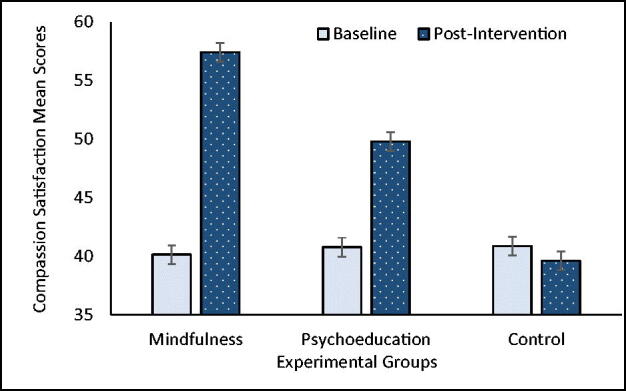
Compassion Satisfaction mean scores (ProQOL) for mindfulness, psychoeducation, and control groups self-rated at baseline and post-intervention. Error bars indicate standard error of the mean.
There was a significant difference between burnout mean scores of psychoeducation and control groups at baseline (2.67; 95% CI [0.60, 4.73], p<.01), but no significant differences were identified between mindfulness and each of two other groups. Caregivers’ burnout mean scores for all three experimental groups are presented in Figure 4. The largest decrease in burnout was observed at post-intervention in the mindfulness group and a noticeable decline was seen in the psychoeducation group, while a relatively small increase appeared in the control group. Strong significant effects of time (F(1, 196) = 562.07, p<.001, η2 = .74), group (F(2, 196) = 85.58, p<.001, η2 = .47) and their interaction (F(2, 196) = 285.70, p<.001, η2 = .75) on burnout were indicated by Mixed ANOVA. Significant differences were found among all three groups at post-intervention, as indicated by post-hoc tests (all p-values <.001).
Figure 4.
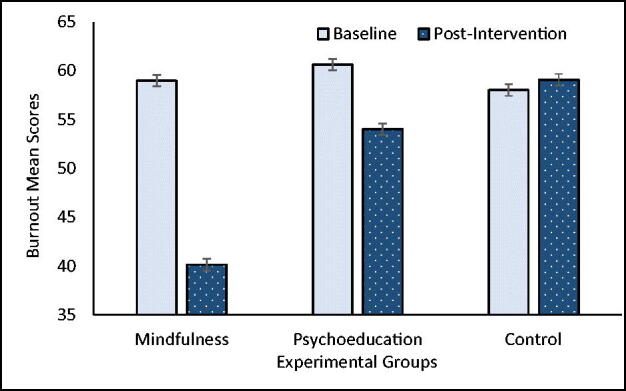
Burnout mean scores (ProQOL) for mindfulness, psychoeducation, and control groups self-rated at baseline and post-intervention. Error bars indicate standard error of the mean.
No statistically significant group differences were identified in traumatic stress at baseline. Figure 5 illustrates the largest decrease in traumatic stress mean scores found in the mindfulness group at post-intervention followed by a smaller decrease in the psychoeducation group. In contrast, a slight increase in traumatic stress was found in the control condition. Significant large effects of time (F(1, 196) = 1173.81, p<.001, η2 = .86), group (F(2, 196) = 164.94, p<.001, η2 = .63) and their interaction (F(2, 196) = 495.28, p<.001, η2 = .84) on traumatic stress were found using Mixed ANOVA. Post-hoc tests provided evidence for significant differences of traumatic stress mean scores among all three groups at post-intervention (all p-values <.001).
Figure 5.
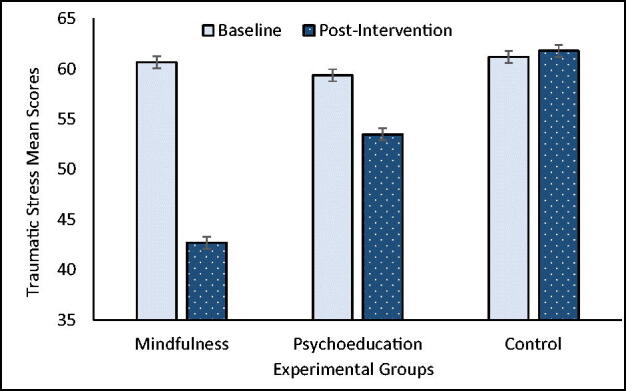
Traumatic Stress mean scores (ProQOL) for mindfulness, psychoeducation, and control groups self-rated at baseline and post-intervention. Error bars indicate standard error of the mean.
