Abstract
Hallux rigidus (HR) is a degenerative disease of the first metatarsophalangeal (MTP1) joint and affects about 2.5% of people older than 50 years. The real etiology of this condition remains under debate. Clinical symptoms, physical exam, and instrumental evidence are important in assessing and grading the disease. The anatomy of the first metatarsal is unique and its configuration may play a significant role in the HR development. The first approach in the early stages of the disease usually begins with shoe modifications and foot orthoses, designed to limit irritation from the dorsal osteophytes, reducing motion and the mechanical stresses on the joint. To prevent or delay the development of HR, shoes should be sufficiently long, comfortable, with high toe box and broad toe-boxed, and should bear an allowed space for the orthotic device. The ideal orthotic appears to require a 3-mm thickness with a correct stiffness, and also increasing and extending the medial metatarsal arch just proximal to the metatarsal head, raising the first metatarsal and allowing the proximal phalanx to rest in a more plantarflexed position, decompressing the dorsal aspect of the joint. The increased foot pronation moment with medial column overload, when present, should be corrected. In addition, the maximum follow-up found by the analyzed studies was of 14.4 years, so the Authors cannot conclude how long conservative care can keep a patient free from pain and able to perform normal daily activities. However, the use of shoe modifications and foot orthoses may be considered a safe treatment and then should be always offered to patients, before any surgical management. (www.actabiomedica.it)
Keywords: Hallux rigidus, Hallux limitus, Conservative treatment, Non-surgical treatment, Orthotics, Orthoses
Introduction
Hallux rigidus (HR), Latin for Stiff Toe, is a degenerative disease of the first metatarsophalangeal (MTP1) joint and affects about 2.5% of people older than 50 years (1). The terms HR and hallux limitus (HL) are often used as synonymous (2); however, the first is defined as pain due to an arthritic and ankylotic joint without movement, while HL is defined as functional pain due to soft tissue tightness, which cause a limited range of motion (ROM) (1).
The term was first introduced by Davies-Colley (3) in 1887, who described the disease as “hallux flexus” and Cotterill (4) first coined the condition of HR shortly thereafter in 1888. The MTP1 seems to play an important role during the gait cycle as it transfers about 119% of an individual’s body weight with each step. Degeneration of the cartilage and osteophyte formation occur dorsally in the early stages of the disease and progress to involve the entire joint (Fig. 1) (1), causing pain and reducing the daily-life and sports activity of the patients (5).
Figure 1.
A schematic drawing of hallux rigidus with the formation of bony spurs (osteophytes) in the dorsal aspect of the first metatarsophalangeal joint.
Conservative treatments are usually the first approach for the early stages of the condition, such as non-steroidal anti-inflammatory drugs (NSAIDs), intra-articular steroid injections, footwear modifications, and orthotics (6). It is very important to clarify to the patients the need for lifestyle modification; indeed, weight loss allows to reduce forefoot weight-bearing during gait and consequent pain (7). If conservative modalities fail, surgery may be taken into consideration.
Currently, there is no consensus that conservative management could stop the clinical worsening of the condition (8). However, the use of shoe modifications and orthotics may alleviate symptoms and limit the degenerative progression of the disease (1).
Anatomy and biomechanics
Hiss (9) was the first author who described the movement of the MTP1 joint in 1937. Since then, many Authors have reported current values on the ROM of this joint. From 65° to 75° of dorsiflexion of the hallux on the first metatarsal is necessary during propulsion and normal gait (Fig. 2).
Figure 2.
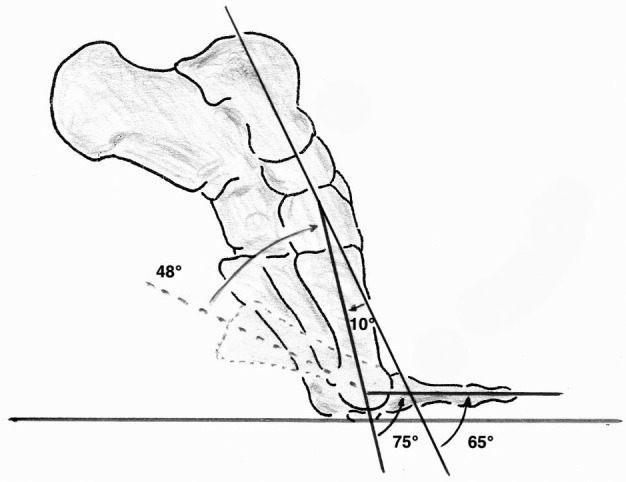
Hallux is flexed dorsally about 65-75° with respect to the first metatarsal after the lifting of the heel raised the base of the first ray of 48° and the first ray has a normal plantar flexion of 10° than the rest of the foot.
The plantarflexion of the first ray is allowed by the action of the peroneus longus tendon pulling on a rigid lateral column and consenting the floor reaction forces to dorsiflex the hallux. Without normal plantarflexion of the first metatarsal, only 25° to 30° of MTP1 joint dorsiflexion can succeed during ambulation. A limitation of dorsiflexion in this articulation of less than 20° is defined as HL. HR is the end stage of HL when the joint becomes ankylosed, without movement (10).
The anatomy of the first metatarsal is unique and its configuration may play a significant role in the HR development (11). The first metatarsal head, differently from the lesser metatarsal heads, have a dorsoplantar diameter smaller than the transverse (12).
The plantar plate of the MTP1 joint is a crucial structure of the capsuloligamentous complex and provides stability to the hallux. Its function is to make a support for tendon and ligaments attachment and, when disrupted, can cause disastrous effects on joint stability. The structure has a static insertion averaging 1.73-mm proximal to the joint line into the metatarsal head and 0.3-mm distal to the joint line into the proximal phalanx (13).
