Abstract
Background and aim of the work:
to review and discuss the literature about rotational malalignment during and after femoral nailing.
Methods:
analysis of the literature on prevention and evaluation of rotation during femoral nailing, clinical and subjective consequences of malrotation and techniques used to correct the deformity, both in the acute and chronic phase.
Results:
malrotation is very common after femoral nailing. The exact definition of a malrotated femur is controversial, but it is widely agreed that a rotational malalignment <10° is considered normal while >30° is a deformity which requires correction. The complaints of the patients with a malrotated femur can be various and can involve the hip, the knee or below the knee. The ability to compensate for the deformity while standing and walking may decrease the symptoms. Surgical correction is feasible with many techniques and devices: the procedure involving derotation, changing the locking screws and maintaining the nail is safe, reproducible and relatively easy.
Conclusions:
prevention of malrotation during femoral nailing is the cornerstone of successful operation outcomes. If rotational malalignment is suspected, prompt diagnosis and adequate surgical treatment are mandatory to overcome this common complication. (www.actabiomedica.it)
Keywords: femoral nailing, malrotation, rotational malalignment, derotation
Introduction
Intramedullary nailing (IMN) has become the gold standard for the treatment of femoral shaft fractures in adults (1, 2). Antegrade and retrograde IMN are safe and highly reproducible techniques to address fractures of femoral shaft, even with proximal (subtrochanteric) and distal (supracondylar) extension. These techniques were proven to be very effective in achieving union in such fractures, due to their biological advantages, which include minimal surgical dissection and indirect fracture reduction without disruption of the fracture hematoma. The incidence of union following IMN of closed femur fractures (and even in re-nailing procedures for femoral shaft non-unions) is nearly 99% (3, 4).
IMN is usually performed as a closed procedure, thus malalignment can frequently occur. The resulting deformity may include improper length, malrotation and angular malalignment (5, 6). These malunions are not always clinically evident and they can often be detected only through accurate and thorough radiological exams. Malrotation is the most frequent malalignment after IMN (range 2.3% to 35%), it is very difficult to detect both radiographically (during and after the operation) and clinically, and it is often underappreciated (7, 8, 9). Patients with bilateral femur shaft fractures have a higher risk of healing with a malrotation of their femurs. This was clearly demonstrated by Citak (10), who, in his series of 24 patients (48 femoral fractures), described 41.2% femoral malrotation >15°. Possible explanations for these results will be discussed later.
The exact angle at which a healed femur con be considered “malrotated” is hard to define. Some authors consider 10° to be the cut-off (11), while others define a malrotation when the malunion exceeds 15° (6, 8, 12). Between 10° and 15° there is a “grey zone”, where a paraphysiological malrotation is acceptable. However, even in moderate malrotation, many reports suggest that these deformities after IMN are usually well tolerated by the patient and do not appear to impede normal activity. On the other hand, for malrotation >30°, there is broad agreement on surgical correction (13, 14).
Evaluation of Rotation During and After Femur Nailing
The data available are not uniform regarding the percentage of malrotation in relation to the level of femoral shaft fractures (proximal, middle or distal third). Thoresen (15) reported a higher frequency of rotational malalignment in distal femoral shaft fractures; Winquist (5), on the contrary, in proximal third; while Jaarsma (8) and Karaman (16) did not find any correlation between torsional deformities and fracture location. Fracture patterns with a higher risk of malrotation include transverse, segmental and comminuted fractures (especially those associated with bone loss) (17).
Patient positioning is considered by some authors to influence the rate and direction of malrotation; generally, the surgeon must be aware of the tendencies towards internal rotation (femur in traction on a fracture table) and external rotation (free-leg on a flat table) in the different positions of the patient (18). Conversely, Tornetta (12) found no correlation between malrotation and patient positioning. Even anterograde and retrograde femoral nailing do not seem to affect the final malrotation rate (6).
A reason for the high incidence of femoral malrotation after nailing is the difficulty to accurately assess the torsion alignment of the femur during the operation. Many techniques currently exist to determine the femoral antetorsion intraoperatively, and they are mainly based on comparison with the contralateral, uninjured femur. However, none of them are absolutely precise in determining the right rotation of the injured femur.
Clinical evaluation during surgery has proven to be an inconsistent method of judging rotation, with missed malrotation >20° in 40% of the cases (8). Comparison of the fractured limb with the uninjured side in a clinical evaluation with observation of foot rotation is feasible only when the patient is supine on a flat table. Even then, the swollen thigh, the rotation of the proximal fragment and other variables make an accurate clinical evaluation extremely difficult, if not impossible. Another clinical method is the comparison of the passive arc of motion of the femoro-acetabular joints: each hip is fully rotated both internally and externally. Assuming that each hip is free of pathology and has a similar amount of total rotation, then a side-to-side difference can be attributed to malrotation through the fracture site. These manoeuvres during surgery are possible only once the nail has been locked; furthermore, femoral anteversion is patient-specific and varies considerably, with significant bilateral differences. In the absence of previous trauma, some people have anteversion differences of 15° between limbs (19).
