Abstract
Background
The use of ultrasound (US) in emergency departments (ED) has become widespread. This includes both traditional US scans performed by radiology departments as well as point-of-care US (POCUS) performed by bedside clinicians. There has been significant interest in better understanding the appropriate use of imaging and where opportunities to enhance cost-effectiveness may exist. The purpose of this systematic review is to identify published evidence surrounding the cost-effectiveness of US in the ED and to grade the quality of that evidence.
Methods
We performed a systematic review of the literature following Preferred Reporting Items for Systematic Review and Meta-Analyses (PRISMA) guidelines. Studies were considered for inclusion if they were: (1) economic evaluations, (2) studied the clinical use of ultrasound, and (3) took place in an emergency care setting. Included studies were critically appraised using the Consolidated Health Economic Evaluation Reporting Standards checklist.
Results
We identified 631 potentially relevant articles. Of these, 35 studies met all inclusion criteria and were eligible for data abstraction. In general, studies were supportive of the use of US. In particular, 11 studies formed a strong consensus that US enhanced cost-effectiveness in the investigation of pediatric appendicitis and 6 studies supported enhancements in the evaluation of abdominal trauma. Across the studies, weaknesses in methodology and reporting were common, such as lack of sensitivity analyses and inconsistent reporting of incremental cost-effectiveness ratios.
Conclusions
The body of existing evidence, though limited, generally demonstrates that the inclusion of US in emergency care settings allows for more cost-effective care. The most definitive evidence for improvements in cost-effectiveness surround the evaluation of pediatric appendicitis, followed by the evaluation of abdominal trauma. POCUS outside of trauma has had mixed results.
Keywords: Ultrasound, Emergency Medicine, Cost-effectiveness, Radiology, Health Economics
Background
Ultrasound (US) is well established as a safe and effective imaging modality for the rapid diagnosis and management of emergency conditions. At the bedside, it also improves success and patient safety during invasive procedures [1–5]. In the wake of technological advances and the increasing availability of imaging technologies, there has been considerable expansion of the use of clinical US—including both radiology-performed consultative studies and point-of-care ultrasound (POCUS) studies [6–11]. A number of initiatives have been promoted to encourage stewardship of imaging resources and the delivery of high-value care. These include the American College of Radiology’s “Appropriateness Criteria” which assists referring physicians in the selection of the most efficacious and medically-appropriate imaging [12]; the American Board of Internal Medicine Foundation’s “Choosing Wisely” initiative that advocates for use of modalities that are evidence-supported, non-duplicative, harm-free, and truly necessary [13]; and the American Institute of Ultrasound in Medicine’s “Ultrasound First” campaign that promotes the practice of ultrasound for its safety, effectiveness, and affordability [14].
There is a common assumption that US is cost-effective in emergency care settings as it is diagnostically valuable, rapid, and less expensive than other imaging modalities like computed tomography (CT) and magnetic resonance imaging (MRI) [15]. However, it is unclear whether the published data either support or refute this assertion.
Cost-effectiveness analysis is a tool that combines economic and health outcome data to produce standardized ratios of costs and benefits. The outputs of CEAs allow for comparison of diagnostics that vary by both price and clinical utility, and generate important data to support decisions related to health policy and investment. The validity and reliability of CEAs are highly dependent on the rigor with which they are conducted. In 2013, health economists developed consensus-based guidelines on the conduct and reporting of health economic evaluations, called the Consolidated Health Economic Evaluation Reporting Standards (CHEERS) checklist [16].
We present a systematic review of the published evidence surrounding the cost-effectiveness of US in emergency care settings. Our aim is to characterize the existing knowledge regarding the costs and benefits of emergency US, to examine the quality of cost-effectiveness studies using the CHEERS checklist, and to provide guidance for future research efforts.
Methods
Search strategy
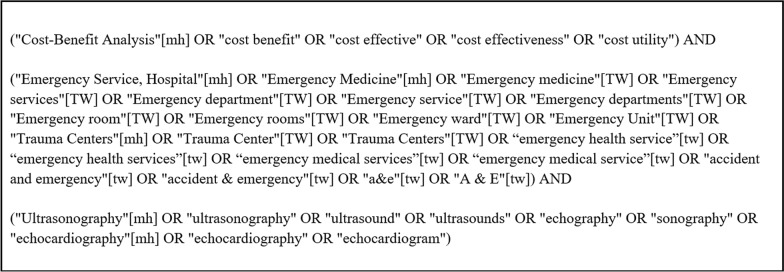
A systematic review of the literature was performed using the Preferred Reporting Items for Systematic Review and Meta-Analyses (PRISMA) guidelines [17]. The review was conducted without date or language restrictions in five major databases (PubMed, Scopus, Embase, Web of Science, and Cochrane). The search terms used are found in Fig. 1.
Fig. 1.
Search terms
Selection of studies and data abstraction
All studies were collated and screened for eligibility through Covidence (www.covidence.org), an online platform for systematic review. Studies were considered for inclusion if they were: (1) economic evaluations that assessed costs and outcomes of comparative strategies; (2) studied the clinical use of US; and (3) took place in an emergency care setting. Two reviewers (BL, NR) with experience in reading, writing and reviewing economic evaluations independently assessed titles and abstracts for inclusion in a blinded fashion. Studies progressed to a full-text review if both reviewers agreed on the relevance based on the research question. Studies then underwent full text reviews for eligibility by each reviewer. Disagreements were resolved by consensus. The following information was extracted from each of the studies in the review: country, year of publication, intervention, comparator, time horizon (the time over which the costs and effect are measured), discount rate (the rate at which future costs and benefits are discounted), perspective (which costs are included or excluded), health outcome, sensitivity analyses (an assessment of the level of uncertainty in the modeling), and findings.
