Abstract
Background/Objectives:
To determine the impact of educational interventions, clinic workflow redesign, and quality improvement coaching on the frequency of advance care planning (ACP) activities for patients over the age of 65.
Design:
Nonrandomized before-and-after study.
Setting:
13 ambulatory care clinics with 81 primary care providers in eastern and central North Carolina.
Participants:
Patients across 13 primary care clinics staffed by 66 physicians, 8 physician assistants and 7 family nurse practitioners.
Interventions:
Interprofessional, interactive ACP training for the entire interprofessional team and quality improvement project management with an emphasis on workflow redesign.
Measurements:
From July 2017 through June 2018—number of ACP discussions, number of written ACP documents incorporated into the electronic medical record (EMR), number of ACP encounters billed.
Results:
Following the interventions, healthcare providers were more than twice as likely to conduct ACP discussions with their patients. Patients were 1.4 times more likely to have an ACP document included in their electronic medical record. Providers were significantly (p < 0.05) more likely to bill for an ACP encounter in only one clinic.
Conclusions:
Implementing ACP education for all clinic staff, planning for workflow changes to involve the entire interprofessional team and supporting ACP activities with quality improvement coaching leads to statistically significant improvements in the frequency of ACP discussions, the number of ACP documents included in the electronic medical record and number of ACP encounters billed.
Keywords: advance care planning, electronic medical records, electronic health records, primary care practice change, geriatrics
Introduction
Advanced Care Planning (ACP) is part of the therapeutic relationship between healthcare providers, patients and families. It explores values and goals of care to inform medical decisions should one lose decision-making capacity.1 ACP discussions over time is the first step that can lead to a billed encounter and ultimately a signed, written document. These discussions are now reimbursable using Medicare Current Procedural Terminology (CPT) codes© for ACP and are becoming more common as a requirement under the Medicare Annual Wellness Visit. Ultimately, respecting patients’ wishes prevents unnecessary medical procedures and reduces end-of-life expenditures.2
In 2015, the Health Resources and Services Administration (HRSA) provided 35.7 million dollars to fund 44 Geriatrics Workforce Enhancement Programs (GWEPS) across 29 states to address geriatrics issues, including ACP. The principal charge of these programs was to integrate geriatric principles into primary care to combat the shortage of primary care geriatricians.3,4
The Center for Aging and Health at the University of North Carolina at Chapel Hill launched the Carolina Geriatrics Workforce Enhancement Program (CGWEP) with a focus on ACP. The literature supports ACP as a key component of high value care for older adults. In 2016 Arnett et al, surveyed 118 healthcare providers engaged in ACP activities across many settings, including primary care. Thirty percent identified training as the greatest barrier to initiating ACP discussions.5 As the population ages providers find themselves confronted with difficult, time consuming end-of-life discussions without adequate training. According to Fulmer et al, only 29% of the 736 physicians surveyed nation-wide reported receiving ACP training.6
The percentage of older adults who complete a written ACP remains low despite the fact that most patients and healthcare providers are interested in planning for end-of-life care. In a nationally representative sample of adults ages 18 and up (n = 7,946), 67.8% expressed concerns about ACP but only 26.3% had completed an ACP.7 In 2015, a systematic review of 150 studies that included 795,909 patients of all ages, found a completion rate of 36.7%. This same review showed higher ACP rates for older adults at 45.6%.8
Many studies postulate that reminders in the electronic medical record (EMR) can increase ACP documentation. In 2018, Lemon et al, conducted a systematic review that included 15 studies. Three of these studied the effect of EMR-generated reminders on the frequency of ACP discussions. In the first study, rates improved from a baseline of 4% before the reminders to 15%. The second study showed gains from 4% to 24%. In the third study, baseline of 11.5% improved to 76%.9 Lemon also cites Linder et al, who showed that using a template in the EMR raised discussion rates from 4% to 63%.9 A randomized controlled trial by Bose-Brill showed improvement in written ACPs from 4% to 40%.9 In summary, the literature shows ACP rates as low as 4% can be improved up to 76% through EMR interventions.9
Adding training on ACP and redesigning clinic workflows further supports improvements. Lemon’s systematic review discusses how combining EMR reminders with training improved the percentage of veterans who completed a written ACP from 36.8% to 46.3% over 6 years.9 While studies included in Lemon’s review had a high risk of bias, the overall trends showed improvement. Additionally, Lemon’s studies focused on documenting advance directives rather than advance care planning discussions. A cluster randomized controlled trial, conducted by Overbeek et al, achieved 93% ACP written documentation for patients who received education and counseling on ACP from their provider compared with 34% of the control subjects.10 A comparison of the findings and approaches from the literature is included as Supplement 1.
