Abstract
The COVID-19 pandemic required the rapid conversion of medical school curricula to virtual instruction. Prior to the crisis, histopathology teaching laboratories at UT Health San Antonio included completion of an Individual Laboratory Quiz before the laboratory session, a Team Application Exercise released and completed during the laboratory session with guidance from faculty, and a graded Team Laboratory Quiz at the end of the laboratory session. Adaptation of this interactive, in-person activity to a fully online platform included releasing the Team Application Exercise earlier to provide ample time for students to work virtually with their teams, conducting laboratory sessions using Microsoft Teams, with 5 to 6 teams led by a single instructor, and requiring the Team Laboratory Quiz to be taken individually for ensuring quiz security and test integrity. For incentivizing collaboration while completing the Team Application Exercise, the final score was either the student’s individual score on the Team Laboratory Quiz or their team’s average, whichever was higher. Comparison of student scores on the modified Team Laboratory Quiz to Team Laboratory Quiz scores using the earlier laboratory format prior to COVID-19 showed a significant decline; however, scores on other weekly quizzes or examinations were unaffected. Students welcomed the early release of Team Application Exercise and easier access to faculty but indicated that the modified Team Laboratory Quiz decreased peer-teaching and learning experience and increased anxiety. Faculty indicated the loss of personal interaction with students as a major theme. These data suggest that novel pedagogical approaches are required for online histopathology instruction to accommodate differences in learning styles while maintaining the benefits of team collaboration.
Keywords: histology, pathology, virtual microscopy, COVID-19, Team-Based Learning, medical education, online, remote teaching, pandemic
Introduction
The ongoing coronavirus disease 2019 (COVID-19) pandemic caused by the severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) has enforced a rapid transition of in-person lectures and team-based small-group activities in the preclinical curriculum in medical schools to remote, online platforms1 such as Zoom (Zoom Video Communications, Inc., San Jose, CA), Microsoft Teams (Microsoft, Redmond, WA), GotoMeeting (LogMeIn, Boston, MA) and others. While electronic learning (E-learning) is not new2 and has been successfully used in the preclinical curriculum3 in the form of recorded lectures and other asynchronous supporting content, the scale of e-learning content development and implementation required to meet the World Health Organization (WHO) and Association of American Medical Colleges (AAMC) COVID-19 guidelines was unprecedented. In line with WHO and AAMC guidelines, histopathology (HP) teaching laboratories at UT Health San Antonio (UTHSA) were also transitioned to fully online, remote exercises.
UT Health San Antonio follows an integrated preclinical curriculum (Figure 1A) in which the disciplines of histology and pathology have been combined. Histopathology laboratories are considered to be a key component of the basic science curriculum as they interface closely with each of the organ-based modules. Not surprisingly, the HP laboratories have evolved continuously4 and were recently redesigned in 2017 for first-year medical students (MS1) and in 2018 for second-year medical students (MS2) as a modified Team-Based Learning (TBL) format that is three pronged (Figure 1B).
Figure 1.

Preclinical curriculum and histopathology laboratory format. A. The preclinical curriculum at UT-Health San Antonio is divided into multiple modules. Students begin with the Molecules to Medicine (M2M) module that runs concurrently with the Language of Medicine module and Clinical Skills. The final preclinical module is the Musculoskeletal and Dermatopathology module. Histopathology teaching laboratories form an integral part of all modules, with the exception of Medicine, Behavior and Society, and Mind, Brain and Behavior module (MBB) modules. B. The currently used histopathology laboratory format was established in 2017 for MS1 students and in 2018 for MS2 students. It consists of an iLab portion that students complete prior to the laboratory session, a TAE portion that students complete during the laboratory session and a graded tLab portion that students complete at the end of the laboratory session, after uploading their TAE. Only the tLab is graded; however, obtaining a score less than 90% on the iLab will result in a 50% deduction in final grade of the laboratory. The TAE is checked for completion and answers to the TAE are posted after the laboratory session. COVID-19 necessitated the adaptation to fully online laboratories. Changes included release of the TAE prior to the laboratory session, individual completion of the tLab rather than as a team, and completion of the laboratory session (Continued) using Microsoft Teams, with 5 to 6 teams led by a faculty instructor. The final score received by a student was either his/her score on the tLab or his/her team’s average, whichever was higher. COVID-19 indicates coronavirus disease 2019; iLab, Individual Laboratory Quiz; tLab, Team Laboratory Quiz; TAE, Team Application Exercise.
Prior to the laboratory session, students complete an Individual Laboratory Quiz (iLab), that is, released 5 to 6 days before the day of the laboratory. The iLab consists of a set of 20 questions in CANVAS (CANVAS, Salt Lake City, Utah) that encompasses various image and text-based question types formatted as multiple drop-down, multiple-choice, match the following, and essay. The iLab queries content covered in module-specific lectures, clinical skills lectures, faculty-provided SoftChalk (SoftChalk LLC., Richmond, Va) summaries, and assigned readings in textbooks. The iLab is open book and allows a student to refer to the required textbooks, provided course materials, and the internet and is completed individually. Most importantly, concise and immediate feedback in the form of scores acquired on the quiz, missed questions, as well as detailed notes describing the basis of the correct response and the inaccuracies of the other choices is provided. The iLab is mandatory and is required to be submitted by each student before the beginning of the laboratory session. Students can attempt the iLab multiple times and need to score at least 90%. Overall, the iLab is considered to be a formative exercise that promotes self-directed and independent learning and provides a flipped classroom approach to the HP laboratory.
During the 2-hour laboratory session, students begin by downloading a Team Application Exercise (TAE) template from Canvas that needs to be completed and uploaded back onto Canvas within 80 minutes. The TAE is a Microsoft PowerPoint–based portfolio consisting of 5 to 6 clinical case–based scenarios relevant to the week’s theme and is designed to help students assimilate basic science knowledge in a clinical context. Completion of the TAE requires the students to capture appropriate images using the provided virtual microscopy specimens, annotate those images, and paste them into the portfolios.4 The TAE also includes provided images the students are required to label as well as prelabeled images (“Your Are The Teacher”) that students correct as needed. Text-based questions pertinent to the clinical case are also included to further integrate the HP teaching materials with the other disciplines taught at week in the module. Students work with their assigned teams of 5 to 7 members to complete, review, and submit the TAE; the entire class of approximately 220 students is divided into 35 to 37 teams to promote active learning in a large laboratory setting. Teams can request help from the faculty to guide them while submitting their responses; faculty typically use the Socratic method of teaching5 by asking questions rather than revealing answers. While the Team Application is not graded, it is marked as Complete/Incomplete. The correct answers are posted onto Canvas immediately following the laboratory session for self-assessment. The TAE component has been assessed previously and was well-liked by students.4
The final component of the session is the Team Laboratory Quiz (tLab), a graded, closed-book quiz taken by each team at the end of the laboratory. The tLab consists of a set of 10 text or image-based questions in Canvas to be completed in 20 minutes. The tLab incorporates all the different question formats used in the iLab and includes content covered in the iLab, TAE, and relevant lectures and summaries designed in SoftChalk. As a team activity, students discuss each question within their teams and one designated student from the team submits the completed tLab quiz. All members of a team are accorded the same points. Students see their tLab scores immediately after submitting the quiz; questions missed or answered incorrectly are marked. In contrast to the iLab, feedback for each question is not provided as this is considered to be an assessment quiz. The tLab is taken using the LockDown Browser (Respondus) on Canvas and requires that all other applications are closed.