Quality assessment
Two reviewers undertook critical appraisal of the included studies using the CHEERS checklist, which comprises 24 items determined by expert consensus to be of importance when reporting economic evaluations of health interventions [16]. The CHEERS checklist was developed to increase transparency and consistency in the reporting of economic evaluations of health interventions, and ultimately lead to better policy, program, and management decisions. A lower score means readers cannot fully understand the modeling assumptions and, therefore, must question the validity and reliability of the presented results. The checklist can also serve to highlight critical gaps in study design, for example when study authors have not described performing a sensitivity analysis to generate confidence intervals it is likely that this step was overlooked.
Results
Overview of included studies
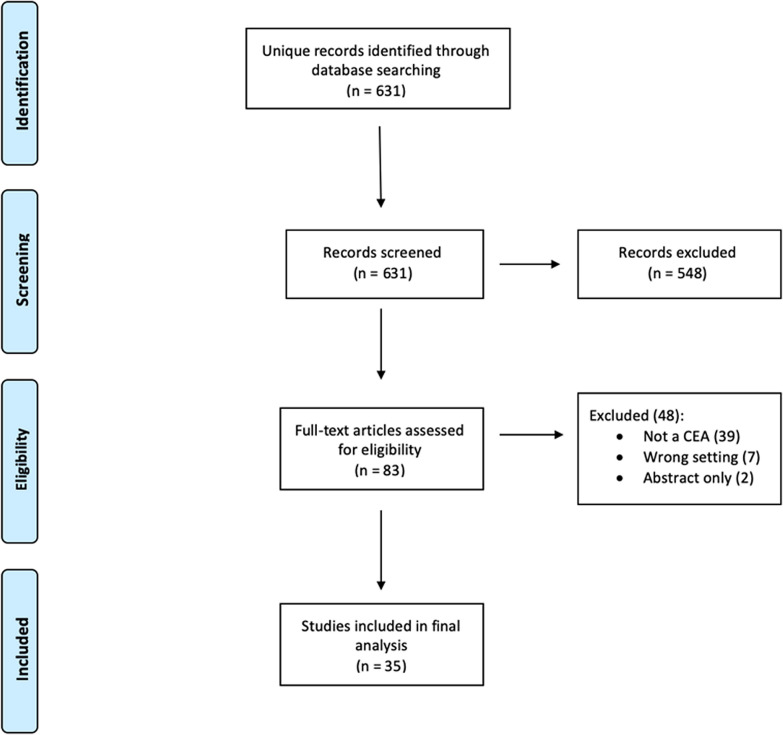
The electronic searches identified 631 potentially relevant articles following the removal of duplicates. After screening titles and abstracts for eligibility, 83 articles remained for full text screening. Of these studies, 35 studies met all inclusion criteria and were eligible for data abstraction. Included studies ranged in publication date from 1996 to 2019, 20 were published in 2014 or later. Studies were excluded in the full-text phase for the following reasons: 39 were not economic evaluations or CEAs, seven were not relevant to the emergency care setting, and two were conference abstracts only. Details are further illustrated in our PRISMA Flow Diagram (Fig. 2).
Fig. 2.
PRISMA flow diagram
Description of included studies
The 35 included studies covered a broad range of applications within emergency US. The most comprehensive body of evidence surrounds the evaluation of pediatric appendicitis. This is followed by trauma, echocardiography, obstetric/gynecologic (OB/GYN), biliary, venous, and renal applications. A small group of studies also evaluate general US processes and impact in the emergency department (ED). Tables 1, 2, 3, 4, 5 and 6 present the principal findings of each study and our grade of the evidence using the CHEERS score.
Table 1.
Evaluation of pediatric appendicitis
| Study | Year | Findings | CHEERS Score (max 24) |
|---|---|---|---|
| Axelrod [18] | 2000 | US can be cost-saving as an adjunct to clinical decision making when deciding to observe or discharge benign pediatric abdominal pain; however, it is not cost-saving when appendicitis is strongly suspected | 14 |
| Pena [19] | 2000 | Staged imaging using US first followed by CT when US was negative or equivocal for pediatric appendicitis produced cost-savings compared to standard of care | 11 |
| Pershad [20] | 2015 | Using US and a clinical decision rule prior to CT for evaluation of pediatric appendicitis is more cost-effective than CT alone | 17 |
| Van Atta [21] | 2015 | Staged imaging with US first in pediatric patients with suspected appendicitis reduces overall cost through CT avoidance | 10 |
| Wagenaar [22] | 2015 | Staged imaging with US first in pediatric patients with suspected appendicitis reduces overall cost through CT avoidance and decreased length of stay | 8 |
| Gregory [23] | 2016 | The most cost-effective approach for assessing pediatric appendicitis is use of a clinical decision rule followed by staged imaging with US first | 22 |
| Anderson [24] | 2017 | A protocol using US and MRI for pediatric appendicitis successfully decreased use of CT scan though without any change in health outcomes and increased radiology costs over the study period | 13 |
| Imler [25] | 2017 | A comparison of US or MRI first in the evaluation of young patients for appendicitis showed higher overall costs and longer ED length of stay in the MRI group | 10 |
| Kharbanda [26] | 2018 | A study across nine pediatric EDs showed that in the evaluation of acute abdominal pain, US first sites had 5.2% lower total costs of treatment than CT first sites | 17 |
| Kobayashi [27] | 2018 | Implementation of an US first appendicitis pathway at a general hospital was unsuccessful in decreasing CT utilization due to poor adherence to the pathway | 8 |
| Nordin [28] | 2018 | Using a standardized reporting template to ensure US quality decreased equivocal studies and the need to perform CT scans for appendicitis in a pediatric ED, leading to further cost-savings estimated at nearly $150,000 per year | 11 |
Table 2.