Methods
The CGWEP ACP project collected data between “July of 2017” and “June of 2018” with 12 months of follow up. The Institutional Review Board of the University of North Carolina at Chapel Hill declared this research exempt. To reach a large number of practices efficiently, the CGWEP partnered with Practice Support Services (PSS) consultants at 2 Area Health Education Centers (AHECs). These PSS teams included clinicians and educators who had credibility with North Carolina primary care providers having previously assisted more than 100 practices in meeting quality improvement goals through better EMR documentation. The CGWEP recruited 13 clinics with 81 primary care providers.
The CGWEP’s ACP projects were designed to improve the percentage of patients over the age of 65 who were engaged in ACP. Engagement was defined in any of 3 ways: 1) Having a written ACP documented in the EMR 2) Having billed for ACP or 3) Documentation of an ACP discussion between patient and provider even if not billed. Patients had the option of declining ACP activities. These declinations were not included in the data. ACP discussions would ideally occur before ACP documents were signed or services billed. Billing for ACP was thought to be the easiest metric to increase because of relatively new Medicare reimbursement for ACP and the ease of incorporating ACP into the Medicare annual wellness visit. The additional revenue (approximately $86 per 99497 coded visit) would serve as an incentive.
Eight practices sought to increase ACP discussions with providers and/or other staff members, following educational and workflow interventions. Workflow redesigns included creating multiple opportunities for interprofessional team members to support ACP and maximizing use of the EMR. Front desk staff reminded patients that their provider was interested in their care preferences. Registered nurses reinforced ACP activities once the provider introduced the topic or social workers provided counseling on ACP. Data could include daily self-report by providers or mention of ACP in the progress note or problem list.
Four practices examined whether or not there was an ACP documented in the EMR before and after the interventions. Practices were free to choose what would be acceptable EMR documentation. There was some variation, but all of the practices used either a Do Not Resuscitate Order (DNR) or the North Carolina Medical Orders for Scope of Treatment (MOST) form.11 Two practices studied if they were able to increase the percentage of encounters billed for ACP. One practice (Site M), studied more than one measure, increasing ACP discussions and billing.
Patient Population
PSS Consultants encouraged ACP activities with all adult patients because ACP is most effective when it is conducted over time. Providers focused on geriatric patients the majority of whom were over age 65 and had chronic conditions. Patients reflected the profile of older adults in North Carolina—84% of whom have at least one chronic disease and 55% have two or more.12 The sample included low income patients from a safety net provider to middle and upper income patients seeing concierge providers.
Electronic Medical Record Preparation
PSS consultants operated as EMR experts, trainers and quality coaches. First, PSS consultants assessed the practice’s EMR capacity to report ACP activities using the 3 measures. Reporting capabilities varied considerably. Some EMRs had the ability to search text within provider’s notes to identify ACP activities while others relied on specific data fields. These fields were often not “turned on” in the EMR requiring additional programming expense. Activating existing data fields or creating searchable “smart phrases” within the EMR were the 2 main EMR interventions.
