Abstract
Introduction:
Although GLAD lesions are quite common, only sporadic case reports describe surgical techniques and clinical outcomes. Even if cartilage defects can result from various pathogenic mechanisms, the resulting defect has some similarities with GLAD, and its management can be a starting point to treat both types of lesion. Aim of the present study is to find a commonly accepted definition for GLAD lesions in order to understand its pathogenesis, diagnosis and possible treatments.
Methods:
A search of PubMed (MEDLINE) database has been performed in June 2020 to identify relevant articles including a combination of the following search terms: “GlenoLabral Articular Disruption” OR “GLAD” AND “shoulder” AND “cartilage, articular”.
Results:
Abstract evaluation included 31 articles in the full-text review. Various studies showed that the performance of MR arthrography in the detection of glenohumeral cartilage lesions, including GLAD lesions, was moderate. Different therapeutic solutions have been described. Arthroscopic debridement of the lesion and reattachment of the labrum have been often used. In case of large articular defects, the labrum could be advanced in the cartilage defect to cover it. In case of cartilage flap with reparable margins, this could be reattached with different suture constructs. Neglected GLAD lesions following a chronic trauma or shoulder instability have not been described in literature.
Conclusions:
The definition of GLAD injury has changed over the time. Many authors associate this lesion with shoulder instability, with trauma in abduction and extra rotation, while Neviaser’s original definition described stable shoulders following a trauma in adduction.(www.actabiomedica.it)
Keywords: GLAD, cartilage defects, GlenoLabral Articular Disruption
Introduction
The GlenoLabral Articular Disruption (GLAD) lesion [1] was originally described in 1993 by Neviaser as a traumatic glenoid cartilage lesion, characterized by anterior shoulder pain and no sign of anterior instability on physical examination or at surgery.
Afterwards, the definition of GLAD lesion developed into a different anatomopathological entity and its pathogenesis and clinical presentation has changed [2]. Various authors [3-5] recognized GLAD lesions in patients which underwent an abduction and external rotation trauma of the arm or an episode of dislocation.
GLAD lesions and similar cartilage injuries of the anteroinferior portion of the glenoid are not a rare finding, but in literature there is still a paucity of evidences and only low-level studies.
Although GLAD lesions are quite common, only sporadic case reports have been published to describe surgical techniques and clinical outcomes. Furthermore, the management of glenoid cartilage articular defects have been subject of study for years. Even if cartilage defects can result from various pathogenic mechanisms, the resulting defect has some similarities with GLAD, and its management can be a starting point to treat both types of lesion.
Aim of the present study is to find a commonly accepted definition for GLAD lesions, in order to understand its pathogenesis, diagnosis and possible treatments.
Materials and Methods
A search of PubMed (MEDLINE) database has been performed in June 2020 to identify relevant articles in this field of research in English Language, according to the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines (Fig. 1) [6]. Additionally, the reference lists of the identified studies were checked for other suitable studies. The search strategy in PubMed included a combination of the following search terms: “GlenoLabral Articular Disruption” OR “GLAD” AND “shoulder” AND “cartilage, articular”. To identify every possible relevant article through database the “results by year” filter was used.
Figure 1.
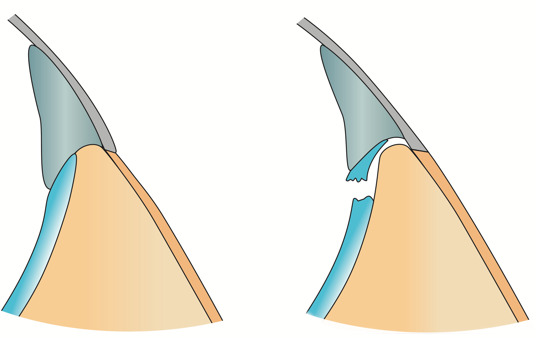
In this schematic illustration the typical characteristics of the GLAD lesion are clearly evident: labral tear, deep fibers of the anterior inferior glenohumeral ligament attached to glenoid and labrum and an anteroinferior cartilage damage of varying degrees.
Results
Study Characteristics
The literature search yielded 299 abstracts for consideration. After removal of duplicates, 291 articles were considered. Abstract evaluation included 31 articles in the full-text review (Table 1). Seven articles were focused on diagnostics, two articles were systematic reviews, eight were focused on the treatment of cartilage defects of the shoulder. Only six articles had GLAD lesions as their main topic. Each of the reviewed studies was classified as having level IV evidence (Table 2).
Table 1.