Evaluation of trauma
| Study | Year | Findings | CHEERS Score (max 24) |
|---|---|---|---|
| Branney [29] | 1997 | Ultrasound use to evaluate acute abdominal trauma can reduce costs through avoidance of peritoneal lavage and reduced length of stay | 10 |
| Partrick [30] | 1998 | Using US as a triage tool in pediatric blunt abdominal trauma may reduce costs through reduced CT scans | 6 |
| Arrillaga [31] | 1999 | In the evaluation of blunt abdominal trauma US decreases time to disposition and procedural costs | 15 |
| Frezza [32] | 1999 | Residents performing FAST is cost-saving compared to US technicians | 8 |
| Melniker [33] | 2006 | Utilizing FAST in the acute management of trauma patients reduces time to operating room, length of stay and overall costs | 7 |
| Hall [34] | 2016 | Performing the cardiac portion of FAST on blunt trauma patients is only cost-effective if they are hypotensive | 23 |
Table 3.
Evaluation of renal, biliary, and venous pathology
| Study | Year | Findings | CHEERS Score (max 24) |
|---|---|---|---|
| Durston [35] | 2001 | Initial POCUS by ED physicians for right-upper quadrant pain followed by radiology department scans if needed, is the most cost-effective approach | 12 |
| Goodacre [36] | 2006 | Assessing for deep vein thrombosis with the Wells score and D-dimer prior to US improves cost-effectiveness by avoiding unnecessary scans | 20 |
| Young [37] | 2010 | There may be a large cost associated with repeating imaging tests for cholecystitis after they have already been performed by proficient ED physicians | 9 |
| Ward [38] | 2010 | In patients with high suspicion for pulmonary embolism but low likelihood of mortality, starting the diagnostic workup with US to assess for deep vein thrombosis and proceeding with only selective CT scanning is cost-effective | 22 |
| Melnikow [39] | 2016 | In patients with suspected kidney stones randomized to initial POCUS, radiology US, or CT there were no significant differences in either outcome or cost | 14 |
| Sternberg [40] | 2017 | An assessment of over 10,000 cases of acute renal colic showed that if US was ordered at the initial visit, overall imaging cost and radiation exposure were lower than if CT scan was ordered initially | 9 |
Table 4.
Evaluation of OB/GYN pathology
| Study | Year | Findings | CHEERS score (max 24) |
|---|---|---|---|
| Hazlett [41] | 1996 | Transvaginal US is cost-saving compared to transabdominal as an initial test in the work-up of pelvic pain in the ED with the exception of patients in the second or third trimester of pregnancy with a palpable abdominal mass or with a full bladder | 6 |
| Durston [42] | 2000 | Initial POCUS by ED physicians in rule-out ectopic cases is cost-effective compared to initial radiology department imaging, although this may delay care in those with adnexal mass or tubal rupture | 12 |
| Al Wattar [43] | 2014 | Twenty-four hour US coverage for OB/GYN emergencies can avert admissions and cost-savings depends on volume | 4 |
Table 5.
Echocardiography
| Study | Year | Findings | CHEERS Score (max 24) |
|---|---|---|---|
| Wyrick [44] | 2008 | Myocardial contrast echocardiography in the ED on selected chest pain patients may be cost-effective through the prevention of unnecessary admissions | 16 |
| Jasani [45] | 2018 | Patients with low-risk chest pain discharged after stress echocardiography in the ED have lower costs and similar health outcomes compared to similar patients admitted to the hospital | 8 |
| Baugh [46] | 2019 | Large variation exists in ordering practices for tests on older patients with syncope in the ED, with CT head and echocardiogram standing out as expensive tests with relatively low yield | 11 |
| Gc [47] | 2019 | In a modeled scenario based on pilot data, the use of tissue Doppler evaluation of diastolic dysfunction in patients with non-ST elevation acute coronary syndrome produced overall cost-savings by decreasing length of stay | 21 |
Table 6.
Miscellaneous studies
| Study | Year | Findings | CHEERS Score (max 24) |
|---|---|---|---|
| McGahan [48] | 2000 | At a single institution, 24-h sonography coverage compared to on-call coverage generated net profit and may have improved patient outcomes | 8 |
| Morrow [49] | 2015 | Ballistics gel can be used to make an effective US training model at a cost-saving with respect to commercially available materials | 7 |
| Allen [50] | 2017 | Downstream imaging after an ED US is increased if the US is performed by a non-radiologist | 12 |
| Huang [51] | 2017 | Introducing a protocol for transcervical US for evaluating pediatric peritonsillar abscess decreased length of stay, surgical procedures and CT scans, however, did not decrease cost | 12 |
| Van Schaik [52] | 2019 | POCUS use in the ED likely produces cost savings by decreasing further diagnostic testing | 12 |
Evaluation of pediatric appendicitis
We identified 11 studies that assessed the cost-effectiveness of US in the evaluation of acute appendicitis [18–28]. The impetus to avoid radiation in the pediatric population has sparked substantial research interest in this area. Universally, these studies found that using US as the initial study to evaluate pediatric patients for appendicitis decreased radiation exposure, overall costs, and length of stay. These results held despite significant rates of inconclusive initial scans. The use of clinical decision rules and US quality templates further increased cost-effectiveness. One study did not find a significant change because of poor adherence to the US first protocol [27].