Transition to a completely online format necessitated selected changes in the laboratory format. All laboratories were conducted remotely but synchronously, using Microsoft Teams, with 5 to 6 teams led by a single instructor. Each team was assigned a virtual room for discussion of the TAE and each faculty instructor was assigned a room as well to answer questions during the laboratory session. Students were expected to continue work in their teams on the TAE template and move to the faculty room with questions or for additional discussion. Faculty instructors were rotated such that each set of teams would be led by a different instructor in each laboratory. However, MS Teams does not have “breakout rooms” as does Zoom, and hence, students assigned to a particular room can move to other faculty rooms, although this was discouraged.
While no changes were made to the iLab content, release, and due dates, the TAE was released at the same time as the iLab (5-6 days before the laboratory session) to provide sufficient time and opportunity for students to interact and discuss the TAE with their teams. For maintaining tLab quiz security and test integrity, both LockDown Browser and Respondus Monitor were used, given the remote nature of testing. Moreover, the tLab was required to be taken individually for assessment of laboratory grades. However, to reduce anxiety and to maintain peer-to-peer collaboration while completing the TAE, the final score for each student was either their individual score on the tLab or their team’s average, whichever was higher. Importantly, there were no significant changes in laboratory content or tLab quizzes compared to previous years. This study presents the results of outcomes assessments of the transition from in-person MS1 and MS2 HP teaching laboratories to an online format as well as student and faculty perceptions.
Methods
Ethical Considerations
This study was approved by internal review board of UTHSA (Protocol Number: HSC20200825E) and determined as exempt based on U.S. Department of Health and Human Services Regulation 45 CFR.
Evaluation of Student Performance
Grades of all MS1 students who took the Molecules to Medicine (M2M) module in the Fall semester of 2017, 2018, 2019, and 2020 as well as grades of all MS2 students who took the Endocrine and Female Reproductive (EFR) module in the Fall semester of 2018, 2019, and 2020 were obtained, de-identified, and used for further analysis. Specifically, individual tLab scores and team averages of each of the 4 HP laboratories in M2M and EFR, scores received in the individual portion of 5 weekly quizzes of M2M and 6 weekly quizzes of EFR, and scores obtained in the midterm and final examinations of M2M and the final examination of EFR were collected for analysis. Endocrine and Female Reproductive does not have a midterm examination.
As M2M and EFR tLabs were taken individually in response to COVID-19, the final score received by the student was either their individual score or the team average score, whichever was higher. Therefore, for HP laboratories in M2M and EFR in Fall 2020, 2 sets of scores were obtained for each student—the individual score (designated 2020) and the final adjusted score (designated 2020a). Both scores were used for further analysis.
Averages of individual tLab scores, team averages of tLab scores, weekly quizzes, midterm examinations, and final examinations were compared across the pre-COVID-19 years (2017, 2018, and 2019) and the COVID-19 year (2020) when all HP laboratories and weekly quizzes were taken virtually. Additionally, individual and team tLab scores in each laboratory were grouped into 4 categories to observe trends: those who received a perfect score of 10.00, those who received a score between 9.00 and 9.99, those who received a score between 8.00 to 8.99, and those received a score below 8.00. Similarly, midterm and final examination scores were also grouped into 4 categories: those who received a perfect score of 100.00, those who received a score between 90.00 and 90.99, those who received a score between 80.00 and 89.99, and those received a score below 80.00.
To avoid confounding data, students who reportedly could not complete their tLab due to poor internet connectivity or missed any of their tLab due to excused absences and therefore, received their team average scores, were excluded. Typically, no more than 2 to 3 students received excused absences for a given laboratory session. Additionally, those students who missed their midterm or final examinations were also excluded from the study. Scores of 212 MS1 students in 2017, 210 students in 2018, 218 students in 2019, and 215 students in 2020 in the M2M module were analyzed; similarly, scores of 221 MS2 students in 2018, 211 students in 2019, and 207 students in 2020 were analyzed. MS1 students were divided into 37 teams of 5 to 6 students per team for all HP laboratories in M2M; similarly, MS2 students were divided into 37 teams for all HP laboratories in EFR except in 2019, where students were divided into 35 teams.
Surveys
Both MS1 and MS2 students were requested to complete surveys after the completion of their respective modules. Similarly, faculty instructors for HP laboratories were also sent surveys; 3 faculty instructors involved in authoring this paper were excluded. Surveys were administered using Qualtrics (Qualtrics LLC); anonymous links to separate surveys were sent via a single email to students and faculty. Participation in the surveys was optional for both students and faculty and not linked to regular student evaluations. A total of 126 MS1 and MS2 students (out of 440; 28.64%) and 5 faculty (out of 11 invitations; 45.45%) completed the surveys. Both surveys were based on a 5-point Likert scale (1 = strongly disagree, 2 = somewhat disagree, 3 = neither agree nor disagree, 4 = somewhat agree, and 5 = strongly agree). Internal consistency of surveys was analyzed by determining Cronbach α using NCSS 2020 Statistical Software (NCSS, LLC). Cronbach α for student surveys was 0.8 and Cronbach α for faculty surveys was 0.92, indicating high reliability.
Thematic analysis of responses to open-ended questions on both student and faculty surveys was performed by 2 independent researchers, using an inductive (open coding) approach. Comments were first sorted and categorized (coded) and codes were agreed upon by the researchers by discussion. For comments that were multifactorial and could be categorized into multiple codes, the comment was copied into all of its relevant categories. Codes were then condensed for the identification of themes and subthemes, followed by interpretation.
Statistical Analysis
Statistical analyses were performed using GraphPad Prism, version 6.0 (GraphPad Software). Shapiro-Wilk normality test indicated that data were not normally distributed (P < .0001). Therefore, nonparametric, 1-way ANOVA (Kruskal-Wallis test) followed by Dunn multiple comparisons test was used to analyze data.
Results
Student Performance on Team Laboratory Quiz Decreased Significantly in Online Histopathology Laboratories
To determine the impact of virtual HP teaching laboratories on student learning, scores on tLab in the M2M module in 2020 was compared to tLab scores from 2017 onward for MS1 students (Figure 2A) and scores on tLab in the EFR module in 2020 was compared to tLab scores from 2018 onward for MS2 students (Figure 2B).
