Abstract
Background and aim:
Open-wedge high tibial osteotomy (HTO) is a good choice in the treatment of varus knee medial osteoarthritis, with the restore of the correct mechanical axis of the lower limb. Autologous adipose derived stem cells (aASCs) are used in cartilage regeneration and in the treatment of early osteoarthritis. Aim of this study is to retrospectively analyze clinical (and radiological) results in two populations of patients with initial varus medial knee osteoarthritis, treated with HTO, with or without associated intra-articular injection of aASCs.
Methods:
In this study we analyze 85 patients treated with HTO for varus knee osteoarthritis with or without Lipogems® intra-articular injection. It was used of a single model of HTO plate. No associated procedure was performed.
Results:
Significant improvement in the daily life activity assessment (KOOS score) was observed in the group treated also with aASCs compared with group treated with isolated HTO.
Conclusions:
We suggest, in these patients, the surgical indication of an open-wedge high tibial osteotomy (HTO) and simultaneous injection with aASCs associated procedure to improve cartilage regeneration, with clinical improvement. (www.actabiomedica.it)
Keywords: high tibial osteotomy, varus knee osteoarthritis, adipose derived stem cells, Lipogems®
Introduction
Before the development of total knee arthroplasty (TKA) as a surgical procedure that had a rapid expansion in the 80s, high tibial osteotomy (HTO) was the most used surgical technique used for the treatment of initial varus knee osteoarthritis (1). Initially the technique involved a minus osteotomy, through removal of lateral bone wedge. Mechanical axis was consequently changed from varus alignment to valgus. The first fixation method was a metallic stample and temporary locking with a cast (2). In the last two decades, HTO has developed as a tibial medial bone plus; the stabilization was obtained with external fixation at the beginning, then converting it with internal fixation using plates of different size and frame (1).
Aim of this intervention is reducing loads on the medial compartment, in patients with initial medial varus knee osteoarthritis, but also to release the posterolateral complex in posterolateral laxity of the knee (3).
With recovery of the correct mechanical axis obtained with HTO, it can happen only a partial remodeling of the articular cartilage, that was overloaded before the surgical correction (4). It was therefore necessary to associate related procedures to this surgical gesture, trying to regenerate the articular cartilage.
Autologous adipose derived stem cells (aASCs) have recently attracted attention, especially in the context of cartilage regeneration (5) and in the treatment of early osteoarthritis. It has recently been reported that intraarticular injection of micro fragmented autologous adipose tissue, leads to a VAS and clinical results improvements, in patients with initial knee osteoarthritis (6).
Materials and Methods
The population involved in this study is composed of patients with varus knee osteoarthritis, treated with HTO, with or without association of aASCs.
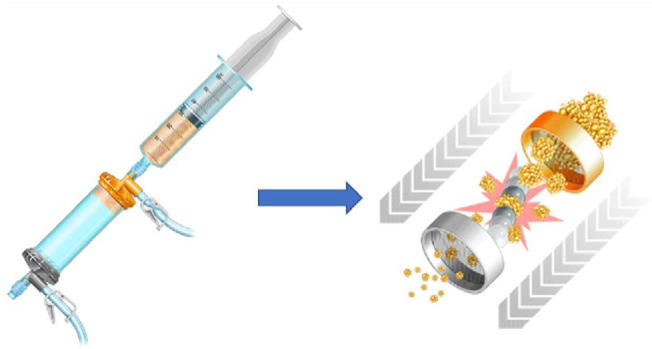
The subjects of the study are patients treated with HTO for varus knee osteoarthritis, from November 2, 2016 to November 2, 2018 at the Department of Orthopedics and Traumatology of Sacro Cuore Hospital - Don Calabria in Negrar di Valpolicella (VR - Italy). Patients were divided into two groups. In the first group, the treatment performed was isolated HTO; in the second group the same intervention was performed with the association of intra-articular injection of aASCs using Lipogems® system (figure 1).
Figure 1.
In order to obtain two groups homogeneous and to avoid variables that could affect the results of the study, only the cases with the following characteristics were selected:
isolated osteotomy surgery, without any associated surgical procedure;
use of a single model of HTO plate (ZIMMER BIOMET® - Dynafix®);
mild to moderate degree of initial osteoarthritis (according to Kellgren e Lawrence scale I-II-III).
