Abstract
Introduction:
Ankylosis is a physically and psychologically distressing condition to a patient. The aim of this study was to evaluate the efficiency of custom-made temporomandibular joint (TMJ) prosthesis (fossa-condyle component) in patients with unilateral ankylosis in restoring the form and functions of the TMJ.
Materials and Methods:
This retrospective study was conducted in ten patients with unilateral TMJ ankylosis who had undergone TMJ reconstruction with custom-made TMJ prosthesis. Clinical parameters assessed were maximal mouth opening, lateral movements, improvement of the pain levels, and dietary efficiency of the patient. The data were analyzed using SPSS version 20 (IBM Corporation, SPSS Inc.; Chicago, IL, USA).
Results:
The mean preoperative mouth opening was 5.70 ± 3.62 mm. After gap arthroplasty, it was 32.50 ± 3.31 mm. The postoperative mouth opening after the reconstruction of TMJ using alloplastic joint prosthesis was 34.90 ± 2.69 mm, and after a mean follow-up period of 4 years, the mean postoperative mouth opening was 34.60 ± 2.50 mm. The mean preoperative movement toward the right and left side was 0.9 ± 1.2 mm and 1.3 ± 1.25 mm, respectively. The mean right and left lateral movements of the TMJ after reconstruction were 3.5 ± 0.97 mm and 3.70 ± 1.06 mm, respectively. There was decrease in deviation of the unaffected jaw during mouth opening and closure. Functional occlusion was maintained postoperatively. There was no appreciable change in the visual analog pain scales. The dietary efficiency improved from a scale of 10 (liquids) to a scale of 0 (no restriction to diet) in eight patients and 1 in two patients. The dietary score improved significantly after alloplastic reconstruction (P = 0.000). No evidence of facial nerve paralysis or foreign body reactions was noted in the patients during the follow-up period. Radiographic assessment revealed good positioning and adaptation of the fossa component and the condylar ramal component both postoperatively and after a mean 4-year follow-up period. There was no evidence of screw loosening or prosthesis breakage during the follow-up period.
Discussion and Conclusion:
The custom-made TMJ-total joint replacement (TJR) devices provide stable, improved long-term results, thereby increasing the quality of life of the patient. The custom-made alloplastic TMJ-TJR prosthesis proves to be the optimal surgical procedure to reconstruct the TMJ in comparison to the autogenous grafts (to avoid complications) in severe degenerated and ankylosed joints. However, long-term clinical and radiological studies on a larger sample size are imperative to establish the versatility of this procedure.
Keywords: Temporomandibular joint ankylosis, temporomandibular joint custom made prosthesis, temporomandibular joint reconstruction
INTRODUCTION
Ankylosis is a physically and psychologically distressing condition to a patient. The temporomandibular joint (TJR) reconstruction is a very challenging procedure for a surgeon because of the integral role of the TMJ in establishing and maintaining proper form and function within the stomatognathic system. The TMJ plays a pivotal role as a secondary growth center for the growth of the mandible and is involved in functions of mastication, speech, and deglutition throughout life.
The traditional treatment modalities that are used in the management of ankylosis are the gap arthroplasty which was later replaced by the interposition gap arthroplasty.[1] The interpositional gap arthroplasty utilizes the advantages of biological tissues such as autogenous bone, myofascial flaps, cartilages, and fascia lata as well as nonbiological materials such as acrylic and silastic.[2] Autogenous bone grafts (costochondral,[3] sternoclavicular,[4] metatarsal,[5] iliac crest,[6] fibula,[7] and coronoid[8]) though have benefits of biological compatibility and growth potential in children, the unpredictable nature of growth of the grafts, the donor-site morbidity, the altered uptake of the grafts, and the chances of reankylosis led to the use of alloplasts as interpositional materials. The function in case of autografts is delayed as early mandibular mobility will result in reduced nascent blood supply to the graft interfering with incorporation of the graft into the host environment leading to graft failure which seems to be another disadvantage of the autogratfs. Marx[9] reported that capillaries can penetrate a maximum thickness of 180 μm–220 μm of tissue, whereas scar tissue surrounding previously operated bone averages 440 μm in thickness. Hence, the success of placing an autogenous graft in multiply operated TMJs or in case of reankylosis is always questionable, and there arose the need for an alternative treatment modality such as alloplastic TMJ prosthesis.
The advantages of the TMJ-total joint replacement (TMJ-TJR) devices are lack of donor-site morbidity, ability to maintain a stable occlusion postsurgically because of lack of dimensional change in implant, as opposed to potential resorption of autogenous graft, opportunity to manipulate prosthesis design to discourage heterotopic bone formation, potential to maintain vertical height of ramus and prevent deviation of jaw, reduced surgical time, decreased hospitalization, and immediate function.[10] There are two categories of TJR devices approved by the Food and Drug Administration for implantation in the United States.[11] They are stock (off-the-shelf) devices which the surgeon has to “make fit” at implantation and custom (patient-fitted) devices which are “made to fit” for each specific case.
Custom TMJ-TJR devices, by the nature of metals used, design of the prosthesis, and biomaterial composition, appear to provide stable, improved long-term outcomes over stock devices. The advantages of the custom-made devices in contrast to stock devices are that the custom-made system is virtually a perfect fit into the host bone every time, making it more predictable, thus reducing operating time. Custom-made joints also allow for a change in anteroposterior and vertical dimensions, thus enabling changes to be made in the occlusion.[12] Studies on total alloplastic TMJ replacement outcomes showed acceptable improvements in terms of both pain levels and jaw functions, thus making these interventions worthy of further evaluation.
