Abstract
Background.
Healthy retail interventions are a recommended intervention strategy to address diet-related diseases, such as obesity and diabetes; however, retail managers are concerned about their bottom line. This study’s aim was to assess the impact of a healthy retail intervention on fruits and vegetables (FV) sales, as well as total sales, in tribally owned convenience stores where grocery stores are scarce.
Method.
We analyzed weekly sales data over the first 6 months of a healthy retail intervention. We assessed the proportion of sales from two FV baskets. The FV basket included all fresh, canned, and dried FV sold at stores; while the fruits, vegetables, and salads (FVS) basket included all FV items as well as all salads sold. We compared mean weekly sales rates in intervention and control stores over the 6-month period using generalized estimating equations models to account for repeated measures.
Results.
Mean weekly FV basket sales rates were higher in intervention stores than control stores in both Nations. Mean weekly FVS baskets sales were significantly higher in intervention stores than control stores in one Nation and were higher, but not statistically significant, in intervention stores in the other Nation. Total sales remained steady throughout the intervention period.
Conclusions.
The THRIVE (Tribal Health and Resilience in Vulnerable Environments) intervention increased FV sales without negatively affecting total sales. Policy and Practice Implications. Healthy retail interventions in tribal convenience stores, where many Native Americans living in rural areas shop due to scarcity of grocery stores, could improve diet-related disparities without reducing total sales.
Keywords: obesity, chronic disease, Native American/American Indian, minority health, nutrition, community intervention, consumer health, health promotion, community-based participatory research, health research
➤BACKGROUND
Healthy retail interventions are a recommended strategy to address the increasing prevalence of obesity, diabetes, and hypertension in the United States. Such interventions use the social-ecological model as a conceptual framework to improve access to healthy foods in a variety of community environments including convenience stores, grocery stores, and school cafeterias (Curran et al., 2005; Gittelsohn et al., 2012; Glanz et al., 2016). While evidence indicates that healthy retail interventions have increased knowledge and availability of healthy foods, as well as the frequency of healthy food purchases among individual shoppers (Gittelsohn et al., 2012; Jernigan et al., 2018; Mhurchu et al., 2010), retail managers want to ensure that store sales will not be adversely affected when healthy foods are promoted (Gittelsohn et al., 2014). Furthermore, a systematic review of barriers and facilitators to implementing healthy retail interventions found that retail managers are key to effective implementation and sustainability of healthy retail interventions but perceive unhealthy products to be more profitable (Middel et al., 2019). Furthermore, Martinez et al. (2018) found from in-depth interviews that food retailers have a high degree of autonomy and an interest in healthy retail interventions; however, they are concerned about the financial bottom line, which is driven by sales, and they perceive customers want unhealthy items based on special requests. Working with retail store managers is key to implementing healthy retail interventions, but health promotion practitioners need evidence that providing healthy foods does not affect store sales. However, few studies have examined the impact of healthy retail interventions on store sales with actual sales data (Foster et al., 2014; Simpson et al., 2018; Song et al., 2009). Foster et al. (2014) found that weekly grocery store sales of some promoted foods increased in intervention stores compared to control stores, and Song et al. (2009) found urban corner store sales increased for a few promoted food items in intervention stores compared to control stores. Another study found that the proportion of sales of healthier options to total sales in a hospital shop increased following the intervention (Simpson et al., 2018). Some studies reported sales following healthy retail interventions in urban, non-Native communities; however, only one study assessed the impact of a healthy retail intervention on sales in a tribal grocery store in the United States (Gustafson et al., 2018), and an Australian study examined sales data in rural stores managed by the Arnhem Land Progress Aboriginal Corporation (Brimblecombe et al., 2017). Tribally owned and operated convenience stores frequently serve as a substantial source of food for many Native Americans (NAs) where grocery stores are scarce (Love et al., 2019). To our knowledge, no studies have assessed the effects of healthy retail interventions on sales in rural, tribal convenience stores in the United States.
Food deserts, places with no or limited food availability (Smith & Morton, 2009), are prominent in rural NA communities where access to nonconvenience stores (e.g., grocery stores and supermarkets) is scarce (Kaufman et al., 2014). Data from a focus group study conducted in Chickasaw Nation and Choctaw Nation of Oklahoma showed that most tribal members (56%) reported living more than 10 miles from a supermarket or grocery store (Love et al., 2019). Furthermore, almost two thirds of participants in this study (65%) reported shopping for food at least once per week at convenience stores (Love et al., 2019).
Convenience stores, retail establishments that provide convenient locations to quickly purchase food and gasoline, are an important and growing source of economic development for many Native American Nations (Robinson, 2014), especially in rural areas. In 2014, 180 Native Nations owned 293 convenience stores across 25 states, and the number is increasing (Robinson, 2014). Tribally owned and operated convenience stores are similar to nontribally owned convenience stores in terms of size, scope, and products sold. While convenience stores are not intended to replace grocery stores and supermarkets, our survey of over 500 NA adults living within rural Chickasaw and Choctaw Nations of Oklahoma found that 65% reported shopping for food at tribally owned convenience stores one or more times per week (Jernigan et al., 2018). Hence, healthy retail interventions in tribally owned and operated convenience stores could significantly improve nutrition in NA communities.