Workflow Analysis
Next, PSS consultants reviewed practice workflows to better incorporate ACP. To accommodate the demands of the schedule, put patients at ease and promote frequent discussions, the PSS consultants recommended an interprofessional team approach. Medical Assistants, Registered Nurses and Social Workers were trained to introduce ACP concepts and remind patients to discuss ACP with their provider. Administrative staff were trained to scan completed ACP documents into the EMR. This team approach and shared responsibility created multiple opportunities for ACP discussions. Lastly, PSS consultants educated providers and staff to capture the appropriate CPT codes for billing.
Interprofessional Training
The workflow changes were reinforced during one-hour long clinic-wide trainings at each site. Interprofessional teams that included all clinic staff participated in discussions with PSS Consultants and CGWEP experts regarding ACP goals and barriers, best practices in initiating ACP discussions, tools to track ACP activities, patient education resources and billing and legal requirements. During a second face-to-face training, (for providers only) the group discussed their experiences initiating ACP discussions. In one clinic (Site M), dyads of providers engaged in role-play, with one provider assuming the role of the patient and the other guiding the simulated ACP discussion. CGWEP faculty debriefed each team, highlighting aspects of the discussion that had gone well and suggesting areas for improvement.
At all 13 clinics, PSS consultants followed up at least monthly either in person, by phone or via email with printed educational materials, e-newsletters, and videos on how to discuss ACP and the complexities of billing. PSS consultants coached providers and staff on ACP care processes during quarterly on-site visits. A video of a 20-minute Lunch and Learn entitled “Advanced Care Planning and the Annual Wellness Visit” is archived on the SEAHEC website and YouTube channel to sustain the training and is available here: https://www.youtube.com/watch?v=IgeKZalc0wU&feature=youtu.be
This study aims to determine the impact of educational interventions, workflow redesign, and quality improvement coaching on the frequency of advance care planning (ACP) activities for patients over the age of 65. In presenting these results, descriptive statistics (means and standard deviations) were used to summarize pre and post-intervention percentages of ACP images in the medical record, ACP discussions, and ACP billed. Generalized estimating equations (GEE) were used to examine the odds of ACP in the medical record, ACP discussions, and ACP billing post intervention as compared to pre-intervention across practices, controlling for within-practice clustering. The Chi-square statistic was used to further examine within-practice intervention effects. Analyses were performed using the SAS Statistical Package (V9.4).
Results
Eight of the 13 clinics in this ACP project were located in eastern North Carolina in the greater Wilmington area. These included Site H that was affiliated with a large medical system with 24 providers and Site L; an Internal Medicine Residency training site with 7 providers and 22 residents. Two of the Wilmington practices (Sites B and C) were solo practitioners who offered concierge medicine, funded by private payments. Outside of Wilmington, Site D was located in a mid-sized city that houses a military base and the remaining 4 sites were in rural southeastern and central North Carolina. One of these, (Site E), operates as a non-profit. In total, 6 of the 13 clinics consisted of solo practitioners. An additional 5 clinics had fewer than 7 providers and 2 were large groups.
Interestingly smaller clinics with fewer providers and solo practitioners showed the greatest intervention efficacy. Those with < 1,000 visits were more than 3 times as likely to have patients engaged in ACP post-intervention (OR = 3.57, p < .0001) while in those with 1,000 or more the improvement was less pronounced (OR = 1.24. p < .0001). Solo practices had very good intervention efficacy, being 7.68 times as likely at post-intervention to have ACP patient engagement (OR = 7.68, p < .0001) as compared to pre-intervention. Non-solo practices showed much less intervention effect (OR = 1.23, p < .0001). The strongest intervention effect was seen in the private pay practices (OR = 4.77, p < .0001). Those accepting traditional insurance payments still showed significant improvements in ACP engagement though post intervention (OR = 1.76, p < 0001). The one “not for profit” site did not show any significant intervention efficacy (OR = 1.13, p = .67). Table 1 describes how ACP activities varied by practice charateristics.
Table 1.
