Abstract
Introduction:
Orofacial clefts (OFCs) are among the most common craniofacial developmental abnormalities worldwide and a significant cause of childhood morbidity and mortality. This study aimed to identify patterns of patient presentation, treatment approaches, and changes in our overall cleft care service between 2007 and 2019.
Methods and Methodology:
A retrospective review of patients managed at a tertiary health facility in Nigeria of all OFC cases operated between 2007 and 2019 was done using the postintervention data retrieved from the Smile Train database. Data of all OFC cases operated within the period were analyzed using the Statistical Package for the Social Sciences. Descriptive statistics were performed using the Statistical Package for the Social Sciences version 20.0.
Results:
A total number of 740 OFC surgeries were performed in 565 patients, consisting of 269 females (48.2%) and 289 males (51.8%). The majority (63%) of the patients presented before the age of 2 years. Thirty-seven percent presented with cleft lip and alveolus, 27.1% with cleft palate only, and 36.7% with cleft lip, alveolus, and palate. Primary cleft lip repair was the most performed surgery (n = 320, 43.2%), the mean age at repair was 2.1 years. Since 2017, additional services such as speech therapy, mixed dentition orthodontics, and nutritional support were added to services provided to our cleft patients. Fifteen patients have undergone speech assessment and three have completed speech treatment. Eight patients have undergone mixed dentition stage orthodontic treatment.
Discussion:
Our services have evolved from simply providing surgical care to comprehensive care with a multidisciplinary team approach and provision of a wide range of services including nutritional counseling, pediatric care, orthodontic services, and speech therapy. We believe these will improve the overall well-being of our patients while we continue to improve on services based on clinical research outcomes.
Keywords: Cleft care, cleft management, orofacial cleft
INTRODUCTION
Orofacial clefts (OFCs) are among the most common craniofacial developmental abnormalities worldwide and a significant cause of childhood morbidity and mortality. The incidence of these anomalies has been reported to vary according to race, gender, and cleft type.[1,2,3,4] The reported prevalence rate of 0.5/1000 by Adeyemo et al. suggests a relatively low prevalence of OFC in Nigeria.[2] This report may point to underascertainment because the study was purely hospital based. It may also be the true estimate since it is comparable to estimate from South Africa where there is a birth defect registry.[1]
It is generally recognized that the optimum approach to the treatment of children born with cleft defects, either of the lip or palate, is multidisciplinary.[1] The combined efforts of a pediatrician, orthodontist, specialist nurse, cleft surgeon, speech therapist, and ear, nose, and throat specialist are believed to provide the best-combined expertise to ensure that the correct interventions are carried out at the appropriate time to ensure the best functional and esthetic result.[1]
A study of parental experiences among parents of children with OFC revealed the prevalence of stigma and social and structural inequalities due to societal perceptions and misconceptions about OFC.[5] The stigma of an unrepaired OFC greatly alters a child's ability to integrate into the social and cultural environment.[3] This underscores the importance of the face in human interaction. It is considered to be a medium of expression of emotions, verbal and nonverbal communication, and a criterion for social acceptance and mate selection.[4] Early and esthetic surgical repair, especially of the highly visible cleft lip (CL), is of immense benefit to both the patient and parents.
Regular audit of surgical cases is important, especially for assessment of treatment outcomes as well as studies on etiology and prevention of cases.[2] This will lead to an improvement in the standard of care delivery and treatment outcome. The present study reviewed data from cases treated at a tertiary health facility in Nigeria between 2007 and 2019 to identify patterns of patient presentation, treatment approaches, and changes in our overall cleft care service. The study center is a major referral tertiary hospital serving a large catchment population of Southwest Nigeria and neighboring zones.