Prisma Flow Diagram for study selection
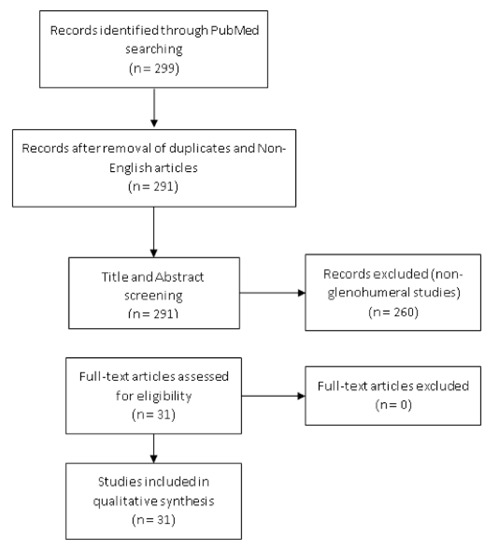 |
Table 2.
Studies included, with description of pathogenic mechanism, type of lesion and therapeutic approach.
| Author | Study | Pathogenic Mechanism | Type of Lesion | Treatment |
| Neviaser (1993) | The GLAD Lesion: Another Cause of Anterior Shoulder Pain | Forced adduction from an abducted and external rotated position | GLAD | Debridement of labral tear, glenoid articular chondroplasty or abrasion arthroplasty |
| Sanders et al. (1998) | The Glenolabral Articular Disruption Lesion: MR Arthrography with Arthroscopic Correlation | Forced adduction from an abducted and external rotated position | GLAD | |
| Amrami et al. (2002) | Radiologic case study. Glenolabral articular disruption (GLAD) lesion | Abduction and external rotation, anterior dislocation and recurrent instability | GLAD | Lateral repair and capsular shift |
| Singh et al. (2003) | MRI of Shoulder Instability: State of the Art | Fall on adducted shoulder | GARD | |
| Waldt et al. (2005) | Anterior Shoulder Instability: Accuracy of MR Arthrography in the Classification of Anteroinferior Labroligamentous Injuries | Instability and impaction of the humeral head against the glenoid | GLAD | |
| Antonio et al. (2007) | First-Time Shoulder Dislocation: High Prevalence of Labral Injury and Age Related Differences revealed by MR Arthrography | First anterior shoulder dislocation | GLAD | |
| Page et al. (2010) | Arthroscopic repair of a chondrolabral lesion associated with anterior glenohumeral dislocation | Shoulder dislocation | GLAF | Reconstruction of the labrum and suture of the cartilage flap |
| O’Brien et al. (2012) | Frequency of glenoid chondral lesions on MR arthrography in patients with anterior shoulder instability | Anterior shoulder instability | GLAD | |
| Galano et al. (2013) | Articular Shear of the Anterior-Inferior Quadrant of the Glenoid: A Glenolabral Articular Disruption Lesion Variant | Shoulder subluxation | GLAD variant | Bankart repair, one removal of the cartilage and microfractures, one suture of the cartilage flap |
| Zhu et al. (2013) | Arthroscopic findings in the recurrent anterior instability of the shoulder | Recurrent anterior shoulder dislocation | GLAD | |
| Lederman et al. (2018) | The Glenoid Labral Articular Teardrop Lesion: A Chondrolabral Injury With Distinct Magnetic Resonance Imaging Findings | 67% of patients had sustained an episode of instability | GLAT | |
| Pogorzelski et al. (2018) | Failure following arthroscopic Bankart repair for traumatic anteroinferior instability of the shoulder: is a glenoid labral articular disruption (GLAD) lesion a risk factor for recurrent instability? | Shoulder instability | GLAD | Debridement of cartilage defect, microfractures and advancement of Bankart repair into the defect |
| Agarwalla et al. (2019) | Concurrent Primary Repair of a Glenoid Labrum Articular Disruption and a Bankart Lesion in an Adolescent: A Case Report of a Novel Technique | Shoulder dislocation | GLAD | Suture of labrum and cartilage flap |
| 13 Studies | At least 4 different mechanisms | 5 Variants | Not a unique treatment |
Pathogenesis and evolution of the definition
The original GLAD lesion described by Neviaser [1] consisted of a superficial anterior inferior labral tear, usually with an inferior-based flap tear, deep fibers of the anterior inferior glenohumeral ligament attached to glenoid and labrum and an anteroinferior cartilage damage of varying degrees, occasionally down to subchondral bone (Figure 1). This lesion resulted following an acute trauma by an adduction force across the chest from an abducted and externally rotated position of the arm.
In 1999 Sanders et al. [7] defined Magnetic Resonance (MR) as a reliable diagnostic methodology for GLAD lesions. Patients examined presented clinically stable shoulders, persistent pain and superficially torn anteroinferior labrum.
In 2002, a radiologic study of Amrami et al. [2] described the GLAD lesion as a source of shoulder instability and pain. From this moment on, GLAD lesions have always been considered as associated with shoulder instability, considering shoulder dislocation as one of the main mechanisms of acute pathogenesis [3-5,8-10].
