Abstract
Background:
Patients who undergo anterior cruciate ligament reconstruction (ACLR) present with deficiencies in strength, functional performance, and biomechanical function at return-to-activity. ACLR patients with abnormal strength and function may be at a greater risk for secondary injury and post-traumatic osteoarthritis.
Purpose:
To examine quadriceps strength, functional performance, and knee biomechanics in patients who are 9, 12, 18, and 24 months post-ACLR.
Design:
Cross-Sectional Study.
Methods:
Eighty-two subjects (45 female) who underwent ACLR and were cleared to return to activity were recruited. Subjects were assigned to one of four groups based on their time from ACLR: 9-months (285.26 ± 8.16 days), 12-months (373.59 ± 8.81 days), 18-months (557.50 ± 11.96 days), and 24-months post-operative (741.05 ± 11.86 days). Quadriceps strength was measured concentrically at 60°/second. Functional performance was assessed by measuring maximal hop distances or heights during dynamic hopping/jumping tests (single leg hop, triple hop, cross-over hop, and single leg vertical hop). Biomechanical function was evaluated during the dynamic hop tests by using peak sagittal plane knee flexion angles recorded during landings. Strength, performance, and biomechanics data were collected for both limbs and reported as symmetry scores (injured/uninjured*100). Self-perceived function was measured using the International Knee Documentation Committee (IKDC) subjective knee form.
Results:
Quadriceps strength in the 9- (77.61±16.73) and 12-month (77.80±13.99) groups were significantly lower (P<.01) when compared to the 24-month group (92.40±15.55). Self-perceived function for the 9-month group (79.33±10.40) was significantly lower (P<.01) when compared to 12- (87.58±10.29), 18- (89.81±8.36), and 24-month (91.59±5.70) groups. Single leg hop distance symmetry was significantly lower (P<.01) for the 9-month group (90.01±9.46) when compared to the 18- (96.24±6.47) and 24-month (96.30±6.46) groups, triple hop symmetry was significantly lower (P < .05) for the 9-month group (90.2±10.03) when compared to the 18- (96.83±9.60) and 24-month (95.91 ± 6.36) groups, and cross-over hop was significantly lower (P< .05) for the 9-month group (88.35±13.53) when compared to the 18-month (95.85±8.63) and 24-month (97.10±4.12) groups.
Conclusions:
Quadriceps strength, self-perceived function, and functional performance, improve 9 to 24 months post-ACLR indicating recovery is ongoing after return-to-activity. Return-to-activity criteria after ACLR should objectively account for strength and function.
Keywords: anterior cruciate ligament, knee, biomechanics, muscle, weakness
INTRODUCTION
Injury to the anterior cruciate ligament (ACL) is a common occurrence, with an incidence of 68.6 per 100,000 person-years per annum.31 In persons that are physically active or the knee is unstable, surgical reconstruction of the anterior cruciate ligament (ACLR) is the recommended path of care. Although ACLR restores sagittal plane knee joint stability, deficiencies in quadriceps strength,26,27,32,36 biomechanical function,20 and functional performance24,33 are present, and often linger even after patients are cleared to return to activity. At the time of return to activity (e.g. 6–9 months after ACLR), ACLR patients present with substantial between limb asymmetry in quadriceps strength5,26,27, gait biomechanics21, and functional performance9.
Return to activity/sport while deficient in strength, biomechanical function, and/or functional performance, can lead to ACL re-injury and/or injury to the contralateral limb.9 A study by Grindem et al9 found that ACLR patients who returned to activity with strength and functional performance symmetry above 90% had a significantly reduced rate of re-injury, while those subjects with poor symmetry had a noticeably higher risk of re-injury. Poor quadriceps strength has also been associated with altered sagittal plane knee flexion angles.21,26 Abnormal knee joint kinematics have predictive ability for primary ACL tears in female athletes,13 and abnormal knee kinetics have been linked to secondary ACL injury.29
Patients who undergo ACLR are usually medically cleared to return to activity at six to seven months post-operative,1 with a return to preinjury level of activity occurring within 24 months of surgery.9 However, within the same 24 month timeframe there is also a high risk of subsequent ACL injury.9,28,42 Previous research found a secondary ACL injury in 6% of subjects, with an equal rate of ACL tears in the ipsilateral and contralateral limb.42 Paterno et al28 studied the incidence rates of ACL injury in patients within two years of ACLR and when compared to controls, ACLR patients were 15 times more likely to incur an ACL injury than healthy controls.
Given the risk of a second ACL injury occurring during the first 24 months post-ACLR, it is imperative to examine the recovery of factors related to injury/reinjury, such as strength, knee joint biomechanics, and functional performance. While quadriceps strength deficiencies have been shown within two years after ACLR,7,16,27,35 the magnitude of functional performance changes and biomechanical function is less studied. Much of the research examining knee joint biomechanics14,21,26,32 or functional hop performance9,10,12,26,33 in ACLR patients was performed within the first 12 months (e.g. 3–12 months post-ACLR) following surgery. Studies that examined biomechanics4,40 in ACLR patients after 12 months post-operative (e.g. on average 3–5 years post-ACLR) did not characterize recovery at multiple timepoints within the high-risk 24-month timeframe. To our knowledge no study has examined functional hop test performance from 12 to 24 months post-operative.
In order to better characterize ACLR patient recovery within 24 months of surgery we propose to examine strength, biomechanics, and functional performance symmetry in persons at 9, 12, 18, and 24 months post-operative. By examining strength, functional hop performance, and knee joint biomechanics at these timepoints we seek to better to understand the amount and type of deficiency present, in order to help clinicians target problem areas for recovery. We hypothesize that ACLR patients at 9 months will present with substantial inter-limb asymmetry in quadriceps strength, knee biomechanics, and functional performance. Furthermore, we hypothesize patients that have had more recovery time after ACLR will demonstrate less asymmetries (i.e. patients 18 months post-operative will be more symmetrical than those at 12 months post-operative). Lastly, we hypothesize that the ACLR patients at 24 months post-operative will present with symmetrical (≥90%) quadriceps strength, biomechanical function, and functional performance.
