Abstract
Objectives:
To determine what information is most important to registered nurses’ (RNs) decisions to call clinicians about suspected UTIs in nursing home residents.
Design:
Web-based discrete-choice experiment with 19 clinical scenarios.
Setting and Participants:
Online survey with a convenience sample of RNs (N=881) recruited from a healthcare research panel.
Methods:
Clinical scenarios used information from 10 categories of resident characteristics: UTI risk, resident type, functional status, mental status, lower urinary tract status, body temperature, physical examination, urinalysis, antibiotic request, and goals of care. Participants were randomized into two deliberation conditions (self-paced, n=437 and forced deliberation, n=444). The degree to which evidence- and non-evidence-based information was important to decision-making was estimated using unconditional multinomial logistic regression.
Results:
For all nurses (22.8%) and the self-paced group (24.1%), lower urinary tract status had the highest importance scores for the decision to call a clinician about a suspected UTI. For the forced-deliberation group, body temperature was most important (23.7%), and lower urinary tract status was less important (21%, p=.001). The information associated with the highest odd of a RN calling about a suspected UTI were painful or difficult urination (OR: 4.85, 95% CI: 4.16, 5.65), obvious blood in urine (OR: 4.66, 95% CI: 3.99, 5.44), and temperature at 101.5° (OR: 3.80, 95% CI: 3.28, 4.42). For the self-paced group, painful or difficult urination (OR: 5.65, 95% CI: 4.53, 7.04) had the highest odds, while obvious blood in urine (OR: 4.39, 95% CI: 3.53, 5.47) had highest odds for the forced-deliberation group.
Conclusions and Implications:
This study highlighted the importance of specific resident characteristics in nurse decision-making about suspected UTIs. Future antimicrobial stewardship efforts should aim to not only improve the previously studied overprescribing practices of clinicians, but to improve nurses’ assessment of signs and symptoms of potential infections and how they weigh resident information.
Brief Summary:
This study examined registered nurses’(RNs) (N=881) decisions to call clinicians about suspected UTIs in nursing home residents and found lower urinary tract status was most important. Understanding why RNs’ decide to call about suspected UTIs may help avoid unnecessary antimicrobial use.
Keywords: nursing care, discrete choice experiment, urinary tract infection, nursing home, decision making
Introduction
In the United States, antimicrobials are the most commonly prescribed drugs in nursing homes (NHs), with an estimated 50–79% of residents receiving these drugs annually1–3 However, antimicrobial overuse in NHs has become a public health crisis because it has contributed to the rise of antimicrobial resistance and the transfer of resistant organisms to other healthcare settings. As a result, the World Health Organization, as well as the Center for Medicare and Medicaid Services, has identified the NH setting as a priority for better antimicrobial stewardship.4,5
However, the organization of care in the NH setting presents challenges to antimicrobial stewardship.5 As the primary workforce in NHs, certified nursing assistants (CNA) are typically the first to recognize symptoms associated with potential infections and then to report them to the licensed practical nurse (LPN) or registered nurse (RN).6 In turn, the nurse conducts an assessment and, if needed, contacts the resident’s clinician to report the potential infection and potentially to initiate antimicrobials.7 RNs are essential brokers of antimicrobials in NH care, as they are primarily responsible for the care of NH residents and often interact with off-site health care clinicians. Nurses are responsible for noting change in resident status, assessing the resident, identifying signs and symptoms of potential infections, collecting and testing urine samples, and deciding when to communicate the findings to the resident’s clinician.8 During this communication, they also may express the need for an antimicrobial.7 As a result, clinicians, who are typically off-site and make infection management decisions based on nurse assessment,9 may overprescribe antimicrobials.10,11 Urinary tract infections (UTIs) are the most common infection in NHs, and clinicians who prescribe antimicrobials depend on nursing staff to provide critical diagnostic information to inform their prescribing decision.10,11 Therefore, one way to potentially reduce unnecessary antimicrobial use is to target the nurse’s decision-making in this process.
Research suggests that several factors influence RN decision-making. A qualitative chart review study of infections in NH residents suggested that a patient’s characteristics (e.g., their age, presenting symptoms, temperature, and UTI risk) were important to nurses’ subsequent actions.6 Other research on nurse decision-making in acute care settings indicates that the nurse’s clinical experience,12 the nurse’s work role,13 and whether the nurse takes time to deliberate14–18 can influence decision-making. However, this study is limited in scope and applicability to RN decision-making about suspected UTIs for NH residents. Current observational research examining antibiotic prescribing does not examine nurse decision-making in NHs and the decision to call a prescriber about a suspected UTI for NH residents.19–25 Instead, existing research is primarily interventional, focusing on using educational strategies to fill knowledge gaps and is not aimed at changing nurse clinical decision-making and behaviors.5,26–28 Understanding what factors drive decision-making, including the clinical information most sought by nurses and whether this information is supported by the evidence, are important to the design of effective interventions. Thus, our discrete choice experiment (DCE) examined NH nurses’ choice of behavior—to call a clinician or not--using a controlled method to parse out the impact of one specific resident attribute/factor against other attributes.21,22 It examined what RNs consider to be the most important resident characteristics and clinical information when they make decisions about whether to notify a clinician about suspected UTIs in NH residents.
