Abstract
Hurricanes and other tropical cyclones have devastating effects on society. Previous case studies have quantified their impact on some health outcomes for particular tropical cyclones, but a comprehensive assessment over longer periods is currently missing. Here, we used data on 70 million Medicare hospitalizations and tropical cyclone exposures over 16 years (1999–2014). We formulated a conditional quasi-Poisson model to examine how tropical cyclone exposure (days greater than Beaufort scale gale-force wind speed; ≥34 knots) affect hospitalizations for 13 mutually-exclusive, clinically-meaningful causes. We found that tropical cyclone exposure was associated with average increases in hospitalizations from several causes over the week following exposure, including respiratory diseases (14.2%; 95% confidence interval [CI]: 10.9–17.9%); infectious and parasitic diseases (4.3%; 95%CI: 1.2–8.1%); and injuries (8.7%; 95%CI: 6.0–11.8%). Average decadal tropical cyclone exposure in all impacted counties would be associated with an estimated 16,772 (95%CI: 8,265–25,278) additional hospitalizations. Our findings demonstrate the need for targeted preparedness strategies for hospital personnel before, during, and after tropical cyclones.
Subject terms: Environmental impact, Public health, Risk factors, Interdisciplinary studies
Tropical cyclones can cause severe damage and can thus have devastating impacts on societies. Here, the authors use Medicare data to show that tropical cyclone exposure in the United States is associated with increased hospitalization rates for older adults from many different acute causes.
Introduction
Tropical cyclones, such as hurricanes and tropical storms, have a devastating impact on the economy1–3, environment4,5, and human health6–8. Exposure to such events is an important public health concern and one of the key drivers for seeking disaster risk reduction measures9. The intensity of tropical cyclones is predicted to change due to anthropogenic climate change10–19. Land subsidence20 and increases in the proportion of impervious surfaces21 may further exacerbate cyclone impacts. A recent report by the National Centers for Environmental Information estimated that storm-related costs in the United States between 1980 and 2017 exceeded $1.3 trillion22. Previous assessments of health impacts have largely focused on single extreme events, including well-known examples, such as Hurricane Katrina in New Orleans (2005)23–25 and Hurricane Sandy in New York City (2012)4,26,27.
Some studies have reviewed general evidence of health impacts of storms and hurricanes, primarily using case studies, for cardiovascular diseases, respiratory diseases, dialysis-, and injury-related hospitalizations, showing harmful impacts overall6,28–33. Other studies have previously used claims and Medicare data to measure impacts of disasters, including how mortality and morbidity was affected in the Medicare population after Hurricane Katrina34, and changes in Medicare cost and utilization35. Findings from these studies motivate exploring whether other causes of hospitalization are impacted by tropical cyclones. There are plausible behavioral and physiological pathways for a relationship between tropical cyclone exposure and many adverse health outcomes—such as respiratory complications, due to electricity cuts affecting breathing apparatus6,36, injuries from trying to evacuate or repair a damaged property6,26, or dietary problems due to disrupted food supply lines6,37. Despite these prior findings and biological plausibility, there is an overall knowledge gap in consistently and comprehensively quantifying how tropical cyclone exposure drives hospitalizations across time and space.
In this work, our aim was to evaluate how hospitalizations from various causes in the United States are associated with tropical cyclone exposure that occurs today, and could become increasingly intense, on average, as a result of global climate change13–15. We found that (i) tropical cyclone exposure was associated with overall increases in hospitalization rates for many causes and sub-causes in the week after exposure, with decreases for some chronic conditions; (ii) hurricane-force tropical cyclone exposure amplified the impact of weaker winds on hospitalization rates; and (iii) after tropical cyclone exposure, increases in hospitalization rates were driven by increases in emergency hospitalizations, with decreases in rates driven by decreases in nonemergency hospitalizations.
Results
Tropical cyclone exposure
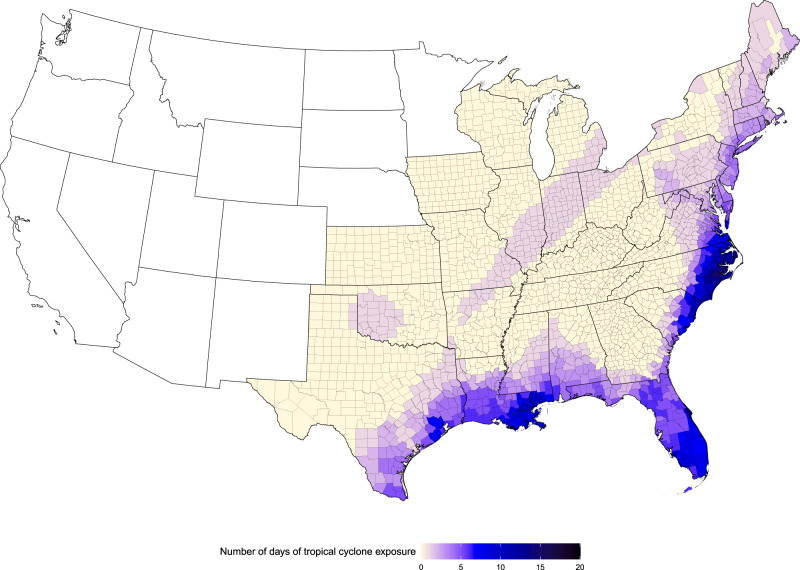
We assigned tropical cyclone exposure to a particular day and county if the peak sustained wind that day in that county reached or exceeded gale force (≥34 knots) on the Beaufort scale, when the tropical cyclone was at the point of closest approach to that county, described in “Methods”. In total, there were 2547 tropical cyclone exposure days in 898 counties during our study period (1999–2014). By county, the number of tropical cyclone exposure days across our study period ranged from 1 to 15, with median of 2 and mean of 2.8. Tropical cyclone exposure occurred from May to October, with the greatest occurrence in September (n = 1337 tropical cyclone exposure days; 52% of all tropical cyclone exposure days). Tropical cyclone exposures were most frequent in the eastern and south-eastern coastal counties (Fig. 1). North Carolina was the single state with the most days of tropical cyclone exposure during the period (n = 413), with Jones and Pamlico Counties, both in North Carolina, each experiencing the most county-level exposure days (n = 15).
Fig. 1. Tropical cyclone exposure days.
Number of days with tropical cyclone exposure by county for 1999–2014.
Medicare hospitalizations
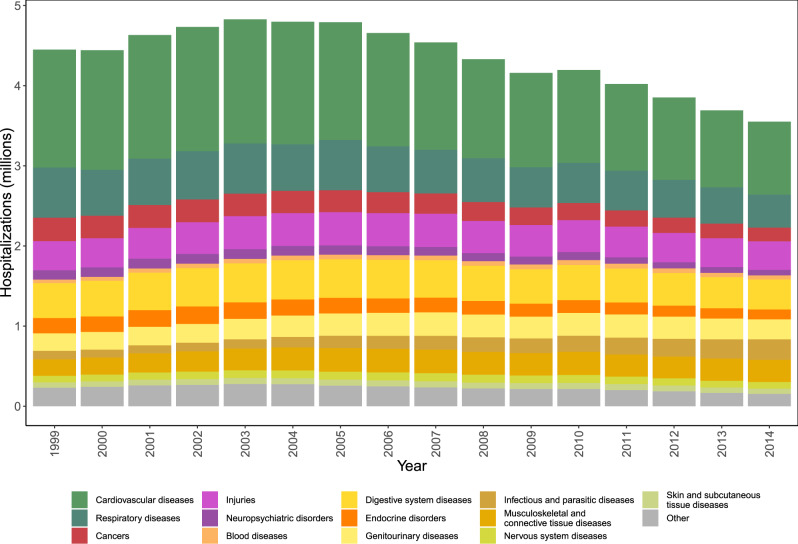
We used data on enrollees from the dynamic Medicare cohort in the 898 counties from 30 states and districts in the United States, which experienced at least one tropical cyclone during our 16-year study period, with information on underlying primary cause of hospitalization and county of residence. From 1999 to 2014, there were 69,682,674 Medicare hospitalizations in the 898 counties impacted by tropical cyclones (Supplementary Table 1). The hospitalizations from these counties included 47.2% of all hospitalizations nationwide during our study period. We grouped the 15,072 possible International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes into 13 main causes (Fig. 2), using the Clinical Classifications Software (CCS) algorithm (Supplementary Table 2)38. Hospitalizations from these 13 causes accounted for 94.8% of the total hospitalizations in our study. Hospitalizations not included in these causes were other hospitalizations (Fig. 2), mainly including rare compilations during pregnancy and ill-defined causes. Cardiovascular (30%), respiratory (12.5%), and digestive system diseases (10%) were the three leading hospitalization causes in our study (Supplementary Table 1).
