Abstract
Background:
Infections of the spine and hip joint are not common and, as described in literature, they are occasionally linked by a psoas abscess. In patients suffering back pain with history of spondylodiscitis, the spine as primary source of infection for a secondary psoas abscess should always be included in differential diagnosis. A delay in diagnosis of the psoas abscess could lead to septic femoral head necrosis.
Case report:
A case of a 65-year-old woman affected by septic femoral head necrosis due to spondylodiscitis and secondary psoas abscess is reported; the patient needed a specific antibiotic therapy then undergoing a total hip arthroplasty (THA).
Discussion and conclusion:
Diagnoses of lumbar spine infection and psoas abscess are difficult and often delayed. Since the symptoms of both are non-specific, high degree of suspicious is necessary. In psoas abscess, an early diagnosis is important, because a delayed treatment could result in septic femoral head necrosis requiring both a prolonged antibiotic therapy and a THA. (www.actabiomedica.it)
Keywords: Spine, Hip, Infection, Spondylodiscitis, Psoas abscess, Femoral head necrosis
Background
Infections of the spine and hip are not common, but they are serious conditions requiring an early diagnosis and an appropriate treatment (1). Both infections are occasionally associated with a psoas abscess: in fact, infection of the spine can cause a psoas abscess (2, 3, 4), which could lead to a septic hip arthritis (5). The high susceptibility of the psoas muscle to infections is explained by its peculiar anatomy: infectious agents can access the muscle by either direct extension or via haematogenous seeding. In most cases, organisms reach this muscle for contiguity from kidneys, ureters, pancreas, large and small intestine and from the spine (secondary psoas abscess). Moreover, the blood supply of the muscle is a predisposing factor for the haematogenous spread from distance sources (primary psoas abscess) (6). The classic signs, including fever, flank pain and limp, are erratically present and diagnosis is often delayed by misinterpretation as arthritis, joint infection, urologic or abdominal disorders (7).
Incidence of spine-associated psoas abscess increase in case of previous spondylodiscitis, invasive procedures on the spine and recurring tuberculosis in industrialized countries.
The spine as primary source of infection for secondary psoas abscess should always be included in differential diagnosis, especially in patients suffering back or hip pain with history of spondylodiscitis (4).
Case report
In July 2018 a 65-year-old woman referred to the emergency department complaining lumbar pain irradiated to the left lower limb which was investigated with plain X-rays (Figure 1 A, B) and then she was discharged with a sciatica diagnosis and corticosteroid treatment. Three weeks later, she experienced increasing pain in the left groin and knee, making weightbearing impossible on that limb. She arrived at our attention and during the physical examination there was no evidence of neither pulmonary or abdominal symptoms nor fever, the left hip joint range of motion was painfully restricted in all directions. A plain radiograph and a CT scan of the left hip showed osteoarthritic changes at an advanced stage, heterogeneous density of femoral head and suspected signs of fracture (Figure 2 A, B). Therefore, she was hospitalized for further investigations. First blood exams showed increased WBC (19500/µL) with neutrophilic preponderance (94.3%) and a CRP of 15.11 mg/dL.
Figure 1.
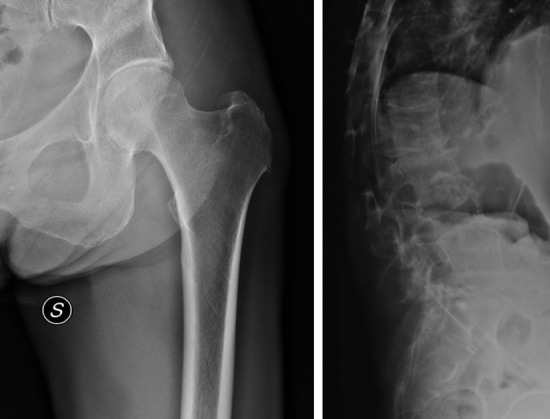
Left hip (A) and lumbar spine (B) X-rays performed at the first access to the emergency room
Figure 2.

Left hip X-ray (A) and CT-scan (B) performed 3 weeks after the first access to the ER
In the following days an increase of the body temperature up to 38.7 °C was recorded and multiple blood samples for colture were obtained and the patient started an empiric antimicrobial therapy with intravenous administration of Ciprofloxacin at the dosage of 400 mg every 12 hours. Meanwhile she underwent a hip and lumbar MRI that revealed hip joint edema, intra-articular effusion and altered signal intensity in the femoral head as well as in the acetabulum, neighboring soft tissues and L4 vertebral body.