A recent description [5] of the simple GLAD lesion defined it as an intra-articular damage in the anteroinferior glenoid without periosteum damage, with labrum detachment and the anchor point for the inferior glenohumeral ligament intact. In the same paper, authors described the association between hyperlaxity of the patient and the risk of developing a GLAD lesion following an episode of shoulder instability.
In a case report, Page et al. [4] described a dual-lesion complex that involved an avulsion of the anteroinferior glenoid labrum and a flap tear of the adjacent articular cartilage [glenoid labral tear and articular cartilage flap (GLAF) lesion]. The articular flap tear involved a large region of the anterior half of the lower glenoid cartilage. This type of lesion derived from an anterior shoulder dislocation and at 7 weeks of follow-up, the patient complained positive apprehension test and clicks during weight lifting. After consideration of the large size and stability of the chondral flap, it was attempted a repair of the flap and a reconstruction of the anteroinferior labral tear. Authors also considered the possibility of excision of articular flap and microfractures, but the size of the resulting defect discouraged the attempt.
In a previous study [8], a Glenoid Articular Rim Divot (GARD) lesion was described in a young patient after a fall on adducted shoulder. This lesion, similarly to GLAF lesion, consisted in an anteroinferior chondral flap. The traumatic mechanism and the association with instability that was present in GLAF lesion and absent in GARD represented the main difference between them.
In a case series [11], Lederman et al. described another variant of chondrolabral injury, the glenoid labral articular teardrop (GLAT) lesion. This lesion had the teardrop appearance of a pedicled displaced chondrolabral flap in the axillary recess on coronal imaging. The GLAT lesion could be found in shoulder MR of 36 retrospectively reviewed patients. Only 67% of the patients had previously sustained an episode of instability or had a clinically unstable shoulder. Therefore, the authors described this new pathognomonic lesion in MR, but no data are available regarding the pathogenesis. Authors performed arthroscopic treatment in 9 patients, 1 debridement, 8 Bankart repair and in 4 of them the labrum was advanced into the defect in order to cover it.
Diagnosis
According to Neviaser [1], the relief of pain with intraarticular injection of lidocaine without the presence of a rotator cuff tear or biceps tendinitis is suggestive but not diagnostic of a GLAD lesion. The author also considered difficult to diagnose a GLAD with CT of MRI.
In a 2011 study, O’Brien et al. [9] retrospectively analysed MR arthrogram association between Hills Sachs (HS) lesions and glenoid chondral abnormalities in patients with clinical anterior shoulder instability. Of 101 patients, 72% had anterior labral injury and 36% had glenoid chondral defects. Furthermore, 46% of HS patients presented a glenoid chondral defect. Interobserver variability for the presence of labral and chondral lesions was 0.965 and 0.858 respectively. This result underlines the specificity of MR arthrogram for the diagnosis of glenoid cartilage defect, but further studies are needed to determine sensitivity of this method. The diagnostic effectiveness of MR arthrography to detect cartilage lesions was reported to be moderate in another study [12].
In a retrospective study of 2005 [13], authors studied the accuracy of MR Arthrography in the classification of anteroinferior labroligamentous injuries of unstable shoulders. Of 104 arthroscopically confirmed diagnoses, only three presented a GLAD lesion. One of them was following an episode of acute instability, while the other two followed chronic instability. In this study, given the poor number of GLAD lesions, the sensitivity and specificity of MR Arthrogram resulted at 100% value. According to authors, the number of GLAD lesions was underrepresented in this series of patients with anterior shoulder instability, since patients with GLAD lesions usually do not show instability of the glenohumeral joint. All the 23 nonclassifiable lesions occurred in patients with a history of chronic instability.
Interobserver agreement in the diagnosis of humeral and glenoid cartilage lesions was well established in a paper by Guntern et al. [12]. MR arthrography of 52 pathologic shoulders showed that sensitivity for glenoidal cartilage lesions was 75% and 75% for the two radiologists, specificity was 66% and 63%, and accuracy was 67% and 65%. Every lesion was confirmed and graded with shoulder arthroscopy. Authors concluded that the performance of MR arthrography in the detection of glenohumeral cartilage lesions is moderate.
Acute and chronic cartilage lesions in shoulder instability
In a study of 40 patients who received a Bankart repair [14], 20 of which had an underlying glenoid defect, there was 15% recurrent dislocation rate in the cohort with an underlying glenoid defect versus 0% in the control group with no underlying lesion. The final Rowe score decreased significantly as the size of the glenoid defect increased.