The evaluation of the profile of the lesser trochanter is one of the most widely used methods to assess femoral rotation during nailing (8, 9, 20). A true lateral view of the knee of the uninjured side is obtained with a fluoroscopy. The distal femur is then held in that position while an antero-posterior view of the proximal femur is obtained to evaluate the profile of the lesser trochanter. This image is either stored digitally or printed out. After positioning the patient, the knee of the injured side is held in the right position after obtaining a true lateral view. The proximal part of the femur is then rotated, either with a Shantz screw, long haemostatic forceps (21) (Fig. 1) or a reduction clamp (22), until the profile of the lesser trochanter is comparable to the saved image of the healthy side.
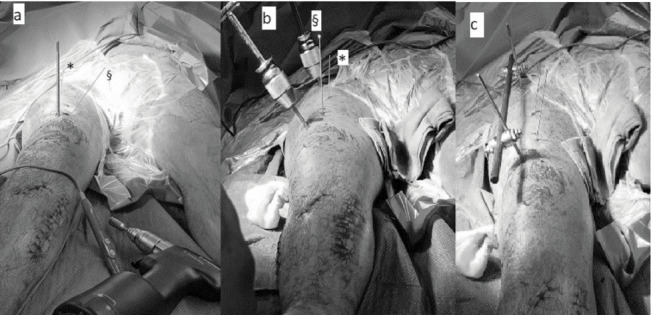
Figure 1.
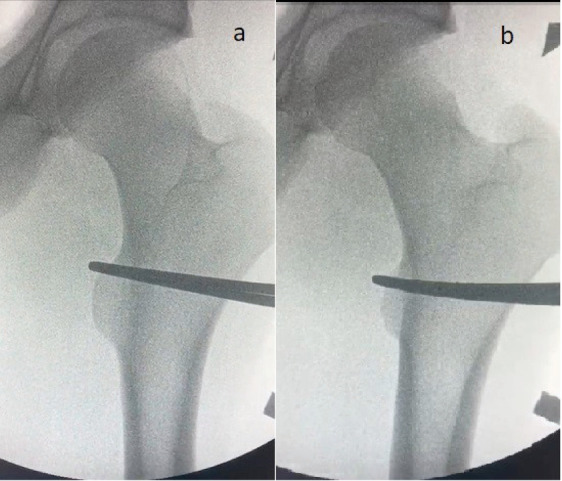
Correction of external rotation of the proximal femur in a shaft fracture. a: the lesser trochanter is fully visible. b: haemostatic forceps are used to internally rotate the proximal femur. The difference in the profile of the lesser trochanter can be noted
After that, the nail can be inserted and locked. With this technique, the difference in rotation between the two sides was reported to be <4° (9). When considered alone, the profile of the lesser trochanter was demonstrated to be an inaccurate method, resulting in a rotational malalignment of up to 19° (8). For this reason, it is advisable to always compare it with the contralateral side. This method cannot be used in bilateral femoral fractures (due to the impossibility of a comparison with the uninjured femur), when the fractures involve the lesser trochanter or in patients with pre-existing hip diseases. Another practical limitation of this technique, often noted by the writing author, is the difficulty to maintain the exact rotation of the proximal femur during reaming and insertion of the nail. The technique of the lesser trochanter, even though very popular, is not widely accepted and similar results in correction or malrotation are obtained with other methods (23).
Another technique is the one described by Hilgert (24) and, similarly, by Tornetta (12). The assumption of this method is the possibility to measure femoral antetorsion with a C-arm. Taking an uninjured femur, the limb is positioned to obtain a perfect lateral view of the knee (overlapping of the posterior condyles). Afterwards, the C-arm is rotated until an axial view of the hip joint is obtained (femoral neck in line with the shaft) (Fig. 2).
Figure 2.
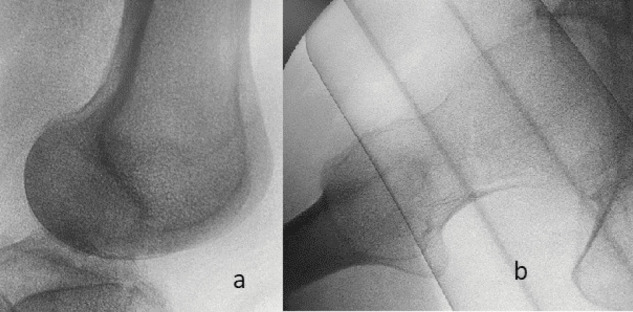
Fluoroscopic image of a perfect lateral view of the knee (a) and axial view of the hip joint (b – in this case with an ipsilateral neck fracture). The degree of rotation of the C-arm to obtain these two images is equivalent to the antetorsion of the femur.