The cost of the devices, material wear and failure, long-term stability, and their restriction in following the growth of the patient have always been a matter of concern in using alloplastic TMJ reconstruction prosthesis. Hence, the purpose of this study was to evaluate the efficiency of custom-made TMJ prosthesis (fossa-condyle component) in patients with ankylosis in terms of restoring form and function of the TMJ. Moreover, an attempt has also been made to reduce the cost factor, which seems to be the main restriction in using these devices in the developing and the underdeveloped countries of the world.
The objectives of the study were to assess the mouth opening, range of mandibular movements possible, usage of the devices in growing patients, and its effect on the growth, the dietary efficacy, and the long-term stability of the device.
MATERIALS AND METHODS
Study design and setting
This study was an evaluative study of patients with unilateral TMJ ankylosis in whom TMJ ankylosis release and TMJ reconstruction with custom-made TMJ-TJR prosthesis were carried out. Patients with unilateral TMJ ankylosis who were referred to the department of oral and maxillofacial surgery from December 2013 to April 2015 were included in the study. The required data were collected from the clinical records of the patient and from the patients at consecutive follow-up period.
Inclusion criteria
Patients within the age group of 10–40 years, with unilateral TMJ ankylosis
Patients who had undergone TMJ ankylosis release and TMJ reconstruction with custom-made alloplastic TMJ prosthesis
Patients presenting no systemic contraindication for the surgical procedure
Those willing to cooperate for the surgery and further follow-up.
Exclusion criteria
Medically compromised patients
Patients allergic to metal alloys
Patients with incomplete clinical and radiological data
Patients who had undergone TMJ reconstruction with autogenous bone grafts.
Parameters assessed
The clinical parameters assessed were maximal mouth opening and lateral movements, the improvement of the pain levels, and the dietary efficiency of the patient. Maximal mouth opening and lateral excursions were evaluated before the release of ankylotic mass, after the release, before the reconstruction of TMJ with the alloplastic joint prosthesis, and thereafter. Radiographic evaluation included orthopantomogram (OPG) and computed tomography (CT) scans. The improvement in pain scales was evaluated by means of visual analog pain scale with a score 0 (no pain) to 10 (maximal bearable pain).[13] Visual analog scores were assessed postrelease of ankylosis, post-TMJ reconstruction, and after a 5-year follow-up period on joint movements. The diet efficiency was similarly assessed with a scale of 0 (with no restriction of diet) to 10 (liquids only).[10] Postoperative evaluation of the position of the prosthesis was done by OPG. The other clinical parameters evaluated were wound infection and evidence of any neurological deficit. Clinically facial nerve paralysis was assessed by evaluating the patient's ability to raise the eyebrows and tight closure of eyelids
Sample size
Inability in mouth opening or a limited mouth opening was the chief complaint in all patients [Figure 1a]. Twenty-one patients presented with ankylosis during the study period of which ten patients who met the inclusion criteria were included in the study.
Figure 1.

(a) Preoperative frontal view. (b) Preoperative computed tomographic scan showing ankylosis of temporomandibular joint - coronal view
Statistical analysis
The data were analyzed using SPSS version 20 (IBM Corporation, SPSS Inc.; Chicago, IL, USA). Paired t-test was used to compare the pre- and post-operative dietary score and laterotrusive movements. Repeated-measure ANOVA was used to compare the mouth opening preoperatively, after gap arthroplasty, after TMJ reconstruction, and after a 5-year follow-up period. A P < 0.05 was considered statistically significant.
The study was carried out after approval from the institutional ethical committee (Tamil Nadu Government Dental College and Hospital, 0430/DE/2010 dated November 21, 2013) adhering to the ethical guidelines of Declaration of Helsinki, and informed consent was obtained from each patient in the regional language (Tamil) for both the surgery and the study explaining the nature of the surgical procedure and the outcome, potential risks, and benefits of participating in the study both during the first, second surgery and even during the follow-up period.
After eliciting a detailed history, a thorough clinical examination was carried out. A two-stage surgery was planned; the first was the release of ankylotic mass and the second was the reconstruction of the TMJ using an alloplastic joint prosthesis. The second stage of the surgery was done after a month of gap arthroplasty.
CT scans were taken preoperatively to assess the extent of ankylosis [Figure 1b]. The fabrication of a custom-made alloplastic joint prosthesis obviates the use of the stereolithographic model. Hence, for each patient, CT scans were taken in axial, coronal, and sagittal sections (0.5 mm thickness) with a three-dimensional (3D) reconstruction after the ankylosis release, and a patient-specific 3D model was then developed using these CT data. The use of the stereolithographic model offers an accurate fabrication of the prosthesis conforming to patient's “specific anatomical morphology and jaw interrelationships.” The joint prosthesis essentially consists of two components, the glenoid fossa component and condylar ramal component, and both the glenoid fossa component and the ramal condylar component were made of cast cobalt-chromium-molybdenum (Co–Cr–Mb) alloy. The glenoid fossa and condylar ramal component had screw holes drilled in it to accommodate screws of 2 and 2.5 mm diameter, respectively.