Five days later microbiological coltures from blood samples showed the presence of Staphylococcus Aureus and a specific antimicrobial therapy was set up adding 2 gr of IV Oxacillin every 4 hours to the Ciprofloxacin. A few days later there was a reduction in WBC count (11500/µL) and in CRP blood levels (13.51 mg/dL).
An additional contrast-enhanced MRI of the lumbar spine and pelvis showed an altered and diffuse signal intensity in the L2-L4 vertebrae and surrounding soft tissues and a fluid collection in the context of psoas muscle as well as in the hip joint demonstrating a pyogenic spondylodiscitis with secondary psoas abscess and hip joint infection (Figure 3 A, B). Blood exams taken at this time showed a normalization of WBC count (7100/µL) and a further decrease in CRP blood levels (7.94 mg/dL).
Figure 3.
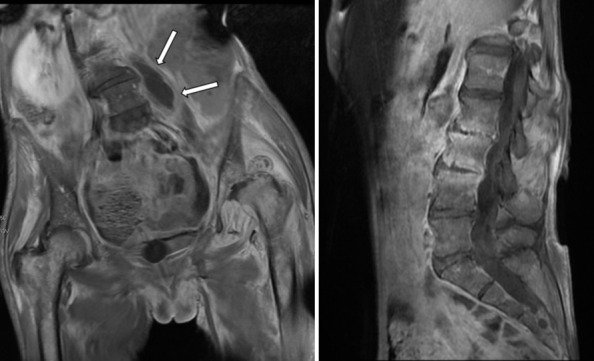
Contrast-enhanced MRI of the pelvis (A) and lumbar spine (B) showing altered and diffuse signal intensity of L2-L4 vertebrae. The psoas abscess is indicated by the arrows.
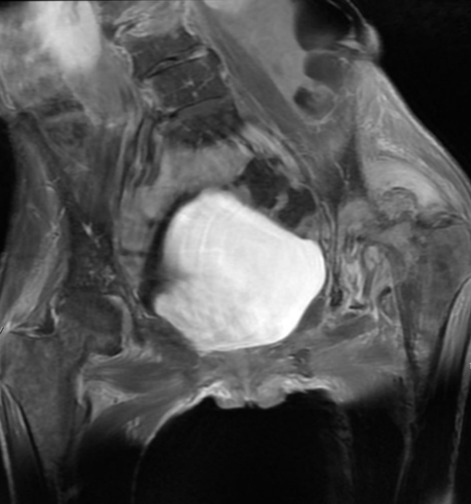
Forty days after hospital admission, an abdominal and pelvis CT scan with contrast was performed which still revealed an organized fluid collection in the psoas measuring 21 × 22 × 53 mm, effusion in the left hip with another organized fluid collection posteriorly to the femoral head (Figure 4). It also showed a cranial acetabular breakthrough and femoral head resorption. Additional L2 CT-guided ago-biopsy was performed and revealed only diffuse fibrosis of the vertebral body. The patient remained apiretic and laboratory exams became normal after five weeks of intravenous antibiotic therapy, so we decided to shift IV administration to 500 mg of oral Levofloxacin a day; moreover, left hip pain was decreasing though weightbearing was still prohibited.
Figure 4.

Abdominal and pelvis CT scan with contrast after 40 days from admission : the psoas abscess is indicated by the arrows
Three months after admission and specific antibiotic therapy, patient underwent a new pelvis and hip MRI (Figure 5) which showed persistent enhancement of the hip while psoas collection was disappeared, allowing to stop antibiotics.
Figure 5.
Pelvis and hip MRI after 3 months with no evidence of residual psoas abscess. At this time antibiotic therapy was therefore suspended
A labelled leukocytes scintigraphy was performed two months later and did not reveal any infection site, so on May 2019, 10 months from the symptoms onset, she underwent preoperative tests including a pelvis and left hip X-ray which showed increased femoral head deformity and cranial acetabular breakthrough following septic osteonecrosis (Figure 6).
Figure 6.