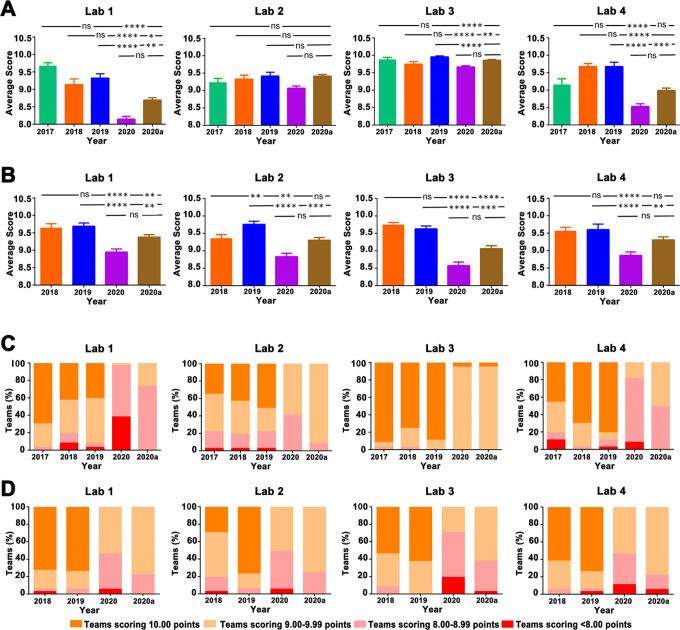
Figure 2.
Student performance in tLab, taken as a team during the years 2017 to 2019 and individually in the year 2020. Scores in 2020 were adjusted such that students received their team’s average score if their individual score was lower than the team average; the final scores that include the adjusted scores is shown as 2020a. A, Average MS1 student scores in tLab in each of the four histopathology laboratories of M2M module. B, Average MS2 student scores in tLab in each of the 4 histopathology laboratories of EFR module. C, Student scores in tLab of each laboratory in MS1 M2M module were grouped as those who received a perfect score of 10.00, those who received a score between 9.00 and 9.99, those who received a score between 8.00 and 8.99, and those who received a score below 8.00. Each stacked bar indicates the percentage of students in each group. D, Student scores in tLab of each laboratory in MS2 EFR module were grouped as those who received a perfect score of 10.00, those who received a score between 9.00 and 9.99, those who received a score between 8.00 and 8.99, and those who received a score below 8.00. Each stacked bar indicates the percentage of students in each group. Scores obtained on each laboratory were compared using Kruskal-Wallis test followed by a Dunn’s multiple comparisons test. ****P ≤ .0001; ***P ≤ .001; **P ≤ .01; *P ≤ .05; ns—P > .05. EFR indicates Endocrine and Female Reproductive; tLab, indicates Team Laboratory Quiz.
The average MS1 student tLab scores in the first HP laboratory in 2020 decreased significantly by 15.6% from 2017, 10.3% from 2018, and 11.6% from 2019 (P < .0001 in all cases). Average scores in laboratories 2 and 3 in 2020 were higher as compared to laboratory 1, with just 1.5% (no significant difference), 6.8% (P < .0001), and 3.6% (P = .0004) decrease in laboratory 2 as compared to 2017, 2018, and 2019, respectively, and 2.2%, −3.6%, and 2.5% (P < .0001 in all cases) in tLab 2020 as compared to 2017, 2018, and 2019, respectively. However, tLab scores significantly decreased again in laboratory 4 by 6.7% (P = .0016), 11.5% (P < .0001), and 11.2% (P < .0001) as compared to scores in 2017, 2018, and 2019, respectively. Overall, there was a significant difference among the groups in each the 4 laboratories in the M2M modules across the years (P < .0001).
Scores in 2020 were adjusted such that students received their team’s average score if their individual score was lower than the team average. In spite of the increased average scores of some students due to the adjustment, the overall pattern of low scores in 2020 remained unaffected. Only the tLab scores in laboratory 2 increased significantly after adjustments (P = .0127).
Similarly, the average tLab scores of MS2 students in the EFR module, who had earlier followed the pre-COVID format of HP laboratories in their first (MS1) year, also decreased in 2020 (P < .0001). Specifically, average scores on the tLab in the first HP laboratory in 2020 decreased by 7.0% and 7.4% as compared to tLab scores in 2018 and 2019 (P < .0001 in all cases). The average tLab scores in laboratory 2 decreased by 5.2% (P = .2836) and 9.1% (P < .0001) in 2020 as compared to tLab scores in 2018 and 2019. Laboratories 3 and 4 also showed significant decreases in tLab scores in 2020 as compared to tLab scores in 2018 and 2019 by 11.7% and 11.0% (P < .0001 in both cases), respectively, and by 7.3% and 8.8% (P < .0001 in both cases) as compared to tLab scores in 2018 and 2019.
To determine whether the distribution of scores was significantly altered in 2020, tLab scores of each laboratory were grouped as those who received a perfect score of 10.00, those who received a score between 9.00 and 9.99, those who received a score between 8.00 and 8.99, and those who received a score below 8.00 for both the M2M (Figure 2C) and EFR (Figure 2D) modules.
Clearly, the number of students receiving a score of 10.00 decreased in all laboratories in the M2M module, with the exception of laboratory 3 where fewer students in 2018 received tLab scores of 10.00. The number of students receiving tLab scores between 8.00 and 8.99 or below 8.00 increased in 2020 across all laboratories, again with the exception of laboratory 3 where more students in 2018 received poor scores. The adjustments to the scores in 2020 impacted those students who scored less than 8.00 or between 8.00 and 8.99.
The distribution of tLab scores in the EFR module appeared to mirror the distribution in the M2M module, with fewer students receiving a 10.00 score in 2020 and more students receiving scores between 8.00 and 8.99 or below 8.00 in 2020 as compared to previous years. Laboratory 2 of 2018 was an exception as it had fewer students receiving a 10.00 score as compared to 2020.
Taken together, these data indicate that the average tLab scores decreased in 2020, with fewer students scoring a perfect score of 10.00.
Team Performance on tLab Decreased Significantly in the Online Histopathology Laboratories
Students are organized as teams for all HP laboratories, with each team consisting of 5 to 7 members and 35 to 37 teams overall. Students learn from each other while completing the TAE and, in the pre-COVID years, also took the tLab collectively, with one team member submitting the tLab quiz. To determine the impact of virtual HP teaching laboratories on team performance, MS1 team average scores on tLab in the M2M module in 2020 was compared to earlier years (Figure 3A). Similarly, MS2 team average scores on tLab in the EFR module in 2020 was compared to tLab scores in 2018 and 2019 (Figure 3B).