Surgical procedure
The surgical procedure was done in two stages. Both the procedures were done under general anesthesia with blind nasal intubation in two patients and fiber-optic-assisted nasoendotracheal intubation in eight patients, for Stage 1 (gap arthroplasty) procedure. For Stage 2 procedure in which the reconstruction of the TMJ was done using alloplastic joint prosthesis, all ten patients were intubated nasoendotracheally. The incision used in all cases was the preauricular incision with a temporal extension, the Al-Kayat–Bramley modification[14] for the purpose of greater access [Figure 2a]. At the root of the zygoma, an inverted L-shaped incision was made just 2 mm above the zygomatic arch, through both the superficial layer of temporalis fascia and periosteum of the zygomatic arch to expose the ankylotic mass [Figure 2b]. The ankylosed segment was removed in increments by upper and lower osteotomy cuts, and a gap of about 1.5 cm was achieved [Figure 2c]. The mouth opening achieved was 31–34 mm after gap arthroplasty. In all the cases, coronoid hypertrophy was observed, and ipsilateral coronoidectomy was performed as an adjuvant therapy to improve the mouth opening.[15] Postoperatively, patients were administered antibiotics and analgesics for 5 days. Active mouth opening exercises were initiated from the third postoperative day. Sutures were removed on the 10th postoperative day. Heister jaw opener was applied thereafter to improve and maintain mouth opening. Patients were followed up every week postoperatively. Patients were taken up for second-stage surgery 1 month later. CT scans were taken before the surgery for the purpose of stereolithographic model [Figure 3a–c] and prosthesis fabrication [Figure 4a and b]. The approach to the field of surgery was through the existing scar. The gap created earlier was cleared of all soft tissue adherence for the insertion of the glenoid fossa component. The glenoid fossa component was then placed to check for its fit and adaptation over the zygomatic arch and temporarily secured to the position using 2 mm × 6 mm screws [Figure 5a]. For the insertion of condylar ramal component, a submandibular incision was planned. Layer-wise dissection was carried out, pterygomasseteric sling was incised, and exposure to bone was made submasseterically. Condylar ramal component was then positioned and checked for its adaptation and fit [Figure 5b]. Intraorally intermaxillary fixation (IMF) was done. After accomplishing it, condylar ramal component was fixed using 2.5 mm × 8 mm screws. IMF was then released and the condylar movements are performed. Then, the screws were finally tightened over the glenoid fossa and condylar ramal component [Figure 5c]. Copious amount of povidone iodine and saline irrigation was done, and closure was accomplished layer-wise using 3-0 vicryl and 3-0 ethilon. Patients were administered antibiotics and analgesics for 5 days. Patients were kept in IMF for 7 days and active physiotherapy was started thereafter. The skin sutures were removed on the 10th day. The patients were followed up periodically monthly once during the immediate postoperative period, and thereafter, yearly follow-up was done.
Figure 2.
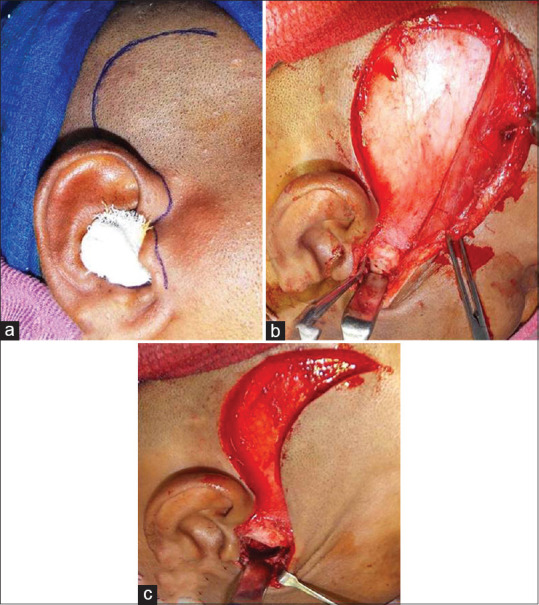
(a) Al-Kayat–Bramley incision. (b) Exposure of ankylotic mass. (c) Gap arthroplasty
Figure 3.
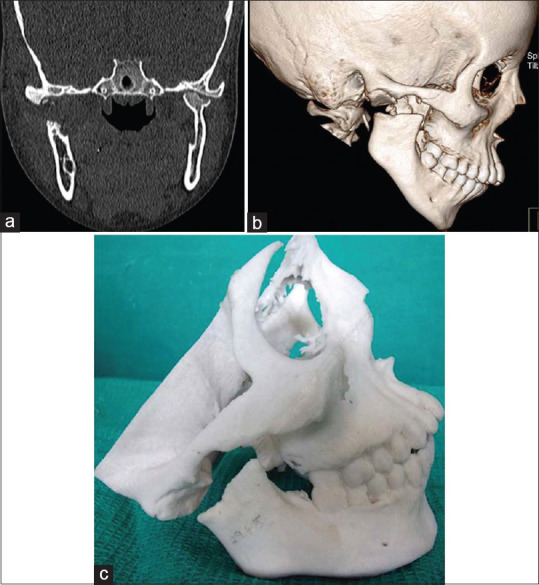
(a) Postoperative computed tomographic showing gap arthroplasty - coronal view. (b) Postoperative computed tomographic showing gap arthroplasty - three-dimensional reconstruction image. (c) Stereolithographic model after gap arthroplasty
Figure 4.