METHODS
Participants
Eighty-two subjects (45 female, 37 male; age = 20.2 ± 6.6 years, height = 170.3 ± 9.0 cm, mass = 73.8 ± 15.2 kg) who had undergone ACLR and were cleared to return to activity by their treating physician were recruited to participate in this study. A sample size of 15 subjects per group was estimated based on an effect size (f) of 1.378 using previous literature examining quadriceps strength at different time points post ACLR (9, 12, and 24 months).15,25,44 Subjects were recruited into one of four groups (9 months ± 21 days, 12 months ± 21 days, 18 months ± 21 days, and 24 months ± 21 days) depending on time from surgery. Subjects were eligible to participate if they: 1) were between 14 to 45 years of age, 2) had an acute ACL injury, 3) had no prior history of knee ligament injury to either limb, 4) had no history of a prior knee surgery to either limb, 5) had no surgical intervention on any knee ligament other than the ACL, 6) were not pregnant, 7) and did not have a cardiac demand-type pacemaker. Fifty-seven of the subjects had surgical reconstruction with a bone-patellar tendon-bone autograft, twenty with a semitendinosus-gracilis autograft, and five with a quadriceps tendon autograft. All subjects had their surgical reconstruction performed by 1 of 3 orthopaedic surgeons from our sports medicine clinic. Objective criteria used by the physicians to clear patients to return to activity included: 1) full range of motion, 2) no visible effusion, 3) completion of a three-week agility program, and 4) successful completion of a leg press test. To pass the leg press test, individuals needed to complete at least 15 repetitions of a single-leg (i.e. ACLR limb) leg press with the knee moving from neutral to 90 degrees of flexion at 100% of body weight. This study was reviewed and approved by the University of Michigan Medical Institutional Review Board.
Study Procedures
All measurements described below were collected in the same session in the Orthopaedic and Rehabilitation Biomechanics laboratory at The University of Michigan. Recruitment took place between 2015–2017.
Quadriceps Strength
Isokinetic quadriceps strength was assessed bilaterally and collected with a Biodex System 3 dynamometer (Biodex Medical Systems; Shirley, NY). Subjects were positioned in the dynamometer with the hip and knee flexed to 90°, and secured into place with straps across the torso, waist, thigh, and shank. Subjects were instructed to perform three sub-maximal (i.e. 50% effort) practice knee extension contractions at a rate of 60° per second prior to attempting the maximal effort trials. Following the sub-maximal contractions, subjects rested for two minutes, and then attempted five maximal intensity concentric knee extensions. The trial with the maximal torque for each leg was selected and used to quantify the isokinetic quadriceps index (Equation 1) for statistical analyses. Limb testing order was randomized for each subject before testing began.
| Equation 1 |
Dynamic Hop Testing Protocol
Subjects performed a battery of dynamic hop tests that are clinically relevant to ACLR patient functional recovery. The hop test battery included: single-leg hop, triple hop, cross-over hop, and single-leg vertical hop. During hopping the MyoMotion 3-dimensional wireless motion analysis system (Noraxon USA Inc., Scottsdale, AZ, USA) sampling at 200Hz was used to record sagittal plane knee flexion angles. Eight wireless inertial measurement units (IMUs) were placed on each subject on specific lower limb and torso segments (left foot, right foot, left shank, right shank, left thigh, right thigh, pelvis, and lower thoracic), and Noraxon footswitch insoles were placed into the subjects’ shoes. Once the footswitch insoles were secured in the shoes, a wireless footswitch sensor was placed on the medial aspect of the corresponding shank and connected to the insole. Once all IMU’s, insoles, and sensors were secured, the subject was then ready to perform the hop testing. Pilot data collected in our laboratory suggest there is a “good-to-high” level of agreement between knee flexion angle measured with IMU’s and with standard motion capture ICCs (3,k) = .85–.99.
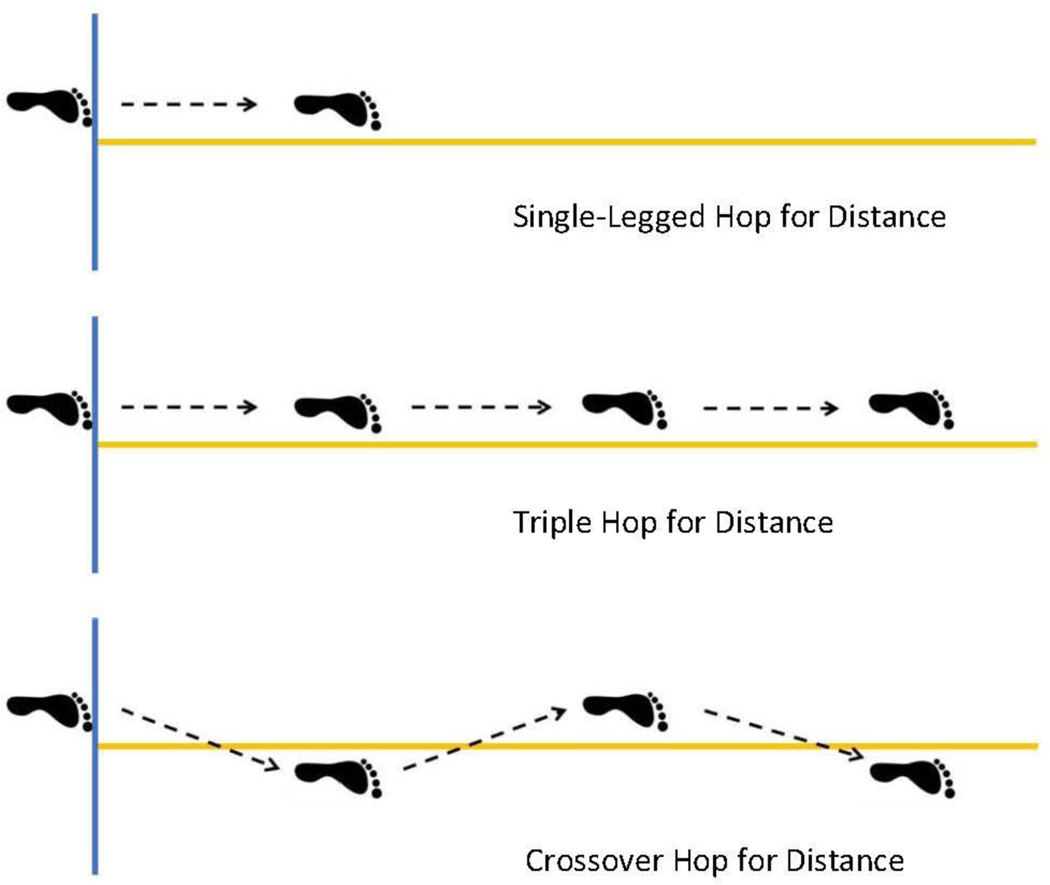
Subjects performed five independent successful attempts, for each limb, for each dynamic hop test. A successful attempt required the subject to hold the final landing of the task for two seconds without shuffling his/her landing foot or making ground contact with any body part other than the landing foot. Subjects were instructed to jump for maximal distance during the single-leg hop, triple hop, and cross-over hop tests, and maximal height for the single leg vertical hop, as is common in post-operative ACLR clinical hop testing (Figure 1). Maximal values for hop distance and hop height were recorded and used for analysis.