Few healthy retail interventions have been implemented in stores in NA communities (Brimblecombe et al., 2017; Gittelsohn et al., 2012). Gittelsohn and colleagues conducted a healthy foods intervention in grocery stores in the Navajo and Apache reservations (Curran et al., 2005; Gittelsohn et al., 2013), while others have conducted healthy intervention research in First Nations communities in Canada (Ho et al., 2008; Mead et al., 2010) and in indigenous communities in Australia (Brimblecombe et al., 2017). The interventions were similar and included cooking demonstrations, promotion of healthy items, and educational information at the point of purchase. These interventions demonstrated an increase in self-reported knowledge and healthy food purchasing (Curran et al., 2005; Gittelsohn et al., 2013; Ho et al., 2008; Mead et al., 2010). However, study investigators cited that limitations in widespread adoption of the interventions, including lack of convenience, minimal engagement with tribal policy makers, and financial difficulties, may limit small stores’ ability to purchase new foods (Curran et al., 2005; Gittelsohn et al., 2013). Furthermore, a review of multiple healthy retail studies reported store owners and managers perceived lack of customer demand for and potential revenue loss with healthy retail interventions (Gittelsohn et al., 2014). Sales data analyses of healthy retail interventions could help public health professionals and health promotion program planners communicate with store managers and engage tribal leadership to design effective healthy retail interventions to improve fruits and vegetables (FV) sales while maintaining overall sales. Although the literature has identified that engaging retail store managers is crucial to effectively implement and sustain healthy retail interventions (Martinez et al., 2018; Middel et al., 2019), more evidence is needed to show store managers their sales will not diminish when healthy options are offered.
➤AIMS
The Tribal Health and Resilience in Vulnerable Environments or “THRIVE” study is a community-based participatory research study that developed and tested a healthy retail intervention in tribally owned and operated convenience stores in the Chickasaw Nation and the Choctaw Nation of Oklahoma (Jernigan et al., 2019). According to the U.S. Census Bureau’s (2011) County Business Patterns, Chickasaw Nation jurisdictional area is 7,270 square miles with approximately 29 grocery stores and four supermarkets, while Choctaw Nation of Oklahoma has a jurisdictional area of 10,602 square miles (~15% of the area of Oklahoma), with 44 grocery stores and six supermarkets (U.S. Census Bureau, 2011).
Implemented between May 2016 and May 2017, the THRIVE study found that participants perceived a healthier food environment postintervention and those who shopped at the stores more frequently reported purchasing healthy foods more often (Jernigan et al., 2018). As part of the THRIVE study we collected weekly sales data from intervention and control stores participating in the study. Here we report the impact of the THRIVE intervention on total sales and sales of FV, the primary healthy foods targeted in the THRIVE intervention. We also examine differences in sales patterns between convenience stores that received the intervention (intervention stores) and those that did not (control stores).
➤METHOD
Setting and Context
The Chickasaw Nation and Choctaw Nation of Oklahoma are among the largest sovereign Native American Nations in the United States (U.S. Census Bureau, 2015; Figure 1). Each Nation owns and operates more than a dozen convenience stores. Stores were selected with community partner input based on similar locations and populations served (Jernigan et al., 2018). Although these tribal convenience stores are similar to nontribal convenience stores, some differences exist. For example, all convenience stores are owned and operated by the Tribal Nations, employees are employed by the Tribal Nations, and all revenue generated is used for operations, health, and social service initiatives across the Nations. In addition, while the tribal convenience stores sell widely marketed commercial food and snacks, they also sell tribally produced food (e.g., canned jams, pickled eggs, pecans) and art. Finally, tribal citizens receive a discount on all purchases made within the stores.
Figure 1.
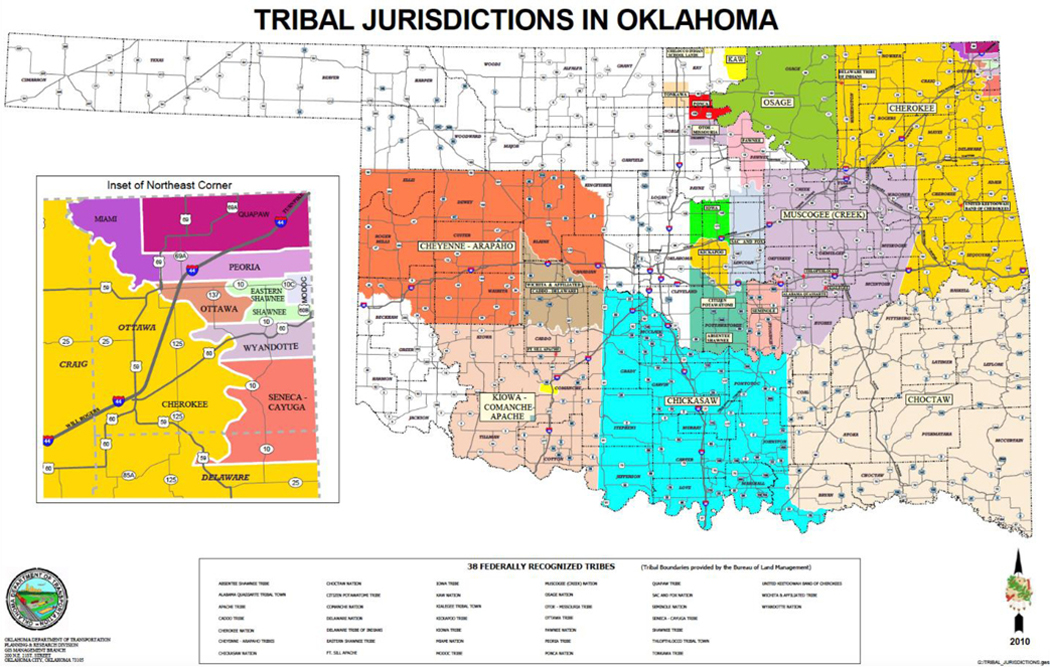
Oklahoma Map of Tribal Jurisdictional Areas, created by Oklahoma Department of Transportation.
