Abstract
Affect intolerance/sensitivity, defined as one’s sensitivity to, or inability to tolerate, affective states, is a transdiagnostic process implicated in the development and maintenance of numerous forms of psychopathology. Mindfulness and acceptance interventions are posited to improve affect intolerance/sensitivity; however, there has been no quantitative synthesis of this research to date. Seven electronic databases were searched up until November 2018. Hedges’ g values, 95% confidence intervals, p-values, and Q-values were calculated for a series of random-effects models. Twenty-five studies (pooled N = 1,778) met eligibility criteria and were included in the qualitative synthesis (n = 22 included in the meta-analysis). There was a small, significant effect of mindfulness and acceptance interventions on improving affect intolerance/sensitivity from pre- to post-intervention (Hedges’ g = −.37, 95% CI = −.52 to −.23, p <.001), with effects maintained up to 6-months (Hedges’ g = −.35, 95% CI = −.61 to −.09, p < .01). There was a significantly larger effect for studies with inactive compared to active controls. No significant effect size differences were found for intervention length (< 8 vs. ≥ 8 sessions), intervention type (mindfulness vs. acceptance) or sample type (clinical vs. non-clinical). Mindfulness and acceptance interventions modestly improve affect intolerance/sensitivity.
Keywords: mindfulness, acceptance, affect intolerance, affect sensitivity, meta-analysis
Introduction
Epidemiological studies have consistently demonstrated high rates of comorbidity across psychological disorders (e.g., Brown, Campbell, Lehman, Grisham, & Mancill, 2001; Kessler et al., 2003; Kessler, Chiu, Demler, Merikangas, & Walters, 2005). There is strong empirical evidence that this overlap is due to core etiological processes that cut across diagnostic categories (Barlow, 2004; Brown & Barlow, 2009; Brown, Chorpita, & Barlow, 1998; Wilamowska et al., 2010). Recent research has focused on parsimoniously treating psychopathology through interventions that target these underlying processes, rather than interventions that target disorder-specific symptoms (Farchione et al., 2012; Hayes & Hofmann, 2019).
One transdiagnostic process that has received considerable empirical attention is affect intolerance/sensitivity. Affect intolerance/sensitivity is a high-level construct that broadly captures one’s sensitivity to (i.e., fear of), or inability to withstand, aversive affective states (Bernstein, Zvolensky, Vujanovic, & Moos, 2009; Leyro, Zvolensky, & Bernstein, 2010; Schmidt, Mitchell, Keough, & Riccardi, 2010). Although more research is needed, factor analytic results suggest that measures of affect intolerance (i.e., distress intolerance, intolerance of uncertainty) and sensitivity (i.e., anxiety sensitivity) may share a common higher-order affect intolerance/sensitivity dimension and may be related to one another as lower-order facets of this higher-order construct (Allan et al., 2018; Allan, Macatee, Norr, Raines, & Schmidt, 2015; Bardeen et al., 2013; Bernstein et al., 2009; Hong & Cheung, 2015; McHugh & Otto, 2012). Affect intolerance/sensitivity is a cognitive-affective individual difference factor, which is empirically distinct from the tendency to experience negative emotional states (McNally, 2002), that serves to amplify emotional responding. In addition, individuals who perceive an emotion as intolerable are more likely to use maladaptive emotion regulation strategies to escape or avoid the emotion, which then serves to maintain or amplify negative emotional states in both the short- and long-term (Leyro et al., 2011; Simon & Gaher, 2005; Jeffries, McLeish, Kraemer, Avallone, & Felming, 2016). As a result, affect intolerance/sensitivity is concurrently and prospectively associated with a wide-range of emotional problems (see Leyro et al., 2011 for a review).
The most commonly studied forms of affect intolerance/sensitivity include distress tolerance, intolerance of uncertainty, and anxiety sensitivity. Distress tolerance (DT) is conceptualized as the ability to withstand broad-based negative emotional states (Simons & Gaher, 2005). Lower levels of DT (i.e., distress intolerance) are linked with higher anxiety and depressive symptoms, eating psychopathology, and substance misuse (Leyro et al., 2011). Intolerance of uncertainty (IU) is a predisposition that captures the inability to tolerate the emotional reactions related to perceived uncertainty (Carleton, 2016). IU has been primarily linked with the development and maintenance of anxiety and other forms of psychopathology and negative health behaviors (e.g., depression; Gentes & Ruscio, 2011; Kraemer, McLeish, & O’Bryan, 2015; McEnvoy et al., 2019). Anxiety sensitivity (AS), defined as the fear of arousal-related sensations due to the perceived negative consequences of those sensations, is a cognitive vulnerability factor that is prospectively and concurrently associated with anxiety psychopathology, depressive symptoms, and negative health behaviors (McNally, 2002; Naragon-Gainey, 2010). Other affect intolerance and sensitivity factors, such as fear of emotions (i.e., Williams, Chambless, & Ahrens, 1997) and disgust sensitivity (i.e., Olatunji & McKay, 2007), have also been shown to be associated with various forms of psychopathology (e.g., Cisler, Olatunji, & Lohr, 2009; Sauer-Zavala et al., 2012). Though generally conceptualized as trait-like, affect intolerance/sensitivity factors are considered malleable processes that can be modified through intervention efforts (e.g., Norr, Allan, Macatee, Keough, & Schmidt, 2014).
Mindfulness- and acceptance-based interventions are posited to improve affect intolerance/sensitivity (e.g., Farb, Anderson, & Segal, 2012; Roemer, Williston, & Rollins, 2015). Mindfulness and acceptance interventions use similar and different techniques to affect emotional and behavioral change through the same theoretical framework: that efforts to change, escape, or avoid uncomfortable internal experiences, rather than the content of the internal experiences themselves, are the key processes contributing to the development, exacerbation, and maintenance of psychopathology (Brown et al., 2007; Hayes et al., 2004). As such, mindfulness- and acceptance-based interventions aim to change one’s relationship to uncomfortable internal experiences by promoting acceptance, non-reactivity, and cognitive de-centering (i.e., the ability to step back to view thoughts as passing mental events; e.g., Hoge et al., 2015; Holzel et al., 2011; Lindsay & Creswell, 2017; Sauer & Baer, 2010; Stockton et al., 2019; Villatte et al., 2016). Both approaches use brief mindfulness practices (e.g., awareness of the breath) and acceptance interventions also use metaphors to facilitate acceptance, nonreactivity, and decentering. With these skills, individuals are better positioned to flexibly and adaptively respond to uncomfortable internal states rather than automatically avoid them (i.e., affect intolerance) or become overwhelmed by them (i.e., affect sensitivity; Keng et al., 2011). Mindfulness and acceptance interventions differ from traditional CBT, which focuses primarily on changing the form or content of internal experiences (e.g., cognitive restructuring, relaxation; Hayes 2004; Luberto et al., 2020). The mindfulness- and acceptance-based interventions that have received the most empirical attention include Acceptance and Commitment Therapy (ACT; Hayes, Pistorello, & Levin, 2012), Mindfulness-Based Cognitive Therapy (MBCT; Segal & Teasdale, 2018), Mindfulness-Based Stress Reduction (MBSR; Kabat-Zinn, 1982), and Dialectical Behavior Therapy (DBT; Linehan, 1993).
Mindfulness- and acceptance-based interventions may improve affect intolerance/sensitivity through nonreactivity, acceptance, and decentering. First, non-reactivity in the presence of uncomfortable emotions may improve one’s ability to tolerate uncomfortable affective states, or reduce their fear of emotions, through exposure and related learning (Treanor, 2011). Instead of automatically engaging in habitual emotional responses that perpetuate emotional problems (e.g., avoidance, suppression), individuals are taught to “stick with” an emotion in the present moment, which generates new learning about emotions (e.g., “I can handle emotions”) and reduces fear of emotional reactions (e.g., aversive body sensations). Over time, individuals may become more willing to experience uncomfortable affective states without engaging in efforts to eliminate them. Second, judgmental (e.g., “I shouldn’t be feeling this way”) or negative (e.g., believing you are going to have a heart attack in response to anxiety symptoms) reactions to emotions increase emotional arousal and contribute to the perceived intolerability of the emotion (e.g., Barlow et al., 2017; Hayes et al., 1996). Mindfulness and acceptance interventions counter this process by helping individuals adopt a nonjudgmental (i.e., accepting) stance towards emotional experiences (Lindsay & Creswell, 2017; Stockton et al., 2019). Lastly, over identifying with emotion-related internal stimuli (e.g., thoughts) heightens the emotion and makes it feel unmanageable (Bernstein et al., 2016). Mindfulness and acceptance interventions teach individuals how to take a step back from (i.e., decenter) internal experiences, resulting in greater ability to manage them without engaging in habitual ways of responding (Sauer & Baer, 2010).
Despite the theoretical link between mindfulness and acceptance-based interventions and affect intolerance/sensitivity, there has been no systematic review of this literature, to date. Indeed, although a large body of literature supports the efficacy of these interventions for treating psychological problems (e.g., Hofmann et al., 2010), the effects of these interventions on the affect intolerance/sensitivity factors that underlie psychological problems have not been synthesized. In line with previous meta-analyses in this area (e.g., Cramer et al., 2016; Veehof, Trompetter, Bohlmeijer, & Schreurs, 2016; Vollestad, Nielsen, & Nielsen, 2012), we included both mindfulness and acceptance interventions. We argue that evidence of shared theoretical underpinnings, core mechanistic processes, and therapeutic goals provide sufficient justification for a shared meta-analysis (Baer & Krietemeyer, 2006; Hayes, 2004; Hayes, Follette, & Linehan, 2004; Roemer, Erisman, & Orsillo, 2008). Therefore, the aim of the current study is to conduct a systematic review and meta-analysis of randomized controlled trials examining the effects of mindfulness- and acceptance-based interventions on affect intolerance/sensitivity. Specifically, the present study aims to: 1) systematically review and synthesize the existing research on mindfulness and acceptance interventions for affect intolerance/sensitivity; 2) estimate the pooled, overall effect size of these results; 3) estimate domain-specific effect sizes for each affect intolerance/sensitivity domain, when applicable; 4) examine potential effect modifiers (including subgroup analyses to account for potential differences between mindfulness and acceptance interventions); and 5) identify avenues for future research in this area. It was hypothesized that mindfulness and acceptance interventions, relative to controls, would significantly improve affect intolerance/sensitivity.
