Abstract
Background:
Volar plating has increasingly become the most used technique for the treatment of unstable distal radius fractures due to the low soft-tissue disturbance and its biomechanical reliability, which allows the early mobilization of the wrist. One of the main goals of the volar locking compression plates design is to avoid those soft tissue complications historically associated to the dorsal plating. However, extensor tendon complications can not be completely excluded.
Method:
The authors report the case of a patient with a complete rupture of the index finger extensor tendons after volar plate fixation of the distal radius. Due to the presence of a severe tendons retraction with a 4-centimeter gap and the neighbouring soft tissues damage, it was decided to fill the gap with a 2-free-end autograft harvested from the Flexor Carpi Radialis (FCR) tendon, using the volar surgical approach performed to remove the plate.
Results:
At the 2-month follow-up, the patient showed the complete recovery of the flexion-extension movements.
Conclusions:
Even though the 2-free-end FCR tendon graft is not commonly reported for the reconstruction of extensor tendons defects, we assume it deserves to be considered as an adequate technique whenever the neighbouring tendons are critically compromised. (www.actabiomedica.it)
Keywords: Distal Radius Volar Plating, Extensor Tendon Injuries, FCR tendon Graft
Introduction
Distal radius fractures account for approximately one third of all fractures in the elderly with an incidence rate of 190-200 per 100,000 person-years (1). Surgical fixation of distal radius fractures has become more popular because of innovations in implant technology, such as low-profile implants with locking fixation. The overall symptomatic complication rate following open reduction and internal fixation has been reported to be as high as 28 percent (2). One of the main goals of the volar locking compression plates design is to avoid those soft tissue complications associated to the dorsal plating. Although nowadays the volar plate fixation is the most used surgical technique for the treatment of distal radius fractures, extensor tendon damages can not be completely excluded.
Among the complications reported in literature, they need to be mentioned: tenosynovitis of the extensor tendons, rupture of Extensor Pollicis Longus (EPL), rupture of Extensor Digitorum Communis, screw penetration of the radiocarpal joint (3). These complications can be less likely to occur with an appropriate pre-operative planning (4). In literature, Lister’s tubercle has been described to hide the screw protrusion through distal locking plate holes, where the EPL tendon is most vulnerable to injury, and often goes undetected with standard lateral views (5). The screws need to be long enough to support the dorsal surface of the distal radius. However, penetration of the extensor compartment when choosing longer screws is plausible. Surgeons need to confirm the screw length using the intra-operative fluoroscopy, to avoid the dorsal cortex penetration. Hill et al. (2015) recommended the intra-operative use of the Dorsal Tangential View (DTV) to best detect dorsal screw penetration after volar plating, based on a cadaveric study (6). Several fluoroscopic views have been described to enhance the ability to detect dorsal cortex screw penetration. The Skyline view and the Carpal Shoot-Through view have been developed to increase the visibility of the dorsal cortex. Both the Skyline and the Carpal-Shoot-Through views place the arm in supination with an elbow flexion of approximately 70-75 degrees and an inclination of 15-20 degrees on the vertical plane. Nevertheless, they differ from each other in the position of the wrist. Namely, in the Skyline view the wrist is placed in full palmar flexion position, whereas in the Carpal-Shoot-Through view is placed in full dorsal flexion position (7, 8).
Case Report
A 58-year-old woman was admitted to our Department with a sudden inability to extend the second finger of her left hand (Fig. 1). No recent trauma was reported. One year earlier she suffered a displaced fracture of the distal radius - 23 C2 according to the AO/OTA classification. Internal fixation by volar plate was performed, using the flexor carpi radialis–radial artery interval (Henry’s approach). The right positioning of the plate, the screws length, as well as the restoration of the volar tilt were intraoperatively assessed by fluoroscopic images. The 4-week x-ray follow-up showed early signs of fracture healing. However, the screws seemed overlong with respect to the dorsal cortical surface in the lateral view (Fig. 2). No extensor tendons functional deficit was found. 12 months later, the patient came back with a complete functional deficit of the index finger extension. Yet, the metacarpo-phalangeal (MCF) and proximal inter-phalangeal (PIP) joint examination proved no stiffness, and the full passive extension was noticed. The Ultrasound Examination suggested an incomplete rupture of the extensor tendon mechanism of the index finger, confirmed by the MRI examination. A second surgery was recommended, consisting in the plate removal and reconstruction of the extensor tendon mechanism, with end-to-end suture or tendon graft in case of a massive tendon defect. The patient rejected the surgery. However, she came back 6 weeks later due to the unacceptable disability and with the result of a chronic lesion. In agreement with the patient it was decided to proceed to the surgical treatment. It was decided to perform a combined dorsal and volar approach, in order to remove the plate and repair the extensor tendon injury. Starting from the dorsal approach, we confirmed the complete rupture of the extensor tendon mechanism of the second finger, the incomplete rupture of the extensor tendon mechanism of the fourth and fifth fingers, and the presence of a widespread tenosynovitis involving the whole extensor tendons apparatus and the retinaculum. The dorsal prominence of the screws was also confirmed. The index finger extensor tendon showed a severe retraction with a 4-centimeter gap, which did not allow its end-to-end suture. A tendon graft using the Palmaris Longus was not taken into consideration due to its congenital absence in our patient. Therefore, it was decided to use a strip harvested from the FCR using the volar surgical approach performed to remove the plate. The graft was used to fill the index finger tendon gap, obtaining a good flexion-extension balance (Fig. 3). The end-to-end suture for the fourth and fifth extensor tendon mechanism was performed. The latter was reinforced by the tenodesis between the Extensor Digiti Minimi and the branch for the fifth finger of the Extensor Digitorum Communis. The tendon sutures were protected by a short hand-wrist splint for 4 weeks. At the splint removal, the patient was discharged to the Rehabilitation Unit to start a targeted rehabilitation program. No post-operative complications occurred. At the 2-month follow-up, a complete recovery of the flexion-extension movements of all the fingers of the left hand was obtained (Fig. 4).