THRIVE Intervention and Trial Design
The THRIVE healthy retail intervention was designed to increase availability, variety, and convenience of ready-to-eat FV using the four Ps framework of product, placement, promotion, and pricing of healthy foods throughout the stores, which has been described in more detail previously (Jernigan et al., 2019). In each Nation, two tribal convenience stores received the intervention while two other tribal convenience stores served as controls (total n = 8). Both Nations identified multiple FV items, including fresh and canned, and salads to promote in their intervention stores during the intervention period. Fresh fruits, vegetables, and salads (FVS) were placed in large open-air coolers in view of store entrances, while signage promoted all types of FVS throughout the intervention stores. The primary pricing strategies focused on offering healthy meals (e.g., salads) and healthy snacks (e.g., FV cups) at or below prices of competing foods, such as higher fat sandwiches or higher fat snacks. This cluster control trial, initially planned for 6 months, was extended to 9 months in Nation A and 12 months in Nation B based on availability of funds and staffing. As part of the THRIVE study, staff conducted regular store site visits to ensure products were available and their placement and promotion followed the intervention protocol (Taniguchi et al., 2020). Detailed methods of the intervention (Jernigan et al., 2019), primary outcomes (Jernigan et al., 2018), and process measures (Taniguchi et al., 2020) have been previously published.
Sales Data Source
The tribal commerce divisions of each Nation extracted weekly sales data for all items, except tobacco and alcohol, sold at each intervention and control store. Extracted weekly sales data over the first 6 months of the intervention in both Nations were provided to the data analysis team by store. Although the intervention for this trial was extended past the initial 6-month period, extraction of weekly sales data was not extended past this initial 6-month period due to funding, logistics of extracting sales data, and commerce division staff time limitations.
Fruit and Vegetable Baskets
In order to assess sales related to the main THRIVE outcome of increasing availability and consumption of FV, we combined all FV into “baskets” similar to previous studies (Crawford et al., 2017), then assessed the proportion of FV sales to total sales. We developed two baskets to assess FV sales at the intervention and control stores during the initial 6-month intervention period for both Nations. We defined one basket as an FV basket, which included all fresh, canned, and dried fruits, as well as all fresh, canned, and dried vegetables sold at the stores. The second basket was an FVS basket, which included all items in the FV basket and any salads sold at the stores.
Statistical Analyses
As conducted in previous studies, we estimated proportional weekly sales rates for each type of FV basket (Närhinen et al., 1998; Simpson et al., 2018). Weekly sales rates for a basket were defined as the proportion of weekly sales for the basket out of total weekly sales in the store. The weekly sales rates for all intervention (control) stores for an FV or FVS basket in a tribal Nation was defined as the proportion of the sum of weekly sales for the FV or FVS basket across all intervention (control) stores in the Nation to the sum of total weekly sales from all intervention (control) stores in the Nation. Weekly sales rates are expressed in dollars per $1,000 of total sales. Generalized linear regression models with an Autoregressive Order 1, AR(1), covariance (Liang & Zeger, 1986) were used for these longitudinal data to estimate mean weekly sales rates for each type of FV basket and to assess the difference in mean weekly sales rates between intervention stores and control stores while adjusting for weekly variations of repeated weekly sales rates assuming these repeated weekly sales rates correlate with an AR(1) covariance structure. For example, for a generalized linear regression model to estimate mean of weekly FV sales rate, the weekly FV sales rate is dependent variable, with repeated weekly sales rates assumed to correlate with an AR(1) covariance structure. SAS Version 9.4 was used for all statistical analyses with a p < .05 considered statistically significant.