METHODOLOGY
A retrospective review of all OFC cases repaired at our center from January 2007 to December 2019 using postsurgical intervention data retrieved from the Smile Train database was done. Retrieved data were initially imputed into Microsoft Excel sheet 2010 (Microsoft, Redmond, WA, USA) and were sorted to identify and eliminate double entries, and this was used in analyzing data for the overall surgical intervention and other services provided within the period under review. The data were sorted again to eliminate patients who had received more than one surgical intervention (retained only first presentation) and this was used to analyze data for patient presentation and diagnosis. Data analyzed included age of patients, gender, cleft type, laterality of cleft, type of repair done, technique of surgical repair, surgical complications, and other services provided. The cleft type was classified as CL and alveolus (CLA) only, CLA palate (CLAP), and cleft palate only (CPO). The CLA was further classified into bilateral CLA and unilateral CLA. The unilateral CLA was further classified into the right and left unilateral CLA. The CLAP cases were also classified into bilateral CL and palate and unilateral CL and palate, which was further classified as right and left unilateral cleft lip and palate. Other types of OFCs using the Tessier OFC classification were also recorded. Descriptive statistics were performed using the Statistical Package for the Social Sciences version 20.0 (SPSS Inc., Chicago, IL, USA).
RESULTS
A total number of 740 OFC surgeries were done in 565 patients within the period under review. There were more males (51.8%) than females (48.2%), with a male: female ratio of 1.1:1. The age range of patients was 0.3–57.9 years (median 1.1 years; mean 5.5 years, standard deviation [SD] ± 9.5) with the majority (63.0%) of the patients under the age of 2 years, while 15.6% were older than 12 years [Table 1]. The most common presentation was CLA (37.5%, n = 209), followed by CLP (36.7%, n = 199) and CPO (27.1%, n = 151). Cases of Tessier OFCs were rare accounting for only 2.1% (n = 11) of all cases seen, and they were more common in females (n = 9). CPO was more common in females (n = 90), while more males presented with left-sided unilateral CLA (n = 60) [Table 2].
Table 1.
Descriptive statistics of operated cases
| Operation | n (%) | Age (years) | Weight (kg) | ||
|---|---|---|---|---|---|
| Median | Mean±SD | Median | Mean±SD | ||
| Primary lip unilateral | 244 (33.3) | 0.3 | 2.7±7.5 | 6.0 | 11.2±15.0 |
| Primary lip bilateral | 76 (10.4) | 0.3 | 2.1±5.9 | 5.5 | 10.0±14.3 |
| Primary cleft palate | 250 (34.1) | 1.9 | 5.5±8.1 | 11.9 | 19.2±17.7 |
| Lip revision | 46 (6.3) | 4.8 | 11.1±14.5 | 16.5 | 29.2±24.9 |
| Fistula repair | 75 (10.2) | 6.9 | 11.4±10.5 | 22.8 | 32.2±21.5 |
| Alveolar bone graft | 38 (5.2) | 9.7 | 13.8±7.4 | 32.0 | 40.0±17.2 |
| Tessier | 11 (0.5) | 0.3±0.1 | 5.6±0.3 | ||
| Total | 740 (100) | ||||
SD: Standard deviation
Table 2.
The distribution into the various cleft types by gender and laterality
| Cleft type | |||||||
|---|---|---|---|---|---|---|---|
| Gender | BCLA | BCLP | RUCLA | LUCLA | CPO | RUCLP | LUCLP |
| Male | 18 | 36 | 39 | 60 | 61 | 29 | 45 |
| Female | 17 | 23 | 29 | 42 | 90 | 37 | 29 |
| Total | 35 | 59 | 68 | 102 | 151 | 66 | 74 |
BCLA: Bilateral cleft lip and alveolus, BCLP: Bilateral cleft lip and palate, RUCLA: Right unilateral cleft lip and alveolus, LUCLA: Left unilateral cleft lip and alveolus, CPO: Cleft palate only, RUCLP: Right unilateral cleft lip and palate, LUCLP: Left unilateral cleft lip and palate
The highest number of surgical interventions was done between 2010 and 2011 (n = 160), dropped over the following years, and increased again in the 2019 operating year [Figure 1]. Primary CL repair was the most performed surgery (n = 320, 43.7%) and the majority of these cases were unilateral lip, while 76 were primary bilateral CL repairs [Table 1]. Most of these surgeries (3.7%) were done under general anesthesia. The median age at repair was 0.3 years (mean: 2.5 years, SD ± 7.1, range: 0.3–51.2). The Millard rotation-advancement technique and its modifications were the most adopted for unilateral CL repair (n = 145, 59.3%), followed by the Tennison–Randall triangular flap technique (n = 90, 37.0%). Other techniques were used in only 3.7% of cases (n = 9). The median age at CL repair was 0.3 years (range: 0.26–30.3) years. The mean ages of the patients at the time of primary lip repair per year are shown in Figure 2, with the highest mean ages recorded between 2007 and 2009.