Fig. 2. Annual Medicare hospitalizations by cause.
Number of Medicare hospitalizations by year and cause of hospitalization for counties with at least one tropical cyclone exposure for 1999–2014.
Association of tropical cyclones exposure with hospitalization rates
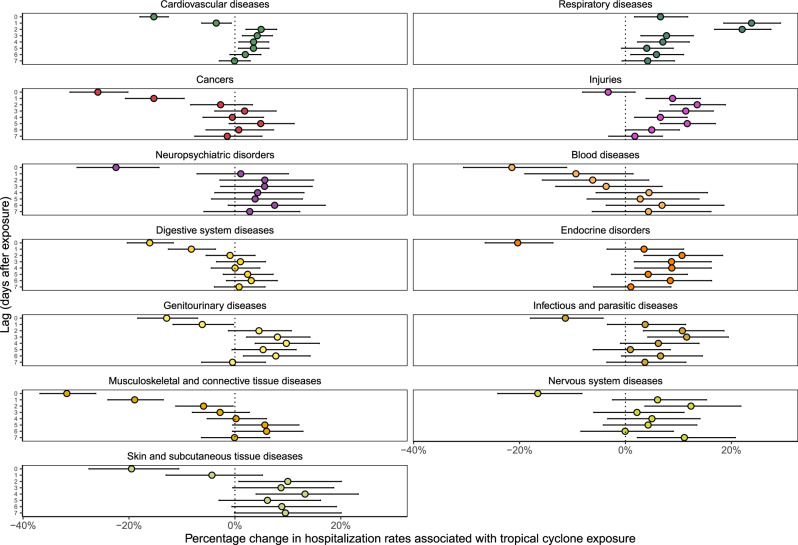
We analyzed the association between tropical cyclone exposure and daily hospitalization rates up to 7 days after the day of exposure, using a conditional quasi-Poisson model, described in detail in “Methods”. We present these results in Fig. 3, which displays results as relative (percentage) changes in hospitalization rates after tropical cyclone exposure. We observed the highest increases in hospitalization rates from respiratory diseases; increases occurred across all studied days after the day of exposure, peaking 1 day after exposure (23.8%; 95% confidence interval [CI]: 18.6, 29.3%). Injury hospitalization rates increased across all studied days after the day of exposure, with a peak at 2 days after the day of exposure (13.5%; 95% CI: 8.5, 18.9%). We observed decreased hospitalization rates on the day of exposure for all other causes. For several causes (cardiovascular diseases, endocrine disorders, genitourinary diseases, infectious and parasitic diseases, nervous system diseases, and skin and subcutaneous tissue diseases) hospitalization risk followed a similar pattern, decreasing on the day of exposure, peaking 1–3 days later, and gradually returning to the rate expected during unexposed days within about a week.
Fig. 3. Percentage change in hospitalization rates with tropical cyclone exposure by cause of hospitalization and lag time.
Lag time is measured in days after tropical cyclone exposure. Dots show the point estimates and error bars represent Bonferroni-corrected 95% confidence intervals.
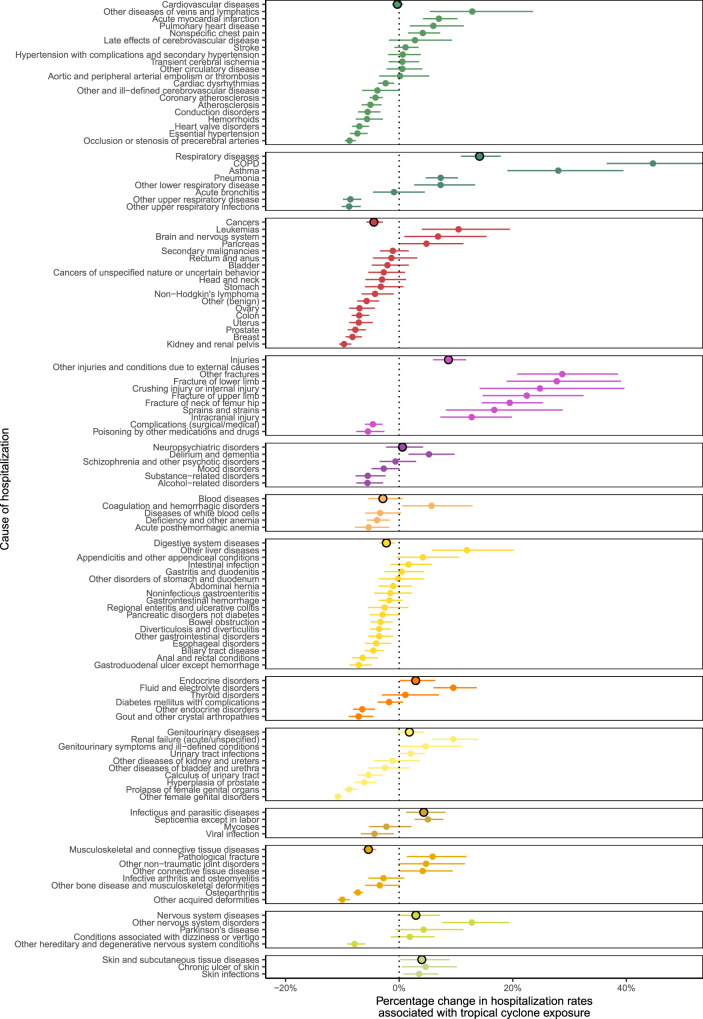
In Fig. 4, we present average relative (percentage) changes in hospitalization rates across the eight examined lag days across the 13 causes in the main analysis, as well as for sub-causes with at least 50,000 hospitalizations during our study period. The sub-causes are linked to the 13 main causes in Supplementary Table 2. Respiratory diseases exhibited the largest average increase in hospitalizations (14.2%; 95% CI: 10.9, 17.9%). We observed the largest decreases in hospitalization rates for cancers (−4.4%; 95% CI: −2.9, −5.8%). Cardiovascular diseases did not change overall (−0.3%; 95% CI: −1.3, 0.7%). There was variation in changes to hospitalization rates for hospitalization sub-causes within each larger cause. For example, within respiratory diseases, we observed the largest increase in hospitalization rates for chronic obstructive pulmonary disease (COPD; 44.7%; 95% CI: 36.6, 54.2%) and the largest decrease in other upper respiratory infections (−8.8%; 95% CI: −6.8, −10.1%).
Fig. 4. Average percentage change in hospitalization rates with tropical cyclone exposure by cause and sub-cause of hospitalization.
Average percentage change in hospitalization rates is across studied lag period (0–7 days after tropical cyclone exposure). Dots show the point estimates and error bars represent 95% confidence intervals.
