Abstract
Background and aim:
The medial patellofemoral ligament (MPFL) is the most important structure commonly injured during lateral patellar dislocation and its rupture accounts for 3% of total knee injuries. MPFL reconstruction (MPFLR) is a reliable procedure with good results but variable rates of recurrent instability. The aim of this study is to underline the proper indications for the MPFLR reconstruction and to explain all the pearls and pitfalls regarding the MPFLR both in our experience and found in the latest literature.
Methods:
A comprehensive search in the latest literature using various combinations of the keywords MPFL, MPFLR, dislocation, treatment was performed. The following data were extracted: diagnosis methods, indications and contraindications for isolated MPFLR, type of management, recurrence of instability, outcomes and complications.
Results:
History of multiple patellar dislocations is the most relevant indication for ligament reconstruction especially after a failed course of conservative treatment in presence of persistent patello-femoral instability. Gold standard technique for MPFLR has not been clearly defined yet.
Conclusions:
There is still poor literature about outcome comparisons, therefore it is challenging to decide which technique is the most appropriate as surgical procedures are continuously developing. The ideal candidates for MPFLR have to be decided after a throughout evaluation and careful planning and, with nowadays knowledge, it is possible to put indication for a reconstruction exposing the patient to minimal risks. (www.actabiomedica.it)
Keywords: MPFL, MPFLR, patello-femoral instability, patellar dislocation, MPFL reconstruction
Introduction
The MPFL is the most important structure commonly injured during lateral patellar dislocation. The typical injury pattern that leads to a patellar dislocation consists in a trauma without direct contact, with the knee performing a movement in flexion, internal rotation and with application of a valgus force.
MPFL lesions account for 3% of total knee injuries. It is commonly found in young females between 10-17 years old, probably due to a major ligamentous laxity and a minor support from the muscular mass compared to the male gender (1). Other predisposing factors for patellar dislocation may include patella alta, lateral patellar tilt, trochlear dysplasia, increased Q-angle, genu valgum, vastus medialis muscle hypoplasia, ligament hyperlaxity, external tibial torsion, subtalar joint pronation and increased femoral anteversion (2).
Rupture of the MPFL typically occurs at the femoral origin. Associated tearing of the vastus medialis oblique (VMO) and the medial retinaculum may also occur with dislocation of the patella, as the MPFL and VMO share common meshing fibers. Additionally, osteochondral fractures may be seen with dislocation as the patella impacts the femur (1,3).
Up to 10 years ago, there was not a reliable surgical treatment for patellar luxation. In the recent years MPFLR configures as the best option, for suitable patients, to regain the pre-lesion activity. Along with the MPFL there are other neighboring structures that prevent lateral displacement of the patella. For instance, the VMO is a patellar dynamic stabilizer; Its contraction aids the proper patellar tracking in the trochlea groove (3). Multiple anatomic and biomechanical studies have proved the MPFL performs its restraining action in the range of movements from full knee extension (0°) until the patella engages the trochlear groove (at roughly 30°) which corresponds to the “Screw Home Mechanism” (1,4).
More recently the roles of the other medial soft tissue restraints have been highlighted. The medial quadriceps tendon-femoral ligament (MQTFL), the medial patella-tibial ligament (MPTL), the medial patella-meniscal ligament (MPML), and the VMO have distinct yet closely related functions to MPFL that contribute to medial patella support, and many new reconstruction techniques have emerged that use the isolated or combined reconstruction of the different knee medial ligamentous structures (5).
The aim of this study is to underline the proper indications for the MPFLR since there are many conditions that are not suitable for this specific procedure. Moreover, our purpose is to explain all the pearls and pitfalls regarding the MPFLR both in our experience and found in the latest literature.
Methods
We performed a comprehensive search of the latest literature using various combinations of the keywords MPFL, MPFLR, patellar dislocation and patellar dislocation treatment. We then extracted the following data to underline the proper indications and explain all the pearls and pitfalls regarding the MPFLR. In addition, we included a small chapter on the anatomy of the interested area to give a better understanding of the MPFL and the surrounding structures.