The surfaces of the MTP1 joint demonstrate unique relationships. Shereff et al. (14) made a cadaveric work on MTP1 joint kinematics, demonstrating the motion available to this articulation. The control group had 76° of dorsiflexion and a mean sagittal plane arc of 111°, the transverse plane translation was equal to 15% of the largeness of the metatarsal head. The HR group demonstrated significantly less motion with mean dorsiflexion of 49°, a mean sagittal arc of 69°, and transverse translation less than half found in the control group. The authors concluded that the abnormal centers of rotation caused an abnormal compression force across the MTP1 joint and decreased ROM. These forces bring to the clinical and radiographic findings frequently found in HR patients (14).
There seems to be a relation between HR associated with an increased foot pronation moment with medial column overload. Patients complaining functional HL had significant resistance to MTP1 dorsiflexion in early propulsion; however, in open kinetic chain there is no restriction of the motion (15).
The pathophysiological mechanisms have not been completely clarified for this condition. It seems to be matched with the pronation moment and hallux alignment, with an extreme preload on the medial column and premature recruitment of the plantar fascia during the early propulsion phase. If the proximal phalangeal dorsal rim cannot clear away the metatarsal head as the windlass engages, the metatarsal head impacts on the dorsal rim of the phalanx and engage the joint. This results in an increased load on the proximal phalanx (16).
Etiology and risk factors
The real etiology of this condition is still not well understood, although several contributing factors have been reported like osteochondral lesions, trauma, inflammatory arthropathies, including rheumatoid arthritis, gout, and seronegative arthropathies (17).
Trauma is the most common cause reported and may happen as a single isolated lesion (eg, fracture) or as the result of repeated micro-traumas (18).
The literature shows a higher incidence in females and approximately 80% of patients with bilateral HR had a history in their family of big toe arthritis or ‘‘bunions.’’ Long-term follow-up of the same patients with HR showed that more than 80% developed bilateral disease (11, 19).
Unilateral HR probably resulted from a traumatic episode (11), in plantar flexion or forced hyperextension, with squeeze and shear forces that induce chondral or osteochondral lesions. A severe distortion or “turf toe” injury in young and active patients (20) can even bring to progressive arthritic alterations over time (21).
In some studies arise the hypothesis that HR appears to be associated with interphalangeal hallux valgus and bilateral involvement is correlated with family history and female gender (11). Other Authors state that structural factors such as a flat or chevron-shaped joint (Fig. 3), long first metatarsal, metatarsus primus elevatus and metatarsus adductus, can also lead to increased risk of HR. The concept that instability of the first ray can predispose to hallux valgus is the corollary to the idea that a flat or chevron-shaped joint can bring to HR. However, most cases seem to be idiopathic (22).
Figure 3.
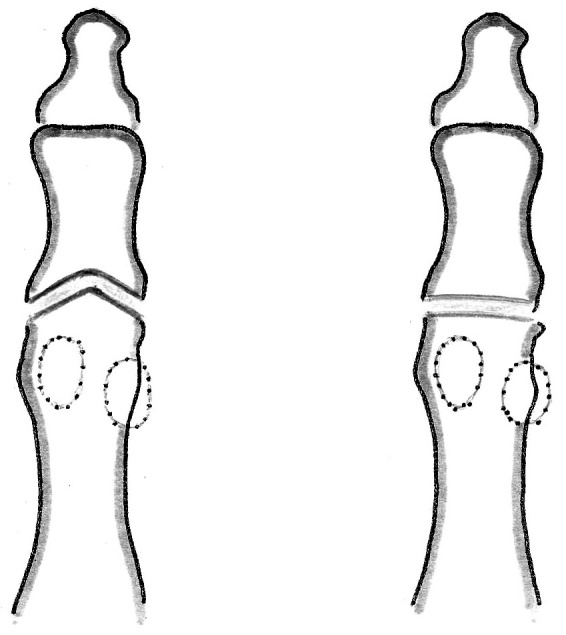
A flat (on right) or chevron-shaped joint (on left) that may predispose to the development of hallux rigidus.
Classification
Over the years, multiple different classification systems have been described for HR to classify and evaluate the severity of the MTP1 joint damage. Beeson et al. (22) reviewed 18 HR classification systems and found no coherence in the construction of the systems as they missed of reliability and scientific validity. Many of the enclosed parameters were based on subjective clinical experience. The authors concluded that the system proposed by Coughlin and Shurnas (23) appears to be the gold standard, as it is based on a combination of objective clinical and radiological findings. However, Regnauld’s classification system also seems to be widely used, alongside the previous classification system, as one of the most complete and exhaustive (24). Some of the changes in this classification system from one reference to the next can be ascribable to the translation from a foreign language (French) to English (22).
Diagnosis
Clinical evaluation
Patients with HR may show altered gait patterns or pain on the lateral aspect of the foot, secondary to the attempt to reduce loading on the MTP1 joint (Fig. 4).
Figure 4.
