Abstract
Introduction
Fasting is a common cultural practice worldwide for both religious and dietary reasons. However, there is concern that fasting may be a risk factor for the development of renal stones. To date, there has not been a systematic assessment of the literature regarding the association between renal stones and fasting.
Methods
We conducted a systematic review following PRISMA guidelines of three databases: Medline-OVID, EMBASE, and CINAHL. All screening and extraction was completed in parallel with two independent reviewers.
Results
Of the 1501 database citations, a total of 10 observational studies with a total of 9906 participants were included. Nine of the studies were conducted in the context of Islamic fasting during Ramadan, with the majority (7/9) finding that renal colic incidence was unaffected by the month of fasting. In contrast, two studies noted an increased incidence among fasting populations. Two other studies noted that urine metabolites and density were altered with fasting but did not translate into clinical outcomes.
Conclusions
Based on the available evidence, it is unlikely that fasting significantly increases the risk of renal stones. Physicians should counsel higher-risk patients on safe fasting practices.
Introduction
The practice of fasting, defined as the deliberate restriction of food or water intake, has been increasingly studied in the medical literature.1 There are diverse fasting practices worldwide, varying in duration and types of permissible intake. Fasting is observed in many religions, including the Bahá’í Faith, Buddhism, Christianity, Hinduism, Islam, Jainism, and Judaism.2–5 Fasting has also traditionally been used as a method of non-violent protest.6 In the 21st century, there has been a rising surge of interest in fasting for health purposes. Intermittent fasting is a popular weight loss diet in which participants fast in cyclical patterns.7 For instance, followers of the “5:2 diet” restrict their caloric intake on two days of a seven-day cycle.8 Studies have demonstrated metabolic benefits to fasting, including improved glycemic control, insulin sensitivity, and appetite reduction, which culminates in overall weight loss.2,9
While the short-term adverse effects of fasting are well-documented and are largely related to symptoms of hypoglycemia (headaches, nausea, and lethargy),10 the long-term health outcomes remain unclear. There is particular concern that fasting may be a risk factor for the development of renal stones. Low urine volume and dehydration are both risk factors for renal stone formation.11,12 Fasting can lead to dehydration, which in turn promotes the secretion of antidiuretic hormone (ADH) and adrenocorticotropic hormone (ACTH). Both hormones reduce urine output and concentrate calcium in urine, the main precipitant of renal stones.13,14
While there have been numerous narrative reviews on the topic, there has not yet been a systematic assessment of literature.15,16 Additionally, previous reviews did not search for studies examining fasting for weight loss, including intermittent fasting or “5:2” studies. As such, a consensus on the best practices of fasting and renal stones has not been reached.17 The aim of this systematic review is to collect all available literature regarding renal stones and fasting. We aim to characterize the incidence of renal stones in fasting populations, in addition to determining the association between the duration of fasting and type of intake with renal stone formation.
Methods
This systematic review was conducted according to the standards and guidelines established by the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) and the fourth edition of the Joanna Briggs Institute Reviewer’s Manual.17,18 We conducted a systematic literature search of three databases: Ovid MEDLINE, Ovid EMBASE, and EBSCO CINAHL plus.
We remained broad with our search criteria to maximize sensitivity. We searched broadly for all types of fasting and did not add specifiers to limit our yield. Our search strategy is described in Supplementary Table 1, with eligibility criteria listed in Table 1.
Table 1.
Eligibility criteria
| Population | Any population currently fasting (either for research purposes, religious reasons, intermittent fasting/dietary) |
| Intervention | N/A (observational or interventional were both eligible) |
| Comparator | N/A |
| Outcomes | Any outcome reported in the literature related to renal stones |
We only examined original, peer-reviewed literature published in the English language. Databases were examined from their inception until March 18, 2020. Published conference posters, papers, and abstracts were eligible for inclusion.
Articles were excluded if they were not relevant to fasting or did not report outcomes related to kidney stones. The definition of fasting was kept broad, including either restriction of food or water intake for any time period. Papers that self-identified as being relevant to fasting were included. Case reports, animal studies, and cadaveric studies were excluded.