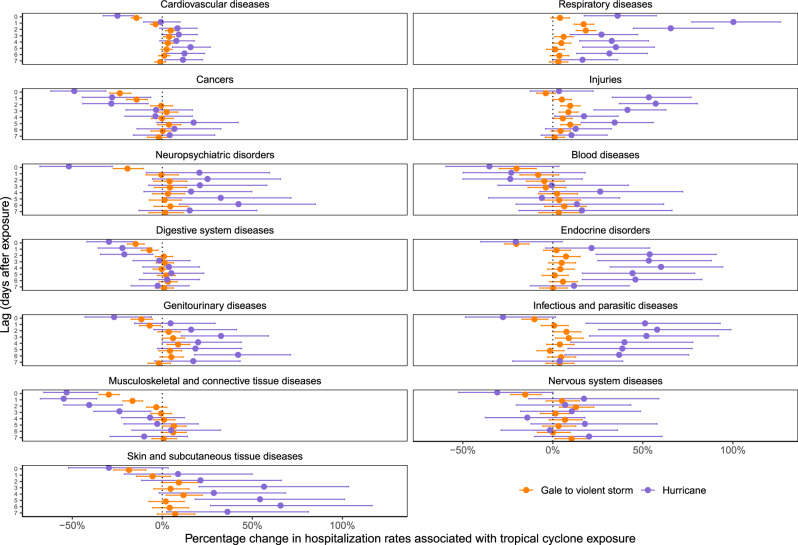
In addition, we examined the distinct impact of tropical cyclone exposures, in which the county’s peak sustained wind was hurricane force (Beaufort scale hurricane-force winds, ≥64 knots) compared to tropical cyclone exposures with lower local winds (Beaufort scale gale- to violent storm-force winds, ≥34 to <64 knots; Fig. 5). Of the 2547 county-day exposures (Fig. 1), 116 (5%) were hurricane force and came from 20 hurricanes. Across causes, the relative (percentage) changes in hospitalization rates during hurricane-force exposures broadly amplified the overall tropical cyclone effects presented in Fig. 3. We observed the highest estimates for respiratory disease hospitalizations, with an 100.3% (95% CI: 77.2, 126.4%) increase 1 day after hurricane exposure compared with a 17.1% (95% CI: 11.8, 22.7%) increase 1 day after exposure to tropical cyclones with lower local winds.
Fig. 5. Percentage change in hospitalization rates with tropical cyclone exposure by cause of hospitalization, intensity of local wind exposure, and lag time.
Lag time is measured in days after tropical cyclone exposure. Dots show the point estimates and error bars represent Bonferroni-corrected 95% confidence intervals.
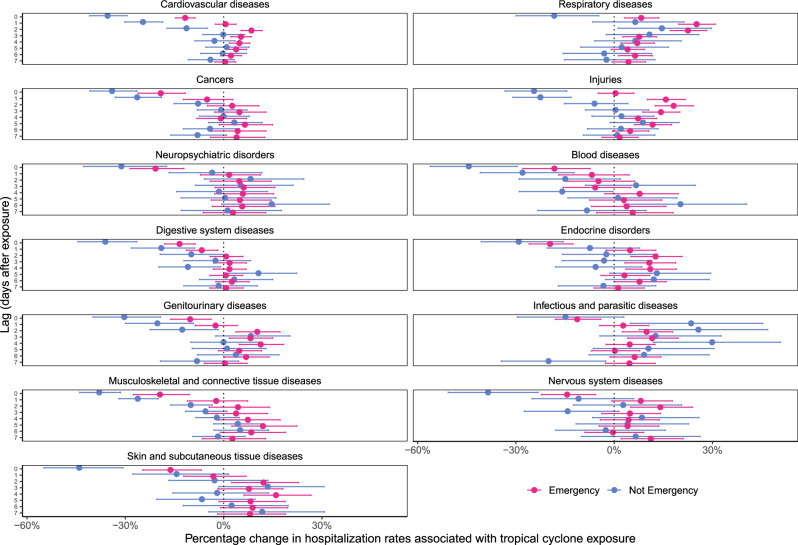
We also examined the association between tropical cyclone exposure and daily hospitalization rates by type of hospital admission (emergency vs. nonemergency; Fig. 6). Generally, nonemergency hospitalization rates decreased in the first few days after tropical cyclone exposure before returning to no change in subsequent days, with the exception of infectious and parasitic diseases, for which we estimated increases in nonemergency hospitalizations for lags 1, 2, and 4. Emergency hospitalization rates for cardiovascular diseases, respiratory diseases, and injuries increased in the days after tropical cyclone exposure, with other causes generally showing lower or no decreases across days, in comparison to nonemergency hospitalizations.
Fig. 6. Percentage change in hospitalization rates with tropical cyclone exposure by cause of hospitalization, type of hospital admission, and lag time.
Lag time is measured in days after tropical cyclone exposure. Dots show the point estimates and error bars represent Bonferroni-corrected 95% confidence intervals.
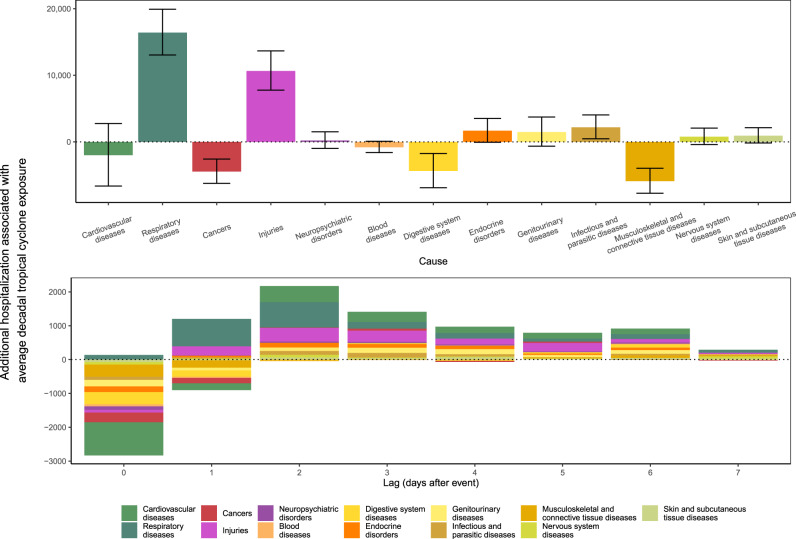
Additional hospitalizations for tropical cyclone exposure
Finally, we estimated the total number of additional hospitalizations for tropical cyclone exposure per decade in the week following the day of exposure across all counties included in our analysis. We used the relative (percentage) changes in hospitalization rate estimates of each cause on day of and each day after exposure, as shown in Figs. 3 and 4, along with the average hospitalization rates during May to October in 1999–2014 and average decadal tropical cyclone exposure, described in detail in “Methods”. Based on this analysis, there would be an estimated 16,772 (95% CI: 8265, 25,278) excess hospitalizations per decade in the eight days (i.e., day of and up to 7 days after exposure), following tropical cyclone exposures in the 30 states and districts included in our analysis (Fig. 7). Respiratory diseases would make up the largest number of additional hospitalizations with 16,413 (95% CI: 13,054, 19,925), followed by injuries with 10,645 (95% CI: 7767, 13,660) and infectious and parasitic diseases with 2185 (95% CI: 458, 4,041). Musculoskeletal and connective tissue disease-related hospitalizations would decrease the most, with 5899 (95% CI: 3970, 7723) fewer overall hospitalizations.
Fig. 7. Change in hospitalizations for the US Medicare population, for an expected number of tropical cyclone exposures by county over a decade.
The top row shows the break down by cause covering the day of tropical cyclone exposure to 7 days afterward, with black bars representing Bonferroni-corrected 95% confidence interval. The bottom row shows the break down by lag days after the exposure.
Sensitivity analyses
Our results were robust to sensitivity analyses of several methods for temperature adjustment. We also fit models (1) including the temperature on the day of tropical cyclone exposure, as well as temperature terms of up to 7 days after exposure and (2) without a temperature term. Our results were robust to these sensitivity analyses.