Figure 1.
Graphic depiction of the hop tests for distance utilized in subject testing. For all tests, subjects hopped on a single leg and were instructed to hop as far as possible in order to achieve maximal distance. For the single-legged hop, a single one-legged forward hop was performed forward. The triple hop required three forward hops to be performed in a row. With the crossover hop, subjects were instructed to perform three consecutive forward hops while crossing the central line with each hop. The first hop crossed medially, the second hop crossed laterally, and the third and final hop crossed medially.
Maximal vertical hop height was measured with the use of a Vertec, vertical jump measuring device (Sports Imports, Hilliard, OH, USA). Prior to testing, a baseline measurement of each subject’s stand and reach height was measured using the Vertec. Subjects stood directly underneath the vanes of the device, raised both arms straight up overhead and pushed away as many vanes as they could reach with both hands simultaneously. This stand and reach value was recorded as the subjects baseline. During the actual testing, subjects were asked to jump as high as they possibly could off one leg, and try to move the highest vane they could reach. The height of the highest vane reached by the subject during the hop was recorded, the baseline value was subtracted, and the final value was kept as a measure of hop height for that attempt.
All measures of functional performance, maximal hop distance and maximal hop height, were converted into symmetry scores (Equation 1) in the same manner as the quadriceps index, and the symmetry values were used for statistical analysis. Dynamic hop test order and limb order were randomized prior to testing. All dynamic hop testing was performed after the strength testing.
Kinematic Data Processing
Sagittal plane knee kinematics for the hop tests were assessed during the landing phases specific to each test, because it is during the landing phases that the greatest loads are experienced in the knee and when most ACL injuries occur. For the single leg forward hop and the single leg vertical hop there is only one hop and one landing. The landing phase for these tasks was defined as initial foot contact with the ground to peak knee flexion. Peak knee flexion was chosen to define the end of the landing as it characterizes the end of the deceleration phase of the movement during which peak ground reaction forces and peak knee moments would occur. For the triple hop and cross-over hop there are three hops and three landing phases. We assessed each of the three landing phases, for both the triple hop and cross-over hop, and defined each landing phase in the same manner as the single leg forward hop and the single leg vertical hop, initial contact to peak knee flexion. Foot contact was identified with the use of footswitch insoles.
For the single leg forward hop and single leg vertical hop the average peak knee flexion for all the attempts for each limb were used for analysis. For triple hop and cross-over hop attempts, the average peak knee flexion values for each of the three landings was calculated, and then an average across all three landing phases was calculated to be used as the peak knee flexion value for that attempt. Symmetry scores were created for each hop task using the test specific peak knee flexion values and calculated in the same manner as the quadriceps index (Equation 1). The symmetry values were used in the statistical analysis.
Patient-Reported Outcomes
Subjects completed the International Knee Documentation Committee (IKDC) form for subjective knee function, and the Tegner activity rating scale for graded physical labor and sports activities. The IKDC is a reliable and valid measure of patient-reported function in the ACLR population.39 The IKDC is comprised of three different types of questions: three11-point Likert scales, fourteen 5-point Likert scales, and one dichotomous “yes” or “no”. The IKDC was processed and scored on a 0 to 100 scale, with 100 being representative of highest knee function, for use in statistical analysis. The Tegner activity rating scale is a standardized grading system for physical activity that is both reliable and valid for use in the ACLR population.2
Statistical Analysis
Separate one-way ANCOVAs with graft type and gender used as a covariates were run for all dependent variables. Dependent variables included: strength (isokinetic quadriceps index), peak knee flexion symmetry from all four hopping tasks, maximal hop distance symmetry for the three applicable hopping tasks, maximal vertical jump height symmetry and score on the IKDC. The independent variable was group (9 months, 12 months, 18 months, or 24 months). One-way ANOVAs were performed to assess demographic differences between groups for subject age, height, and weight, and chi-square regression was used to assess between group difference in the categorical variables (gender and graft type). Due to the low frequency of graft type per timepoint, Fisher’s Exact Test was used to assess significance. Least Significant Difference post hoc comparisons were performed once ANCOVA between group significant differences were found. Binomial logistic regression analyses were completed, with statistical significance determined using the Wald chi-square test, to examine the between group difference in the rate of subjects that met acceptable clinical criteria (i.e. 90% limb symmetry indices) for quadriceps strength, functional performance (distance or height hopped), biomechanical function (peak knee flexion for the hop/jump tests), and self-reported function (≥85% score on IKDC). Given the variability in our participants’ activity levels at time of return to activity, we wanted to consider the effect that activity level may have played on our outcome measures. Therefore, regression analyses were performed examining the relationship between the Tegner activity score and any dependent variable where the ANCOVAs showed between group differences (i.e. strength and functional performance). The a priori α level was set at P ≤ .05 for all tests. Statistical analyses were performed with SPSS (version 22; IBM Corp, Armonk, NY).