➤RESULTS
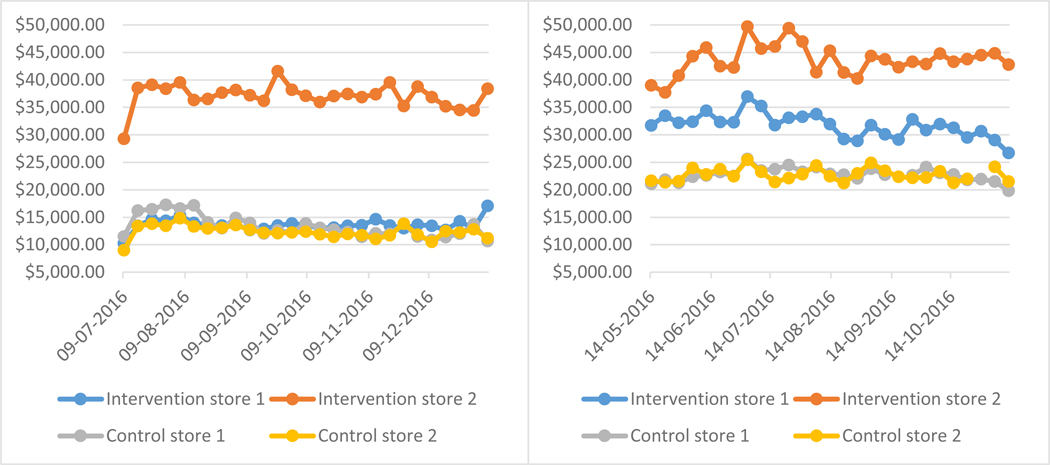
During the first 6 months of the intervention, sales data were provided for 26 weeks for all Nation A intervention and control stores, 26 weeks for Nation B intervention stores, and 25 weeks for Nation B control stores. Total weekly sales remained relatively steady in each store throughout the first 6 months of the intervention period (Figures 2a and b). In Nation A, one intervention store had higher total weekly sales than the other three stores (Figure 2a), and in Nation B both intervention stores had higher total weekly sales than control stores (Figure 2b).
Figure 2.
Total weekly sales for intervention and control stores in Nation A (left side) and Nation B (right side) for the first six months of the intervention, 7/9/2016-1/7/2017 for Nation A and 5/14/2016-11/12/2016 for Nation B.
Weekly Sales of Fruits and Vegetables in Intervention Versus Control Stores
During the first 6 months of the intervention in Nation A, the mean weekly sales rate of the FV basket was significantly higher for intervention stores than control stores ($6.47 vs. $3.88 per $1,000; p = .0023; Table 1). Similarly, during the first 6 months of the intervention in Nation B, the mean weekly sales rate of the FV basket was significantly higher in intervention stores ($5.10 vs. $2.80 per $1,000; p < .0001; Table 1). When salads were added to the FV basket, the mean FVS basket weekly sales rate was significantly higher in intervention stores compared to control stores in Nation B ($9.22 vs. $4.18 per $1,000; p < .0001) and was higher, but not statistically significant, in intervention stores in Nation A ($8.15 vs $5.76 per $1,000; p = .07428; Table 1).
TABLE 1.
Weekly Sales Rate of Two Fruit and Vegetable Market Baskets in Intervention Stores and Two Control Storesa and Differences in Sales Rates Between Intervention and Control Stores, First 6 Months of the Intervention: 2016
| Market basket | Food items included | Store | Mean weekly sales ratea | Comparison | Difference in mean weekly salesa,b [95% CI] | p |
|---|---|---|---|---|---|---|
|
| ||||||
| Nation A | ||||||
| FV market basket | Fruits and vegetables | Intervention | $6.47 | Intervention vs. control | $2.59 [0.92, 4.25] | .002341 |
| Control | $3.88 | |||||
| FVS market basket | Fruits, vegetables and salads | Intervention | $8.15 | Intervention vs. control | $2.39 [−0.23, 5.02] | .07428 |
| Control | $5.76 | |||||
| Nation B | ||||||
| FV market basket | Fruits and vegetables | Intervention | $5.10 | Intervention vs. control | $2.29 [1.31, 3.28] | <.0001 |
| Control | $2.80 | |||||
| FVS market basket | Fruits, vegetables and salads | Intervention | $9.22 | Intervention vs. control | $5.04 [3.20, 6.87] | <.0001 |
| Control | $4.18 | |||||
Note. FV = fruits and vegetables; FVS = fruits, vegetables, and salads. Bold text indicates statistically significant differences in mean weekly sales.
Weekly sales rates are expressed in dollars per $1,000 in total sales. Weekly sales rates for all intervention (control) stores for a market basket in a Tribal Nation was defined as the proportion of the sum of weekly sales for the market basket across all intervention (control) stores in the Nation to the sum of total weekly sales from all intervention (control) stores in the Nation. Mean sales rates are the mean of the weekly sales rates over the first 6-month intervention period.
Difference in mean weekly sales rates is defined as the “mean weekly sales rate across all intervention stores in the Nation minus the mean weekly sales rate across all control stores in the Nation.”