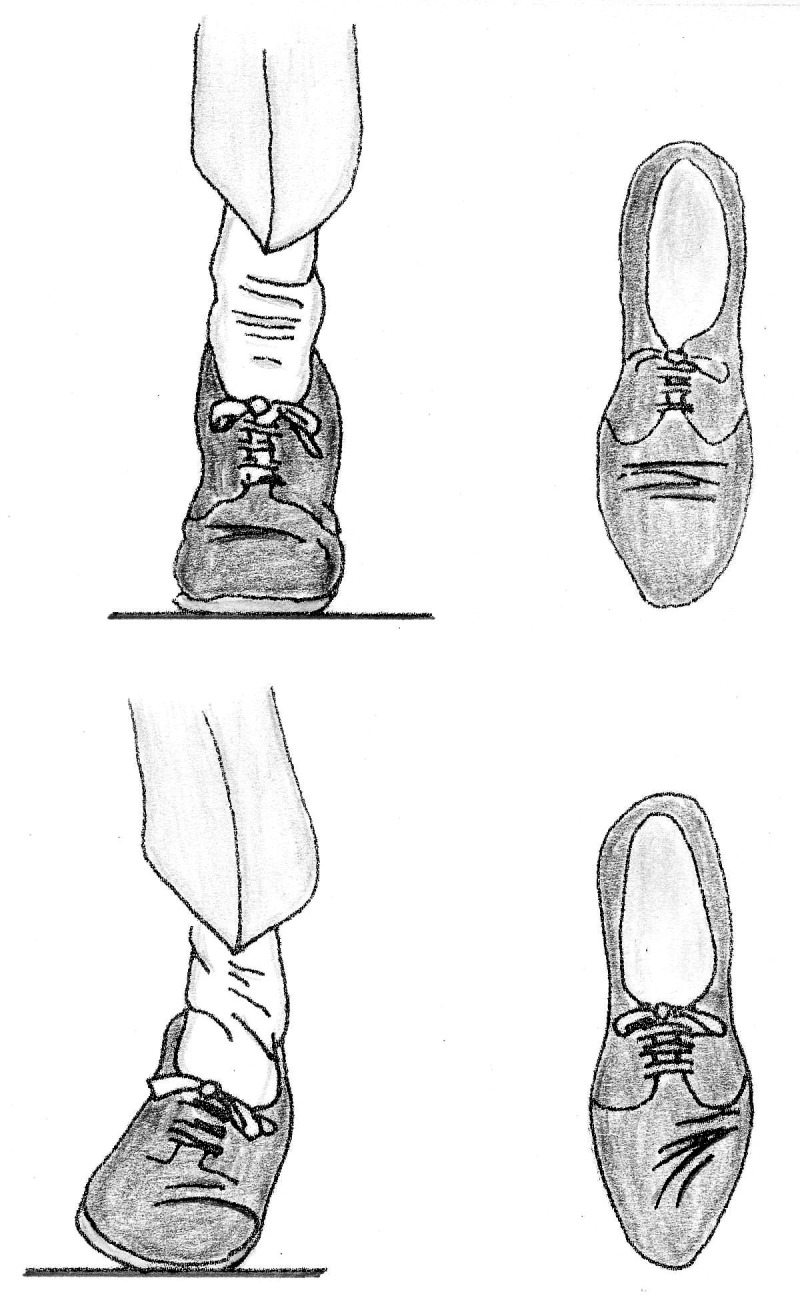
Hallux rigidus patients may show gait alterations with walking on the outer edge of the foot, secondary to the attempt to reduce loading on the first metatarsophalangeal joint.
Patients may also report some limitations on wearing determined types of shoes due to dorsal osteophytes present on the first metatarsal head and proximal phalanx. In addition, patients may report numbness along the medial border of the big toe as the osteophytes may compress on the dorsomedial cutaneous nerve (25). As the pathology advances, acute flare-ups become more severe and frequent (26), and they are sometimes mistaken for gout.
During the physical examination, the affected foot should be evaluated in the laying and standing positions. The standing position will give information regarding the function and dynamic alignment of the hallux, while the laying position will relax the soft tissues and help to evaluate ROM. The MTP1 joint is often tender dorsally with palpable osteophytes. For the possible compression by the dorsal osteophytes on the dorsomedial cutaneous nerve, sensation deficits and vascular function of the foot should be assessed. Evaluating the ROM of the MTP1 joint is crucial, because it may be an indicator of the severity of arthritis. A decreased passive and active ROM, most notably in dorsiflexion, is the most common finding. In the early stages of HR, pain during passive ROM ordinarily occurs at or near the endpoints of flexion. However, pain in midrange motion shows a more diffuse level of arthritic change in the MTP1 joint (1).
ROM may be measured clinically using a goniometer; however, goniometric measurement showed to be unreliable and difficult to reproduce in a standardized mode as it is affected by different factors including instrumentation and various patient types (27).
Vulcano et al. proposed a new reliable and reproducible method for measuring the MTP1 ROM using dynamic X-rays and they noted a significant difference between clinical ROM and radiographic ROM, with clinical dorsiflexion equal to or less than the radiographic one. The difference seemed to be more pronounced in patients with dorsiflexion less than 30 degrees (28).
The hallux interphalangeal joint should also be accurately examined. This joint could also be arthritic and the surgeon should avoid performing an arthrodesis of IP and MTP1 joints to prevent abnormal gait patterns (26).
Imaging
For an accurate evaluation, weight-bearing anteroposterior (AP), lateral and oblique views of the affected foot should be achieved. The degree of the MTP1 joint space is best noted on the oblique view. In advanced stages of HR, osteophytic formation may be observed in the periarticular area of the proximal phalanx and metatarsal head. It is relevant to note that the dorsal osteophytes may obstruct the AP view of the joint. Deland et al. (29) reported that osteophytes may lead to an apparent more severe arthritis of the joint. Usually, the dorsal aspect of the MTP1 joint is affected first. Joint sclerosis and subchondral cysts may be also present. Other studies as magnetic resonance imaging (MRI) and computed tomography (CT) images should not be necessary for diagnosis or plan surgery, but they may be helpful after a sprain or jamming episode with an osteochondral defect of the MTP1 joint (1).
Treatment
Most of the available literature concerning HR focuses on the operative treatment of this condition. In this study, we were interested in discovering what the outcomes are from non-operative treatment through shoe modifications and foot orthoses emphasizing the patient’s perspective. In the early stages of this condition, the first approach starts with shoe modifications, intra-articular injections, and, as in other pathologies (30, 31), activity modification (6). Taping and orthotics designed to shrink MTP impingement may also be useful (2). Medical therapy primarily involves oral nonsteroidal anti-inflammatory drugs (NSAIDs) to reduce swelling and joint pain. However, it has been noted that oral therapy alone is insufficient to obtain pain relief (25).