Anatomy
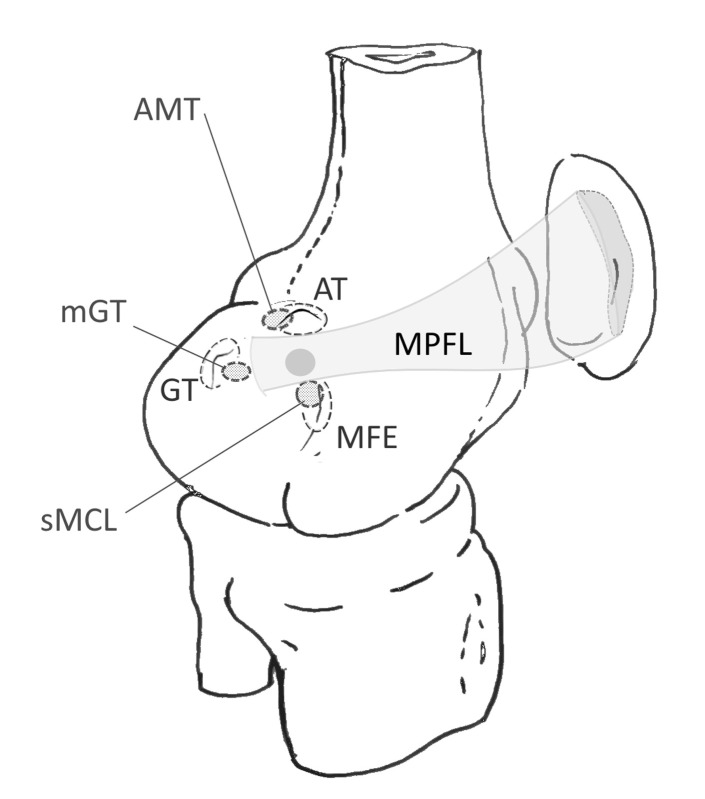
Nomura et al. (6), in a study on a total of 20 knee specimens, reported a description of the MPFL. The length was 58.8 ± 4.7 mm, while the width and thickness were respectively 12 ± 3.1 mm and 0.44 ± 0.19 mm at the middle point. Two functional bundles were described: an inferior-straight and a superior oblique one, with the latter closely associated to the VMO. (6) The structures of the MPFL originate from the medial femoral condyle, just distal to the adductor tubercle and proximal to the attachment of the medial collateral ligament (MCL) and insert on the medial and superior margin of the patella. The superior fibers merge with the patellar tendon and the VMO (Figure 1) (1,3,6-8).
Figure 1.
MPFL attachment areas in darker shading; AT Adductor Tubercle; AMT Adductor Magnus Tendon; GT Gastrocnemius Tubercle; mGT medial Gastrocnemius Tendon; sMCL superficial Medial Collateral Ligament; MFE Medial Femoral Condyle.
The medial patellar stabilizers, as already stated, are composed of the medial retinaculum the MPFL, the MQTFL, the MPTL, the MPML, and the VMO.
MQTFL is a separate independent anatomic structure which extends from the distal deep quadriceps tendon to the adductor tubercle region, just proximal to the MPFL insertion, which ensures a static connection between the medial femur and the extensor mechanism of the anterior knee throughout the ROM. (9) The proximal medial patello-femoral complex (MPFC) consists of the MPFL and the MQTFL (10).
In the coronal plane there are 6 degrees of valgus between femur and tibia, and a similar angle is present between the trochlear groove and the anterior tibial tubercle. Due to these, there is a lateral force vector acting on the patella while the quadriceps contracts. The MPFL is the main medial stabilizer of the patella, providing about 50-60% of the counteracting mechanism (3,6,11-13).
Dejour and Lecoutre (14) first described the condition known as trochlear dysplasia, which is a congenital condition consisting in a progressive filling of the trochlear groove and leads to displacement of the patella even during the normal mobility of the knee. Trochlear dysplasia presents with MPFL laxity and subsequent multiple patellar dislocations.
Diagnosis
Clinical examination is essential, and it is the first step to take to formulate a diagnosis. In case there is a dislocated patella it is necessary to reduce it by fully extending the affected knee and medializing a lateralized patella. In case this is an inaugural trauma it is likely for the patient to experience hemarthrosis which can be drained; by drawing blood we relieve the pain and facilitate the following clinical and radiological examinations (1).
Physical examination consists in evaluation of range of motion, apprehension sign and pain with patellar compression. If we divide the patella in 4 areas longitudinally on the coronal plane and have more than 2 of lateralization it is a positive sign of patellar instability (1,3,6,10).
In the acute setting, patients with MPFL rupture will present with pain and tenderness along the medial retinaculum. There may also be a block to motion due to an osteochondral fragment displacement. The presence of apprehension with lateralization of the patella and the absence of a firm end point to lateral translation suggests previous dislocation and damage to MPFL.