Study selection and extraction
Study selection was completed in duplicate by two independent, parallel reviewers (AL, SK) for both title and abstract screening, as well as full-text screening. Covidence was used for data management and screening. Data extraction was performed in duplicate by two independent investigators (AL, SK), with a third (AK) resolving discrepancies. Risk of bias assessment was graded using the RoBANS tool for non-randomized studies.
Results
Search yield
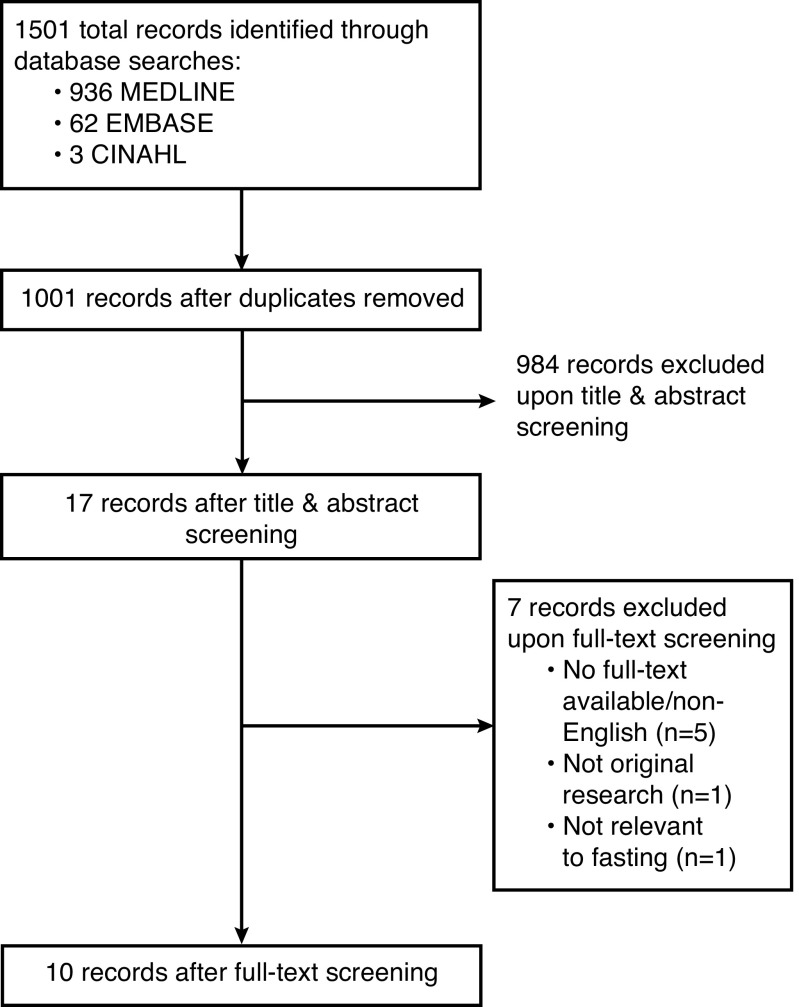
Results of the study screening process are available in the PRISMA diagram (Fig. 1). Of the 1501 original database citations, 500 total duplicates were removed. After title and abstract screening, 17 were eligible for full-text evaluation. After a hand-search of relevant journals and citations, no additional studies were added. Of the 17 full-text articles, a total of 10 were included in this systematic review.
Fig. 1.
PRISMA diagram of study screening process.
Inter-rater reliability for study screening for abstract and full-text screening was 99.2% and 94.0%, respectively. The authors were in substantial agreement, with a calculated κ of 0.73 for abstract screening and 0.88 for full-text.
Article characteristics
Details of the included studies are outlined in Table 2.
Table 2.
