Abstract
Background
Total hip arthroplasty (THA) performed for displaced femoral neck fractures (FNF) is becoming a more frequent treatment in the active elderly population. The complication profiles associated with THA surgical approaches in the fracture setting are unclear. The purpose of this study was to compare a series of THA for FNF performed via the direct anterior (DA) approach vs alternative approaches (anterolateral and posterolateral).
Methods
A retrospective review identified 52 patients who underwent primary THA for FNF between 2009 and 2018, including 20 via the DA approach and 32 by alternative approaches. All procedures were exclusively performed by high-volume arthroplasty surgeons. Perioperative results, complications, and clinical outcomes were compared with those of routine statistical methods. Mean follow-up duration was 3 years (range, 1-8).
Results
The average age was 74 years (range, 57-92) with similar baseline characteristics between the 2 groups (P = .09). The DA cohort demonstrated significantly shorter length of stay (3 days vs 5 days, P < .01) and discharge to home vs skilled nursing facility (40.0% vs 9.4% P = .014). There was a trend toward decreased complications (0% vs 16%, P = .08). There were no dislocations or fractures in either cohort. Final Harris Hip Scores (94 vs 81, P = .07) and return to community ambulation (96%) were similar between DA and alternative approach groups.
Conclusion
The DA approach to THA performed for FNF appears safe with improved outcomes compared with alternative approaches. Larger studies are needed to verify these results.
Keywords: Femoral neck fracture, Total hip arthroplasty, Direct anterior approach
Introduction
Femoral neck fractures (FNFs) are a common orthopedic injury which can result in significant morbidity and mortality. With the increasing age of our population, the number of hip fractures is expected to continue to rise [1,2]. There are a variety of methods for surgical treatment of acute FNFs, including internal fixation and partial or total hip arthroplasty (THA) [3]. Owing to the high rate of nonunion encountered with internal fixation, estimated to be approximately 33%, arthroplasty is becoming a more frequently selected treatment [4,5]. In 2013 alone, nearly a 40% increase in utilization of THA for FNFs was seen compared to the previous decade [6,7].
The reason for the increased use of THA is thought to be partially due to decreased complication rates and possible economic advantages compared with the alternative options. Recent studies indicate lower rates of failure, revision, mortality, and hospital length of stay. These same reports also demonstrate superior clinical and functional outcomes with THA compared with hemiarthroplasty [[5], [6], [7], [8]].
Despite the growing support for the use of THA in the management of acute FNFs, concerns regarding potential increased blood loss, surgical duration, and dislocation risks remain [4,6,9]. It has been recommended by some to avoid certain approaches or use technology such as dual mobility components to reduce the risk of dislocation after THA for a FNF [10]. Many of these prior studies, however, have not evaluated the complication profile of THA for FNFs based on surgical approach. The purpose of this study was to compare perioperative results, complications, and clinical outcomes in a series of THAs performed for acute FNFs via the direct anterior (DA) approach vs alternative approaches (anterolateral and posterolateral) when the procedure was performed by high-volume joint surgeons. Our hypothesis was that DA THAs performed for FNFs would have fewer complications and superior clinical outcomes than alternative approaches.
Material and methods
After obtaining institutional review board approval, a retrospective review of THAs was performed for acute FNFs at our hospital between 2009 and 2018. All data were obtained via chart review including baseline patient characteristics and demographics, perioperative course, complications requiring readmissions and reoperations, and final clinical follow-up with Harris Hip Scores (HHS).