The degree of rotation of the C-arm in relation to a horizontal axis is equivalent to the antetorsion of the femur. Intraoperatively, the antetorsion can be measured in the uninjured side and then reproduced in the fractured femur before nail locking. Even in bilateral femur fractures, one can assume a standard antetorsion of the femur (for example 15°) and then lock the nails with this theoretical antetorsion.
Another method used to check rotation of two fracture stumps is the comparison between the cortical thickness above and below the fracture. Moreover, the difference in diameter between proximal and distal fragments can suggest malrotation, especially where the femur has a different bone cross-section (oval rather than round) (25, 26). An important limitation of this method is that it is only effective in detecting considerable rotational deformity in transverse fractures.
Recent studies based on computer navigation have demonstrated that the injured femur can be accurately locked to match the femoral anteversion of the uninjured side (27, 28): the probability of rotational deformities >15° was significantly reduced thanks to the use of navigation. This method can minimize fluoroscopic requirements, but can be performed only with unilateral femoral shaft fractures (29). However, the disadvantages of this technique are computer instrumentation, software availability and high costs.
In the post-operative period, malrotation can be clinically noted only in a small amount of patients (8, 30). Comparing foot rotation can be difficult, due to concomitant lower limbs injury and the physiological oedema of the thigh that tends to externally rotate the limb. After some days or weeks, the possible malrotation can be better detected (Fig. 3a) and, in a deambulatory patient, the tendence to internally or externally rotate the foot can be noted during walking (31, 32). The patient themselves can complain of the aesthetical aspect of the deformity.
Figure 3.
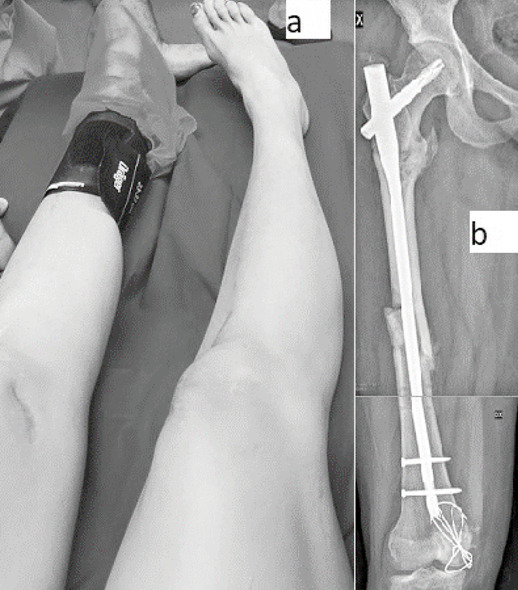
Clinical (a) and radiological (b) picture of internal rotation deformity after IMN of right femur. The deformity can be suspected in plain X-rays – see the position of the patella – (b) and it is obvious with clinical observation (a).
Standard X-rays, both antero-posterior and lateral, are usually acquired after IMN (Fig. 3b). Evaluating only the injured femur is not sufficient to detect a possible rotational deformity; when in doubt of malrotation, a standard antero-posterior X-ray of the pelvis can be done with the feet in neutral rotation, forming a 90° angle with the X-ray table. In case of malrotation, the profile of the lesser trochanters will vary between the two sides (Fig. 4). This exam is very effective, but positioning the patient correctly may be extremely difficult.
Figure 4.
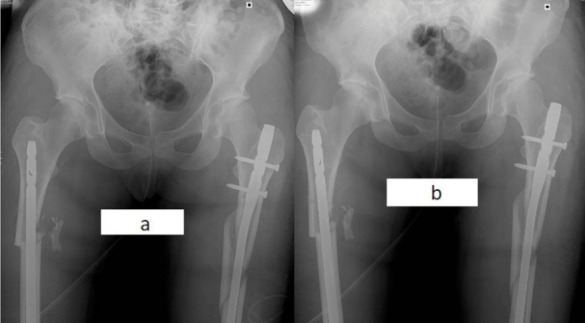
Antero-posterior X-ray of IMN for bilateral femur fracture. a: the patient is supine with feet free to rotate. b: the patient is supine with feet forced in neutral position. A marked difference of the profile of the lesser trochanters can been noted, suggesting a malrotation.
A non-invasive, radiation-free method to detect malrotation is examination with ultrasound, but this is very operator-dependent and poorly reproducible (30, 33).