Details of included studies
| Citation, country | Study design | Type of fasting | Sample size | Mean age (SD) | Sex (M/F) | Summary of key outcome |
|---|---|---|---|---|---|---|
| Abdolreza 2011, Iran27 | Prospective observational | Ramadan | 610 | 37.6 | 441/169 | Admissions due to renal colic were higher during the first two weeks of Ramadan (p<0.05) |
| Al Assaad 2018, Lebanon28 | Prospective observational | Ramadan | 3536 | 54.1 | 2041/1495 | No change in renal colic incidence in Ramadan months (p=0.615) |
| Al-Hadramy 1997, Saudi Arabia22 | Retrospective | Ramadan | NR | NR | All male | No change in renal colic incidence in Ramadan months (p=0.223) |
| Al Mahayni 2018, Saudi Arabia20 | Retrospective observational | Ramadan | 237 | 45.8 | 178/59 | No change in renal colic incidence in Ramadan months (p=0.599) |
| Basiri 2004, Iran23 | Retrospective observational | Ramadan | 574 | 36.4 | 398/173 | No change in renal colic incidence in Ramadan months (p=0.32) |
| Cevik 2016, Pakistan24 | Prospective observational | Ramadan | 176 | 40.5 | 112/64 | Fasting in Ramadan does not change the number of renal colic visits, although fasting during Ramadan was associated with increased urine density and decreased WBC count |
| Habib 2014, U.S.25 | Prospective observational | Ramadan | 43 | 51 | 41:2 | No significant difference between groups fasting and not fasting for renal stone incidence (0 stones in cohort) |
| Hodgkinson et al26 | Prospective observational | Fasting for 12 hours | 156 | 20–55 | All male | Lower uric acid levels were found in healthy patients |
| Miladipour et al19 | Prospective observational | Ramadan | 57 | 30–55 | All male | Urine biochemistry varied significantly during fasting with decrease in the concentration of certain electrolytes (calcium, phosphate, magnesium) while certain electrolytes increased (uric acid, and potassium). These biochemistry changes were similar between recurrent calculus formers and participants with no history of renal colic, with the exception of serum sodium, which was significantly lower in the calculus former group while fasting. However, this did not translate into increased risk of calculus formation during fasting for either group |
| Sagy et al21 | Retrospective | Ramadan | 4517 | 37.9 | 3446/1071 | There was an increase in renal colic related ED visits during the first 2 weeks of Ramadan (RR 1.267, 95% CI 1.031–1.502) among Muslims but not among Jews (1.061, 95% CI 0.885–1.238) |
CI: confidence interval; ED: emergency department; RR: relative risk; SD: standard deviation; WBC: white blood cell.
All 10 articles were observational studies, with the majority (6/10) prospective in nature and the remaining four (4/10) retrospective. The majority (9/10) of the included studies were specific to fasting during Ramadan, a Muslim holy month that involves abstinence from food and water during daytime hours.2 The remaining study was a plasmic and uric acid level study of men after a single fast for 12 hours.19 There were no studies related to intermittent fasting or other weight loss diets.
The majority of studies were located in the Middle East (n=7), with the remainder located in Pakistan (n=1), the U.S. (n=1), and England (n=1).
Our systematic review includes the results of 9906 fasting participants, with an average sample size of 1111 per study. Three studies included only male participants.19–21
Details of the risk of bias for each study are provided in Table 3. Four studies were graded as low-risk of bias, while six studies were graded as intermediate-to high-risk. Studies were graded down due to bias in participation selection, confounding due to temperature/seasonal variation, and potential for missing data.
Table 3.
Risk of bias assessment
| Study | Year | Participant selection | Confounding | Measurement of exposure | Blinding | Incomplete outcome data | Total |
|---|---|---|---|---|---|---|---|
| Abdolreza et al27 | 2011 | 1 | 1 | 1 | 1 | 1 | 5 |
| Al Assaad et al28 | 2018 | 2 | 1 | 2 | 1 | 1 | 7 |
| Al-Hadramy et al22 | 1997 | 1 | 1 | 2 | 1 | 1 | 6 |
| Al Mahayni et al20 | 2018 | 1 | 1 | 2 | 1 | 1 | 6 |
| Basiri et al23 | 2004 | 1 | 1 | 2 | 1 | 1 | 6 |
| Cevik et al24 | 2016 | 2 | 2 | 2 | 1 | 1 | 8 |
| Habib et al25 | 2014 | 1 | 1 | 1 | 1 | 1 | 5 |
| Hodgkinson et al26 | 1976 | 1 | 1 | 1 | 1 | 1 | 5 |
| Miladipour et al19 | 2012 | 1 | 1 | 1 | 1 | 1 | 5 |
| Sagy et al21 | 2017 | 2 | 2 | 2 | 1 | 1 | 8 |
Adapted from the RoBANS tool.39 A score of “1” indicates low-risk, “2” indicates high-risk, and “0’ is unclear.