Evaluation of trauma
Six studies examined US in the setting of acute trauma [29–34]. They found that US decreases time to the operating room for patients with injury, decreases the use of CT scans in children, decreases length of stay, and decreases invasive procedures such as peritoneal lavage in adults. One study specifically examined the cardiac portion of the focused assessment with sonography in trauma (FAST) exam in blunt trauma patients, finding it was only cost-effective in the setting of hypotension [34].
Evaluation of renal, biliary, and venous pathology
Six studies examined US in the setting of renal, biliary, or venous pathology [35–40]. The use of US to evaluate acute flank pain had mixed findings. One study suggested no efficiency gains with US use due to high-numbers of subsequent CT orders, and another found that using US as the initial radiology modality decreases costs and radiation exposure despite a 20% subsequent use of CT to further evaluate patients [39, 40]. Two studies assessed the evaluation of biliary pathology. One study showed that in the evaluation of right-upper quadrant pain, initial POCUS by ED providers followed by radiology department scans if needed was the most cost-effective approach, and a second study described large costs associated with additional imaging after ED POCUS significant for acute cholecystitis [35, 37]. In the evaluation of venous thromboembolism, protocols using clinical screening tools, D-dimer testing, and US to decrease CT usage were the most cost-effective [36, 38].
Evaluation of OB/GYN pathology
Three studies assessed US in the evaluation of emergency OB/GYN complaints [41–43]. One study showed that an initial approach of transvaginal instead of transabdominal US is cost-saving in all patients other than those in the second or third trimester of pregnancy [41]. Another study described benefits and drawbacks of POCUS as the initial test in a rule-out ectopic pregnancy scenario showing higher rates of detection of ectopic pregnancy at the first visit, but with an overall increase in number of US studies performed and the potential of other missed pathology [42]. Finally, a third study found that at high-volume sites 24 h a day US coverage to assess for OB/GYN pathology can avert admissions [43].
Echocardiography
Four studies assessed echocardiography in the emergency care setting [44–47]. Three of the studies focused on decreasing hospitalization using US to provide earlier risk-stratification of patients with acute chest pain or acute cardiac issues [44, 45, 47]. One study assessed the cost-effectiveness of a variety of emergency department modalities to evaluate syncope in older patients, finding that CT head and echocardiography where among the most expensive and least revealing tests that are commonly ordered [46].
Miscellaneous studies
Finally, we identified a collection of studies evaluating the downstream impact of emergency US on resource utilization [48–52]. One study found that patients who had POCUS as opposed to radiology scans were at increased risk of having further confirmatory studies ordered compared to those who had the initial US done by radiology [50]. Another small observational study of POCUS in the ED produced a contrary finding, noting that a bedside US performed by an emergency physician could lead to decreased testing afterwards [52].
Quality assessment of included studies
While we tailored our search criteria to identify formal attempts at CEA, considerable variability remained in the quality of the economic evaluations conducted in the studies we identified. Most studies received about half the possible points on the CHEERS checklist. Inadequacy in the performance or the reporting of study perspectives, preference-based health outcomes (patient-reported preferences for different health states used to calculate metrics such as quality-adjusted life-years), modeling assumptions, transparency of costs, characterization of uncertainty, and incremental cost-effectiveness ratios contributed to the majority of downgrading. For example, only nine of the 35 studies presented any characterization of the uncertainty surrounding their cost-effectiveness results, only seven presented an incremental cost-effectiveness ratio, and only 11 explicitly stated the economic perspective from which they were calculating costs.
Discussion
To our knowledge, this is the first systematic review to broadly evaluate the cost-effectiveness of US in the emergency care setting across all applications, including both radiology-performed and POCUS exams. The body of literature identified through this systematic review is fairly consistent in supporting the increased cost-effectiveness of integrating US in emergency care settings across a variety of applications. Healthcare systems have begun to focus on value-based approaches throughout the hospital including the ED [53], and the demonstration of cost-effectiveness of US has the potential to lead to an expansion of its role in ED patient care.
Of the studies identified in this systematic review, those pertaining to the cost-effectiveness of US in the ED evaluation for pediatric appendicitis were the most plentiful and consistent in demonstration of cost-effectiveness gains, particularly when used in conjunction with clinical decision rules [18–28]. Three of the studies identified in this review were amongst the most rigorous we identified using CHEERS methodology [20, 23, 26]. When combined with the decreased radiation exposure of this approach, these studies add to the case for the widespread adoption of an US first approach in the ED evaluation of pediatric appendicitis.
Use of POCUS evaluation of trauma is ubiquitous and recommended by the American College of Surgeons [54]. The six studies we identified demonstrated consistent cost-effectiveness gains when POCUS is used in the evaluation of trauma [29–34]. These studies, however, generally had poor cost-effectiveness methodology and reporting, with the exception of the investigation by Hall et al. which concluded that in blunt trauma patients the cardiac component of the FAST exam is only cost-effective when a patient is hypotensive [34].