Means scores for symptoms of depression did not differ significantly at baseline among the three groups. Caregivers’ symptoms of depression mean scores at baseline and post-intervention for all three groups are presented in Figure 6. The largest decline in symptoms of depression was found in the mindfulness group followed by an apparent but smaller decline in the psychoeducation group at post-intervention, whereas no decrease was evident in the control group. Similar to stress, Mixed ANOVA revealed significant and large effects of time (F(1, 196) = 367.89, p<.001, η2 = .65) and interaction between time and group (F(2, 196) = 240.55, p<.001, η2 = .71) on caregivers’ symptoms of depression scores. There was also a significant moderate group effect (F(2, 196) = 30.57, p<.001, η2 = .24) on caregivers’ symptoms of depression. Post-hoc tests showing significant differences among all three groups at post-intervention (all p-values <.01).
Figure 6.
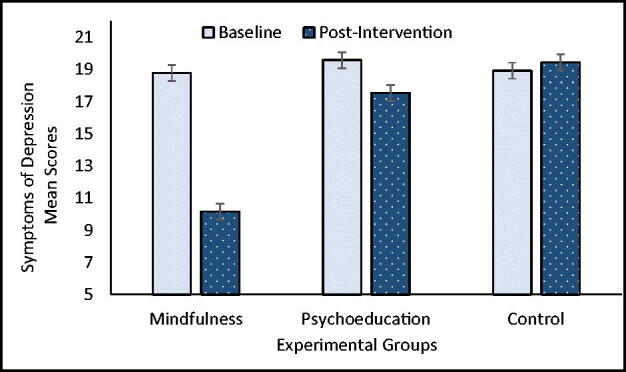
Symptoms of depression mean scores (BDI-II) for mindfulness, psychoeducation, and control groups self-rated at baseline and post-intervention. Error bars indicate standard error of the mean.
Discussion
Parental caregiving of children with ID and ASD is sometimes accompanied by positive effects that provide some balance to the adverse effects on their physical and mental wellbeing (Beighton and Wills 2019). However, there is a dearth of research on the positive effects of caregiving when the caregiver is a paid employee. Most of the research suggests that, depending on the intensity and duration of caregiving, work stress and burnout may compromise caregivers’ quality of life in terms of overall health, mental health, and wellbeing (Hatton et al. 1999, Skirrow and Hatton 2007). Furthermore, the bidirectional effects of client challenging behaviors on their caregivers, and caregiver stress and burnout on their clients, create an escalating negative behavioral spiral (Bluth and Wahler 2011, Sameroff 1995, Singh, Lancioni, Karazsia, and Myers 2016). This negative cycle can be broken by intervening with the caregiver, client, or both. Given the number of clients compared to caregivers, it is often more prudent and relatively easier to intervene with the caregivers rather than with the clients.
The results of the present study showed that the mindfulness component of the MBPBS program was significantly better at enhancing compassion satisfaction and in reducing caregiver perceived psychological stress, burnout, secondary traumatic stress, and symptoms of depression when compared to psychoeducation and inservice training-as-usual. Thus, the findings support our hypothesis that mindfulness training would be the most effective of the three experimental conditions in enhancing caregiver quality of life. A significant strength of the study is the use of an RCT design that included a mindfulness program as the experimental condition, a psychoeducation training program as the active comparison condition, and an inservice training-as-usual program as the control condition. The study was undertaken in the “real world” context of group homes thereby making it an effectiveness study as opposed to an RCT efficacy study under ideal conditions. This speaks to the generalizability of the findings to other community-based settings. Another important aspect of the study is that the training was only for three days, thus making it reasonably short and feasible for most agencies to incorporate it in their regular training schedule.