Outcomes
Nine studies examined the incidence of renal colic or renal stones in relation to the month of Ramadan. There were contrasting results regarding the outcomes. The majority (n=7) of studies found that the risk of renal colic did not differ in non-Ramadan months or among non-fasters.20–26 Emergency department visits related to renal colic were often used to calculate the number of renal stone diagnoses. One study specifically assessed the impact of fasting on patients with a diagnosis of gout, finding that there were no significant differences in the incidence of either gout arthritic flares or renal colic.26
However, two studies noted that there was a significant increase (p<0.05) in emergency department visits related to renal colic during the first two weeks of Ramadan.21,27 Specifically, Sagy et al found that the increase in renal colic visits was significantly higher among Muslim patients, and that this association did not exist among non-Muslim patients.21 In both studies, temperature was controlled for either through statistical adjustment or between-group comparisons. This is an important consideration, as three other studies, Al Mahayni et al, and Al-Hadramy et al, and Basiri et al, noted that higher ambient temperatures were significantly associated with the number of renal stone admissions, regardless of the presence of fasting.20,22,23
Four studies examined metabolites and biomarkers related to fasting and renal stones. Miladipour et al found that urine biochemistry altered significantly with fasting during Ramadan in comparison to a period before fasting.19 The authors noted decreased concentration of calcium, phosphate, and magnesium with increased concentration of uric acid, sodium, and potassium. These biochemistry changes did not translate into increased risk of calculus formation during fasting and were noted to be largely similar between recurrent calculus formers and participants with no history of renal colic. Similarly, Cevik et al found that Ramadan fasting increased urine density in comparison to the non-fasting period, though did not increase the number of renal stone admissions visits.24 Habib et al found no significant changes in urea or creatinine in fasters with gout, as well as no change in renal stone incidence, in comparison to prior to fasting.25
Hodgkinson et al was the only study that examined potential markers for stone formation outside of the context of Ramadan.26 Twelve healthy men were asked to fast for 12 hours, which significantly reduced plasma uric acid levels (p<0.001) in comparison to a control group. The authors, therefore, suggested that fasting plays a minimal role in renal stone formation, and that purine-rich foods may play a much larger role. However, purine-rich diets were not studied and this association was made after a single fast of 12 hours.
Discussion
To date, this is the first systematic assessment of literature regarding fasting and renal stones. Due to the varied reporting styles of the studies, as well as the limited evidence base, we were unable to complete a meta-analysis on the reported outcomes. Ten studies with a total of 9906 participants were included, with participants either fasting or living in a country where fasting was a dominant cultural norm. Nine of the studies were conducted in the context of Islamic fasting during Ramadan, with the majority finding that renal colic incidence was unaffected by the month of fasting. In contrast, two studies noted an increased incidence among fasting populations. Two other studies noted that urine metabolites and density were altered with fasting; however, in those studies, the metabolite change did not translate into clinical outcomes.
Ultimately, there is limited evidence to suggest that fasting increases the risk of kidney stone formation. Still, physicians should continue to advise fasting patients to monitor water consumption to avoid dehydration. According to current guidelines, patients should attempt to produce 2.5 L of urine output per day, particularly if they have risk factors related for renal stone formation.28 While fasting may limit the timing of water consumption, efforts can still be made to ensure adequate intake. Discussion of other risk factors, such as family history, should be included in counselling.29
Our research aligns well with the current literature base related to fasting. Previous studies have noted that fasting during Ramadan is safe for patients with chronic kidney disease, as well as renal transplant patients one year post-transplant. 30,31 Other studies have shown that fasting does not demonstrate adverse effects in patients with either type I or type II diabetes.32,33 Most religions exempt fasting for participants who are sick, pregnant, or lactating.34,35 However, it is important to note that there is limited robust clinical evidence on the long-term outcomes of intake restriction.36
As such, it is important to note several limitations of this systematic review. First, almost all studies were conducted in the context of Ramadan, with several studies limited to only men. This limits the generalizability of our findings. Second, only four studies controlled for ambient temperature, which is significantly associated with renal stone formations. Third, there were no studies that directly compared whether history of renal stones correlated with increased stone incidence while fasting. Finally, most studies were retrospective in design, rather than prospectively following a cohort. Therefore, studies may be subject to publication bias, particularly if criticisms of fasting are against cultural or social norms.37,38 Cultural and social norms may also limit the accuracy of self-reported fasting habits, as participants may feel pressured to conform. Studies should ensure that data is collected in a non-judgmental manner and with full anonymity.