The most commonly used and accepted exam to assess malrotation is the one described by Jeanmart (34) using CT scans, which consists in acquiring axial cuts at the level of the femoral neck and the femoral condyles. The angle between the axis of the femoral neck and the line tangent to the posterior condyles represents the angle of antetorsion of the femur. This angle can be compared to the uninjured side (even though some anatomic variability between the two femurs is widely accepted) (Fig. 5).
Figure 5.

CT scans with axial cuts at the level of the femoral neck and the femoral condyles. The angle between the two lines (along the femoral neck and tangent to the posterior condyles) in the injured femur (black lines) is compared with the contralateral side (white lines), revealing a possible different rotation (nearly 40° in this case)
Clinical and Subjective Implications of Femur Malrotation
As discussed above, rotational deformity after IMN is the most common form of malunion. Torsional differences <10° are considered normal variations, while differences >15° are considered torsional deformities by some authors (3, 5, 8). Rotational malalignment between 10° and 14° is considered a “controversial zone” by many authors, while Kent (14) defines it a “difficult area” when the deformity is between 15° and 30°, because he believes that a large proportion of people will tolerate this deformity. There is no doubt that a >30° difference of rotation between the femurs can lead, very frequently, to serious complaints (13, 14). Large degrees of malrotation lead to a higher incidence of hip, knee and ankle osteoarthritis (35). The crucial point is what can be considered a symptomatic rotational malalignment of the femoral shaft, with its clinical, objective and subjective implications (8, 30).
Patients with a femur malrotation tend to compensate the deformity by rotating the lumbo-sacral junction, the hip and lower extremity (knee, ankle, foot) on the whole (36). With this compensatory posture, a mild to moderate malrotation could be well tolerated and the patient can be totally asymptomatic. Usually, all the patients compensate even for considerable rotational malalignment while standing and to an even greater extent when walking (32).
Yildirim (31) argues that an external rotation deformity >10° leads to patellofemoral joint symptoms. The patient complains about pain during demanding activities (especially climbing stairs, running and activities stressing the patellofemoral joint).
Karaman (16) reported a retrospective comparative study on 24 monolateral femoral shaft fractures treated with closed antegrade IMN. The femurs were analysed with CT scan and rotational malalignment was determined comparing the injured and the uninjured side. 41.7% of the patients had a rotational malalignment >10° (range 10°-25°) compared to the unaffected side. After analysing Lysholm Score System and WOMAC knee, the scores were significantly worse in patients with rotational malalignment compared to those without. Especially when climbing stairs and doing sports activities, the patients with rotational malalignment complain about anterior knee pain. Increase in mediolateral forces, caused by the torsional deformity of the femur, leads to augmented patellofemoral contact pressure. This abnormally high stress on the articular surface may lead to chondromalacia and, later on, to degenerative arthritis. The author did not find any correlation between the malrotation direction (internal or external) and the patients complains. Some patients even reported hip pain, correlated with a degree of malrotation, while ankle and foot pain were not reported by any patients in the study.
Gugala (32) reported 16 patients enrolled in his study. The femur alignment, analysed by CT scan, revealed internal rotation in five patients (range 3°-13°) and external rotation in eleven patients (range 3°-32°). The patients were asked to fill in a questionnaire measuring patient functional satisfaction with the overall outcomes. There was no statistically significant association between the direction or extent of foot rotational alignment and patient satisfaction. The author observed that external rotation malalignment did appear to be better tolerated than internal malrotation.
Citak (10) reported 24 patients with bilateral femur fractures. Femoral malrotation >15° was detected in 10 cases; in four cases, a revision surgery was required, while the other six patients had no pain nor other subjective symptoms and did not require revision surgery. The conclusions, similar to the ones drawn by Gugala were that, between a certain range of deformity, functional symptoms seem to correlate more with the ability to compensate for the rotational deformity rather than with the entity of the malrotation.
Surgical Correction of a Malrotated Femur
In symptomatic patients with moderate to severe malrotation, once the degree of rotational malalignment of the femur is calculated, the deformity should be corrected. If the deformity is detected soon after surgery, surgical correction should be done as early as possible. If performed immediately, the operation is much easier, because the surgeon can act on a fresh, ununited fracture. Furthermore, the patient has not compensated with hip, knee, ankle and foot posture yet and they have not changed their gait. Otherwise, in delayed cases, the fracture is usually healed and the operation has to be carried out with an extra surgical step (osteotomy of the femur), and changing the fixation device is often required (37).