Discussion
We used data over 16 years on 70 million Medicare hospitalizations and a comprehensive database of county-level local winds associated with tropical cyclones to examine how tropical cyclone wind exposures affect hospitalizations from 13 mutually-exclusive, clinically-meaningful causes, along with common sub-causes. We found the highest increases in respiratory disease hospitalization rates the day of and up to 7 days after the day of tropical cyclone exposure. Hospitalization rates from several causes decreased on the day of exposure, then increased 1–3 days after the day of exposure, returning back to no association by 7 days after. There was variation by sub-cause of hospitalization within each of the 13 causes. Hurricane-force tropical cyclone exposure amplified the impacts compared to cyclones with weaker winds. Changes in emergency hospitalization rates drove increases in hospitalization rates, with decreases driven by reductions in nonemergency hospitalizations. By our analysis, on average there would be increases in overall number of hospitalizations following tropical cyclone wind exposure, with the largest increases in respiratory diseases and injuries.
Acute vs. chronic causes of hospitalization
The observed decreases in hospitalization rates on the day of exposure for most causes are plausible, as the immediate risk to life by making a journey during a tropical cyclone may deter many from seeking treatment at hospital. In general, the decision to make an urgent visit to a hospital for the treatment would be largely based on patients’ feeling of pain, shortness of breath, and which symptoms of a potential adverse health condition they may have noticed. Unless a negative health outcome is so acute that it requires immediate treatment, patients may delay care due to risk of additional harm from tropical cyclone exposure. Consistent with this, we observed general increases in average hospitalization rates in a county exposed to tropical cyclone winds for more acute adverse health outcomes, such as COPD and leukemia, while hospitalizations for chronic conditions, such as hemorrhoids or osteoarthritis, decreased. Canceled inpatient appointments might also play a key factor here, with nonemergency procedures being delayed or rescheduled39. The subsequent peak 1–3 days after exposure may in part be driven by patients visiting the hospital for care missed at locations other than the hospital (e.g., at home or at the family physician’s offices) due to disruption from a tropical cyclone. There is also evidence that proximity to a tropical cyclone’s path may result in the area’s ambulatory (outpatient) care being disrupted39.
Direct vs. indirect tropical cyclone hospitalizations
Tropical cyclone wind exposure can impact hospitalizations via direct (e.g., from physical trauma during exposure) or indirect (e.g., disrupting normal care management at local health care providers, causing damage to critical infrastructure which subsequently impacts health, or via longer-term impacts from stress) pathways6. Direct impacts would have more immediate impacts on hospitalizations. Longer-term, indirect impacts, such as from stress to do with the loss of property from a disaster, may not be fully measured by our analysis, as they could manifest themselves further in time than a week after a disaster40. There may be cases where tropical cyclone exposure could prevent normal medical care or management, compelling people go to the hospital to access resources that they would otherwise get outside the hospital without the storm.
Respiratory diseases
One likely explanation for the elevated rates in respiratory hospitalizations following tropical cyclone exposure is that those with respiratory issues may need power for medical equipment to breathe6. Power outages commonly result from tropical cyclone winds36. During or following a tropical cyclone, the potential loss of power can trigger a faster hospital visit for some in this group, as existing chronic conditions may become unmanageable without ventilators, nebulizers, or oxygen concentrators41. Because of the immediate risk to life, even the danger of leaving home in a storm or hurricane may not deter those seeking medical care for respiratory diseases.
Injuries
Injury hospitalizations are impacted by tropical cyclone exposure both directly and indirectly. During and immediately after tropical cyclones exposure, common injuries originate from transport accidents, structural collapse of buildings, wind-borne debris, falling trees, and downed power lines32. Days after exposure, other injuries such as puncture wounds, lacerations, falls from roof structures, chainsaw mishaps, and burns take more prominence in hospitalizations32. Though tropical cyclone wind exposure may bring about injuries in the Medicare population, those injured may not choose to seek treatment on a dangerous day to leave a property, which would explain the decrease in hospitalizations on the day of tropical cyclone exposure. This may be because the injury may not be life-threatening and the risk of getting caught in a tropical cyclone may be viewed as greater than not seeking treatment immediately42. There is also possibility of the indirect injuries occurring in the days following a tropical cyclone, e.g., during a clean-up process6,43. Houses and properties caught in a tropical cyclone may be severely damaged or nearly destroyed2; the subsequent clean up may present risks for hurting oneself accidentally, e.g., from electrocution6.
Cardiovascular diseases
In our analyses, we did not observe overall changes in average cardiovascular disease hospitalization rates after tropical cyclone exposure. Specifically, we observed a decrease in hospitalization rates on the day of and day after tropical cyclone, followed by a small increase over 2–6 days afterward. This contrasts previous studies reporting overall average increases, though those studies focused on case studies of single hurricane events28,31. For average changes in cause-specific hospitalizations within the broader cardiovascular disease cause group, we observed both positive and negative associations; acute myocardial infarctions (heart attacks) increased after tropical cyclone wind exposures, but non-acute cardiovascular hospitalizations, such as heart valve disorders, decreased. In a study associating snowstorms in Boston with cardiovascular disease hospitalizations, a similar lag pattern was observed44. Tropical cyclone exposure could also indirectly lead to increases in acute cardiovascular disease hospitalizations, due to increased stress and physical challenges brought about during and following exposure6. Disruption of access to essential medicines from closure of local supply sources, such as pharmacies, may also contribute to negative cardiovascular health outcomes45,46. Although we did not observe short-term changes (i.e., in first week after tropical cyclone exposure) in cardiovascular disease hospitalizations, longer-term negative impacts of tropical cyclone exposure on cardiovascular diseases have been observed, several years after exposure itself47.
Neuropsychiatric disorders
Hospitalizations from neuropsychiatric disorders showed no overall average association with tropical cyclone exposure, though we observed an initial decrease of hospitalizations on the day of exposure. We observed an increase in delirium and dementia hospitalizations in the week after tropical cyclone exposure. There is evidence from studies of earthquakes in Japan that disasters can aggravate dementia, both over short- and long-term periods; short-term increases in dementia hospitalizations may be due to moving vulnerable dementia patients out of care and nursing homes, which can cause stress from moving, while also providing worse care in evacuation sites48. Longer-term impacts after disasters may be due to the stress of a domestic property being damaged or destroyed. Tropical cyclone exposure can cause stress and anxiety following potential financial concerns, intimate partner violence, loss of property, loss of family and friends, and other sources of insecurity28,40,49.
Cancers
We observed an overall reduction in cancer-related hospitalizations during the day of and week after tropical cyclone exposure. This association was largely driven by the reduction in cancer-related admissions on the day of and the day after exposure. Hospitalizations and treatment for cancers decrease in general in the aftermath of natural disasters, due to the damage to infrastructure, communication systems and medication, and medical record losses50. We observed different and distinct associations between tropical cyclone exposure and cause-specific hospitalizations within the broader cancer cause group. This may be due to more acute admissions needing immediate attention, such as leukemia or brain and nervous system cancer, while some prearranged admissions for patients with known cancers may be delayed39. For some cancers, lack of access to essential cancer medicine due to supply line disruption may compel a patient to travel to hospital6.
Endocrine disorders and genitourinary diseases
An overall increase in endocrine disorder and genitourinary hospitalizations is plausible, as tropical cyclones can result in decreased availability of adequate food, water, and medicine, as well as electricity to store medicines properly6. Tropical cyclones can severely disrupt food and water supply lines, as well as close off medicine sources, either by locations closing temporarily or by discouraging those who need it from venturing into danger6. Electricity supplies which maintain medicines are often cut off during a storm or hurricane, at least temporarily36. Access to dialysis due to renal failure in the aftermath of a tropical cyclone would also rely on constant supply of electricity, which—when cut at home or unavailable at a local care provider—may result in additional hospitalizations for fluid and electrolyte disorders51.