A classic antero-posterior (AP) view x-ray can be useful to evaluate the bone quality and correct alignment but not a direct correlation with patello-femoral instability. A true lateral, on the other hand, shows radiographic signs of trochlea dysplasia, such as: the crossing sign and the double contour (16). The Merchant view (weight bearing with knees at 45° of flexion) grants the possibility to evaluate the patello-femoral alignment and can also reveal bone avulsion from the medial side of the patella (3).
In order to confirm the diagnosis, it is necessary an MRI to directly study the MPFL and the remaining medial stabilizers of the knee (Figure 2-3) (1).
Figure 2.
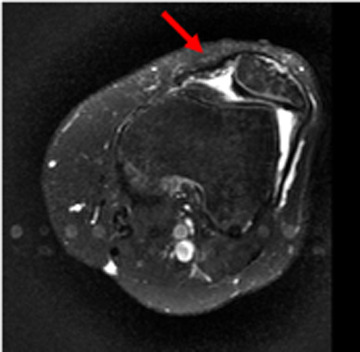
Left Knee MPFL injury of a 34years old man. A transverse T2-FSE MR image of the knee shows attenuation of signal of the MPFL.
Figure 3.

Right Knee MPLF injury of a 41years old woman. A transverse T2 MR image of the knee obtained at the level of the MPFL patellar insertion shows complete avulsion of the MPFL from its patellar insertion.
In case we suspect underlying knee conditions closely related to the injury that are identified as contraindications for MPFL reconstruction, such as trochlea dysplasia or tibial tubercle misalignment, the CT scan following the Lyon protocol can facilitate the diagnosis.
Classification
MPFL injuries have been classified into four categories based on location either at the level of the MPFL patellar insertion, within the mid-substance of the ligament, at the femoral origin, or in more than one location. Patellar insertion MPFL injuries can be further subdivided into three categories: type P0 with purely ligamentous disruption, type P1 with a bony avulsion fragment, and type P2 with bony avulsion involving the articular surface of the medial facet of the patella. A schematic representation of the latter classification is reported in Figure 4 (2).
Figure 4.
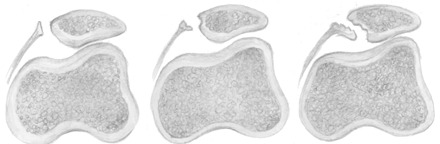
Three types of patellar MPFL injuries: a type P0 with ligamentous disruption at the patellar attachment; b type P1 with bony avulsion fracture from medial margin of the patella; c type P2 with bony avulsion involving articular cartilage from the medial facet of the patella.
Patellar MPFL avulsion injury comprised two different types of osteochondral avulsion fractures: P1 without articular cartilage involvement (only bone from medial patellar margin) and P2 with articular cartilage involvement (medial patellar facet articular surface). In chronic instability cases, medial patellar ossicles can occasionally be observed as a sign of previous patellar MPFL avulsion fracture.
Between 40 and 90 % of MPFL injuries are located in the femoral attachment, whereas some studies have reported figures up to 50 to 60 % at the patellar insertion (17-19).
Indications
According to the latest literature the most common indication for isolated Medial Patellar-Femoral Ligament Reconstruction is recurrent patello-femoral instability (20-22), while common reasons for not performing it include bony malalignment, trochlear dysplasia and patella alta.
MPFLR in presence of patello-femoral instability is usually indicated after 2 or more episodes of patellar dislocation; while MPFLR after the first episode of dislocation is sometimes considered, depending on the authors, in presence of ongoing symptoms of instability (as lateral subluxation), osteochondral fracture or failure of conservative management, such as bracing and physiotherapy.
Many authors set many other indications for isolated MPFLR (Table 1), such as symptomatic patellar-femoral instability associated with pain, positive physical examination findings, positive imaging, and participation in sport (22-25).
Table 1.
Indications for isolated MPFLR
| Recurrent patellar instability |
| Failed conservative measures |
| Primary patellar dislocation |
| Patellar instability— positive clinical examination |
| Patellar dislocations |
| - With ongoing instability symptoms |
| - Associated osteochondral fracture |
| Painful subluxation |
| - Excessive lateral mobility/laxity on examination |
| - Positive patellar apprehension |
| Patellar instability—Imaging positive CT-MRI |
| Loose osteochondral lesion |
| Participation in sports |
Gold standard treatment for MPFLR have not been clearly defined yet. Surgical techniques are continuously developing, and the relative credits versus non-operative management will become clear as more data become available. In the meantime, there are certain principles to which the orthopedic surgeon should adhere to perform an MPFLR:
Evaluate each patient for factors that predispose to patellar instability;
The location of injury to the MPFL should be identified and the repair should be focused on this site if possible;
Based on the available literature, open techniques seem to outperform arthroscopic ones. Proper tensioning of the MPFL is critical. Overtightening of the MPFL should be avoided.