Cost-effectiveness of consultative ED US was demonstrated across a variety of applications, including echocardiography, appendicitis, venous thromboembolism, renal, and obstetric. This is consistent with a prior narrative review that demonstrated increased cost-efficiency of US across the spectrum of clinical medicine [55].
The studies identified in this review generally support the cost-effectiveness of POCUS, although some reach the alternative conclusion. The aforementioned studies evaluating POCUS in trauma consistently demonstrated cost savings. Additionally, multiple studies demonstrated potential cost savings in POCUS for biliary and OB/GYN applications [35, 37, 42]. However, one study failed to identify cost savings in POCUS for patients with suspected kidney stones and another demonstrated additional downstream imaging after initial POCUS [39, 50]. Contrarily, a separate study identified in this review demonstrated that POCUS leads to decreased downstream testing and can lower direct and indirect costs associated with diagnostic workups [52]. Given the large number of supporting studies publication bias should be considered, but an assessment of this falls outside of the scope of our manuscript.
None of the studies included in this systematic review specifically address the widely-inferred cost-effectiveness of POCUS due to increased efficiency (US scans are both performed and interpreted at the bedside in real time by a clinician who can immediately integrate the results into patient management) and patient throughput, or the decreased adverse iatrogenic events due to US guidance of procedures [56–59]. This highlights a gap that could be addressed by future research.
This systematic review sought to identify all relevant articles by searching five databases without language or date restrictions; however, it remains possible that pertinent articles were missed. Multiple independent reviewers were utilized at each step of the study selection and data abstraction process to minimize the likelihood of excluding relevant studies. Additionally, the mixed quality of methodology and reporting surrounding the economic evaluations conducted in these studies is notable. Most authors did not frame their analysis as a formal cost-effectiveness study, which may have led to the lack of robust methodology. Both past and recent reviews of cost-effectiveness studies in radiology have highlighted the need for standardized approaches [60, 61]. This limited utilization of established health economics modeling and reporting standards calls into question the reliability of results and makes comparability across studies difficult.
Conclusions
In summary, the body of existing evidence, though limited, is generally supportive of the cost-effectiveness of US in the emergency care setting. The strongest evidence of cost-effectiveness of ultrasound in the ED exists in the evaluation of pediatric appendicitis and of abdominal trauma. Further study, using established best-practice standards in the methodology of cost-effectiveness analysis, is needed to definitively establish the cost-effectiveness of consultative and POCUS across a variety of applications in emergency care settings.
Acknowledgements
Not applicable.
Abbreviations
- CEA
Cost-effectiveness analysis
- ED
Emergency Department
- FAST
Focused Assessment with Sonography in Trauma
- POCUS
Point-of-Care Ultrasound
- US
Ultrasound
- CT
Computed Tomography
- PRISMA
Preferred Reporting Items for Systematic Review and Meta-Analyses
- CHEERS
Consolidated Health Economic Evaluation Reporting Standards
- OB/GYN
Obstetric/Gynecologic
- MRI
Magnetic Resonance Imaging
Authors' contributions
NR conceived the project. NR & BL undertook critical appraisal of the included studies using the CHEERS checklist. All authors performed analysis of the scored studies and contributed to writing the manuscript. All authors read and approved the final manuscript.
Funding
No funding to report.
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Bioeffects Committee of the American Institute of Ultrasound in Medicine American Institute of Ultrasound in Medicine consensus report on potential bioeffects of diagnostic ultrasound: executive summary. J Ultrasound Med. 2008;27:503–515. doi: 10.7863/jum.2008.27.4.503. [DOI] [PubMed] [Google Scholar]
- 2.Bierig SM, Jones A. Accuracy and cost comparison of ultrasound versus alternative imaging modalities, including CT, MR, PET, and angiography. J Diagn Med Sonogr. 2009;25:138–144. doi: 10.1177/8756479309336240. [DOI] [Google Scholar]
- 3.Moore CL, Copel JA. Point-of-care ultrasonography. N Engl J Med. 2011;364:749–757. doi: 10.1056/NEJMra0909487. [DOI] [PubMed] [Google Scholar]
- 4.Shekelle PG, Wachter RM, Pronovost PJ, et al. Making health care safer II: an updated critical analysis of the evidence for patient safety practices. Evid Rep Technol Assess. 2013;211:1–945. [PMC free article] [PubMed] [Google Scholar]
- 5.Lamperti M, Bodenham AR, Pittiruti M, et al. International evidence-based recommendations on ultrasound-guided vascular access. Intensive Care Med. 2012;38(7):1105–1117. doi: 10.1007/s00134-012-2597-x. [DOI] [PubMed] [Google Scholar]
- 6.Smith-bindman R, Miglioretti DL, Johnson E, et al. Use of diagnostic imaging studies and associated radiation exposure for patients enrolled in large integrated health care systems, 1996–2010. JAMA. 2012;307(22):2400–2409. doi: 10.1001/jama.2012.5960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Smith-bindman R, Kwan ML, Marlow EC, et al. Trends in use of medical imaging in US health care systems and in Ontario, Canada, 2000–2016. JAMA. 2019;322(9):843–856. doi: 10.1001/jama.2019.11456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Moore CL, Molina AA, Lin H. Ultrasonography in community emergency departments in the United States: access to ultrasonography performed by consultants and status of emergency physician-performed ultrasonography. Ann Emerg Med. 2006;47(2):147–153. doi: 10.1016/j.annemergmed.2005.08.023. [DOI] [PubMed] [Google Scholar]
- 9.Sanders J, Noble VE, Raja AS, et al. Access to and use of point-of-care ultrasound in the emergency department. West J Emerg Med. 2015;16(5):747–752. doi: 10.5811/westjem.2015.7.27216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Leschyna M, Hatam E, Britton S, et al. Current state of point-of-care ultrasound usage in Canadian emergency departments. Cureus. 2019 doi: 10.7759/cureus.4246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chamberlain MC, Reid SR, Madhok M. Utilization of emergency ultrasound in pediatric emergency departments. Pediatr Emerg Care. 2011;27(7):628–632. doi: 10.1097/PEC.0b013e3182259908. [DOI] [PubMed] [Google Scholar]
- 12.American College of Radiology (2020) ACR Appropriateness Criteria. https://acsearch.acr.org/list. Accessed Feb 15 2020.