RESULTS
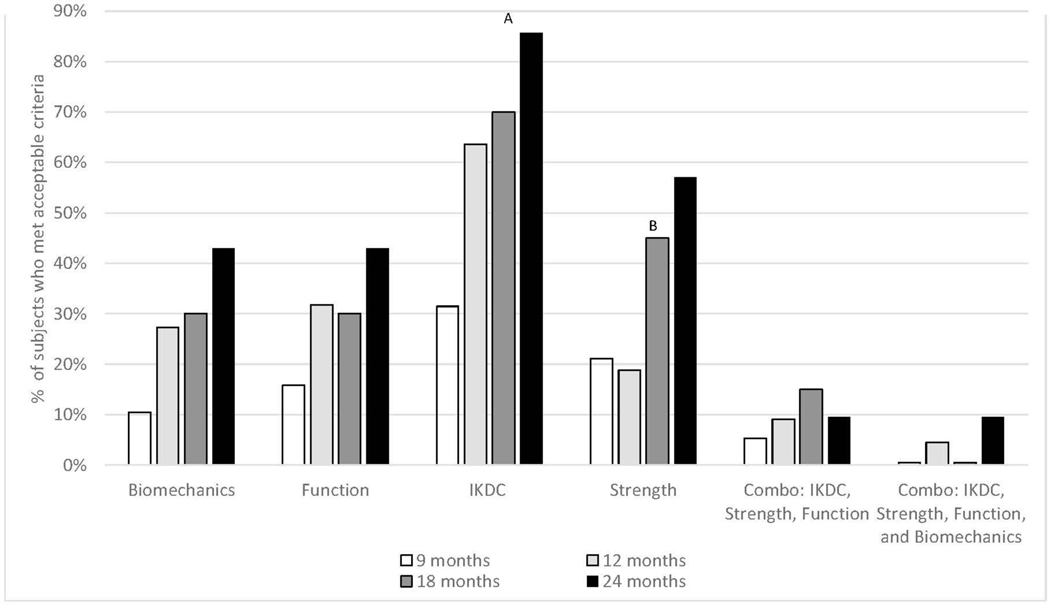
No significance differences in demographics were found between groups (P > .05) (Table 1). Descriptive statistics including means and standard deviations for all variables for each group can be found in Table 2. Significant between group differences were noted for the IKDC (F3,76 = 8.04, P < 0.001), quadriceps index (F3,76 = 3.97, P = .01), and maximal hop distance symmetry for single leg hop (F3,76 = 4.18, P = .01), triple hop (F3,76 = 3.07, P = .03), and cross-over hop (F3,76 = 3.69, P = .02). Post hoc analyses showed significant difference in the isokinetic quadriceps strength index between the 9- and 24-month groups, (P = .01), and between the 12- and 24-month groups, (P = .01). A significant difference in IKDC scores was found between the 9- and 12-months groups, (P < .01), the 9- and 18-month groups, (P < .001), and the 9- and 24-month groups, (P < .001). Significant differences in hop symmetry were found for the maximal single leg hop distance, maximal triple hop distance, maximal cross-over hop distance between the 9 months and 18-month groups and the 9-month and 24-month groups (P ≤ .03). No significant between group differences in peak knee flexion symmetry were found during any hop test (P > .05). Significant differences for the number of patients meeting clinical recommendations for isokinetic quadriceps strength index (x2 = 9.06, P = .03), was noted between the 9- and 24-month groups (P = .02), and the 12- and 24-month groups (P = .01) (Figure 2). Significant differences were also noted between the number of patients meeting clinical recommendations for the IKDC at 9 months when compared with the remaining 3 groups (P < 0.05). No significant differences were found between groups for the percentage of subjects who met the clinical criteria for functional performance or biomechanical function (P > .05).
Table 1.
Patient Demographic Information.
| Groups | N | Age (years) | Sex | Height (cm) | Mass (kg) | Graft type | Concomitant | Time (Surgery to Test, days) | Tegner Scores (Score, # of subjects with score) | Return to Preinjury Activity |
|---|---|---|---|---|---|---|---|---|---|---|
| 9 months | 19 | 19.5 ± 5.7 | Male= 8 Female= 11 | 168.9 ± 10.2 | 75.0 ± 20.2 | BPTB= 14 STG= 3 QUAD= 2 | MMR= 2/ LMR= 1 MMX= 0 / LMX= 6 CMB= 2 / Other= 0 | 285.26 ± 8.16 | T10=0/ T9=3/ T8=2/ T7=2/ T6=2/ T5=6/ T4=4/ T3=0/ | 4 |
| 12 months | 22 | 20.2 ± 7.8 | Male= 9 Female= 13 | 169.1 ± 8.2 | 70.0 ± 10.4 | BPTB= 15 STG= 5 QUAD= 2 | MMR= 1 / LMR= 2 MMX= 0 / LMX= 3 CMB= 2 / Other= 1 | 373.59 ± 8.81 | T10=2/ T9=9/ T8=0/ T7=2/ T6=3/ T5=3/ T4=3 /T3=0/ | 10 |
| 18 months | 20 | 20.5 ± 6.6 | Male= 12 Female= 8 | 174.3 ± 9.5 | 75.9 ± 15.3 | BPTB= 15 STG= 4 QUAD= 1 | MMR= 2 / LMR= 2 MMX= 0 / LMX= 4 CMB= 2 / Other= 0 | 557.50 ± 11.96 | T10=3/ T9=9/ T8=1/ T7=3/ T6=2/ T5=1/ T4=0/ T3=1 | 13 |
| 24 months | 21 | 20.5 ± 6.4 | Male= 8 Female= 13 | 169.1 ± 7.4 | 74.6 ± 14.5 | BPTB= 13 STG= 8 QUAD= 0 | MMR= 1 / LMR= 4 MMX= 0 / LMX= 2 CMB= 0 / Other= 2 | 741.05 ± 11.86 | T10=0/ T9=9/ T8=0/ T7=5/ T6=4/ T5=3/ T4=0/ T3=0/ | 10 |
Abbreviations: BPTB, Bone-patellar tendon-bone, STG, Semitendinosus-Gracilis, QUAD, Quadriceps Tendon, MMR, Medial Meniscus Repair, LMR, Lateral Meniscus Repair, MMX, Medial Meniscectomy, LMX, Lateral Meniscectomy, CMB, multiple meniscal intervention, Other, Abrading/ Debriding, Return to Preinjury Activity, the number of subjects who returned to preinjury level of activity per group.
Subjects did not significantly differ in Age, Sex, Height, Mass, or Graft Type between Groups.
Table 2.