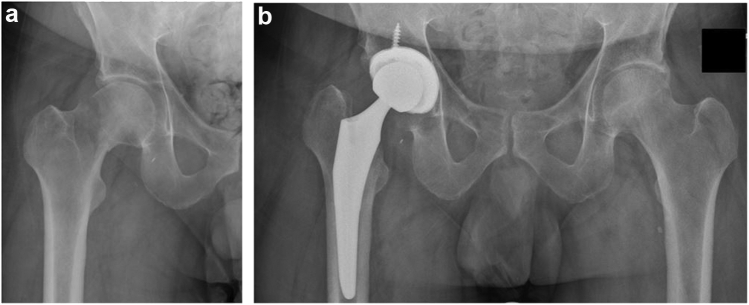
A total of 52 consecutive patients who had at least 1 year of follow-up were identified; 20 of whom underwent a DA approach compared with 32 (7 anterolateral and 25 posterolateral) by alternative approaches (Fig. 1). The average age was 74 years (range, 57-92) with similar baseline demographic data and operative characteristics between the 2 groups (Table 1). There was no statistically significant difference noted in age, sex, laterality, fracture type, BMI, preoperative ambulatory status, or American Society of Anesthesiologists classification (all P ≥ .087). Length of follow-up was noted to be shorter in the DA cohort than that in the alternative approach group (median: 2.4 vs 3.0 years, P = .047). All surgeries were performed by high-volume subspecialty total joint surgeons (>100 procedures per year) or the arthroplasty fellow. Surgical approach was based on surgeon preference, with all approaches performed by multiple surgeons through the study period. Postoperative protocols were the same between groups, with the exception of posterior hip precautions included for the posterolateral approach group.
Figure 1.
Anteroposterior radiographs demonstrating an acute femoral neck fracture (a), treated with a total hip arthroplasty (b).
Table 1.
Demographic and operative characteristics.
| Variable | Direct anterior approach (N = 20) | Anterolateral or posterior approach (N = 32) | P value |
|---|---|---|---|
| Age at surgery (y) | 75.2 (58.1, 92.9) | 76.7 (58.2, 91.9) | .93 |
| Sex (male) | 7 (35.0%) | 9 (28.1%) | .76 |
| Laterality (right) | 13 (65.0%) | 12 (37.5%) | .087 |
| Fracture type | 1.00 | ||
| Basicervical | 2 (10.0%) | 3 (9.4%) | |
| Subcapital | 8 (40.0%) | 14 (43.8%) | |
| Transcervical | 10 (50.0%) | 15 (46.9%) | |
| BMI | 25.9 (16.2, 35.5) | 25.6 (18.1, 37.1) | .72 |
| Preoperative ambulation status | 1.00 | ||
| Community ambulator | 20 (100.0%) | 31 (96.9%) | |
| Household ambulator | 0 (0.0%) | 1 (3.1%) | |
| ASA classification | .25 | ||
| 2 | 7 (35.0%) | 7 (21.9%) | |
| 3 | 13 (65.0%) | 24 (75.0%) | |
| 4 | 0 (0.0%) | 1 (3.1%) | |
| Cement or pressfit | .28 | ||
| Cement | 0 (0.0%) | 3 (9.4%) | |
| Pressfit | 20 (100.0%) | 29 (90.6%) | |
| Arthroplasty specialist | .21 | ||
| Staff surgeon | 13 (65.0%) | 26 (81.3%) | |
| Fellow | 7 (35.0%) | 6 (18.8%) | |
| Length of follow-up (y) | 2.4 (1.1, 4.5) | 3.0 (1.0, 7.9) | .047 |
The sample median (minimum, maximum) is given for continuous variables. P values result from a Wilcoxon rank sum test (continuous and ordinal variables) or Fisher’s exact test (categorical variables).
ASA, American Society of Anesthesiologists; BMI, body mass index.
Bold indicates a statistical significance (P < .05).