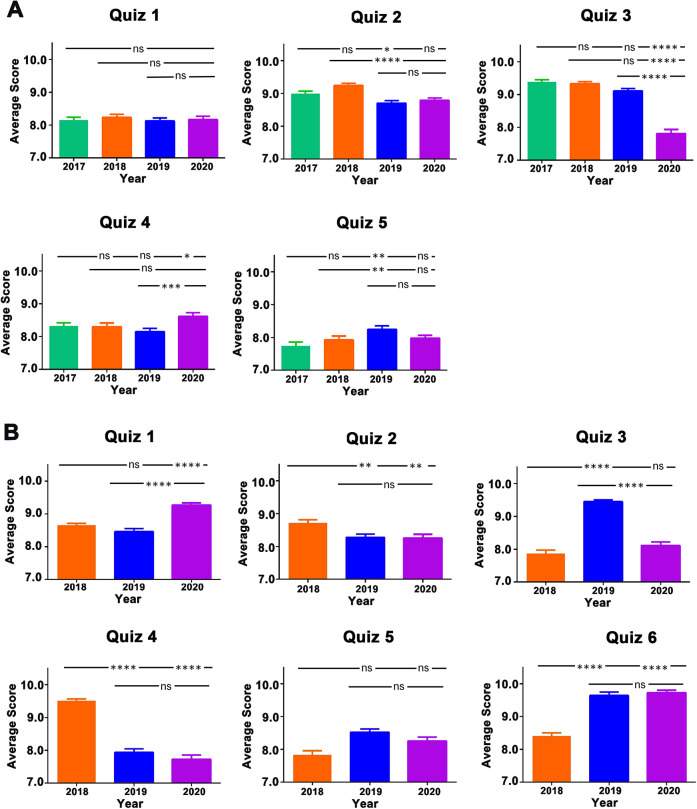
Figure 3.
Team performance in quizzes, taken as a team during the years 2017 to 2019 and individually in the year 2020. Scores in 2020 were adjusted such that students received their team’s average score if their individual score was lower than the team average; the final team scores that include the adjusted scores is shown as 2020a. A, Average MS1 team scores in tLab in each of the 4 histopathology laboratories of M2M module. B, Average MS2 team scores in tLab in each of the 4 histopathology laboratories of EFR module. C, Team scores in tLab of each laboratory in MS1 M2M module were grouped into those teams who received a perfect score of 10.00, those teams who received a score between 9.00 and 9.99, those teams who received a score between 8.00 and 8.99, and those teams who received a score below 8.00. Each stacked bar indicates the percentage of teams in each group. D, Team scores in tLab of each laboratory in MS2 EFR module were grouped as those who received a perfect score of 10.00, those who received a score between 9.00 and 9.99, those who received a score between 8.00 and 8.99, and those who received a score below 8.00. Each stacked bar indicates the percentage of students in each group. Team average scores obtained on each laboratory were compared using Kruskal-Wallis test followed by a Dunn’s multiple comparisons test. ****P ≤ .0001; ***P ≤ .001; **P ≤ .01; *P ≤ .05; ns—P > .05. EFR indicates Endocrine and Female Reproductive; tLab, Team Laboratory Quiz.
The tLab team average scores in the first M2M HP laboratory in 2020 decreased significantly by 15.8% from 2017, 10.8% from 2018, and 12.6% from 2019 (P < .0001 in all cases). Average score in laboratory 2 in 2020 was higher as compared to laboratory 1, with decrease by only 1.9%, 2.8%, and 3.7% in laboratory 2 as compared to 2017, 2018, and 2019, respectively (no significant difference). Laboratory 3 showed a decline in average score by 2.2%, 0.8%, and 2.9% in 2020 as compared to 2017, 2018, and 2019, respectively (P < .0001 in all cases). tLab scores significantly decreased again in laboratory 4 by 6.9% (P = .0001), 11.8% (P = .0001), and 11.8% (P < .0001) as compared to scores in 2017, 2018, and 2019, respectively. Overall, a significant difference in team averages was noted across the years in each of the 4 M2M laboratories (P < .0001), including laboratory 2 (P = .0266). Although some students in a team received their team average scores due to the adjustment, overall team average scores of each laboratory after adjustments did not increase significantly as compared to the original score.
Similarly, the team average scores of MS2 students in the EFR module also decreased in 2020 in all 4 HP laboratories as compared to team average scores in 2018 and 2019 (P < .0001 in all cases). Specifically, average scores on the tLab in the first HP laboratory in 2020 decreased by 7.3% and 7.6% as compared to tLab scores in 2018 and 2019 (P < .0001 in all cases). The average tLab scores in laboratory 2 decreased by 5.7% and 9.5% in 2020 as compared to tLab scores in 2018 and 2019 (P = .0021 and P < .0001, respectively). Laboratories 3 and 4 also showed significant decreases in team average scores in 2020 as compared to team average scores in 2018 and 2019 by 12.0% and 10.9% (P < .0001 in both cases) and by 7.4% and 7.7% (P < .0001 in both cases).
To determine whether the distribution of scores was significantly altered in 2020, tLab scores of each laboratory were grouped into teams that received a perfect score of 10.00, between 9.00 and 9.99, between 8.00 and 8.99, and those that received a score below 8.00 for both the M2M (Figure 3C) and EFR (Figure 3D) modules. Interestingly, none of the teams received a score of 10.00 in M2M laboratories 1, 2, and 4, with the exception of laboratory 3 where only 2 teams received a score of 10.00. The adjustments to the scores in 2020 impacted those teams who averaged less than 8.00 or between 8.00 and 8.99.
The distribution of tLab scores in the EFR module appeared to mirror the distribution in the M2M module, with no team receiving a 10.00 score in 2020 and more students receiving scores between 8.00 and 8.99 or below 8.00 in 2020 as compared to previous years. Taken together, these data indicate that the team average scores significantly decreased in 2020.
Student Performances on Weekly Quizzes Were Mostly Unaltered or Performed Better With Remote Teaching
Both MS1 and MS2 students take weekly quizzes on Mondays that are based on content covered in the previous week. Importantly, each HP laboratory session is associated with a weekly quiz, taken 2 to 3 days prior to the laboratory. Specifically, the 4 M2M tLab quizzes were taken in the same week as weekly quizzes 1, 3, 4, and 5. Similarly, the 4 EFR tLab quizzes were taken in the same week as weekly quizzes 1, 2, 3, and 4. Therefore, student performance on the weekly quizzes was analyzed to determine whether remote teaching due to COVID-19 resulted in decreased weekly quiz scores, similar to that observed in tLab. Importantly, there were no significant changes in questions on the weekly quizzes from the previous years. As shown in Figure 4A, student performance in M2M weekly quiz 1 in 2020 was similar (P = .7576) across the years 2017 (−0.2%), 2018 (0.8%), and 2019 (−0.5%), in contrast to performance in the first HP tLab. Weekly quiz 3 in 2020 showed a significant decrease (P < .0001) as compared to 2017 (16.7%), 2018 (16.3%), and 2019 (14.2%), while there was a significant increase in scores in weekly quiz 4 in 2020 (P = .0004) as compared to 2017 (3.5%, P = .0335) and 2019 (5.7%; P = .0002). Performance in weekly quiz 5 was not statistically significant from any other year.