Weekly Sales Over Time
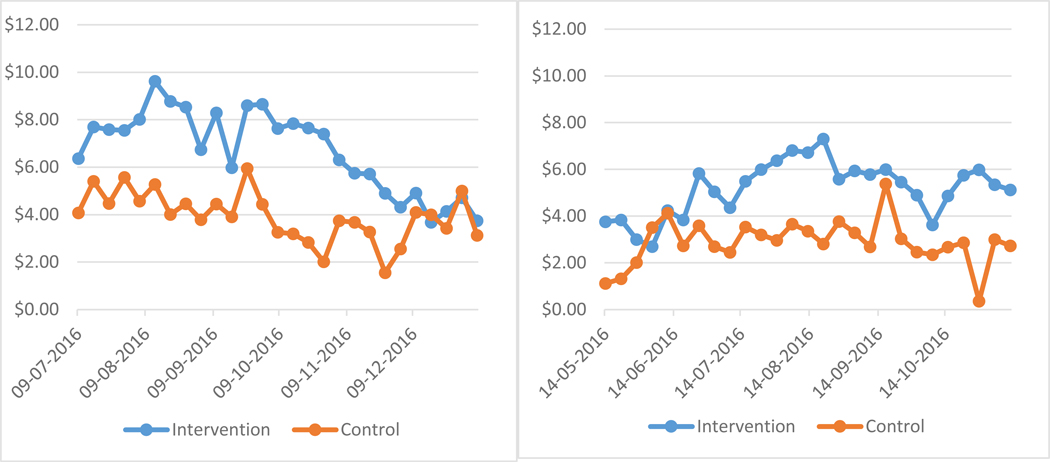
There was some weekly variation in the FV basket sales rates in all stores in both Nations (Figures 3a and b) with some differences by Nation. In Nation A, the FV basket sales were higher in the intervention stores than the control stores for the first 3 months of the intervention, and then FV sales rates began to decline in all stores. However, in the fourth month the intervention store FV basket sales rate began to decrease, while the control store FV basket sales increased, fell, and increased again in the sixth month, which resulted in sales being approximately the same for Nation A intervention and control stores by the sixth month of the intervention (Figure 3a). In Nation B, the FV basket sales rates were higher in the intervention stores for the first 2 weeks of the intervention. In the following 2 weeks, intervention sales rates dropped while control sales rates rose so that both had similar FV basket sales rates for approximately 2 weeks. After the initial month, Nation B intervention stores’ FV market basket sales rate increased and remained higher than the control store rate for the remaining 6 months of the intervention (Figure 3b).
Figure 3.
Weekly Sales Rates of Fruit and Vegetable Market Basket for intervention and control stores in Nation A (left side) and Nation B (right side) for the first six months of the intervention, 7/9/2016-1/7/2017 for Nation A and 5/14/2016-11/12/2016 for Nation B.
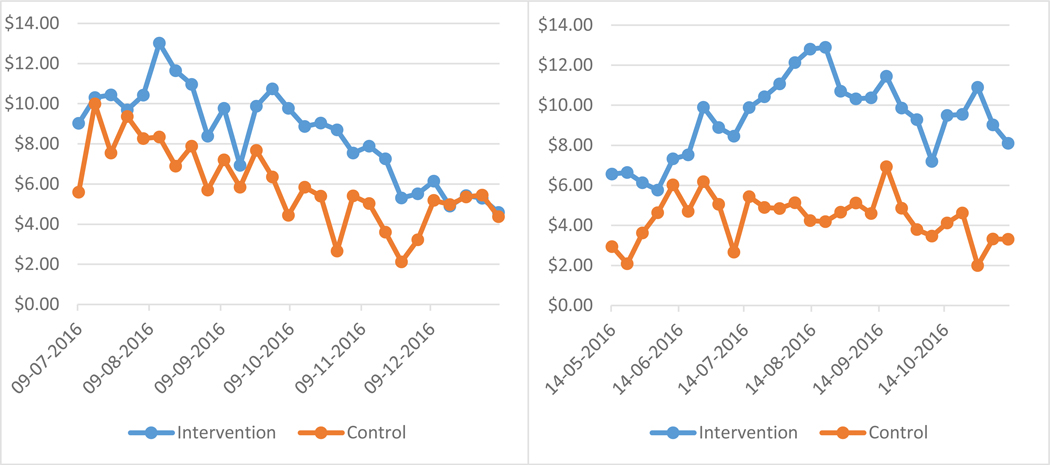
Similarly, there was some weekly variation in the FVS basket sales rates in all stores in both Nations (Figures 4a and b) with similar differences by Nation. In Nation A, the FVS basket sales rate patterns were similar to the FV sales rates over time. Although FVS sales rates were higher in intervention stores through the fifth month, FVS sales rates began to decline after 1 month in both intervention and control stores. In the third month, FVS sales rebounded in intervention stores, while continuing to decline in control stores. In the fifth month, FVS basket sales rates in Nation A control stores rose gradually until sales were approximately the same for intervention and control stores by the sixth month of the intervention (Figure 4a). In Nation B, the FVS basket sales started out and remained higher in the intervention stores for the entire 6-month period. The intervention store FVS sales rates steadily increased during the third month then fell in the fourth month back to the 2-month rate, while control store FVS sales remained flat during these months. In the fifth and sixth months, the difference in FVS sales rates in the intervention and control stores remained large (Figure 4b).
Figure 4.
Weekly Sales Rates of Fruit, Vegetable, and Salad Market Basket for intervention and control stores in Nation A (left side) and Nation B (right side) for the first six months of the intervention, 7/9/2016-1/7/2017 for Nation A and 5/14/2016-11/12/2016 for Nation B.
➤DISCUSSION
The results of this study demonstrate that a healthy retail intervention implemented in tribally owned and operated convenience stores did not reduce total sales in intervention stores, which remained steady throughout the first 6 months of the intervention. These findings are consistent with Simpson et al.’s (2018) findings that total sales were not affected by a healthy retail intervention at a hospital shop, and with the increased sales during and after a healthy retail control trial in rural indigenous Australian stores (Brimblecombe et al., 2017). Furthermore, the healthy retail intervention increased FV sales as a proportion of the total sales in intervention stores compared to control stores during the first 6 months of the intervention. This finding is similar to previous findings that promotion of healthy alternatives increased sales of healthy foods in other types of stores, including corner stores (Song et al., 2009), cafeterias and small retail stores (Gittelsohn et al., 2012), and a hospital shop (Simpson et al., 2018).