Other diseases
When a storm or hurricane passes through an area, stagnant and unclean water is often left behind52,53, which can be optimal breeding grounds for many diseases, including infectious and parasitic, skin and subcutaneous, and blood and digestive system diseases53,54, though absolute numbers are small compared with other hospitalization causes. Following the tornado in Joplin, Missouri, in 2011, unusual fungal skin infections were recorded55. Hospitalizations were caused by debris from the tornado infected with some fungus that is more common in uninhabited areas, but rarely makes it into humans’ bodies. The increase in skin and subcutaneous disease may follow this pathway too, as of a result of cleaning up after the storm. Infectious diseases may also take time to be noticeable, as symptoms would only show up a few days after acquisition of an infection.
Planning for tropical cyclone hospitalizations
Other disasters, such as earthquakes and tsunamis, can also overwhelm hospital capacity in a very short time56,57. Similar lessons of how to best assign hospital personnel from our work will be valuable to minimize patient suffering or, ultimately, death. While some cause-specific hospitalization rates may not change on average in the week following a tropical cyclone, the changing distribution of hospitalization rates during the post-cyclone week requires careful planning. Although many health care systems already have provisions in place, findings from our study may further inform planning.
Strengths and limitations
For our study, we leveraged hospitalization data from 70 million Medicare hospitalizations and linked those to a curated tropical cyclone exposure dataset in 30 states and districts over a 16-year period to comprehensively characterize the impact of tropical cyclones on cause-specific hospitalization rates in a vulnerable population. Nonetheless, our study also has some limitations. First, exposure misclassification is likely. Our results are based on patient county of residence; this may not necessarily be the location of the patient during a tropical cyclone. Furthermore, although we conducted analyses at the county level, tropical cyclone wind fields tend to be larger than the size of a county58. Any misclassification, nonetheless, is likely non-differential as it is not expected to be correlated with the outcomes assessed. Any resulting bias, therefore, would be toward the null59. Second, we also cannot exclude the possibility of some residual confounding. By design (matching), our study controls for all factors varying across counties, as well as month and season. We further adjusted for day of week, long-term trends, and temperature. Any variable inducing residual confounding bias, thus, would have to covary with hospitalization rates and tropical cyclone exposure within county and be independent of the variables we have already incorporated in analyses. It is unlikely that our results are attributable to confounding bias.
Future research
We chose to focus on seniors, an already vulnerable population. Our results may not generalize to younger populations; further studies to investigate associations in different age groups are warranted. It will also be important to understand the differential impacts of tropical cyclones on health outcomes by geography, as well as socioeconomic and demographic factors. Further work is needed to specifically understand which hospitals would need to be prepared with the forecast of a tropical cyclone, along with which sources of health care are disrupted. Some negative health outcomes may also be acute and severe enough that those afflicted never get to hospital and die; in these cases, as with other disasters, such as earthquakes60, rapid access to treatment is essential. There is some limited evidence to suggest that there are measurable long-term impacts on health in the years after a disaster47,48. There are plausible causal links between health outcomes and tropical cyclone exposure for many of the associations here6,28–33, but more work needs to be done to identify and formalize these pathways. Characterizing longer-term health impacts of tropical cyclones is critical. We also focused on defining a tropical cyclone by wind speed, as it has direct relevance for identifying a tropical cyclone and therefore emergency planning33,61. Understanding in more detail whether including more information about specific tropical cyclone-related hazards, such as rainfall and flooding, in combination with wind, modify the impact of tropical cyclones on health outcomes will be an important direction of future research. Our study included millions of hospitalizations over a decade across all counties impacted by tropical cyclones in the United States during this period. In more recent years, however, many catastrophic tropical cyclones have made landfall and future studies should include these data.
Conclusion
Our work provides valuable information on how cause-specific hospitalizations can be impacted by tropical cyclones, which can be used for preparedness planning, including hospital and physician preparedness. Adequate forecasting of tropical cyclones might help, for example, in the planning of setting up shelters to provide electricity and common medications and creating easy ways for vulnerable people with certain chronic conditions to find and use those resources outside of the hospital. While our study is the first step in identifying areas of improvement in hospital preparation, enabling and improving planning in this way would be a major innovation, which could save many lives of those who are hospitalized during tropical cyclones, and should be a public health priority.
Methods
Study population
We obtained Medicare inpatient claims data from the Center for Medicare and Medicaid Service (CMS) and assembled data from Medicare beneficiaries, aged 65 years or older, enrolled in the fee-for-service program for at least 1 month from January 1, 1999, to December 31, 2014, and residing in the United States. For each enrollee, we extracted county and state of residence from the Medicare enrollee record file, and the date and principal ICD-9-CM code for each hospitalization from the Medicare Provider Analysis and Review (MEDPAR) file. We restricted analyses to counties that experienced at least one tropical cyclone exposure during the study period. Hospitalizations were aggregated to the county level based on the patient’s county of residence, and included both emergency and nonemergency hospitalizations.
This study was approved by the Institutional Review Board at the Harvard T.H. Chan School of Public Health.
Outcome assessment
We grouped the 15,072 possible ICD-9-CM codes by the CCS hierarchy algorithm38, developed by the Agency for Healthcare Research and Quality, into 18 mutually-exclusive and clinically-meaningful CCS level 1 disease causes. We excluded five causes that occur rarely in older adults, such as pregnancy or fertility issues, and those that were ill-defined. This left 13 level 1 causes, accounting for 94.8% of recorded hospitalizations. These 13 level 1 causes were: cardiovascular diseases, respiratory diseases, cancers, injuries, neuropsychiatric disorders, blood diseases, digestive system diseases, endocrine disorders, genitourinary diseases, infectious and parasitic diseases, musculoskeletal and connective tissue diseases, nervous system diseases, and skin and subcutaneous tissue diseases. We additionally investigated associations with CCS level 3 causes; to avoid unstable model outputs, we restricted this secondary analysis to sub-causes with >50,000 total hospitalizations across all counties during the study period.
Exposure assessment
We obtained data on tropical cyclone wind exposure in the United States from the hurricaneexposure (version 0.1.1) and hurricaneexposuredata (version 0.1.0) packages in R, with full space and time coverage over our study period, and described in detail elsewhere58,62–64. In brief, an exhaustive assessment of tropical cyclones was generated from those recorded in the HURDAT2 dataset based on wind field modeling and validation against observations from weather stations65. First, all tropical cyclones were measured for how close they came to at least one US county. Cyclones that came within 250 km were retained for further wind modeling58. For these, the wind field at each county’s population mean center was modeled every 15 min, while the storm was tracked, providing an estimate of peak local winds that the storm brought to that county66. This modeling used a double exponential wind model to estimate 1-min surface wind at each county center, based on the storm’s forward speed, direction, and maximum wind speed66,67. We used daily estimates of maximum wind sustained speed by county to generate classifications of these exposures. This tropical cyclone wind exposure dataset covered the 898 counties in 30 state or district units (29 states and Washington DC) with at least one tropical cyclone wind exposure during 1999–2014.
From continuous estimates of local storm-associated winds, we classified a county as exposed to tropical cyclone winds based using a cut point from the Beaufort wind scale68. The Beaufort scale is an empirical measure that relates locally measured wind speed to observed conditions on sea or land from 0 (calm) to 12 (Hurricane force). In contrast, the Saffir–Simpson wind scale provides a classification for storm-wide, rather than local, wind intensity69. Our primary analysis focused on tropical cyclone winds, i.e., ≥34 knots, which include both hurricanes and tropical storms. We defined tropical storm exposure when the peak sustained wind that day in the population center of the county associated with the tropical cyclone reached or exceeded 34 knots (63 km/h, 39 mph; gale-force wind on the Beaufort scale) up to 64 knots (119 km/h, 74 mph; violent storm-force wind on the Beaufort scale), when the tropical cyclone was at the point of closest approach to that county. We defined hurricane exposure when the peak sustained wind that day in the population center of the county associated with the tropical cyclone reached or exceeded 64 knots (119 km/h, 74 mph; hurricane-force wind on the Beaufort scale), when the tropical cyclone was at the point of closest approach to that county. In secondary analysis, we used a three-category exposure variable (unexposed, gale to violent storm wind exposure, and hurricane wind exposure).