Suture repairs should be stout, and anchors used to further strengthen the repair when feasible. In a bio-mechanical evaluation, MPFL repairs using suture anchors in addition to sutures failed at 142 N, whereas suture repair alone failed at 37 N (15).
The ideal candidate for an isolated MPFLR should fit the following profile (15), with regards to potential risk factors for recurrent patellar dislocation:
- Trochlear morphology: normal or type A dysplasia
- Tibial tuberosity–trochlear sulcus angle of 0 to 5° valgus or a tibial tuberosity-trochlear groove distance less than 20 mm with the knee at 0° of flexion
- No excessive increase in the patellar height ratio (Caton-Deschamps index <1.2 or Insall-Salvati index <1.4)
- Patellar tilt less than 20° when measured on an axial image, using the posterior femoral condyles as a reference line, or some tilt but no lateral tightness on physical examination with the patella reduced
In presence of underlying causes, isolated MPFLR is not recommended because without the resolution of the underlying condition, there would not be benefit for the patient (Table 2).
Table 2.
Reasons to not perform an isolated MPFLR
| Bony malalignment |
| - Excessive femoral anteversion |
| - Increased knee valgus angle |
| - Increased Q-angle |
| - Excessive tibial torsion |
| - Increased TT-TG distance |
| - Abnormal pelvic geometry |
| - Abnormal hind foot position |
| Dysplasias |
| - Trochlear dysplasia |
| - Patellar dysplasia |
| Patella alta |
| Neurogenic abnormality |
| General ligamentous laxity |
| Contralateral patellar instability |
| Obesity |
| Patellofemoral arthrosis |
| Severe osteochondral lesion |
| Patellofemoral arthritis |
| Other ligamentous or meniscal injury |
| Patellofemoral crepitus |
| Associated fractures |
| Inability to comply to treatment protocol |
| Joint infection |
In this perspective, bony malalignment is the most common reason for not performing an isolated MPFLR. There is no agreement between authors for the specific Q angle, according to different authors the cut-off spans from a minimum of 15° to 25° (23,26-27). In presence of an increased tibial tubercle-trochlear groove (TT-TG) distance there is no indication to perform an isolated MPFLR. Even in this case there is no agreement in literature for a specific distance threshold since multiple cut-offs are reported: 22mm (28), 20mm (29), and 15mm (22).
Other malalignments are stated as reasons to avoid an isolated MPFLR, among these we find increased knee valgus, excessive femoral anteversion (EFA) and excessive tibial torsion (ETT). Even for these there is not a univocal threshold, in fact different cutoffs are considered for the knee valgus, (greater than 10, 7 or 5° (22, 25, 30)), and for EFA (greater than 35 or 20°) (22, 31).
Patella alta is often considered as a contraindication for isolated MPFLR, and as before, different cut-offs are set by different authors: accounting the Insall-Salviati ratio, there is a threshold that varies from 1.2 to 1.3 mm (25,32). Whereas the Caton-Deschamps index presented cut-offs from 1.2 to 1.35 mm (33,34).
Dysplasia of both the trochlea and patella are described as a contraindication to perform an isolated MPFLR, and the Authors do not agree with the specific amount of dysplasia. In case of trochlear dysplasia, a trochlear-sulcus angle greater than 150° (23) or 145° (32) can be considered viable for surgery.
Discussion
An injury to the MPFL occurs with a rate between 94-100% following a patellar dislocation (3,6,11). Traumatic lesions to this ligament, if not treated, can lead to recurring dislocation in 14-44% of cases, osteochondral lesions and, eventually, to early osteoarthritis (35). In order to avoid any future complication, a surgical procedure to re-establish the normal anatomy, is mandatory due to the high chances to experience more recurrent episodes of dislocation compared to conservative treatments of any sort (11).