Mean weekly sales also differed by Nation, which may be a reflection of differences in the implemented intervention and how individual store managers implemented the intervention. This finding supports the evidence that engaging store managers in healthy retail interventions is key to implementation and sustainability success (Martinez et al., 2018). While weekly FV sales rates were higher for intervention stores than control stores throughout most of the 6 months in Nation B, the weekly sales rates in intervention stores dropped for 2 weeks at the beginning of the intervention. This may have been the result of delivery difficulties of FV items early in the intervention, which was reported by the commerce divisions and reflected in low or no availability of some fruit items on site evaluation forms completed close to these 2 weeks in Nation B intervention stores (Taniguchi et al., 2020). In Nation A, sales rates in intervention store were higher than control stores for a few months, and then gradually decreased to the control store rates by the end of the 6-month period. Reasons for this decline are unclear; however, one possible explanation comes from marketing research studies indicating that sales promotions increase sales over the short term but they are not sustained over the long term (Hawkes, 2009), on average 10 weeks according to one study (Nijs et al., 2001). This may explain the decrease in Nation A weekly sales rates since the intervention in Nation A relied more on promotion healthy foods, while Nation B promoted healthy foods and added more healthy foods to their inventory. The implications of a declining effect of the intervention include that healthy retail interventions may need to include periodic “updates” to one or more of the four Ps and/or continued engagement of retail managers to identify and address barriers to implementation. Another possible explanation may be seasonal variations in consumption of FV or seasonal volatility of produce sales, which are factors cited in other studies for declines in FV during fall and winter months (Glanz & Yaroch, 2004; Jahns et al., 2016; McLaughlin, 2004). The declines in weekly sales rates in October for both intervention and control stores in Nation A seem to follow this pattern, but the weekly sales in Nation B do not seem fit this pattern. These seasonal variations in produce sales has implications for implementing and sustaining healthy retail interventions through months when fresh FV are less available. Finally, the increase in sales of FV in Nation A control stores in December may indicate control stores began to adopt some aspects of the intervention before the intervention period was over. Commerce divisions in both Nations indicated store managements were receiving consumer requests for intervention foods in nonintervention stores and tried to accommodate these requests while balancing the need to adhere to study implementation protocols.
This study had some limitations. First, the process evaluation site visit frequency conducted by the staff as part of this intervention did not align with the weekly sales data and the sample of items assessed on the site visit form did not include all items in the FV and FVS baskets. Therefore, no direct assessment of availability of these items or the relationship between availability and sales could be evaluated. However, site visit reports collected indicate most produce assessed on these forms was available throughout most of the intervention period in intervention stores, including fruits (70%–100%) in both Nations, and fresh vegetables (95%–96%) and salads (96%–99%) in Nation B (Taniguchi et al., 2020). A few produce items in Nation A intervention stores, including fresh vegetable packs (55%–75%) and salads (45%–76%), were available less often but still fairly often (Taniguchi et al., 2020). In addition, as noted above there may have been some contamination with control stores offering more FVS items, which was previously reported as higher in Nation A than Nation B (Jernigan et al., 2018). These sales data seem to indicate this may have occurred toward the end of the 6 months in Nation A due to the increased sales in the control stores; however, if contamination occurred the results would be biased toward the null so our findings would be stronger without the contamination. Second, weekly sales data were missing for a week in one Nation B control store and another week in another Nation B control store. However, it is unlikely either missing week of sales data would change the estimated mean weekly sale rates significantly because the observed findings remained similar for other weeks. Finally, the total sales data provided by tribal commerce divisions included sales of some nonfood items sold at the stores, such as health and hygiene products (e.g., medicine, lip balm, or toothbrushes) or car accessories (e.g., car phone charger, antifreeze, or brake fluid). Fluctuations in sales of these nonfood items may have affected the denominator used for sales rate calculations; however, according to the commerce divisions of both Nations these nonfood items made up a low proportion of the total store sales (8% in Nation A and 5% in Nation B) with minimal fluctuation in the proportion of total sales.
➤PUBLIC HEALTH IMPLICATIONS.
Since healthy retail interventions depend on store managers for successful implementation and sustainability, engaging store managers is key to intervention success. These findings provide health promotion practitioners with additional evidence that healthy retail interventions designed to increase FV availability do not reduce overall sales, including when implemented in rural, tribally owned convenience stores. Additionally, findings indicate FV sales increased as a proportion of total sales. However, these findings also have implications for sustaining store operator engagement and intervention viability. In order to sustain higher FV sales rates, promotions may need to be updated periodically to remind and keep shoppers interested in making healthy purchases. This information along with previously published process and outcomes results can inform tribal leaders and health planners to develop similar healthy retail interventions within their own community contexts in efforts to improve the health of Native people.
Acknowledgments
Author’s Note: We thank the following members of the institutional review boards of the Chickasaw Nation and the Choctaw Nation of Oklahoma for their guidance and contributions: Bobby Saunkeah, Michael Peercy, Danielle Branam, and David Wharton. We would like to thank the commerce division partners in both Nations, especially Mr. W. Kyle Groover and Mr. Chad McCage. We thank Ms. Shondra McCage for leadership in facilitating preliminary intervention work within the store settings. We would also like to acknowledge Jennifer Spiegel and JoAnna Owens for their work in collecting process evaluations for stores in Chickasaw Nation. This study was funded by the National Heart, Lung, and Blood Institute (Grant No. HL117729). The contents of this publication are solely the authors’ responsibility and do not necessarily represent the official views of the National Heart, Lung, and Blood Institute or the National Institutes of Health. The funding agency did not participate in the study design, data collection, analysis, decision to publish, or preparation of the manuscript.