Methods
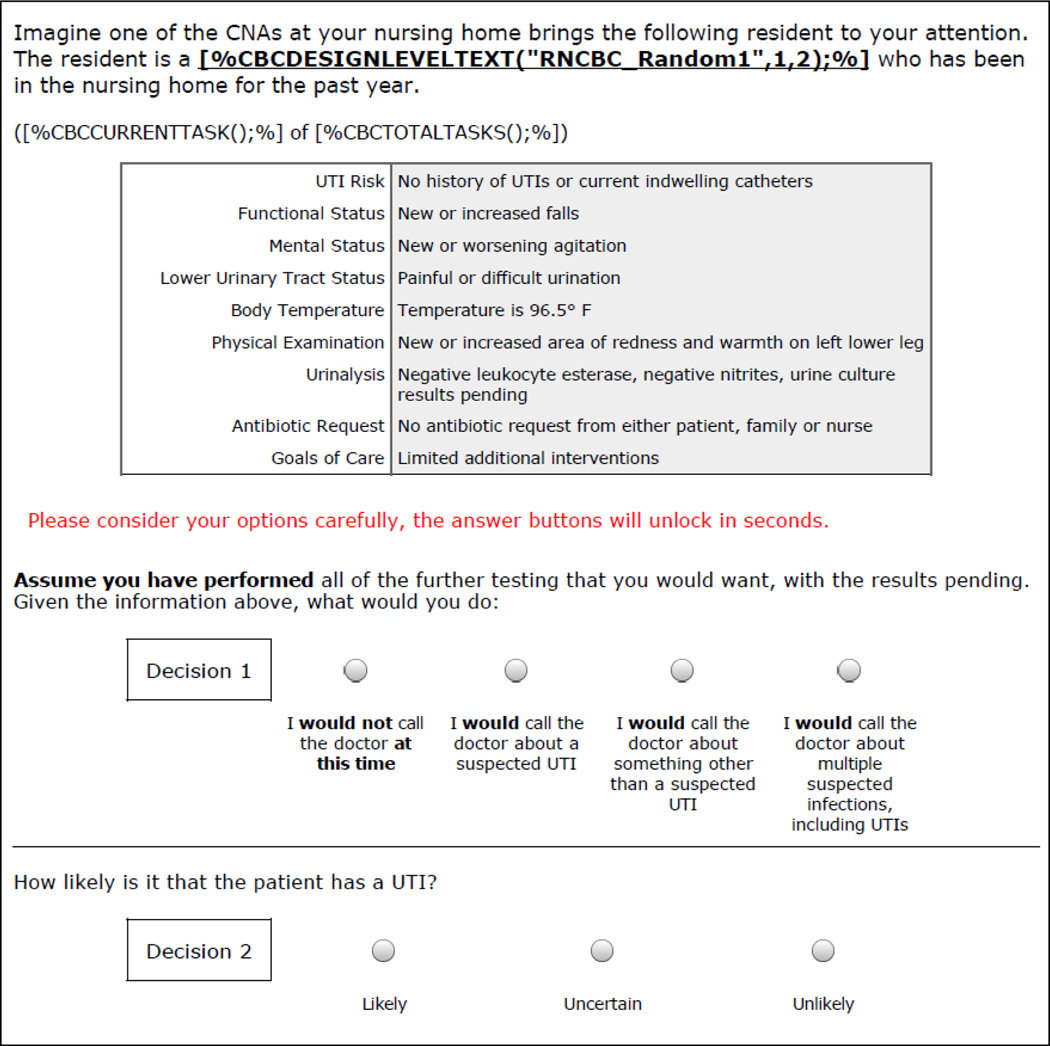
Discrete choice experimental (DCE) design is a method of quantifying preferences while varying the level of given characteristics.29,30 As part of a larger study examining decision-making about antibiotic prescribing for UTIs,31 we conducted an experiment to examine the clinical information most important to RN decision-making for residents with suspected UTIs by varying levels of nursing home (NH) resident characteristics (N=881). We focused on RN decision-making in this study (as opposed to CNAs and LPNs) because they are responsible for resident assessments and lead decision-making about resident care. Using an online survey, we presented RN participants with 19 discrete choice scenarios that varied by 10 resident categories: lower urinary tract status, body temperature, urinalysis, UTI risk, physical examination, mental status, antimicrobial request, functional status, goals of care, and resident type (Table 1). For each scenario, RNs decided if they would or would not call the doctor. If they decided to call, we asked if they would be calling about a suspected UTI, multiple infections, or something else (Figure 1). We derived importance scores of the characteristics and odds ratios for clinical information within each characteristic. All study procedures were approved by the institutional review board at the University of North Carolina at Chapel Hill (IRB no. 16-0207).
Table 1.
Categories of Information Used in UTI Decision-Making Survey
| Category | Information | Evidence-Based Criteria? |
|---|---|---|
| Lower Urinary Tract Signs or Symptoms | • No lower urinary tract signs or symptoms | |
| • Painful or difficult urination | Yes3,32,35,37 | |
| • Obvious blood in urine | Yes32,34 | |
| • Change in urine clarity or odor | No34 | |
| • New or worsening frequency | Yes34–37 | |
| Body Temperature | • Temperature is 97.5°F | |
| • Temperature is 101.5°F | Yes3,32,35–37 | |
| • Temperature is 99.5°F | Yes3,32,44 | |
| • Temperature is 96.5°F | No | |
| Urinalysis | • Negative leukocyte esterase, negative nitrates, urine results pending | Rule out |
| • Positive leukocyte esterase, positive nitrates, urine results pending | Yes32 | |
| • Positive leukocyte esterase, negative nitrates, urine results pending | No | |
| • Unavailable/Not performed | No | |
| UTI Risk | • No history of UTIs or current indwelling catheters | |
| • Current indwelling catheter and history of three UTIs over the past year | Equivocal52 | |
| • History of three UTIs over past year but no current indwelling catheter | No | |
| • Current indwelling catheter but no history of prior UTIs over past year | Equivocal52 | |
| Physical Examination | • Normal physical exam | |
| • New suprapubic tenderness or costovertebral angle tenderness | Yes3,34–37 | |
| • New or increased area of redness and warmth on left lower leg | No53 | |
| • New or increased cough and work of breathing | No53 | |
| Mental Status | • Usual state of health | |
| • New or worsening confusion | Yes35–37 | |
| • New or worsening agitation | Yes35–37 | |
| • Sleeping more than usual | No3 | |
| Antimicrobial Request | • No antimicrobial request from either patient, family, or nurse | |
| • Antimicrobial request from family | No23,54–58 | |
| • Antimicrobial request from resident | No23,54–58 | |
| Functional Status | • Usual state of health | |
| • New or increase falls | No3 | |
| • New or increased resistance to care | No | |
| • New or worsening difficulties with ambulation or transfers | No3 | |
| • Reduced intake of food and liquids | No3 | |
| Goals of Care | • Comfort care measures | |
| • Full scope of treatment | No | |
| • Limited additional interventions | No | |
| Patient Type | • 84 year-old cognitively-intact man | |
| • 84 year-old cognitively-intact woman | Equivocal59 | |
| • 84 year-old man with dementia | Equivocal24,60,61 | |
| • 84 year-old woman with dementia | Equivocal24,59–61 | |
Note. Evidence-based information is bolded and citations are provided. No = Non-evidence-based criteria, equivocal response means evidence is mixed. The reference group for each category is italicized. The following categories of information were considered as evidence: level A (controlled trials), level B (comparative studies) and level C (expert opinion); both nursing home specific studies and studies about older persons in general were considered relevant.
Figure 1. Layout of the Discrete Choice Experiment Questions.
Sample Recruitment
All participants were recruited from an online panel of Medefield®, a global market research firm. The panel is an actively managed health care community of over 100,000 screened and verified nursing and medical professionals. Eligibility criteria for the nurses in this study included (a) having a current license as an RN, (b) being English-language proficient, and (c) currently practicing in an NH in the United States. RNs were recruited via an email invitation describing the specifications of the study (i.e., duration, focus, and honorarium) and including a web link to the survey. The link took participants to the survey eligibility questions (including a question that confirmed that the participant was currently a licensed RN, working in an NH, and not a nurse practitioner), and then to the full survey. Participants received a $35 or a $60 honorarium (for the self-paced versus forced-deliberation group, respectively) upon completion of the survey.