Figure 1.
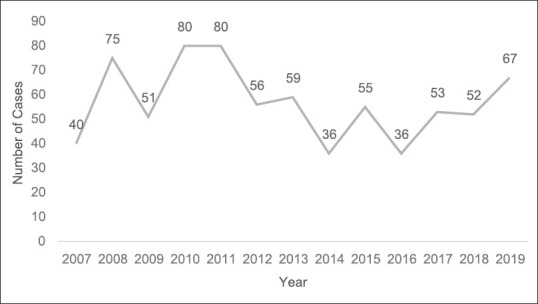
Showing the yearly distribution of surgical cases
Figure 2.
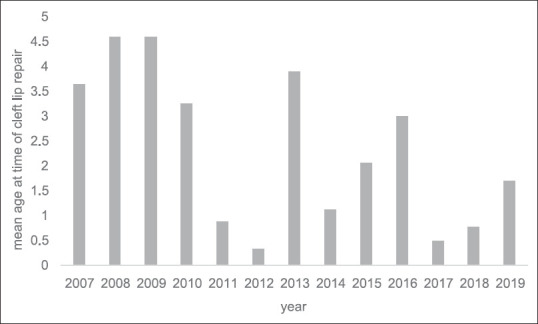
Shows the mean age of patients at the time of primary cleft lip repair per year
The most common method of repair of BCL was the modified Millard Forked Flap technique which was used in 72.4% (n = 55) of the cases, the straight-line technique in only 5.3% (n = 4), and other techniques in 7.9% (n = 6). A total of 46 lip nose revision surgeries were performed, resulting in an approximate revision rate of 14.4%. Two hundred and fifty primary palatoplasty cases were done within the period, of which four were submucous cleft of the palate. The median age at repair was 1.9 (range: 0.8–45.5) years. The von Langenbeck technique was the most commonly used technique of repair of cleft palate (89.2%, n = 223), Bardach two-flap technique (6.4%, n = 16), Furlow's double-opposing Z-plasty (0.8%, n = 2), and Veau–Wardill–Kilner technique (0.8%, n = 2). A total cases of oronasal fistula repair were 75, resulting in an estimated complication rate of primary palatoplasty of 30%. Von Langenbeck technique was the most used in oronasal fistula closure (89.3%) and the mean age of the patients at the time of primary palate repair per year is shown in Figure 3, with the highest mean age recorded in 2013.
Figure 3.
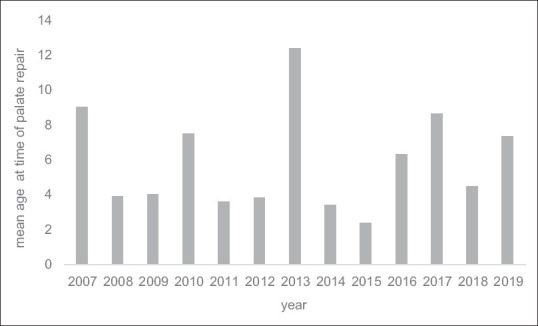
Shows the mean age of patients at the time of primary cleft palate repair per year
Thirty-eight alveolar bone graft cases were done within the period, the median age of patients was 9.7 (range 7.0–30.9) years. Since the 2017 operating year, additional services such as speech therapy and nutritional support were added to services provided to our cleft patients.