Left hip AP X-ray at 10 months from symptoms onset, preoperatively to total hip replacement, showing severe femoral head deformity and cranial acetabular breakthrough following septic osteonecrosis
On June 2019, once established the absence of S. Aureus in the nasal, inguinal and axillary swab, the patient underwent THA with a cemented “dual-mobility” cup and a cementless stem through direct anterior approach (Profemur Z stem ®, Liberty cup ®, MicroPort Orthopedics, Shanghai, China). Intraoperative findings revealed abundant capsular fibrosis, both femoral head and acetabulum resorption and severe acetabular deformity. Intraoperative samples submitted for coltural examination were thereafter negative and a short-term 24 hours postoperative antibiotic prophylaxis with amoxicillin was administrated.
At 9-months follow-up, there were no clinical, laboratory or radiographic signs of infection in the left hip and lumbar spine and there were no radiographic signs of mobilization of THA loosening (Figure 7).
Figure 7.

AP X-ray of total hip replacement at 9-months follow-up. The implant consisted in a cemented “dual-mobility” cup and a cementless stem through a direct anterior approach
Discussion
This case is explanatory of how a delayed diagnosis of spondylodiscitis complicated with a psoas pyogenic abscess could lead to a septic femoral head necrosis requiring a THA as a unique final solution.
To our knowledge, there are a few similar cases described in literature (5, 10).
Secondary psoas abscess is caused by the spread from an adjacent infectious process; in the study of the Japanese group of Wong et al. infectious spondylitis, among all the causes, was found to be the most common for secondary psoas abscess (11). Pyogenic spondylodiscitis is indicated as one of the most frequent cause of secondary psoas abscess in many others studies. In fact, Ricci et al. noted that 10% of secondary psoas abscess cases were caused by disc infection (9); Walsh et al. reported 4 out of 11 patients with an iliopsoas abscess who had lumbar osteomyelitis or disc space infections (8) and Muckley et al. emphasized the spine as the source of infection for a secondary psoas abscess (4). Wong et al (11) also noted that spondylitis is the main manifestation of haematogenous osteomyelitis in middle-aged patients (>50 years old), with S. Aureus involved in most cases. The reported case is in line with this evidence. Besides, the literature support to think this infection been primarily originated in the lumbar spine, because a psoas abscess only rarely extends proximally (1).
Due to nonspecific symptoms, diagnosis of psoas abscess is frequently missed at initial presentation in the emergency room. Most patients complain back, hip or flank pain and this may lead to misdiagnoses of sciatica, arthritis or joint infection. Only few patients present the classical triad of fever, back pain and a groin or flank mass. Often, only with aggravating symptoms (progressive back pain, weight loss, unilateral leg swelling, loss of hip extension) further examinations are taken. Furthermore, initial antibiotic treatment may compromise early diagnoses through amelioration of symptoms and signs of infection. Common laboratory findings with psoas abscess include leukocytosis, elevated ESRs, elevated blood urea nitrogen levels and pyuria. Elevation of the CRP level usually corresponds to the extent of infection (4).
Kumagai et al. (1) proposed some infection pathways from psoas abscesses into the hip joint. One of these was through the iliopsoas bursa: this structure has been found to communicate with the hip joint in many examined cadavers (5). One more pathway proposed is the spread along the iliopsoas muscle, which crosses the hip joint capsule at the thinnest portion between the iliofemoral and iliopubic ligaments (3). We consider that in the reported case the infection started as hematogenous spondylodiscitis, spreading distally through the psoas muscle as an ossifluent abscess and then penetrated the hip joint via the iliopsoas bursa. This hypothesis seems to be likely looking at the imaging.
Radiologic patterns for psoas abscess (loss of psoas shadow, abnormal soft-tissue shadows, gas inclusions, bony destruction of the spine and abscess calcification) are not consistently found.
For diagnostic imaging of psoas abscesses, CT has been established as the standard imaging study to assess the characteristics and extent of an abscess and diagnostic rates of 88-100% are reported(12). Besides, accurate CT imaging can demonstrate any co-existing causative retro- or intra-peritoneal disease (11).
Immediately following the diagnosis of iliopsoas abscess, a prompt treatment is mandatory: it consists in abscess drainage (surgical or percutaneous) and appropriate antimicrobial therapy (12). For secondary abscess, it is essential to associate abscess drainage with causative treatment of the primary infectious focus: drainage alone may result in recurrence rates up to 50% (4).