Manipulation under anesthesia and intraarticular steroid injections have been shown to provide good relief in some patients with HR, but only in patients in early stages and with pain relief of 3-6 months (32). Injection of platelet-rich plasma or bone marrow aspirate has lowered pain and stiffness while improving the quality of life parameters; however, the current scientific evidence is too poor to draw definitive conclusions (33).
In late stages, a wide range of surgical procedures are available including joint-sparing procedure, as interposition arthroplasties or joint-sacrificing techniques, and indications vary based on joint involvement and patient expectations (34).
In the early-middle grade of HR, cheilectomy is a reliable procedure, because may removes excess osteophytes, preventing dorsal impingement (35) with or without phalangeal osteotomy (36), and improve ROM.
Although first MTP fusion is still the standard treatment, especially in advanced stages HR, patients often desire to maintain joint movements (37). Patients can opt for a prosthetic implant, avoiding the movement restrictions required from an arthrodesis, but accepting the risk of complications or late failures (38).
As in other conditions (39), shoe modifications and orthotics may be useful for reducing pain by modifying the biomechanics of the MTP1 joint. Physical therapy may also be useful, involving joint manipulation, mobilization, and improving ROM. Gait training, rest, and local ice reduce pain and inflammation. The application of newer experimental modalities, such as extracorporeal shockwave therapy, iontophoresis, and ultrasonography therapy has yet to be shown to be an evidence-based practice for the treatment of HR, but they have been proposed. However, evidence supporting the use of these complementary therapies is still poor (1).
Shoe modifications
Shoe modifications and orthoses can play an important role in the nonsurgical management of forefoot pathology. Therapeutic footwear may improve patient gait and increase the level of ambulation (40).
Already in 1897 Bradford (41) noted alterations caused by incorrect shoes through an analysis of historical art. Contemporary shoes for women continue to cause deformity and predispose to injury, even more so than in the past. In particular, poorly fitting shoes are a major contributing factor to the difference in the incidence of foot disorders between men and women, mostly for those over 61 (42).
Traditionally, men’s shoes tend to be wider and have lower heels than women’s ones and this could explain, even only partially, the different incidence of forefoot problems in men compared to women. As widely showed in pathophysiology, the prevalence of several musculoskeletal foot conditions in women is largely related to the result of biomechanical changes caused by ill-fitting shoes. In particular, the altered biomechanics (associated with shoes with narrow toe box and high-heeled shoes) has been linked to the genesis of several forefoot syndromes, including hallux disorders (43).
Shoe selection is very important because shoes with an elevated heel will bring to preload the MTP1 in dorsal flexion, which is probably to worsen symptoms over time. Particular types of footwear can accentuate the symptomatology, for example, those with rigid upper and stitching or reinforcements in the back in correspondence with the MTP1 joint; but also the adoption of some sports footwear, such as soccer and golf type, or safety shoes for work reasons seem also to favor the development (44). Differently, a shoe with a soft upper and roomy toe box will minimize the osteophyte’s irritation. Shoes with high toe box may be useful to prevent direct contact between the shoe and the dorsal osteophytes hereby taking pressure off the joint. Some authors recommend a possible stretch with a ball and ring stretcher to adapt the deformity further; this can be made to help accommodate dorsal osteophytes and works best on a soft leather shoe (45).
Ready-made shoes may be necessary to allow space for the orthotic device. In resistant cases, the shoes may be changed to include a forefoot rocker and an extended steel shank in the shoe’s sole. These changes will decrease further the quantity of motion in the forefoot and the moment forces that are brought into play by the foot at midstance to push-off. To assure good communication between the prescribing physician and the orthotic practitioner, a written prescription should include all of the necessary elements and specific for each patient (45).
The latest studies affirm that HR is best managed with a hard-soled shoe or rigid insert that alleviates pain by restricting motion across the joint (46). Also, a large retrospective analysis suggests that HR symptoms usually get better even without surgery (47).
Although few studies have confronted over-the-counter (OTC) inserts with custom orthotics, hard-soled shoes and rigid inserts may relieve pain by restricting motion across the MTP joint (45, 48).
Adding an OTC stiffening shoe insert can improve function and pain for three months or more. Although some authors recommend using a curved sole, or rocker-bottom shoe, to reduce movement at the MTP1 joint, its effectiveness has not been widely studied (49).
Depending on cases, the clinician will also have to educate the patient on lifestyle changes, such as reducing weight-bearing and starting a regular physical activity; the latter, useful not only in these cases but in the vast majority of pathologies (50, 51).
Orthotics
Unfortunately, there is scarce evidence to sustain the role of orthotics and supportive shoes for the treatment of HR and this treatment modality may be best appropriate for lower grades of HR and in selected groups of patients (52).
Hoffmann et al. in 1905 (53) did a comparative study of barefooted and shoe-wearing patients and noticed that abnormal biomechanics of the foot can predispose to disorders of the MTP1 joint and that shoes can further compound these abnormal factors. Moreover, further studies have sustained the idea that abnormal biomechanics of the feet may give rise to dysfunction of the MTP1 and, subsequently, to disorder. Shoe modifications and orthotics have been commonly used in the treatment of HR to modify the biomechanics of the first MTP1 joint, limiting irritation from the dorsal osteophytes and reducing motion and mechanical stresses on the joint (53).
An extended shank is a common orthosis utilized in the management of HR. Made of carbon graphite composite or either spring steel, these shanks are fitted between the layers of the sole, expanding from the heel to the toe. Shanks may be placed in almost any type of shoes and may be used together with a rocker sole to increase its function (45).
The shank also works as a splint, preventing the shoe from bending and limiting the dorsiflexion of the great toe during the gait and decreasing the forces acting across the midfoot and forefoot. The rocker sole is one of the most used modifications, its principal function is to rock the foot from heel-strike to toe-off without requesting the shoe or foot to flex. Unfortunately, many orthoses reduce the space inside the shoe, thus being able to increase the pressure on the dorsal aspect of the MTP1 joint. Thus, a high toe box to avoid direct contact between the dorsal osteophyte and shoe should also be used (40).