After the exclusion of all patients operated with plate of another company and those undergoing associated surgery, 85 patients were included. Of these subjects, 43 were treated with HTO and 42 with HTO with intra articular injection of aASCs, using Lipogems® system. All the patients were affected by mild-moderate grade medial knee osteoarthritis. All the operations were performed by the same surgeon with the same fixation method (same plate type) and no associated procedure was performed. One year after surgery, all patients underwent surgery to remove the HTO plates.
Functional evaluation of clinical and subjective situation of all patients was performed through validated scores: KOOS (Knee Injury and Osteoarthritis Outcome Score) (7,8), Lysholm Knee Questionnaire / Tegner Activity Scale (9,10) and IKDC (International Knee Documentation Comittee) (11, 12, 13, 14). These scores were submitted to patients before the surgery (T0) (figure 3A) and after one year (T1) (figure 3B).
Figure 3A.

Figure 3B.

Figure 2.
Radiological evaluation of knee osteoarthritis was done at T0 and at T1 (simultaneously with the plate removal) rating the degree of severity with the KL scale (15).
Results
A significant clinical improvement was observed in all patients treated with HTO (with or without aASCs).
All the variables measured at follow-up showed statistically significant differences compared with baseline.
Similar improvement at follow-up compared baseline was observed between patients treated with HTO (group A) and patients treated with HTO associated with Lipogems® (group B).
Similarly, significant differences at follow up were observed for all the observed variables.
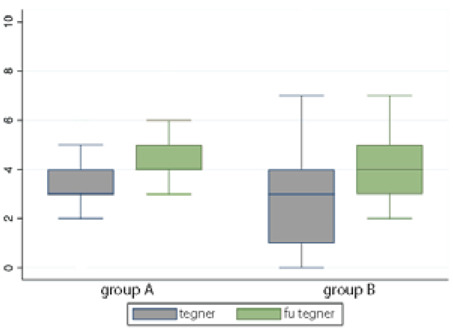
Notably, no significant difference was found in the subjective evaluation using the IKDC and Lysholm / Tegner tests, between group A and group B (Figure 4A, B, C).
Figure 4A.
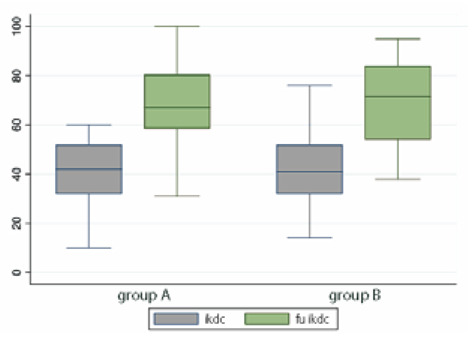
Figure 4B.
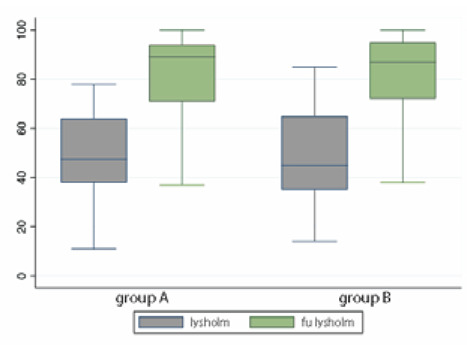
Figure 4C.
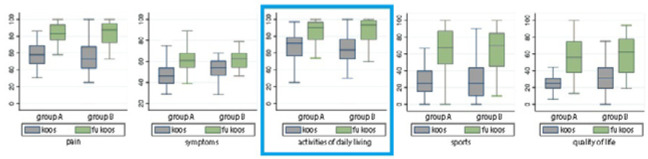
On average, KOOS score demonstrated only non-significant variations in both the treatment groups, in terms of assessment of pain, symptoms, sports and quality of life.
Conversely, a significant improvement in the activities of daily living assessment was observed in the group B compared with group A (p<0.05) (figure 5).
Figure 5.
Importantly, there was no significant difference at follow up in the radiological assessment according to the Kellgren Lawrence scale.
Overall, the study cohort was stratified according to the severity of osteoarthritis (mild vs moderate).