These findings add to the evidence base for the effectiveness of mindfulness-based programs in reducing perceived stress in caregivers of individuals with ID and ASD. For example, group home staff who received a 7-day intensive MBPBS training reported significantly reduced perceived stress and the group home agency reported zero staff turnover due to stress following training (Singh et al. 2015). In a proof-of-concept study, community group home staff who received training in the 7-day intensive MBPBS program reported significantly reduced perceived stress and staff turnover (Singh, Lancioni, Karazsia, and Myers 2016). In an RCT study, staff in a congregate care facility were randomized into two groups, with one group receiving training in the 7-day intensive MBPBS program and the other in the standard agency training-as-usual program (Singh, Lancioni, Karazsia, and Chan, et al. 2016). Those trained in MBPBS reported significantly greater reduction in perceived psychological stress than those who received the standard agency training. Finally, in another RCT, the effects of training group home staff on the full MBPBS program or the PBS component alone were evaluated on a range of caregiver, client, and agency outcome variables, including perceived stress and professional quality of life of the caregivers (Singh, Lancioni, Medvedev, et al. 2020). Although both MBPBS and PBS were effective, outcomes for participants in the MBPBS condition were significantly and uniformly superior to those in the PBS alone condition. The results clearly showed that training in MBPBS enabled the caregivers to significantly reduce their perceived psychological stress, increase compassion satisfaction, and decrease compassion fatigue. The contribution of the present study is that it provides empirical evidence from an RCT of the central role of mindfulness and related contemplative practices in enhancing the quality of life of professional caregivers.
Meta-analyses of current research attest to the effectiveness of mindfulness-based interventions on stress and mental health in both healthy (Chiesa and Serretti 2009, Khoury et al. 2015) and clinical populations (de Abreu Costa et al. 2019). However, the reviewed research was based on formal 8-week mindfulness-based programs, such as the Mindfulness-Based Stress Reduction program (Kabat-Zinn 1990). What the present study adds is that caregivers can reduce and maintain their stress at nonpathological levels with a 3-day low-threshold practice, which includes a number of contemplative practices that enhance their quality of life. The addition of these contemplative practices to mindfulness programs, as in the present study, constitute what has been called second generation programs (Van Gordon et al. 2015) that not only improve psychological and emotional wellbeing but also enable personal transformation and transcendence.
The present study included contemplative practices such as the four immeasurables, five hindrances, three poisons, and ethical precepts. In practical terms, the four immeasurables (i.e. lovingkindness, compassion, empathetic joy, and equanimity) provide the caregivers foundational grounding in attitudinal and emotional modes of attending to their mental state before they respond to their clients who may be engaging in aggressive and destructive behaviors. Such behaviors might produce negative emotional states in caregivers, who might then respond to the clients with aversive or punishing contingencies. Thus, in this context, lovingkindness meditation could enable them to respond in a more positive or wholesome manner given that this practice has been shown to have a strong effect on negative emotions (Fredrickson et al. 2008, Shonin et al. 2015). Indeed, meta-analyses suggest that lovingkindness practices generally improve health and wellbeing and enhance positive emotions in clinical and non-clinical populations (Galante et al., 2014, Zeng et al. 2015). Caregivers can use other contemplative practices, such as the three poisons, to better understand the difference between skillful and unskillful intentions and reactions when they respond to their clients’ needs. Furthermore, caregivers can check their mental state for the presence of any of the five hindrances (i.e. desire, aversion, sloth and torpor, restlessness and worry, and doubt) that may thwart them from acting mindfully in response to client behavior. When used skillfully, these practices reduce stress and enhance wellbeing in both general and clinical populations.
The field of mindfulness research suffers from many methodological challenges (Van Dam et al. 2018), with one of the key issues being the need for appropriate comparison and control groups (Davidson and Kaszniak 2015). Decisions regarding efficacy or effectiveness of an intervention are usually made when the experimental intervention is assessed against an effective comparison or a control intervention in an RCT. Given the nature of mindfulness programs, participants in the control group invariably know that they are in the control group thus violating the assumption of blindness to their experimental condition. When this happens, it leads to the problem of differential demand characteristics of participants in each condition affecting intervention outcomes. Thus, no-treatment or waitlist control conditions do not provide adequate controls in mindfulness intervention research. One of the key strengths of the present study was the use of a three-arm RCT which included two active experimental groups (with putative equivalent effectiveness) and an accepted inservice training provided by the agency, thus greatly reducing the impact of differential demand characteristics. The use of psychoeducation training as a comparison condition and inservice training-as-usual as a control condition, with nonspecific factors being matched as much as possible across the three conditions, attests to the robustness of the research design used in the present study. Another strength of the study was that the followup data showed maintenance of psychological wellbeing at 32 weeks post-intervention. In effectiveness studies, showing short-term gains are inconsequential because caregivers continuously face stress in their daily interactions with clients. This study showed that with training in mindfulness the caregivers were able to deal with difficult situations without raising their stress level or decreasing their quality of life.