In a systematic review by Ruckstuhl et al. [15] there was a 57% incidence of glenoid cartilage lesions in unstable shoulders, including all lesions due to both acute trauma and chronic degeneration. Authors found only few reports on post-traumatic GH cartilage lesions without bony lesions, showing that this type of shoulder pathology is not prevalent. Furthermore, this study concluded that glenohumeral cartilage lesions caused by an acute trauma are rare, and they are mostly caused by chronic traumas, associated with shoulder instability, rotator cuff injury or impingement syndrome.
Zhu et al. [5] studied arthroscopically 31 patients with recurrent anterior shoulder dislocation and they were divided in a hyper-laxity group and a trauma group. All the patients suffered from anteroinferior labrum injury, but only 3 of them presented a GLAD lesion. Every GLAD patient was in the hyperlaxity group. However, in this study 29,4% of hyperlaxity group and 78,6% of trauma group presented some form of “cartilage damage of anteroinferior glenoid cavity” associated with any type of anteroinferior labrum injury. This data confirmed that lax patients have a lower risk of cartilage damage but seem to have a statistically significant higher risk of GLAD lesion.
Treatment of GLAD lesions
Management of GLAD lesions is based on restoring articular surface by debriding chondral tissue and removing loose bodies from the glenohumeral joint space. The repair of labral injury is mandatory for shoulder stability. Decision making is usually defined by the dimension of articular defect. A small articular flap can be debrided, and the labrum can be advanced into the defect. Eventually, in case of a large defect, the articular surface is debrided, and the defect can be left unfilled [16].
Pogorzelski et al. [17] in a retrospective case series of 72 patients studied the possible causes of failure after arthroscopic Bankart repair. In 10 cases of failure, 30% were patients with GLAD lesion, showing that GLAD is a statistically significant factor associated with failure of surgical treatment. In this case series, GLAD lesions were treated with debridement of margins, microfractures of subchondral bone and advancement of the repaired labrum to partially cover the cartilage defect. In 7 cases of GLAD lesion, 3 (42,8%) resulted in clinical failure.
An association between knee meniscectomy and increased risk of developing osteoarthritis [18] has been described. A direct association between glenohumeral articular defect or GLAD and the risk of osteoarthritis has not been established, yet. However, the same principle influences the management of these lesions of the shoulder, especially in young patients.
Various studies reported different approaches in restoring articular surface. Galano et al. [10] described two cases of GLAD-like articular damage associated with anteroinferior Bankart and SLAP tear in 15-years old sportive patients. The two extensive shear lesions of the glenoid cartilage were treated differently. In the first case the GLAD-like flap was considered unstable, it was removed and microfractures were associated with Bankart repair in “standard fashion”. In the second case the articular flap was considered reparable and it was reattached using a cartilage fixation device (SmartNail PLA 1.5 mm x 25 mm, ConMed Linvatec, Largo, Florida). In both cases the results were reported as satisfactory with full painless range of motion. In both cases shoulders were unstable preoperatively and showed anterior apprehension.
Page and Bathia [4] described a technique in which the labral tissue was overlapped with the chondral edge to provide stability to the articular lesion.
In a recent case report [19], authors described a hybrid technique that simultaneously performed a primary repair of both labral and articular injuries without the use of additional implants for the articular lesion. Suture was used to imbricate capsular tissue, passed beneath the labrum, and was subsequently advanced through the GLAD lesion. According to authors, this construct restored tension to the anterior band of the inferior glenohumeral ligament, recreated the anteroinferior labral bumper, and effectively reduced the cartilage flap to the anterior inferior glenoid.
Treatment of cartilage defects
Currently, no consensus exists regarding the treatment of articular cartilage defects. No studies assessed the clinical outcomes of nonsurgical interventions in patients with chondral defects of the glenohumeral joint [20]. Nonsurgical treatment options include NSAIDs, physical therapy, corticosteroid injections, and viscosupplementation. Operative management includes chondral debridement, techniques of chondral repair and microfractures.
In Literature most studies described attempts to stimulate a cartilage repair of the glenoid articular surface with microfractures. A study from McCarty III et al. [21] represented a first attempt to establish a flow-chart for the treatment of articular defects of the shoulder. In this paper, the pathogenesis of articular defects is not described for all cases but, since most of the treated shoulder present concomitant Hill Sachs lesions, it is conceivable that most of them are related to shoulder instability.
Microfracture technique has been successfully adopted to stimulate a growth factors inflow from the subchondral bone in full thickness cartilage defects [21,22]. Millet et al. [22], in a case series with a mean follow-up of 47 months, reported a mean of 20 points of improvement in ASES Score and a failure rate of 19% (6 of 31 shoulders). Of the 6 cases of failure, 3 underwent Total Shoulder Arthroplasty and the mean time from the microfracture procedure to reoperation on the index shoulder averaged 35 months (range, 6 to 66 months).