Figure 1.

Patient inability to extend the second finger of the left hand
Figure 2.
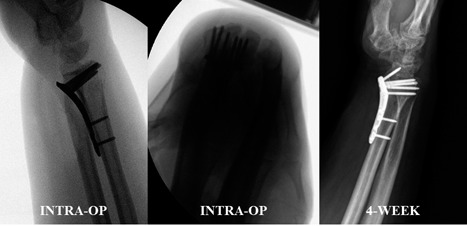
Intra-operative and 4-week follow-up x-ray
Figure 3.

FCR tendon graft used to fill the index finger extensor tendon gap
Figure 4.

Clinical outcome at the 2-month follow-up
Discussion
Tendon rupture following dorsal plating of distal radius fractures is a well-documented complication. Surgeons have more recently adopted volar plating to minimize the tendon issues usually seen with dorsal plating. Although, a number of extensor tendon injuries are still noted. Al-Rashid M. et al. (2006) published a series which reported a 4.4% to 8.6% incidence of extensor tendon rupture following volar plating (9). There is no consensus regarding the optimal technique to manage tendon injuries following volar plating of the distal radius. Tendon transfers appear to be a reliable option, as they were commonly described to treat both flexor and extensor ruptures. Namely, the Extensor Indicis Proprius (EIP) to EPL tendon transfer is a good and reproducible option. Lemmen et al. demonstrated that the EIP has an appropriate caliber, expendable to treat EPL lesions (10). In addition to tendon transfers, primary repairs, interphalangeal arthrodeses, and tendon graftings were all techniques used to manage these kind of complications. Palmaris Longus tendon interpositional reconstruction is most frequently used to overcome the tendon defects in 4-5 Verdan’s extensor zones. In patients with a skin and tendon defect, composite venous flaps and Palmaris Longus tendon reconstruction could be an alternative procedure to fix the gap formation in zones 4 and 5. Another feasible option, described for zones 4 and 5, is the tendon allograft from a cadaveric donor (11). Where applicable, an easier valuable solution to overcome an extensor tendon defect in these zones, is to suture the distal end of the defective tendon to a neighbouring tendon in a side-to-side fashion, in order to obtain motor strength from the neighbouring intact tendon. It is also reported by Al-Qattan MM a two-stage reconstruction using a silicone rod for significant tissue defects with a massive tendon gap. This technique prescribes the application of a tendon rod to the extensor tendon gap. Secondary to that procedure, the gap area is later reconstructed using a tendon graft that can be harvested from any donor area, and the silicone rod is removed with two small incisions at the distal and proximal area of the gap. After the rod is removed, the tendon graft is inserted in its place (12). As far as our patient is concerned, the end-to-end suture was not applicable for the treatment of the index finger injury, due to a chronic lesion, which led to a relevant tendon gap. It was feasible only for the fourth and fifth fingers. The fifth extensor tendon suture was ensured with the tenodesis between the Extensor Digiti Minimi and the branch for the fifth finger of the Extensor Digitorum Communis, to enhance the motor strength. The Palmaris Longus tendon graft was not possible due to its absence. The allograft from a cadaveric donor was refused from our patient, so it was not considered. For this reason, as valid alternative, it was decided to harvest a 2-free-end graft from the FCR for filling the gap. FCR arises from the medial epicondyle of the humerus along with the other flexor muscles of the forearm. It runs on the radial side of the forearm and finally attaches mainly to the base of the second metacarpal bone and also to the third metacarpal bone by a small slip (13). Its tendon is described in literature as one of the most used grafts for hand and wrist tendon reconstruction. It may be used to stabilize the base of the first metacarpal bone in trapeziectomy, to reconstruct the scapholunate and lunotriquetral interosseous ligaments in advanced Kien-böck’s disease, to reconstruct the scapho-lunate ligament linkage in the Brunelli’s Technique (14, 15).
In conclusion, even though the 2-free-end FCR tendon graft is not commonly reported for the reconstruction of extensor tendon defects, we assume it deserves to be considered as an adequate technique whenever the neighbouring tendons are critically compromised and the Palmaris Longus transfer is not applicable.