Figure 4.
Student performance in the individual portion of the weekly quizzes of the module. Weekly quizzes, based on content covered in the previous week, were always taken 2 to 3 days prior to each histopathology laboratory session. Student performance on weekly quizzes were analyzed to determine whether remote teaching due to COVID-19 resulted in decreased scores, similar to that observed in tLab. A, Average MS1 student scores in each of the 5 weekly quizzes in M2M module during the years 2017 to 2020. B, Average MS2 student scores in each of the 6 weekly quizzes in EFR module during the years 2018 to 2020. Average scores on each quiz were compared using Kruskal-Wallis test followed by a Dunn’s multiple comparisons test. ****P ≤ .0001; ***P ≤ .001; **P ≤ .01; *P ≤ .05; ns—P > .05. COVID-19 indicates coronavirus disease 2019; EFR, Endocrine and Female Reproductive; tLab, Team Laboratory Quiz.
Figure 4B shows performance of MS2 students in the EFR module weekly quizzes. Scores on weekly quiz 1 in 2020 increased by 7.1% and 9.6% as compared to those in 2018 and 2019 (P < .0001 for both years). Weekly quiz 2 scores were not significantly different from scores in 2019 (P > .999) but decreased as compared to scores in 2017 by 5.0% (P = .0096). Scores of weekly quiz 3 in 2020 decreased significantly by 14.2% as compared to 2019 (P < .0001) but was not significantly different from the scores in 2017 (increased by 3.1%; P = .1799). Weekly quiz 4 scores in 2020 decreased by 18.7% (P < .0001) as compared to those in 2018 but was not significantly different from the 2019 score (2.7% decrease, P > .999). The weekly quiz 5 scores were not statistically significant across all the years (P = .1421). These data suggest that while student scores decreased in HP laboratories, their performance in weekly quizzes were, for the most part, similar to prior year performances.
Students Performed Better in Module Examinations in 2020 Than in the Previous Years
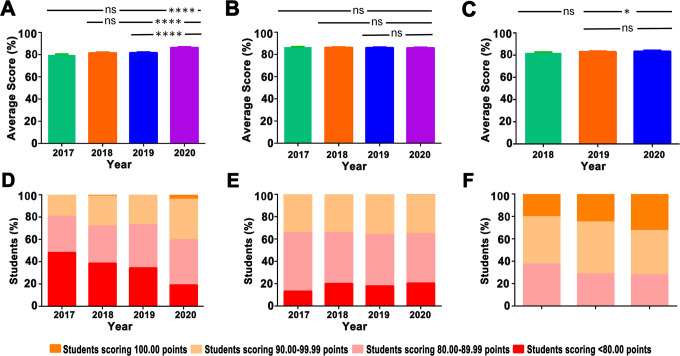
Since tLab scores decreased significantly in 2020, midterm and final examination scores in M2M module were analyzed (Figure 5). Student scores in midterm examinations in 2020 increased by 8.3% as compared to 2017 scores, 6.0% as compared to 2018 scores, and 5.7% as compared to 2019 scores (P < .0001 across all years). While 1, 3, and 1 students scored 100.00 points in 2017, 2018, and 2019, respectively, 9 students scored 100.00 points in 2020; additionally, fewer students scored below 80.00 points in 2020. Performance in final examinations in M2M module was not significantly different; the distribution of scores also paralleled scores in earlier years.
Figure 5.
Student performance in module examinations. Scores on midterm and final examinations were analyzed to determine whether fully online teaching due to COVID-19 resulted in decreased scores, similar to that observed in tLab. A, Average MS1 student scores in midterm examinations in M2M module during the years 2017 to 2020. B, Average MS1 student scores in final examinations in M2M module during the years 2017 to 2020. C, Average MS2 student scores in final examinations in EFR module during the years 2018 to 2020. D, MS1 student scores on the midterm examinations of each year in M2M module were grouped as those who received a perfect score of 100.00, those who received a score between 90.00 and 90.99, those who received a score between 80.00 and 89.99, and those who received a score below 80.00. Each stacked bar indicates the percentage of students in each group. E, MS1 student scores on the final examinations of each year in M2M module were grouped as those who received a perfect score of 100.00, those who received a score between 90.00 and 90.99, those who received a score between 80.00 and 89.99, and those who received a score below 80.00. Each stacked bar indicates the percentage of students in each group. F, MS2 student scores on the final examinations of each year in EFR module were grouped as those who received a perfect score of 100.00, those who received a score between 90.00 and 90.99, those who received a score between 80.00 and 89.99, and those who received a score below 80.00. Each stacked bar indicates the percentage of students in each group. Average scores on each examination were compared using Kruskal-Wallis test followed by a Dunn multiple comparisons test. ****P ≤ .0001; *P ≤ .05; ns—P > .05. COVID-19 indicates coronavirus disease 2019; EFR, Endocrine and Female Reproductive; tLab, Team Laboratory Quiz.
Similarly, student performance in the final examination in the EFR module also increased by 1.8% in 2020 as compared to scores in 2018 (P = .0242) and by 0.7% from 2019 (P = .0450). Interestingly, 33% students scored between 90 and 99 in 2020 as compared to 20% in 2017 and 25% in 2018, again suggesting improved performance in the final examination. Together, these data suggest that performance in online HP laboratories did not appear to affect performance in midterm or final examinations.
Students Liked the Early Release of the Team Application Exercise but Preferred to Take the Team Laboratory Quiz in Teams
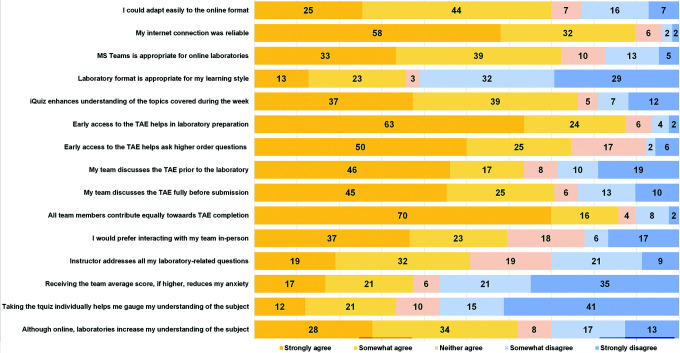
Student opinions of the online HP laboratories and the modified format were evaluated via surveys measured on a 5-point Likert scale (Figure 6) that also included 2 open-ended questions (Tables 1 and 2).
Figure 6.
Student responses on a survey querying the COVID-19-modified histopathology laboratories. Shown are student responses on the surveys designed using a 5-point Likert scale. Numbers correspond to the percentage of students selecting a particular option. COVID-19 indicates coronavirus disease 2019.
Table 1.