Method
Literature Search
A literature search was conducted with assistance from a medical librarian in Pubmed/MEDLINE, PsycINFO, PsycArticles, CINAHL, Cochrane Database of Systematic Reviews, Embase, and Web of Science up until November 2018. Specific affect intolerance/sensitivity search terms were extracted from the most recent literature review of distress tolerance (e.g., distress tolerance, intolerance of uncertainty, frustration tolerance, tolerance of ambiguity; Leyro et al., 2010) as well as other empirical studies in this area (e.g., anxiety sensitivity, fear of emotions, disgust sensitivity; Bernstein et al., 2009; Olatunji et al., 2007; Williams et al., 1997). We also included search terms related to the behavioral capacity to tolerate aversive emotions (e.g., task persistence, mirror tracing persistence task; Leyro et al., 2010). Given significant heterogeneity in the terminology used to index affect intolerance/sensitivity across studies (Leyro et al., 2011), we also included broad search terms related to emotional vulnerability (e.g., emotion regulation) to effectively capture all relevant studies. Mindfulness and acceptance search terms included a combination of broad (e.g., mindfulness) and intervention-specific terms (e.g., MBCT, MBSR, DBT, ACT). Publication dates were not limited. See the Appendix A for the full search strategy in MEDLINE.
Eligibility Criteria
Inclusion and exclusion criteria were specified in advance via a study protocol. Randomized controlled trials of mindfulness- and acceptance-based interventions that assessed at least one affect intolerance/sensitivity outcome were eligible for inclusion. Studies with adults (i.e., ≥18 years of age), across any population or clinical condition, were eligible for inclusion. Unpublished manuscripts, conference presentations, and dissertations were excluded. Non-English manuscripts were excluded.
Mindfulness- and acceptance-based interventions.
In order to be eligible, mindfulness- and acceptance-based interventions must have included at least one session of formal didactic and experiential training in building mindfulness or acceptance skills as part of a skills-training intervention. Although intervention-specific search terms of the most common mindfulness and acceptance interventions were used (e.g., MBCT, MBSR, ACT), any mindfulness or acceptance intervention that met the above criteria were eligible for inclusion. Studies that included an experimental manipulation or acute mindfulness or acceptance induction were excluded. In addition, studies that included traditional cognitive behavioral therapy (CBT) only, without mindfulness or acceptance training, were excluded. Movement-based mind-body interventions (e.g., yoga, tai chi) were also excluded. Both individual and group delivered interventions were eligible for inclusion.
Affect intolerance/sensitivity.
Affect intolerance/sensitivity was operationalized based on the existing empirical literature, which suggests that it is a common higher-order factor that explains the covariance between several lower-order affect intolerance and sensitivity facets (Allan et al., 2015; Bardeen et al., 2013; Bernstein et al., 2009; Hong & Cheung, 2015; McHugh & Otto, 2012). We included outcomes that assessed both the perceived (measured via self-report) and behavioral (measured via task persistence) capacity to tolerate aversive emotional states. Outcomes that did not exclusively assess affect intolerance or sensitivity (e.g., physical distress tolerance, pain tolerance) were excluded.
Data Extraction and Synthesis
Two independent reviewers (KMK, CMLKMK) extracted data from each study following Cochrane guidelines (Higgins & Green, 2011). Data were reported using Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (Moher, Liberati, Tezlaff, & Altman, 2009). Discrepancies were recorded and resolved through discussion with a third reviewer (DLH). The following data were extracted from each study: study sample, including presenting problem; intervention type, format (individual vs. group) and dose; comparison group type (i.e., active comparison and inactive control) and format; affect intolerance and sensitivity outcomes and timepoints; results for effects on affect intolerance and sensitivity. Quantitative data for meta-analysis (i.e., mean and standard deviation of the pre-intervention, post-intervention, and follow-up for each group) were extracted by one reviewer (KMK) and independently verified by a second reviewer (CML). When available, we extracted means and standard deviations of affect intolerance/sensitivity subscale measures and computed an aggregate effect size. When multiple affect intolerance/sensitivity outcomes were reported in one study or across multiple publications for the same study, an aggregate effect size was computed.
Risk of Bias Assessment
Two independent reviewers (KMK, CML) evaluated risk of bias according to Cochrane Collaboration guidelines (Higgins & Green, 2011). Each of the following domains were rated as high, low, or unclear: random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessors, incomplete data, selective reporting, baseline imbalance and differential attrition. Reviewers provided a justification for their rating, which was used to resolve discrepancies and reach a consensus rating. Studies with a high risk of bias rating on more than one domain were considered “high risk.”
Meta-Analysis
Hedges’ g values, 95% confidence intervals, p-values, and Q-values were calculated for a series of models using Comprehensive Meta-Analysis (Version 3; Bornstein et al., 2014). Effect sizes were calculated using pre-to-post changes in mean using the following formula:
First, for the primary model, an overall pre- to post-intervention pooled effect size was calculated. Second, as a preliminary test of maintenance effects, we estimated the effect size from baseline up to a 6-month follow-up period among studies with follow-up periods. Third, separate domain-specific effect sizes were estimated for each affect intolerance/sensitivity domain (e.g., anxiety sensitivity, distress tolerance), when appropriate (i.e., ≥ 5 studies per domain).
We conducted exploratory subgroup analyses to examine several modifiers of the pooled, overall effect: (1) comparison group (i.e., inactive vs. active); (2) intervention length (i.e., < 8 sessions vs. ≥ 8 sessions); (3) intervention type (i.e., mindfulness- vs. acceptance-based interventions); and (4) study population (i.e., clinical vs. non-clinical). Comparison groups were coded as active if they included any activity and were coded as inactive if they included no treatment, waitlist, or treatment as usual (i.e., continuing services already provided to participants as part of their standard care; Malouf et al., 2017; Morton, Snowdon, Gopold, & Guymer, 2012). Standard mindfulness and acceptance interventions are typically 8 or more sessions. Given the proliferation of brief mindfulness and acceptance interventions (e.g., Schumer et al., 2018), we aimed to examine whether there were differential effects for standard vs. brief treatments. Therefore, intervention length was coded as < 8 sessions (i.e., brief) vs. ≥ 8 sessions (i.e., standard). Intervention type was coded as mindfulness-based if it included MBCT, MBSR, DBT, or was adapted from those interventions and as acceptance-based if it included ACT or was adapted from ACT. For interventions that included a combination of MBSR, MBCT, DBT, or ACT, they were coded based on how they were described in the study (i.e., “mindfulness-based” or “acceptance-based”). Study population was coded as clinical if the sample had a physical or mental health diagnosis or elevated psychological symptoms. All other study populations were coded as non-clinical.
We selected to use random-effects models on an a priori basis due to the heterogeneity in study populations, interventions, and outcome measures. For studies with three groups, we selected a strategy based on the appropriateness of combining groups, based on Cochrane guidelines (Higgins & Green, 2011). For the two studies that included multiple comparisons, we combined relevant intervention groups for a single comparison when possible (Dixon et al., 2015), or conducted two comparisons adjusting the sample size to N/2 to avoid overestimation of effects (Lanza et al., 2014). We examined heterogeneity of the included studies using the I2 statistic. Funnel plots were generated to assess publication bias and a fail-safe N was calculated to determine the number of studies with null effects needed to produce a non-significant pooled effect size. Subgroup comparisons were evaluated using the Q-value statistic. We conducted sensitivity analyses, excluding outlier studies that fell outside of the funnel plot. When applicable, we contacted authors to obtain missing data.
Results
Literature Search
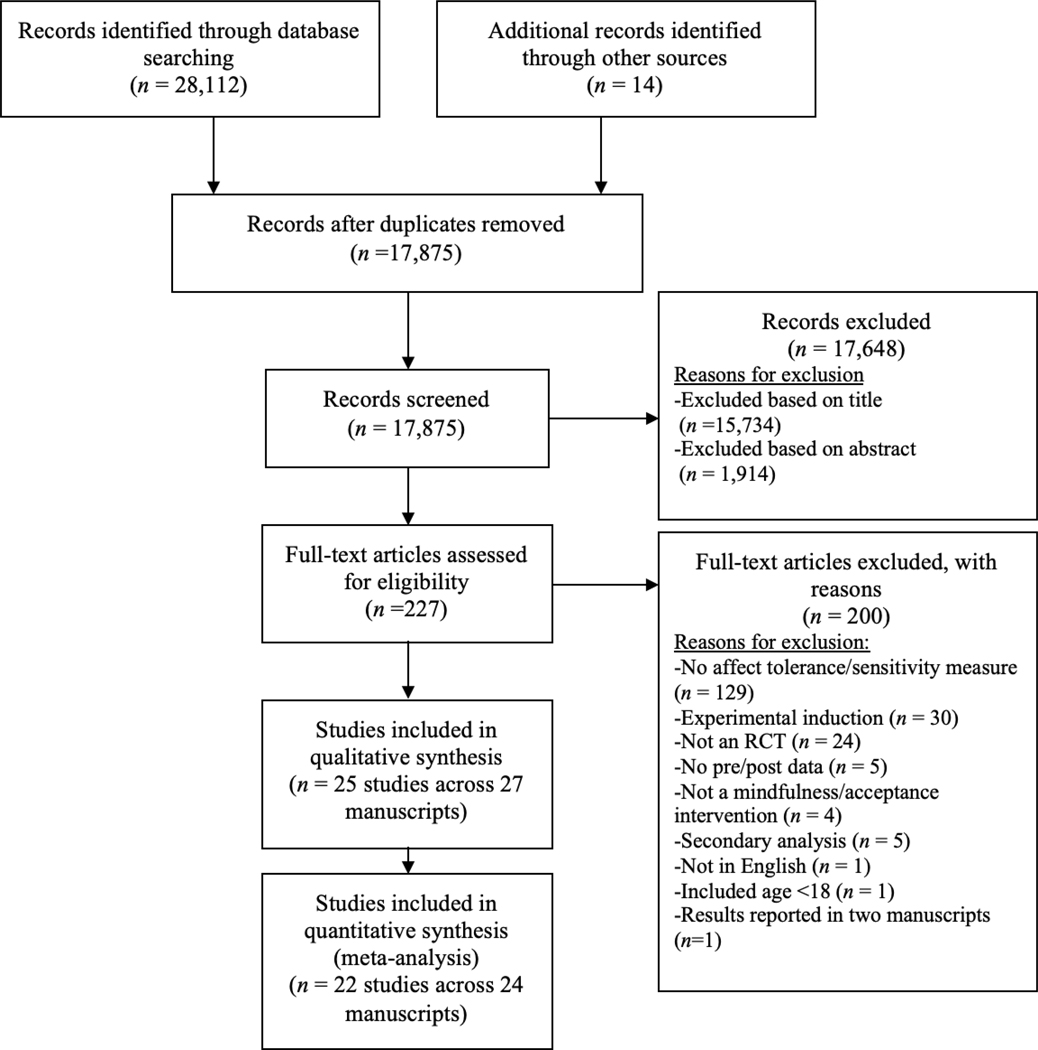
The search strategy yielded 28,126 results (Figure 1). After removing duplicates (n = 10,251), 17,875 titles and abstracts were screened. A total of 15,734 records were excluded based on irrelevant title and 1,914 were excluded after abstract review, leaving 227 full-text articles that were assessed for eligibility. The most common reason for exclusion was the lack of an affect intolerance or sensitivity outcome measure (n = 129). In total, 25 unique studies met our eligibility criteria and were included in the qualitative synthesis. Two studies reported pre-intervention, post-intervention, and follow-up results across two manuscripts (Gonzalez-Menendez, Fernandez, Rodriguez, & Villagra, 2014; Lanza, Garcia, Lamelas, Gonzalez-Menendez, 2014; Lotan, Tanay, & Berstein, 2013; Tanay, Lotan, & Bernstein, 2012).