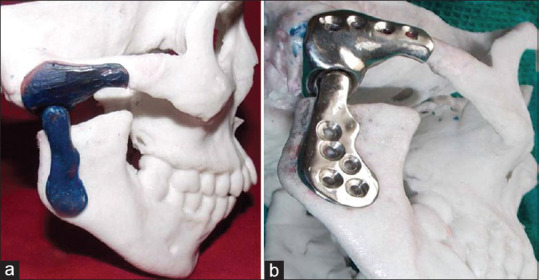
(a) Fabrication of custom-made temporomandibular joint prosthesis. (b) Custom-made temporomandibular joint prosthesis made using cobalt-chromium-molybdenum
Figure 5.
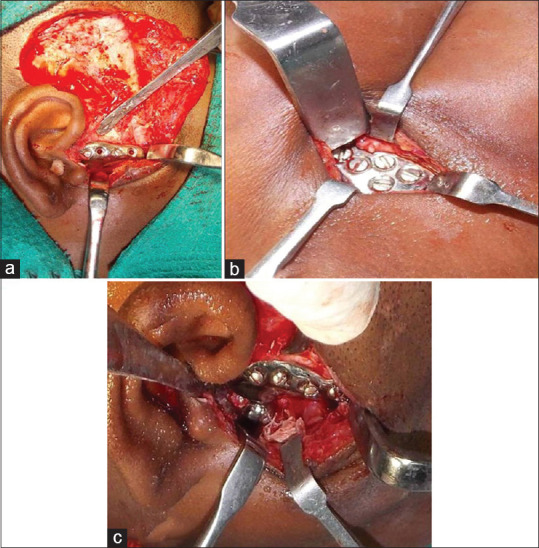
(a) Fixation of glenoid fossa component of the temporomandibular joint prosthesis. (b) Fixation of condylar-ramal component of the temporomandibular joint prosthesis. (c) Custom-made temporomandibular joint prosthesis fixation
RESULTS
Twenty-one patients presented with ankylosis during the study period of which ten patients who met the inclusion criteria were assessed. The mean follow-up period was 4 years. The mean age of the patients included in the study was 17.8 ± 2.66 years. 80% of the patients were male, and the ankylosis was attributed to trauma in all the cases. Left-sided ankylosis was observed in six patients [Table 1].
Table 1.
Demographic data of the patient
| Age of the patient in yrs | Sex | Ankylosis side | Etiology of Ankylosis |
|---|---|---|---|
| 14 | Male | Left | Trauma |
| 16 | Female | Right | Trauma |
| 18 | Male | Right | Trauma |
| 20 | Male | Left | Reankylosis |
| 22 | Male | Left | Trauma |
| 15 | Male | Left | Reankylosis |
| 17 | Male | Right | Trauma |
| 16 | Female | Left | Trauma |
| 19 | Male | Right | Trauma |
| 21 | Male | Left | Reankylosis |
The mean preoperative mouth opening was 5.70 ± 3.62 mm [Figure 6a]; after gap arthroplasty, it was 32.50 ± 3.31 mm [Figure 6b]. The postoperative mouth opening after the reconstruction of TMJ using alloplastic joint prosthesis was 34.90 ± 2.69 mm [Figure 6c], and after a mean period of 4-year follow-up, it was 34.60 ± 2.50 mm [Figure 6d]. Statistical analysis using repeated-measures ANOVA showed that there was a significant improvement in mouth opening postoperatively both after gap arthroplasty and alloplastic TMJ reconstruction and after 4-year follow-up (P = 0.0001) compared with preoperative mouth opening [Table 2].
Figure 6.

(a) Preoperative mouth opening. (b) Postoperative mouth opening after gap arthroplasty. (c) Postoperative mouth opening after alloplastic temporomandibular joint reconstruction. (d) Postoperative mouth opening after 5-year follow-up
Table 2.
Mouth opening in mm
| Serial number | Maximum Incisal Opening (MIO) | P | |||
|---|---|---|---|---|---|
| Preoperative | After gap arthroplasty | After alloplastic TMJ reconstruction | 5-year follow-up | ||
| 1. | 6 | 26 | 30 | 32 | <0.001* |
| 2. | 0 | 30 | 34 | 30 | |
| 3. | 10 | 35 | 36 | 35 | |
| 4. | 10 | 37 | 39 | 37 | |
| 5. | 0 | 35 | 38 | 38 | |
| 6. | 4 | 30 | 33 | 35 | |
| 7. | 6 | 32 | 34 | 36 | |
| 8. | 7 | 34 | 35 | 36 | |
| 9. | 9 | 31 | 33 | 32 | |
| 10. | 5 | 35 | 37 | 35 | |
| Mean | 5.7 | 32.5 | 34.9 | 34.6 | |
*Repeated Measures ANOVA: The mean difference is statistically significant. TMJ=Temporomandibular joint
The mean preoperative movement toward the right and left side was 0.9 ± 1.2 mm and 1.3 ± 1.25 mm, respectively. The mean right and left lateral movements of the TMJ after reconstruction were 3.5 ± 0.97 mm and 3.70 ± 1.06 mm, respectively. There was significant improvement in lateral movements of the jaw following the reconstruction of the joint (P = 0.000) [Table 3]. There was decrease in deviation of the unaffected jaw during mouth opening and closure. Functional occlusion was maintained postoperatively.