In acute correction, a safe and relatively easy procedure to address malrotation consists in changing the distal locking screws, leaving the femoral nail in situ (37, 38). The patient is supine on a radiolucent table, with the two legs free and draped. A Shantz screw is inserted into the femur, proximal to the fracture site, and another one is inserted distally. They can be inserted parallel to each other or with different angles; in the latter choice, the degree and direction of rotation of the distal screw is determined by the pre-operative CT scan, representing the angular deformity the surgeon wants to correct. The angle between the screws can be measured with a goniometer or other protractor (for example, the one used for the Maquet tibial osteotomy) (38). The closer these screws are positioned, the easier it is to compare the angle between them. The writing author suggests inserting two extra Kirschner wires, just proximal and distal to the fracture site, in order to better view the different rotation between fracture stumps (Fig. 6a). The distal locking screws are now removed and the femur can be rotated in the direction opposite the deformity. The rotation can be achieved acting on the distal Shantz screw, with the proximal femur maintained still with the other screw. The Shantz screws need to have strong purchase in the bone: the writing author suggests positioning the proximal one in the subtrochanteric region and the distal one just proximal to the metaphysis. When the Shantz screws (or the Kirschner wires) become parallel, the correction is obtained (in case they have been initially positioned with the desired degree of rotation to correct) (Fig. 6b). During correction of rotation, if the backstroke technique has been used during primary nailing, it could be necessary to apply traction to the femur before rotating it, and then compact it again. The correct rotational alignment can be now furthermore checked with a C-arm, comparing the antero-posterior aspect of the lesser trochanter and the lateral view of the knee with the uninjured side, as described above when nailing a fresh femur fracture. The writing author suggests now to connect the two Shantz screws with the bar of an external fixator: this is useful to maintain the correction of the rotation, even if we have to move the limb to better perform the new distal locking (Fig. 6c).
Figure 6.
Surgical correction of malrotated femur in acute phase. a: the proximal K-wire (*) is perpendicular to the femur; the distal K-wire is positioned with an angulation according to the rotation deformity (§). b: acting on the distal Shantz screw, the distal femur is externally rotated, getting the K-wires parallel. c: the bar of an external fixator is positioned to maintain derotation while locking the nail.
Now we can proceed to distal locking with two or more screws. In case of mild to severe malrotation deformity (>25-30°), it is possible to place new distal locking screws through new drill holes without interference from the previous insertion site for the locking screws. In case of correction of malrotation <20° (after thorough discussion with the patient about the real necessity to correct it), the aforementioned risk in distal locking can be overcome by using alternative locking holes (if the nail design allows it) or, alternatively, the nail could be advanced or retracted to avoid the previous screw tracks.
In chronic cases, after positioning the Shantz screw, a lateral approach is required to perform a circumferential osteotomy around the femoral nail (Fig. 7): this can be achieved with a chisel, an oscillating saw or using a Gigli saw. The level of the osteotomy is chosen by the surgeon, while some authors suggest a subtrochanteric osteotomy (39). Once the femur has been derotated, bone graft can be added around the osteotomy site (38).
Figure 7.
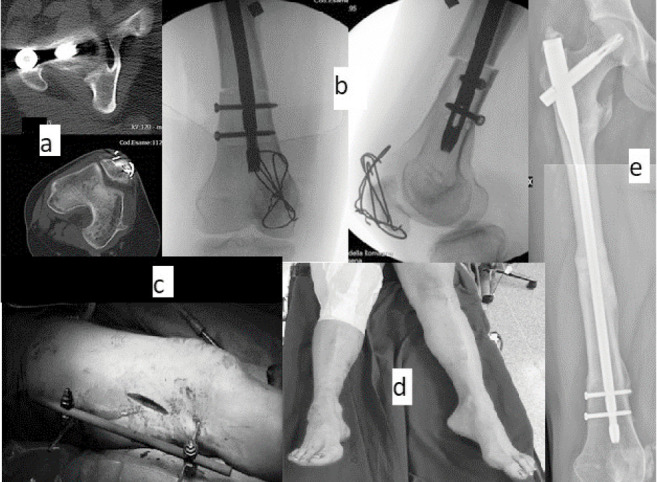
Same clinical case of Fig. 3. Surgical correction of chronic malrotation. a: CT scan revealing 30° of internal rotation. b: fluoroscopy image of the osteotomy and the new distal locking screws. c: lateral approach and external fixator to help maintain the derotation osteotomy. d: clinical appearance at the end of the procedure. e: bone healing three months after surgery.
Other methods to correct rotational deformity have been described; most of them rely on substituting or adding a new fixation device (external fixation, plate and screws, intramedullary devices) (40, 41, 42). In case of removal of the original device, the operation could be technically difficult, leading to major blood loss and requiring extra time. In chronic cases, if the surgeon decides to remove the nail, a transverse osteotomy is performed with an open technique (as discussed before) or with an intramedullary saw; the latter technique reduces the disruption of the periosteal blood supply and aids bone healing (43). After that, the rotational correction is made and a new device positioned (larger nail or plate and screws or external fixator).