Statistical methods
For comparison, the anterolateral and posterolateral approaches were combined into one group of 32 patients, classified as the alternative approach group. Continuous variables were summarized with the sample median and range. Categorical variables were summarized with number and percentage. Comparisons of baseline characteristics and follow-up length between the DA and alternative approach groups were made using a Wilcoxon rank sum test (continuous and ordinal variables) or Fisher’s exact test (categorical variables). Comparisons of postoperative outcomes between the DA and alternative approach groups were made using a log-rank test (complication, reoperation, dislocation), a linear regression model that was adjusted for follow-up length (HHS), a Wilcoxon rank sum test (hospital length of stay), or Fisher’s exact test (discharge destination, postoperative ambulation status, and worsening of ambulation status from preoperative to postoperative time). P values <0.05 were considered as statistically significant, and all statistical tests were two-sided. Statistical analyses were performed using the R Statistical Software (version 3.6.2; R Foundation for Statistical Computing, Vienna, Austria).
Results
Postoperative outcomes were compared between the DA and alternative approach cohorts, delineated in Table 2. Compared with the alternative approach group, patients undergoing DA THA had a significantly shorter hospital length of stay (median: 3 vs 5 days, P = .001). In addition, patients undergoing DA THA were more frequently discharged home rather than a skilled nursing facility (40.0% vs 9.4%, P = .014).
Table 2.
Comparison of postoperative outcomes between direct anterior and anterolateral/posterior surgical approaches.
| Postoperative outcome | Direct anterior approach (N = 20) | Anterolateral or posterior approach (N = 32) | P value |
|---|---|---|---|
| Complication | 0 (0.0%) | 5 (15.6%) | .089 |
| Reoperation | 0 (0.0%) | 2 (6.3%) | .30 |
| Dislocation | 0 (0.0%) | 0 (0.0%) | 1.00 |
| Harris Hip Score | 94 (62, 100) | 81 (44, 100) | .072 |
| Hospital length of stay (d) | 3 (2, 10) | 5 (2, 8) | .001 |
| Discharge destination | .014 | ||
| Home | 8 (40.0%) | 3 (9.4%) | |
| Skilled nursing facility | 12 (60.0%) | 29 (90.6%) | |
| Postoperative ambulation status | .52 | ||
| Community ambulator | 20 (100.0%) | 30 (93.8%) | |
| Household ambulator | 0 (0.0%) | 2 (6.3%) | |
| Worsening of ambulation status from preoperative to postoperative | 0 (0.0%) | 1 (3.1%) | 1.00 |
The sample median (minimum, maximum) is given for continuous variables. P values result from a log-rank test (complication, reoperation, dislocation), a linear regression model that was adjusted for follow-up length (Harris Hip Score), a Wilcoxon rank sum test (hospital length of stay), or Fisher’s exact test (discharge destination, postoperative ambulation status, and worsening of ambulation status from preoperative to postoperative).
Bold indicates a statistical significance (P < .05).
Overall, complications requiring a readmission or reoperation occurred less often in patients undergoing DA THA; however, this did not reach statistical significance (0.0% vs 15.6%, P = .089). Complications in the alternative approach group included a distal femur fracture (1), acute postoperative infection requiring irrigation and debridement (1), acetabular component loosening (1), postoperative hematoma (1), and mechanically assisted crevice corrosion and adverse local tissue reaction (1). There were no notable differences in reoperation or dislocation rates or ambulation status between the 2 surgical approach groups (all P ≥ .30).
There was no difference in HHS between the DA THA group compared with the alternative approach group in linear regression analysis adjusting for length of follow-up (median: 94 vs 81, P = .072). At final follow-up, 96% of patients were community ambulators with no significant difference between cohorts (P = .52).
Discussion
With a growing population of independent and active elderly in the United States, there is a commensurate increase in the incidence of FNFs and heightened focus on best treatment options—internal fixation vs arthroplasty. Historically there has been a high rate of reported complications, including a 10% dislocation rate, when THA has been performed in the setting of an acute FNF [11]. This high complication rate has previously directed surgeons away from total joint arthroplasty, instead preferring internal fixation or hemiarthroplasty as the treatment of choice. More recent data, however, have demonstrated up to a 33% rate of nonunion and 35% rate of reoperation in patients who undergo internal fixation [12]. Similarly, there is a concern for acetabular wear and erosion with hemiarthroplasty [13,14]. Owing to these limitations, there is an increasing body of literature that supports THA as the preferred treatment for FNFs. These studies report superior clinical outcomes as well as economic advantages related to a lower reoperation rate [4,6,8,[15], [16], [17]].