According to a 2015 Cochrane review, the difference between non-operative and operative treatment it is not in the functional scores, which are similar, but in a lower risk of recurrent dislocations with surgery at the price of surgical complications (36). As already stated, it is strong opinion for patients who experience multiple patellar dislocations, to undergo MPFL reconstruction. This might be the most relevant indication for ligament reconstruction (20,23,36) especially after a failed course of conservative treatment. Usually only elite athletes undergo MPFLR after only one dislocation.
Patella alta, trochlear dysplasia or increased TT-TG distance are predisposing factors which can definitely spike the risk of traumatic first events but at the same time their recurrency (3,4,12,29). All the aforementioned conditions preclude the possibility of a simple MPFL reconstruction due to a high risk of re-rupture of the graft. Therefore, associated procedures must be performed to decrease the likelihood of re-injury. It is not in the purpose of this paper to discuss trochleoplasty or tibial tubercle transposition, but persistent instability beyond 30° of knee flexion suggests bony malalignment (29,37).
Around 130 surgical techniques have been proposed since 1915, the year of the first ever published manuscript about this topic (21,38-39), and there is no universal consensus yet about the best procedure. In fact, multiple variations in graft sources have been suggested in literature, including semitendinous, gracilis, partial quadriceps, partial patellar tendon, allograft or artificial tendons (40-41), and none of them proved to have better results over the others. Moreover, there are variations in both patellar and femoral fixation and angle of knee flexion during fixation. Because of the many variables, it is still an endeavor to find the best surgical treatment, even though the technique has been refined thanks to a better understanding of the origin and insertion of the ligament.
Fortunately, the surgical procedures are more reproducible because there is consensus about the necessity to recreate an accurate and isometric ligament through an anatomical placement, especially, of the femoral bone tunnel (15,43). The Schöttle point, this is the exact area where to place the femoral tunnel during the reconstruction procedure in order to restore the isometry of the ligament (44).
As stated, every technique has its complications. In literature, sutures for MPFL are considered easier to be performed but are not as stable as trans-patellar bone tunnels (24% vs 8.6% of hypermobility respectively). On the other hand, bone tunnels carry the risk of iatrogenic fractures (0,9-3.6%) and highest complication rate (21.6%) (11,45-46).
Overall the cumulative rate of complications following reconstruction is 26.1% according to Shah et al. (46) which might be affected by possible misdiagnosed predisposing conditions and, especially, by technical errors that account for 50% of graft failures.
Re-dislocations following a reconstruction have a low and variable rate. In the cohort of 209 patients evaluated by Howells et al. (21) the re-dislocation rate was a surprising 0% with a single patellar tunnel technique and the use of a suspensory button. Mayer et al. (45) had only 3 cases out of 104 (2,9%) using an implant-free V-shaped patellar tunnel. While Enderlein et al. (40) experienced a 4.5% in a pool of 240 cases with a particular type of transpatellar tunnel and no graft fixation.
Conclusion
In conclusion there is still sparse literature about outcome comparisons, therefore it is challenging to decide which technique is the most appropriate. At the same time the ideal candidates for MPFL reconstruction have to be decided after a throughout evaluation and careful planning. In the past predisposing pathologies were overlooked but, with nowadays knowledge, it is possible to put indication for a reconstruction exposing the patient to minimal risks.