Conclusions
Rotational malalignment is very common after closed IMN of the femur. While mild degrees of malrotation are well tolerated by the patient, moderate and severe malrotation can cause pain and disability. After IMN of the femur, it is very difficult to understand if a patient’s complaints are due to a possible malrotation or to other factors connected to the injury. In case malrotation exceeds 30°, it should be addressed as early as possible. The operation has to be discussed accurately with the patient and a CT scan is mandatory to assess the degree of malrotation. Maintaining the nail and exchanging distal locking screws after derotation is the most widely used technique: every step should be carried out thoroughly and a C-arm is fundamental to check the final result.
Conflict of Interest:
Each author declares that he or she has no commercial associations (e.g. consultancies, stock ownership, equity interest, patent/licensing arrangement etc.) might pose a conflict of interest in connection with the submitted article
References
- 1.Bucholz RW, Jones A. Fractures of the shaft of the femur. J Bone Joint Surg Am. 1991;73(10):1561–1566. [PubMed] [Google Scholar]
- 2.Brumback RJ, Virkus WW. Intramedullary nailing of the femur: reamed versus nonreamed. J Am Acad Orthop Surg. 2000;8(2):83–90. doi: 10.5435/00124635-200003000-00002. [DOI] [PubMed] [Google Scholar]
- 3.Wolinsky PR, McCarty E, Shyr Y, Johnson K. Reamed intramedullary nailing of the femur: 551 cases. J Trauma. 1999;46(3):392–399. doi: 10.1097/00005373-199903000-00007. [DOI] [PubMed] [Google Scholar]
- 4.Swanson EA, Garrard EC, Bernstein DT, OʼConnor DP, Brinker MR. Results of a systematic approach to exchange nailing for the treatment of aseptic femoral nonunions. J Orthop Trauma. 2015;29(1):21–27. doi: 10.1097/BOT.0000000000000166. [DOI] [PubMed] [Google Scholar]
- 5.Winquist RA, Hansen ST, Clawson DK. Closed intramedullary nailing of femoral fractures. A report of five hundred and twenty cases. 1984. J Bone Joint Surg Am. 2001;83(12):1912. [PubMed] [Google Scholar]
- 6.Ricci WM, Bellabarba C, Evanoff B, Herscovici D, DiPasquale T, Sanders R. Retrograde versus antegrade nailing of femoral shaft fractures. J Orthop Trauma. 2001;15(3):161–169. doi: 10.1097/00005131-200103000-00003. [DOI] [PubMed] [Google Scholar]
- 7.Langer JS, Gardner MJ, Ricci WM. The cortical step sign as a tool for assessing and correcting rotational deformity in femoral shaft fractures. J Orthop Trauma. 2010;24(2):82–88. doi: 10.1097/BOT.0b013e3181b66f96. [DOI] [PubMed] [Google Scholar]
- 8.Jaarsma RL, Pakvis DF, Verdonschot N, et al. Rotational malalignment after intramedullary nailing of femoral fractures. J Orthop Trauma. 2004;18:403–409. doi: 10.1097/00005131-200408000-00002. [DOI] [PubMed] [Google Scholar]
- 9.Jaarsma RL, Verdonschot N, van der Venne R, et al. Avoiding rotational malalignment after fractures of the femur by using the profile of the lesser trochanter: an in vitro study. Arch Orthop Trauma Surg. 2005;125:184–187. doi: 10.1007/s00402-004-0790-2. [DOI] [PubMed] [Google Scholar]
- 10.Citak M, Suero EM, O’Loughlin PF, et al. Femoral malrotation following intramedullary nailing in bilateral femoral shaft fractures. Arch Orthop Trauma Surg. 2011;131(6):823–827. doi: 10.1007/s00402-010-1245-6. [DOI] [PubMed] [Google Scholar]
- 11.Sennerich T, Sutter P, Ritter G, Zapf S. Computertomographische Kontrolle des Antetorsionswinkels nach Oberschenkelschaftfrakturen des Erwachsenen [Computerized tomography follow-up of the ante-torsion angle after femoral shaft fractures in the adult] Unfallchirurg. 1992;95(6):301–305. [PubMed] [Google Scholar]