38 patients presented a K-L grade =1, whereas 47 patients presented a K-L grade 2 and 3.
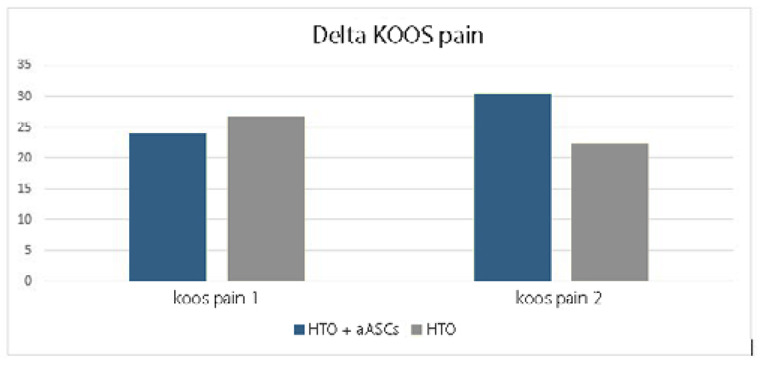
Clinical outcomes between the two groups (mild vs moderate osteoarthritis) were compared at follow-up according to the different treatment. No significant difference was observed in the two groups in terms of clinical improvement using different KOOS variable scores.
Nevertheless, there was a trend towards subjective improvement of symptoms (pain variable) in patients with mild arthrosis treated with HTO and aASCs compared with patients with mild osteoarthritis treated with HTO alone. (figure 6)
Figure 6.
Discussion
The management of chondral disease includes conservative therapies and surgical procedures. Encouraging results have been reported using mesenchymal stem cells (MSCs), either alone or in association with surgery (16).
In literature some studies were published about aASCs and surgery of many different types.
Some authors assessed the effectiveness of the arthroscopic or conservative treatments in patients diagnosed with knee OA (Kellgren-Lawrence grade 2 to 4) with 5 years of follow-up, concluding that arthroscopy provided no benefit in decreasing or delaying arthroplasty and that it can relieve symptoms only up to 2 years (17). Cattaneo et al. (18) also studied the safety and potential benefits of using aASCs injection associated with the arthroscopic chondral shaving for the treatment of diffused knee chondropathy.
Bisicchia et al. (19) tried to study association between aASCs and microfractures, that is more effective in clinical terms than microfractures alone in patients affected by symptomatic knee focal chondral lesions.
Recently, Lipogems® has ben studied also for treatment of meniscal tears. Malanga et al. (20) demonstrated that autologous micro-fragmented adipose tissue injected directly into meniscal tears following trephination of the tear along with a joint injection under direct ultrasound guidance, can be a safe and clinically significant treatment option for degenerative meniscus tears and knee osteoarthritis.
In this study, 85 patients were treated for the same pathological condition, mild and moderate varus knee osteoarthritis. The same surgical technique was performed in all the patients, HTO, using the same specific plate type. In 42 of these patients, intra-articular injection of aASCs with Lipogems® was done as an associated procedure.
At the follow up, in addition to scores, a radiological control was performed, coinciding with the removal of the HTO plate.
In a recent study of Kim and Koh (21), data of two groups of patients were analyzed, similarly to those evaluated in our study. In their analysis, only scores calculated by IKDC and Lysholm were considered. A second look arthroscopic evaluation at the follow up was done. Their results were positive in the group of patients treated with aASCs (arthroscopic point of view, ICRS grading) and according to IKDS score.
Our results are therefore comparable with those reported in literature by similar studies.
In addition, our study cohort was stratified according to the severity of osteoarthritis (mild vs moderate) and evaluated with koos variables.
In the variables examined, the results obtained by this type of intervention (HTO) in patients with varus knee osteoarthritis, were positive, with a clear clinical improvement between T0 and T1. This confirm of the indication for this technique, in patients affected by this pathology.
In the distinction between the two groups, a statistically significant difference emerged according to KOOS scale. A significant improvement in the activities of daily living (ADL) assessment was observed in the group B compared with group A (p<0.05).
Radiological evaluation before and after surgery showed no worsening of these patients according to Kellgren and Lawrence scale. From this point of view, no differences were showed between the two groups examined.