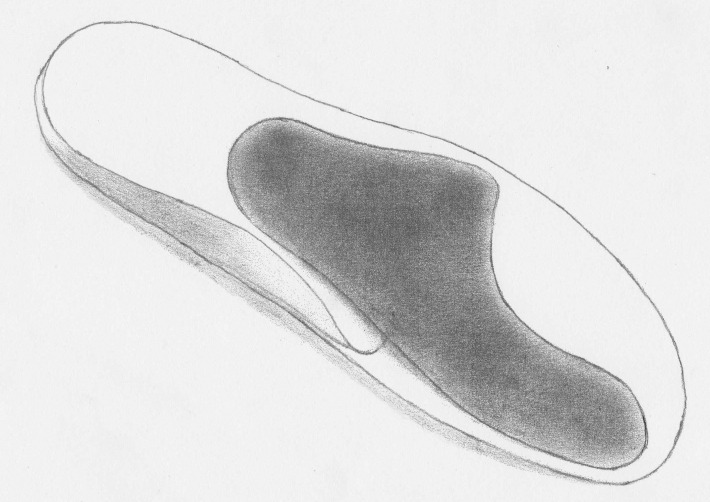
The correct foot orthoses should supply adequate shock attenuation and shock absorption, provide suitable cushioning, redeploy weight-bearing pressures, splint and support via the total-contact concept, reduce shear, correct or support flexible deformities, limit joint motion, and accommodate fixed deformities. Foot orthoses may be prefabricated or, better, custom made directly from a mold of the subject’s foot (Fig. 5) (39, 52).
Figure 5.

Custom-made foot orthoses are contoured devices made from a plaster cast.
The orthotic approach has two main goals: mechanically limit dorsal impingement of the MTP1 joint and limit or eliminate mechanical irritation of the dorsal osteophytes by regulating the shoe wear to adapt the deformity. Reaching these goals ensures the best possible outcome of conservative management (45).
Thompson et al. state that the use of orthoses is more effective than NSAIDs therapy in the treatment of osteoarthritis (54). In their study, one hundred percent of the subjects (N=64), with a mean age of 63 years, wore orthoses for relief of pain and had a statistically significant longer period of pain relief than those treated only with NSAIDs.
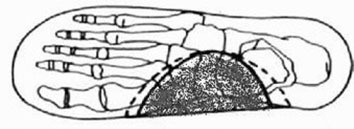
Dorsal impingement of MTP1 may be confined in several ways. Rigid support can be extended below the hallux to directly limits dorsal flexion and to reduce loads through the MTP1 joint (Morton’s extension) (Fig. 6).
Figure 6.
A schematic drawing of Morton’s extension, a rigid carbon foot orthotic that extends to the distal tip of the hallux. It may reduce hallux rigidus’ pain improving load distribution.
Prefabricated devices made from carbon fiber or spring steel are usable and can be used alone or in combination with a custom-made orthotic. Sammarco et al. (45) use a base of the orthotic with a custom-molded piece of polypropylene and stated that a 3-mm thickness may provide the correct stiffness. Authors also recommend increasing and extending the medial metatarsal arch just proximal to the metatarsal head, raising the first metatarsal and allowing the proximal phalanx to rest in a more plantarflexed position, decompressing the dorsal aspect of the joint (Fig. 7).
Figure 7.
A schematic drawing in which the medial metatarsal arch can be positioned just proximal to the metatarsal head, raising the first metatarsal and allowing the proximal phalanx to rest in a more plantarflexed position, decompressing the dorsal aspect of the joint.
Few studies in the literature analyzed shoe modifications and orthoses effectiveness for the treatment of HR. Grady, et al. (46) stated that out of 772 patients with symptomatic HR (n=772), 428 (55%) patients were successfully treated conservatively with 362 (84%) of these 428 patients treated with the use of orthoses. Among them, 38% of patients required surgery, and 6% of patients did not respond to conservative management.
Smith (55) conducted a long-term follow-up study of 22 patients (24 feet) to explore the efficacy of non-operative treatment for HR pathology, with an average follow-up time of 14.4 years. Thirteen patients were able to modify their shoes by using shoes with wide space in the toe box. Seven patients had pain relief by avoiding high heels. Of all the patients, 63% would sustain their original decision of non-operative treatment. Moreover, pain level remained constant in 92% of cases over an average of 14.4 years and there seemed to be no relationship between subjective complaints and radiographic evidence of progression of the condition.
Welsh et al. (48) conducted an observational study with 35 patients with foot orthoses with a follow-up period of 24 weeks. The pain score, as measured on the modified pain subscale of the foot function index (FFI), was 48 mm at baseline and improved to 14.5 mm at the end of 24 weeks (p <0001). He concluded that orthotics could provide a reduction in mechanically induced pain to a level that is considered a sufficient analgesic response to treatment.
Conclusion
Unfortunately, there is poor evidence to sustain the role of orthotics and supportive shoes for the treatment of HR. However, orthoses and shoe modifications have been used to off-load the forefoot and thus reduce pain from weight-bearing pressure.
The most suitable footwear should be with a high toe box, where a hard-soled shoe or rigid insert may alleviate pain by restricting motion across the joint, including a forefoot rocker and an extended steel shank in the shoe’s sole. To prevent or delay the development of HR, shoes should be sufficiently long, comfortable, broad toe-boxed, and should bear an allowed space for the orthotic device.
The ideal orthotic should have a custom-molded piece of polypropylene, with a 3-mm thickness provided the correct stiffness. It’s also necessary to increase and extend the medial metatarsal arch just proximal to the metatarsal head, raising the first metatarsal and allowing the proximal phalanx to rest in a more plantarflexed position, decompressing the dorsal aspect of the joint. Besides, the maximum follow-up found by the analyzed studies was of 14.4 years, so authors cannot conclude how long conservative care can keep a patient free from pain and able to perform normal daily activities.