DISCUSSION
A remarkable method of achieving quality improvement in any aspect of clinical medicine is a careful clinical audit.[1] Our OFC management team is multidisciplinary, involving nurses, maxillofacial surgeons, pediatric cardiologists, speech therapists, nutritionists, pediatric dentists, orthodontists, anesthesiologists, and otorhinolaryngologists (ORLs). Regular OFC clinic runs once a week, with an average of two new cases every clinic day. Management protocol entails psychological and feeding counseling of all new cases by the team nurses followed by an assessment by the pediatric cardiologists and ORL. CL repair is done at 3 months of age, provided the following conditions are met; patient weighs at least 4.5Kg; with minimum hemoglobin concentrationn of 10 g/dl and cleared for surgery by the team anesthesiologist and pediatric cardiologist. Simple presurgical orthopedics with lip strapping was always done by the orthodontist for wide clefts.
The mean age of patients at the time of CL and palate repair was above 2 years. However, the majority of the cases were repaired at 3 months of age for CL and 12–18 months for cleft palate. The relatively high mean is due to the late presentation of a number of our cases (37.0%) after the age of 2 years which was a common phenomenon at the onset of the program, and this is not uncommon in our environment.[5,6] Reasons for delay in presentation include ignorance and financial constraint.[6,7] Patients' inability to pay out of pocket for the required surgical intervention may have resulted in a backlog of cases we saw at the onset of the sponsored surgical intervention program at our center in the first few years. The gender distribution of patients in this series showing a slightly higher male preponderance overall, and a higher incidence of cleft palate among females, is consistent with published data on the epidemiology of OFC.[8,9] Other studies also show similar gender distribution patterns.[10,11,12,13,14,15] CLA was the most common diagnosis made which concur with previous local studies which also showed a similar trend.[15,16] Other authors have however reported CL and palate to be more prevalent in their centers.[17,18,19,20] Furthermore, similar to previous studies, we found unilateral clefts occurring more often on the left than the right side.[11,21]
The versatility of Millard's rotation-advancement technique (with primary closed rhinoplasty) of CL repair makes it the most common choice (used in 59% of cases) at our center. However, the Tennison–Randall triangular flap technique was also used. A comparison of the outcome of both techniques among patients in an earlier study found no significant differences in the surgical outcomes from the two techniques. Nonetheless, Millard's technique resulted in a greater increase in postoperative horizontal length and vertical lip height, and a greater reduction in nasal width and total nasal width, while the Tennison–Randall technique showed a better reduction of Cupid's-bow width and better philtral height.[21] The BCL repair is done using a modification of Millard's forked flap technique as described by Adeyemo et al.[22] Eleven cases of facial clefts were recorded. This is likely to be an underestimation of cases of facial clefting since the pro forma for data recording did not make specific provision for such diagnosis.
CP repair is routinely done at 12 months of age in our center or as soon as possible in patients who present later than 12 months. The mean age at which cleft palate was repaired in our series was high, and this is due to late presentation. The late presentation may have been aided by the fact that the cleft palate is not visible in contrast to CL, and therefore, caregivers are not as motivated to seek care (especially in CPO cases) compared to the highly visible CL. Furthermore, some parents were not aware their child had a CP until they noticed speech impairment or the child started school. Majority of our CP cases are repaired using the von Langenbeck bipedicled flap technique with intravelar veloplasty, adjunctive use of vomer flap is incorporated in wide cases. We have also found the Bardach technique to be quite useful in cases of bilateral complete cleft of the palate. Complications following palate repair (such as oronasal fistula formation, occurring mostly at the junction of hard and soft palate) have previously been estimated from local data to be 29.8%.[7] Data from this study resulted in an estimate of about 30% and this was extrapolated from number of cases of oronasal fistula repair. The cases of submucous cleft palate recorded within the review period are much higher than previously reported.[8] Although the issue of underascertainment is still relevant, especially as this was an hospital record-based study and many cases may not present due to the inconspicuous nature of the condition.
The routine protocol of managing alveolar cleft at our center is secondary alveolar bone grafting using autogenous bone harvested from the iliac crest at between the ages of 7 and 9 years. This is to allow for the positioning of the erupting lateral incisor and guide eruption of canine by our orthodontics team. Grafting before eruption of the permanent canine teeth generally has been reported to result in more stability with better crestal bone support.[23] All patients for alveolar cleft repair had presurgical orthodontics assessment and palatal expansion if required and afterward orthodontic alignment of teeth.