Covariate data
We obtained data on temperature from the Parameter-elevation Regressions on Independent Slopes Model (PRISM), which gathers climate observations from a wide range of monitoring networks and applies sophisticated quality control measures to generate a nationwide temperature dataset, with full space and time coverage over our study period70. We used gridded daily estimates at a resolution of 4 km2 to generate area-weighted daily temperatures by county.
Statistical analysis
We analyzed the association between daily hospitalization rates and tropical cyclone exposure by applying a conditional quasi-Poisson model71. The quasi-Poisson formulation accounts for potentially overdispersed outcomes. This approach examines contrasts within matched strata, similar to a case-crossover study design, thus eliminating any confounding bias that could arise by factors varying across strata in a computationally efficient way71. Specifically, we matched on county and Julian day of the year, controlling for non-time-varying factors varying across counties in our analyses, as well as seasonality. We flexibly adjusted for longer-term time trends in factors that varied over our study period, and could covary with both tropical cyclone exposure and hospitalization rates. We also adjusted for the mean temperature at the day of the tropical cyclone exposure and day of week. Finally, we included in this model unconstrained distributed lag terms for the exposure72,73, to quantify the association between tropical cyclone exposure and hospitalization rates up to 7 days after exposure. Specifically, we fit the following model:
| 1 |
where denotes the number of CCS level 1-defined cause-specific hospitalizations in county c and day t; the stratum-specific intercepts (not estimated in the conditional Poisson model); lag-specific coefficients (log rate ratios) for tropical cyclone exposure, with lags between the day of tropical cyclone exposure and day of hospitalization and the cumulative effect of tropical cyclone exposure on cause-specific hospitalizations over eight days (lags 0–7); the day of week; a natural spline with two degrees of freedom to flexibly model time trends (seasonal trends are captured through matching); and the offset with population the number of Medicare enrollees in each county and year. We applied the Bonferroni–Holm method to adjust CIs for multiple comparisons74. The 95% CIs were corrected by using α = 0.05/D, where D = 13, the number of causes in our main analysis75.
We assessed whether estimated effects varied for emergency vs. nonemergency CCS level 1 hospitalization causes by fitting stratified analyses by admission type, using the same model as described above. In secondary analyses, we evaluated associations between tropical cyclone exposure and CCS level 3 cause-specific hospitalizations. We present the CCS level 3 associations as the average change in cause-specific hospitalization rate over lags 0–7, i.e., . We used a three-category exposure term to estimate independent effects of tropical cyclone wind exposures separated into gale-force to violent storm-force and hurricane-force intensities for CCS level 1 causes.
Finally, we used the cumulative rate ratio estimates and average cause-specific hospitalization rates during May to October for each cause across 1999–2014, to calculate the expected number of excess (or fewer) hospitalizations during the week following the expected number of tropical cyclone exposures by county over a decade. Specifically, we multiplied the observed average weekly hospitalization rates for each county in May to October across 1999–2014 by the corresponding population of Medicare enrollees, () (ref. 73), where n is the average number of tropical cyclone exposures per year in each country times ten (number of years in a decade).
We present all results as percentage changes in hospitalization rates, unless otherwise noted. We conducted all statistical analyses using the R Statistical Software, version 3.6.3 (Foundation for Statistical Computing, Vienna, Austria)76. To specify the models, we used the gnm function from the gnm package, version 1.1-1 (refs. 71,77). We also used the ns function from the splines package, version 3.6.3 (ref. 78).
Sensitivity analyses
We assessed the sensitivity of our results to temperature adjustment. We fit models (1) including the described temperature term, as well as temperature terms of up to 7 days after exposure and (2) with no temperature term. Our results were robust to these sensitivity analyses.
Supplementary information
Acknowledgements
R.M.P. was supported by the Earth Institute postdoctoral research fellowship at Columbia University. F.D. was funded by the Climate Change Solutions Fund. Funding was also provided by the National Institute of Environmental Health Sciences (NIEHS) grants R01 ES030616, R01 ES028805, R01 ES028033, R01 MD012769, R01 AG066793, R01 ES029950, R21 ES028472, P30 ES009089, and P42 ES010349. The computations in this paper were run on the Research Computing Environment (RCE) supported by the Institute for Quantitative Social Science in the Faculty of Arts and Sciences at Harvard University. We thank Ben Sabath and Danielle Braun for assistance with computational challenges, Jane W. Baldwin for discussions on tropical cyclones, and James E. Bennett for discussions on the statistical model.
Author contributions
All authors contributed to study concept and interpretation of results. R.M.P. collated and organized hospitalization files. R.M.P. collated and organized the storm and hurricane data from the dataset provided by G.B.A. R.M.P., G.B.A., and M.-A.K. developed the statistical model, which was implemented by R.M.P. R.M.P. performed the analysis, with input from M.-A.K., G.B.A., R.C.N., and F.D. A.N.-A. assisted with interpretation of results. R.M.P. and M.-A.K. wrote the first draft of the paper; all authors contributed to revising and finalizing the paper.
Data availability
Tropical cyclone exposure data are publicly available via the R packages hurricaneexposure (version 0.1.1) and hurricaneexposuredata (version 0.1.0) [https://github.com/geanders/hurricaneexposuredata/blob/master/data/storm_winds.rda], based on tropical cyclones recorded in the HURDAT2 dataset [https://www.aoml.noaa.gov/hrd/hurdat/Data_Storm.html]. Medicare enrollees dynamic cohort data are publicly available, upon purchase and after an application process, from the Centers for Medicare & Medicaid Services (CMS) [https://www.cms.gov/Research-Statistics-Data-and-Systems/CMS-Information-Technology/AccesstoDataApplication/index].
Code availability
All code for analysis and visualization presented in this manuscript is available at www.github.com/rmp15/tropical_cyclones_hospitalizations_nat_comms.
Competing interests
The authors declare no competing interests.
Footnotes
Peer review information Nature Communications thanks James Shultz, Kai Chen and the other anonymous reviewer(s) for their contribution to the peer review of this work. Peer reviewer reports are available.
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
The online version contains supplementary material available at 10.1038/s41467-021-21777-1.
References
- 1.Burton, M. L. & Hicks, M. J. Hurricane Katrina: preliminary estimates of commercial and public sector damages. Defense http://www.marshall.edu/cber/research/katrina/Katrina-Estimates.pdf (2005).
- 2.Goldstein, W., Peterson, A. & Zarrilli, D. A. One city, rebuilding together. https://www1.nyc.gov/assets/home/downloads/pdf/reports/2014/sandy_041714.pdf (2014).
- 3.Weinkle, J. et al. Normalized hurricane damage in the continental United States 1900–2017. Nat. Sustain. 1, 808–813 (2018).
- 4.Manuel, J. The long road to recovery: Environmental health impacts of Hurricane Sandy. Environ. Health Perspect.121, a152–159 (2013). [DOI] [PMC free article] [PubMed]
- 5.Pardue, J. H. et al. Chemical and microbiological parameters in New Orleans floodwater following Hurricane Katrina. Environ. Sci. Technol.39, 8591–8599 (2005). [DOI] [PubMed]
- 6.Lane, K.et al. Health effects of coastal storms and flooding in urban areas: a review and vulnerability assessment. J. Environ. Public Health2013, 913064 (2013). [DOI] [PMC free article] [PubMed]
- 7.Rappaport, E. N. Fatalities in the United States from Atlantic tropical cyclones: new data and interpretation. Bull. Am. Meteorol. Soc.95, 341–346 (2014).
- 8.Rappaport, E. N. & Blanchard, B. W. Fatalities in the United States indirectly associated with Atlantic tropical cyclones. Bull. Am. Meteorol. Soc.97, 150909130522008 (2016).