Thematic Analysis of Student Comments: “What Aspects of Online Histopathology Laboratories Worked Best?”
| Theme | Frequency (%) | Example |
|---|---|---|
| Early access to the TAE helped | 52 (41.3) | “Nice to have the TAE available ahead of time” |
| Subthemes | ||
| It gives me more time | 18 (14.3) | “It allows me to take my time exploring he reading in Robbins as well as other sources” |
| It allows us to ask more questions | 10 (7.9) | “It allows us to come to the HP lab sessions with meaningful questions to ask the instructor” |
| Although remote, teamwork continues | 17 (13.5) | “The ability to work as a team remotely on the labs, and achieve the learning objectives that were specifically taught through the HP lab PowerPoint” |
| Faculty-led sessions help answer questions | 34 (27.0) | “Ability of the faculty to answer to multiple people at the same time in these large group settings is very helpful” |
| Lab format works well | 5 (4.0) | “Teams format we have right now is best for labs” |
| SoftChalk summaries, iLab and Team Application Template are most helpful in enhancing the learning experience | 27 (21.4) | “i-quiz and team application, soft-chalks!” |
Abbreviations: HP, histopathology; iLab, Individual Laboratory Quiz; TAE, Team Application Exercise.
Table 2.
Thematic Analysis of Student Comments: “What Aspects of Online Histopathology Laboratories Did Not Work?”
| Theme | Frequency (%) | Example |
|---|---|---|
| Taking the tLab individually does not work | 68 (54.0) | “Making the tquiz individual is not working for me” |
| Subthemes | ||
| Discussing questions with my team helps me learn | 24 (19.0) | “We learn so much through taking real team quizzes because of the discussions that take place over the questions” |
| We cannot view which questions we missed | 38 (30.2) | “We are not able to learn from our missed questions” |
| My learning experience decreased | 33 (26.2) | “…more conducive to my learning if we could take tquizzes together” |
| Incentive for collaboration decreased | 42 (33.3) | “The “team” aspect of the HP labs did not work for our group because we found it more productive to study individually for the HP quiz” |
| Anxiety for laboratories increased | 25 (19.8) | “individual tquiz portion of the test is extremely difficult and stressing” |
| Faculty-led sessions are unequal | 22 (17.5) | “Difference in lab instructors puts some teams at an advantage over others” |
| Subtheme | ||
| Students move out of assigned rooms | 14 (11.1) | “You may have had to wait a long time to have your questions addressed due to the glut of extra attendees” |
| Learning objectives, individual quiz and team application template are not compatible with team quiz in some sessions | 41 (32.5) | “Week 5 tquiz was very different from the learning objectives, the iLab, and the TAE” |
| Not all laboratories have associated lectures or SoftChalks | 23 (18.3) | “We do not have enough background information or normal histology lectures to reference” and “Need a SoftChalk or handout that corresponds to that specific lab” |
| Team average is not representative of grades | 8 (6.3) | “I do not feel that the average of our individual scores adequately represents our team’s performance because it does not take into account teamwork and discussion” |
Abbreviations: HP, histopathology; iLab, Individual Laboratory Quiz; TAE, Team Application Exercise; tLab, Team Laboratory Quiz.
Of the 126 students who responded, 48% were males, 42% were females and 10% preferred not disclose their sex. These numbers are representative of the preclinical medical school classes. Most students who responded were between 18 and 24 years of age (67%); 23% were between the ages of 25 to 34; and 9% chose to not indicate their age. Interestingly, 55% of students had taken fully online classes before the M2M and EFR modules and 70% of students could easily adapt to the online format of the HP laboratories. Most (90%) had reliable internet connections and 72% agreed with using MS Teams for the laboratories.
The iLab was considered useful for understanding topics covered during the week (76%). Most students (87%) agreed that early access to the TAE advantageous in preparing for the laboratory and felt that this led to higher order questions (75%) and early discussion of the TAE within teams (64%). The TAE was fully discussed before submission (71%) and most students agreed that it was a team effort (85%). Surprisingly, only 51% indicated that their questions were answered by faculty instructors.
Interestingly, only 37% of students indicated that the grading change (higher of the individual tLab score or the team average score) reduced their anxiety and only 33% agreed that taking the tLab individually helped them determine their level of understanding of the subject.
Overall, 62% of students agreed that the online HP laboratories helped in their learning although 60% of students indicated their preference for an in-person format. Thematic analysis of student comments in the open-ended questions confirmed that students preferred early access to the TAE (41%) as it gave them more time to reference study material (14%), complete their TAE in collaboration at their own pace with their teams that was facilitated using MS Teams and Google Slides (14%) and ask higher order questions (8%). Approximately 27% of students felt that the faculty helped answer their questions and 21% felt that the iLab, TAE, and faculty-prepared summaries in SoftChalk were useful in enhancing their learning experience.
When asked to comment about aspects of online HP laboratories that were challenging, a major theme was taking the tLab quiz individually (54%) as it eliminated team-based discussion (19%), decreased learning experience (26%) not only because of the lack of discussion but also because students could not ascertain which questions they missed (30%). This led to decreased collaboration within teams as students preferred to study individually for the tLab (33%), which, in turn, increased anxiety (20%). Stress was also compounded in some laboratory sessions in which the tLab quizzes were dependent, in part, on assigned reading and not fully covered either by lectures or SoftChalk-based study materials (18%), or when the iLab, TAE or the learning objectives were not representative of the tLab (33%).
Faculty Instructors Preferred In-Person Teaching
Faculty instructors who taught in HP laboratories were also asked about their opinions of the online HP laboratories via 5-point Likert scale surveys (Figure 7) that also included 2 open-ended questions (Table 3).
Figure 7.
Responses of faculty instructors teaching in histopathology laboratories on a survey querying the COVID-19 modified histopathology laboratories. Survey was designed using a 5-point Likert scale. Numbers correspond to the percentage of faculty selecting a particular option. COVID-19 indicates coronavirus disease 2019.
Table 3.
Thematic Analysis of Faculty Comments.
| Theme | Frequency (%) | Example |
|---|---|---|
| What aspects of online histopathology laboratories worked best? | ||
| Answering student questions | 3 (60.0) | “It seems that students wait for shorter time to have their questions addressed” |
| What aspects of online histopathology laboratories did not work? | ||
| Human interaction is missing | 3 (60.0) | “…personal interaction that extends beyond the question asked fosters the learning experience and is essentially missing in the virtual session.” |
| Socratic method of teaching is challenging | 2 (40.0) | “I like asking questions in the Socratic method, but this is challenging in the online setting.” |
Of the 5 faculty who responded, 60% were males; 40% preferred not disclose their sex. Three (60%) of the faculty held MD degrees, 1 had dual MD/PhD degree, and 1 preferred not to disclose their terminal degree. Two instructors (40%) were in the age range of 75 to 84 years, 1 instructor was in the age range of 25 to 34 years, and 2 (40%) preferred to not disclose their age. A majority of instructors who responded had taught in the HP laboratories for more than 15 years (60%), 1 had taught for 11 to 15 years, and 1 for less than 5 years. This correlated with their experience in teaching fully online classes, with 80% having never taught in fully online courses. Only 50% could adapt easily to the online format although their internet connections were reliable (80%). Most (60%) agreed that MS Teams was appropriate for the laboratories.