REFERENCES
- Brimblecombe J, Ferguson M, Chatfield MD, Liberato SC, Gunther A, Ball K, Moodie M, Miles E, Magnus A, Mhurchi CN, Leach AJ, & Bailie R. (2017). Effect of a price discount and consumer education strategy on food and beverage purchases in remote Indigenous Australia: A stepped-wedge randomised controlled trial. The Lancet Public Health, 2(2), E82–E95. 10.1016/S2468-2667(16)30043-3 [DOI] [PubMed] [Google Scholar]
- Crawford B, Byun R, Mitchell E, Thompson S, Jalaludin B, & Torvaldsen S. (2017). Socioeconomic differences in the cost, availability and quality of healthy food in Sydney. Australian and New Zealand Journal of Public Health, 41(6), 567–571. 10.1111/1753-6405.12694 [DOI] [PubMed] [Google Scholar]
- Curran S, Gittelsohn J, Anliker J, Ethelbah B, Blake K, Sharma S, & Caballero B. (2005). Process evaluation of a store-based environmental obesity intervention on two American Indian reservations. Health Education Research, 20(6), 719–729. 10.1093/her/cyh032 [DOI] [PubMed] [Google Scholar]
- Foster GD, Karpyn A, Wojtanowski AC, Davis E, Weiss S, Brensinger C, Tierney A, Guo W, Brown J, Spross C, Leuchten D, Burns PJ, & Glanz K. (2014). Placement and promotion strategies to increase sales of healthier products in supermarkets in low-income, ethnically diverse neighborhoods: A randomized controlled trial. American Journal of Clinical Nutrition, 99(6), 1359–1368. 10.3945/ajcn.113.075572 [DOI] [PubMed] [Google Scholar]
- Gittelsohn J, Kim EM, He S, & Pardilla M. (2013). A food store–based environmental intervention is associated with reduced BMI and improved psychosocial factors and food-related behaviors on the Navajo nation. Journal of Nutrition, 143(9), 1494–1500. 10.3945/jn.112.165266 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gittelsohn J, Laska MN, Karpyn A, Klingler K, & Ayala GX (2014). Lessons learned from small store programs to increase healthy food access. American Journal of Health Behavior, 38(2), 307–315. 10.5993/AJHB.38.2.16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gittelsohn J, Rowan M, & Gadhoke P. (2012). Interventions in small food stores to change the food environment, improve diet, and reduce risk of chronic disease. Preventing Chronic Disease, 9, E59–E59. 10.5888/pcd9.110015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glanz K, Johnson L, Yaroch AL, Phillips M, Ayala GX, & Davis EL (2016). Measures of retail food store environments and sales: Review and implications for healthy eating initiatives. Journal of Nutrition Education and Behavior, 48(4), 280–288.e281. 10.1016/j.jneb.2016.02.003 [DOI] [PubMed] [Google Scholar]
- Glanz K, & Yaroch AL (2004). Strategies for increasing fruit and vegetable intake in grocery stores and communities: Policy, pricing, and environmental change. Preventive Medicine, 39(Suppl. 2), S75–S80. 10.1016/j.ypmed.2004.01.004 [DOI] [PubMed] [Google Scholar]
- Gustafson CR, Kent R, & Prate MR Jr. (2018). Retail-based healthy food point-of-decision prompts (PDPs) increase healthy food choices in a rural, low-income, minority community. PLOS ONE, 13(12), Article e0207792. 10.1371/journal.pone.0207792 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawkes C. (2009). Sales promotions and food consumption. Nutrition Reviews, 67(6), 333–342. 10.1111/j.1753-4887.2009.00206.x [DOI] [PubMed] [Google Scholar]
- Ho LS, Gittelsohn J, Rimal R, Treuth MS, Sharma S, Rosecrans A, & Harris SB (2008). An integrated multi-institutional diabetes prevention program improves knowledge and healthy food acquisition in Northwestern Ontario first nations. Health Education & Behavior, 35(4), 561–573. 10.1177/1090198108315367 [DOI] [PubMed] [Google Scholar]
- Jahns L, Johnson LK, Scheett AJ, Stote KS, Raatz SK, Subar AF, & Tande D. (2016). Measures of diet quality across calendar and winter holiday seasons among midlife women: A 1-year longitudinal study using the automated self-administered 24-hour recall. Journal of the Academy of Nutrition and Dietetics, 116(12), 1961–1969. 10.1016/j.jand.2016.07.013 [DOI] [PubMed] [Google Scholar]
- Jernigan VBB, Salvatore AL, Williams M, Wetherill M, Taniguchi T, Jacob T, Cannady T, Grammar M, Standridge J, Fox J, Owens JT, Spiegel J, Love C, Teague T, & Noonan C. (2019). A healthy retail intervention in Native American convenience stores: The THRIVE community-based participatory research study. American Journal of Public Health, 109(1), 132–139. 10.2105/AJPH.2018.304749 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jernigan VBB, Williams M, Wetherill M, Taniguchi T, Jacob T, Cannady T, Grammar M, Standridge J, Fox J, Wiley A, Tingle J, Spiegel J, Riley M, Love C, Noonan C, Weedn A, & Salvatore AL (2018). Using community-based participatory research to develop healthy retail strategies in Native American-owned convenience stores: The THRIVE study. Preventive Medicine Reports, 11, 148–153. 10.1016/j.pmedr.2018.06.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaufman P, Dicken C, & Williams R. (2014). Measuring access to healthful, affordable food in American Indian and Alaska Native tribal areas. http://ageconsearch.umn.edu/record/262120/files/49690_eib131_errata.pdf