Survey Development
The study survey was developed in three steps. First, the research team developed a literature-based list of evidence- and non-evidence-based information used in decision-making for UTIs.31 Second, cognitive interviews with 30 nurses (recruited from Medefield®) were conducted between December 2017-February 2018, to gather feedback on the survey formatting, individual items, response options, and issues with the software. Third, a pilot test of the survey was administered in February 2018, to a sample of 80 RNs to determine the appropriateness of the survey. After minor modifications, the final version of the survey was administered online in March 2018, and then again from June-July 2018, to boost the sample due to detected outliers (see below).
Measures
DCE Scenarios.
We presented RN participants with 19 discrete choice scenarios that varied by 10 resident categories (e.g., lower urinary tract status, body temperature, urinalysis).29,30 and type of information (e.g. painful urination or blood in urine). The information within each category was drawn from the literature,3,32–37 and paralleled the information used in the DCE of antibiotic prescribing for UTIs.31 RNs were asked what they would do given the information in the scenario and assuming no further testing was needed. The four response options included, “I would not call the doctor at this time,” “I would call the doctor about a suspected UTI,” “I would call the doctor about something other than a suspected UTI,” and “I would call the doctor about multiple suspected infections, including UTIs.” The information varied systematically over the scenarios and with the respondents, allowing us to calculate how their decisions (whether or not to call) changed when we varied the information (resident characteristics).30
Time to Deliberate.
All respondents were randomized to a time condition, either self-paced (n = 437, 49.6%) or forced deliberation (n = 444, 50.4%).12,16,18,38,39 In the self-paced condition, participants could indicate their answer at any time, while in the forced-deliberation condition, participants were forced to consider each scenario for at least 30 seconds before selecting an answer. The goal of forced deliberation was to encourage slow decision-making (and discourage fast, intuitive decision-making).
Respondent Characteristics.
Respondent demographic data included sex, age, race, and ethnicity. Data regarding their work and workplace included 11 items for NH characteristics (e.g., use of electronic health records), years of experience, work role (unit nurse, nursing supervisor, infection control nurse), and degree type (Diploma/ADN, BSN, and MSN). As an attention check for the survey, respondents completed a brief measure of personality traits using the Ten-Item Personality Inventory(TIPI),40 a validated and widely used short-form version of the Big Five Personality Inventory. The 10-item TIPI has been shown to retain 70% of the variance and 85% of the re-test reliability of the larger 44-item Inventory.41 In the Inventory, items are coupled into five pairs assessing each of the five factors of personality including extraversion, agreeableness, conscientiousness, emotional stability, and openness to experiences.42 We expect that a participant, who answers one item in a certain direction, would answer its companion item in a similar way. If a participant was inattentive, they would have discrepant scores on the paired TIPI items due to reverse coding.
Data Analysis
Participants were excluded as outliers if they met any of these criteria: (a) total survey completion time > 720 minutes (which suggests they were inattentive to the survey), (b) total survey completion time < ((median minutes) − 2.5 × (median absolute deviation)), (c) UTI item response avoidance = 3 (i.e., complete avoidance), and (d), total TIPI item pair difference score > ((median score) + 5.0 × (median absolute deviation)). We then examined the degree to which evidence- and non-evidence-based information was important to RN decision-making by examining the importance scores for the decision, “I would call about a suspected UTI.”
We used unconditional multinomial logistic (MNL) regression suitable for the categorical responses of the DCE scenarios. The latent utilities of each category (e.g. lower urinary tract status) and each type of information (e.g., painful or difficult urination) were estimated at the sample level, serving as a numerical representation of the sum of the relative value of each type of information modeled to best match nurses’ responses. With all utilities scaled, the utilities within categories were compared across RNs to determine the relative importance of each type of information. To examine the role of deliberation, the sample-level utilities were compared between the groups (self-paced vs. forced deliberation) and used to compute importance scores to compare the scales of the utilities via a Swait-Louviere test for differences in preferences versus differences in scales appropriate for multinomial (categorical or, choice) responses.43 Statistical significance was defined throughout as p < .05 (two-sided). Estimates were transformed into odds ratio (OR) estimates with corresponding 95% confidence intervals (CIs). Additionally, we compared the distribution of importance scores by RN characteristics to determine if any differences in importance scores were related to respondent characteristics. Finally, we examined if calling the doctor about a suspected UTI was associated with assignment to the self-paced or the forced-deliberation group.
Results
Sample Characteristics
A total of 970 eligible participants completed the survey. A proportion (n = 89, 9.2%) were excluded as outliers, 23 of these observations (2.4%) were excluded because of a survey completion time greater than 720 minutes. The remaining 881 participants were 77% female, 75% White, 15% Black/African American, and 11% Hispanic/Latino (Table 2). The mean age was 40 years old, and the RNs were primarily unit nurses (56%) and nursing supervisors (22%). Half (50%) held a Bachelor of Science in Nursing degree or an associate degree (28%), and 18% held a Master of Science in Nursing (MSN). Bivariate comparisons on those designated as outliers (n = 89) found that excluded participants did not demonstrate differences in demographics or clinical characteristics from included participants.
Table 2.