Quadriceps Strength Symmetry, Functional Performance Symmetry, Biomechanical Function Symmetry, and IKDC values per group: means +− SD and percentage of subjects per group who met the clinical threshold.
| 9 months | 12 months | 18 months | 24 months | |
|---|---|---|---|---|
| N | 19 | 22 | 20 | 21 |
| Quadriceps Index | 77.61 ± 16.73c | 77.80 ± 13.99d | 86.74 ± 19.14 | 92.40 ± 15.55c,d |
| # of subjects with QI≥ 90% | 4 (21.1%) | 4 (18.8%) | 9 (45.0%) | 12 (57.1%) |
| SLH PKF Symmetry | 86.25 ± 12.94 | 87.01 ± 12.73 | 94.23 ± 18.36 | 92.85 ± 14.08 |
| # of subjects with SLH PKF Sym ≥ 90% | 8 (42.1%) | 7 (31.8%) | 12 (60.0%) | 13 (61.9%) |
| TH PKF Symmetry | 88.59 ± 11.63 | 90.95 ± 7.97 | 93.05 ± 12.19 | 94.34 ± 12.13 |
| # of subjects with TH PKF Sym ≥ 90% | 10 (52.6%) | 12 (54.5%) | 12 (60.0%) | 15 (71.4%) |
| CH PKF Symmetry | 86.87 ± 10.40 | 89.69 ± 10.40 | 93.70 ± 16.20 | 92.63 ± 11.24 |
| # of subjects with CH PKF Sym ≥ 90% | 8 (42.1%) | 12 (54.5%) | 10 (50.0%) | 13 (61.9%) |
| SLVH PKF Symmetry | 90.32 ± 17.88 | 88.91 ± 10.94 | 89.25 ± 14.49 | 90.72 ± 13.09 |
| # of subjects with SLVH PFK Sym ≥ 90% | 10 (52.6%) | 11 (50.0%) | 8 (40.0%) | 12 (57.1%) |
| SLH Max Distance Symmetry | 90.01 ± 9.46b,c | 93.48 ± 5.53 | 96.24 ± 6.47b | 96.30 ± 6.46c |
| # of subjects with SLH MD Sym ≥ 90% | 13 (68.4%) | 17 (77.3%) | 16 (80.0%) | 17 (81.0%) |
| TH Max Distance Symmetry | 90.26 ± 10.03b,c | 93.24 ± 6.25 | 96.83 ± 9.60b | 95.91 ± 6.36c |
| # of subjects with TH MD Sym ≥ 90% | 12 (63.2%) | 16 (72.7%) | 18 (90.0%) | 18 (85.7%) |
| CH Max Distance Symmetry | 88.35 ± 13.53b,c | 93.18 ± 8.31 | 95.85 ± 8.63b | 97.10 ± 4.12c |
| # of subjects with CH MD Sym ≥ 90% | 10 (52.6%) | 17 (77.3%) | 16 (80.0%) | 20 (95.2%) |
| SLVH MH Symmetry | 87.06 ± 17.35 | 89.64 ± 18.43 | 89.67 ± 16.42 | 90.70 ± 15.13 |
| # of subjects with SLVH MH Sym ≥ 90% | 6 (31.6%) | 9 (40.9%) | 8 (40.0%) | 11 (52.4%) |
| IKDC | 79.33 ± 10.40a,b,c | 87.58 ± 10.29a | 89.81 ± 8.36b | 91.59 ± 5.70c |
| # of subjects with IKDC ≥ 85% | 6 (31.5%) | 14 (63.6%) | 14 (70.0%) | 18 (85.7%) |
(Denotes between group significance: a- significance between the 9 and 12 months groups; b- significance between the 9 and 18 months groups; c- significance between the 9 and 24 months groups; d- significance between the 12 and 24 months groups.)
Abbreviations: IKDC, International Knee Documentation Committee Knee Form, QI, Quadriceps Index, SLH, Single Leg Forward Hop, TH, Triple Hop, CH, Cross-Over Hop, SLVH, Single Leg Vertical Hop, PKF, Peak Knee Flexion, MD, Maximal Distance, MH, Maximal Height, Sym, Symmetry.
Figure 2.
Percentage of subjects who met the acceptable criteria per outcome variable for each group.
Abbreviations: IKDC, International Knee Documentation Committee Knee Form, Biomech, Biomechanical Function, Function, Functional Hop Performance, Comb, Combined.
Acceptable strength symmetry is ≥90%, acceptable biomechanical function is peak knee flexion symmetry ≥90% for all four hop tests, acceptable functional performance is hop distance/ height symmetry ≥90% for all four hop tests, acceptable IKDC scores are >85.
DISCUSSION
The purpose of this study was to examine quadriceps strength, sagittal plane knee kinematics, and functional performance after patients were cleared to return-to-activity post-ACLR. Patients 9- and 12-months post-ACLR were similar in terms of strength and function displaying the greatest asymmetries (strength > 20% asymmetry; average function asymmetry across hopping tasks 10%). Patients in the 18- and 24-month groups were also similar in terms of strength and function displaying smaller asymmetries than the 9- and 12-month groups (strength ~10% asymmetry; average function asymmetry across hopping tasks ~6%). Our results suggest that longer time periods post-ACLR may be beneficial to achieving symmetrical strength and function.
We found substantial quadriceps strength asymmetry (>20%) in subjects who were 9 and 12 months post-ACLR. The quadriceps strength deficits found in our study are similar to those found in prior research (11.1 – 27.1%) that examined ACLR patients at 12 months post-operative.7,16 Clinical recommendations for quadriceps strength is a level of asymmetry less than 10% (> 90% symmetry) since greater levels of asymmetry have been linked to a higher risk of secondary injury (injury to the ipsilateral or contralateral knee) following ACLR.9 Within the 9- and 12-month groups, only four subjects from each group (21.1% and 18.8% of subjects respectively) met the 90% strength symmetry criterion (table 2). Our data suggest that at 12 months post-operative, muscle strength for the majority of patients is not at acceptable levels and therefore return-to-activity is likely not safe. Our finding supports the recommendation that strength assessments be incorporated in ACLR return to activity criteria and considered more strongly than time from surgery when clearing an ACLR patient to resume activity.9 Further, it is clear a more concerted focus on regaining strength during rehabilitation, or new approaches to allow for better strength recovery after ACLR are necessary.