Diclosures:
Each author declares that he or she has no commercial associations (e.g. consultancies, stock ownership, equity interest, patent/licensing arrangement etc.) that might pose a conflict of interest in connection with the submitted article
Conflict of interest:
Each author declares that he or she has no commercial associations (e.g. consultancies, stock ownership, equity interest, patent/licensing arrangement etc.) that might pose a conflict of interest in connection with the submitted article
References
- 1.Rosinski A, Chakrabarti M, Gwosdz J, McGahan PJ, Chen JL. Double-Bundle Medial Patellofemoral Ligament Reconstruction With Allograft. Arthrosc Tech. 2019 May;8(5):e513–e520. doi: 10.1016/j.eats.2019.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sillanpaa PJ. First-time patellar dislocation: surgery or conservative treatment. Sport Med Arthrosc. 2012;20(3):128–135. doi: 10.1097/JSA.0b013e318256bbe5. [DOI] [PubMed] [Google Scholar]
- 3.Duthon VB. Acute traumatic patellar dislocation. Orthop Traumatol Surg Res. 2015 Feb;101 doi: 10.1016/j.otsr.2014.12.001. [DOI] [PubMed] [Google Scholar]
- 4.Sanchis-Alfonso V. How to Deal With Chronic Patellar Instability: What Does the Literature Tell Us. Sports Health. 2016 Jan-Feb;8(1):86–90. doi: 10.1177/1941738115604156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.LaPrade MD, Kallenbach SL, Aman ZS, et al. Biomechanical evaluation of the medial stabilizers of the patella. Am J Sports Med. 2018;46:1575–1582. doi: 10.1177/0363546518758654. [DOI] [PubMed] [Google Scholar]
- 6.Nomura E, Inoue M, Osada N. Anatomical analysis of the medial patellofemoral ligament of the knee, especially the femoral attachment. Knee Surg Sports Traumatol Arthrosc. 2005 Oct;13(7):510–5. doi: 10.1007/s00167-004-0607-4. [DOI] [PubMed] [Google Scholar]
- 7.Kang HJ, Wang F, Chen BC, Su YL, Zhang ZC, Yan CB. Functional bundles of the medial patellofemoral ligament. Knee Surg Sports Traumatol Arthrosc. 2010 Nov;18(11):1511–6. doi: 10.1007/s00167-010-1090-8. [DOI] [PubMed] [Google Scholar]
- 8.Fujino K, Tajima G, Yan J, Kamei Y, Maruyama M, Takeda S, Kikuchi S, Shimamura T. Morphology of the femoral insertion site of the medial patellofemoral ligament. Knee Surg Sports Traumatol Arthrosc. 2015 Apr;23(4):998–1003. doi: 10.1007/s00167-013-2797-0. [DOI] [PubMed] [Google Scholar]
- 9.John P, Fulkerson M.D. Medial Quadriceps Tendon Femoral Ligament: Surgical Anatomy and Reconstruction Technique to Prevent Patella Instability Arth Tech. 2013;2(2):125–128. doi: 10.1016/j.eats.2013.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Espregueira-Mendes J, Andrade R. Combined Soft Tissue Reconstruction of the Medial Patellofemoral Ligament and Medial Quadriceps TendoneFemoral Ligament. Arthroscopy Techniques. doi: 10.1016/j.eats.2019.01.006. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hendawi T, Godshaw B, Flowers C, Stephens I, Haber L, Waldron S. Autograft vs Allograft Comparison in Pediatric Medial Patellofemoral Ligament Reconstruction. Ochsner J. 2019 Summer;19(2):96–101. doi: 10.31486/toj.18.0081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yeung M, Leblanc MC, Ayeni OR, Khan M, Hiemstra LA, Kerslake S, Peterson D. Indications for Medial Patellofemoral Ligament Reconstruction: A Systematic Review. J Knee Surg. 2016 Oct;29(7):543–554. doi: 10.1055/s-0035-1564730. [DOI] [PubMed] [Google Scholar]
- 13.Krebs C. The medial patellofemoral ligament: Review of the literature. J Ortho. 2018;15 doi: 10.1016/j.jor.2018.05.004. 596-599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dejour DRP, Lecoultre B. Douleur et instabilité rotulienne: essai de classification. Med Hyg. 1998;5:1466–70. [Google Scholar]
- 15.Wang CH, Ma LF, Zhou JW, Ji G, Wang HY, Wang F, Wang J. Double-bundle anatomical versus single-bundle isometric medial patellofemoral ligament reconstruction for patellar dislocation. Int Orthop. 2013 Apr;37(4):617–24. doi: 10.1007/s00264-013-1788-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Scott W.N, et al. Insall & Scott. Surgery of the knee. (Sixth edition) 2018 [Google Scholar]