Sample Characteristics (N = 881)
| Characteristics | N (%) or M (SD) |
|---|---|
| Demographic | |
| Female | 681 (77.3) |
| Age | 40.3 (12.0) |
| Race | |
| White | 661 (75.0) |
| Black/African American | 130 (14.8) |
| Asian | 61 (6.9) |
| Other | 29 (3.3) |
| Hispanic/Latino | 95 (10.8) |
| Clinical | |
| Uses electronic health records | 730 (82.9) |
| Has wireless network | 781 (88.7) |
| Position | |
| Unit nurse | 495 (56.2) |
| Nursing supervisor | 189 (21.5) |
| Director of Nursing | 45 (5.1) |
| Assistant Director of Nursing | 49 (5.6) |
| Minimum Data Set nurse | 57 (6.5) |
| Staff development coordinator | 9 (1.0) |
| Other | 37 (4.2) |
| Infection control nurse | 238 (27.0) |
| Infection control training in the last year | 626 (71.1) |
| Nursing experience | |
| 0–5 years | 181 (20.5) |
| 6–10 years | 266 (30.2) |
| 11–15 years | 155 (17.6) |
| 16–20 years | 92 (10.4) |
| > 20 years | 187 (21.2) |
| Years employed at current job | 6.1 (5.3) |
| Degree | |
| Diploma degree | 31 (3.5) |
| Associate’s Degree (ADN) | 246 (28.0) |
| Bachelor of Science in Nursing (BSN) | 443 (50.4) |
| Master of Science in Nursing (MSN) | 154 (17.5) |
| Other | 5 (0.6) |
Resident Characteristic Categories and Forced Time to Deliberate
In Table 3, we examined the importance of resident characteristics when RNs choose to make the decision, “I would call about a suspected UTI,” and how the importance of these characteristics differed by deliberation condition and the clinical experience of the RN. When deciding to call a prescriber about a suspected UTI, 22.8% identified lower urinary tract status as the most important characteristic, followed by body temperature (22.2%), urinalysis (18%), UTI risk (9.7%), and physical examination (7.8%). We found a significant difference between the self-paced and forced-deliberation groups on the importance of resident characteristics (p=.001). The self-paced group followed the same pattern as the overall sample (lower urinary tract status 24.1%, body temperature 19.7%, urinalysis 18.4%, UTI risk 10%, and physical examination 17.2%), while for the forced-deliberation group, body temperature (23.7%) and lower urinary tract status 21% were most important. We also found significant differences for infection control nurses and nurses with infection training (i.e., who attended an infection control course in the past year) when compared to nurses without this role or training (p<.001). For infection control nurses and nurses with infection control training lower urinary tract status was most important (28.4% and 22.8% respectively), while body temperature was most important for nurses without this role or training (22–23%).
Table 3.
Importance Scores for Calling a Provider About a Suspected UTI, Overall, by Time Condition, and RN Experience, Work Role and Clinical Degree (N = 881)
| Category | |||||||
|---|---|---|---|---|---|---|---|
| Characteristic | Lower Urinary Tract Status | Body Temperature | Urinalysis | UTI Risk | Physical Examination | All Others | p |
| Total (All Nurses) | 22.8% | 22.2% | 18.0% | 9.7% | 7.8% | 19.5% | |
| Time Condition | .001 | ||||||
| Self-Paced | 24.1% | 19.7% | 18.4% | 10.0% | 7.2% | 20.7% | |
| Forced Deliberation | 21.0% | 23.7% | 16.9% | 8.9% | 8.4% | 21.1% | |
| Experience | |||||||
| Years | .16 | ||||||
| 0–5 | 25.0% | 17.6% | 16.5% | 11.7% | 8.5% | 20.6% | |
| 6+ | 22.4% | 23.2% | 18.1% | 8.9% | 7.4% | 20.0% | |
| Work Role | |||||||
| Unit nurse | .036 | ||||||
| Yes | 22.0% | 21.4% | 17.2% | 11.0% | 8.1% | 20.4% | |
| No | 24.1% | 23.4% | 19.4% | 7.1% | 7.7% | 18.3% | |
| Nursing supervisor | .30 | ||||||
| Yes | 24.2% | 22.5% | 17.1% | 6.4% | 7.6% | 22.3% | |
| No | 22.3% | 22.0% | 18.2% | 10.3% | 7.9% | 19.3% | |
| Infection control nurse | <.001 | ||||||
| Yes | 28.4% | 19.8% | 15.9% | 10.9% | 8.0% | 17.0% | |
| No | 21.2% | 22.6% | 18.1% | 8.9% | 7.7% | 21.4% | |
| Infection control training | <.001 | ||||||
| Yes | 22.8% | 21.6% | 17.8% | 10.1% | 7.9% | 19.7% | |
| No | 21.4% | 22.5% | 17.1% | 7.9% | 7.2% | 24.0% | |
| Degree | |||||||
| Diploma/ADN | <.001 | ||||||
| Yes | 22.9% | 20.5% | 18.4% | 7.9% | 9.1% | 21.3% | |
| Other | 22.7% | 22.9% | 17.7% | 10.6% | 7.2% | 18.9% | |
| BSN degree | <.001 | ||||||
| Yes | 23.0% | 22.8% | 17.7% | 10.1% | 6.8% | 19.7% | |
| Other | 23.2% | 21.3% | 18.3% | 9.2% | 8/8% | 19.1% | |
| MSN degree | <.001 | ||||||
| Yes | 23.8% | 22.2% | 16.6% | 11.4% | 7.7% | 18.2% | |
| Other | 22.8% | 21.9% | 17.9% | 9.2% | 7.7% | 20.5% | |
Note. All others = Mental Status, Antimicrobial Request, Functional Status, Goals of Care, Patient Type. Importance scores for response #2 only (“I would call about a suspected UTI.”), p value tests distribution of the set of utilities of sub-models against the total model using likelihood ratio test; two-sided.
Information
Within each resident characteristic category (e.g., lower urinary tract status, body temperature), we wanted to examine what information was associated with the decision to call about a suspected UTI. For example, within lower urinary tract status we examined what signs and symptoms (painful or difficult urination, obvious blood in urine, change in clarity or odor, new or worsening frequency) RNs associated with the decision to call about a suspected UTI. We generated part-worth utility scores for the 30 types of clinical information as odds ratios (Table 4_. When deciding to call a provider about a suspected UTI, the importance of the information differed slightly by whether the RN was in the self-paced or deliberation group. For the self-paced group, the importance of information to nurses’ decision to call about a suspected UTI was as follows: “painful or difficult urination” (OR: 5.65, 95% CI: 4.53, 7.04), “obvious blood in urine” (OR: 4.90, 95% CI: 3.93, 6.11), “positive leukocyte esterase, positive nitrates” (OR: 3.75, 95% CI: 3.09, 4.55), and “temperature is 101.5°” (OR: 3.74, 95% CI: 3.05, 4.59). For nurses in the forced-deliberation group, the importance of information was as follows: “obvious blood in urine” (OR: 4.39, 95% CI: 3.53, 5.47), “painful or difficult urination” (OR: 4.21, 95% CI: 3.39, 5.21), “temperature is 101.5°” (OR: 3.95, 95% CI: 3.18, 4.90), and “positive leukocyte esterase, positive nitrates” (OR: 3.30, 95% CI: 2.73, 4.00).
Table 4.