- Liang K-Y, & Zeger SL (1986). Longitudinal data analysis using generalized linear models. Biometrika, 73, 13–22. 10.2307/2336267 [DOI] [Google Scholar]
- Love CV, Taniguchi TE, Williams MB, Noonan CJ, Wetherill MS, Salvatore AL, Jacob T, Cannady TK, Standridge J, Spiegel J, & Jernigan VBB (2019). Diabetes and obesity associated with poor food environments in American Indian communities: The THRIVE study. Current Developments in Nutrition, 3(Suppl. 2), 63–68. 10.1093/cdn/nzy099 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martinez O, Rodriguez N, Mercurio A, Bragg M, & Elbel B. (2018). Supermarket retailers’ perspectives on healthy food retail strategies: In-depth interviews. BMC Public Health, 18, Article 1019. 10.1186/s12889-018-5917-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin EW (2004). The dynamics of fresh fruit and vegetable pricing in the supermarket channel. Preventive Medicine, 39(Suppl. 2), S81–S87. 10.1016/j.ypmed.2003.12.026 [DOI] [PubMed] [Google Scholar]
- Mead E, Gittelsohn J, Roache C, & Sharma S. (2010). Healthy food intentions and higher socioeconomic status are associated with healthier food choices in an Inuit population. Journal of Human Nutrition and Dietetics, 23(Suppl. 1), 83–91. 10.1111/j.1365-277X.2010.01094.x [DOI] [PubMed] [Google Scholar]
- Mhurchu CN, Blakely T, Jiang Y, Eyles HC, & Rodgers A. (2010). Effects of price discounts and tailored nutrition education on supermarket purchases: A randomized controlled trial. American Journal of Clinical Nutrition, 91(3), 736–747. 10.3945/ajcn.2009.28742 [DOI] [PubMed] [Google Scholar]
- Middel CN, Schuitmaker-Warnaar TJ, Mackenbach JD, & Broerse JE (2019). Systematic review: A systems innovation perspective on barriers and facilitators for the implementation of healthy food-store interventions. International Journal of Behavioral Nutrition and Physical Activity, 16(1), Article 108. 10.1186/s12966-019-0867-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Närhinen M, Nissinen A, & Puska P. (1998). Sales data of a supermarket: A tool for monitoring nutrition interventions. Public Health Nutrition, 1(2), 101–107. 10.1079/PHN19980016 [DOI] [PubMed] [Google Scholar]
- Nijs VR, Dekimpe MG, Steenkamps J-BEM, & Hanssens DM (2001). The category-demand effects of price promotions. Marketing Science, 20(1), 1–22. 10.1287/mksc.20.1.1.10197 [DOI] [Google Scholar]
- Robinson MS (2014). Gas stations, convenience stores, and “gasinos” in Indian country. Indian Gaming. http://www.indiangaming.com/istore/Nov14_Robinson.pdf [Google Scholar]
- Simpson N, Bartley A, Davies A, Perman S, & Rodger AJ (2018). Getting the balance right: Tackling the obesogenic environment by reducing unhealthy options in a hospital shop without affecting profit. Journal of Public Health, 40(4), e545–e551. 10.1093/pubmed/fdy053 [DOI] [PubMed] [Google Scholar]
- Smith C, & Morton LW (2009). Rural food deserts: Low-income perspectives on food access in Minnesota and Iowa. Journal of Nutrition Education and Behavior, 41(3), 176–187. 10.1016/j.jneb.2008.06.008 [DOI] [PubMed] [Google Scholar]
- Song H-J, Gittelsohn J, Kim M, Suratkar S, Sharma S, & Anliker J. (2009). A corner store intervention in a low-income urban community is associated with increased availability and sales of some healthy foods. Public Health Nutrition, 12(11), 2060–2067. 10.1017/S1368980009005242 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taniguchi TE, Salvatore AL, Williams MB, Love CV, Noonan CJ, Cannady TK, Standridge J, Fox J, Spiegel J, Owens J, Grammar M, Wiley A, & Jernigan VBB (2020). Process evaluation tool development and fidelity of healthy retail interventions in American Indian tribally-owned convenience stores: The THRIVE study. Current Developments in Nutrition, 4(Suppl. 1), 33–41. 10.1093/cdn/nzz073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Census Bureau. (2011). American Indian and Alaska Native heritage month: November 2011. https://www.census.gov/newsroom/releases/archives/facts_for_features_special_editions/cb11-ff22.html
- U.S. Census Bureau. (2015). Fact sheet: American Indians and Alaska Natives. [Google Scholar]