Conclusions
This study revealed improved clinical results in both groups at follow-up, correlated with the simultaneous improvement obtained with the scores used.
There was a significant difference in the group treated with intra-articular injection of aASCs in the context of daily activities on the KOOS scale.
Radiological evaluation at follow-up showed no differences compared with baseline in terms of worsening of osteoarthritis. There were no differences between the two groups examined.
This study has limitations that need to be acknowledged. Number of patients is limited and does not allow to obtain absolute conclusions. Radiological analysis by MRI relative to the degree of chondral damage of the affected compartment, before surgery and at the follow up, could have give us very useful information about the use of aASC in cartilage regeneration.
In the surgery associated with Lipogems® injection, compared to isolated HTO, the trend shows more important improvement of the pain symptom in patients with moderate osteoarthritis compared with subjects with mild osteoarthritis. Initial pain condition is therefore a parameter to consider in the indication to this kind of treatment. Our conclusion is that in patients with varus knee osteoarthritis, the indication for an open-wedge high tibial osteotomy (HTO) must always be considered. In this context, simultaneous injection with aASCs should be considered as an associated procedure to improve cartilage regeneration, with clinical improvement in some of the functional outcomes.
Conflict of Interest:
Each author declares that he or she has no commercial associations (e.g. consultancies, stock ownership, equity interest, patent/licensing arrangement etc.) that might pose a conflict of interest in connection with the submitted article
References
- 1.Prodromos CC, Amendola A, Jakob RP. “High tibial osteotomy: indications, techniques, and postoperative management”. Instr Course Lect. 2015;64:555–65. [PubMed] [Google Scholar]
- 2.Coventry MB. “Oteotomy about the knee for degenerative and rheumatoid arthritis”. J Bone Joint Surg Am. 1973;55(1):23–48. [PubMed] [Google Scholar]
- 3.Niemeyer P, Stöhr A, Köhne M, Hochrein A. “Medial opening wedge high tibial osteotomy”. Oper Orthop Traumatol. 2017; Aug;29(4):294–305. doi: 10.1007/s00064-017-0509-5. [DOI] [PubMed] [Google Scholar]
- 4.Matsunaga D, Akizuki S, Takizawa T, Yamazaki I, Kuraishi J. “Repair of articular cartilage and clinical outcome after osteotomy with microfracture or abrasion arthroplasty for medial gonarthrosis”. Knee. 2007;14:465–471. doi: 10.1016/j.knee.2007.06.008. [DOI] [PubMed] [Google Scholar]
- 5.Hurley ET, Yasui Y, Gianakos AL, Seow D, Shimozono Y, Kerkhoffs GMMJ, Kennedy JG. “Limited evidence for adipose-derived stem cell therapy on the treatment of osteoarthritis”. Knee Surg Sports Traumatol Arthrosc. 2018 Nov;26(11):3499–3507. doi: 10.1007/s00167-018-4955-x. [DOI] [PubMed] [Google Scholar]
- 6.Hudetz D, Borić I, Rod E, Jeleč Ž, Radić A, Vrdoljak T, Skelin A, Lauc G, Trbojević-Akmačić I, Plečko M, Polašek O, Primorac D. “The effect of intra-articular injection of autologous microfragmented fat tissue on proteoglycan synthesis in patients with knee osteoarthritis”. Genes (Basel) 2017, 13;8(10):270. doi: 10.3390/genes8100270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Roos EM, Roos HP, Lohmander LS, Ekdahl C, Beynnon BD. “Knee injury and Osteoarthritis Outcome Score (KOOS) e development of a self-administered outcome measure”. J Orthop Sports Phys Ther. 1998;28:88e96. doi: 10.2519/jospt.1998.28.2.88. [DOI] [PubMed] [Google Scholar]
- 8.Monticone M, Ferrante S, Salvaderi S, Rocca B, Totti V, Foti C, Roi GS. “Development of the Italian version of the knee injury and osteoarthritis outcome score for patients with knee injuries: cross-cultural adaptation, dimensionality, reliability, and validity”. Osteoarthritis Cartilage. 2012 Apr;20(4):330–5. doi: 10.1016/j.joca.2012.01.001. doi: 10.1016/j.joca.2012.01.001. Epub 2012 Jan 10. [DOI] [PubMed] [Google Scholar]
- 9.Échelle de Lysholm-Tegner. www.orthopaedicscore.com/scorepages/ tegner lysholm knee.html.