Table 3.
Temporomandibular joint movements: Laterotrusive movements
| Serial number | Laterotrusive movements in mm (right) | P | Laterotrusive movements in mm (left) | P | ||
|---|---|---|---|---|---|---|
| Preoperative | Postoperative (after alloplastic TMJ reconstruction) | Preoperative | Postoperative (after alloplastic TMJ reconstruction) | |||
| 1 | 0 | 2 | 0.000* | 2 | 3 | <001* |
| 2 | 2 | 4 | 0 | 2 | ||
| 3 | 3 | 5 | 0 | 3 | ||
| 4 | 0 | 4 | 2 | 4 | ||
| 5 | 0 | 2 | 3 | 5 | ||
| 6 | 0 | 3 | 1 | 4 | ||
| 7 | 2 | 4 | 0 | 3 | ||
| 8 | 0 | 4 | 3 | 5 | ||
| 9 | 2 | 4 | 0 | 3 | ||
| 10 | 0 | 3 | 2 | 5 | ||
| Mean | 0.9 | 3.5 | 1.3 | 3.7 | ||
*Paired t-test - the mean difference is significant at 0.05 level. TMJ=Temporomandibular joint
There was no appreciable change in the visual analog pain scales post release of ankylosis, after TMJ reconstruction, and in the 4-year follow-up period on joint movements.
Subjective evaluation of improvement in the diet efficiency was assessed as rated by the patient. The dietary efficiency improved from a scale of 10 (liquids) to a scale of 0 (no restriction to diet) in eight patients and 1 in two patients. The dietary score improved significantly after alloplastic reconstruction (P = 0.000) [Table 4].
Table 4.
Dietary score
| Preoperative | Postoperative (after alloplastic TMJ reconstruction) | P |
|---|---|---|
| 10 | 0 | <0.001* |
| 9 | 0 | |
| 10 | 1 | |
| 8 | 0 | |
| 7 | 0 | |
| 10 | 1 | |
| 9 | 0 | |
| 8 | 0 | |
| 9 | 0 | |
| 10 | 0 |
Diet efficiency as rated by patient, 0 equals the ability to chew any consistency of food without difficulty, 10 equals liquids only. *Paired t-test - the mean difference is significant at 0.05 level. TMJ=Temporomandibular joint
The mean intraoperative time for the procedure for the reconstruction of the TMJ using alloplastic joint was 133.20 ± 8.18 min. No evidence of facial nerve paralysis or foreign body reactions was noted in the patients during the follow-up period.
Radiographic assessment revealed good positioning and adaptation of the fossa component and the condylar ramal component both postoperatively [Table 5] and after a 4-year follow-up period [Figure 7a and b]. There was no evidence of screw loosening or prosthesis breakage during the follow-up period indicating a good stability of the device.
Table 5.
Radiographic assessment of temporomandibular joint prosthesis
| Adaptation of prosthesis | |
|---|---|
| Glenoid fossa component | Ramal component |
| Good | Good |
| Good | Good |
| Good | Good |
| Good | Good |
| Good | Good |
| Good | Good |
| Good | Good |
| Good | Good |
| Good | Good |
| Good | Good |
Figure 7.
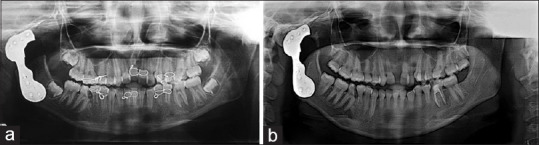
(a) Immediate postoperative orthopantomogram showing temporomandibular joint prosthesis. (b) Postoperative orthopantomogram after 5-year follow-up showing good adaptation of temporomandibular joint prosthesis
DISCUSSION
The multiple disadvantages of an autogenous graft have led the surgeons to consider alloplastic replacement of TMJ as a better and viable option. A review of literature reveals that an alloplastic TMJ replacement could produce a favorable and successful outcome, especially in patients with reankylosis.
Mercuri et al.[16] in their study reported decrease in pain by 49%, improvement in jaw function by 43%, improvement in dietary intake by 50%, and increase in maximum jaw opening by 31%. Garrett et al.[17] reported an average decrease in pain of 65%, a 71% increase in diet, and a 66% increase in Maximum Incisal Opening (MIO) when using a metal-on-metal TMJ reconstruction system. Fernandes[18] reported in his study that 75% of patients had improvement in mastication. In the present study, subjective evaluation of pain and efficiency of diet was done. All the patients had ankylosed joints and restriction of mouth opening as their primary complaint with no history of pain in the joints. Hence, postoperative improvements in pain showed no appreciable changes. There was 100% improvement in efficiency of the diet, which could be attributed to the improved jaw function following the reconstruction of the TMJ.
Mercuri and Giobbie-Hurder[19] showed a 30% improvement in the mandibular range of motion and Wolford et al.[20] using the Techmedica patient-fitted TMJ-TJR device published a statistically significant improvement in incisal opening. In a study on simultaneous treatment of TMJ ankylosis with severe mandibular deficiency by standard TMJ prosthesis by Hu et al.,[21] the mean postoperative mouth opening achieved was 31.5 mm. Fernandes[18] reported a postoperative mouth opening of 31.5 ± 3.41 mm. The postoperative mouth opening after the reconstruction of TMJ using alloplastic joint prosthesis was 34.90 ± 2.69 mm, and after a 4-year follow-up, the mean postoperative mouth opening was 34.60 ± 2.50 mm in the current study which is very similar to the above-mentioned studies.