Similarly, Frank et al. [23] reported, in a retrospective study, a statistically significant decrease in VAS and improvements in SST and ASES Score in patients with full-thickness cartilage defects treated with microfracture of glenoid and humeral head. However, authors excluded from the study patients with concomitant labral tears, thus excluding an important source of pain and shoulder instability.
At 10-years of follow-up, authors reported clinical of microfracture technique [24]. Results were positive, showing reduction of pain and improved function for come patients. However, 21,4% of patients required conversion to arthroplasty in less than 10 years, and 33% to 42% of patients could have potential clinical failure.
The same study group in 2014 [25] focused attention on focal glenoid cartilage defects in younger patients. Authors described an arthroscopic technique which consisted in debridement of chondral defect, microfracture and subsequent implantation of a micronized allogeneic cartilage scaffold enriched with platelet-rich plasma. No data regarding clinical or radiological results were reported in this paper.
In 2015 Wang et al. [26] studied in a rabbit shoulder model radiologic and histologic results of microfracture alone and microfracture associated with autologous matrix-induced chondrogenesis (AMIC). At 32 weeks, the T2 index (ratio of T2 values of healing to intact glenoids) was significantly lower for the microfracture group relative to the AMIC group. However, histologic investigation suggested inferior healing in the AMIC group relative to the microfracture group, which exhibited improvements in integration of repair tissue with subchondral bone over time. Thus, authors concluded that improvements conferred by AMIC were limited to magnetic resonance imaging outcomes, whereas microfractures appeared to promote increased fibrous tissue deposition and more hyaline-like repair.
Various case reports and case series have been published to describe surgical technique and early results of osteochondral autograft transplantation [27,28], fresh osteochondral allograft transplantation [29,30], autologous chondrocyte implantation [31,32], but these techniques have not been routinely adopted.
Discussion
Although the original definition attributed GLAD lesions to adduction trauma with no shoulder instability [1], it is currently necessary to modify the definition of this type of lesion. Multiple authors have described GLAD lesions following acute trauma associated with shoulder instability and dislocations [3-5,8-10]. Furthermore, no reports exist describing an isolated cartilage defect without associated lesions, since any patient is unlikely to undergo arthroscopy exclusively for a cartilage injury.
In current literature there is little evidence of reports regarding chronic GLAD lesions (Figure 2). The work of Pogorzelski [17] is the first description of GLAD as a cause of recurrent instability. This draws attention to all cases of instability following undiagnosed or not treated of the GLAD, with exclusive treatment of the labrum. In the previously described work by Zhu et al. [5], GLAD lesions followed recurrent instability in patients with congenital laxity and no patient belonged to the trauma group. However, authors did not describe arthroscopic anatomy of this kind of chronic lesions. These studies confirm the existence of chronic GLAD, but the difference in terms of treatment remains unclear.
Figure 2.
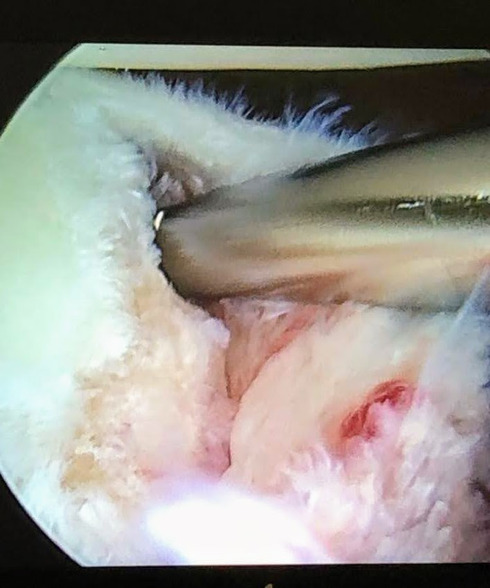
Antero-superior portal arthroscopic image showing an avulsion of the labrum with detachment of a large cartilage fragment. The degenerative aspect of the cartilage and labrum highlights a chronic GLAD lesion.
Various studies have described MR Arthrography as a reliable method with moderate specificity for the diagnosis of GLAD lesions [9,12,13]. Actually, these studies have quite limited patient cohorts. In addition, the reported sensitivity and specificity were approximately 60%, which means that about 4 out of 10 patients did not receive a complete diagnosis. As described by these findings, it is quite common to find a GLAD lesion during arthroscopic surgery without a previous diagnosis, with the sudden need to change the operative planning. In addition, in clinical practice simple shoulder MR is widely used as the only imaging performed after physical examination. This leads to undiagnosed lesions that developed in chronic lesion, remaining symptomatic for a long time and worsening the cartilage damage.