Included studies would be strengthened by evaluating the amount of water consumed per day. For example, for fasters who follow Ramadan, water consumption is permitted before sunrise and after sunset. This may vary significantly between participants and influence outcomes. Further research is needed to determine if the timing of water intake plays a role in renal stone formation independent of total water consumption.
Strengths of our review include the systematic search of three databases using a broad search strategy. Previous reviews have only conducted narrative assessments based on limited searching and inclusion criteria. In addition, our title and abstract screening was conducted in duplicate with two independent reviewers and high inter-rater agreement, which minimized the possibility of missed studies. In contrast to a non-systematic literature review, our synthesis was able to best characterize the breadth of the research while minimizing narrative biases.
The findings of this systematic review highlight three areas of future research. First, interventional trials with a control group are needed to provide high-quality evidence into the risks of fasting in relation to renal stones. Second, both metabolite biomarkers and clinical outcomes should be included in future study designs. This may elucidate the biochemical mechanism linking fasting with renal stone formation. Finally, variations in fasting patterns, such as intermittent fasting or fasting for consecutive days, should also be evaluated. This will be particularly relevant given the uptake of fasting for weight loss among the general public. While our search yielded only one study related to fasting outside of the context of Ramadan, we hope to highlight the need for additional research in this field.
Conclusions
Based on the available evidence, it is unlikely that fasting significantly increases the risk of renal stones. Physicians should counsel higher-risk patients on safe fasting practices. Further high-quality research is required to examine different fasting patterns and fasting in populations at high risk for renal stone formation.
Supplementary Information
Supplementary Table 1.
Search strategy (adapted for Embase and CINAHL)
| # | Searches |
|---|---|
| 1 | ((renal OR kidney OR urin*) adj1 (stone* or calcul* or colic*)).ti,ab. |
| 2 | (nephrolith* OR urolithiasis*).ti,ab. |
| 3 | 1 OR 2 |
| 4 | (fast* OR Ramadan*).ti,ab. |
| 5 | 3 AND 4 |
Database: Ovid MEDLINE: Epub ahead-of-print, in-process, and other non-indexed citations from Ovid MEDLINE® Daily and Ovid MEDLINE® 1946 to March 18, 2020.
Footnotes
Competing interests: The authors report no competing personal or financial interests related to this work.
This paper has been peer-reviewed.
References
- 1.Persynaki A, Karras S, Pichard C. Unraveling the metabolic health benefits of fasting related to religious beliefs: A narrative review. Nutrition. 2017;35:14–20. doi: 10.1016/j.nut.2016.10.005. [DOI] [PubMed] [Google Scholar]
- 2.Venegas-Borsellino C, Martindale RG. From religion to secularism: the benefits of fasting. Curr Nutrit Reports. 2018;7:131–8. doi: 10.1007/s13668-018-0233-2. [DOI] [PubMed] [Google Scholar]
- 3.McKnight S. Bahai.org. Fasting. USA: Phyllis tickle; 2010. [Accessed Aug. 7, 2020]. Fasting: The ancient practices. The ancient practices. Available at: https://www.bahai.org/beliefs/life-spirit/devotion/fasting. [Google Scholar]