Subjects in the 18- and 24-month groups had quadriceps strength symmetry of 86.7% and 92.4%, respectively. Both the 18- and 24-month groups had higher levels of strength symmetry (~8% and 14% higher, respectively) when compared to the 9- and 12-month groups, with the difference in strength symmetry in the 24-month group achieving statistical significance. The amount of strength symmetry we found at 18- and 24-months post-operative is consistent with prior research,11,16,17,35,41 and suggests that strength improvements in ACLR patients continue to occur after completion of formal rehabilitation and return-to-activity. Despite the higher levels of strength in the 18 and 24 month groups, and the 24 month group mean higher than the clinically recommended criteria of 90% symmetry, it should be noted that individually a large percentage of patients in both groups did not meet the 90% symmetry level. In fact, 55% and 43% of subjects in the 18- and 24-month groups, respectively, were unable to meet the ≥90% symmetry criteria. Additionally, muscle strength recovery within each group was variable amongst the ACLR patients in our study, with some subjects (4 out of 19) achieving acceptable strength at 9 months post-operative, and yet a high percentage of patients failing to meet this criterion at 24 months post-operative. Variability in muscle strength after ACLR appears to be common (range of strength asymmetry at 6 months, 3% - 40%)19 and beyond.19,22,27 Lepley et al18 noted that subjects with less strength deficiency had participated in rehabilitation protocols that incorporated early post-operative cryotherapy, closed-chain exercise, range of motion restoration, in addition to exercises that focus on proprioception, agility, and balance. In our study, we did not control for patient rehabilitation facility, and as such cannot confirm consistency in the rehabilitation protocols performed by each subject. It’s likely that variance in quadriceps strength symmetry in ACLR patients within each group is due in part to variance in rehabilitation protocols (i.e. the inclusion/ exclusion of therapeutic exercise that addresses early recovery of range-of motion, strength, and neuromuscular control).
Functional symmetry (distance/ height) for the four hop tests were similar between the 9- and 12-month groups, with mean symmetry across the two groups ranging from 87.1% to 93.5%. Both groups, on average, achieved 90% symmetry for single leg hop and triple hop distance, with cross-over hop distance in the 12 month group also meeting the criterion. Despite these mean values achieving 90% symmetry, it is important to note that recommended functional performance symmetry, associated with reduced risk of secondary injury, is ≥90% for all tests included in a hop test battery.8,12,23 When we examined the hop test battery as a whole, there was no significant difference between the 9- and 12-month groups, with only 3 (15.8%) subjects in the 9-month group and 7 (31.8%) subjects in the 12-month group meeting the symmetry criteria for all four hop tests, and deemed as having acceptable functional performance (Figure 2).
Prior research by Grindem et al9 reported 55.0% patients at 12 months post-ACLR successfully completed the hop test battery. The difference in findings between studies for hop test battery success rate at 12 months post-operative may be due to differences in patient population, as Grindem included only those who had participated in high demand sport prior to injury and were expecting to return to the same level of sport following completion of rehabilitation. The activity level of the subjects in our study was quite diverse, ranging from normal daily activity to high-level sport and it would logically follow that those subjects participating in higher level of activity would present with better functional performance. We considered level of activity in our analyses and found a significant relationship between both subjective function and single leg hop performance with activity level. However, level of activity was not associated with functional performance on triple hop, cross-over hop, or single leg vertical hop, which are considered to be more difficult. Lastly, it should also be noted that instead of the 6-meter speed hop used by Grindem et al,9 we used the single-leg vertical hop, which had a lower success rate than the other three hop tests across all groups, and most likely reduced the overall success rate of the functional hop test battery (table 2). The single-leg vertical hop has been recommended for use in functional performance hop test batteries because of its value in discriminating between healthy vs ACL-injured limbs in previous literature.10 It has been proposed that vertical hop tests characterize a different aspect of functional performance than the hops for distance,10 and the disparity between the forward hop tests and vertical hop test in our study would support this conclusion.
The 18 and 24-month groups were significantly higher in hop distance symmetry, for 3 of the 4 hop tests, compared to the 9-month group. The patients 24 months post-ACLR were the only group to achieve mean functional performance values for all four hop tests that met acceptable levels of function, with symmetry values ranging from 90.7% to 97.1% across the four hop tests. These higher mean hop symmetry values indicate that improvements in functional performance do continue more than a year after completion of formal rehabilitation. It is also important to note that the rate of successful completion of all four hop tests was 27.1% higher in the 24 months group compared to the 9 months group, though this difference in success rate did not reach statistical significance. Despite the higher success rate for functional performance in the 24 month group, 57% of subjects were still unable to meet the 90% threshold for all four hop tests, further supporting the need for improved functional recovery in ACLR patients.
No significant differences in sagittal plane peak knee flexion angle were noted during the four hop tests between any of our four groups. Similar to functional hop testing, the range of mean knee flexion symmetry in the 9- and 12-month groups was close to or above 90%, with symmetry level ranging from 86.3% to 91%. However, if we apply the same criteria for successful achievement of functional hop performance to knee flexion angle symmetry, requiring ≥90% symmetry of knee flexion during all four hop tests, less than 10.5% and 27.3% of subjects met the recommended criteria in the 9- and 12-month groups respectively. The percentage of subjects who met the biomechanical criteria in the 18- and 24-month groups was 30% and 42.9%, which was not significantly higher than the earlier groups. The lack of significant difference between subjects in the early timepoints (9 and 12 month) and the later timepoints (18 and 24 month) is surprising since later groups had higher levels of functional performance symmetry, which has been related to knee joint kinematics previously.6 However, a study performed by Xergia et al43 examined single leg forward hop distance symmetry in male ACLR patients between six and nine months post-operative, and found moderate positive correlations between hop distance and isokinetic knee extension strength, but no correlation with knee flexion angle. Furthermore, a study by Trigsted et al38 found that although ACLR patients had symmetrical hop distances during functional testing, these same subjects still exhibited altered landing biomechanics, including asymmetrical peak knee flexion. Given our findings and the findings of previous research,3 it would seem that although knee flexion angle does play a role in functional hop performance, it is probably one of multiple variables, such as hip and ankle joint kinetics and kinematics,38 and non-biomechanical values such as balance and confidence.37
Patient perceived function was higher in the 12-, 18-, and 24-month groups (87.6%, 89.8%, 91.6%, respectively) when compared to the 9 month group (79.3%). Previous research has found that self-perceived function in ACLR patients improves over time.5,34 In a prior study performed in our lab we found improvements in IKDC from return to sport to after 12 months post-surgical.5 Additionally, prior research has also shown a relationship between patient reported function and both strength30 and functional hop testing.23 Given that we saw higher levels of strength and functional hop performance in the 18- and 24-month groups it is not surprising that patient perceived function was also higher.
LIMITATIONS
This study employed cross-sectional design to assess strength, biomechanical function, and functional performance in four separate groups of ACLR patients, at different times post-ACLR surgery. While this allows us to compare what different patients look like at different time point post-ACLR it would be valuable to make a longitudinal assessment of these variables over time to examine within-patient recovery. Also, the subjects in this study performed their post-ACLR rehabilitation at various physical therapy facilities. We recognize that rehabilitation protocols and procedures can vary between facilities, and that those variations can affect patient outcome and recovery.