- 9.UNISDR. Sendai Framework for Disaster Risk Reduction 2015 - 2030. In Third World Conf. Disaster Risk Reduction, Sendai, Japan, 14-18 March 2015, 1–25 (2015).
- 10.McMichael, A. J., Woodruff, R. E. & Hales, S. Climate change and human health: present and future risks. Lancet 367, 859–869 (2006). [DOI] [PubMed]
- 11.Smith, K. R. et al. in Climate Change 2014 Impacts, Adaptation and Vulnerability: Part A: Global and Sectoral Aspects (Cambridge University Press, 2015).
- 12.Haines, A. & Ebi, K. The imperative for climate action to protect health. N. Engl. J. Med. 380, 263–273 (2019). [DOI] [PubMed]
- 13.IPCC. Climate Change 2013: the Physical Science Basis. Working Group I Contribution to the Fifth Assessment Report of the Intergovernmental Panel on Climate Change. (Cambridge University Press, 2013).
- 14.Vecchi, G. A. et al. Tropical cyclone sensitivities to CO2 doubling: roles of atmospheric resolution, synoptic variability and background climate changes. Clim. Dyn. 53, 5999–6033 (2019).
- 15.Knutson, T. et al. Tropical cyclones and climate change assessment part II: projected response to anthropogenic warming. Bull. Am. Meteorol. Soc.101, E303–E322 (2020).
- 16.Knutson T, et al. Tropical cyclones and climate change assessment part I: detection and attribution. Bull. Am. Meteorol. Soc. 2019;100:1987–2007. doi: 10.1175/BAMS-D-18-0189.1. [DOI] [Google Scholar]
- 17.Kossin JP. A global slowdown of tropical-cyclone translation speed. Nature. 2018;558:104–107. doi: 10.1038/s41586-018-0158-3. [DOI] [PubMed] [Google Scholar]
- 18.Kossin JP, Emanuel KA, Vecchi GA. The poleward migration of the location of tropical cyclone maximum intensity. Nature. 2014;509:349–352. doi: 10.1038/nature13278. [DOI] [PubMed] [Google Scholar]
- 19.Kossin JP, Olander TL, Knapp KR. Trend analysis with a new global record of tropical cyclone intensity. J. Clim. 2013;26:9960–9976. doi: 10.1175/JCLI-D-13-00262.1. [DOI] [Google Scholar]
- 20.Galloway, D., Jones, D. R. & Ingebritsen, S. E. Land subsidence in the United States. US Geol. Surv. Circ.1182, 1–175 (2000).
- 21.Nowak DJ, Greenfield EJ. Tree and impervious cover in the United States. Landsc. Urban Plan. 2012;107:21–30. doi: 10.1016/j.landurbplan.2012.04.005. [DOI] [Google Scholar]
- 22.NOAA. U.S. billion-dollar weather and climate disasters. https://www.ncdc.noaa.gov/billions/ (2018).
- 23.CDC. Mortality associated with Hurricane Katrina - Florida and Alabama, August-October 2005 (Morbidity and Mortality Weekly Report, 2006). [PubMed]
- 24.Brunkard, J., Namulanda, G. & Ratard, R. Hurricane Katrina deaths, Louisiana, 2005. Disaster Med. Public Health Prep. 2, 215–223 (2008). [DOI] [PubMed]
- 25.Edwards, T. D., Young, R. A. & Lowe, A. F. Caring for a surge of Hurricane Katrina evacuees in primary care clinics. Ann. Fam. Med. 5, 170–174 (2007). [DOI] [PMC free article] [PubMed]
- 26.Seil, K., Spira-Cohen, A. & Marcum, J. Injury deaths related to Hurricane Sandy, New York City, 2012. Disaster Med. Public Health Prep. 10, 378–385 (2016). [DOI] [PubMed]
- 27.Greene, S. K., Wilson, E. L., Konty, K. J. & Fine, A. D. Assessment of reportable disease incidence after Hurricane Sandy, New York City, 2012. Disaster Med. Public Health Prep. 7, 513–521 (2013). [DOI] [PubMed]
- 28.Bourque, L. B., Siegel, J. M., Kano, M. & Wood, M. M. Weathering the storm: the impact of hurricanes on physical and mental health. Ann. Am. Acad. Pol. Soc. Sci. 604, 129–151 (2006).
- 29.Diaz, J. H. The public health impact of hurricanes and major flooding. J. La. State Med. Soc.156, 145–150 (2004). [PubMed]
- 30.Greenough, G. et al. The potential impacts of climate variability and change on health impacts of extreme weather events in the United States. Environ. Health Perspect.109, 191–198 (2001). [DOI] [PMC free article] [PubMed]
- 31.Hendrickson, L. A., Vogt, R. L., Goebert, D. & Pon, E. Morbidity on Kauai before and after Hurricane Iniki. Prev. Med. 26, 711–716 (1997). [DOI] [PubMed]
- 32.Shultz JM, Russell J, Espinel Z. Epidemiology of tropical cyclones: the dynamics of disaster, disease, and development. Epidemiol. Rev. 2005;27:21–35. doi: 10.1093/epirev/mxi011. [DOI] [PubMed] [Google Scholar]
- 33.Yan, M. et al. Tropical cyclone exposures and risks of emergency Medicare hospital admission for cardiorespiratory diseases in 175 urban United States counties, 1999–2010. Epidemiology (2021). 10.1097/EDE.0000000000001337. [DOI] [PMC free article] [PubMed]
- 34.Burton LC, et al. Health of Medicare Advantage plan enrollees at 1 year after Hurricane Katrina. Am. J. Manag. Care. 2009;15:13–22. [PubMed] [Google Scholar]
- 35.Rosenheim, N., Grabich, S. & Horney, J. A. Disaster impacts on cost and utilization of Medicare. BMC Health Serv. Res. 18, 89 (2018). [DOI] [PMC free article] [PubMed]
- 36.Liu, H., Davidson, R. A., Rosowsky, D. V. & Stedinger, J. R. Negative binomial regression of electric power outages in hurricanes. J. Infrastruct. Syst.11, 258–267 (2005).
- 37.Bloom, M. S., Palumbo, J., Saiyed, N., Lauper, U. & Lin, S. Food and waterborne disease in the greater New York City area following Hurricane Sandy in 2012. Disaster Med. Public Health Prep.10, 503–511 (2016). [DOI] [PubMed]
- 38.Elixhauser, A., Steiner, C. & Palmer, L. Clinical Classifications Software (CCS), 2014 (U.S. Agency for Healthcare Research and Quality, 2014).
- 39.Radcliff TA, Chu K, Der-Martirosian C, Dobalian A. A model for measuring ambulatory access to care recovery after disasters. J. Am. Board Fam. Med. 2018;31:252–259. doi: 10.3122/jabfm.2018.02.170219. [DOI] [PubMed] [Google Scholar]
- 40.Hikichi, H. et al. Increased risk of dementia in the aftermath of the 2011 Great East Japan Earthquake and Tsunami. Proc. Natl. Acad. Sci. USA113, E6911–E6918 (2016). [DOI] [PMC free article] [PubMed]
- 41.Rand, D. A., Mener, D. J., Lerner, E. B. & DeRobertis, N. The effect of an 18-hour electrical power outage on an urban emergency medical services system. Prehospital Emerg. Care9, 391–397 (2005). [DOI] [PubMed]
- 42.Noe, R. S. et al. Disaster-related injuries and illnesses treated by American Red Cross disaster health services during Hurricanes Gustav and Ike. South. Med. J.106, 102–108 (2013). [DOI] [PMC free article] [PubMed]
- 43.CDC MMWR. Rapid needs assessment of two rural communities after Hurricane Wilma - Hendry County, Florida, November 1–2, 2005. MMWR Morb. Mortal Wkly Rep.55, 429–431 (2006). [PubMed]
- 44.Bobb JF, et al. Time-course of cause-specific hospital admissions during snowstorms: an analysis of electronic medical records from major hospitals in Boston, Massachusetts. Am. J. Epidemiol. 2017;185:283–294. doi: 10.1093/aje/kww219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Baggett J. Florida disasters and chronic disease conditions. Prev. Chronic Dis. 2006;3:1–3. [PMC free article] [PubMed] [Google Scholar]
- 46.CDC Healthy Aging Program. CDC’s disaster planning goal: protect vulnerable older adults. https://www.cdc.gov/aging/pdf/disaster_planning_goal.pdf (2007).