- 4.Julka S, Sachan A, Bajaj S, et al. Glycemic management during Jain fasts. Ind J Endocrin Metabol. 2017;21:238. doi: 10.4103/2230-8210.192489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Peel M. Hunger strikes: Understanding the underlying physiology will help doctors provide proper advice. BMJ. 1997;315:829–30. doi: 10.1136/bmj.315.7112.829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mattson MP, Wan R. Beneficial effects of intermittent fasting and caloric restriction on the cardiovascular and cerebrovascular systems. J Nutrit Biochem. 2005;16:129–37. doi: 10.1016/j.jnutbio.2004.12.007. [DOI] [PubMed] [Google Scholar]
- 7.Dyson P. Popular diets: Are they effective for people with type 2 diabetes? Pract Diab. 2014;31:187–92. doi: 10.1002/pdi.1863. [DOI] [Google Scholar]
- 8.Golbidi S, Daiber A, Korac B, et al. Health benefits of fasting and caloric restriction. Curr Diab Rep. 2017;17:123. doi: 10.1007/s11892-017-0951-7. [DOI] [PubMed] [Google Scholar]
- 9.Michalsen A. Prolonged fasting as a method of mood enhancement in chronic pain syndromes: A review of clinical evidence and mechanisms. Curr Pain Headache Rep. 2010;14:80–7. doi: 10.1007/s11916-010-0104-z. [DOI] [PubMed] [Google Scholar]
- 10.Borghi L, Meschi T, Schianchi T, et al. Urine volume: Stone risk factor and preventive measure. Nephron. 1999;81:31–7. doi: 10.1159/000046296. [DOI] [PubMed] [Google Scholar]
- 11.Embon OM, Rose GA, Rosenbaum T. Chronic dehydration stone disease. Br J Urol. 1990;66:357–62. doi: 10.1111/j.1464-410X.1990.tb14954.x. [DOI] [PubMed] [Google Scholar]
- 12.Walters D. Stress as a principal cause of calcium oxalate urolithiasis. Int Urol Nephrol. 1986;18:271–5. doi: 10.1007/BF02082713. [DOI] [PubMed] [Google Scholar]
- 13.Kalaitzidis RG, Damigos D, Siamopoulos KC. Environmental and stressful factors affecting the occurrence of kidney stones and the kidney colic. Int Urol Nephrol. 2014;46:1779–84. doi: 10.1007/s11255-014-0758-2. [DOI] [PubMed] [Google Scholar]
- 14.Curhan GC, Curhan SG. Dietary factors and kidney stone formation. Comprehens Ther. 1994;20:485–9. [PubMed] [Google Scholar]
- 15.Emami-Naini A, Roomizadeh P, Baradaran A, et al. Ramadan fasting and patients with renal diseases: A mini review of the literature. J Res Med Sci. 2013;18:711. [PMC free article] [PubMed] [Google Scholar]
- 16.Shamsa A. Fasting and urinary stones. J Fasting Health. 2013;1:85–9. [Google Scholar]
- 17.Moher D, Shamseer L, Clarke M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4:1. doi: 10.1186/2046-4053-4-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chapter 11: Systematic Reviews – Introduction JBI Reviewer’s Manual – JBI GLOBAL WIKI [Internet] [Accessed March 30, 2020]. Available at: https://wiki.joannabriggs.org/display/MANUAL/1.1+Introduction+to+JBI+Systematic+reviews.
- 19.Miladipour AH, Shakhssalim N, Parvin M, et al. Effect of Ramadan fasting on urinary risk factors for calculus formation. Iran J Kidney Dis. 2012;6:33–8. [PubMed] [Google Scholar]
- 20.Al Mahayni AO, Alkhateeb SS, Abusaq IH, et al. Does fasting in Ramadan increase the risk of developing urinary stones? Saudi Med J. 2018;39:481. doi: 10.15537/smj.2018.5.22160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sagy I, Zeldetz V, Halperin D, et al. The effect of Ramadan fast on the incidence of renal colic emergency department visits. QJM. 2017;110:571–6. doi: 10.1093/qjmed/hcx079. [DOI] [PubMed] [Google Scholar]
- 22.Al-Hadramy MS. Seasonal variations of urinary stone colic in Arabia. J Pakistan Med Assoc. 1997;47:281–3. [PubMed] [Google Scholar]
- 23.Basiri A, Moghaddam SM, Khoddam R, et al. Monthly variations of urinary stone colic in Iran and its relationship to the fasting month of Ramadan. J Pakistan Med Assoc. 2004;54:6–7. [PubMed] [Google Scholar]