Hu et al.[21] suggested that their previous studies on autogenous bone grafts, including rib grafts and coronoid process grafts for the treatment of ankylosis, showed that there were no significant differences of mouth opening among rib grafts, coronoid process grafts, and alloplastic TMJ prostheses. However, both rib grafts and coronoid process grafts reported bone resorption and recurrence of TMJ ankylosis. In contrast to this, in our previous study using sternoclavicular graft, the mean postoperative mouth opening after a follow-up period of 4 years was 26.7 ± 7.57 mm and there were two cases of reankylosis.[22]
There was no evidence of reankylosis or significant decrease in mouth opening in any of the cases in the current study. This is one of the greatest advantages of alloplastic TMJ reconstruction. The reasons for the low recurrence of ankylosis after alloplastic TMJ prostheses are that the fossa prosthesis covers the exposure of the bone and prevents downward bone formation by acting as a barrier; second, the stability of the osteotomy gap is maintained by the mandibular prosthesis.[23]
The results of the lateral excursive movements in this study showed sufficient improvements in the lateral movements to the unaffected side following the reconstruction of the TMJ after gap arthroplasty. In a study of long-term follow-up of the CAD/CAM patient fitted with total TMJ reconstruction system by Mercuri and Giobbie-Hurder,19 the multiple regression analysis confirmed what is seen clinically with unilateral alloplastic reconstructions. The unilaterally reconstructed patient will exhibit greater lateral excursion to the reconstructed side than to the nonreconstructed side. This is attributable not only to the loss of lateral pterygoid function on the implanted side but also to the formation of periarticular scar tissue. This was evident in our study also. Fernandes[18] published a postoperative lateralization movement of (3.1 ± 1.71 mm). The mean right and left lateral movements of the TMJ after reconstruction were 3.5 ± 0.97 mm and 3.70 ± 1.06 mm in the current study. The improved mandibular function is due to the fact that the center of rotation of the condylar prosthesis is placed much more inferior than that of the natural condyle.
Another advantage of the TMJ-TJR prosthesis is that they can bear more stress than the autogenous bone grafts without resorption. The longevity of prosthesis for any joint is dependent on materials, design, stability, and functional loading. For the average adult, the biting forces generated at the molars are approximately 60 pounds and that for the incisors are 35 pounds.[24] There were no issues of wear of the prosthesis even after a mean follow-up period of 4 years. The lower functional loads by the patients as well as the stability of the device could explain the longevity of these TMJ prostheses.
According to Lindqvist et al.,[25] the alloplastic replacement of the condyle alone had the disadvantage of causing resorption of the fossa. In 1965, Christensen et al.[26] added a TMJ condylar prosthesis to the TMJ fossa eminence prosthesis, to form a TMJ total joint replacement. Since then, a number of modifications have been made in the TMJ replacement devices. The custom TMJ-TJR devices published in the literature[27] are manufactured using commercially pure titanium as the fossa backing for ultrahigh molecular weight polyethylene articulating surface; wrought alloyed titanium for the ramus component and wrought Co–Cr–Mb for the articulating condylar head. However, taking the cost into consideration, in this study, a custom-made TMJ-TJR prosthesis having both fossa and condylar component made of Co–Cr–Mb alloy was used.
The absence of a posterior stop in the stock and metal on metal custom TMJ-TJR devices leads to posterior dislocation of the condylar head. If the condylar head is not perfectly aligned in the center of the fossa component in both the mediolateral and anteroposterior position, the condylar head may get displaced and impinge on the external auditory canal resulting in pain, malocclusion, or even infection in case of pressure-related perforation of the cartilaginous portion of the auditory canal.[21] This is of particular concern where the condyle needs to be placed in the centric position in case of orthognathic mandibular surgeries, especially in combination with counterclockwise mandibular rotation procedures. Hence, in the custom-made TMJ-TJR prosthesis used in the present study, even though it is a metal on metal, a posterior stop was placed.
Mercuri et al.[28] reviewed the outcomes of total alloplastic replacement with periarticular autogenous fat graft harvested from the abdomen and grafted around the articulating portion of their prosthesis, and Hu et al.[21] also placed free fat grafts harvested from submandibular incision around the TMJ prostheses as they felt that this prevents blood clot formation and osteogenesis, thereby preventing ectopic bone formation or reankylosis. However, in the current study, even though no autogenous tissue was interposed, there were no cases of heterotrophic bone formation or reankylosis.
Pearce et al.[29] and Malis et al.[30] reported a single-stage technique for the replacement of ankylosed joint using a custom-made prosthesis. The concern for a single-stage surgery is the exact replication of the presurgical plan during surgery. Any excessive trimming of the bone may jeopardize the fit of the components resulting in instability of the prosthesis. In the current study, a two-stage procedure was planned for all the patients. The advantages of the two-stage surgical procedure were that the glenoid fossa and ramal area were adequately prepared during the stage of ankylotic mass removal. This enabled easier fabrication as well as accurate fit of the prosthesis during the second stage eliminating any need for surgical template. There was no major postoperative complication in the study, except for scar in the submandibular region which was acceptable.