Nonetheless, a limitation of the present study was its reliance on self-reported ordinal rating scales to obtain outcome data, thus potentially involving a common method bias. The fact that we collected data on multiple constructs (i.e. stress, quality of life indicators, symptoms of depression) using multi-item rating scales within the same assessment may have resulted in spurious effects due to the measurement instruments rather than to the constructs being measured. That is, correlations among the items measuring these constructs could be affected by response dependency due to response styles, social desirability, and priming effects which are unrelated to the true correlations among the constructs being measured (Podsakoff et al. 2003). Future research should consider using Rasch analysis to transform ordinal scores into interval-level data that increases precision of ordinal scales while simultaneously reducing measurement error due to response dependency (Medvedev et al. 2017, Medvedev, Krägeloh, et al. 2018, Medvedev, Titkova, et al. 2018). Measuring multiple constructs using multiple methods or instruments can also be considered to enhance both reliability and validity (Bagozzi and Yi 1993). Another limitation is that we measured mindfulness practice only in terms of the time caregivers spent in formal meditation. However, the mindfulness program used in this study emphasized that in addition to formal meditation practice caregivers take advantage of opportunities at work and home to engage in informal practice of mindfulness (e.g. how to nonjudgmentally observe, accept, and let go of negative thoughts that arise when clients or their own children are being aggressive, destructive, or disruptive). These informal daily mindfulness practices may have a direct effect on outcomes and thus need to be measured as well (e.g. through experience sampling methods; Larson and Csikszentmihalyi 2014).
Mindfulness-based programs are typically multi-component by design, including not only formal meditation practices (e.g. Samatha and insight meditations), but also related practices (e.g. body-scan, yoga). Given time constraints for formal meditation practice, evaluating the relative contribution of each major component in a mindfulness-based program may provide useful leads for developing personalized programs that may speak to specific challenges in individuals. MBPBS is a multicomponent mindfulness program that incorporates sitting meditation, contemplative practices, and behavioral techniques. Following earlier studies that examined the comparative effects of the full MBPBS program to the PBS component alone (Singh, Lancioni, Chan, et al. 2020) and the full program, the mindfulness component, and the PBS component (Singh, Lancioni, Medvedev, Hwang, et al. 2020), the present study examined the effects of the mindfulness program by itself. Future research should examine the sub-components of the mindfulness program to assess the relative contributions of the meditation and contemplative practices. Information provided by deconstructing mindfulness-based practices may provide the first steps in developing individualized mindfulness practices.
Disclosure statement
The authors declare no conflict of interest and they do not work for, consult to, and own shares in or receive funding from any company or organization that would benefit from this article.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study
References
- Bagozzi, R. P. and Yi, Y.. 1993. Multitrait-multimethod matrices in consumer research: Critique and new developments. Journal of Consumer Psychology, 2, 143–170. [Google Scholar]
- Beck, A. T., Steer, R. A. and Brown, G. K.. 1996. Beck depression inventory: second edition manual. San Antonio, TX: The Psychological Corporation. [Google Scholar]
- Beck, A. T., Steer, R. A. and Carbin, M. G.. 1988. Psychometric properties of the Beck Depression Inventory: Twenty-five years of evaluation. Clinical Psychology Review, 8, 77–100. [Google Scholar]
- Beighton, C. and Wills, J.. 2019. How parents describe the positive aspects of parenting their child who has intellectual disabilities: A systematic review and narrative synthesis. Journal of Applied Research in Intellectual Disabilities: JARID, 32, 1255–1279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bethay, J. S., Wilson, K. G., Schnetzer, L. W., Nassar, S. L. and Bordieri, M. J.. 2013. A controlled pilot evaluation of acceptance and commitment training for intellectual disability staff. Mindfulness, 4, 113–121. [Google Scholar]