- 10.Tegner Y, Lysholm J. “Rating systems in the evaluation of knee ligament injuries”. Clin Orthop. 1985;198:43–9. [PubMed] [Google Scholar]
- 11.Girgis FG, Marshall JL, Monajem A. “The cruciate ligaments of the knee joint. Anatomical, functional and experimental analysis,”. Clin. Orthop. Feb. 1975;(106):216–231. doi: 10.1097/00003086-197501000-00033. [DOI] [PubMed] [Google Scholar]
- 12.Amis AA, Dawkins GP. “Functional anatomy of the anterior cruciate ligament. Fibre bundle actions related to ligament replacements and injuries,”. J. Bone Joint Surg. Br. Mar. 1991;73(2):260–267. doi: 10.1302/0301-620X.73B2.2005151. [DOI] [PubMed] [Google Scholar]
- 13.Hollis JM, Takai S, Adams DJ, Horibe S, Woo SL. “The effects of knee motion and external loading on the length of the anterior cruciate ligament (ACL): a kinematic study,”. J. Biomech. Eng. May 1991;113(2):208–214. doi: 10.1115/1.2891236. [DOI] [PubMed] [Google Scholar]
- 14.Duthon VB, Barea C, Abrassart S, Fasel JH, Fritschy D, Ménétrey J. “Anatomy of the anterior cruciate ligament,”. Knee Surg. Sports Traumatol. Arthrosc. Off. J. ESSKA. Mar. 2006;14(3):204–213. doi: 10.1007/s00167-005-0679-9. [DOI] [PubMed] [Google Scholar]
- 15.Kellgren JH, Lawrence JS. “Radiological assessment of osteo-arthrosis”. Ann Rheum Dis. 1957;16:494–502. doi: 10.1136/ard.16.4.494. doi: 10.1136/ard.16.4.494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Russo A, Screpis D, Di Donato SL, Bonetti S, Piovan G, Zorzi C. “Autologous micro-fragmented adipose tissue for the treatment of diffuse degenerative knee osteoarthritis: an update at 3 year follow-up”. Journal of Experimental Orthopaedics. 2018;5:52. doi: 10.1186/s40634-018-0169-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Su X, Li C, Liao W, Liu J, Zhang H, Li J, Li Z. “Comparison of arthroscopic and conservative treatments for knee osteoarthritis: a 5-year retrospective comparative study”. Arthroscopy. 2018;34(3):652–659. doi: 10.1016/j.arthro.2017.09.023. [DOI] [PubMed] [Google Scholar]
- 18.Cattaneo G, De Caro A, Napoli F, Chiapale D, Trada P, Camera A. “Micro-fragmented adipose tissue injection associated with arthroscopic procedures in patients with symptomatic knee osteoarthritis”. BMC Musculoskelet Disord. 2018;19:176. doi: 10.1186/s12891-018-2105-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bisicchia S, Bernardi G, Pagnotta SM, Tudisco C. “Micro-fragmented stromal-vascular fraction plus microfractures provides better clinical results than microfractures alone in symptomatic focal chondral lesions of the knee”. Knee Surgery, Sports Traumatology, Arthroscopy. 2020 Jun;28(6):1876–1884. doi: 10.1007/s00167-019-05621-0. [DOI] [PubMed] [Google Scholar]
- 20.Malanga GA, Chirichella PS, Hogaboom NS, Capella T. “Clinical evaluation of micro-fragmented adipose tissue as a treatment option for patients with meniscus tears with osteoarthritis: a prospective pilot study”. International Orthopaedics (SICOT) 2020 doi: 10.1007/s00264-020-04835-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kim YS, Koh YG. “Comparative Matched-Pair Analysis of Open-Wedge High Tibial Osteotomy With Versus Without an Injection of Adipose-Derived Mesenchymal Stem Cells for Varus Knee Osteoarthritis”. Am J Sports Med. 2018 Sep;46(11):2669–2677. doi: 10.1177/0363546518785973. [DOI] [PubMed] [Google Scholar]