CONCLUSION
Subjects in the 9- and 12-month groups differed in strength and functional performance when compared to the 18- and 24-month groups. While groups with more time had more strength and function, a number of patients continued to present with asymmetry at 2 years post-ACLR. These asymmetries could place patients at risk for future injury or osteoarthritis. We recommend that clinicians use objective criteria including, quadriceps strength, hop testing, and measures of patient-reported function to assess when patients may return to activity/sports.
What is known about this subject:
Quadriceps strength, patient perceived function, and functional performance are impaired at the time of return to sport/activity after ACLR.
What this study adds to existing knowledge:
This work begins to explore how strength and function recover over the 24 months after ACLR. No work to our knowledge has compared strength and function at various time points during the ACLR recovery process. Further, we explore the number of patients that are passing recommended clinical criteria during the 24 months after ACLR.
REFERENCES
- 1.Barber-Westin SD, Noyes FR. Factors used to determine return to unrestricted sports activities after anterior cruciate ligament reconstruction. Arthroscopy. 2011;27(12):1697–1705. [DOI] [PubMed] [Google Scholar]
- 2.Briggs KK, Lysholm J, Tegner Y, et al. The reliability, validity, and responsiveness of the Lysholm score and Tegner activity scale for anterior cruciate ligament injuries of the knee: 25 years later. Am J Sports Med. 2009;37(5):890–897. [DOI] [PubMed] [Google Scholar]
- 3.Burland JP, Lepley AS, DiStefano LJ, Lepley LK. No shortage of disagreement between biomechanical and clinical hop symmetry after anterior cruciate ligament reconstruction. Clin Biomech (Bristol, Avon). 2019;68:144–150. [DOI] [PubMed] [Google Scholar]
- 4.Chang EW, Johnson S, Pollard C, Hoffman M, Norcross M. Landing biomechanics in anterior cruciate ligament reconstructed females who pass or fail a functional test battery. Knee. 2018;25(6):1074–1082. [DOI] [PubMed] [Google Scholar]
- 5.Curran MT, Lepley LK, Palmieri-Smith RM. Continued Improvements in Quadriceps Strength and Biomechanical Symmetry of the Knee After Postoperative Anterior Cruciate Ligament Reconstruction Rehabilitation: Is It Time to Reconsider the 6-Month Return-to-Activity Criteria? J Athl Train. 2018;53(6):535–544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Di Stasi SL, Logerstedt D, Gardinier ES, Snyder-Mackler L. Gait patterns differ between ACL-reconstructed athletes who pass return-to-sport criteria and those who fail. Am J Sports Med. 2013;41(6):1310–1318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Feller JA, Webster KE. A randomized comparison of patellar tendon and hamstring tendon anterior cruciate ligament reconstruction. Am J Sports Med. 2003;31(4):564–573. [DOI] [PubMed] [Google Scholar]
- 8.Grindem H, Logerstedt D, Eitzen I, et al. Single-legged hop tests as predictors of self-reported knee function in nonoperatively treated individuals with anterior cruciate ligament injury. Am J Sports Med. 2011;39(11):2347–2354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Grindem H, Snyder-Mackler L, Moksnes H, Engebretsen L, Risberg MA. Simple decision rules can reduce reinjury risk by 84% after ACL reconstruction: the Delaware-Oslo ACL cohort study. Br J Sports Med. 2016;50(13):804–808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gustavsson A, Neeter C, Thomee P, et al. A test battery for evaluating hop performance in patients with an ACL injury and patients who have undergone ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2006;14(8):778–788. [DOI] [PubMed] [Google Scholar]
- 11.Hamada M, Shino K, Horibe S, et al. Single- versus bi-socket anterior cruciate ligament reconstruction using autogenous multiple-stranded hamstring tendons with endoButton femoral fixation: A prospective study. Arthroscopy. 2001;17(8):801–807. [DOI] [PubMed] [Google Scholar]
- 12.Hartigan EH, Axe MJ, Snyder-Mackler L. Time line for noncopers to pass return-to-sports criteria after anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 2010;40(3):141–154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hewett TE, Myer GD, Ford KR, et al. Biomechanical measures of neuromuscular control and valgus loading of the knee predict anterior cruciate ligament injury risk in female athletes: a prospective study. Am J Sports Med. 2005;33(4):492–501. [DOI] [PubMed] [Google Scholar]
- 14.Ithurburn MP, Paterno MV, Ford KR, Hewett TE, Schmitt LC. Young Athletes With Quadriceps Femoris Strength Asymmetry at Return to Sport After Anterior Cruciate Ligament Reconstruction Demonstrate Asymmetric Single-Leg Drop-Landing Mechanics. Am J Sports Med. 2015;43(11):2727–2737. [DOI] [PubMed] [Google Scholar]
- 15.Jordan MJ, Aagaard P, Herzog W. Rapid hamstrings/quadriceps strength in ACL-reconstructed elite Alpine ski racers. Med Sci Sports Exerc. 2015;47(1):109–119. [DOI] [PubMed] [Google Scholar]
- 16.Kobayashi A, Higuchi H, Terauchi M, et al. Muscle performance after anterior cruciate ligament reconstruction. Int Orthop. 2004;28(1):48–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lee S, Seong SC, Jo H, Park YK, Lee MC. Outcome of anterior cruciate ligament reconstruction using quadriceps tendon autograft. Arthroscopy. 2004;20(8):795–802. [DOI] [PubMed] [Google Scholar]
- 18.Lepley LK. Deficits in Quadriceps Strength and Patient-Oriented Outcomes at Return to Activity After ACL Reconstruction: A Review of the Current Literature. Sports Health. 2015;7(3):231–238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lepley LK, Palmieri-Smith RM. Quadriceps Strength, Muscle Activation Failure, and Patient-Reported Function at the Time of Return to Activity in Patients Following Anterior Cruciate Ligament Reconstruction: A Cross-sectional Study. J Orthop Sports Phys Ther. 2015;45(12):1017–1025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lepley LK, Wojtys EM, Palmieri-Smith RM. Combination of eccentric exercise and neuromuscular electrical stimulation to improve biomechanical limb symmetry after anterior cruciate ligament reconstruction. Clin Biomech (Bristol, Avon). 2015;30(7):738–747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lewek M, Rudolph K, Axe M, Snyder-Mackler L. The effect of insufficient quadriceps strength on gait after anterior cruciate ligament reconstruction. Clin Biomech (Bristol, Avon). 2002;17(1):56–63. [DOI] [PubMed] [Google Scholar]