- Biglan, A., Layton, G. L., Backen Jones, L., Hankins, M. and Rusby, J. C.. 2013. The value of workshops on psychological flexibility for early childhood special education staff. Topics in Early Childhood Special Education, 32, 196–210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bluth, K. and Wahler, R. G.. 2011. Does effort matter in mindful parenting? Mindfulness, 2, 175–178. [Google Scholar]
- Brooker, J., Julian, J., Webber, L., Chan, J., Shawyer, F. and Meadows, G.. 2013. Evaluation of an occupational mindfulness program for staff employed in the disability sector in Australia. Mindfulness, 4, 122–136. [Google Scholar]
- Chiesa, A. and Serretti, A.. 2009. Mindfulness-based stress reduction for stress management in healthy people: A review and meta-analysis. Journal of Alternative and Complementary Medicine (New York, N.Y.), 15, 593–600. [DOI] [PubMed] [Google Scholar]
- Cohen, S., Kamarck, T. and Mermelstein, R.. 1983. A global measure of perceived stress. Journal of Health and Social Behavior, 24, 385–396. [PubMed] [Google Scholar]
- Cohen, S. and Williamson, G.. 1988. Psychological stress in a probability sample of the United States. In Spacapan S. & Oskamp S., eds. The social psychology of health: Claremont symposium on applied social psychology. Newbury Park, CA: Sage, pp. 31–63. [Google Scholar]
- Dane, A. V. and Schneider, B. H.. 1998. Program integrity in primary and early secondary prevention: Are implementation effects out of control? Clinical Psychology Review, 18, 23–45. [DOI] [PubMed] [Google Scholar]
- Davidson, R. J. and Kaszniak, A. W.. 2015. Conceptual and methodological issues in research on mindfulness and meditation. The American Psychologist, 70, 581–592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Abreu Costa, M., de Oliveira, G. S. D., Tatton-Ramos, T., Manfro, G. G. and Salum, G. A.. 2019. Anxiety and stress-related disorders and mindfulness-based interventions: A systematic review and multilevel meta-analysis and meta-regression of multiple outcomes. Mindfulness, 10, 996–1005. [Google Scholar]
- Dusenbury, L., Brannigan, R., Falco, M. and Hansen, W. B.. 2003. A review of research on fidelity of implementation: Implications for drug abuse prevention in school settings. Health Education Research Theory & Practice, 18, 237–256. [DOI] [PubMed] [Google Scholar]
- Feagans Gould, L., Dariotis, J. K., Greenberg, M. T. and Mendelson, T.. 2016. Assessing fidelity of implementation (FOI) for school-based mindfulness and yoga interventions: A systematic review. Mindfulness, 7, 5–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fredrickson, B. L., Cohn, M. A., Coffey, K. A., Pek, J. and Finkel, S. M.. 2008. Open hearts build lives: Positive emotions, induced through loving-kindness meditation, build consequential personal resources. Journal of Personality and Social Psychology, 95, 1045–1062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galante, J., Galante, I., Bekkers, M.-J. and Gallacher, J.. 2014. Effect of kindness-based meditation on health and well-being: A systematic review and meta-analysis. Journal of Consulting and Clinical Psychology, 82, 1101–1114. [DOI] [PubMed] [Google Scholar]
- Gardner, B., Rose, J., Mason, O., Tyler, P. and Cushway, D.. 2005. Cognitive therapy and behavioural coping in the management of work-related stress: An intervention study. Work & Stress, 19, 137–152. [Google Scholar]
- Hastings, R. P. and Horne, S.. 2004. Positive perceptions held by support staff in community mental retardation services. American Journal on Mental Retardation, 109, 53–62. [DOI] [PubMed] [Google Scholar]
- Hatton, C., Emerson, E., Rivers, M., Mason, H., Mason, L., Swarbrick, R., Kiernan, C., Reeves, D. and Alborz, A.. 1999. Factors associated with staff stress and work satisfaction in services for people with intellectual disability. Journal of Intellectual Disability Research, 43, 253–267. [DOI] [PubMed] [Google Scholar]
- Hensel, J. M., Lunsky, Y. and Dewa, C. S.. 2012. Exposure to client aggression and burnout among community staff who support adults with intellectual disabilities in Ontario, Canada. Journal of Intellectual Disability Research : Jidr, 56, 910–915. [DOI] [PubMed] [Google Scholar]