- 13.American Board of Internal Medicine Foundation (2020) Choosing Wisely Initiative. https://www.choosingwisely.org. Accessed Feb 15 2020.
- 14.American Institute of Ultrasound in Medicine (2020) Ultrasound First. http://www.ultrasoundfirst.org. Accessed Feb 15 2020.
- 15.Sistrom CL, McKay NL. Costs, charges, and revenues for hospital diagnostic imaging procedures: differences by modality and hospital characteristics. J Am Coll Radiol. 2005;2(6):511–519. doi: 10.1016/j.jacr.2004.09.013. [DOI] [PubMed] [Google Scholar]
- 16.Husereau D, Drummond M, Petrou S, et al. Consolidated health economic evaluation reporting standards (CHEERS) statement. Int J Technol Assess Health Care. 2013;29(2):117–122. doi: 10.1017/S0266462313000160. [DOI] [PubMed] [Google Scholar]
- 17.Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. Ann Intern Med. 2009;151(4):W65–94. doi: 10.7326/0003-4819-151-4-200908180-00136. [DOI] [PubMed] [Google Scholar]
- 18.Axelrod DA, Sonnad SS, Hirschl RB. An economic evaluation of sonographic examination of children with suspected appendicitis. J Pediatr Surg. 2000;35(8):1236–1241. doi: 10.1053/jpsu.2000.8761. [DOI] [PubMed] [Google Scholar]
- 19.Peña BM, Taylor GA, Fishman SJ, Mandl KD. Costs and effectiveness of ultrasonography and limited computed tomography for diagnosing appendicitis in children. Pediatrics. 2000;106(4):672–676. doi: 10.1542/peds.106.4.672. [DOI] [PubMed] [Google Scholar]
- 20.Pershad J, Waters TM, Langham MR, Li T, Huang EY. Cost-effectiveness of diagnostic approaches to suspected appendicitis in children. J Am Coll Surg. 2015;220(4):738–746. doi: 10.1016/j.jamcollsurg.2014.12.019. [DOI] [PubMed] [Google Scholar]
- 21.Van atta AJ, Baskin HJ, Maves CK, , et al. Implementing an ultrasound-based protocol for diagnosing appendicitis while maintaining diagnostic accuracy. Pediatr Radiol. 2015;45(5):678–685. doi: 10.1007/s00247-014-3220-9. [DOI] [PubMed] [Google Scholar]
- 22.Wagenaar AE, Tashiro J, Wang B, et al. Protocol for suspected pediatric appendicitis limits computed tomography utilization. J Surg Res. 2015;199(1):153–158. doi: 10.1016/j.jss.2015.04.028. [DOI] [PubMed] [Google Scholar]
- 23.Gregory S, Kuntz K, Sainfort F, Kharbanda A. Cost-effectiveness of integrating a clinical decision rule and staged imaging protocol for diagnosis of appendicitis. Value Health. 2016;19(1):28–35. doi: 10.1016/j.jval.2015.10.007. [DOI] [PubMed] [Google Scholar]
- 24.Anderson KT, Bartz-kurycki M, Austin MT, et al. Approaching zero: implications of a computed tomography reduction program for pediatric appendicitis evaluation. J Pediatr Surg. 2017;52(12):1909–1915. doi: 10.1016/j.jpedsurg.2017.08.050. [DOI] [PubMed] [Google Scholar]
- 25.Imler D, Keller C, Sivasankar S, et al. Magnetic resonance imaging versus ultrasound as the initial imaging modality for pediatric and young adult patients with suspected appendicitis. Acad Emerg Med. 2017;24(5):569–577. doi: 10.1111/acem.13180. [DOI] [PubMed] [Google Scholar]
- 26.Kharbanda AB, Christensen EW, Dudley NC, et al. Economic analysis of diagnostic imaging in pediatric patients with suspected appendicitis. Acad Emerg Med. 2018;25(7):785–794. doi: 10.1111/acem.13387. [DOI] [PubMed] [Google Scholar]
- 27.Kobayashi E, Johnson B, Goetz K, Scanlan J, Weinsheimer R. Does the implementation of a pediatric appendicitis pathway promoting ultrasound work outside of a children's hospital? Am J Surg. 2018;215(5):917–920. doi: 10.1016/j.amjsurg.2018.03.017. [DOI] [PubMed] [Google Scholar]
- 28.Nordin AB, Sales S, Nielsen JW, Adler B, Bates DG, Kenney B. Standardized ultrasound templates for diagnosing appendicitis reduce annual imaging costs. J Surg Res. 2018;221:77–83. doi: 10.1016/j.jss.2017.07.002. [DOI] [PubMed] [Google Scholar]
- 29.Branney SW, Moore EE, Cantrill SV, Burch JM, Terry SJ. Ultrasound based key clinical pathway reduces the use of hospital resources for the evaluation of blunt abdominal trauma. J Trauma. 1997;42(6):1086–1090. doi: 10.1097/00005373-199706000-00017. [DOI] [PubMed] [Google Scholar]