- 17.Guerrero P. Medial patellofemoral ligament injury patterns and associated pathology in lateral patella dislocation: an MRI study. Sports Med Arthrosc Rehabil Ther Technol. 2009;1:17. doi: 10.1186/1758-2555-1-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kepler CK. Zone of injury of the medial patellofemoral ligament after acute patellar dislocation in children and adolescents. Am J Sports Med. 2011;39:1444–1449. doi: 10.1177/0363546510397174. [DOI] [PubMed] [Google Scholar]
- 19.Weber-Spickschen TS. The relationship between trochlear dysplasia and medial patellofemoral ligament rupture location after patellar dislocation: an MRI evaluation. Knee. 2011;18(3):185–188. doi: 10.1016/j.knee.2010.04.002. [DOI] [PubMed] [Google Scholar]
- 20.Csintalan RP, Latt LD, Fornalski S, Raiszadeh K, Inacio MC, Fithian DC. Medial patellofemoral ligament (MPFL) reconstruction for the treatment of patellofemoral instability. J Knee Surg. 2014 Apr;27(2):139–46. doi: 10.1055/s-0033-1360652. [DOI] [PubMed] [Google Scholar]
- 21.Howells NR, Barnett AJ, Ahearn N, Ansari A, Eldridge JD. Medial patellofemoral ligament reconstruction: a prospective outcome assessment of a large single centre series. J Bone Joint Surg Br. 2012 Sep;94(9):1202–8. doi: 10.1302/0301-620X.94B9.28738. [DOI] [PubMed] [Google Scholar]
- 22.Ma LF, Wang F, Chen BC, Wang CH, Zhou JW, Wang HY. Medial retinaculum plasty versus medial patellofemoral ligament reconstruction for recurrent patellar instability in adults: a randomized controlled trial. Arthroscopy. 2013;29(5):891–897. doi: 10.1016/j.arthro.2013.01.030. [DOI] [PubMed] [Google Scholar]
- 23.Mehta VM, Inoue M, Nomura E, Fithian DC. An algorithm guiding the evaluation and treatment of acute primary patellar dislocations. Sports Med Arthrosc Rev. 2007;15(2):78–8. doi: 10.1097/JSA.0b013e318042b695. [DOI] [PubMed] [Google Scholar]
- 24.Ronga M, Oliva F, Longo UG, Testa V, Capasso G, Maffulli N. Isolated medial patellofemoral ligament reconstruction for recurrent patellar dislocation. Am J Sports Med. 2009;37(9):1735–1742. doi: 10.1177/0363546509333482. [DOI] [PubMed] [Google Scholar]
- 25.Hiemstra LA, Kerslake S, Kupfer N, Lafave M. Patellofemoral Stabilization: Postoperative Redislocation and Risk Factors Following Surgery. Orthop J Sports Med. 2019 Jun;7(6):2325967119852627. doi: 10.1177/2325967119852627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hiemstra LA, Kerslake S, Kupfer N, Lafave M. Patellofemoral Stabilization: Postoperative Redislocation and Risk Factors Following Surgery. Orthop J Sports Med. 2019 Jun;7(6):2325967119852627. doi: 10.1177/2325967119852627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Drez D, Jr, Edwards TB, Williams CS. Results of medial patellofemoral ligament reconstruction in the treatment of patellar dislocation. Arthroscopy. 2001;17(3):298–306. doi: 10.1053/jars.2001.21490. [DOI] [PubMed] [Google Scholar]
- 28.Lippacher S, Dreyhaupt J, Williams SR, Reichel H, Nelitz M. Reconstruction of the medial patellofemoral ligament: Clinical outcomes and return to sports. Am J Sports Med. 2014;42(7):1661–1668. doi: 10.1177/0363546514529640. [DOI] [PubMed] [Google Scholar]
- 29.Zhou JW, Wang CH, Ji G, Ma LF, Wang J, Zhang F, Dong JT, Wang F. A minimally invasive medial patellofemoral ligament arthroscopic reconstruction. Eur J Orthop Surg Traumatol. 2014 Feb;24(2):225–30. doi: 10.1007/s00590-012-1162-1. [DOI] [PubMed] [Google Scholar]
- 30.Ellera Gomes JL, Stigler Marczyk LR, César de César P, Jungblut CF. Medial patellofemoral ligament reconstruction with semitendinosus autograft for chronic patellar instability: a follow-up study. Arthroscopy. 2004;20(2):147–151. doi: 10.1016/j.arthro.2003.11.006. [DOI] [PubMed] [Google Scholar]
- 31.Hinterwimmer S, Imhoff AB, Minzlaff P, et al. Anatomical two-bundle medial patellofemoral ligament reconstruction with hardware-free patellar graft fixation: technical note and preliminary results. Knee Surg Sports Traumatol Arthrosc. 2013;21(9):2147–2154. doi: 10.1007/s00167-013-2498-8. [DOI] [PubMed] [Google Scholar]