Interestingly, 60% of the faculty felt that the current lab format was not conducive with their teaching style, even with increased access to resources during online laboratories. While their preparation for online HP laboratories was similar to their preparation for the in-person format (80%), all (100%) of the instructors felt that they interacted with fewer students and preferred in-person teaching laboratories, perhaps because they could not judge student understanding better during in-person laboratories (80%) and were unable to fully address student questions online (80%). Some instructors (40%) disagreed that students learn better with online HP laboratories, but most (80%) were happy to contribute to teaching in the laboratories, whether they were online or in-person.
Thematic analysis of open-ended questions indicated that faculty felt that the online format was suitable for answering student questions (60%); however, they missed the in-person interaction (60%), especially when using the Socratic method of teaching by asking questions (40%).
Discussion
The current COVID-19 pandemic has driven an abrupt transition from face-to-face instruction to varying degrees of online teaching. In response to social restrictions instituted due to the COVID-19 pandemic last spring, UTHSA began immediate transition to remote learning for students in the preclinical curriculum. Histopathology teaching laboratories previously taught in-person in a common assembly room were redesigned for remote teaching via MS Teams to continue progression through the preclinical curriculum. While the most commonly utilized online platforms among institutions transitioning to remote learning during the current pandemic are those of Zoom and Google (Alphabet Inc., Mountain View, CA),6 neither students nor faculty expressed difficulty accessing or utilizing MS Teams to participate in the laboratories (Figures 6 and 7), and most felt their internet connectivity was sufficiently reliable. About 50% of the students had initially taken fully online courses and most could easily adapt to the online format. In contrast, 60% of faculty instructors who responded had been teaching for more than 15 years and 80% had never taught a fully online course before. Not surprisingly, faculty were equally divided among those who could transition easily to the online format and those who could not.
Remote learning through online educational activities is not novel and includes massive open online courses, prerecorded lectures, online interactive sessions, tutorials made using platforms such as SoftChalk, and web/videoconferencing.7-9 Over the last decade or more, most medical schools have developed an integrated preclinical curriculum, accompanied by a reduction in contact hours10-12 and a corresponding increase in self-directed student learning, including asynchronous remote learning.13 This transition increasingly emphasizes self-directed learning, problem-based learning, TBL, and flipped classroom lectures. Online delivery of courses has the potential to enhance student engagement, geographical accessibility, and synchronous/asynchronous learning and assessment.14-17 However, this change has not been easy in terms of preparing online activities by faculty or in learning remotely by students. A recent meta-synthesis analytical review of medical educational practices in response to past endemic and epidemic crises similar to the current pandemic reported the importance of faculty innovation and ability to adapt rapidly to implement remote learning platforms.6
Remote learning, however, has disadvantages as well. Medical students at the University of California at San Diego were polled in March 2020 for their impressions regarding remote learning and perceived preparation for future stages of learning,18 including USMLE step I and third year clinical clerkships. They reported negative impacts on the quality of instruction and their ability to participate in the preclinical curriculum using remote learning platforms. Narrative responses of the students included comments about “digital fatigue, decreased ability to participate, and lack of clinical skills and hands-on lab learning” as notable deficits. More specifically, over 71% of respondents felt that the quality of instruction in histology was very negatively or somewhat negatively affected by remote learning. And over 75% of respondents felt that remote learning adversely affected their ability to participate in the curriculum. Students felt less connected with the medical school as a consequence to pandemic-related remote learning. Therefore, it is important that technology-based teaching platforms perform outcomes assessments to determine application effectiveness and sustainability19; yet, outcomes measures are infrequently seen in reports related to transitions in medical education formats.
The outcomes assessments of the changes implemented to the HP laboratories at UTHSA have identified actionable items that can be used to strengthen the pre-pandemic format. Clearly, the early release of the TAE was positively received by students as it gave them more time to peruse the study material related to the clinical cases, discuss the cases with their teams, and ask more meaningful questions of the laboratory instructors (Table 1). In contrast, the conversion of tLab to an individual format was perceived to decrease learning experience due to lack of team-based discussion that resulted from an increased focus on self-study rather than team-based collaboration for the tLab, resulting in an unanticipated increased in stress and anxiety (Table 2).
The individual and team averages in the tLab decreased, with fewer students receiving scores of 10/10 (Figures 2 and 3). Interestingly, MS1 student scores appeared to improve after the first tLab of the M2M module but dipped in the fourth tLab (Figures 2 and 3). This decrease in scores may have been a function of the difficulty of subject matter for students as the fourth laboratory session covered the basic concepts of dysplasia and neoplasia as well as morphological features of dysplastic and neoplastic cells. In contrast, MS2 student scores on the tLabs in the EFR module were consistently lower than previous years although weekly quizzes, based on non-laboratory module content remained high. The lower tLab scores may indicate a longer lag time of adjusting to the new format as these students completed most of their first academic year with the previous laboratory format. The MS1 students directly began their preclinical studies with the COVID-19 modified laboratory format and perhaps could adapt more easily.
Interestingly, the tLab scores did not correlate with the consistently high scores for each of these sets of students on the weekly module quizzes designed to test knowledge of material covered during each week of a module (Figure 4). Additionally, grades on midterm and final exams in these modules were consistent from pre-pandemic to pandemic periods (Figure 5), indicating that the changes in the laboratory format in response to the pandemic did not adversely affect the learning experience. While it would have been more relevant to analyze HP-specific questions in the examinations, it was difficult to distinguish questions based solely on HP, as most incorporated multiple other disciplines, thereby complicating question analysis.
It was previously thought that the tLab performance reflected the overall understanding of each student in the team. However, based on surveys, it appears that each member of a team became an “expert” on a particular topic and thereby played their part in contributing to the tLab. Students felt that taking the tLab together as a team allowed greater learning through discussion of the questions (Table 2). When taken individually, only a few students could master all the topics in the given time and this resulted in decreased scores on the tLab. The identification of poorly performing students who were earlier hidden as they received their team’s scores can be important in setting up early interventions. However, a long-term study that follows the performance of these students over multiple modules will be necessary to determine if their grades in the HP laboratories is reflective of their overall grades in the preclinical years.
Contrary to design intention, taking the tLab individually increased testing anxiety despite the students receiving their score or their team’s average score, which ever was higher (Table 2). The shift to remote learning in response to the COVID-19 pandemic likely generated increased levels of general anxiety within student populations, which was compounded by isolation and a sense of being disconnected.19,20 Interestingly, a recent study found that while student participation in optional, remote teaching sessions appeared to be higher than pre-pandemic student attendance figures and that student completion of course assignments was high, student-to-student collaboration was minimal.21 Medical students come to rely on social interactions and bonding to deal with the inherently rigorous medical school curriculum. However, their performance in weekly quizzes and module examinations suggest that additional explanations are required. It is possible that some of these students felt the burden of needing to score high on every tLab so as to not be responsible for bringing down their team averages.