- 30.Partrick DA, Bensard DD, Moore EE, Terry SJ, Karrer FM. Ultrasound is an effective triage tool to evaluate blunt abdominal trauma in the pediatric population. J Trauma. 1998;45(1):57–63. doi: 10.1097/00005373-199807000-00012. [DOI] [PubMed] [Google Scholar]
- 31.Arrillaga A, Graham R, York JW, Miller RS. Increased efficiency and cost-effectiveness in the evaluation of the blunt abdominal trauma patient with the use of ultrasound. Am Surg. 1999;65(1):31–35. [PubMed] [Google Scholar]
- 32.Frezza EE, Ferone T, Martin M. Surgical residents and ultrasound technician accuracy and cost-effectiveness of ultrasound in trauma. Am Surg. 1999;65(3):289–291. [PubMed] [Google Scholar]
- 33.Melniker LA, Leibner E, Mckenney MG, Lopez P, Briggs WM, Mancuso CA. Randomized controlled clinical trial of point-of-care, limited ultrasonography for trauma in the emergency department: the first sonography outcomes assessment program trial. Ann Emerg Med. 2006;48(3):227–235. doi: 10.1016/j.annemergmed.2006.01.008. [DOI] [PubMed] [Google Scholar]
- 34.Hall MK, Omer T, Moore CL, Taylor RA. Cost-effectiveness of the cardiac component of the focused assessment of sonography in trauma examination in blunt trauma. Acad Emerg Med. 2016;23(4):415–423. doi: 10.1111/acem.12936. [DOI] [PubMed] [Google Scholar]
- 35.Durston W, Carl ML, Guerra W, et al. Comparison of quality and cost-effectiveness in the evaluation of symptomatic cholelithiasis with different approaches to ultrasound availability in the ED. Am J Emerg Med. 2001;19(4):260–269. doi: 10.1053/ajem.2001.22660. [DOI] [PubMed] [Google Scholar]
- 36.Goodacre S, Stevenson M, Wailoo A, Sampson F, Sutton AJ, Thomas S. How should we diagnose suspected deep-vein thrombosis? QJM. 2006;99(6):377–388. doi: 10.1093/qjmed/hcl051. [DOI] [PubMed] [Google Scholar]
- 37.Young N, Kinsella S, Raio CC, et al. Economic impact of additional radiographic studies after registered diagnostic medical sonographer (RDMS)-certified emergency physician-performed identification of cholecystitis by ultrasound. J Emerg Med. 2010;38(5):645–651. doi: 10.1016/j.jemermed.2008.10.016. [DOI] [PubMed] [Google Scholar]
- 38.Ward MJ, Sodickson A, Diercks DB, Raja AS. Cost-effectiveness of lower extremity compression ultrasound in emergency department patients with a high risk of hemodynamically stable pulmonary embolism. Acad Emerg Med. 2011;18(1):22–31. doi: 10.1111/j.1553-2712.2010.00957.x. [DOI] [PubMed] [Google Scholar]
- 39.Melnikow J, Xing G, Cox G, et al. Cost analysis of the STONE randomized trial: can health care costs be reduced one test at a time? Med Care. 2016;54(4):337–342. doi: 10.1097/MLR.0000000000000487. [DOI] [PubMed] [Google Scholar]
- 40.Sternberg KM, Littenberg B. Trends in imaging use for the evaluation and followup of kidney stone disease: a single center experience. J Urol. 2017;198(2):383–388. doi: 10.1016/j.juro.2017.01.072. [DOI] [PubMed] [Google Scholar]
- 41.Hazlett KS, Wagner A, Guidi C, Victoria D, Weir S, Wise S. Cost effectiveness of pelvic sonogram in the emergency room: endovaginal vs. transabdominal examination. Emergency Radiol. 1996;3(5):231–235. doi: 10.1007/BF01507780. [DOI] [Google Scholar]
- 42.Durston WE, Carl ML, Guerra W, Eaton A, Ackerson LM. Ultrasound availability in the evaluation of ectopic pregnancy in the ED: comparison of quality and cost-effectiveness with different approaches. Am J Emerg Med. 2000;18(4):408–417. doi: 10.1053/ajem.2000.7310. [DOI] [PubMed] [Google Scholar]
- 43.Al Wattar BH, Frank M, Fage E, Gupta P. Use of ultrasound in emergency gynaecology. J Obstet Gynaecol. 2014;34(2):172–173. doi: 10.3109/01443615.2013.839641. [DOI] [PubMed] [Google Scholar]
- 44.Wyrick JJ, Kalvaitis S, Mcconnell KJ, Rinkevich D, Kaul S, Wei K. Cost-efficiency of myocardial contrast echocardiography in patients presenting to the emergency department with chest pain of suspected cardiac origin and a nondiagnostic electrocardiogram. Am J Cardiol. 2008;102(6):649–652. doi: 10.1016/j.amjcard.2008.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Jasani G, Papas M, Patel AJ, et al. Immediate stress echocardiography for low-risk chest pain patients in the emergency department: a prospective observational cohort study. J Emerg Med. 2018;54(2):156–164. doi: 10.1016/j.jemermed.2017.10.019. [DOI] [PubMed] [Google Scholar]