- Hwang, Y.-S. and Singh, N. N.. 2016. Mindfulness. In Singh N. N., ed. Handbook of evidence-based practices in intellectual and developmental disabilities. New York, NY: Springer, pp. 311–346. [Google Scholar]
- Iadarola, S., Levato, L., Harrison, B., Smith, T., Lecavalier, L., Johnson, C., Swiezy, N., Bearss, K. and Scahill, L.. 2018. Teaching parents behavioral strategies for autism spectrum disorder (ASD): Effects on stress, strain, and competence. Journal of Autism and Developmental Disorders, 48, 1031–1041. [DOI] [PubMed] [Google Scholar]
- Innstrand, S. T., Espnes, G. A. and Mykletun, R.. 2004. Job stress, burnout, and job satisfaction: An intervention study for staff working with people with intellectual disabilities. Journal of Applied Research in Intellectual Disabilities, 17, 119–126. [Google Scholar]
- Kabat-Zinn, J. 1990. Full catastrophe living: Using the wisdom of your body and mind to face stress, pain, and illness. New York: Delta [Google Scholar]
- Khoury, B., Sharma, M., Rush, S. E. and Fournier, C.. 2015. Mindfulness-based stress reduction for healthy individuals: A meta-analysis. Journal of Psychosomatic Research, 78, 519–528. [DOI] [PubMed] [Google Scholar]
- Korsitas, S., Iacano, T., Carling-Jenkins, R. and Chan, J.. 2010. Exposure to challenging behaviour and support worker/house supervisor wellbeing. Melbourne: The Centre for Developmental Disability Health Victoria. [Google Scholar]
- Larson, R. L. and Csikszentmihalyi, M.. 2014. The experience sampling method. In Csikszentmihalyi M., Flow and the foundations of positive psychology. New York: Springer, pp. 21–34. [Google Scholar]
- McConachie, D. A. J., McKenzie, K., Morris, P. G. and Walley, R. M.. 2014. Acceptance and mindfulness-based stress management for support staff caring for individuals with intellectual disabilities. Research in Developmental Disabilities, 35, 1216–1227. [DOI] [PubMed] [Google Scholar]
- Medvedev, O. N., Krägeloh, C. U., Titkova, E. A. and Siegert, J. R.. 2018. Rasch analysis and ordinal-to-interval conversion tables for the depression, anxiety and stress scale. Journal of Health Psychology, 25, 1374–1383. [DOI] [PubMed] [Google Scholar]
- Medvedev, O. N., Siegert, R. J., Kersten, P. and Krägeloh, C. U.. 2017. Improving the precision of the Five Facet Mindfulness Questionnaire using a Rasch approach. Mindfulness, 8, 995–1008. [Google Scholar]
- Medvedev, O. N., Titkova, E. A., Siegert, R. J., Hwang, Y.-S. and Krägeloh, C. U.. 2018. Evaluating short versions of the Five Facet Mindfulness Questionnaire using Rasch analysis. Mindfulness, 9, 1411–1422. [Google Scholar]
- Muthén, B. and Kaplan, D.. 1985. A comparison of some methodologies for the factor analysis of non-normal Likert variables. British Journal of Mathematical and Statistical Psychology, 38, 171–189. [Google Scholar]
- Mutkins, E., Brown, R. F. and Thorsteinsson, E. B.. 2011. Stress, depression, workplace supports and burnout in intellectual disability support staff. Journal of Intellectual Disability Research, 55, 500–510. [DOI] [PubMed] [Google Scholar]
- Myers, R. E., Winton, A. S. W., Lancioni, G. E. and Singh, N. N.. 2014. Mindfulness in developmental disabilities. In: Singh N. N., ed. Psychology of meditation. New York: Nova Science, pp. 209–240. [Google Scholar]
- Noone, S. J. and Hastings, R. P.. 2009. Building psychological resilience in support staff caring for people with intellectual disabilities: pilot evaluation of an acceptance-based intervention. Journal of Intellectual Disabilities : Joid, 13, 43–53. [DOI] [PubMed] [Google Scholar]
- Noone, S. J. and Hastings, R. P.. 2010. Using acceptance and mindfulness-based workshops with support staff caring for adults with intellectual disabilities. Mindfulness, 1, 67–73. [Google Scholar]
- Podsakoff, P.M., MacKenzie, S.B., Lee, J.Y. and Podsakoff, N.P.. 2003. Common method biases in behavioral research: A critical review of the literature and recommended remedies. The Journal of Applied Psychology, 88, 879–903. [DOI] [PubMed] [Google Scholar]
- Rose, J., Jones, F. and Fletcher, C. B.. 1998. The impact of a stress management programme on staff well-being and performance at work. Work & Stress, 12, 112–124. [Google Scholar]