In addition to the relatively long-standing surgical intervention services provided at our center, additional services such as postsurgical orthodontic treatment were included in July 2017, speech assessment and therapy in July 2018, and nutritional support services in July 2019. These additional services were necessitated by the needs of our patients, as the patients who were treated in infancy grew to require other treatments. This shows an evolution toward a truly comprehensive multidisciplinary cleft care team which will be improved upon within the near future. We provide a specially constituted infant formula for our cleft patients in their infancy to help with their nutrition, especially to those whose mothers are having difficulty breastfeeding or those with unsatisfactory growth rate despite breastfeeding. This formula consists majorly of locally available ingredients such as yellow corn, guinea corn, soybeans, and air-dried fish. Anecdotal evidence has shown significant improvements in the weight gain of our patients on this formula.
The 2010–2011 operating years recorded a peak in the number of surgical interventions, and the number operated yearly declined afterward with the least number of operated cases recorded in 2014 and 2016. This was due majorly to an increase in the number of centers within the catchment area of our institution assessing the grant of the Smile Train Organization. However, an increase in the frequency of community outreaches by our team has resulted in a gradual increase in cleft patient inflow at our clinic. We expect these numbers to increase in the following years since only West African College of Surgeons certified clefts surgeons will be allowed to conduct cleft surgeries.
CONCLUSION
The past 12 years has revealed a gradual expansion in the range of cleft care provided at our center. This has evolved from simply providing surgical care to a multidisciplinary team approach and provision of a wide range of services including nutritional counseling, pediatric care, orthodontic services, speech therapy, in addition to the required surgical interventions. We believe that these will improve the overall well-being of our patients while we continue to improve on services following clinical research outcomes.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
Our sincere appreciation goes to Smile Train Organization (http://www.smiletrain.org/).
REFERENCES
- 1.Kromberg JG, Jenkins T. Common birth defects in South African Blacks. S Afr Med J. 1982;62:599–602. [PubMed] [Google Scholar]
- 2.Adeyemo WL, James O, Butali A. Cleft lip and palate: Parental experiences of stigma, discrimination, and social/structural inequalities. Ann Maxillofac Surg. 2016;6:195–203. doi: 10.4103/2231-0746.200336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Conway JC, Taub PJ, Kling R, Oberoi K, Doucette J, Jabs EW. Ten-year experience of more than 35,000 orofacial clefts in Africa. BMC Pediatr. 2015;15:8. doi: 10.1186/s12887-015-0328-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fink B, Neave N. The biology of facial beauty. Int J Cosmet Sci. 2005;27:317–25. doi: 10.1111/j.1467-2494.2005.00286.x. [DOI] [PubMed] [Google Scholar]
- 5.Oladele AO, Olabanji JK, Awe OO. Adolescent and adult cleft lip and palate, in Ile-Ife, Nigeria. Niger J Clin Pract. 2012;15:403–7. doi: 10.4103/1119-3077.104512. [DOI] [PubMed] [Google Scholar]
- 6.Adeyemo WL, Ogunlewe MO, Desalu I, Ladeinde AL, Mofikoya BO, Adeyemi MO, et al. Cleft deformities in adults and children aged over six years in Nigeria: Reasons for late presentation and management challenges. Clin Cosmet Investig Dent. 2009;1:63–9. doi: 10.2147/ccide.s6686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Abdurrazaq TO, Micheal AO, Lanre AW, Olugbenga OM, Akin LL. Surgical outcome and complications following cleft lip and palate repair in a teaching hospital in Nigeria. Afr J Paediatr Surg. 2013;10:345–57. doi: 10.4103/0189-6725.125447. [DOI] [PubMed] [Google Scholar]