- 46.Baugh CW, Sun BC, Syncope Risk Stratification Study Group Variation in diagnostic testing for older patients with syncope in the emergency department. Am J Emerg Med. 2019;37(5):810–816. doi: 10.1016/j.ajem.2018.07.043. [DOI] [PubMed] [Google Scholar]
- 47.Gc VS, Alshurafa M, Sturgess DJ, et al. Cost-minimisation analysis alongside a pilot study of early tissue doppler evaluation of diastolic dysfunction in emergency department non-ST elevation acute coronary syndromes (TEDDy-NSTEACS) BMJ Open. 2019 doi: 10.1136/bmjopen-2018-023920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Mcgahan JP, Cronan MS, Richards JR, Jones CD. Comparison of US utilization and technical costs before and after establishment of 24-hour in-house coverage for US examinations. Radiology. 2000;216(3):788–791. doi: 10.1148/radiology.216.3.r00se19788. [DOI] [PubMed] [Google Scholar]
- 49.Morrow DS, Broder J. Cost-effective, reusable, leak-resistant ultrasound-guided vascular access trainer. J Emerg Med. 2015;49(3):313–317. doi: 10.1016/j.jemermed.2015.04.005. [DOI] [PubMed] [Google Scholar]
- 50.Allen B, Carrol LV, Hughes DR, Hemingway J, Duszak R, Rosenkrantz AB. Downstream imaging utilization after emergency department ultrasound interpreted by radiologists versus nonradiologists: a medicare claims-based Study. J Am Coll Radiol. 2017;14(4):475–481. doi: 10.1016/j.jacr.2016.12.025. [DOI] [PubMed] [Google Scholar]
- 51.Huang Z, Vintzileos W, Gordish-dressman H, Bandarkar A, Reilly BK. Pediatric peritonsillar abscess: outcomes and cost savings from using transcervical ultrasound. Laryngoscope. 2017;127(8):1924–1929. doi: 10.1002/lary.26470. [DOI] [PubMed] [Google Scholar]
- 52.Van Schaik GWW, Van Schaik KD, Murphy MC. Point-of-care ultrasonography (POCUS) in a community emergency department: an analysis of decision making and cost savings associated with POCUS. J Ultrasound Med. 2019;38(8):2133–2140. doi: 10.1002/jum.14910. [DOI] [PubMed] [Google Scholar]
- 53.Farmer SA, Brown NA. Value-based approaches for emergency care in a new era. Ann Emerg Med. 2017;69(6):684–686. doi: 10.1016/j.annemergmed.2016.11.045. [DOI] [PubMed] [Google Scholar]
- 54.American College of Surgeons . Advanced trauma life support: student course manual. 10. Chicago: Illinois; 2018. [Google Scholar]
- 55.Bierig SM, Jones A. Accuracy and cost comparison of ultrasound versus alternative imaging modalities, including CT, MR, PET, and angiography. J Diagn Med Sonography. 2009;25(3):38–144. doi: 10.1177/8756479309336240. [DOI] [Google Scholar]
- 56.Blaivas M, Harwood RA, Lambert MJ. Decreasing length of stay with emergency ultrasound examination of the gallbladder. Acad Emerg Med. 1999;6:1020–1023. doi: 10.1111/j.1553-2712.1999.tb01186.x. [DOI] [PubMed] [Google Scholar]
- 57.Burgher SW, Tandy TK, Dawdy MR. Transvaginal ultrasonography by emergency physicians decreases patient time in the emergency department. Acad Emerg Med. 1998;5:802–807. doi: 10.1111/j.1553-2712.1998.tb02507.x. [DOI] [PubMed] [Google Scholar]
- 58.Leung J, Duffy M, Finckh A. Real-time ultrasonographically guided internal jugular vein catheterization in the emergency department increases success rates and reduces complications: a randomized, prospective study. Ann Emerg Med. 2006;48:540–547. doi: 10.1016/j.annemergmed.2006.01.011. [DOI] [PubMed] [Google Scholar]
- 59.Randolph AG, Cook DJ, Gonzales CA, Pribble CG. Ultrasound guidance for placement of central venous catheters: a meta-analysis of the literature. Crit Care Med. 1996;24:2053–2058. doi: 10.1097/00003246-199612000-00020. [DOI] [PubMed] [Google Scholar]
- 60.Zhou A, Yousem DM, Alvin MD. Cost-effectiveness analysis in radiology: a systematic review. J Am Coll Radiol. 2018;15(11):1536–1546. doi: 10.1016/j.jacr.2018.06.018. [DOI] [PubMed] [Google Scholar]
- 61.Otero HJ, Rybicki FJ, Greenberg D, Neumann PJ. Twenty years of cost-effectiveness analysis in medical imaging: are we improving? Radiology. 2008;249(3):917–925. doi: 10.1148/radiol.2493080237. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated or analyzed during this study are included in this published article.