Figure 1.
PRISMA Flow Diagram
Note. Two studies were excluded from the meta-analysis due to unavailable data in the manuscript and an inability to contact authors to obtain it. One study was excluded for only including a behavioral outcome.
Sample Characteristics
In the 25 included studies, the pooled sample size was N = 1,778 (range 19–503). Samples included individuals with anxiety disorders or elevated anxiety symptoms (k = 8), healthy and unselected samples (k = 4), individuals with medical conditions (k = 4), individuals with borderline personality disorder (BPD) or elevated BPD symptoms (k = 3), other psychological disorders or symptoms (k = 3), treatment seeking undergraduate students (k = 1), incarcerated males (k = 1), and incarcerated women with substance use disorders (k = 1).
Interventions Characteristics
Most studies included adapted versions of ACT (k = 8), traditional or adapted MBSR (k = 6), and DBT skills training (k = 5). The remaining studies included other mindfulness-based interventions (k = 3), MBCT (k = 1), acceptance-based behavior therapy (k =1), or acceptance-based exposure therapy (k = 1). The total number of sessions within each intervention was highly variable across studies, ranging from 1 – 20 sessions (median and mode = 8). Session length was also variable, ranging from 60 – 150 minutes (median and mode = 120 minutes). Most interventions were delivered in a group format (k = 18), with the remaining interventions delivered in an individual format (k = 5) or a self-guided, bibliotherapy format (k = 2).
Comparison Group Characteristics
Most studies included an inactive control (k = 15), such as a waitlist or no-treatment. Active comparisons (k = 10) typically included cognitive-behavioral therapy, support groups, or other forms of psychotherapy. One study supplied control group participants with a book describing mindfulness skills (Victorson et al., 2017).
Outcome Measures
Affect intolerance/sensitivity was typically assessed via self-report (k = 24). Two studies assessed the outcome via behavioral measure (one study assessed both self-report and behavioral outcomes). Self-report outcomes included anxiety sensitivity (k = 9), distress tolerance (k = 7), intolerance of uncertainty (k = 4), fear of emotions (k = 4), disgust sensitivity (k = 1), and visceral sensitivity (k = 1). Behavioral measures included the mirror tracing persistence task (k = 1) and persistence on a speech task (i.e., duration [in seconds] one is able to persist on a distressing speech; k = 1).
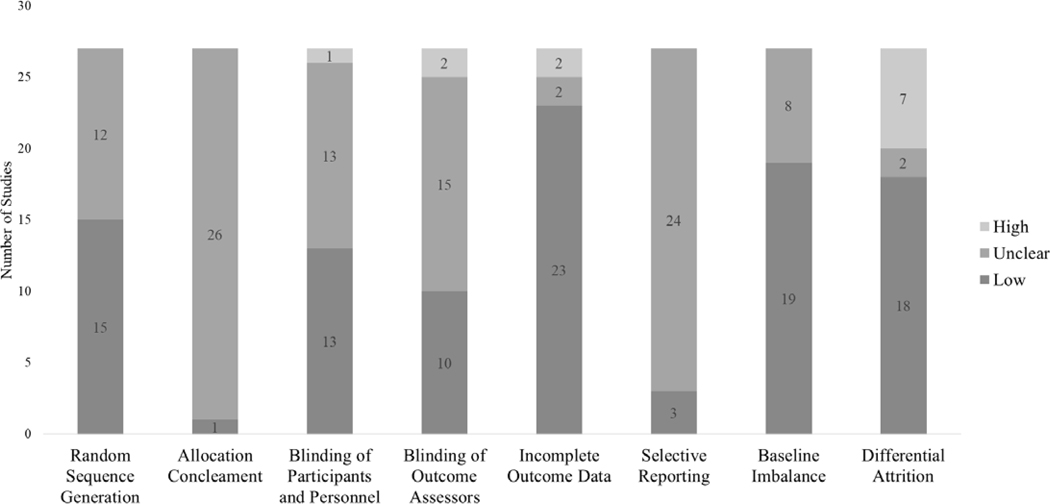
Risk of Bias
Risk of bias is summarized in Figure 2 (also see Appendix B). Overall, risk of bias was low or unclear across most studies. All studies had at least one risk of bias domain rated as unclear. Only one study was considered “high risk” (i.e., more than one rating of high risk across domains; Hazlett-Stevens & Oren, 2017), 10 studies had one rating of high risk, and 16 studies had no ratings of high risk. In general, studies showed lower or unclear risk of bias for random sequence generation, allocation concealment, selective reporting, and baseline imbalance. Potential sources of bias included differential attrition (7 high risk), incomplete outcome data (2 high risk), blinding of outcome assessors (2 high risk), and blinding of participants and personnel (1 high risk).
Figure 2.
Risk of Bias across Studies
Meta-Analyses
Primary Analyses
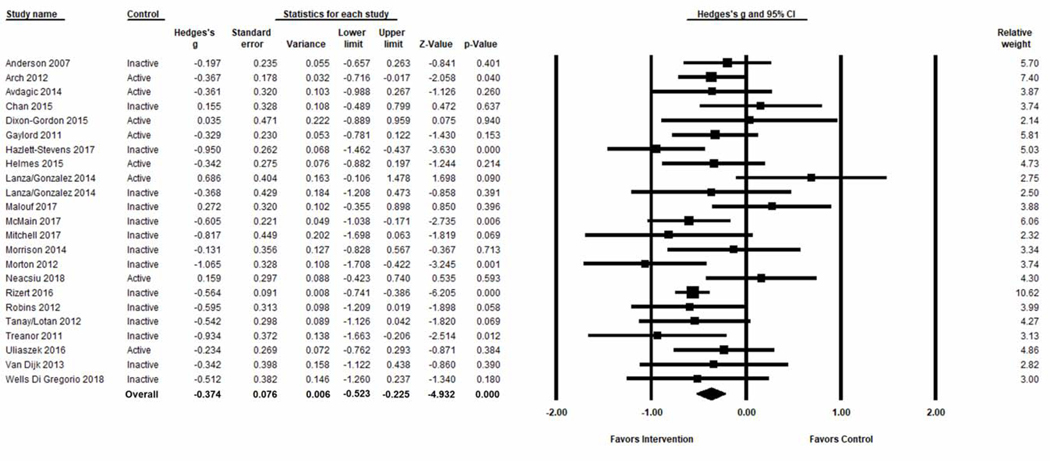
Two studies were not included in the meta-analysis because we were unable to extract data or contact study authors (Gloster et al., 2015; Victorson et al., 2017). Further, only two studies assessed affect intolerance/sensitivity with a behavioral measure (Dixon-Gordon et al., 2015; England et al., 2012), precluding our ability to separately examine effects for behavioral outcomes. Therefore, to reduce statistical heterogeneity, behavioral outcomes were excluded from the meta-analysis. In total, 22 unique studies were included in the meta-analysis. There were two studies (Lanza et al., 2014; Malouf et al., 2017) with unusually robust effects that fell outside the funnel plot (see Appendix C). We report sensitivity analyses, excluding these studies, alongside main analyses below.
Results from pre- to post-intervention are presented in Figure 3. There was significant heterogeneity across studies (I2 = 40.23), supporting the use of random effects models. Overall, there was a small, statistically significant pooled effect of mindfulness and acceptance interventions on improving affect intolerance/sensitivity from pre- to post-intervention (Hedges’ g = −.37, 95% CI = −.52 to −.23, p <.001). The funnel plot (see Appendix C) was mostly symmetric and the classic failsafe N suggested that 231 studies with missing null findings would be needed to create a non-significant result (p > .05). When two studies were excluded in sensitivity analyses, there was a similar but larger pooled effect from pre- to post-intervention (Hedges’ g = −.44, 95% CI = −.57 to −.32, p <.001).
Figure 3.
Pooled effects on affect intolerance and sensitivity from pre-intervention to post-intervention
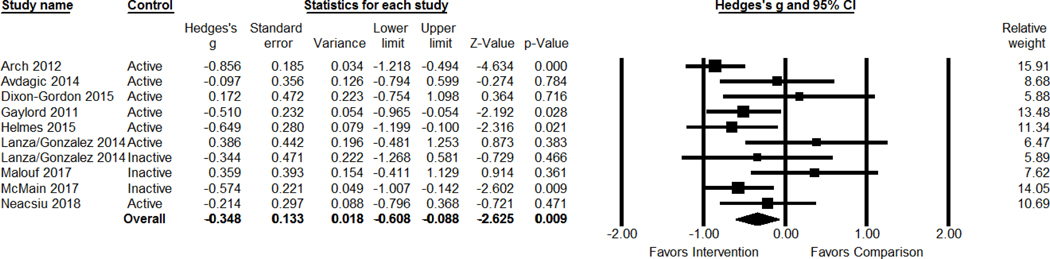
Results from pre-intervention up to the 6-month follow-up are presented in Figure 4. The length of the follow-up periods ranged from 1 to 6 months. There was significant heterogeneity across studies (I2 = 46.87). There was a small, statistically significant pooled effect of mindfulness and acceptance interventions on affect intolerance/sensitivity from pre-intervention up to the 6-month follow-up (Hedges’ g = −.35, 95% CI = −.61 to −.09, p < .01). In the sensitivity analysis with two studies removed, there was again a similar, yet larger, moderate effect from pre-intervention up to the 6-month follow-up (Hedges’ g = −.51, 95% CI = −.72 to −.30, p <.001). We did not estimate an effect size from baseline to longer follow-up periods because only two studies included a follow-up greater than 6 months.
Figure 4.
Pooled effects on affect intolerance and sensitivity from pre-intervention up to 6-month follow-up
Domain-Specific Analyses
The only affect intolerance/sensitivity domains that were included in ≥ 5 studies were anxiety sensitivity and distress tolerance. There was a small effect of mindfulness and acceptance interventions on anxiety sensitivity from pre- to post-intervention (k = 9; Hedges’ g = −.37, 95% CI = −.57 to −.10, p < .01; I2 = 55.90). In the sensitivity analysis, there was a similar, yet larger effect (Hedges’ g = −.43, 95% CI = −.61 to −.24, p < .001).
There was a small effect of mindfulness and acceptance interventions on distress tolerance from pre-to post-intervention (k = 7; Hedges’ g = −.37, 95% CI = −.63 to −.05, p < .05; I2 = 32.54). In the sensitivity analysis, there was a similar, yet larger effect (Hedges’ g = −.45, 95% CI = −.70 to −.21, p < .001).