ACP Activities by Practice Characteristics.
| Practice characteristics | OR | p value | |
|---|---|---|---|
| Visits per Year* | < 1,000 | 3.57 | < 0.0001 |
| >1,000 | 1.24 | < 0.0001 | |
| No, of Providers | Solo | 7.68 | < 0.0001 |
| More than 1 provider | 1.23 | < 0.0001 | |
| Dominant Payment Type | Private Pay | 4.77 | < 0.0001 |
| Commercial Insurance | 1.76 | < 0.0001 | |
| Not for Profit/Sliding Scale | 1.13 | = .67 | |
* Note study visits at post intervention used as a relative measure of clinic size.
Data by type of ACP outcome is reported for patients across 13 primary care sites with 81 providers (66 Physicians, 8 Physician Assistants and 7 Family Nurse Practitioners) on 3 measures: frequency of ACP discussions, numbers of ACP documents recorded in the EMR and ACP encounters billed. All outcomes are for patients age 65 and older. The number of patients varied by practice. For the 8 practices seeking to improve ACP discussion rates 5,131 patients were eligible pre-intervention “July 2017” and 4,831 post-intervention “June 2018.” Four practices that sought to increase ACP EMR documentation had 3,040 patients eligible pre-intervention and 3,419 post-intervention. Two practices studied ACP billing for 1,482 patients initially and 1,343 patients at post-intervention. In all, 9,653 patients were eligible pre-intervention and 9,593 post-intervention.
Patients Having ACP Discussions With Healthcare Providers
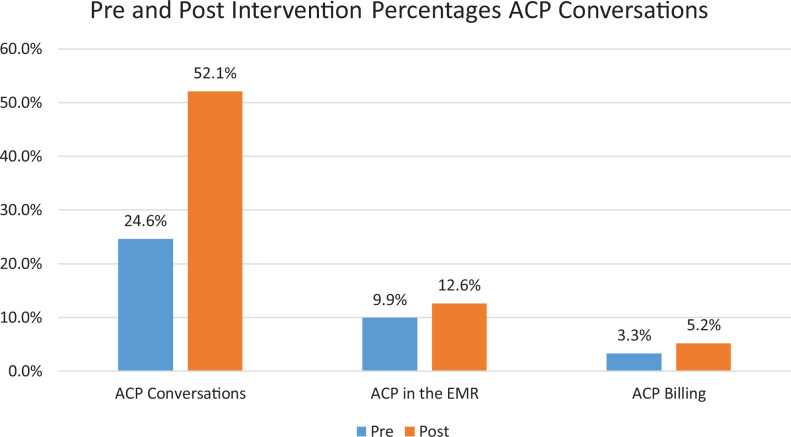
At all 8 sites, ACP discussions with providers increased post-intervention, with 52.1% of visits after the intervention discussing ACP vs. 24.6% before, a 27.5% increase. The increase was statistically significant, with providers more than twice as likely to have discussions post intervention (OR = 2.2 (95% CI: 1.1, 4.6), p = 0.03) as compared to pre-intervention.
Four of the 8 sites had statistically significant gains in the frequency of ACP discussions. The impact of the interventions varied by practice. Site D had an increase of 71.8% (p < 0.0001) and Site C and Site F had similarly large significant increases (66.8% and 64.9% respectively, both p < .0001 unadjusted for multiple comparisons). Increases varied in the remaining practices from 0.9% to 5.7%.
ACP Documented in the EMR
Four sites focused on EMR documentation. A total of 3,040 patients’ EMRs were reviewed at baseline and 3,419 post intervention. At pre-test, an average of 9.9% of patients have ACP in the EMR, while at post-test this increased to 12.6% (a 2.7% absolute increase). Results of the GEE model showed a patient was 1.4 times more likely to have ACP in the EMR after the intervention (OR = 1.4 (95% CI: 1.2, 1.6), p < 0.0001) as compared to before the intervention.