There is a controversy regarding alloplastic reconstruction of TMJ in growing patients; however, patients with a history of recent ankylosis with no evident facial asymmetry and a history of reankylosis were included even when the patient was in the growth period and one of the major advantages of the custom-made prosthesis was by using the stereolithographic model, the height of the ramus could be established, and there were no incidence of reankylosis which seemed to be the major issue with autogenous reconstruction in case of growing patients. Hence, TMJ-TJR custom-made prosthesis could be a viable alternative even in growing patients with no obvious facial asymmetry and in case of reankylosis.
The limitations of the study are a small sample size and a short-term follow-up period. The future research should be directed toward addressing the main drawbacks of the alloplastic TMJ reconstruction such as reducing the cost of TMJ-TJR devices and substantial evidence for usage in growing patients, and since TMJ-TJR is a biomechanical rather than a biological solution, there may arise the need for revision surgery to remove scar tissue from the articulating components of the implant or even replacement of the implant over time due to material wear and/or failure. In this regard, studies are needed on the use of proper biomaterials and design configurations to decrease material wear and increase device longevity under functional loading.
CONCLUSION
The reconstruction of TMJ with custom-made TMJ prosthesis has been proved to be successful in this study, as it has been mentioned in various literature, by many authors. The custom-made TMJ-TJR devices provide stable, improved long-term results, thereby increasing the quality of life of the patient. The postoperative outcomes such as mouth opening, lateral movements, masticatory efficiency, and prevention of lateral deviation and restoration of functional occlusion were satisfactory for all the patients, during the entire follow-up period. The custom-made alloplastic TMJ-TJR prosthesis proves to be the optimal surgical procedure to reconstruct the TMJ in comparison to the autogenous grafts (to avoid complications) in severe degenerated and ankylosed joints. However, long-term clinical and radiological studies on a larger sample size are imperative to establish the versatility of this procedure.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Movahed R, Mercuri LG. Management of temporomandibular joint ankylosis. Oral Maxillofac Surg Clin North Am. 2015;27:27–35. doi: 10.1016/j.coms.2014.09.003. [DOI] [PubMed] [Google Scholar]
- 2.Dimitroulis G. A critical review of interpositional grafts following temporomandibular joint discectomy with an overview of the dermis-fat graft. Int J Oral Maxillofac Surg. 2011;40:561–8. doi: 10.1016/j.ijom.2010.11.020. [DOI] [PubMed] [Google Scholar]
- 3.Khalid F, Kamisetty A, Robertson B. Costochondral grafting in TMJ Ankylosis-Benefits and limitations. Br J Oral Maxillofac Surg. 2019;57:e70. [Google Scholar]
- 4.Dayashankara Rao JK, Dar N, Sharma A, Sheorain AK, Malhotra V, Arya V. Evaluation of the sternoclavicular graft for the reconstruction of temporomandibular joint after gap arthroplasty. Ann Maxillofac Surg. 2017;7:194–201. doi: 10.4103/ams.ams_120_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Al-Hudaid A, Aldialami A, Helmi J, Al-Wesabi M, Madfa A. Management of temporomandibular joint ankylosis in Yemeni children by metatarsal bone grafts. J Oral Res. 2017;6:216–21. [Google Scholar]
- 6.Liu X, Shen P, Zhang S, Yang C, Wang Y. Effectiveness of different surgical modalities in the management of temporomandibular joint ankylosis: A meta-analysis. Int J Clin Exp Med. 2015;8:19831–9. [PMC free article] [PubMed] [Google Scholar]
- 7.Resnick CM, Genuth J, Calabrese CE, Taghinia A, Labow BI, Padwa BL. Temporomandibular joint ankylosis after ramus construction with free fibula flaps in children with hemifacial microsomia. J Oral Maxillofac Surg. 2018;76:2001e1–15. doi: 10.1016/j.joms.2018.05.004. [DOI] [PubMed] [Google Scholar]
- 8.Yang YT, Li YF, Jiang N, Bi RY, Zhu SS. Grafts of autogenous coronoid process to reconstruct the mandibular condyle in children with unilateral ankylosis of the temporomandibular joint: Long-term effects on mandibular growth. Br J Oral Maxillofac Surg. 2018;56:107–12. doi: 10.1016/j.bjoms.2017.12.001. [DOI] [PubMed] [Google Scholar]
- 9.Marx RE. Bone and bone graft healing. Oral Maxillofac Surg Clin North Am. 2007;19:455–66. doi: 10.1016/j.coms.2007.07.008. v. [DOI] [PubMed] [Google Scholar]
- 10.Johnson NR, Roberts MJ, Doi SA, Batstone MD. Total temporomandibular joint replacement prostheses: A systematic review and bias-adjusted meta-analysis. Int J Oral Maxillofac Surg. 2017;46:86–92. doi: 10.1016/j.ijom.2016.08.022. [DOI] [PubMed] [Google Scholar]