Subgroup Analyses
See Table 2 for summary of subgroup analyses of the pooled, overall effect. Studies with inactive controls (Hedges’ g = −.49, 95% CI = −.67 to −.31, p <.001) had a significantly larger effect than those with active comparisons (Hedges’ g = −.19, 95% CI = −.40 to .02, p = .07), Q [1] = 4.47, p = .04. In sensitivity analyses, there was a significant medium pooled effect for studies with inactive controls (Hedges’ g = −.54, 95% CI = −.69 to −.39, p < .001) and a significant small effect for active comparisons (Hedges’ g = −.26, 95% CI = −.46 to −.07, p <.01), with a significantly larger effect for inactive control studies than active comparison studies (Q [1] = 4.88, p = .03).
Table 2.
Subgroup Results
| Moderator Variable | k | Hedges’ g | 95% CI | QBetween |
|---|---|---|---|---|
| Control Type | ||||
| Active | 8 | −.19 | −.40 to .02 | 4.47* |
| Inactive | 15 | −.49** | −.67 to −.31 | |
| Intervention Type | ||||
| Mindfulness | 14 | −.33** | −.51 to −.14 | .54 |
| Acceptance | 9 | −.44** | −.69 to −.19 | |
| Intervention Length | ||||
| < 8 sessions | 5 | −.35* | −.66 to −.04 | .03 |
| ≥ 8 sessions | 18 | −.38** | −.55 to −.20 | |
| Study Population | ||||
| Clinical | 17 | −.37** | −.54 to −.21 | .00 |
| Non-Clinical | 6 | −.38* | −.72 to −.03 |
Note. k = number of studies
p < .01
p < .05
When comparing mindfulness- to acceptance-based interventions, there were significant small effects for both mindfulness-based (Hedges’ g = −.33, 95% CI = −.51 to −.14, p <.01) and acceptance-based interventions (Hedges’ g = −.44, 95% CI = −.69 to −.19, p < .001). There was no significant difference between these effect sizes (Q [1] = .54, p = .46). In sensitivity analyses, each of these effects were larger (Hedges’ g = −.37, 95% CI = −.55 to −.19, p <.001 for mindfulness-focused; Hedges’ g = −.53, 95% CI = −.67 to −.40, p <.001 for acceptance-focused), with no significant difference between these effect sizes (Q [1] = 2.01, p = .16).
When comparing studies with fewer than 8 mindfulness or acceptance intervention sessions (i.e., brief) to studies with 8 or more intervention sessions (i.e., standard), there was a small significant effect for <8 intervention sessions (Hedges’ g = −.35, 95% CI = −.66 to −.04, p < .05) and a small significant effect for ≥ 8 intervention sessions (Hedges’ g = −.38, 95% CI = −.55 to −.20, p <.001). There was no significant difference between these effect sizes (Q [1] = .03, p = .87). In sensitivity analyses, the results were again similar: there were significant small effects for both < 8 interventions sessions (Hedges’ g = −.35, 95% CI = −.66 to −.04, p <.05) and ≥ 8 sessions (Hedges’ g = −.45, 95% CI = −.60 to −.30, p <.001), with no significant difference between effect sizes (Q [1] = .37, p = .54).
In terms of study population, there were small significant effects for both clinical (Hedges’ g = −.37, 95% CI = −.54 to −.21, p <.001) and non-clinical samples (Hedges’ g = −.38, 95% CI = −.72 to −.03, p <.05), with no significant difference between effect sizes, Q [1] = .00, p = .99. In sensitivity analyses, results were similar: there were small significant effects for both clinical (Hedges’ g = −.43, 95% CI = −.57 to −.29, p <.001) and non-clinical samples (Hedges’ g = −.49, 95% CI = −.80 to −.19, p <.01), with no significant difference between effect sizes, Q [1] = .15, p = .70.
Discussion
The current systematic review and meta-analysis examined the effects of RCTs (n = 25 in the qualitative synthesis and n = 22 in the meta-analysis) of mindfulness and acceptance interventions on affect intolerance/sensitivity. Overall, mindfulness and acceptance interventions demonstrated a small-to-medium effect on affect intolerance/sensitivity. This effect was maintained at follow-up periods ranging from one to six months post-intervention. Most studies were considered low or moderate risk (i.e., ≤ 1 high risk domain), and only one study was considered “high risk” (i.e., high risk of bias ratings in more than one domain), though many studies also had many areas of unclear risk.
While there is evidence that the individual constructs (e.g., AS, DT, IU) included in this meta-analysis share a higher-order affect intolerance/sensitivity dimension (Allan et al., 2015; Bardeen et al., 2013; Bernstein et al., 2009; Hong & Cheung, 2015; McHugh & Otto, 2012), some work suggests that there is utility in studying them as distinct constructs (e.g., Allan et al., 2018; Carleton et al., 2007; Laposa et al., 2015). Therefore, we estimated separate domain-specific effect sizes, when applicable. Overall, mindfulness and acceptance interventions demonstrated similar small-to-medium effects on anxiety sensitivity and distress tolerance. These results suggest that mindfulness and acceptance interventions may improve one’s broad-based sensitivity to, or ability to tolerate, a whole host of negative emotional states, rather than one specific emotional domain (e.g., anxiety). However, there were too few studies to estimate domain-specific effect sizes for other affect intolerance/sensitivity constructs (e.g., intolerance of uncertainty, fear of emotions). Given strong interrelationships among affect intolerance/sensitivity measures, we would expect similar effects of mindfulness and acceptance interventions on intolerance of uncertainty, fear of emotions, and other constructs (e.g., disgust sensitivity). Additional research is needed to examine whether these interventions target broad-based affect intolerance/sensitivity or whether there are domain-specific effects.
Numerous theoretical models have purported that reduced affect intolerance/sensitivity is a mechanistic process underlying the salutary effects of mindfulness and acceptance interventions on psychological outcomes (e.g., Farb et al., 2012; Roemer et al., 2015). Findings from the current meta-analysis provide support for these models and suggest that mindfulness and acceptance interventions are effective for changing one’s tolerance of, and sensitivity to, uncomfortable emotions. An important next step in this line of research is to examine whether changes in affect intolerance/sensitivity lead to downstream improvements in psychological outcomes as mindfulness/acceptance theoretical models posit. While several studies have shown that CBT improves symptoms of anxiety and depression through reductions in affect intolerance/sensitivity (e.g., Schmidt et al., 2014; Timpano et al., 2016), few such mediational analyses have been conducted for mindfulness and acceptance interventions. In one of the only studies to date, Arch and colleagues (2012) found that, among individuals with anxiety disorders, session-by-session improvements in anxiety sensitivity mediated the effects of ACT on worry symptoms, but not behavioral avoidance outcomes, quality of life, or depressive symptoms. More research is needed to test the degree to which targeting affect intolerance/sensitivity produces downstream improvements in relevant clinical outcomes (Nielsen et al., 2018).
It also remains unclear, based on current literature, which intervention components are necessary or most potent for engaging affect intolerance/sensitivity processes. Mindfulness and acceptance interventions include a multitude of therapeutic components, practices, didactics, and skills (e.g., seated meditations, metaphors, values-based practices). While this multidimensionality is considered a strength, it also makes it difficult to discern which components are necessary for engaging affect intolerance/sensitivity or other key processes. Though mindfulness and acceptance interventions utilize similar strategies (e.g., brief mindfulness meditations), mindfulness-based interventions place more emphasis on formal meditation. Interestingly, findings from the current meta-analysis suggested that mindfulness and acceptance interventions had a similar effect on affect intolerance/sensitivity. One possible interpretation of this finding is that formal meditation practice may not be a necessary component or does not provide added value above and beyond other therapeutic components for engaging affect intolerance/sensitivity. In support of this interpretation, there is mixed evidence that greater formal meditation practice is associated with better clinical outcomes in mindfulness-based interventions (Lloyd, White, Eames, & Crane, 2018; Parsons, Crane, Parsons, Fjorback, & Kuyken, 2017). Two recent studies found that increases in mindfulness skills broadly, and non-reactivity specifically, meditated the effects of mindfulness training on affect intolerance/sensitivity, suggesting that therapeutic components that foster these skills may be particularly important (Garland et al., 2012; Keng, Smoski, Robins, Ekblad, & Brantley, 2012). Future work should consider utilizing dismantling or factorial designs (e.g., Multiphase Optimization Strategy; Collins, Murphy, & Strecher, 2007) to elucidate the differential and interactive effects of mindfulness and acceptance intervention components for engaging affect intolerance/sensitivity and mindfulness skills.
Similar effects sizes for mindfulness and acceptance interventions also suggests that any structural differences between these interventions (e.g., use of different therapeutic strategies) likely did not contribute to the statistical heterogeneity observed in the current meta-analysis and that assumptions regarding shared goals and processes are justified (Baer & Krietemeyer, 2006; Hayes, 2004; Hayes, Follette, & Linehan, 2004; Roemer, Erisman, & Orsillo, 2008). Similar effect sizes, along with existing empirical evidence of a shared framework, increase confidence in drawing conclusions regarding the combined effect of mindfulness and acceptance interventions on affect intolerance/sensitivity. These results suggest that it may be appropriate for researchers to consider grouping mindfulness and acceptance interventions together in future work. However, subgroup analyses should be interpreted with caution. Indeed, it is possible that there were too few studies in each group to detect significant differences. In addition, some may argue that mindfulness and acceptance are distinct interventions that happen to equally target affect intolerance/sensitivity (i.e., equivalent effect sizes do not justify combining these interventions). More research is needed to continue to explore shared or distinct mechanisms in mindfulness and acceptance interventions and potential similarities or differences in targeting affect intolerance/sensitivity across interventions.
Subgroup analyses also revealed that standard interventions (i.e., eight or more sessions) had a similar effect as brief interventions (i.e., fewer than eight sessions; Hedges’ g = −.38 vs. .35, respectively). Recent meta-analyses, however, suggest that longer mindfulness training durations are associated with stronger effects (Khoury, Sharma, Rush, & Fournier, 2015; Spijkerman, Pots, & Bohlmeijer, 2016), and that brief mindfulness interventions may not produce strong effects on negative affectivity (Schumer, Lindsay, & Creswell, 2018). More research directly comparing the effects of brief interventions to standard 8-week or longer interventions is needed to determine whether higher dose interventions are required for producing changes in key transdiagnostic processes. In addition, subgroup analysis examining study population demonstrated that there were similar effects of mindfulness and acceptance interventions for both clinical and non-clinical populations. This finding is clinical and non-clinical populations generally consistent with previous meta-analyses, which have found that benefit from mindfulness training (e.g., Schumer et al., 2018; Spijkerman et al., 2016).