- 8.Butali A, Adeyemo WL, Mossey PA, Olasoji HO, Onah II, Adebola A, et al. Prevalence of orofacial clefts in Nigeria. Cleft Palate Craniofacial J. 2014;51:320–5. doi: 10.1597/12-135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Butali A, Mossey PA. Epidemiology of Orofacial clefts in Africa: Methodological challenges in ascertainment. Pan Afr Med J. 2009;2:5. doi: 10.4314/pamj.v2i1.51705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shapira Y, Blum I, Haklai Z, Shpack N, Amitai Y. Nonsyndromic orofacial clefts among Jews and non-Jews born in 13 hospitals in Israel during 1993-2005. Community Dent Oral Epidemiol. 2018;46:586–91. doi: 10.1111/cdoe.12395. [DOI] [PubMed] [Google Scholar]
- 11.Azeez B, Keyla PR, Deborah VD, Ronald M, Mekonen AE, Wasiu LA, et al. Descriptive epidemiology of orofacial clefts in Africa using data from 46,502 Smile Train surgeries. J Public Heal Epidemiol. 2017;9:114–21. [Google Scholar]
- 12.Eshete M, Butali A, Deressa W, Pagan-Rivera K, Hailu T, Abate F, et al. Descriptive epidemiology of orofacial clefts in ethiopia. J Craniofac Surg. 2017;28:334–7. doi: 10.1097/SCS.0000000000003234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jensen BL, Kreiborg S, Dahl E, Fogh-Andersen P. Cleft lip and palate in Denmark, 1976-1981: Epidemiology, variability, and early somatic development. Cleft Palate J. 1988;25:258–69. [PubMed] [Google Scholar]
- 14.Pavri S, Forrest CR. Demographics of orofacial clefts in Canada from 2002 to 2008. Cleft Palate Craniofac J. 2013;50:224–30. doi: 10.1597/10-223. [DOI] [PubMed] [Google Scholar]
- 15.Adeola D, Ononiwu C, Eguma S. Cleft lip and palate in northern Nigerian children. Ann Afr Med. 2003;2:6–8. [Google Scholar]
- 16.Efunkoya AA, Omeje KU, Amole IO, Osunde OD, Akpasa IO. A review of cleft lip and palate management: Experience of a Nigerian Teaching Hospital. Afr J Paediatr Surg. 2015;12:257–60. doi: 10.4103/0189-6725.172566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yılmaz HN, Özbilen EÖ, Üstün T. The prevalence of cleft lip and palate patients: A single-center experience for 17 Years. Turk J Orthod. 2019;32:139–44. doi: 10.5152/TurkJOrthod.2019.18094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Impellizzeri A, Giannantoni I, Polimeni A, Barbato E, Galluccio G. Epidemiological characteristic of Orofacial clefts and its associated congenital anomalies: Retrospective study. BMC Oral Health. 2019;19:290. doi: 10.1186/s12903-019-0980-5. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 19.Sato Y, Yoshioka E, Saijo Y, et al. Trajectories of the Psychological Status of Mothers of Infants With Nonsyndromic Orofacial Clefts: A Prospective Cohort Study From the Japan Environment and Children's Study. The Cleft Palate-Craniofacial Journal. 2020 Aug; doi: 10.1177/1055665620951399. doi:10.1177/1055665620951399. [DOI] [PubMed] [Google Scholar]
- 20.Vyas T, Gupta P, Kumar S, Gupta R, Gupta T, Singh H. Cleft of lip and palate: A review. J Fam Med Prim Care. 2020;9:2621. doi: 10.4103/jfmpc.jfmpc_472_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Adetayo AM, James O, Adeyemo WL, Ogunlewe MO, Butali A. Unilateral cleft lip repair: A comparison of treatment outcome with two surgical techniques using quantitative (anthropometry) assessment. J Korean Assoc Oral Maxillofac Surg. 2018;44:3–11. doi: 10.5125/jkaoms.2018.44.1.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Adeyemo WL, James O, Adeyemi MO, Ogunlewe MO, Ladeinde AL, Butali A, et al. An evaluation of surgical outcome of bilateral cleft lip surgery using a modified Millard's (Fork Flap) technique. Afr J Paediatr Surg. 2013;10:307–10. doi: 10.4103/0189-6725.125419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dasari MR, Babu VR, Apoorva C, Allareddy S, Devireddy SK, Kanubaddy SR. Correction of secondary alveolar clefts with iliac bone grafts. Contemp Clin Dent. 2018;9:S100–6. doi: 10.4103/ccd.ccd_109_18. [DOI] [PMC free article] [PubMed] [Google Scholar]