Therefore, it is necessary to clarify that GLAD lesions may be secondary to chronic trauma or instability. In this case, the pathological anatomy and pathogenesis are different from the acute ones. The arthroscopic aspect of these chronic lesions shows chronic cartilage degeneration, such as the sliding of the cartilage fibers and margins remodelling. Consequently, the treatment of chronic lesions may also differ from that of acute GLAD, even if this has not been described in literature.
Authors of the present study have treated arthroscopically, over the past 15 years, 600 shoulder instabilities. In 30 cases (5%) a GLAD-like injury was found. The treatment of the acute lesions consisted in margins debridement and subsequent suture of the labrum. This type of surgery allows a good healing of the cartilage and a restoration of the articular surface. Chronic GLAD lesions need further treatment, which can be represented by an advance in labrum repair to cover the cartilage defect. In extensive injuries, the advancement of labrum can influence negatively the range of motion of the shoulder. Very extensive or chronic GLAD lesions can be assimilated to cartilage defects, and therefore must be treated like the latter. In case of wide cartilage defects, authors usually associate microfractures to the labrum repair. Finally, some very wide cartilage defects (>2cm2) required a matrix assisted autologous bone marrow mesenchymal stem cells implant to cover the loss of glenoid cartilage.
The risk of developing osteoarthritis should be another subject for future studies. On the one hand, a shoulder that remained unstable after treatment can favour osteoarthritis; on the other, a stiff shoulder after excessive advancement of labrum repair in an attempt to cover the GLAD lesion can also represent a cause of shoulder osteoarthritis.
Conclusions
Further clinical studies are needed to better understand the pathogenesis, diagnosis and best treatment options for GLAD lesions. Neviaser’s historical definition must be reviewed and re-evaluated in the light of the new arthroscopic knowledge that has highlighted a whole series of associated lesions ranging from Bankart lesion to GLAF, GLAT, capsular lesions and others. It is necessary to understand if the GLAD lesion can be the primum movens of the whole spectrum of lesions, causing anterior shoulder pain in the absence of instability and if a small cartilage lesion can cause such an intense pain that induced the patient to undergo surgery. Based on current studies, it is possible to suggest that in the past therapies focused primarily on treating lesions associated with GLAD, rather than on GLAD itself.
References
- 1.Neviaser TJ. The GLAD lesion: Another cause of anterior shoulder pain. Arthroscopy: The Journal of Arthroscopic & Related Surgery. 1993;9(1):22–23. doi: 10.1016/s0749-8063(05)80339-1. doi: 10.1016/S0749-8063(05)80339-1. [DOI] [PubMed] [Google Scholar]
- 2.Amrami KK, Sperling JW, Bartholmai BJ, Sundaram M. Radiologic case study. Glenolabral articular disruption (GLAD) lesion. Orthopedics. 2002;25(1):29–95-96. doi: 10.3928/0147-7447-20020101-11. [DOI] [PubMed] [Google Scholar]
- 3.Antonio GE, Griffith JF, Yu AB, Yung PSH, Chan KM, Ahuja AT. First-time shoulder dislocation: High prevalence of labral injury and age-related differences revealed by MR arthrography. J Magn Reson Imaging. 2007;26(4):983–991. doi: 10.1002/jmri.21092. doi: 10.1002/jmri.21092. [DOI] [PubMed] [Google Scholar]
- 4.Page R, Bhatia DN. Arthroscopic repair of a chondrolabral lesion associated with anterior glenohumeral dislocation. Knee Surg Sports Traumatol Arthrosc. 2010;18(12):1748–1751. doi: 10.1007/s00167-010-1095-3. doi: 10.1007/s00167-010-1095-3. [DOI] [PubMed] [Google Scholar]
- 5.Zhu W, Lu W, Zhang L, et al. Arthroscopic findings in the recurrent anterior instability of the shoulder. Eur J Orthop Surg Traumatol. 2014;24(5):699–705. doi: 10.1007/s00590-013-1259-1. doi: 10.1007/s00590-013-1259-1. [DOI] [PubMed] [Google Scholar]