Evidence Categories with Importance Scores and Utilities for All Nurses (N = 881) and by Time Condition Group
| “I would call about a suspected UTI” Importance Scores (%) and Utilities (OR, [95% CI]) |
|||
|---|---|---|---|
| Categories and Information | Total (All Nurses) | Self-Paced Group (n=437; 49.6%) | Forced-deliberation group N=444; 50.4%) |
| Lower Urinary Tract Status | 22.8% | 24.1% | 21.0% |
| No lower urinary tract signs/symptoms | 0.00 | 0.00 | 0.00 |
| Painful or difficult urination | 4.85 (4.16, 5.65) * | 5.65 (4.53, 7.04) * | 4.21 (3.39, 5.21) * |
| Obvious blood in urine | 4.66 (3.99, 5.44) * | 4.90 (3.93, 6.11) * | 4.39 (3.53, 5.47) * |
| Change in urine clarity or odor | 2.76 (2.39, 3.18) * | 3.09 (2.52, 3.78) * | 2.45 (2.00, 2.99) * |
| New or worsening frequency | 2.27 (1.93, 2.67) * | 2.12 (1.69, 2.66) * | 2.41 (1.91, 3.04) * |
| Body Temperature | 22.2% | 19.7% | 23.7% |
| Temperature is 97.5°F | 0.00 | 0.00 | 0.00 |
| Temperature is 101.5°F | 3.80 (3.28, 4.42) * | 3.74 (3.05, 4.59) * | 3.95 (3.18, 4.90) * |
| Temperature is 99.5°F | 1.71 (1.51, 1.95) * | 1.90 (1.59, 2.28) * | 1.57 (1.31, 1.87) * |
| Temperature is 96.5°F | 0.82 (0.72, 0.92) * | 0.90 (0.76, 1.07) | 0.74 (0.63, 0.89) * |
| Urinalysis | 18.0% | 18.4% | 16.9% |
| Negative leukocyte esterase, negative nitrates | 0.00 | 0.00 | 0.00 |
| Positive leukocyte esterase, positive nitrates | 3.48 (3.04, 3.99) * | 3.75 (3.09, 4.55) * | 3.30 (2.73, 4.00) * |
| Positive leukocyte esterase, negative nitrates | 2.16 (1.90, 2.47) * | 2.20 (1.83, 2.65) * | 2.14 (1.78, 2.58) * |
| Unavailable/Not performed | 1.48 (1.30, 1.68) * | 1.45 (1.21, 1.74) * | 1.52 (1.26, 1.82) * |
| UTI Risk | 9.7% | 10.0% | 8.9% |
| No history of UTIs or current indwelling catheters | 0.00 | 0.00 | 0.00 |
| Current indwelling catheter + history of three UTIs | 1.96 (1.68, 2.28) * | 2.06 (1.66, 2.55) * | 1.87 (1.51, 2.33) * |
| History of three UTIs over past year | 1.46 (1.28, 1.67) * | 1.54 (1.28, 1.85) * | 1.39 (1.15, 1.68) * |
| Current indwelling catheter | 1.20 (1.03, 1.39) * | 1.18 (0.96, 1.45) | 1.22 (0.99, 1.51) |
| Physical Examination | 7.8% | 7.2% | 8.4% |
| Normal physical exam | 0.00 | 0.00 | 0.00 |
| Suprapubic/costovertebral angle tenderness | 1.71 (1.52, 1.93) * | 1.67 (1.42, 1.98) * | 1.76 (1.49, 2.09) * |
| Redness and warmth on left lower leg | 1.15 (1.01, 1.31) * | 1.31 (1.08, 1.58) * | 1.02 (0.84, 1.23) |
| Cough and work of breathing | 1.09 (0.96, 1.25) | 1.26 (1.04, 1.51) * | 0.98 (0.81, 1.18) |
| Mental Status | 6.3% | 5.7% | 6.9% |
| Usual state of health | 0.00 | 0.00 | 0.00 |
| New/Worsening confusion | 1.54 (1.35, 1.76) * | 1.50 (1.25, 1.81) * | 1.59 (1.32, 1.92) * |
| New/Worsening agitation | 1.52 (1.33, 1.73) * | 1.43 (1.19, 1.72) * | 1.62 (1.35, 1.95) * |
| Sleeping more than usual | 1.20 (1.05, 1.36) * | 1.25 (1.04, 1.51) * | 1.15 (0.96, 1.38) |
| Antimicrobial Request | 5.2% | 4.6% | 6.2% |
| No antimicrobial request | 0.00 | 0.00 | 0.00 |
| Antimicrobial request from family | 1.44 (1.25, 1.65) * | 1.33 (1.10, 1.62) * | 1.55 (1.28, 1.89) * |
| Antimicrobial request from resident | 1.31 (1.13, 1.50) * | 1.39 (1.14, 1.70) * | 1.23 (1.00, 1.50) * |
| Functional Status | 4.7% | 4.6% | 4.3% |
| Usual state of health | 0.00 | 0.00 | 0.00 |
| New/Increased falls | 1.38 (1.20, 1.60) * | 1.39 (1.13, 1.70) * | 1.35 (1.10, 1.67) * |
| New/Increased resistance to care | 1.26 (1.09, 1.45) * | 1.22 (1.00, 1.50) | 1.28 (1.04, 1.57) * |
| New/Worsening difficulties with ambulation/transfers | 1.18 (1.02, 1.36) * | 1.20 (0.98, 1.48) | 1.14 (0.93, 1.40) |
| Reduced intake of food and liquids | 1.15 (0.99, 1.33) | 1.08 (0.88, 1.32) | 1.23 (1.00, 1.51) |
| Goals of Care | 2.2% | 3.5% | 1.1% |
| Comfort care measures | 0.00 | 0.00 | 0.00 |
| Full scope of treatment | 1.16 (1.04, 1.30) * | 1.29 (1.10, 1.51) * | 1.07 (0.91, 1.26) |
| Limited additional interventions | 1.14 (1.02, 1.27) * | 1.21 (1.03, 1.42) * | 1.08 (0.92, 1.27) |
| Resident Type | 1.1% | 2.3% | 2.6% |
| 84 year-old cognitively-intact man | 0.00 | 0.00 | 0.00 |
| 84 year-old cognitively-intact woman | 1.07 (0.93, 1.22) | 1.18 (0.98, 1.43) | 0.96 (0.79, 1.16) |
| 84 year-old man with dementia | 1.03 (0.85, 1.25) | 1.08 (0.82, 1.42) | 0.97 (0.73, 1.27) |
| 84 year-old woman with dementia | 0.99 (0.82, 1.19) | 1.17 (0.90, 1.52) | 0.83 (0.64, 1.08) |
Note. Evidence-based information is bolded. OR = Odds ratio, CI = Confidence interval.
p < .05; two-sided.