This meta-analysis indicated that the type of comparison group moderated the effect of mindfulness and acceptance interventions on affect intolerance and sensitivity. Effects were significantly larger for studies with inactive compared to active comparison groups (Hedges’ g = −.49 vs. −.19, respectively). It is important to note that three out of the eight studies with active comparisons included cognitive-behavioral therapy (CBT), a robust comparator. This finding is in line with recent meta-analyses, which showed that mindfulness-based interventions did not differ from other evidence-based interventions across clinical outcomes (e.g., Goldberg et al., 2017; Khoo et al., 2019). These findings might suggest that mindfulness/acceptance and CBT interventions may produce a similar effect on affect intolerance/sensitivity and that clinicians have the option to choose between these interventions based on patient preferences. However, it is important to note that the effect sizes in the current meta-analysis are of a smaller magnitude than effect sizes of CBT on anxiety sensitivity (Smits et al., 2008). More research directly comparing mindfulness/acceptance, traditional CBT, and other types of treatments is needed to draw firm conclusions about the unique effects of mindfulness/acceptance on affect intolerance/sensitivity.
Sensitivity analyses were conducted to examine whether pooled effects differed when two outlier studies were removed (i.e., identified via funnel plot). These outlier studies had unusually large effects favoring control conditions. Across all analyses, when these outliers were removed, effect sizes became larger in favor of mindfulness and acceptance interventions, suggesting that these studies had an impact on the meta-analytic results. While the sensitivity analyses may be more indicative of the true effect of mindfulness and acceptance interventions, these results should be interpreted with caution. Indeed, more research with appropriate time and attention matched controls is needed to determine the true effect of these interventions on affect intolerance/sensitivity (e.g., Zeidan et al., 2010).
This meta-analysis identified several additional directions for future research. First, there is consensus that one’s perceived ability to tolerate distress (measured via self-report) is distinct from one’s actual capacity to withstand distress (measured via behavioral tasks; McHugh et al., 2011). There were too few studies to separately examine the effect of mindfulness and acceptance interventions on behavioral indices of affect intolerance/sensitivity. Future work in this area should include both self-report and behavioral indices of affect intolerance/sensitivity to better understand their interrelationships and to determine whether mindfulness and acceptance interventions differentially engage behavioral and self-report indices. Second, while there is evidence that the individual constructs included in this meta-analysis share a higher-order affect intolerance/sensitivity dimension (Allan et al., 2015; Bardeen et al., 2013; Bernstein et al., 2009; Hong & Cheung, 2015; McHugh & Otto, 2012), it is important to note that a factor analytic model which includes each of these constructs has yet to be tested. Therefore, it is possible that the included constructs are not all hierarchically related, representing a potential source of heterogeneity in the overall analyses (i.e., when the affect intolerance/sensitivity constructs are combined) and suggesting that the aggregate effect should be interpreted with caution. Similar domain-specific effect sizes for anxiety sensitivity and distress tolerance increase our confidence in drawing conclusions regarding the effect of mindfulness and acceptance interventions on an overall affect intolerance/sensitivity construct. Future work is needed to comprehensively test the factor structure of affect intolerance/sensitivity and to examine whether mindfulness and acceptance interventions differentially engage each individual domain. Third, more than half of the included studies used an inactive control group (e.g., waitlist). Thus, positive findings from these studies may be due to non-specific treatment factors (e.g., time, attention) rather than active mindfulness and acceptance treatment components. It is imperative for future studies to include time and attention matched active control groups (e.g., MacCoon et al., 2012; Zeidan et al., 2010). Lastly, this meta-analysis did not extract data related to home practice or homework, which is often an integral component of mindfulness and acceptance interventions. Future meta-analyses may consider examining whether home practice compliance moderates the effect of mindfulness and acceptance on transdiagnostic processes.
Additional limitations of the current meta-analysis include potential publication bias due to the exclusion of unpublished studies. Indeed, missing studies with null findings may have biased the results, though the failsafe N suggested that a large number of studies with null findings would be needed to create a non-significant result. Further, including unpublished studies may result in other forms of bias due to the lack of peer review. We also did not include non-English studies, limiting the generalizability of findings. Despite these limitations, results from this meta-analysis suggest that mindfulness and acceptance interventions may be effective for improving affect intolerance/sensitivity, with effects maintained up to six months. Future work aimed at optimizing these interventions for transdiagnostic process engagement is warranted.
Supplementary Material
Table 1.
Summary of Included Studies
| Reference | Sample | Intervention | Comparison | Intervention dose | Timepoints | Outcome (Measure) | Results |
|---|---|---|---|---|---|---|---|
| Anderson et al. (2007) | Healthy adults (N = 86) | MBSR | Inactive | 2 h once/week × 8 weeks | 2 (BL, post) | AS (ASI) | ↓ at post |
| Arch et al. (2012) | One or more DSM-IV anxiety disorder (N = 143) | ACT | Active | 1 h once/week × 12 weeks | 4 (BL, post, 6mo, 12mo) | AS (ASI) | NS for all timepoints |
| Avdagic et al. (2014) | DSM-IV GAD (N = 51) | ACT | Active | 2 h once/week × 6 weeks | 3 (BL, post, 3mo) | IU (IUS-27) | NS for all timepoints |
| Chan et al. (2015) | COPD (N = 41) | Adapted MBSR | Inactive | 1 h once/week × 8 weeks | 2 (BL, post) | AS (ASI-3) | NS |
| Dixon-Gordon et al. (2015) | Women with DSM-IV BPD (N = 19) | DBT-ER or DBT-IE | Active | 2 h once/week × 7 weeks | 3 (BL, post, 7wk) | DT (DTS, MPTC-C) | NS for all timepoints for DTS and MPTC-C |
| England et al. (2012) | Public speaking anxiety (DSM-IV nongeneralized SAD; N = 45) | Exposure with Acceptance | Active | 2 h X 6 sessions | 2 (BL, post) | DT (Speech latency) | NS |
| Gaylord et al. (2011) | Women with IBS (N = 97) | Adapted MBSR | Active | 2 h once/week × 8 weeks; half day retreat | 3 (BL, post, 3mo) | Visceral Sensitivity (VSI) | NS at post; ↓ at 3mo |
| Gloster et al. (2015) | Panic disorder and/or agoraphobia | ACT | Inactive | 90–120 min 2x/week × 4 | 2 (BL, post) | AS (ASI) | NS |
| with prior unsuccessful tx (N = 43) | weeks | ||||||
| Gonzalez-Menendez et al. (2014) | Follow-up to Lanza et al. 2014; Women inmates with SUD (N = 37) | ACT | Active | 1.5 h once/week × 16 weeks | 2 (12 mo, 18 mo) | AS (ASI) | NS |
| Hazlett-Stevens et al. (2017) | Unselected sample (N = 92) | MBSR bibliotherapy workbook (no contact) | Inactive | suggested 10-week schedule | 2 (BL, post) | AS (ASI) | ↓ at post |
| Helmes et al. (2017) | Older adults with elevated anxiety (N = 52) | MBCT | Active | 1.5 h once/week × 8 weeks | 3 (BL, post, 1mo) | AS (ASI) | ↓ at post and 1mo |
| Lanza et al. (2014) | Women inmates with SUD (N = 50) | ACT | Active and Inactive (i.e., 3 groups) | 1.5 h once/week × 16 weeks | 3 (BL, post, 6mo) | AS (ASI) | Greater ↓ for CBT than ACT and control on ASI-Somatic at post; Greater ↓ in CBT and ACT compared to control on ASI-Cognitive at post; Greater ↓ in ACT than control in ASI-Cognitive at 6mo; Greater ↓ in CBT than ACT in ASI-Social at post; all other analyses NS |
| Lotan et al. (2013) | Community sample (N = 53) | Mindfulness Skills Training | Inactive | 1 h once/week × 4 weeks | 2 (BL, post) | DT (DTS) | ↓ at post |
| Malouf et al. (2017) | Male inmates (N = 40) | REVAMP | Inactive | 90 min 2x/week × 4 weeks | 3 (BL, post, 3mo post release) | DT (MIND-DI) | NS at all timepoints |
| McMain et al. (2017) | DSM-IV BPD with recent suicidal or NSSI episodes (N = 84) | DBT skills group | Inactive | 2 h once/week × 20 weeks | 3 (BL, post, 3mo) | DT (DTS) | ↑ at all timepoints |
| Mitchell et al. (2017) | Adults with DSM-IV ADHD (N = 22) | Mindful awareness | Inactive | 2.5 h once/week × 8 weeks | 2 (BL, post) | DT (DTS) | ↑ at post |
| Morrison et al. (2014) | Undergraduates with delay discounting difficulties (N = 34) | One session based on ACT | Inactive | 60–90 min session | 2 (BL, 1 week) | DT (DTS) | NS |
| Morton et al. (2012) | 4 or more DSM-IV BPD criteria (N = 41) | ACT + TAU | Inactive | 2 h X 12 sessions | 2 (BL, post) | Fear of emotions (ACS) | ↓ at post |
| Neacsiu et al. (2018) | DSM-IV mood or anxiety disorder with high emotion dysregulation (N = 44) | DBT skills group | Active | 2 h once/week × 15 weeks | 3 (BL, post, 2mo) | Disgust sensitivity (DPSS-R) | NS at all timepoints |
| Ritzert et al. (2016) | Adults with difficulties with anxiety symptoms (N = 503) | Mindfulness and Acceptance Workbook for Anxiety (no contact with therapist) | Inactive | suggested 12-week timeline | 2 (BL, post) | AS (ASI) | ↓ at post |
| Robins et al. (2012) | Unselected sample (N = 56) | MBSR | Inactive | 2.5 h once/week × 8 weeks | 2 (BL, post) | Fear of emotions (ACS) | ↓ at post on ACS-total; ↓ at post on ACS-Dep, ACS-Pos |
| Tanay et al. (2012) | Same sample as Lotan et al. (2013); community sample (N = 53) | Mindfulness Skills Training | Inactive | 1 h once/week × 4 weeks | 2 (BL, post) | AS (ASI-3) | ↓ at post |
| Treanor et al. (2011) | DSM-IV GAD (N = 31) | ABBT | Inactive | 4 90-min and 12 1 hr once/week (except last 2 were biweekly) | 2 (BL, post) | IU and fear of emotions (IUS-27, ACS) | ↓ at post on ACS-total and all subscales; ↓ at post on IUS |
| Uliaszek et al. (2016) | Treating seeking undergraduate students (N = 54) | DBT skills group | Active | 2 h once/week × 12 weeks | 2 (BL, post) | DT (DTS) | NS |
| Van Dijk et al. (2013) | Diagnosis of bipolar disorder I or II (N = 26) | DBT-based psychoeducation groups | Inactive | 1.5 h once/week × 12 weeks | 2 (BL, post) | Fear of emotions (ACS) | NS for ACS-total or subscales |
| Victorson et al. (2017) | Men with prostate cancer (N = 43) | MBSR | Active | 2.5 h once/week × 8 weeks; half day retreat | 4 (BL, post, 6mo, 12mo) | IU (IUS) | NS |
| Wells-Di Gregorio et al. (2018) | Individuals with advanced cancer (N = 28) | CBT-ACT | Inactive | 3 1.5 h sessions × 6 weeks | 2 (BL, post) | IU (IUS-27) | NS (p = .058) |
Note. ABBT: Acceptance-Based Behavior Therapy; ACT: Acceptance and Commitment Therapy; CBT: Cognitive Behavioral Therapy; DBT: Dialectical Behavior Therapy; DBT-ER: Dialectical Behavior Therapy- Emotion Regulation; DBT-IE: Dialectical Behavior Therapy-Interpersonal Effectiveness; MBCT: Mindfulness-Based Cognitive Therapy; MBSR: Mindfulness-Based Stress Reduction; REVAMP: Re-entry Values and Mindfulness Program; TAU: treatment as usual; AS: anxiety sensitivity; DT: distress tolerance; IU: intolerance of uncertainty; ASI: Anxiety Sensitivity Index; ASI-Cognitive: Anxiety Sensitivity- Cognitive subscale; ASI-Social: Anxiety Sensitivity Index-Social subscale; ASI-Somatic: Anxiety Sensitivity Index- Somatic Subscale; ASI-3: Anxiety Sensitivity Index-3; ACS: Affective Control Scale; ACS-Dep; Affective Control Scale-Depression subscale; ACS-Pos: Affective Control Scale-Positive Emotion subscale; DPSS-R: Disgust Propensity and Sensitivity Scale-Revised; DTS: Distress Tolerance Scale; IUS: Intolerance of Uncertainty Scale; IUS-27: Intolerance of Uncertainty Scale-27; MIND-DI: Mindfulness Inventory Nine Dimensions: Distress Intolerance; MTPT-C: Mirror-Tracing Persistence Task-Computerized; VSI: Visceral Sensitivity Index; BL: baseline; NS: nonsignificant; N = number of participants randomized, which may be different from the number analyzed; Only group-by-time effects presented.