- 6.Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement | Systematic Reviews | Full Text. Accessed July 16, 2020. https://systematicreviewsjournal.biomedcentral.com/articles/10.1186/2046-4053-4-1 . [DOI] [PMC free article] [PubMed]
- 7.Sanders TG, Tirman PF, Linares R, Feller JF, Richardson R. The glenolabral articular disruption lesion: MR arthrography with arthroscopic correlation. American Journal of Roentgenology. 1999;172(1):171–175. doi: 10.2214/ajr.172.1.9888763. doi: 10.2214/ajr.172.1.9888763. [DOI] [PubMed] [Google Scholar]
- 8.Singh RB, Hunter JC, Smith KL. Mri of shoulder instability: state of the art. Current Problems in Diagnostic Radiology. 2003;32(3):127–134. doi: 10.1016/s0363-0188(03)00014-8. doi: 10.1016/S0363-0188(03)00014-8. [DOI] [PubMed] [Google Scholar]
- 9.O’Brien J, Grebenyuk J, Leith J, Forster BB. Frequency of glenoid chondral lesions on MR arthrography in patients with anterior shoulder instability. European Journal of Radiology. 2012;81(11):3461–3465. doi: 10.1016/j.ejrad.2012.05.013. doi: 10.1016/j.ejrad.2012.05.013. [DOI] [PubMed] [Google Scholar]
- 10.Galano GJ, Weisenthal BM, Altchek DW. Articular Shear of the Anterior-Inferior Quadrant of the Glenoid: A Glenolabral Articular Disruption Lesion Variant. :3. [PubMed] [Google Scholar]
- 11.Lederman ES, Flores S, Stevens C, Richardson D, Lund P. The Glenoid Labral Articular Teardrop Lesion: A Chondrolabral Injury With Distinct Magnetic Resonance Imaging Findings. Arthroscopy: The Journal of Arthroscopic & Related Surgery. 2018;34(2):407–411. doi: 10.1016/j.arthro.2017.08.236. doi: 10.1016/j.arthro.2017.08.236. [DOI] [PubMed] [Google Scholar]
- 12.Guntern DV, Pfirrmann CWA, Schmid MR, et al. Articular cartilage lesions of the glenohumeral joint: diagnostic effectiveness of MR arthrography and prevalence in patients with subacromial impingement syndrome. Radiology. 2003;226(1):165–170. doi: 10.1148/radiol.2261012090. doi: 10.1148/radiol.2261012090. [DOI] [PubMed] [Google Scholar]
- 13.Waldt S, Burkart A, Imhoff AB, Bruegel M, Rummeny EJ, Woertler K. Anterior Shoulder Instability: Accuracy of MR Arthrography in the Classification of Anteroinferior Labroligamentous Injuries. Radiology. 2005;237(2):578–583. doi: 10.1148/radiol.2372041429. doi: 10.1148/radiol.2372041429. [DOI] [PubMed] [Google Scholar]
- 14.Rhee YG, Lim CT. Glenoid defect associated with anterior shoulder instability: results of open Bankart repair. Int Orthop. 2007;31(5):629–634. doi: 10.1007/s00264-006-0234-4. doi: 10.1007/s00264-006-0234-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ruckstuhl H, de Bruin ED, Stussi E, Vanwanseele B. Post-traumatic glenohumeral cartilage lesions: a systematic review. BMC Musculoskelet Disord. 2008;9(1):107. doi: 10.1186/1471-2474-9-107. doi: 10.1186/1471-2474-9-107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Elser F, Braun S, Dewing CB, Millett PJ. Glenohumeral Joint Preservation: Current Options for Managing Articular Cartilage Lesions in Young, Active Patients. Arthroscopy: The Journal of Arthroscopic & Related Surgery. 2010;26(5):685–696. doi: 10.1016/j.arthro.2009.10.017. doi: 10.1016/j.arthro.2009.10.017. [DOI] [PubMed] [Google Scholar]
- 17.Pogorzelski J, Fritz EM, Horan MP, Katthagen JC, Provencher MT, Millett PJ. Failure following arthroscopic Bankart repair for traumatic anteroinferior instability of the shoulder: is a glenoid labral articular disruption (GLAD) lesion a risk factor for recurrent instability? Journal of Shoulder and Elbow Surgery. 2018;27(8):e235–e242. doi: 10.1016/j.jse.2018.02.055. doi: 10.1016/j.jse.2018.02.055. [DOI] [PubMed] [Google Scholar]
- 18.Englund M, Lohmander LS. Risk factors for symptomatic knee osteoarthritis fifteen to twenty-two years after meniscectomy. Arthritis & Rheumatism. 2004;50(9):2811–2819. doi: 10.1002/art.20489. doi: 10.1002/art.20489. [DOI] [PubMed] [Google Scholar]