In the reported case the severe complication occurred of a septic hip arthritis followed by a femoral head osteonecrosis was probably due to a delayed diagnosis and a missed immediate abscess drainage, which led to a successful but prolonged antibiotic therapy, finally requiring the implantation of a THA for the severe degenerative hip changes, with a doubtful long-term implant survival.
Conclusion
Diagnoses for lumbar spine infection and psoas abscess are difficult and often delayed, as the symptoms of both are non-specific (1). A high degree of suspicious in necessary to achieve early diagnosis of psoas abscess in older patients with nonspecific symptoms. In patients with infection signs and back or hip pain or history of spinal surgery, psoas abscess should always be considered.
In case of psoas abscess, early diagnosis is crucial because any delayed treatment can result in poor results (2, 8, 9).
Orthopedic surgeons should know that both the lumbar spine and hip joint communicate through the psoas muscle, making it possible for infection to spread. Thus, patients with suspect of infection in those areas needs an early investigation through MRI or CT scan in order to determine the extension of the infection.
CT-guided percutaneous catheter drainage or surgical drainage with appropriate antibiotic therapy represents an effective treatment in most patients to prevent further complications.
Conflict of interest:
Each author declares that he or she has no commercial associations (e.g. consultancies, stock ownership, equity interest, patent/licensing arrangement etc.) that might pose a conflict of interest in connection with the submitted article
References
- 1.Kumagai K, Ushiyama T, Kawasaki T, Matsusue Y. Extension of lumbar spine infection into osteoarthritic hip through psoas abscess. J Orthop Sci. 2005;10:91–94. doi: 10.1007/s00776-004-0847-7. [DOI] [PubMed] [Google Scholar]
- 2.Gruenwald I, Abrahamson J, Cohen O. Psoas abscess: case report and review of the literature. J Urol. 1992;147:1624–6. doi: 10.1016/s0022-5347(17)37650-4. [DOI] [PubMed] [Google Scholar]
- 3.Levitin B, Rubin LA, Rubenstein JD. Occult retroperitoneal abscess presenting as septic arthritis of the hip. J Rheumatol. 1982;9:904–8. [PubMed] [Google Scholar]
- 4.Muckley T, Schütz T, Kirschner M, et al. Psoas abscess: the spine as a primary source of infection. Spine. 2003;28:E106–13. doi: 10.1097/01.BRS.0000050402.11769.09. [DOI] [PubMed] [Google Scholar]
- 5.Beredjiklian PK, Adler L, Wong K, et al. Prevertebral abscess with extension into the hip joint. Am J Orthop. 2001;30:572–5. [PubMed] [Google Scholar]
- 6.Mallick IH, Thoufeeq MH, Rajendran TP. Iliopsoas abscesses. Postgrad Med J. 2004;80:459–62. doi: 10.1136/pgmj.2003.017665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chern CH, Hu SC, Kao WF, et al. Psoas abscess: making an early diagnosis in the ED. Am J Emerg Med. 1997;15:83–8. doi: 10.1016/s0735-6757(97)90057-7. [DOI] [PubMed] [Google Scholar]
- 8.Walsh TR, Reilly JR, Hanley E, et al. Changing etiology of iliopsoas abscess. Am J Surg. 1992;163:413–6. doi: 10.1016/0002-9610(92)90043-q. [DOI] [PubMed] [Google Scholar]
- 9.Ricci MA, Rose FB, Meyer KK. Pyogenic psoas abscess: worldwide variations in etiology. World J Surg. 1986;10:834–43. doi: 10.1007/BF01655254. [DOI] [PubMed] [Google Scholar]
- 10.Kaku N, Tsumura H, Takashita M, et al. Two cases of pyogenic coxitis following pyogenic spondylitis. Orthop Traumatol (Seikei Geka To Saigai Geka) 2000;49:1015–20. in Japanese. [Google Scholar]
- 11.Wong OF, Ho PL, Lam SK. Retrospective review of clinical presentations, microbiology, and outcomes of patients with psoas abscess. Hong Kong Med J. 2013;19:416–23. doi: 10.12809/hkmj133793. [DOI] [PubMed] [Google Scholar]
- 12.Santaella RO, Fishman EK, Lipsett PA. Primary vs secondary iliopsoas abscess: presentation, microbiology and treatment. Arch Surg. 1995;130:1309–13. doi: 10.1001/archsurg.1995.01430120063009. [DOI] [PubMed] [Google Scholar]