- 32.Panni AS, Alam M, Cerciello S, Vasso M, Maffulli N. Medial patellofemoral ligament reconstruction with a divergent patellar transverse 2-tunnel technique. Am J Sports Med. 2011;39(12):2647–2655. doi: 10.1177/0363546511420079. [DOI] [PubMed] [Google Scholar]
- 33.Raghuveer RK, Mishra CB. Reconstruction of medial patellofemoral ligament for chronic patellar instability. Indian J Orthop. 2012;46(4):447–454. doi: 10.4103/0019-5413.97259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Arendt EA, Dahm DL, Dejour D, Fithian DC. Patellofemoral joint: from instability to arthritis. Instr Course Lect. 2014;63:355–368. [PubMed] [Google Scholar]
- 35.Schöttle PB, Fucentese SF, Romero J. Clinical and radiological outcome of medial patellofemoral ligament reconstruction with a semitendinosus autograft for patella instability. Knee Surg Sports Traumatol Arthrosc. 2005 Oct;13(7):516–21. doi: 10.1007/s00167-005-0659-0. [DOI] [PubMed] [Google Scholar]
- 36.Smith TO, Donell S, Song F, Hing CB. Surgical versus non-surgical interventions for treating patellar dislocation. Cochrane Database Syst Rev. 2015 Feb 26;2:CD008106. doi: 10.1002/14651858.CD008106.pub3. [DOI] [PubMed] [Google Scholar]
- 37.Fujino K, Tajima G, Yan J, Kamei Y, Maruyama M, Takeda S, Kikuchi S, Shimamura T. Morphology of the femoral insertion site of the medial patellofemoral ligament. Knee Surg Sports Traumatol Arthrosc. 2015 Apr;23(4):998–1003. doi: 10.1007/s00167-013-2797-0. [DOI] [PubMed] [Google Scholar]
- 38.Buckens CF, Saris DB. Reconstruction of the medial patellofemoral ligament for treatment of patellofemoral instability: a systematic review. Am J Sports Med. 2010 Jan;38(1):181–8. doi: 10.1177/0363546509353132. [DOI] [PubMed] [Google Scholar]
- 39.Jibri Z, Jamieson P, Rakhra KS, Sampaio ML, Dervin G. Patellar maltracking: an update on the diagnosis and treatment strategies. Insights Imaging. 2019 Jun 14;10(1):65. doi: 10.1186/s13244-019-0755-1. doi: 10.1186/s13244-019-0755-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Enderlein D, Nielsen T, Christiansen SE, Faunø P, Lind M. Clinical outcome after reconstruction of the medial patellofemoral ligament in patients with recurrent patella instability. Knee Surg Sports Traumatol Arthrosc. 2014 Oct;22(10):2458–64. doi: 10.1007/s00167-014-3164-5. [DOI] [PubMed] [Google Scholar]
- 41.Schottle PB, Hensler D, Imhoff AB. Anatomical double bundle MPFL reconstruction with an aperture fixation. Knee Surg Sports Traumatol Arthrosc. 2010;18:147–151. doi: 10.1007/s00167-009-0868-z. [DOI] [PubMed] [Google Scholar]
- 42.Aframian A, Smith TO, Tennent TD, Cobb JP, Hing CB. Origin and insertion of the medial patellofemoral ligament: a systematic review of anatomy. Knee Surg Sports Traumatol Arthrosc. 2017 Dec;25(12):3755–3772. doi: 10.1007/s00167-016-4272-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Fujino K, Tajima G, Yan J, Kamei Y, Maruyama M, Takeda S, Kikuchi S, Shimamura T. Morphology of the femoral insertion site of the medial patellofemoral ligament. Knee Surg Sports Traumatol Arthrosc. 2015 Apr;23(4):998–1003. doi: 10.1007/s00167-013-2797-0. [DOI] [PubMed] [Google Scholar]
- 44.Schöttle PB, Schmeling A, Rosenstiel N, Weiler A. Radiographic landmarks for femoral tunnel placement in medial patellofemoral ligament reconstruction. Am J Sports Med. 2007 May;35(5):801–4. doi: 10.1177/0363546506296415. [DOI] [PubMed] [Google Scholar]
- 45.Mayer P, Schuster P, Schlumberger M, Eichinger M, Pfaff M, Immendörfer M, Richter J. Midterm Results after Implant-Free Patellar Fixation Technique for Medial Patellofemoral Ligament Reconstruction. J Knee Surg. 2019 Jul 3 doi: 10.1055/s-0039-1692654. [DOI] [PubMed] [Google Scholar]
- 46.Shah JN, Howard JS, Flanigan DC, Brophy RH, Carey JL, Lattermann C. A systematic review of complications and failures associated with medial patellofemoral ligament reconstruction for recurrent patellar dislocation. Am J Sports Med. 2012 Aug;40(8):1916–23. doi: 10.1177/0363546512442330. [DOI] [PMC free article] [PubMed] [Google Scholar]