Highlights.
Affect intolerance/sensitivity is a risk factor for psychological disorders
We examined the effects of mindfulness/acceptance on affect intolerance/sensitivity
There was a small-to-medium effect size, with effects maintained up to 6 months
Control group status was a significant moderator
Mindfulness/acceptance are modestly effective for improving this target
Acknowledgments
Funding: KMK was supported by the NIH under Grant 2T32AT000051. DLH was supported by the NIH under grant 1K23AT010157–01. CML was supported by the NIH under grant 1K23AT009715–02. GYY was supported by the NIH under grant K24AT009465
Footnotes
Conflict of Interest: The authors declare no conflict of interest
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Allan NP, Cooper D, Oglesby ME, Short NA, Saulnier KG, & Schmidt NB (2018). Lower-order anxiety sensitivity and intolerance of uncertainty dimensions operate as specific vulnerabilities for social anxiety and depression within a hierarchical model. Journal of Anxiety Disorders, 53, 91–99. 10.1016/j.janxdis.2017.08.002 [DOI] [PubMed] [Google Scholar]
- Allan NP, Macatee RJ, Norr AM, Raines AM, & Schmidt NB (2015). Relations between common and specific factors of anxiety sensitivity and distress tolerance and fear, distress, and alcohol and substance use disorders. Journal of Anxiety Disorders, 33, 81–89. 10.1016/j.janxdis.2015.05.002 [DOI] [PubMed] [Google Scholar]
- Anderson ND, Lau MA, Segal ZV, & Bishop SR (2007). Mindfulness‐based stress reduction and attentional control. Clinical Psychology & Psychotherapy: An International Journal of Theory & Practice, 14, 449–463. 10.1002/cpp.544 [DOI] [Google Scholar]
- Arch JJ, Eifert GH, Davies C, Vilardaga JCP, Rose RD, & Craske MG (2012). Randomized clinical trial of cognitive behavioral therapy (CBT) versus acceptance and commitment therapy (ACT) for mixed anxiety disorders. Journal of Consulting and Clinical Psychology, 80, 750. 10.1037/a0028310 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arch JJ, Wolitzky-Taylor KB, Eifert GH, & Craske MG (2012). Longitudinal treatment mediation of traditional cognitive behavioral therapy and acceptance and commitment therapy for anxiety disorders. Behaviour Research and Therapy, 50, 469–478. 10.1016/j.brat.2012.04.007 [DOI] [PubMed] [Google Scholar]
- Avdagic E, Morrissey SA, & Boschen MJ (2014). A randomised controlled trial of acceptance and commitment therapy and cognitive-behaviour therapy for generalised anxiety disorder. Behaviour Change, 31, 110–130. 10.1017/bec.2014.5 [DOI] [Google Scholar]
- Baer RA, & Krietemeyer J (2006). Overview of mindfulness-and acceptance-based treatment approaches. In Baer RA (Eds.), Mindfulness-based treatment approaches: Clinician’s guide to evidence base and applications (pp. 3–27). Elesvier. [Google Scholar]
- Bardeen JR, Fergus TA, & Orcutt HK (2013). Testing a hierarchical model of distress tolerance. Journal of Psychopathology and Behavioral Assessment, 35, 495–505. 10.1007/s10862-013-9359-0 [DOI] [Google Scholar]
- Barlow DH (2004). Anxiety and its disorders: The nature and treatment of anxiety and panic. New York, NY: Guilford press. [Google Scholar]
- Barlow DH, Farchione TJ, Sauer-Zavala S, Latin HM, Ellard KK, Bullis JR, … & Cassiello-Robbins C (2017). Unified protocol for transdiagnostic treatment of emotional disorders: Therapist guide. New York, NY: Oxford University Press. [Google Scholar]
- Bernstein A, Hadash Y, Lichtash Y, Tanay G, Shepherd K, & Fresco DM (2015). Decentering and related constructs: A critical review and metacognitive processes model. Perspectives on Psychological Science, 10, 599–617. 10.1177/1745691615594577 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernstein A, Zvolensky MJ, Vujanovic AA, & Moos R (2009). Integrating anxiety sensitivity, distress tolerance, and discomfort intolerance: A hierarchical model of affect sensitivity and tolerance. Behavior Therapy, 40, 291–301. 10.1016/j.beth.2008.08.001 [DOI] [PubMed] [Google Scholar]
- Bishop SR, Lau M, Shapiro S, Carlson L, Anderson ND, Carmody J, … & Devins G (2004). Mindfulness: A proposed operational definition. Clinical psychology: Science and Practice, 11, 230–241. 10.1093/clipsy.bph077 [DOI] [Google Scholar]
- Borenstein M, Hedges L, Higgins J, Rothstein H. (2014). Comprehensive meta- analysis version 3. Biostat: Englewood, NJ. [Google Scholar]
- Brown KW, Ryan RM, & Creswell JD (2007). Mindfulness: Theoretical foundations and evidence for its salutary effects. Psychological Inquiry, 18, 211–237. 10.1080/10478400701598298 [DOI] [Google Scholar]
- Brown TA, & Barlow DH (2009). A proposal for a dimensional classification system based on the shared features of the DSM-IV anxiety and mood disorders: Implications for assessment and treatment. Psychological Assessment, 21, 256. 10.1037/a0016608 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown TA, Campbell LA, Lehman CL, Grisham JR, & Mancill RB (2001). Current and lifetime comorbidity of the DSM-IV anxiety and mood disorders in a large clinical sample. Journal of Abnormal Psychology, 110, 585. 10.1037/0021-843X.110.4.585 [DOI] [PubMed] [Google Scholar]
- Brown TA, Chorpita BF, & Barlow DH (1998). Structural relationships among dimensions of the DSM-IV anxiety and mood disorders and dimensions of negative affect, positive affect, and autonomic arousal. Journal of Abnormal Psychology, 107, 179. 10.1037/0021-843X.107.2.179 [DOI] [PubMed] [Google Scholar]
- Carleton RN (2016). Fear of the unknown: One fear to rule them all?. Journal of Anxiety Disorders, 41, 5–21. 10.1016/j.janxdis.2016.03.011 [DOI] [PubMed] [Google Scholar]
- Carleton RN, Sharpe D, & Asmundson GJ (2007). Anxiety sensitivity and intolerance of uncertainty: Requisites of the fundamental fears?. Behaviour Research and Therapy, 45, 2307–2316. 10.1016/j.brat.2007.04.006 [DOI] [PubMed] [Google Scholar]
- Chan RR, Giardino N, & Larson JL (2015). A pilot study: mindfulness meditation intervention in COPD. International Journal of Chronic Obstructive Pulmonary Disease, 10, 445. 10.2147/COPD.S73864 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cisler JM, Olatunji BO, & Lohr JM (2009). Disgust, fear, and the anxiety disorders: A critical review. Clinical Psychology Review, 29, 34–46. 10.1016/j.cpr.2008.09.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collins LM, Murphy SA, & Strecher V (2007). The multiphase optimization strategy (MOST) and the sequential multiple assignment randomized trial (SMART): new methods for more potent eHealth interventions. American Journal of Preventive Medicine, 32, S112–S118. 10.1016/j.amepre.2007.01.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cramer H, Lauche R, Haller H, Langhorst J, & Dobos G (2016). Mindfulness-and acceptance-based interventions for psychosis: a systematic review and meta-analysis. Global Advances in Health and Medicine, 5, 30–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dixon-Gordon KL, Chapman AL, & Turner BJ (2015). A preliminary pilot study comparing dialectical behavior therapy emotion regulation skills with interpersonal effectiveness skills and a control group treatment. Journal of Experimental Psychopathology, 6, 369–388. 10.5127/jep.041714 [DOI] [Google Scholar]
- England EL, Herbert JD, Forman EM, Rabin SJ, Juarascio A, & Goldstein SP (2012). Acceptance-based exposure therapy for public speaking anxiety. Journal of Contextual Behavioral Science, 1, 66–72. 10.1016/j.jcbs.2012.07.001 [DOI] [Google Scholar]
- Farb NA, Anderson AK, & Segal ZV (2012). The mindful brain and emotion regulation in mood disorders. The Canadian Journal of Psychiatry, 57, 70–77. 10.1177/070674371205700203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farchione TJ, Fairholme CP, Ellard KK, Boisseau CL, Thompson-Hollands J, Carl JR, … & Barlow DH (2012). Unified protocol for transdiagnostic treatment of emotional disorders: A randomized controlled trial. Behavior Therapy, 43, 666–678. 10.1016/j.beth.2012.01.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldberg SB, Tucker RP, Greene PA, Davidson RJ, Wampold BE, Kearney DJ, & Simpson TL (2018). Mindfulness-based interventions for psychiatric disorders: A systematic review and meta-analysis. Clinical Psychology Review, 59, 52–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes SC (2004). Acceptance and commitment therapy, relational frame theory, and the third wave of behavioral and cognitive therapies. Behavior Therapy, 35, 639–665. 10.1016/S0005-7894(04)80013-3 [DOI] [PubMed] [Google Scholar]
- Hayes SC, Follette VM, & Linehan M (Eds.). (2004). Mindfulness and acceptance: Expanding the cognitive-behavioral tradition. Guilford Press. [Google Scholar]
- Hayes SC, Pistorello J, & Levin ME (2012). Acceptance and commitment therapy as a unified model of behavior change. The Counseling Psychologist, 40, 976–1002. 10.1177/0011000012460836 [DOI] [Google Scholar]
- Hayes SC, Wilson KG, Gifford EV, Follette VM, & Strosahl K (1996). Experiential avoidance and behavioral disorders: A functional dimensional approach to diagnosis and treatment. Journal of Consulting and Clinical Psychology, 64, 1152. 10.1037/0022-006X.64.6.1152 [DOI] [PubMed] [Google Scholar]
- Hazlett-Stevens H, & Oren Y (2017). Effectiveness of Mindfulness-Based Stress Reduction Bibliotherapy: A Preliminary Randomized Controlled Trial. Journal of Clinical Psychology, 73, 626–637. 10.1002/jclp.22370 [DOI] [PubMed] [Google Scholar]
- Helmes E, & Ward BG (2017). Mindfulness-based cognitive therapy for anxiety symptoms in older adults in residential care. Aging & Mental Health, 21, 272–278. 10.1080/13607863.2015.1111862 [DOI] [PubMed] [Google Scholar]