Early rehabilitation and mobilization are critical considerations in the management of acute FNFs. The DA approach has been reported to have improved early rehabilitation when compared with alternate approaches [17,26]. In our study, we found a significantly reduced hospital length of stay in the patients that underwent THA via the DA approach vs the anterolateral or posterolateral approaches. In addition, a significantly larger proportion of these patients were discharged to their home rather than to a skilled nursing facility than in the alternative approach group. These findings were in spite of a similar baseline ambulatory status and American Society of Anesthesiologists classification between groups. Although beyond the scope of this study, improved rehabilitation and less utilization of extended care facilities could potentially have a significant cost-saving on health-care expenditures related to acute FNF treatment.
Owing to the perceived higher dislocation rate after THA, authors have previously recommended against performing the procedure through a posterolateral surgical approach and encouraged the use of dual mobility implants in an effort to decrease the risk of postoperative dislocations [18]. A limitation from these early studies was that the procedures were not always performed by surgeons who specialize in total joint arthroplasty. Recent studies have demonstrated improved outcomes when procedures were completed at high-volume arthroplasty centers [19,20]. In the present study, which included THAs only performed by high-volume arthroplasty, we noted an overall low complication rate independent of approach used. No patient suffered a postoperative dislocation in either cohort. In contrast to other studies, we did not find a statistically significant difference in complication rates between the anterior and alternative approaches [21,22]. Notably, we did not encounter previously described complications with the anterior approach, such as intraoperative fractures, which was likely a result of the surgeon experience with the approach [[23], [24], [25]].
Late clinical outcomes were similar between cohorts, with no statistical difference in ambulatory status between groups. Importantly, 96% of patients remained community ambulators at final follow-up. The DA approach had a higher HHS (94 vs 81), but the difference was neither statistically significant (P = .072) nor clinically meaningful (<16 points) [27].
There are several limitations to this study, including all the limitations inherent to a retrospective review study design. In addition, this was performed at an institution which does not have a high trauma volume, thereby limiting the sample size. Owing to the low numbers, the possibility of a type II error (ie, a false-negative finding) is important to consider; we cannot conclude that there is no true difference in a given outcome between the DA and alternative approach groups simply because of the presence of a nonsignificant P value. We did not include complications that did not require readmission or reoperation, so we are likely underestimating overall complications in both cohorts. Finally, the procedures were performed by arthroplasty surgeons who routinely perform THA through the various approaches studied. Selection bias for approach based on surgeon comfort is a concern. As such, these results may not be generalizable.
Conclusions
The DA approach to THA performed for acute FNF appears safe with improved outcomes, including shorter hospital length of stay and increased discharge to home, when compared with alternative approaches to the hip. Larger studies are needed to verify these results.
Conflict of interests
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this article.