- 12.Tornetta P, 3rd, Ritz G, Kantor A. Femoral torsion after interlocked nailing of unstable femoral fractures. J Trauma. 1995;38(2):213–219. doi: 10.1097/00005373-199502000-00011. [DOI] [PubMed] [Google Scholar]
- 13.Gugenheim JJ, Probe RA, Brinker MR. The effects of femoral shaft malrotation on lower extremity anatomy. J Orthop Trauma. 2004;18(10):658–664. doi: 10.1097/00005131-200411000-00002. [DOI] [PubMed] [Google Scholar]
- 14.Kent ME, Arora A, Owen PJ, Khanduja V. Assessment and correction of femoral malrotation following intramedullary nailing of the femur. Acta Orthop Belg. [PubMed] [Google Scholar]
- 15.Thoresen BO, Alho A, Ekeland A, Strømsøe K, Follerås G, Haukebø A. Interlocking intramedullary nailing in femoral shaft fractures. A report of forty-eight cases. J Bone Joint Surg Am. 1985;67(9):1313–1320. [PubMed] [Google Scholar]
- 16.Karaman O, Ayhan E, Kesmezacar H, Seker A, Unlu MC, Aydingoz O. Rotational malalignment after closed intramedullary nailing of femoral shaft fractures and its influence on daily life. Eur J Orthop Surg Traumatol. 2014;24(7):1243–1247. doi: 10.1007/s00590-013-1289-8. [DOI] [PubMed] [Google Scholar]
- 17.Lindsey JD, Krieg JC. Femoral malrotation following intramedullary nail fixation. J Am Acad Orthop Surg. 2011;19(1):17–26. doi: 10.5435/00124635-201101000-00003. [DOI] [PubMed] [Google Scholar]
- 18.Stephen DJ, Kreder HJ, Schemitsch EH, Conlan LB, Wild L, McKee MD. Femoral intramedullary nailing: comparison of fracture-table and manual traction. a prospective, randomized study. J Bone Joint Surg Am. 2002;84(9):1514–1521. doi: 10.2106/00004623-200209000-00002. [DOI] [PubMed] [Google Scholar]
- 19.Reikerås O, Høiseth A, Reigstad A, Fönstelien E. Femoral neck angles: a specimen study with special regard to bilateral differences. Acta Orthop Scand. 1982;53(5):775–779. doi: 10.3109/17453678208992291. [DOI] [PubMed] [Google Scholar]
- 20.Kim JJ, Kim E, Kim KY. Predicting the rotationally neutral state of the femur by comparing the shape of the contralateral lesser trochanter. Orthopedics. 2001;24(11):1069–1070. doi: 10.3928/0147-7447-20011101-18. [DOI] [PubMed] [Google Scholar]
- 21.Park J, Yang KH. Correction of malalignment in proximal femoral nailing--Reduction technique of displaced proximal fragment. Injury. 2010;41(6):634–638. doi: 10.1016/j.injury.2010.01.114. [DOI] [PubMed] [Google Scholar]
- 22.Afsari A, Liporace F, Lindvall E, Jr Infante A, Sagi HC, Haidukewych GJ. Clamp-assisted reduction of high subtrochanteric fractures of the femur. J Bone Joint Surg Am. 2009;91(8):1913–1918. doi: 10.2106/JBJS.H.01563. [DOI] [PubMed] [Google Scholar]
- 23.Ricci WM, Gallagher B, Haidukewych GJ. Intramedullary nailing of femoral shaft fractures: current concepts. J Am Acad Orthop Surg. 2009;17(5):296–305. doi: 10.5435/00124635-200905000-00004. [DOI] [PubMed] [Google Scholar]
- 24.Hilgert RE, Ohrendorf K, Schäfer FK, et al. Bildwandlergestützte Vermeidung einer Torsionsabweichung zur Gegenseite bei der Oberschenkelmarknagelung [Preventing malrotation during intramedullary nailing of femoral fractures] Unfallchirurg. 2006;109(10):855–861. doi: 10.1007/s00113-006-1093-6. [DOI] [PubMed] [Google Scholar]
- 25. Ao surgery reference: https://surgeryreference.aofoundation.org/orthopedic-trauma/adult-trauma/femoral-shaft/simple-transverse-middle-1-3-fractures/antegrade-nailing .