Discussion
This controlled experiment examined the importance of different types of NH resident information and characteristics of RNs’ decisions to contact a clinician about a suspected UTI. Overall, we found that lower urinary tract status and body temperature were the most important resident characteristics for nurses deciding to call a doctor about a suspected UTI. This finding aligns with the current UTI management literature that suggests that the onset of lower urinary tract symptoms and a change in body temperature are evidence-based reasons to suspect a UTI.35–37 Urinalysis was the third most important information for the nurses in our sample, however, urinalysis is not considered a sound tool for UTI diagnoses and has been linked to overprescribing antimicrobials for asymptomatic bacteruria.44 Thus, future efforts should emphasize the importance of symptoms and to decrease RNs’ reliance on non-evidence-based tests such as urinalysis.
When we examined if deliberation time related to the use of different information for decision-making, we found that RNs who were forced to deliberate prioritized different information than those who were self-paced. Previous research on forced deliberation and nurse decision-making suggests that time pressure leads to more conservative practice which can result in the use of inappropriate interventions,16 poorer patient ratings of care quality,15,45 more testing, and potential overtreatment.46 Previous research has found that when clinicians are forced to deliberate, they make more thoughtful decisions by weighing the pros and cons of a given decision.47 In the context of our findings, one could conclude that when forced to deliberate, RNs prioritize absolute information (information with a clear number), such as body temperature, when making the decision to call a clinician. Currently, we do not know if deliberation leads to better NH resident outcomes. However, given the lack of research on time for deliberation and NH nurse decision-making, we advocate for future research to explore how time pressure and deliberation speed may affect nurse decision-making in NHs.
This study has implications for nursing practice in NHs. For example, if a resident has cloudy or odorous urine without other indicators of infection,3,34 nurses can initiate a symptom management strategy such as increasing a resident’s fluid intake, which could ultimately improve resident quality of life and avoid unnecessary antibiotics.21,48 Similarly, providing good personal hygiene to alleviate perineal discomfort and treating constipation to relieve urination frequency, urgency, and burning are symptom management strategies nurses can initiate to potentially improve resident quality of life.21,48 If an RN were to consult with the resident’s clinician and implement these strategies, the symptom management may provide relief, and avoid antimicrobial use. Future research on increasing RN focus on communication with providers about UTI signs/symptoms alongside efforts to improve RNs’ urinary symptom management skills could relieve the suffering of NH residents and provide non-pharmacological alternatives to antimicrobial use.
Our study was limited by a convenience sample that was over representative of RNs with Bachelor’s in nursing (BSN) degrees. Recent estimates suggest that BSNs compose approximately 42% of the U.S. nursing workforce, and NHs have even less BSN prepared RNs, 49 which suggests that our sample was more educated than the typical RNs working in NH settings. Although this distribution limits the generalizability of our findings to the entire NH RN population, it should be noted that the top three information rankings (e.g., urinary tract status, body temperature, and urinalysis) did not differ by degree type (Diploma/ADN, BSN, MSN). Another limitation of this study is that it used hypothetical scenarios that did not reflect the actual experience of RN real-world decision-making. We understand that what RNs do in practice may differ from how they responded in the experiment, and that a strength of nursing practice in NHs is that the staff develop long-term relationships with the residents. This means that the reality of NH nursing practice may be based on other, more resident-specific information than what we provided. Finally, for the purposes of the experiment, we limited the resident information to a discrete list, and we acknowledge that nurses may weigh other information (e.g. a resident’s ability to communicate symptoms) when making decisions. However, for this exploratory experiment, we relied on the current evidence about UTI antibiotic prescribing to guide our study. Nonetheless, this study was one of the first large-scale experiments examining RN decision-making when a NH resident has a potential UTI and, therefore, has implications for future research and practice efforts aiming to change RN management of urinary symptoms and suspected infections.
Conclusions and Implications
The findings from this study have several implications for improving the care of NH residents. A better understanding of what impacts RNs’ decisions to call clinicians about suspected UTIs may help target future interventions that facilitate evidence-based nursing assessment and symptom management to avoid unnecessary antimicrobial use.50,51 Nurses have been identified as the “first responders” of antibiotic stewardship, meaning that nurses, including RNs, are the first to assess a resident’s change in status and consider whether to communicate this information to the clinician.51 Our study provides evidence that nurses weigh different information in each clinical situation, and that this information leads to calling or not calling the health care provider. Future antimicrobial stewardship efforts should aim to not only improve the prescribing practices of clinicians, but to improve nurses’ assessments of the signs and symptoms of potential infections and how they weigh resident information. Given the differences we found when RNs had infection control training and were put under a forced-deliberation condition, our work highlights the potential benefit of clinical support systems that improve RNs’ knowledge about infections such as UTIs and changes the process of decision-making.50 Designing interventions to help nurses take the time to deliberate over the information they receive and empower them to use the time to respond to the signs and symptoms of UTIs with appropriate symptom management strategies, could potentially relieve NH resident suffering. These efforts could impact the overprescribing of antimicrobials and enhance antimicrobial stewardship for NH residents with suspected UTIs.
Acknowledgments:
The sponsor had no role in the design, methods, subject recruitment, data collections, analysis and preparation of paper.
Funding Source: This work was supported by the Agency for Healthcare Research and Quality 1R01HS024519–01
Footnotes
Conflicts of Interest: The authors for this work have no conflicts of interest.