Will the transitions in medical education so quickly developed in response to the pandemic prove useful beyond the current pandemic? More specifically, what is the future of remotely conducted HP teaching laboratories? Students at the Adelson School of Medicine, Ariel University in Israel indicated their preference to continue online learning past the current pandemic.13 However, student satisfaction with laboratory-based courses taught remotely significantly decreased as compared to previous years with in-person instruction.22 It was thought that such dissatisfaction would only increase with longer courses conducted remotely. Given that our students preferred to collaborate in-person rather than remotely, it appears that in-person HP laboratories that would be modified to incorporate our current findings will likely continue in the future.
Acknowledgments
The authors appreciate the assistance of students and faculty instructors in the histopathology laboratories at UT Health San Antonio who participated in this study. The authors would also like to thank Drs. Jeff Jackson and Deborah Chang, as well as Leslie Cano, Undergraduate Medical Education, for their help with collating laboratory reviews.
Footnotes
Declaration of Conflicting Interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article. This article was competitively selected by Academic Pathology’s Editors, from among abstracts submitted in response to a Special Call for COVID-19 Papers, to receive an article processing fee waiver sponsored by the Association of Pathology Chairs.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article
ORCID iD: Ramaswamy Sharma  https://orcid.org/0000-0003-2346-5305
https://orcid.org/0000-0003-2346-5305
References
- 1. Rose S. Medical student education in the time of COVID-19. JAMA. 2020;323(21):2131–2132. doi:10.1001/jama.2020.5227 [DOI] [PubMed] [Google Scholar]
- 2. Ruiz JG, Mintzer MJ, Leipzig RM. The impact of E-learning in medical education. Acad Med. 2006;81(3):207–212. doi:10.1097/00001888-200603000-00002 [DOI] [PubMed] [Google Scholar]
- 3. Ward JP, Gordon J, Field MJ, Lehmann HP. Communication and information technology in medical education. Lancet. 2001;357(9258):792–796. doi:10.1016/S0140-6736(00)04173-8 [DOI] [PubMed] [Google Scholar]
- 4. King TS, Sharma R, Jackson J, Fiebelkorn KR. Clinical case-based image portfolios in medical histopathology. Anat Sci Educ. 2019;12(2):200–209. doi:10.1002/ase.1794 [DOI] [PubMed] [Google Scholar]
- 5. Elder L, Paul R. The role of Socratic questioning in thinking, teaching, and learning. The Clearing House. 1998;71(5):297–301. doi:10.1080/00098659809602729 [Google Scholar]
- 6. Camargo CP, Tempski PZ, Busnardo FF, Martins MA, Gemperli R. Online learning and COVID-19: a meta-synthesis analysis. Clinics (Sao Paulo). 2020;75:e2286. doi:10.6061/clinics/2020/e2286 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Merrell RC. Education and distance learning: changing the trends. Stud Health Technol Inform. 2004;104:141–146. doi:10.3233/978-1-60750-947-9-141 [PubMed] [Google Scholar]
- 8. Taylor D, Grant J, Hamdy H, Grant L, Marei H, Venkatramana M. Transformation to learning from a distance. MedEdPublish. 2020;9(1):76. doi:10.15694/mep.2020.000076.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Zhou T, Huang S, Cheng J, Xiao Y. The distance teaching practice of combined mode of massive open online course micro-video for interns in emergency department during the COVID-19 epidemic period. Telemed J E Health. 2020;26(5):584–588. doi:10.1089/tmj.2020.0079 [DOI] [PubMed] [Google Scholar]
- 10. Buja LM. Medical education today: all that glitters is not gold. BMC Med Educ. 2019;19(1):110. doi:10.1186/s12909-019-1535-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Norman G. Medical education: past, present and future. Perspect Med Educ. 2012;1(1):6–14. doi:10.1007/s40037-012-0002-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Rutledge C, Walsh CM, Swinger N, et al. Gamification in action: theoretical and practical considerations for medical educators. Acad Med. 2018;93(7):1014–1020. doi:10.1097/ACM.0000000000002183 [DOI] [PubMed] [Google Scholar]
- 13. Sandhaus Y, Kushnir T, Ashkenazi S. Electronic distance learning of pre-clinical studies during the COVID-19 pandemic: a preliminary study of medical student responses and potential future impact. Isr Med Assoc J. 2020;22(8):489–493. [PubMed] [Google Scholar]
- 14. Bao W. COVID-19 and online teaching in higher education: a case study of Peking University. Hum Behav Emerg Technol. 2020;2(2):113–115. doi:10.1002/hbe2.191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Evans DJR, Bay BH, Wilson TD, Smith CF, Lachman N, Pawlina W. Going virtual to support anatomy education: a STOPGAP in the midst of the Covid-19 pandemic. Anat Sci Educ. 2020;13(3):279–283. doi:10.1002/ase.1963 [DOI] [PubMed] [Google Scholar]
- 16. Kay D, Pasarica M. Using technology to increase student (and faculty satisfaction with) engagement in medical education. Adv Physiol Educ. 2019;43(3):408–413. doi:10.1152/advan.00033.2019 [DOI] [PubMed] [Google Scholar]
- 17. Pather N, Blyth P, Chapman JA, et al. Forced disruption of anatomy education in Australia and New Zealand: an acute response to the Covid-19 pandemic. Anat Sci Educ. 2020;13(3):284–300. doi:10.1002/ase.1968 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Shahrvini B, Baxter SL, Coffey CS, MacDonald BV, Lander L. Pre-clinical remote undergraduate medical education during the COVID-19 pandemic: a survey study. Preprint. Res Sq. 2020;rs.3.rs–33870. doi:10.21203/rs.3.rs-33870/v1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Gaur U, Majumder MAA, Sa B, Sarkar S, Williams A, Singh K. Challenges and opportunities of preclinical medical education: COVID-19 crisis and beyond. SN Compr Clin Med. 2020:1–6. doi:10.1007/s42399-020-00528 -1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Chinelatto LA, Costa TRD, Medeiros VMB, et al. What you gain and what you lose in COVID-19: perception of medical students on their education. Clinics (Sao Paulo). 2020;75:e2133. doi:10.6061/clinics/2020/e2133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Garg M, Eniasivam A, Satterfield J, Norton B, Austin E, Dohan D. Rapid transition of a preclinical health systems science and social justice course to remote learning in the time of coronavirus. Med Educ Online. 2020;25(1):1812225. doi:10.1080/10872981.2020.1812225 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Vollbrecht PJ, Porter-Stransky KA, Lackey-Cornelison WL. Lessons learned while creating an effective emergency remote learning environment for students during the COVID-19 pandemic. Adv Physiol Educ. 2020;44(4):722–725. doi:10.1152/advan.00140.2020 [DOI] [PMC free article] [PubMed] [Google Scholar]