- 11.Mercuri LG. Temporomandibular joint replacement devices-Dark past to challenging future. Stomatological Dis Sci. 2019;3:3. [Google Scholar]
- 12.Elledge R, Mercuri LG, Attard A, Green J, Speculand B. Review of emerging temporomandibular joint total joint replacement systems. Br J Oral Maxillofac Surg. 2019;57:722–8. doi: 10.1016/j.bjoms.2019.08.009. [DOI] [PubMed] [Google Scholar]
- 13.Zheng J, Chen X, Jiang W, Zhang S, Chen M, Yang C. An innovative total temporomandibular joint prosthesis with customized design and 3D printing additive fabrication: A prospective clinical study. J Transl Med. 2019;17:4. doi: 10.1186/s12967-018-1759-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Al-Kayat A, Bramley P. A modified pre-auricular approach to the temporomandibular joint and malar arch. Br J Oral Surg. 1979;17:91–103. doi: 10.1016/s0007-117x(79)80036-0. [DOI] [PubMed] [Google Scholar]
- 15.Kaban LB, Bouchard C, Troulis MJ. A protocol for management of temporomandibular joint ankylosis in children. J Oral Maxillofac Surg. 2009;67:1966–78. doi: 10.1016/j.joms.2009.03.071. [DOI] [PubMed] [Google Scholar]
- 16.Mercuri LG, Wolford LM, Sanders B, White RD, Hurder A, Henderson W. Custom CAD/CAM total temporomandibular joint reconstruction system: Preliminary multicenter report. J Oral Maxillofac Surg. 1995;53:106–15. doi: 10.1016/0278-2391(95)90381-x. [DOI] [PubMed] [Google Scholar]
- 17.Garrett WR, Abbey PA, Christensen R. Temporomandibular joint reconstruction with a custom total temporomandibular joint prosthesis: Use in the multiply operated patient. Surg Technol Int. 1997;6:347–54. [PubMed] [Google Scholar]
- 18.Fernandes TC. Assessment of clinical parameters and patient satisfaction submitted to rehabilitation with total joint prostheses of temporomandibular joint. Physiother Res Rep. 2017;1:1–8. [Google Scholar]
- 19.Mercuri LG, Giobbie-Hurder A. Long-term outcomes after total alloplastic temporomandibular joint reconstruction following exposure to failed materials. J Oral Maxillofac Surg. 2004;62:1088–96. doi: 10.1016/j.joms.2003.10.012. [DOI] [PubMed] [Google Scholar]
- 20.Wolford LM, Mercuri LG, Schneiderman ED, Movahed R, Allen W. Twenty-year follow-up study on a patient-fitted temporomandibular joint prosthesis: The Techmedica/TMJ concepts device. J Oral Maxillofac Surg. 2015;73:952–60. doi: 10.1016/j.joms.2014.10.032. [DOI] [PubMed] [Google Scholar]
- 21.Hu Y, Zhang L, He D, Yang C, Chen M, Zhang S, et al. Simultaneous treatment of temporomandibular joint ankylosis with severe mandibular deficiency by standard TMJ prosthesis. Sci Rep. 2017;7:45271. doi: 10.1038/srep45271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Thirunavukkarasu R, Balasubramaniam S, Balasubramanian S, Gopalakrishnan SK, Panchanathan S. Sternoclavicular joint graft in temporomandibular joint reconstruction for ankylosis. Ann Maxillofac Surg. 2018;8:292–8. doi: 10.4103/ams.ams_209_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mercuri LG. The role of custom-made prosthesis for temporomandibular joint replacement. Rev Esp Cir Oral Maxilofac. 2013:1–10. [Google Scholar]
- 24.Throckmorton GS. Temporomandibular joint biomechanics. Oral Maxillofac Surg Clin North Am. 2007;12:27. [Google Scholar]
- 25.Lindqvist C, Söderholm AL, Hallikainen D, Sjövall L. Erosion and heterotopic bone formation after alloplastic temporomandibular joint reconstruction. J Oral Maxillofac Surg. 1992;50:942–9. doi: 10.1016/0278-2391(92)90051-z. [DOI] [PubMed] [Google Scholar]
- 26.Christensen RW, Alexander R, Curry JT, Christensen MS, Dollar JV. Hemi and total TMJ reconstruction using the Christensen prostheses: A retrospective and prospective evaluation. Surg Technol Int. 2004;12:292–303. [PubMed] [Google Scholar]
- 27.Gerbino G, Zavattero E, Bosco G, Berrone S, Ramieri G. Temporomandibular joint reconstruction with stock and custom-made devices: Indications and results of a 14-year experience. J Craniomaxillofac Surg. 2017;45:1710–5. doi: 10.1016/j.jcms.2017.07.011. [DOI] [PubMed] [Google Scholar]
- 28.Mercuri LG, Alcheikh Ali F, Woolson R. Outcomes of total alloplastic replacement with peri-articular autogenous fat grafting for management of re-ankylosis of the temporomandibular joint. J Oral Maxillofac Surg. 2008;66:1794–803. doi: 10.1016/j.joms.2008.04.004. [DOI] [PubMed] [Google Scholar]
- 29.Pearce CS, Cooper C, Speculand B. One stage management of ankylosis of the temporomandibular joint with a custom-made total joint replacement system. Br J Oral Maxillofac Surg. 2009;47:530–4. doi: 10.1016/j.bjoms.2009.04.024. [DOI] [PubMed] [Google Scholar]
- 30.Malis DD, Xia JJ, Gateno J, Donovan DT, Teichgraeber JF. New protocol for 1-stage treatment of temporomandibular joint ankylosis using surgical navigation. J Oral Maxillofac Surg. 2007;65:1843–8. doi: 10.1016/j.joms.2005.11.080. [DOI] [PubMed] [Google Scholar]