- 24.Cevik Y, Corbacioglu SK, Cikrikci G, Oncul V, Emektar E. The effects of Ramadan fasting on the number of renal colic visits to the emergency department. Pak J Med Sci. 2016;32:18. doi: 10.12669/pjms.321.8248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Habib G, Badarny S, Khreish M, et al. The impact of Ramadan fast on patients with gout. J Clin Rheum. 20:353–6. doi: 10.1097/RHU.0000000000000172. 201. [DOI] [PubMed] [Google Scholar]
- 26.Hodgkinson A. Uric acid disorders in patients with calcium stones. Br J Urol. 1976;48:1–5. doi: 10.1111/j.1464-410X.1976.tb02729.x. [DOI] [PubMed] [Google Scholar]
- 27.Abdolreza N, Omalbanin A, Mahdieh TS, et al. Comparison of the number of patients admitted with renal colic during various stages of peri-Ramadan month. Saudi J Kid Dis Transplant. 2011;22:1199. [PubMed] [Google Scholar]
- 28.Al Assaad RG, Bachir R, El Sayed MJ. Impact of Ramadan on emergency department visits and on medical emergencies. Eur J Emerg Med. 2018;25:440–4. doi: 10.1097/MEJ.0000000000000485. [DOI] [PubMed] [Google Scholar]
- 29.Krieger JN, Kronmal RA, Coxon V, et al. Dietary and behavioral risk factors for urolithiasis: Potential implications for prevention. Am J Kidney Dis. 1996;28:195–201. doi: 10.1016/S0272-6386(96)90301-7. [DOI] [PubMed] [Google Scholar]
- 30.Bragazzi NL. Ramadan fasting and chronic kidney disease: A systematic review. J Res Med Sci. 2014;19:665–76. [PMC free article] [PubMed] [Google Scholar]
- 31.Bernieh B, Mohamed AO, Wafa A. Ramadan fasting and renal transplant recipents: Clinical and biochemical effects. Saudi J Kidney Dis Transpl. 1994;5:470–3. [PubMed] [Google Scholar]
- 32.Khogeer Y, Siliman MI, Al Fayez SF. Ramadan fasting and diabetes, safety, and state of control. Ann Saudi Med. 1987;7:6–7. [Google Scholar]
- 33.Bekhadir J, El Ghomari H, Klicken N, et al. Muslims with non-insulin diabetes fasting during Ramadan: Treatment with glibenclamide. Br Med J. 1993;307:292–5. doi: 10.1136/bmj.307.6899.292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Setrakian HV, Rosenman MB, Szucs KA. Breastfeeding and the Bahá’í faith. Breastfeed Med. 2011;6:221–5. doi: 10.1089/bfm.2010.0098. [DOI] [PubMed] [Google Scholar]
- 35.Bajaj S, Khan A, Fathima FN, et al. South Asian consensus statement on women’s health and Ramadan. Ind J Endocrinol Metab. 2012;16:508. doi: 10.4103/2230-8210.97995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Horne BD, Muhlestein JB, Anderson JL. Health effects of intermittent fasting: Hormesis or harm? A systematic review. Am J Clin Nutr. 2015;102:464–70. doi: 10.3945/ajcn.115.109553. [DOI] [PubMed] [Google Scholar]
- 37.Schielke S. Being good in Ramadan: Ambivalence, fragmentation, and the moral self in the lives of young Egyptians. J Royal Anthropol Inst. 2009;15:S24–40. doi: 10.1111/j.1467-9655.2009.01540.x. [DOI] [Google Scholar]
- 38.Ilkilic I, Ertin H. Ethical conflicts in the treatment of fasting Muslim patients with diabetes during Ramadan. Med Health Care Philos. 2017;20:561–70. doi: 10.1007/s11019-017-9777-y. [DOI] [PubMed] [Google Scholar]
- 39.Kim SY, Park JE, Lee YJ, et al. Testing a tool for assessing the risk of bias for non-randomized studies showed moderate reliability and promising validity. J Clin Epidemiol. 2013;66:408–14. doi: 10.1016/j.jclinepi.2012.09.016. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Table 1.
Search strategy (adapted for Embase and CINAHL)
| # | Searches |
|---|---|
| 1 | ((renal OR kidney OR urin*) adj1 (stone* or calcul* or colic*)).ti,ab. |
| 2 | (nephrolith* OR urolithiasis*).ti,ab. |
| 3 | 1 OR 2 |
| 4 | (fast* OR Ramadan*).ti,ab. |
| 5 | 3 AND 4 |
Database: Ovid MEDLINE: Epub ahead-of-print, in-process, and other non-indexed citations from Ovid MEDLINE® Daily and Ovid MEDLINE® 1946 to March 18, 2020.