- 22.Lisee C, Lepley AS, Birchmeier T, O’Hagan K, Kuenze C. Quadriceps Strength and Volitional Activation After Anterior Cruciate Ligament Reconstruction: A Systematic Review and Meta-analysis. Sports Health. 2019;11(2):163–179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Logerstedt D, Grindem H, Lynch A, et al. Single-legged hop tests as predictors of self-reported knee function after anterior cruciate ligament reconstruction: the Delaware-Oslo ACL cohort study. Am J Sports Med. 2012;40(10):2348–2356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Noyes FR, Barber SD, Mangine RE. Abnormal lower limb symmetry determined by function hop tests after anterior cruciate ligament rupture. Am J Sports Med. 1991;19(5):513–518. [DOI] [PubMed] [Google Scholar]
- 25.Oberlander KD, Bruggemann GP, Hoher J, Karamanidis K. Altered landing mechanics in ACL-reconstructed patients. Med Sci Sports Exerc. 2013;45(3):506–513. [DOI] [PubMed] [Google Scholar]
- 26.Palmieri-Smith RM, Lepley LK. Quadriceps Strength Asymmetry After Anterior Cruciate Ligament Reconstruction Alters Knee Joint Biomechanics and Functional Performance at Time of Return to Activity. Am J Sports Med. 2015;43(7):1662–1669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Palmieri-Smith RM, Thomas AC, Wojtys EM. Maximizing quadriceps strength after ACL reconstruction. Clin Sports Med. 2008;27(3):405–424, vii-ix. [DOI] [PubMed] [Google Scholar]
- 28.Paterno MV, Rauh MJ, Schmitt LC, Ford KR, Hewett TE. Incidence of contralateral and ipsilateral anterior cruciate ligament (ACL) injury after primary ACL reconstruction and return to sport. Clin J Sport Med. 2012;22(2):116–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Paterno MV, Schmitt LC, Ford KR, et al. Biomechanical measures during landing and postural stability predict second anterior cruciate ligament injury after anterior cruciate ligament reconstruction and return to sport. Am J Sports Med. 2010;38(10):1968–1978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Pietrosimone B, Blackburn JT, Harkey MS, et al. Greater Mechanical Loading During Walking Is Associated With Less Collagen Turnover in Individuals With Anterior Cruciate Ligament Reconstruction. Am J Sports Med. 2016;44(2):425–432. [DOI] [PubMed] [Google Scholar]
- 31.Sanders TL, Maradit Kremers H, Bryan AJ, et al. Incidence of anterior cruciate ligament tears and reconstruction: a 21-year population-based study. The American journal of sports medicine. 2016;44(6):1502–1507. [DOI] [PubMed] [Google Scholar]
- 32.Schmitt LC, Paterno MV, Ford KR, Myer GD, Hewett TE. Strength Asymmetry and Landing Mechanics at Return to Sport after Anterior Cruciate Ligament Reconstruction. Med Sci Sports Exerc. 2015;47(7):1426–1434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Schmitt LC, Paterno MV, Hewett TE. The impact of quadriceps femoris strength asymmetry on functional performance at return to sport following anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 2012;42(9):750–759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Spindler KP, Huston LJ, Wright RW, et al. The prognosis and predictors of sports function and activity at minimum 6 years after anterior cruciate ligament reconstruction: a population cohort study. Am J Sports Med. 2011;39(2):348–359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Tashiro T, Kurosawa H, Kawakami A, Hikita A, Fukui N. Influence of medial hamstring tendon harvest on knee flexor strength after anterior cruciate ligament reconstruction. A detailed evaluation with comparison of single- and double-tendon harvest. Am J Sports Med. 2003;31(4):522–529. [DOI] [PubMed] [Google Scholar]
- 36.Thomas AC, Wojtys EM, Brandon C, Palmieri-Smith RM. Muscle atrophy contributes to quadriceps weakness after anterior cruciate ligament reconstruction. J Sci Med Sport. 2016;19(1):7–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Thomee R, Kaplan Y, Kvist J, et al. Muscle strength and hop performance criteria prior to return to sports after ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2011;19(11):1798–1805. [DOI] [PubMed] [Google Scholar]
- 38.Trigsted SM, Post EG, Bell DR. Landing mechanics during single hop for distance in females following anterior cruciate ligament reconstruction compared to healthy controls. Knee Surg Sports Traumatol Arthrosc. 2017;25(5):1395–1402. [DOI] [PubMed] [Google Scholar]
- 39.van Meer BL, Meuffels DE, Vissers MM, et al. Knee injury and Osteoarthritis Outcome Score or International Knee Documentation Committee Subjective Knee Form: which questionnaire is most useful to monitor patients with an anterior cruciate ligament rupture in the short term? Arthroscopy. 2013;29(4):701–715. [DOI] [PubMed] [Google Scholar]
- 40.Ward SH, Blackburn JT, Padua DA, et al. Quadriceps Neuromuscular Function and Jump-Landing Sagittal-Plane Knee Biomechanics After Anterior Cruciate Ligament Reconstruction. J Athl Train. 2018;53(2):135–143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wojtys EM, Huston LJ. Longitudinal effects of anterior cruciate ligament injury and patellar tendon autograft reconstruction on neuromuscular performance. Am J Sports Med. 2000;28(3):336–344. [DOI] [PubMed] [Google Scholar]
- 42.Wright RW, Dunn WR, Amendola A, et al. Risk of tearing the intact anterior cruciate ligament in the contralateral knee and rupturing the anterior cruciate ligament graft during the first 2 years after anterior cruciate ligament reconstruction: a prospective MOON cohort study. Am J Sports Med. 2007;35(7):1131–1134. [DOI] [PubMed] [Google Scholar]
- 43.Xergia SA, Pappas E, Georgoulis AD. Association of the Single-Limb Hop Test With Isokinetic, Kinematic, and Kinetic Asymmetries in Patients After Anterior Cruciate Ligament Reconstruction. Sports Health. 2015;7(3):217–223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Zwolski C, Schmitt LC, Thomas S, Hewett TE, Paterno MV. The Utility of Limb Symmetry Indices in Return-to-Sport Assessment in Patients With Bilateral Anterior Cruciate Ligament Reconstruction. Am J Sports Med. 2016;44(8):2030–2038. [DOI] [PubMed] [Google Scholar]