References
- 1.Nicolle LE, Bentley DW, Garibaldi R, Neuhaus EG, Smith PW. Antimicrobial use in long-term-care facilities. SHEA Long-Term-Care Committee. Infect Control Hosp Epidemiol. 2000;21(8):537–545. [DOI] [PubMed] [Google Scholar]
- 2.van Buul LW, Veenhuizen RB, Achterberg WP, et al. Antibiotic Prescribing In Dutch Nursing Homes: How Appropriate Is It? Journal of the American Medical Directors Association. 2015;16(3):229–237. [DOI] [PubMed] [Google Scholar]
- 3.van Buul LW, Vreeken HL, Bradley SF, et al. The Development of a Decision Tool for the Empiric Treatment of Suspected Urinary Tract Infection in Frail Older Adults: A Delphi Consensus Procedure. J Am Med Dir Assoc. 2018;19(9):757–764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Meddings J, Saint S, Krein SL, et al. Systematic Review of Interventions to Reduce Urinary Tract Infection in Nursing Home Residents. J Hosp Med. 2017;12(5):356–368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Katz MJ, Gurses AP, Tamma PD, Cosgrove SE, Miller MA, Jump RLP. Implementing Antimicrobial Stewardship in Long-term Care Settings: An Integrative Review Using a Human Factors Approach. Clin Infect Dis. 2017;65(11):1943–1951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Allemann H, Sund-Levander M. Nurses’ actions in response to nursing assistants’ observations of signs and symptoms of infections among nursing home residents. Nursing open. 2015;2(3):97–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Walker S, McGeer A, Simor AE, Armstrong-Evans M, Loeb M. Why are antibiotics prescribed for asymptomatic bacteriuria in institutionalized elderly people? A qualitative study of physicians’ and nurses’ perceptions. CMAJ : Canadian Medical Association journal = journal de l’Association medicale canadienne. 2000;163(3):273–277. [PMC free article] [PubMed] [Google Scholar]
- 8.Wilson BM, Shick S, Carter RR, et al. An online course improves nurses’ awareness of their role as antimicrobial stewards in nursing homes. American Journal of Infection Control. 2017;45(5):466–470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rhee SM, Stone ND. Antimicrobial stewardship in long-term care facilities. Infectious Disease Clinics of North America. 2014;28:237–246. [DOI] [PubMed] [Google Scholar]
- 10.Fleming A, Bradley C, Cullinan S, Byrne S. Antibiotic prescribing in long-term care facilities: a qualitative, multidisciplinary investigation. BMJ open. 2014;4(11):e006442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Schweizer AK, Hughes CM, Macauley DC, O’Neill C. Managing urinary tract infections in nursing homes: a qualitative assessment. Pharmacy world & science : PWS. 2005;27(3):159–165. [DOI] [PubMed] [Google Scholar]
- 12.Yang H, Thompson C, Bland M. The effect of clinical experience, judgment task difficulty and time pressure on nurses’ confidence calibration in a high fidelity clinical simulation. BMC Med Inform Decis Mak. 2012;12:113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Broom A, Broom J, Kirby E, Scambler G. Nurses as Antibiotic Brokers: Institutionalized Praxis in the Hospital. Qualitative Health Research. 2017;27(13):1924–1935. [DOI] [PubMed] [Google Scholar]
- 14.Cao X, Naruse T. Effect of time pressure on the burnout of home-visiting nurses: The moderating role of relational coordination with nursing managers. Jpn J Nurs Sci. 2019;16(2):221–231. [DOI] [PubMed] [Google Scholar]
- 15.Teng C, Shyu YL, Chiou W, Fan H, Lam SM. Interactive effects of nurse-experienced time pressure and burnout on patient safety: A cross-sectional survey. International journal of nursing studies. 2010;47(11):1442–1450. [DOI] [PubMed] [Google Scholar]
- 16.Thompson C, Dalgleish L, Bucknall T, et al. The effects of time pressure and experience on nurses’ risk assessment decisions: a signal detection analysis. Nursing research. 2008;57(5):302–311. [DOI] [PubMed] [Google Scholar]
- 17.Thompson C, Yang H. Nurses’ decisions, irreducible uncertainty and maximizing nurses’ contribution to patient safety. Healthcare quarterly (Toronto, Ont). 2009;12 Spec No Patient:e178–185. [DOI] [PubMed] [Google Scholar]
- 18.Yang H, Thompson C, Bland M. Do nurses reason ‘adaptively’ in time limited situations: the findings of a descriptive regression analysis. BMC Med Inform Decis Mak. 2014;14:96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Daneman N, Gruneir A, Newman A, et al. Antibiotic use in long-term care facilities. Journal of Antimicrobial Chemotherapy. 2011;66(12):2856–2863. [DOI] [PubMed] [Google Scholar]
- 20.Eure T, LaPlace LL, Melchreit R, et al. Measuring Antibiotic Appropriateness for Urinary Tract Infections in Nursing Home Residents. Infect Control Hosp Epidemiol. 2017;38(8):998–1001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gbinigie OA, Ordóñez-Mena JM, Fanshawe TR, Plüddemann A, Heneghan C. Diagnostic value of symptoms and signs for identifying urinary tract infection in older adult outpatients: Systematic review and meta-analysis. Journal of Infection. 2018;77(5):379–390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lemoine L, Dupont C, Capron A, et al. Prospective evaluation of the management of urinary tract infections in 134 French nursing homes. Med Mal Infect. 2018;48(5):359–364. [DOI] [PubMed] [Google Scholar]
- 23.Lim CJ, Kwong MW, Stuart RL, et al. Antibiotic prescribing practice in residential aged care facilities--health care providers’ perspectives. The Medical journal of Australia. 2014;201(2):98–102. [DOI] [PubMed] [Google Scholar]
- 24.Mitchell SL, Shaffer ML, Loeb MB, et al. Infection management and multidrug-resistant organisms in nursing home residents with advanced dementia. JAMA Intern Med. 2014;174(10):1660–1667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pettersson E, Vernby A, Molstad S, Lundborg CS. Infections and antibiotic prescribing in Swedish nursing homes: a cross-sectional study. Scandinavian journal of infectious diseases. 2008;40(5):393–398. [DOI] [PubMed] [Google Scholar]
- 26.Cooper D, McFarland M, Petrilli F, Shells C. Reducing Inappropriate Antibiotics for Urinary Tract Infections in Long-Term Care: A Replication Study. J Nurs Care Qual. 2019;34(1):16–21. [DOI] [PubMed] [Google Scholar]
- 27.Heath B, Bernhardt J, Michalski TJ, et al. Results of a Veterans Affairs employee education program on antimicrobial stewardship for older adults. American journal of infection control. 2016;44(3):349–351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Leduc A. Reducing the treatment of asymptomatic bacteriuria in seniors in a long-term care facility. The Canadian nurse. 2014;110(7):25–30. [PubMed] [Google Scholar]
- 29.Bech-Larsen T, Nielsen NA. A comparison of five elicitation techniques for elicitation of attributes of low involvement products. Journal of Economic Psychology. 1999;20(3):315–341. [Google Scholar]
- 30.de Bekker-Grob EW, Hol L, Donkers B, et al. Labeled versus unlabeled discrete choice experiments in health economics: an application to colorectal cancer screening. Value Health. 2010;13(2):315–323. [DOI] [PubMed] [Google Scholar]