Appendix A. Supplementary data
References
- 1.Lewiecki E.M., Wright N.C., Curtis J.R. Hip fracture trends in the United States, 2002 to 2015. Osteoporos Int. 2018;29(3):717. doi: 10.1007/s00198-017-4345-0. [DOI] [PubMed] [Google Scholar]
- 2.Johnell O., Kanis J. Epidemiology of osteoporotic fractures. Osteoporos Int. 2005;16(Suppl 2):S3. doi: 10.1007/s00198-004-1702-6. [DOI] [PubMed] [Google Scholar]
- 3.Florschutz A.V., Langford J.R., Haidukewych G.J., Koval K.J. Femoral neck fractures: current management. J Orthop Trauma. 2015;29(3):121. doi: 10.1097/BOT.0000000000000291. [DOI] [PubMed] [Google Scholar]
- 4.Schmidt A.H., Swiontkowski M.F. Femoral neck fractures. Orthop Clin North Am. 2002;33(1):97. doi: 10.1016/s0030-5898(03)00074-9. [DOI] [PubMed] [Google Scholar]
- 5.Lu-Yao G.L., Keller R.B., Littenberg B., Wennberg J.E. Outcomes after displaced fractures of the femoral neck. A meta-analysis of one hundred and six published reports. J Bone Joint Surg Am. 1994;76(1):15. doi: 10.2106/00004623-199401000-00003. [DOI] [PubMed] [Google Scholar]
- 6.Stronach B.M., Bergin P.F., Perez J.L. The rising use of total hip arthroplasty for femoral neck fractures in the United States. Hip Int. 2020;30(1):107. doi: 10.1177/1120700019832989. [DOI] [PubMed] [Google Scholar]
- 7.Boniello A.J., Lieber A.M., Denehy K., Cavanaugh P., Kerbel Y.E., Star A. National trends in total hip arthroplasty for traumatic hip fractures: an analysis of a nationwide all-payer database. World J Orthop. 2020;11(1):18. doi: 10.5312/wjo.v11.i1.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hernandez N.M., Chalmers B.P., Perry K.I., Berry D.J., Yuan B.J., Abdel M.P. Total hip arthroplasty after in situ fixation of minimally displaced femoral neck fractures in elderly patients. J Arthroplasty. 2018;33(1):144. doi: 10.1016/j.arth.2017.07.035. [DOI] [PubMed] [Google Scholar]
- 9.Wang F., Zhang H., Zhang Z., Ma C., Feng X. Comparison of bipolar hemiarthroplasty and total hip arthroplasty for displaced femoral neck fractures in the healthy elderly: a meta-analysis. BMC Musculoskelet Disord. 2015;16:229. doi: 10.1186/s12891-015-0696-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Guyen O. Hemiarthroplasty or total hip arthroplasty in recent femoral neck fractures? Orthop Traumatol Surg Res. 2019;105(1S):S95. doi: 10.1016/j.otsr.2018.04.034. [DOI] [PubMed] [Google Scholar]
- 11.Sim F.H., Stauffer R.N. Management of hip fractures by total hip arthroplasty. Clin Orthop Relat Res. 1980;(152):191. [PubMed] [Google Scholar]
- 12.Schmidt A.H., Leighton R., Parvizi J., Sems A., Berry D.J. Optimal arthroplasty for femoral neck fractures: is total hip arthroplasty the answer? J Orthop Trauma. 2009;23(6):428. doi: 10.1097/BOT.0b013e3181761490. [DOI] [PubMed] [Google Scholar]
- 13.Iamthanaporn K., Chareancholvanich K., Pornrattanamaneewong C. Reasons for revision of failed hemiarthroplasty: are there any differences between unipolar and bipolar? Eur J Orthop Surg Traumatol. 2018;28(6):1117. doi: 10.1007/s00590-018-2176-0. [DOI] [PubMed] [Google Scholar]
- 14.Schiavi P., Pogliacomi F., Colombo M., Amarossi A., Ceccarelli F., Vaienti E. Acetabular erosion following bipolar hemiarthroplasty: a Role for the size of femoral head? Injury. 2019;50(Suppl 4):S21. doi: 10.1016/j.injury.2018.11.057. [DOI] [PubMed] [Google Scholar]
- 15.Ravi B., Pincus D., Khan H., Wasserstein D., Jenkinson R., Kreder H.J. Comparing complications and costs of total hip arthroplasty and hemiarthroplasty for femoral neck fractures: a propensity score-matched, population-based study. J Bone Joint Surg Am. 2019;101(7):572. doi: 10.2106/JBJS.18.00539. [DOI] [PubMed] [Google Scholar]