Similar to the findings for ACP discussions, 2 of the practices showed improvement of less than 1% (between 0.57% and 0.95%). These increases at Site H and Site R respectively were not significant (p = 0.80 and p = 0.37). Again, increases varied by practice, with the largest increases seen by Site I (an increase of 6.2%, p = 0.0007 unadjusted for multiple comparisons). A significant increase (3%) was also seen by Site L (p = 0.04 unadjusted for multiple comparisons).
Billing ACP
Finally, 2 sites experimented with increasing the number of patients who had ACP billable encounters with a primary care provider. The pre-intervention group included 1,482 patients vs. 1,343 post intervention.
The percentage of patient encounters billed for ACP increased from 3.3% pre-intervention to 5.2% post-intervention. This 1.9% increase was not statistically significant across practices with an OR = 1.3 (95% CI: .93, 1.9), p = 0.12).
Once again, within practice differences were apparent. Site J showed less than 0.5% increase (p = 0.59) while Site K increased by 3.3% post intervention (p = 0.04, unadjusted for multiple comparisons). Site K’s increase in billing is significant (p < 0.05). See Figure 1 for a graphical representation of the impact of the ACP interventions across all 3 measures. Table 2 describes the statistically significant results for each measure.
Figure 1.
Impact of interventions on ACP conservations, ACP in the EMR and ACP billing.
Table 2.
Analysis of ACP Activities by Practice Site.
| ACP outcomes | Site | Pre intervention | Post intervention | Increase | p value | ||||
|---|---|---|---|---|---|---|---|---|---|
| ACP Discussion | N | # of Discussions | N | # of Discussions | |||||
| A | 1048 | 10 | 0.95% | 1049 | 39 | 3.7% | 2.8% | < 0.0001 | |
| B | 326 | 71 | 21.8% | 160 | 44 | 27.5% | 5.7% | 0.164 | |
| C | 178 | 40 | 22.5% | 150 | 134 | 89.3% | 66.8% | < 0.0001 | |
| D | 839 | 216 | 25.7% | 481 | 469 | 97.5% | 71.8% | < 0.0001 | |
| E | 101 | 29 | 28.7% | 131 | 41 | 31.3% | 2.6% | 0.671 | |
| F | 309 | 91 | 29.4% | 389 | 367 | 94.3% | 64.9% | < 0.0001 | |
| G | 1052 | 471 | 44.8% | 1172 | 536 | 45.7% | 0.9% | 0.649 | |
| M* | 1278 | 290 | 22.7% | 1299 | 352 | 27.1% | 4.4% | 0.01 | |
| ACP Document in EMR | N | Document in EMR | N | Document in EMR | |||||
| H | 359 | 48 | 13.4% | 617 | 86 | 13.9% | 0.5% | 0.80 | |
| I | 765 | 98 | 12.8% | 865 | 164 | 19% | 6.2% | 0.0007 | |
| L | 638 | 39 | 6.1% | 638 | 58 | 9.1% | 3% | 0.04 | |
| M* | 1278 | 94 | 7.4% | 1299 | 108 | 8.3% | .95% | 0.37 | |
| ACP Encounter Billed | N | Billed | N | Billed | |||||
| J | 1096 | 44 | 4% | 1070 | 48 | 4.5% | 0.5% | 0.59 | |
| K | 386 | 10 | 2.6% | 273 | 16 | 5.9% | 3.3% | 0.04 | |
* Note Site M studies 2 interventions. Data is reported for both.
Discussion
This study of 9,962 patients shows that combining continuing education, workflow interventions and quality improvement coaching in primary care practices can improve ACP activities using 3 measures (1) the frequency of ACP discussions, (2) increased documentation of a patient’s wishes through a written ACP in the EMR, and (3) billing for ACP encounters. ACP interventions are operationally supported by Medicare reimbursement. The interventions were generally more effective in smaller practices with more private pay patients.