Conflict of interest:
Each author declares that he or she has no commercial associations (e.g. consultancies, stock ownership, equity interest, patent/licensing arrangement etc.) that might pose a conflict of interest in connection with the submitted article
References
- 1.Court-Brown C. M, Caesar B. “Epidemiology of adult fractures: A review,”. Injury. 2006;37:691–697. doi: 10.1016/j.injury.2006.04.130. [DOI] [PubMed] [Google Scholar]
- 2.Arora R, Lutz M, Hennerbichler A, Krappinger D, Espen D, Gabl M. “Complications following internal fixation of unstable distal radius fracture with a palmar locking-plate,”. J. Orthop. Trauma. 2007;21:316–322. doi: 10.1097/BOT.0b013e318059b993. [DOI] [PubMed] [Google Scholar]
- 3.Berglund L. M, Messer T. M. “Complications of volar plate fixation for managing distal radius fractures,”. Journal of the American Academy of Orthopaedic Surgeons. 2009;17:369–77. doi: 10.5435/00124635-200906000-00005. [DOI] [PubMed] [Google Scholar]
- 4.Totoki Y, Yoshii Y, Kusakabe T, Akita K, Ishii T. “Screw Length Optimization of a Volar Locking Plate Using Three Dimensional Preoperative Planning in Distal Radius Fractures,”. J. hand Surg. Asian-Pacific Vol. 2018;23:520–527. doi: 10.1142/S2424835518500522. [DOI] [PubMed] [Google Scholar]
- 5.Dolce D, Goodwin D, Ludwig M, Edwards S. “Intraoperative evaluation of dorsal screw prominence after polyaxial volar plate fixation of distal radius fractures utilizing the Hoya view: a cadaveric study,”. Hand. 2014;9:511–515. doi: 10.1007/s11552-014-9616-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hill B. W, Shakir I, Cannada L. K. “Dorsal screw penetration with the use of volar plating of distal radius fractures: How can you best detect?,”. J. Orthop. Trauma. 2015;29:408–413. doi: 10.1097/BOT.0000000000000361. [DOI] [PubMed] [Google Scholar]
- 7.Marsland D, Hobbs C. M, Sauvé P. S. “Volar locking plate fixation of distal radius fractures: use of an intra-operative ‘carpal shoot through’ view to identify dorsal compartment and distal radioulnar joint screw penetration,”. Hand. 2014;9:516–21. doi: 10.1007/s11552-014-9607-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Riddick A. P, Hickey B, White S. P. “Accuracy of the skyline view for detecting dorsal cortical penetration during volar distal radius fixation,”. J. Hand Surg. Eur. Vol. 2012;37:407–411. doi: 10.1177/1753193411426809. [DOI] [PubMed] [Google Scholar]
- 9.Al-Rashid M, Theivendran K, Craigen M. A. C. “Delayed ruptures of the extensor tendon secondary to the use of volar locking compression plates for distal radial fractures,”. J. Bone Jt. Surg. - Ser. Br. 2006;88:1610–2. doi: 10.1302/0301-620X.88B12.17696. [DOI] [PubMed] [Google Scholar]
- 10.Lemmen M. H. M, Schreuders T. A. R, Stam H. J, Hovius S. E. R. “Evaluation of restoration of extensor pollicis function by transfer of the extensor indicis,”. J. Hand Surg. Eur. Vol. 1999;24:46–9. doi: 10.1016/s0266-7681(99)90025-6. [DOI] [PubMed] [Google Scholar]
- 11.Türker T, Hassan K, Capdarest-Arest N. “Extensor tendon gap reconstruction: A review,”. Journal of Plastic Surgery and Hand Surgery. 2016;50:1–6. doi: 10.3109/2000656X.2015.1086363. [DOI] [PubMed] [Google Scholar]
- 12.Al-Qattan M. “Two-staged extensor tendon reconstruction for zone 6 extensor tendon loss of the fingers: Indications, technique and results,”. J. Hand Surg. Eur. Vol. 2015;40:276–8. doi: 10.1177/1753193413517626. [DOI] [PubMed] [Google Scholar]
- 13.Potu B.K, Kumar V, Annam S, Sirasanagandla S.R. “A morphometric study on flexor carpi radialis muscle of the forearm: A cadaveric study,”. Morphologie. 2016;100:12–6. doi: 10.1016/j.morpho.2015.09.001. [DOI] [PubMed] [Google Scholar]
- 14.Henry M. “Outcomes assessment of lunate replacement arthroplasty with intrinsic carpal ligament reconstruction in Kienböck’s disease,”. Hand. 2014;9:364–9. doi: 10.1007/s11552-014-9624-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Brunelli G.A, Brunelli G.R. “A new technique to correct carpal instability with scaphoid rotary subluxation: A preliminary report,”. J. Hand Surg. Am. 1995;20:82–5. doi: 10.1016/s0363-5023(95)80175-8. [DOI] [PubMed] [Google Scholar]