- 26.Langer JS, Gardner MJ, Ricci WM. The cortical step sign as a tool for assessing and correcting rotational deformity in femoral shaft fractures. J Orthop Trauma. 2010;24(2):82–88. doi: 10.1097/BOT.0b013e3181b66f96. [DOI] [PubMed] [Google Scholar]
- 27.Gösling T, Oszwald M, Kendoff D, Citak M, Krettek C, Hufner T. Computer-assisted antetorsion control prevents malrotation in femoral nailing: an experimental study and preliminary clinical case series. Arch Orthop Trauma Surg. 2009;129(11):1521–1526. doi: 10.1007/s00402-009-0871-3. [DOI] [PubMed] [Google Scholar]
- 28.Khoury A, Liebergall M, Weil Y, Mosheiff R. Computerized fluoroscopic-based navigation-assisted intramedullary nailing. Am J Orthop (Belle Mead NJ) 2007;36(11):582–585. [PubMed] [Google Scholar]
- 29.Kendoff D, Citak M, Gardner MJ, Gösling T, Krettek C, Hüfner T. Navigated femoral nailing using noninvasive registration of the contralateral intact femur to restore anteversion. Technique and clinical use. J Orthop Trauma. 2007;21(10):725–730. doi: 10.1097/BOT.0b013e31812f69a9. [DOI] [PubMed] [Google Scholar]
- 30.Bråten M, Terjesen T, Rossvoll I. Torsional deformity after intramedullary nailing of femoral shaft fractures. Measurement of anteversion angles in 110 patients. J Bone Joint Surg Br. 1993;75(5):799–803. doi: 10.1302/0301-620X.75B5.8376444. [DOI] [PubMed] [Google Scholar]
- 31.Yildirim AO, Aksahin E, Sakman B, et al. The effect of rotational deformity on patellofemoral parameters following the treatment of femoral shaft fracture. Arch Orthop Trauma Surg. 2013;133(5):641–648. doi: 10.1007/s00402-013-1705-x. [DOI] [PubMed] [Google Scholar]
- 32.Gugala Z, Qaisi YT, Hipp JA, Lindsey RW. Long-term functional implications of the iatrogenic rotational malalignment of healed diaphyseal femur fractures following intramedullary nailing. Clin Biomech (Bristol, Avon) 2011;26(3):274–277. doi: 10.1016/j.clinbiomech.2010.11.005. [DOI] [PubMed] [Google Scholar]
- 33.Kh Salem, Maier D, Keppler P, Kinzl L, Gebhard F. Limb malalignment and functional outcome after antegrade versus retrograde intramedullary nailing in distal femoral fractures. J Trauma. 2006;61:375–381. doi: 10.1097/01.ta.0000230282.65606.81. [DOI] [PubMed] [Google Scholar]
- 34.Jeanmart L, Baert AL, Wackenheim A. Atlas of Pathological Computer Tomography. Vol. 3. Springer, Berlin, Heidelberg, New York; Computer Tomography of Neck, Chest, Spine and Limbs; pp. 171–177. [Google Scholar]
- 35.Eckhoff DG. Effect of limb malrotation on malalignment and osteoarthritis. Orthop Clin North Am. 1994;25(3):405–414. [PubMed] [Google Scholar]
- 36.Jaarsma RL, Ongkiehong BF, Grüneberg C, Verdonschot N, Duysens J, van Kampen A. Compensation for rotational malalignment after intramedullary nailing for femoral shaft fractures. An analysis by plantar pressure measurements during gait. Injury. 2004;35(12):1270–1278. doi: 10.1016/j.injury.2004.01.016. [DOI] [PubMed] [Google Scholar]
- 37.Sloan Matthew MD, MS, Lim Daniel MD, Mehta Samir MD. Femoral Derotation for the Acutely Malrotated Femur Following Intramedullary Nail Fixation, Techniques in Orthopaedics. January 16, 2019 [Google Scholar]
- 38.Jagernauth S, Tindall AJ, Kohli S, Allen P. New Technique: A Novel Femoral Derotation Osteotomy for Malrotation following Intramedullary Nailing. Case Rep Orthop. doi: 10.1155/2012/837325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Samuel AW. Malrotation of the femur after intramedullary nailing. Injury. 1996;27(6):438–440. doi: 10.1016/0020-1383(96)00047-2. [DOI] [PubMed] [Google Scholar]
- 40.Brinker MR, Gugenheim JJ, O’Connor DP, London JC. Ilizarov correction of malrotated femoral shaft fracture initially treated with an intramedullary nail: a case report. Am J Orthop (Belle Mead NJ) 2004;33(10):489–493. [PubMed] [Google Scholar]
- 41.Chiodo CP, Jupiter JB, Alvarez G, Chandler HP. Oblique osteotomy for multiplanar correction of malunions of the femoral shaft. Clin Orthop Relat Res. 2003;(406):185–194. doi: 10.1097/01.blo.0000038042.63743.d6. [DOI] [PubMed] [Google Scholar]
- 42.Winquist RA. Closed intramedullary osteotomies of the femur. Clin Orthop Relat Res. 1986;(212):155–164. [PubMed] [Google Scholar]
- 43.Stahl JP, Alt V, Kraus R, Hoerbelt R, Itoman M, Schnettler R. Derotation of post-traumatic femoral deformities by closed intramedullary sawing. Injury. 2006;37(2):145–151. doi: 10.1016/j.injury.2005.06.042. [DOI] [PubMed] [Google Scholar]