Interventions included continuing education Lunch and Learns for the entire interprofessional team, flyers, role-plays, quality improvement coaching, and workflow modifications. These interventions significantly increased the number of patients who received ACP counseling and paves the way for better tracking of ACP documents and billing.
Improving the frequency of ACP documents captured in the EMR, and supporting access to these documents by multiple providers, would lead to improved compliance with patients’ wishes for care. It is important to note though, that documentation alone is not proof of ongoing meaningful goals of care discussions between patient and providers. Each of the 3 measures studied serve as a proxy for the ongoing, in depth conversations that comprise ACP and are not goals in and of themselves. Rates of ACP in the EMR in this study, and in medical practice more broadly, continue to be low. In this study, at best, 19% of the older adult patients had an ACP document in their EMR. Until ACP becomes a standard part of the EMR, physicians will remain ill-informed as to their patients’ desires for end-of-life care.
Interestingly, only 2 practices studied their billing rate. A third practice began collecting billing data but discontinued because patients complained about incurring Medicare copays for ACP services. As the payment landscape shifts towards more bundled and value-based systems it is likely that ACP services will be further incentivized and become more commonplace. Based on the payment issue and the fact that for each of the 3 measures studied, only half of the practices achieved significant increases, additional research is needed to understand the patterns of ACP and how payment policy influences these patterns.
Limitations
All of the practices were located in central or southeastern North Carolina and 11 out of 13 were small, independent clinics. This study did not embed change processes in multi-site practices or across large healthcare systems. The practices represented a sample of convenience in that all practices had pre-existing relationships with AHEC PSS consultants. Further, these practices self-selected the geriatrics topic of ACP for their quality improvement work. Because of these factors, providers may have been more motivated to demonstrate improvement as compared to primary care practitioners in general.
Conclusions
ACP addresses patients’ end-of-life wishes, provides less futile care and lowers costs. Using existing relationships and providing frequent quality improvement coaching, workflow redesigns, EMR adaptation, and education can improve the frequency of ACP discussions and the EMR documentation of patient wishes. Billing for these services was less likely to be an area of interest to the primary care practices in our sample despite Medicare reimbursement. It is expected that interest in ACP activities will grow should primary care providers outside of these sites receive training and support and learn of the availability of reimbursement.
This study was supported by the Health Resources and Services Administration (HRSA) of the U.S. Department of Health and Human Services (HHS), Geriatrics Workforce Enhancement Program grant number 2UQHP28734. The contents are those of the author(s) and do not necessarily represent the official views of, nor an endorsement, by HRSA, HHS or the United States Government.
Supplemental Material
Supplemental Material, ACP_Supplement_1_Literature_review for Educational Interventions to Improve Advance Care Planning Discussions, Documentation and Billing by Cristine B. Henage, J. Marvin McBride, Joseph Pino, Jessica Williams, Jill Vedovi, Nicole Cannady, Liz Riley Buno, Toni Chatman, Jan Busby-Whitehead and Ellen Roberts in American Journal of Hospice and Palliative Medicine®
Footnotes
Authors’ Note: We certify that this is novel work that lends statistically significant support to the concept that training healthcare providers in Advance Care Planning (ACP) combined with redesigned clinic workflows can increase the frequency of ACP discussions, the number of ACP documents scanned into the electronic medical record and the number of ACP encounters billed. The study was designed by Drs. Henage, McBride, Pino, Busby-Whitehead and Roberts. Data was collected by Ms. Williams, Ms. Bruno, and Ms. Chatman. All authors participated in the analysis and interpretation of data, and preparation of manuscript. The authors would like to acknowledge the contributions of administrators from Wake Area Health Education Center Diane C. Yelverton, MS, RNC and Elaine B. Owens, MPA, and thank them for their leadership and support. In addition, we acknowledge Anne Hunt, ScD, for her contributions to the statistical analysis of the data.