- 19.Agarwalla A, Puzzitiello RN, Leong NL, Forsythe B. Concurrent Primary Repair of a Glenoid Labrum Articular Disruption and a Bankart Lesion in an Adolescent: A Case Report of a Novel Technique. Case Reports in Orthopedics. 2019;2019:1–6. doi: 10.1155/2019/4371860. doi: 10.1155/2019/4371860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Seidl AJ, Kraeutler MJ. Management of Articular Cartilage Defects in the Glenohumeral Joint. Journal of the American Academy of Orthopaedic Surgeons. 2018;26(11):e230–e237. doi: 10.5435/JAAOS-D-17-00057. doi: 10.5435/JAAOS-D-17-00057. [DOI] [PubMed] [Google Scholar]
- 21.McCarty LP, Cole BJ. Nonarthroplasty Treatment of Glenohumeral Cartilage Lesions. Arthroscopy: The Journal of Arthroscopic & Related Surgery. 2005;21(9):1131–1142. doi: 10.1016/j.arthro.2005.06.023. doi: 10.1016/j.arthro.2005.06.023. [DOI] [PubMed] [Google Scholar]
- 22.Millett PJ, Huffard BH, Horan MP, Hawkins RJ, Steadman JR. Outcomes of Full-Thickness Articular Cartilage Injuries of the Shoulder Treated With Microfracture. Arthroscopy: The Journal of Arthroscopic & Related Surgery. 2009;25(8):856–863. doi: 10.1016/j.arthro.2009.02.009. doi: 10.1016/j.arthro.2009.02.009. [DOI] [PubMed] [Google Scholar]
- 23.Frank RM, Van Thiel GS, Slabaugh MA, Romeo AA, Cole BJ, Verma NN. Clinical Outcomes after Microfracture of the Glenohumeral Joint. Am J Sports Med. 2010;38(4):772–781. doi: 10.1177/0363546509350304. doi: 10.1177/0363546509350304. [DOI] [PubMed] [Google Scholar]
- 24.Wang KC, Frank RM, Cotter EJ, et al. Long-term Clinical Outcomes After Microfracture of the Glenohumeral Joint: Average 10-Year Follow-up. Am J Sports Med. 2018;46(4):786–794. doi: 10.1177/0363546517750627. doi: 10.1177/0363546517750627. [DOI] [PubMed] [Google Scholar]
- 25.Shin JJ, Mellano C, Cvetanovich GL, Frank RM, Cole BJ. Treatment of Glenoid Chondral Defect Using Micronized Allogeneic Cartilage Matrix Implantation. Arthroscopy Techniques. 2014;3(4):e519–e522. doi: 10.1016/j.eats.2014.05.014. doi: 10.1016/j.eats.2014.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wang VM, Karas V, Lee AS, et al. Assessment of glenoid chondral healing: comparison of microfracture to autologous matrix-induced chondrogenesis in a novel rabbit shoulder model. Journal of Shoulder and Elbow Surgery. 2015;24(11):1789–1800. doi: 10.1016/j.jse.2015.06.008. doi: 10.1016/j.jse.2015.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Scheibel M, Bartl C, Magosch P, Lichtenberg S, Habermeyer P. Osteochondral autologous transplantation for the treatment of full-thickness articular cartilage defects of the shoulder. J Bone Joint Surg Br. 2004;86(7):991–997. doi: 10.1302/0301-620x.86b7.14941. doi: 10.1302/0301-620x.86b7.14941. [DOI] [PubMed] [Google Scholar]
- 28.Kircher J, Patzer T, Magosch P, Lichtenberg S, Habermeyer P. Osteochondral autologous transplantation for the treatment of full-thickness cartilage defects of the shoulder: results at nine years. J Bone Joint Surg Br. 2009;91(4):499–503. doi: 10.1302/0301-620X.91B4.21838. doi: 10.1302/0301-620X.91B4.21838. [DOI] [PubMed] [Google Scholar]
- 29.Riff AJ, Yanke AB, Shin JJ, Romeo AA, Cole BJ. Midterm results of osteochondral allograft transplantation to the humeral head. J Shoulder Elbow Surg. 2017;26(7):e207–e215. doi: 10.1016/j.jse.2016.11.053. doi: 10.1016/j.jse.2016.11.053. [DOI] [PubMed] [Google Scholar]
- 30.DiPaola MJ, Jazrawi LM, Rokito AS, et al. Management of humeral and glenoid bone loss--associated with glenohumeral instability. Bull NYU Hosp Jt Dis. 2010;68(4):245–250. [PubMed] [Google Scholar]
- 31.Romeo AA, Cole BJ, Mazzocca AD, Fox JA, Freeman KB, Joy E. Autologous chondrocyte repair of an articular defect in the humeral head. Arthroscopy. 2002;18(8):925–929. doi: 10.1053/jars.2002.36144. doi: 10.1053/jars.2002.36144. [DOI] [PubMed] [Google Scholar]
- 32.Buchmann S, Salzmann GM, Glanzmann MC, Wörtler K, Vogt S, Imhoff AB. Early clinical and structural results after autologous chondrocyte transplantation at the glenohumeral joint. J Shoulder Elbow Surg. 2012;21(9):1213–1221. doi: 10.1016/j.jse.2011.07.030. doi: 10.1016/j.jse.2011.07.030. [DOI] [PubMed] [Google Scholar]