- 47.Jiao, Z. et al. Effect of Hurricane Katrina on incidence of acute myocardial infarction in New Orleans three years after the storm. Am. J. Cardiol.109, 502–505 (2012). [DOI] [PubMed]
- 48.Furukawa, K., Ootsuki, M., Kodama, M. & Arai, H. Exacerbation of dementia after the earthquake and tsunami in Japan. J. Neurol.259, 1243 (2012). [DOI] [PubMed]
- 49.Steven Picou, J. & Hudson, K. Hurricane Katrina and mental health: a research note on Mississippi Gulf Coast residents. Sociol. Inq.80, 513–524 (2010). [DOI] [PubMed]
- 50.Man, R. X. G., Lack, D. A., Wyatt, C. E. & Murray, V. The effect of natural disasters on cancer care: a A systematic review. Lancet Oncol. 19, e482-e499 (2018). [DOI] [PubMed]
- 51.Kelman, J. et al. Dialysis care and death following Hurricane Sandy. Am. J. Kidney Dis. 65, 109–115 (2015). [DOI] [PubMed]
- 52.Pullen, L. C. Puerto Rico after Hurricane Maria. Am. J. Transplant.18, 283–284 (2018). [DOI] [PubMed]
- 53.Ligon BL. Infectious diseases that pose specific challenges after natural disasters: a review. Semin. Pediatr. Infect. Dis. 2006 doi: 10.1053/j.spid.2006.01.002. [DOI] [PubMed] [Google Scholar]
- 54.Noe, R. et al. Skin disorders among construction workers following Hurricane Katrina and Hurricane Rita: an outbreak investigation in New Orleans, Louisiana. Arch. Dermatol. 143, 1393–1398 (2007). [DOI] [PubMed]
- 55.Fanfair, R. N. et al. Necrotizing cutaneous mucormycosis after a tornado in Joplin, Missouri, in 2011. N. Engl. J. Med.367, 2214–2225 (2012). [DOI] [PubMed]
- 56.Blaskey, S., Baudoin-Laarman, L. & Koerner, C. Thousands Of injuries overwhelm Mexico City’s hospitals After devastating earthquake. Buzzfeed Newshttps://www.buzzfeednews.com/article/sarahblaskey/thousands-of-injuries-overwhelm-mexico-citys-hospitals (2017).
- 57.Carballo, M., Daita, S. & Hernandez, M. Impact of the tsunami on healthcare systems. J. R. Soc. Med.98, 390–395 (2005). [DOI] [PMC free article] [PubMed]
- 58.Anderson GB, et al. Assessing United States county-level exposure for research on tropical cyclones and human health. Environ. Health Perspect. 2020;128:107009. doi: 10.1289/EHP6976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Carroll, R. J., Ruppert, D., Stefanski, L. A. & Crainiceanu, C. M. Measurement Error in Nonlinear Models: A Modern Perspective 2nd edn (Chapman and Hall/CRC, 2006).
- 60.Brown, D. B., Smith, M. J., Chibi, M. T., Hassani, N. & Lotfi, B. Minimizing postdisaster fatalities. Fed. Pract. 34, 10–13 (2017). [PMC free article] [PubMed]
- 61.WMO. Tropical cyclones. https://public.wmo.int/en/our-mandate/focus-areas/natural-hazards-and-disaster-risk-reduction/tropical-cyclones (2020).
- 62.Anderson, G. B. et al. Hurricaneexposure: Explore and Map County-level Hurricane Exposure in the United States. (R Packag. version 0.1.1, 2020).
- 63.Anderson, G. B. & Eddelbuettel, D. Hosting data packages via drat: a case study with hurricane exposure data. R J. 9, 486–497 (2017). [DOI] [PMC free article] [PubMed]
- 64.Anderson, G. B. et al. Hurricaneexposuredata: Data Characterizing Exposure to Hurricanes in United States Counties. (R Packag. version 0.1.0, 2020).
- 65.Landsea, C., Franklin, J. & Beven, J. The revised Atlantic hurricane database (HURDAT2). National Hurricane Centre https://www.nhc.noaa.gov/data/hurdat/hurdat2-format-atlantic.pdf (2014).
- 66.Willoughby, H. E., Darling, R. W. R. & Rahn, M. E. Parametric representation of the primary hurricane vortex. Part II: a new family of sectionally continuous profiles. Mon. Weather Rev. 134, 1102–1120 (2006).
- 67.Anderson, G. B., Schumacher, A., Guikema, S., Quiring, S. & Ferreri, J. Stormwindmodel: model tropical cyclone wind speeds. https://cran.r-project.org/web/packages/stormwindmodel/index.html (2020).
- 68.National Meteorological Library. National meteorological library and archive fact sheet 6 — The Beaufort Scale. MET Officehttps://fdocuments.in/document/fact-sheet-no-6-beaufort-scale.html (2010).
- 69.Schott, T. et al. The Saffir-Simpson hurricane wind scale. National Hurricane Centre https://www.nhc.noaa.gov/pdf/sshws.pdf (2012).
- 70.Daly, C. & Bryant, K. The PRISM climate and weather system - an introduction. Prism Climate Group https://prism.oregonstate.edu/documents/PRISM_history_jun2013.pdf (2013).
- 71.Armstrong, B., Gasparrini, A. & Tobias, A. Conditional Poisson models: a flexible alternative to conditional logistic case cross-over analysis. BMC Med. Res. Methodol. 14, 122 (2014). [DOI] [PMC free article] [PubMed]
- 72.Schwartz, J. The distributed lag between air pollution and daily deaths. Epidemiology 11, 320–326 (2000). [DOI] [PubMed]
- 73.Bobb, J. F., Obermeyer, Z., Wang, Y. & Dominici, F. Cause-specific risk of hospital admission related to extreme heat in older adults. JAMA J. Am. Med. Assoc. 312, 2659–2667 (2014). [DOI] [PMC free article] [PubMed]
- 74.Holm, S. A simple sequentially rejective multiple test procedure. Scand. J. Stat. 6, 65–70 (1979).
- 75.Dunn, O. J. Multiple comparisons among means. J. Am. Stat. Assoc. 56, 52–64 (1961).
- 76.R Core Team. R: A Language and Environment for Statistical Computing (R Foundation for Statistical Computing Foundation for Statistical Computing, 2012).
- 77.Turner, H. & Firth, D. Generalized nonlinear models in R: an overview of the gnm package. Soc. Res. https://cran.r-project.org/web/packages/gnm/vignettes/gnmOverview.pdf (2008).
- 78.Gasparrini, A. Distributed lag linear and non-linear models in R: the package dlnm. J. Stat. Softw. 43, 1–20 (2011). [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Tropical cyclone exposure data are publicly available via the R packages hurricaneexposure (version 0.1.1) and hurricaneexposuredata (version 0.1.0) [https://github.com/geanders/hurricaneexposuredata/blob/master/data/storm_winds.rda], based on tropical cyclones recorded in the HURDAT2 dataset [https://www.aoml.noaa.gov/hrd/hurdat/Data_Storm.html]. Medicare enrollees dynamic cohort data are publicly available, upon purchase and after an application process, from the Centers for Medicare & Medicaid Services (CMS) [https://www.cms.gov/Research-Statistics-Data-and-Systems/CMS-Information-Technology/AccesstoDataApplication/index].
All code for analysis and visualization presented in this manuscript is available at www.github.com/rmp15/tropical_cyclones_hospitalizations_nat_comms.