- 16.Kahlenberg C.A., Richardson S.S., Schairer W.W., Cross M.B. Rates and risk factors of conversion hip arthroplasty after closed reduction percutaneous hip pinning for femoral neck fractures-A population analysis. J Arthroplasty. 2018;33(3):771. doi: 10.1016/j.arth.2017.10.004. [DOI] [PubMed] [Google Scholar]
- 17.Chulsomlee K., Sa-Ngasoongsong P., Kulachote N. Hip muscle power recovery after hip replacement using anterior-based muscle-sparing approach in elderly femoral neck fracture: a prospective study in 40 patients. Orthop Res Rev. 2018;10:31. doi: 10.2147/ORR.S153451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Homma Y., Baba T., Ozaki Y. In total hip arthroplasty via the direct anterior approach, a dual-mobility cup prevents dislocation as effectively in hip fracture as in osteoarthritis. Int Orthop. 2017;41(3):491. doi: 10.1007/s00264-016-3332-y. [DOI] [PubMed] [Google Scholar]
- 19.Maceroli M., Nikkel L.E., Mahmood B. Total hip arthroplasty for femoral neck fractures: improved outcomes with higher hospital volumes. J Orthop Trauma. 2016;30(11):597. doi: 10.1097/BOT.0000000000000662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ames J.B., Lurie J.D., Tomek I.M., Zhou W., Koval K.J. Does surgeon volume for total hip arthroplasty affect outcomes after hemiarthroplasty for femoral neck fracture? Am J Orthop (Belle Mead NJ) 2010;39(8):E84. [PubMed] [Google Scholar]
- 21.Kunkel S.T., Sabatino M.J., Kang R., Jevsevar D.S., Moschetti W.E. A systematic review and meta-analysis of the direct anterior approach for hemiarthroplasty for femoral neck fracture. Eur J Orthop Surg Traumatol. 2018;28(2):217. doi: 10.1007/s00590-017-2033-6. [DOI] [PubMed] [Google Scholar]
- 22.Dimitriou D., Helmy N., Hasler J., Flury A., Finsterwald M., Antoniadis A. The role of total hip arthroplasty through the direct anterior approach in femoral neck fracture and factors affecting the outcome. J Arthroplasty. 2019;34(1):82. doi: 10.1016/j.arth.2018.08.037. [DOI] [PubMed] [Google Scholar]
- 23.Oba T., Inaba Y., Saito I., Fujisawa T., Saito T. Risk factors for prolonged operative time in femoral neck fracture patients undergoing hemiarthroplasty through direct anterior approach. J Orthop Sci. 2018;23(6):977. doi: 10.1016/j.jos.2018.07.003. [DOI] [PubMed] [Google Scholar]
- 24.Jewett B.A., Collis D.K. High complication rate with anterior total hip arthroplasties on a fracture table. Clin Orthop Relat Res. 2011;469(2):503. doi: 10.1007/s11999-010-1568-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Watts C.D., Houdek M.T., Wagner E.R., Sculco P.K., Chalmers B.P., Taunton M.J. High risk of wound complications following direct anterior total hip arthroplasty in obese patients. J Arthroplasty. 2015;30(12):2296. doi: 10.1016/j.arth.2015.06.016. [DOI] [PubMed] [Google Scholar]
- 26.Mayr E., Nogler M., Benedetti M.G. A prospective randomized assessment of earlier functional recovery in THA patients treated by minimally invasive direct anterior approach: a gait analysis study. Clin Biomech (Bristol, Avon) 2009;24(10):812. doi: 10.1016/j.clinbiomech.2009.07.010. [DOI] [PubMed] [Google Scholar]
- 27.Singh J.A., Schleck C., Harmsen S., Lewallen D. Clinically important improvement thresholds for Harris Hip Score and its ability to predict revision risk after primary total hip arthroplasty. BMC Musculoskelet Disord. 2016;17:256. doi: 10.1186/s12891-016-1106-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.