- Rose, J., Madurai, T., Thomas, K., Duffy, B. and Oyebode, J.. 2010. Reciprocity and burnout in direct care staff. Clinical Psychology & Psychotherapy, 17, 455–462. [DOI] [PubMed] [Google Scholar]
- Sameroff, A. J. 1995. General systems theories and developmental psychopathology. In Cicchetti D. & Cohen D. J., eds. Developmental psychopathology: Theory and methods. New York, NY: Wiley, pp. 659–695. [Google Scholar]
- Shonin, E., Van Gordon, W., Compare, A., Zangeneh, M. and Griffiths, M. D.. 2015. Buddhist-derived lovingkindness and compassion meditation for the treatment of psychopathology: A systematic review. Mindfulness, 6, 1161–1180. [Google Scholar]
- Singh, N. N., Lancioni, G. E., Chan, J., McPherson, C. L. and Jackman, M. M.. 2020. Mindfulness-Based Positive Behavior Support. In Ivtzan I., ed. Handbook of mindfulness-based programs: Mindfulness interventions from education to health and therapy. London, UK: Routledge, pp. 42–52. [Google Scholar]
- Singh, N. N., Lancioni, G. E., Karazsia, B. T., Myers, R. E., Winton, A. S. W., Latham, L. L. and Nugent, K.. 2015. Effects of training staff in MBPBS on the use of physical restraints, staff stress and turnover, staff and peer injuries, and cost effectiveness in developmental disabilities. Mindfulness, 6, 926–937. [Google Scholar]
- Singh, N. N., Lancioni, G. E., Karazsia, B. T. and Myers, R. E.. 2016. Caregiver training in Mindfulness-Based Positive Behavior Supports (MBPBS): Effects on Caregivers and Adults with Intellectual and Developmental Disabilities. Frontiers in Psychology, 7, 98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh, N. N., Lancioni, G. E., Karazsia, B. T., Chan, J. and Winton, A. S. W.. 2016. Effectiveness of caregiver training in mindfulness-based positive behavior support (MBPBS) vs. training-as-usual (TAU): A randomized controlled Trial. Frontiers in Psychology, 7, 1549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh, N. N., Lancioni, G. E., Medvedev, O. N., Hwang, Y.-S. and Myers, R. E.. 2020. A component analysis of the Mindfulness-Based Positive Behavior Support (MBPBS) program for mindful parenting by mothers of children with autism spectrum disorder. Mindfulness, 12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh, N. N., Lancioni, G. E., Medvedev, O. N., Myers, R. E., Chan, J., McPherson, C. L., Jackman, M. M. and Kim, E.. 2020. Comparative effectiveness of caregiver training in Mindfulness-Based Positive Behavior Support (MBPBS) and Positive Behavior Support (PBS) in a randomized controlled trial. Mindfulness, 11, 99–111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skirrow, P. and Hatton, C.. 2007. Burnout amongst direct care workers in services for adults with intellectual disabilities: A systematic review of research findings and initial normative data. Journal of Applied Research in Intellectual Disabilities, 20, 131–144. [Google Scholar]
- Smith, T. and Iadarola, S.. 2015. Evidence Base Update for Autism Spectrum Disorder . J Clin Child Adolesc Psychol, 44, 897–922. [DOI] [PubMed] [Google Scholar]
- Stamm, B. H. 2010. The concise ProQOL manual. 2nd ed. Pocatello, ID: ProQOL.org. [Google Scholar]
- Van Dam, N. T., van Vugt, M. K., Vago, D. R., Schmalzl, L., Saron, C. D., Olendzki, A., Meissner, T., Lazar, S. W., Kerr, C. E., Gorchov, J., Fox, K. C. R., Field, B. A., Britton, W. B., Brefczynski-Lewis, J. A. and Meyer, D. E.. 2018. Mind the hype: A critical evaluation and prescriptive agenda for research on mindfulness and meditation. Perspectives on Psychological Science: A Journal of the Association for Psychological Science, 13, 36–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Gordon, W., Shonin, E. and Griffiths, M.. 2015. Towards a second generation of mindfulness-based interventions. The Australian and New Zealand Journal of Psychiatry, 49, 591–592. [DOI] [PubMed] [Google Scholar]
- Yu, Y., McGrew, J. H. and Boloor, J.. 2019. Effects of caregiver-focused programs on psychosocial outcomes in caregivers of individuals with ASD: A meta-analysis. Journal of Autism and Developmental Disorders, 49, 4761–4779. [DOI] [PubMed] [Google Scholar]
- Zeng, X., Chiu, C. P. K., Wang, R., Oei, T. P. S. and Leung, F. Y. K.. 2015. The effect of loving-kindness meditation on positive emotions: A meta-analytic review. Frontiers in Psychology, 6, 1693. [DOI] [PMC free article] [PubMed] [Google Scholar]