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This project was supported by funds from the Bureau of Health Professions (BHPr), Health Resources and Services Administration (HRSA), Department of Health and Human Services (DHHS) under grant number # U1QHP28734 Carolina Geriatric Workforce Enhancement Program. This information or content and conclusions are those of the authors and should not be construed as the official position or policy of, nor should any endorsements be inferred by the BHPr, HRSA, DHHS or the US Government. The Center for Aging and Health, Carolina Geriatric Workforce Enhancement Program also provided support for this activity. The sponsors had no role in the design, methods, analysis, or preparation of the manuscript.
ORCID iD: Cristine B. Henage  https://orcid.org/0000-0002-3963-8170
https://orcid.org/0000-0002-3963-8170
Supplemental Material: Supplemental material for this article is available online.
References
- 1. Dying in America: Improving and Honoring Individual Preferences Near the End of Life. Institute of Medicine. The National Academies Press; 2014. [PubMed] [Google Scholar]
- 2. Lunder U, Červ B, Kodba-Čeh H. Impact of advance care planning on end-of-life management. Curr Opin Support Palliat Care. 2017;11(4):293–298. [DOI] [PubMed] [Google Scholar]
- 3. Health Resources and Services Administration. July 13, 2015. Accessed September 16, 2019. https://www.hrsa.gov/about/news/press-releases/2015-07-13-geriatric-workforce.html
- 4. Geriatrics Workforce by the numbers. American Geriatrics Society. 2017. Accessed September 16, 2019. https://www.americangeriatrics.org/geriatrics-profession/about-geriatrics/geriatrics-workforce-numbers
- 5. Arnett K, Sudore RL, Nowels D, Feng CX, Levy CR, Lum HD. Advance care planning: understanding clinical routines and experiences of interprofessional team members in diverse healthcare settings. Am J Hosp Palliat Med. 2017;34(10):946–953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Fulmer T, Escobedo M, Berman A, Koren MJ, Hernández S, Hult A. Physicians’ views on advance care planning and end-of-life care conversations. J Am Geriatr Soc. 2018;66(6):1201–1205. [DOI] [PubMed] [Google Scholar]
- 7. Rao JK, Anderson LA, Lin FC, Laux JP. Completion of advance directives among U.S. consumers. Am J Prev Med. 2014;46(1):65–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Yadav KN, Gabler NB, Cooney E, et al. Approximately one in three US adults completes any type of advance directive for end-of-life. Health Aff. 2017;36(7):1244–1251. [DOI] [PubMed] [Google Scholar]
- 9. Lemon C, De Ridder M, Khadra M. Do electronic medical records improve advance directive documentation? A systematic review. Am J Hosp Palliat Med. 2018;36(3):255–263. [DOI] [PubMed] [Google Scholar]
- 10. Overbeek A, Korfage IJ, Jabbarian LJ, et al. Advance care planning in frail older adults: a cluster randomized controlled trial. J Am Geriatr Soc. 2018;66(6):1089–1095. [DOI] [PubMed] [Google Scholar]
- 11. Caprio AJ, Rollins VP, Roberts E. Health care professionals’ perceptions and use of the medical orders for scope of treatment (MOST) form in North Carolina nursing homes. J Am Med Dir Assoc. 2012;13(2):162–168. [DOI] [PubMed] [Google Scholar]
- 12. North Carolina is Aging! NC Department of Health and Human Services, Division of Aging and Adult Services. 2019. Accessed July 15, 2020. https://files.nc.gov/ncdhhs/documents/files/NC%20State%20Aging%20Profile%202018.pdf
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material, ACP_Supplement_1_Literature_review for Educational Interventions to Improve Advance Care Planning Discussions, Documentation and Billing by Cristine B. Henage, J. Marvin McBride, Joseph Pino, Jessica Williams, Jill Vedovi, Nicole Cannady, Liz Riley Buno, Toni Chatman, Jan Busby-Whitehead and Ellen Roberts in American Journal of Hospice and Palliative Medicine®