Despite this, the use of shoe modifications and foot orthoses may be considered a safe treatment and should be always offered to patients, before any surgical management. Notwithstanding the good quality of the selected articles, further studies with a longer follow-up period and high-quality RCTs are needed to provide more solid proofs.
Conflict of interest:
Each author declares that he or she has no commercial associations that might pose a conflict of interest in connection with the submitted article.
References
- 1.Lam A, Chan JJ, Surace MF, Vulcano E. Hallux rigidus: How do I approach it? World J Orthop. 2017 May 18;8(5):364–371. doi: 10.5312/wjo.v8.i5.364. doi: 10.5312/wjo.v8.i5.364. eCollection 2017 May 18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Colò G, Alessio-Mazzola M, Dagnino G, Felli L. Long-Term Results of Surgical Treatment of Valenti Procedures for Hallux Rigidus: A Minimum Ten-Year Follow-Up Retrospective Study. J Foot Ankle Surg. 2019 Mar;58(2):291–294. doi: 10.1053/j.jfas.2018.08.055. doi: 10.1053/j.jfas.2018.08.055. [DOI] [PubMed] [Google Scholar]
- 3.Davies-Colley M. Contraction of the metatarsophalangeal joint of the great toe. BMJ. 1887;1:728. [Google Scholar]
- 4.Cotterill J. Stiffness of the great toe in adolescents. BMJ. 1888;1:1158. doi: 10.1136/bmj.1.1378.1158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Saxena A, Valerio DL, Behan SA, Hofer D. Modified Valenti Arthroplasty in Running and Jumping Athletes With Hallux Limitus/Rigidus: Analysis of One Hundred Procedures. J Foot Ankle Surg. 2019 Jul;58(4):609–616. doi: 10.1053/j.jfas.2018.07.009. doi: 10.1053/j.jfas.2018.07.009. Epub 2018 Dec 13. [DOI] [PubMed] [Google Scholar]
- 6.Colò G, Samaila EM, Magnan B, Felli L. Valenti resection arthroplasty for hallux rigidus: A systematic review. Foot Ankle Surg. 2019 Dec 5 doi: 10.1016/j.fas.2019.11.009. pii: S1268-7731(19)30209-7 doi: 10.1016/j.fas.2019.11.009. (Epub ahead of print) [DOI] [PubMed] [Google Scholar]
- 7.Nakai K, Zeidan H, Suzuki Y, Kajiwara Y, Shimoura K, Tatsumi M, Nishida Y, Bitoh T, Yoshimi S, Aoyama T. Relationship between forefoot structure, including the transverse arch, and forefoot pain in patients with hallux valgus. J Phys Ther Sci. 2019 Feb;31(2):202–205. doi: 10.1589/jpts.31.202. doi: 10.1589/jpts.31.202. Epub 2019 Feb 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Caravelli S, Mosca M, Massimi S, Pungetti S, Russo A, Fuiano M, Catanese G, Zaffagnini S. A Comprehensive and Narrative Review of Historical Aspects and Management of Low-Grade Hallux Rigidus: Conservative and Surgical Possibilities. Musculoskelet Surg. 2018 Dec;102(3):201–211. doi: 10.1007/s12306-018-0530-3. doi: 10.1007/s12306-018-0530-3. Epub 2018 Feb 1. [DOI] [PubMed] [Google Scholar]
- 9.HISS JM. Functional Foot Disorders. Los Angeles: Los Angeles Press; 1937. p. 251. [Google Scholar]
- 10.Camasta CA. Hallux Limitus and Hallux Rigidus. Clinical Examination, Radiographic Findings, and Natural History. Clin Podiatr Med Surg. 1996 Jul;13(3):423–48. [PubMed] [Google Scholar]
- 11.Coughlin MJ, Shurnas PS. Hallux rigidus: demographics, etiology, and radiographic assessment. Foot Ankle Int. 2003;24(10):731–43. doi: 10.1177/107110070302401002. [DOI] [PubMed] [Google Scholar]
- 12.Sarrafian SK. Anatomy of the foot and ankle. 2nd edition. Philadelphia: J.B. Lippincott Company; 1993. [Google Scholar]
- 13.Lucas DE, Hunt KJ. Hallux Rigidus: Relevant Anatomy and Pathophysiology. Foot Ankle Clin. 2015 Sep;20(3):381–9. doi: 10.1016/j.fcl.2015.04.001. doi: 10.1016/j.fcl.2015.04.001. Epub 2015 Jul 4. [DOI] [PubMed] [Google Scholar]
- 14.Shereff MJ, Bejjani FJ, Kummer FJ. Kinematics of the first metatarsophalangeal joint. J Bone Joint Surg Am. 1986;68-A(3):392–8. [PubMed] [Google Scholar]
- 15.Roukis TS, Jacobs PM, Dawson DM, et al. A prospective comparison of clinical, radiographic, and intra-operative features of hallux rigidus. J Foot Ankle Surg. 2002;41:76–95. doi: 10.1016/s1067-2516(02)80031-x. [DOI] [PubMed] [Google Scholar]
- 16.Christensen JC, Jennings MM. Normal and abnormal function of the first ray. Clin Podiatr Med Surg. 2009 Jul;26(3):355–71. doi: 10.1016/j.cpm.2009.03.004. Table of Contents doi: 10.1016/j.cpm.2009.03.004. [DOI] [PubMed] [Google Scholar]
- 17.Drago J, Oloff L, Jacobs AM. A comprehensive review of hallux limitus. J Foot Surg. 1984;23(3):213–20. [PubMed] [Google Scholar]