- 31.Kistler CE, Beeber AS, Zimmerman S, et al. Nursing Home Clinicians’ Decision to Prescribe Antibiotics for a Suspected Urinary Tract Infection: Findings From a Discrete Choice Experiment. J Am Med Dir Assoc. 2020;21(5):675–682.e671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.High KP, Bradley SF, Gravenstein S, et al. Clinical practice guideline for the evaluation of fever and infection in older adult residents of long-term care facilities: 2008 update by the Infectious Diseases Society of America. Clin Infect Dis. 2009;48(2):149–171. [DOI] [PubMed] [Google Scholar]
- 33.Loeb MB, Craven S, McGeer AJ, et al. Risk factors for resistance to antimicrobial agents among nursing home residents. American journal of epidemiology. 2003;157(1):40–47. [DOI] [PubMed] [Google Scholar]
- 34.Nace DA, Perera SK, Hanlon JT, et al. The Improving Outcomes of UTI Management in Long-Term Care Project (IOU) Consensus Guidelines for the Diagnosis of Uncomplicated Cystitis in Nursing Home Residents. J Am Med Dir Assoc. 2018;19(9):765–769.e763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Stone ND, Ashraf MS, Calder J, et al. Surveillance Definitions of Infections in Long-Term Care Facilities: Revisiting the McGeer Criteria. Infection Control & Hospital Epidemiology. 2012;33(10):965–977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Loeb M, Bentley DW, Bradley S, et al. Development of minimum criteria for the initiation of antibiotics in residents of long-term-care facilities: results of a consensus conference. Infect Control Hosp Epidemiol. 2001;22(2):120–124. [DOI] [PubMed] [Google Scholar]
- 37.Loeb M, Brazil K, Lohfeld L, et al. Effect of a multifaceted intervention on number of antimicrobial prescriptions for suspected urinary tract infections in residents of nursing homes: cluster randomised controlled trial. BMJ (Clinical research ed). 2005;331(7518):669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kahneman D. Thinking, fast and slow. . 1st ed. New York: Farrar, Straus and Giroux; 2011. [Google Scholar]
- 39.Kahneman D, Tversky A. Prospect Theory - Analysis of Decision under Risk. . Econometrica. 1979;47(2):263–291. [Google Scholar]
- 40.Gosling SD, Rentfrow PJ, Swann WB. A very brief measure of the Big-Five personality domains. Journal of Research in Personality. 2003;37(6):504–528. [Google Scholar]
- 41.Rammstedt B, John OP. Measuring personality in one minute or less: A 10-item short version of the Big Five Inventory in English and German. Journal of Research in Personality. 2007;41(1):203–212. [Google Scholar]
- 42.Costa PT, McCrae RR. Normal personality assessment in clinical practice: The NEO Personality Inventory. Psychological Assessment. 1992;4(1):5–13. [Google Scholar]
- 43.Swait J, Louviere J. The role of the scale parameter in the estimation and comparison of multinomial logit models. Journal of Marketing Research. 1993;30(3):305–314. [Google Scholar]
- 44.Sloane PD, Kistler CE, Reed D, Weber DJ, Ward K, Zimmerman S. Urine Culture Testing in Community Nursing Homes: Gateway to Antibiotic Overprescribing. Infect Control Hosp Epidemiol. 2017;38(5):524–531. [DOI] [PubMed] [Google Scholar]
- 45.Teng C, Hsiao F, Chou T. Nurse-perceived time pressure and patient-perceived care quality. Journal of Nursing Management. 2010;18(3):275–284. [DOI] [PubMed] [Google Scholar]
- 46.Elwyn G, Miron-Shatz T. Deliberation before determination: the definition and evaluation of good decision making. Health Expectations. 2010;13(2):139–147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Scherer LD, de Vries M, Zikmund-Fisher BJ, Witteman HO, Fagerlin A. Trust in deliberation: The consequences of deliberative decision strategies for medical decisions. Health Psychology. 2015;34(11):1090–1099. [DOI] [PubMed] [Google Scholar]
- 48.Midthun S, Paur R, Lindseth G. Urinary Tract Infections: Does the Smell Really Tell? Journal of Gerontological Nursing. 2004;30(6):4–9. [DOI] [PubMed] [Google Scholar]
- 49.Smiley RA, Lauer P, Bienemy C, et al. The 2017 National Nursing Workforce Survey. Journal of Nursing Regulation. 2018;9(3):S1–S88. [Google Scholar]
- 50.Jones W, Drake C, Mack D, Reeder B, Trautner B, Wald H. Developing Mobile Clinical Decision Support for Nursing Home Staff Assessment of Urinary Tract Infection using Goal-Directed Design. Applied clinical informatics. 2017;8(2):632–650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Manning ML, Pfeiffer J, Larson EL. Combating antibiotic resistance: The role of nursing in antibiotic stewardship. American Journal of Infection Control. 2016;44(12):1454–1457. [DOI] [PubMed] [Google Scholar]
- 52.Wang L, Lansing B, Symons K, et al. Infection rate and colonization with antibiotic-resistant organisms in skilled nursing facility residents with indwelling devices. European Journal of Clinical Microbiology & Infectious Diseases. 2012;31(8):1797–1804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Cortes-Penfield NW, Trautner BW, Jump RLP. Urinary Tract Infection and Asymptomatic Bacteriuria in Older Adults. Infect Dis Clin North Am. 2017;31(4):673–688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Jerant A, Fenton JJ, Kravitz RL, et al. Association of Clinician Denial of Patient Requests With Patient Satisfaction. JAMA Intern Med. 2018;178(1):85–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Kravitz RL, Bell RA, Azari R, Kelly-Reif S, Krupat E, Thom DH. Direct Observation of Requests for Clinical Services in Office Practice: What Do Patients Want and Do They Get It? Archives of Internal Medicine. 2003;163(14):1673–1681. [DOI] [PubMed] [Google Scholar]
- 56.Strumiło J, Chlabicz S, Pytel-Krolczuk B, Marcinowicz L, Rogowska-Szadkowska D, Milewska AJ. Combined assessment of clinical and patient factors on doctors’ decisions to prescribe antibiotics. BMC Fam Pract. 2016;17:63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Zikmund-Fisher BJ, Kullgren JT, Fagerlin A, Klamerus ML, Bernstein SJ, Kerr EA. Perceived Barriers to Implementing Individual Choosing Wisely(®) Recommendations in Two National Surveys of Primary Care Providers. J Gen Intern Med. 2017;32(2):210–217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Butler CC, Rollnick S, Pill R, Maggs-Rapport F, Stott N. Understanding the culture of prescribing: qualitative study of general practitioners’ and patients’ perceptions of antibiotics for sore throats. BMJ (Clinical research ed). 1998;317(7159):637–642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Mody L, Juthani-Mehta M. Urinary Tract Infections in Older Women: A Clinical Review. JAMA. 2014;311(8):844–854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.D’Agata E, Loeb MB, Mitchell SL. Challenges in assessing nursing home residents with advanced dementia for suspected urinary tract infections. J Am Geriatr Soc. 2013;61(1):62–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Kovach CR, Logan BR, Simpson MR, Reynolds S. Factors Associated With Time to Identify Physical Problems of Nursing Home Residents With Dementia. American Journal of Alzheimer’s Disease & Other Dementias®. 2010;25(4):317–323. [DOI] [PMC free article] [PubMed] [Google Scholar]