- Higgins JP, & Green S (Eds.). (2011). Cochrane handbook for systematic reviews of interventions (Vol. 4). John Wiley & Sons. [Google Scholar]
- Hofmann SG, & Hayes SC (2019). The future of intervention science: Process-based therapy. Clinical Psychological Science, 7, 37–50. 10.1177/2167702618772296 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hofmann SG, Sawyer AT, Witt AA, & Oh D (2010). The effect of mindfulness-based therapy on anxiety and depression: A meta-analytic review. Journal of Consulting and Clinical Psychology, 78, 169–183. 10.1037/a0018555 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoge EA, Bui E, Goetter E, Robinaugh DJ, Ojserkis RA, Fresco DM, & Simon NM (2015). Change in decentering mediates improvement in anxiety in mindfulness-based stress reduction for generalized anxiety disorder. Cognitive Therapy and Research, 39, 228–235. 10.1007/s10608-014-9646-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hölzel BK, Lazar SW, Gard T, Schuman-Olivier Z, Vago DR, & Ott U (2011). How does mindfulness meditation work? Proposing mechanisms of action from a conceptual and neural perspective. Perspectives on Psychological Science, 6, 537–559. 10.1177/1745691611419671 [DOI] [PubMed] [Google Scholar]
- Hong RY, & Cheung MWL (2015). The structure of cognitive vulnerabilities to depression and anxiety: Evidence for a common core etiologic process based on a meta-analytic review. Clinical Psychological Science, 3, 892–912. 10.1177/2167702614553789 [DOI] [Google Scholar]
- Garland EL, Gaylord SA, Palsson O, Faurot K, Mann JD, & Whitehead WE (2012). Therapeutic mechanisms of a mindfulness-based treatment for IBS: effects on visceral sensitivity, catastrophizing, and affective processing of pain sensations. Journal of Behavioral Medicine, 35, 591–602. 10.1007/s10865-011-9391-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gaylord SA, Palsson OS, Garland EL, Faurot KR, Coble RS, Mann JD, … & Whitehead WE (2011). Mindfulness training reduces the severity of irritable bowel syndrome in women: results of a randomized controlled trial. The American Journal of Gastroenterology, 106, 1678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gentes EL, & Ruscio AM (2011). A meta-analysis of the relation of intolerance of uncertainty to symptoms of generalized anxiety disorder, major depressive disorder, and obsessive–compulsive disorder. Clinical Psychology Review, 31, 923–933. 10.1016/j.cpr.2011.05.001 [DOI] [PubMed] [Google Scholar]
- Gloster AT, Sonntag R, Hoyer J, Meyer AH, Heinze S, Ströhle A, … & Wittchen HU (2015). Treating treatment-resistant patients with panic disorder and agoraphobia using psychotherapy: A randomized controlled switching trial. Psychotherapy and Psychosomatics, 84, 100–109. 10.1159/000370162 [DOI] [PubMed] [Google Scholar]
- González Menéndez A, Fernández P, Rodríguez F, & Villagrá P (2014). Long-term outcomes of Acceptance and Commitment Therapy in drug-dependent female inmates: A randomized controlled trial. International Journal of Clinical and Health Psychology, 14, 18–27. [Google Scholar]
- Jeffries ER, McLeish AC, Kraemer KM, Avallone KM, & Fleming JB (2016). The role of distress tolerance in the use of specific emotion regulation strategies. Behavior Modification, 40, 439–451. 10.1177//0145445515619596 [DOI] [PubMed] [Google Scholar]
- Kabat-Zinn J (1982). An outpatient program in behavioral medicine for chronic pain patients based on the practice of mindfulness meditation: Theoretical considerations and preliminary results. General hospital psychiatry, 4(1), 33–47. [DOI] [PubMed] [Google Scholar]
- Keng SL, Smoski MJ, & Robins CJ (2011). Effects of mindfulness on psychological health: A review of empirical studies. Clinical Psychology Review, 31, 1041–1056. 10.1016/j.cpr.2011.04.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keng SL, Smoski MJ, Robins CJ, Ekblad AG, & Brantley JG (2012). Mechanisms of change in mindfulness-based stress reduction: Self-compassion and mindfulness as mediators of intervention outcomes. Journal of Cognitive Psychotherapy, 26, 270–280. 10.1891/0889-8391.26.3.270 [DOI] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, & Walters EE (2005). Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry, 62, 593–602. 10.1001/archpsyc.62.6.593 [DOI] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Koretz D, Merikangas KR, … & Wang PS (2003). The epidemiology of major depressive disorder: results from the National Comorbidity Survey Replication (NCS-R). JAMA, 289, 3095–3105. 10.1001/jama.289.23.3095 [DOI] [PubMed] [Google Scholar]
- Khoo EL, Small R, Cheng W, Hatchard T, Glynn B, Rice DB, … & Poulin PA (2019). Comparative evaluation of group-based mindfulness-based stress reduction and cognitive behavioural therapy for the treatment and management of chronic pain: A systematic review and network meta-analysis. Evidence-Based Mental Health, 22, 26–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khoury B, Sharma M, Rush SE, & Fournier C (2015). Mindfulness-based stress reduction for healthy individuals: A meta-analysis. Journal of Psychosomatic Research, 78, 519–528. 10.1016/j.jpsychores.2015.03.009 [DOI] [PubMed] [Google Scholar]
- Kraemer KM, McLeish AC, & O’Bryan EM (2015). The role of intolerance of uncertainty in terms of alcohol use motives among college students. Addictive Behaviors, 42, 162–166. 10.1016/j.addbeh.2014.11.033 [DOI] [PubMed] [Google Scholar]
- Lanza PV, Garcia PF, Lamelas FR, & González‐Menéndez A (2014). Acceptance and commitment therapy versus cognitive behavioral therapy in the treatment of substance use disorder with incarcerated women. Journal of clinical psychology, 70, 644–657. 10.1002/jclp.22060 [DOI] [PubMed] [Google Scholar]
- Laposa JM, Collimore KC, Hawley LL, & Rector NA (2015). Distress tolerance in OCD and anxiety disorders, and its relationship with anxiety sensitivity and intolerance of uncertainty. Journal of Anxiety Disorders, 33, 8–14. 10.1016/j.janxdis.2015.04.003 [DOI] [PubMed] [Google Scholar]
- Leyro TM, Zvolensky MJ, & Bernstein A (2010). Distress tolerance and psychopathological symptoms and disorders: a review of the empirical literature among adults. Psychological Bulletin, 136, 576. 10.1037/a0019712 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindsay EK, & Creswell JD (2017). Mechanisms of mindfulness training: Monitor and Acceptance Theory (MAT). Clinical Psychology Review, 51, 48–59. 10.1016/j.cpr.2016.10.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linehan MM (1993). Skills training manual for treating borderline personality disorder. New York, NY: Guilford Press. [Google Scholar]
- Lloyd A, White R, Eames C, & Crane R (2018). The utility of home-practice in mindfulness-based group interventions: A systematic review. Mindfulness, 9, 673–692. 10.1007/s12671-017-0813-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lotan G, Tanay G, & Bernstein A (2013). Mindfulness and distress tolerance: relations in a mindfulness preventive intervention. International Journal of Cognitive Therapy, 6, 371–385. 10.1521/ijct.2013.6.4.371 [DOI] [Google Scholar]
- MacCoon DG, Imel ZE, Rosenkranz MA, Sheftel JG, Weng HY, Sullivan JC, … & Lutz A (2012). The validation of an active control intervention for Mindfulness Based Stress Reduction (MBSR). Behaviour Research and Therapy, 50, 3–12. 10.1016/j.brat.2011.10.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malouf ET, Youman K, Stuewig J, Witt EA, & Tangney JP (2017). A pilot RCT of a values-based mindfulness group intervention with jail inmates: Evidence for reduction in post-release risk behavior. Mindfulness, 8, 603–614. 10.1007/s12671-016-0636-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McEvoy PM, Hyett MP, Shihata S, Price JE, & Strachan L (2019). The impact of methodological and measurement factors on transdiagnostic associations with intolerance of uncertainty: A meta-analysis. Clinical Psychology Review, 73, 101778. 10.1016/j.cpr.2019.101778 [DOI] [PubMed] [Google Scholar]
- McHugh RK, Daughters SB, Lejuez CW, Murray HW, Hearon BA, Gorka SM, & Otto MW (2011). Shared variance among self-report and behavioral measures of distress intolerance. Cognitive Therapy and Research, 35, 266–275. 10.1007/s10608-010-9295-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McHugh RK, & Otto MW (2012). Refining the measurement of distress intolerance. Behavior Therapy, 43, 641–651. 10.1016/j.beth.2011.12.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McMain SF, Guimond T, Barnhart R, Habinski L, & Streiner DL (2017). A randomized trial of brief dialectical behaviour therapy skills training in suicidal patients suffering from borderline disorder. Acta Psychiatrica Scandinavica, 135, 138–148. 10.1111/acps.12664 [DOI] [PubMed] [Google Scholar]
- McNally RJ (2002). Anxiety sensitivity and panic disorder. Biological Psychiatry, 52, 938–946. 10.1016/S0006-3223(02)01475-0 [DOI] [PubMed] [Google Scholar]
- Mitchell JT, McIntyre EM, English JS, Dennis MF, Beckham JC, & Kollins SH (2017). A pilot trial of mindfulness meditation training for ADHD in adulthood: Impact on core symptoms, executive functioning, and emotion dysregulation. Journal of Attention Disorders, 21, 1105–1120. 10.1177/1087054713513328 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moher D, Liberati A, Tetzlaff J, & Altman DG (2009). Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Annals of Internal Medicine, 151, 264–269. 10.7326/0003-4819-151-4-200908180-00135 [DOI] [PubMed] [Google Scholar]