- 18.Edenfield KM, Michaudet C, Nicolette GW, Carek PJ. Foot and Ankle Conditions: Midfoot and Forefoot Conditions. FP Essent. 2018 Feb;465:30–34. [PubMed] [Google Scholar]
- 19.Samaila EM, Ditta A, Negri S, Leigheb M, Colò G, Magnan B. Central Metatarsal Fractures: A Review and Current Concepts. Acta Biomed. 2020 May 30;91(4-S):36–46. doi: 10.23750/abm.v91i4-S.9724. doi: 10.23750/abm.v91i4-S.9724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nihal A, Trepman E, Nag D. First ray disorders in athletes. Sports Med Arthrosc Rev. 2009 Sep;17(3):160–6. doi: 10.1097/JSA.0b013e3181a5cb1f. doi: 10.1097/JSA.0b013e3181a5cb1f. [DOI] [PubMed] [Google Scholar]
- 21.York PJ, Wydra FB, Hunt KJ. Injuries to the great toe. Curr Rev Musculoskelet Med. 2017 Mar;10(1):104–112. doi: 10.1007/s12178-017-9390-y. doi: 10.1007/s12178-017-9390-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Beeson P, Phillips C, Corr S, Ribbans W. Classification systems for hallux rigidus: a review of the literature. Foot Ankle Int. 2008;29:407–414. doi: 10.3113/FAI.2008.0407. PMID: 18442456 DOI: 10.3113/FAI.2008.0407. [DOI] [PubMed] [Google Scholar]
- 23.Coughlin MJ, Shurnas PS. Hallux rigidus. Grading and longterm results of operative treatment. J Bone Joint Surg Am. 2003;85-A:2072–2088. PMID: 14630834. [PubMed] [Google Scholar]
- 24.Regnauld B. Hallux rigidus. In: Elson R, editor. The Foot. Berlin: Springer; 1986. pp. 335–350. [Google Scholar]
- 25.Deland JT, Williams BR. Surgical management of hallux rigidus. J Am Acad Orthop Surg. 2012;20:347–358. doi: 10.5435/JAAOS-20-06-347. PMID: 22661564 DOI:10.5435/JAAOS-20-06-347. [DOI] [PubMed] [Google Scholar]
- 26.Shurnas PS. Hallux rigidus: etiology, biomechanics, and nonoperative treatment. Foot Ankle Clin. 2009;14(1):1–8. doi: 10.1016/j.fcl.2008.11.001. [DOI] [PubMed] [Google Scholar]
- 27.Gajdosik RL, Bohannon RW. Clinical measurement of range of motion. Review of goniometry emphasizing reliability and validity. Phys Ther. 1987;67:1867–1872. doi: 10.1093/ptj/67.12.1867. PMID: 3685114 DOI: 10.1093/ptj/67.12.1867. [DOI] [PubMed] [Google Scholar]
- 28.Vulcano E, Tracey JA, Myerson MS. Accurate Measurement of First Metatarsophalangeal Range of Motion in Patients With Hallux Rigidus. Foot Ankle Int. 2016;37:537–541. doi: 10.1177/1071100715621508. PMID: 26660863 DOI:10.1177/1071100715621508. [DOI] [PubMed] [Google Scholar]
- 29.Deland JT, Williams BR. Surgical management of hallux rigidus. J Am Acad Orthop Surg. 2012;20:347–358. doi: 10.5435/JAAOS-20-06-347. PMID: 22661564 DOI: 10.5435/JAAOS-20-06-347. [DOI] [PubMed] [Google Scholar]
- 30.Dellenbaugh SG, Bustillo J. Arthritides of the foot. Med Clin North Am. 2014 Mar;98(2):253–65. doi: 10.1016/j.mcna.2013.10.004. doi: 10.1016/j.mcna.2013.10.004. Epub 2014 Jan 8. [DOI] [PubMed] [Google Scholar]
- 31.Hamid KS, Parekh SG. Clinical Presentation and Management of Hallux Rigidus. Foot Ankle Clin. 2015 Sep;20(3):391–9. doi: 10.1016/j.fcl.2015.04.002. doi: 10.1016/j.fcl.2015.04.002. Epub 2015 Jul 2. [DOI] [PubMed] [Google Scholar]
- 32.Solan MC, Calder JD, Bendall SP. Manipulation and injection for hallux rigidus. Is it worthwhile? J Bone Joint Surg Br. 2001;83:706–708. doi: 10.1302/0301-620x.83b5.11425. PMID: 11476310 DOI: 10.1302/0301620X.83B5.11425. [DOI] [PubMed] [Google Scholar]
- 33.Hauser RA, Hauser MA, Cukla JK. A retrospective observational study on HackettHemwall Dextrose Prolotherapy for unresolved foot and toe pain at an outpatient charity clinic in rural Illinois. J Prolotherapy. 2011;3:543–551. [Google Scholar]
- 34.Galois L, Hemmer J, Ray V, Sirveaux F. Surgical options for hallux rigidus: state of the art and review of the literature. Eur J Orthop Surg Traumatol. 2019 Aug 7 doi: 10.1007/s00590-019-02528-x. doi: 10.1007/s00590-019-02528-x. (Epub ahead of print) [DOI] [PubMed] [Google Scholar]
- 35.Sidon E, Rogero R, Bell T, McDonald E, Shakked RJ, Fuchs D, Daniel JN, Pedowitz DI, Raikin SM. Long-term Follow-up of Cheilectomy for Treatment of Hallux Rigidus. Foot Ankle Int. 2019 Oct;40(10):1114–1121. doi: 10.1177/1071100719859236. doi: 10.1177/1071100719859236. Epub 2019 Jul 16. [DOI] [PubMed] [Google Scholar]