- Morrison KL, Madden GJ, Odum AL, Friedel JE, & Twohig MP (2014). Altering impulsive decision making with an acceptance-based procedure. Behavior Therapy, 45, 630–639. 10.1016/j.beth.2014.01.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morton J, Snowdon S, Gopold M, & Guymer E (2012). Acceptance and commitment therapy group treatment for symptoms of borderline personality disorder: A public sector pilot study. Cognitive and Behavioral Practice, 19, 527–544. 10.1016/j.cbpra.2012.03.005 [DOI] [Google Scholar]
- Naragon-Gainey K (2010). Meta-analysis of the relations of anxiety sensitivity to the depressive and anxiety disorders. Psychological Bulletin, 136, 128. 10.1037/a0018055 [DOI] [PubMed] [Google Scholar]
- Neacsiu AD, Rompogren J, Eberle JW, & McMahon K (2018). Changes in problematic anger, shame, and disgust in anxious and depressed adults undergoing treatment for emotion dysregulation. Behavior Therapy, 49, 344–359. 10.1016/j.beth.2017.10.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nielsen L, Riddle M, King JW, Aklin WM, Chen W, Clark D, … & Green P (2018). The NIH Science of Behavior Change Program: Transforming the science through a focus on mechanisms of change. Behaviour Research and Therapy, 101, 3–11. 10.1016/j.brat.2017.07.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norr AM, Allan NP, Macatee RJ, Keough ME, & Schmidt NB (2014). The effects of an anxiety sensitivity intervention on anxiety, depression, and worry: Mediation through affect tolerances. Behaviour Research and Therapy, 59, 12–19. 10.1016/j.brat.2014.05.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olatunji BO, & McKay D (2007). Disgust and psychiatric illness: have we remembered?. The British Journal of Psychiatry, 190, 457–459. 10.1192/bjp.bp.106.032631 [DOI] [PubMed] [Google Scholar]
- Parsons CE, Crane C, Parsons LJ, Fjorback LO, & Kuyken W (2017). Home practice in Mindfulness-Based Cognitive Therapy and Mindfulness-Based Stress Reduction: A systematic review and meta-analysis of participants’ mindfulness practice and its association with outcomes. Behaviour Research and Therapy, 95, 29–41. 10.1016/j.brat.2017.05.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ritzert TR, Forsyth JP, Sheppard SC, Boswell JF, Berghoff CR, & Eifert GH (2016). Evaluating the effectiveness of ACT for anxiety disorders in a self-help context: Outcomes from a randomized wait-list controlled trial. Behavior Therapy, 47, 444–459. 10.1016/j.beth.2016.03.001 [DOI] [PubMed] [Google Scholar]
- Robins CJ, Keng SL, Ekblad AG, & Brantley JG (2012). Effects of mindfulness‐based stress reduction on emotional experience and expression: A randomized controlled trial. Journal of Clinical Psychology, 68, 117–131. 10.1002/jclp.20857 [DOI] [PubMed] [Google Scholar]
- Roemer L, Erisman SM, & Orsillo SM (2008). Mindfulness and acceptance-based treatments for anxiety disorders. In Antony AM & Murray SB (Eds.), Oxford handbook of anxiety and related disorders (pp. 476–487). Oxford University Press. [Google Scholar]
- Roemer L, Williston SK, & Rollins LG (2015). Mindfulness and emotion regulation. Current Opinion in Psychology, 3, 52–57. 10.1016/j.copsyc.2015.02.006 [DOI] [Google Scholar]
- Sauer S, & Baer RA (2010). Mindfulness and decentering as mechanisms of change in mindfulness-and acceptance-based interventions. In Baer RA (Eds.), Assessing Mindfulness and Acceptance Processes in Clients (pp. 25–50). Context Press. [Google Scholar]
- Sauer-Zavala S, Boswell JF, Gallagher MW, Bentley KH, Ametaj A, & Barlow DH (2012). The role of negative affectivity and negative reactivity to emotions in predicting outcomes in the unified protocol for the transdiagnostic treatment of emotional disorders. Behaviour Research and Therapy, 50, 551–557. 10.1016/j.brat.2012.05.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Segal ZV, & Teasdale J (2018). Mindfulness-based cognitive therapy for depression. New York, NY: Guilford Publications. [Google Scholar]
- Schmidt NB, Capron DW, Raines AM, & Allan NP (2014). Randomized clinical trial evaluating the efficacy of a brief intervention targeting anxiety sensitivity cognitive concerns. Journal of Consulting and Clinical Psychology, 82, 1023. 10.1037/a0036651 [DOI] [PubMed] [Google Scholar]
- Schmidt NB, Mitchell M, Keough M, & Riccardi C (2011). Anxiety and its Disorders. In Zvolensky MJ, Bernstein A & Vujanovic AA (Eds.), Distress Tolerance: Theory, research, and clinical applications (pp. 105–125). New York, NY: Guilford Press. [Google Scholar]
- Schumer MC, Lindsay EK, & Creswell JD (2018). Brief mindfulness training for negative affectivity: A systematic review and meta-analysis. Journal of Consulting and Clinical Psychology, 86, 569. 10.1037/ccp0000324 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smits JA, Berry AC, Tart CD, & Powers MB (2008). The efficacy of cognitive-behavioral interventions for reducing anxiety sensitivity: A meta-analytic review. Behaviour Research and Therapy, 46(9), 1047–1054. 10.1016/j.brat.2008.06.010 [DOI] [PubMed] [Google Scholar]
- Spijkerman MPJ, Pots WTM, & Bohlmeijer ET (2016). Effectiveness of online mindfulness-based interventions in improving mental health: A review and meta-analysis of randomised controlled trials. Clinical Psychology Review, 45, 102–114. 10.1016/j.cpr.2016.03.009 [DOI] [PubMed] [Google Scholar]
- Simons JS, & Gaher RM (2005). The Distress Tolerance Scale: Development and validation of a self-report measure. Motivation and Emotion, 29, 83–102. 10.1007/s11031-005-7955-3 [DOI] [Google Scholar]
- Stockton D, Kellett S, Berrios R, Sirois F, Wilkinson N, & Miles G (2019). Identifying the underlying mechanisms of change during acceptance and commitment therapy (ACT): A systematic review of contemporary mediation studies. Behavioural and Cognitive Psychotherapy, 47, 332–362. 10.1017/S1352465818000553 [DOI] [PubMed] [Google Scholar]
- Tanay G, Lotan G, & Bernstein A (2012). Salutary proximal processes and distal mood and anxiety vulnerability outcomes of mindfulness training: A pilot preventive intervention. Behavior Therapy, 43, 492–505. 10.1016/j.beth.2011.06.003 [DOI] [PubMed] [Google Scholar]
- Timpano KR, Raines AM, Shaw AM, Keough ME, & Schmidt NB (2016). Effects of a brief anxiety sensitivity reduction intervention on obsessive compulsive spectrum symptoms in a young adult sample. Journal of Psychiatric Research, 83, 8–15. 10.1016/j.jpsychires.2016.07.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Treanor M (2011). The potential impact of mindfulness on exposure and extinction learning in anxiety disorders. Clinical Psychology Review, 31, 617–625. 10.1016/j.cpr.2011.02.003 [DOI] [PubMed] [Google Scholar]
- Treanor M, Erisman SM, Salters-Pedneault K, Roemer L, & Orsillo SM (2011). Acceptance-based behavioral therapy for GAD: Effects on outcomes from three theoretical models. Depression and Anxiety, 28, 127–136. 10.1002/da.20766 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uliaszek AA, Rashid T, Williams GE, & Gulamani T (2016). Group therapy for university students: A randomized control trial of dialectical behavior therapy and positive psychotherapy. Behaviour Research and Therapy, 77, 78–85. 10.1016/j.brat.2015.12.003 [DOI] [PubMed] [Google Scholar]
- Van Dijk S, Jeffrey J, & Katz MR (2013). A randomized, controlled, pilot study of dialectical behavior therapy skills in a psychoeducational group for individuals with bipolar disorder. Journal of Affective Disorders, 145, 386–393. 10.1016/j.jad.2012.05.054 [DOI] [PubMed] [Google Scholar]
- Veehof MM, Trompetter HR, Bohlmeijer ET, & Schreurs KMG (2016). Acceptance- and mindfulness-based interventions for the treatment of chronic pain: a meta-analytic review. Cognitive Behaviour Therapy, 45, 5–31. [DOI] [PubMed] [Google Scholar]
- Victorson D, Hankin V, Burns J, Weiland R, Maletich C, Sufrin N, … & Brendler C (2017). Feasibility, acceptability and preliminary psychological benefits of mindfulness meditation training in a sample of men diagnosed with prostate cancer on active surveillance: results from a randomized controlled pilot trial. Psycho‐Oncology, 26, 1155–1163. 10.1002/pon.4135 [DOI] [PubMed] [Google Scholar]
- Villatte JL, Vilardaga R, Villatte M, Vilardaga JCP, Atkins DC, & Hayes SC (2016). Acceptance and Commitment Therapy modules: Differential impact on treatment processes and outcomes. Behaviour Research and Therapy, 77, 52–61. 10.1016/j.brat.2015.12.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vøllestad J, Nielsen MB, & Nielsen GH (2012). Mindfulness‐and acceptance‐based interventions for anxiety disorders: A systematic review and meta‐analysis. British Journal of Clinical Psychology, 51, 239–260. [DOI] [PubMed] [Google Scholar]
- Wells‐Di Gregorio SM, Marks DR, DeCola J, Peng J, Probst D, Zaleta A, … & Magalang U (2019). Pilot randomized controlled trial of a symptom cluster intervention in advanced cancer. Psycho-Oncology, 28, 76–84. 10.1002/pon.4912 [DOI] [PubMed] [Google Scholar]
- Wilamowska ZA, Thompson-Hollands J, Fairholme CP, Ellard KK, Farchione TJ, & Barlow DH (2010). Conceptual background, development, and preliminary data from the unified protocol for transdiagnostic treatment of emotional disorders. Depression and Anxiety, 27, 882–890. 10.1002/da.20735 [DOI] [PubMed] [Google Scholar]
- Williams KE, Chambless DL, & Ahrens A (1997). Are emotions frightening? An extension of the fear of fear construct. Behaviour Research and Therapy, 35, 239–248. 10.1016/S0005-7967(96)00098-8 [DOI] [PubMed] [Google Scholar]
- Zeidan F, Johnson SK, Gordon NS, & Goolkasian P (2010). Effects of brief and sham mindfulness meditation on mood and cardiovascular variables. The Journal of Alternative and Complementary Medicine, 16, 867–873. 10.1089/acm.2009.0321 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.