- 36.Andrew J. Elliott, Stephanie C. Sayres, Martin J. O’Malley. Treatment of Advanced Stages of Hallux Rigidus with Cheilectomy and Proximal Phalangeal Osteotomy Surgical Technique. JBJS Essent Surg Tech. 2013 Sep;3(3):e14. doi: 10.2106/JBJS.ST.M.00026. Published online 2013 Jul 24. doi: 10.2106/JBJS.ST.M.00026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Patel HA, Kalra R, Johnson JL, Huntley SR, Lehtonen EJ, McGwin G, Naranje S, Shah A. Is interposition arthroplasty a viable option for treatment of moderate to severe hallux rigidus? - A systematic review and meta-analysis. Foot Ankle Surg. 2018 Jul 23 doi: 10.1016/j.fas.2018.07.006. pii: S1268-7731(18)30091-2. doi: 10.1016/j.fas.2018.07.006. (Epub ahead of print) [DOI] [PubMed] [Google Scholar]
- 38.Horisberger M, Haeni D, Henninger HB, Valderrabano V, Barg A. Total arthroplasty of the metatarsophalangeal joint of the hallux. Foot Ankle Int. 2016;37:755–765. doi: 10.1177/1071100716637901. [DOI] [PubMed] [Google Scholar]
- 39.Colò G, Rava A, Samaila EM, Palazzolo A, Talesa G, Schiraldi M, Magnan B, Ferracini R, Felli L. The Effectiveness of Shoe Modifications and Orthotics in the Conservative Treatment of Civinini-Morton Syndrome: State of Art. Acta Biomed. 2020 May 30;91(4-S):60–68. doi: 10.23750/abm.v91i4-S.9713. doi: 10.23750/abm.v91i4-S.9713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Janisse DJ, Janisse E. Shoe modification and the use of orthoses in the treatment of foot and ankle pathology. J Am Acad Orthop Surg. 2008;16:152–8. doi: 10.5435/00124635-200803000-00006. [DOI] [PubMed] [Google Scholar]
- 41.Bradford EH. The human foot in art. J Bone Joint Surg Am. 1897;(s1-s10):148–161. [Google Scholar]
- 42.Frey C. Foot health and shoewear for women. Clin Orthop. 2000;(372):32–44. doi: 10.1097/00003086-200003000-00005. [DOI] [PubMed] [Google Scholar]
- 43.Goud A, Khurana B, Chiodo C, Weissman BN. Women’s musculoskeletal foot conditions exacerbated by shoe wear: an imaging perspective. Am J Orthop (Belle Mead NJ) 2011 Apr;40(4):183–91. [PubMed] [Google Scholar]
- 44.Beeson P, Phillips C, Corr S, Ribbans WJ. Hallux rigidus: a cross-sectional study to evaluate clinical parameters. Foot (Edinb) 2009 Jun;19(2):80–92. doi: 10.1016/j.foot.2008.12.001. doi: 10.1016/j.foot.2008.12.001. Epub 2009 Apr 17. [DOI] [PubMed] [Google Scholar]
- 45.Sammarco VJ, Nichols R. Orthotic management for disorders of the hallux. Foot Ankle Clin. 2005 Mar;10(1):191–209. doi: 10.1016/j.fcl.2004.09.003. doi: 10.1016/j.fcl.2004.09.003. [DOI] [PubMed] [Google Scholar]
- 46.Becker BA, Childress MA. Common Foot Problems: Over-the-Counter Treatments and Home Care. Am Fam Physician. 2018 Sep 1;98(5):298–303. [PubMed] [Google Scholar]
- 47.Grady JF, Axe TM, Zager EJ, Sheldon LA. A retrospective analysis of 772 patients with hallux limitus. J Am Podiatr Med Assoc. 2002;92(2):102–108. doi: 10.7547/87507315-92-2-102. [DOI] [PubMed] [Google Scholar]
- 48.Welsh BJ, Redmond AC, Chockalingam N, Keenan AM. A case-series study to explore the efficacy of foot orthoses in treating first metatarsophalangeal joint pain. J Foot Ankle Res. 2010;3:17. doi: 10.1186/1757-1146-3-17. doi: 10.1186/1757-1146-3-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Jerilyn TX, Menz HB, Murley GS, Munteanu SE. Effectiveness of shoe stiffening inserts for first metatarsophalangeal joint osteoarthritis: a proof-of-concept study. Am J Phys Med Rehabil. 2016;95(2):103–111. doi: 10.1097/PHM.0000000000000350. [DOI] [PubMed] [Google Scholar]
- 50.Colò G, Cavagnaro L, Alessio-Mazzola M, Zanirato A, Felli L, Formica M. Incidence, diagnosis and management of sacroiliitis after spinal surgery: a systematic review of the literature. Musculoskelet Surg. 2019 May 7 doi: 10.1007/s12306-019-00607-0. doi: 10.1007/s12306-019-00607-0. (Epub ahead of print) [DOI] [PubMed] [Google Scholar]
- 51.Colò G, Massarini M, Cavagnaro L, Felli L, Ferracini R. Exercise therapy indications in metastatic bone patients. Minerva Ortop e Traumatol. 2020;71:000–000. DOI: 10.23736/S0394-3410.19.03960-2. [Google Scholar]
- 52.Kunnasegaran R, Thevendran G. Hallux Rigidus: Nonoperative Treatment and Orthotics. Foot Ankle Clin. 2015;20:401–412. doi: 10.1016/j.fcl.2015.04.003. PMID: 26320555 DOI: 10.1016/j.fcl.2015.04.003. [DOI] [PubMed] [Google Scholar]
- 53.Hoffmann P. The feet of barefooted and shoe-wearing peoples. J Bone Joint Surg Am. 1905;23(2):105–36. [Google Scholar]
- 54.Thompson JA, Jennings MB, Hodge W. Orthotic therapy in the management of osteoarthritis. J Am Podiatr Med Assoc. 1992;82(3):136–139. doi: 10.7547/87507315-82-3-136. [DOI] [PubMed] [Google Scholar]
- 55.Smith RW, Katchis SD, Ayson LC. Outcomes in HR patients treated nonoperatively: a long-term follow-up study. Foot Ankle Int. 2000;21(11):906–913. doi: 10.1177/107110070002101103. [DOI] [PubMed] [Google Scholar]