Abstract
Background and aim of the work:
subcutaneous Achilles tendon lesions are common degenerative tendon tears, often related to sport activities, multiple pharmacotherapies and internal medical comorbidities. Neglect an Achilles tendon lesion can affect walk ability, while neglect a bilateral lesion could really lead to a serious limitation of self-sufficiency in daily living. We report a case of chronic bilateral Achilles tendon lesion successful treated with LARS augmentation, along with some clinical considerations concerning the clinical outcome.
Methods:
we report a case of a chronic bilateral Achilles tendon lesion in an elderly man with multiple comorbidities, successful treated with LARS reconstruction, along with some considerations concerning possible intraoperative issues and the clinical outcome.
Results:
good functional result was obtained as documented with pre and postoperative American Orthopedic Foot And Ankle Society Scale and the “Foot And Ankle Disability Index”, without complications.
Conclusions:
a bilateral Achilles tendon rupture is a very disabling pathology, that needs prompt diagnosis and treatment to prevent further complications. LARS reconstruction could be an effective method in selected patients to avoid some intraoperative issues related to patient comorbidities and ability to follow complex postoperative rehabilitation protocols. (www.actabiomedica.it)
Keywords: bilateral, Achilles tendon, lesion, chronic, LARS
Background and aim of the work
Achilles tendon rupture is increasing in time in younger and older patients and is mostly related to sport activities, chronic corticosteroids and fluoroquinolones therapy and internal medicine comorbidities (1, 2). Typically, this is a pathology more frequent in males between the third and fifth decade of life, with acute injuries occurring in younger patients (3). Diagnosis of Achilles tendon rupture is mostly clinical, consisting in finding a palpable gap in the Achilles tendon region and a positive Thompson test (4) related to the specific medical history; whereas in doubtful cases and to confirm the diagnosis ultrasonography or MRI should be performed (5).
A bilateral Achilles tendon rupture is a very disabling pathology, that needs prompt diagnosis and treatment, to ensure a fast and complete recovery to the patient (6).
In literature there are few descriptions of bilateral simultaneous Achilles tendon ruptures and neglected Achilles tendon rupture that can cause some problems to the patient and the surgeon in terms of a full functional recovery and surgical options (7,8); but it’s hard to find cases with both the conditions combined (9).
Various techniques are described for reconstructing chronic Achilles tendon lesions with autologous grafts and plasty, but these are not free of complications and often require a wide surgical exposure (10-13).
Materials and Methods
In June 2015 a 76 year old man came to our service (where at that time most of the authors were working) bringing a MRI of both legs, done few days earlier, showing a complete bilateral Achilles tendon rupture with large areas of tendinosis and a tendinous gap of 5 cm in the right and 4 cm in the left one.
The patient was able to walk independently, although with the help of two crutches and limping. Walking was achieved with flat foot step bilaterally and in absence of the push-off phase. The physical examination revealed a bilateral hypotrophy of the triceps surae muscles, a positive Thompson and Matles test and a palpable gap proximal to the distal insertion of the Achilles tendon bilaterally (Figure 1). In the same consult the patient revealed that the beginning of symptoms dated back in February of the same year, after feeling a strong pain in the right Achilles region, in the context of an accidental fall. Within a few days, he felt the same pain in the left Achilles region while walking up the stairs, consequently needing two crutches to walk.
Figure 1.

Clinical presentation and patient position on the operating table
The bilateral Achilles tendon lesions, related to those episodes, were misunderstood with simple ankle sprains by his primary care physician, and so treated with anti-inflammatory drugs, ice and ankle braces. Following failure to resolve symptoms the patient underwent to a specialist examination with a neurologist, which resulted negative.
Four months after the injury, persisting the gait abnormality, was prescribed a MRI of booth legs and the patient was addressed to our service, allowing us to diagnose the bilateral Achilles tendon rupture. The patient clinical history revealed a chronic atrial fibrillation treated with oral anticoagulants, an ascending aorta ectasia, a previous spontaneous pneumothorax, HCV in treatment with interferon, a hiatal hernia, a low grade of kidney failure, a BPH and a rheumatic polymyalgia in treatment with corticosteroids (5mg prednisone 1 pill per day) for more than 15 years.
In July 2015 in our service a bilateral surgical reconstruction of the Achilles tendon with implantation of one LARS per side was performed, with a one day hospitalization.
Intraoperatively (Figure 2) we found a tendinous gap as described in the MRI (5 cm in the right Achilles tendon and 4 cm in the left one), in presence of fatty degeneration of both tendon stumps, also beginning to involve the belly muscles of the triceps surae, conditions that could make dangerous the use of tendon plasty or transfers, thus necessitating the use of distal transosseus tunnels and interference screws in the calcaneus and proximal transfascial suture of the synthetic ligament (Figure 3). Postoperatively bilateral below knee plaster cast were made with the ankle in neutral position, allowing protected weight bearing with a walker for four weeks. At thirty days postoperatively we removed the plaster casts, allowing passive and active mobilization of the ankles to gain range of motion and muscles strengthening with protected weight bearing for thirty days more. At 60 days postoperatively the walker was substituted with crutches allowing complete weight bearing.
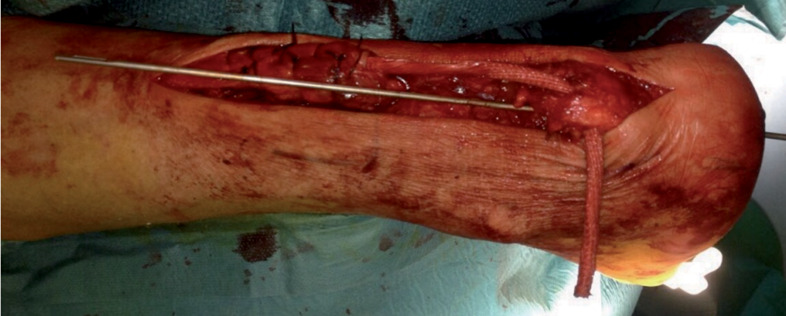
Figure 2.

Intraoperative view: remnants of ruptured native tendon
Figure 3.
Lars implantation: transosseus tunnel and transfascial proximal suture
Results
We made serial evaluations of disability according to the American Orthopedic Foot And Ankle Society Scale (AOFAS) and the “Foot And Ankle Disability Index” (FADI), preoperatively and postoperatively, listed below:
| AOFAS preoperatively: 43% | FADI preoperatively: 23,1 |
| AOFAS at 3 months: 50% | FADI at 3 months: 40 |
| AOFAS at 6 months: 85% | FADI at 6 months: 63,7 |
| AOFAS at 9 months: 87% | FADI at 9 months: 71,2 |
| AOFAS at 12 months: 92% | FADI at 12 months: 85,6 |
We also prescribed a control MRI at 8 months postoperatively showing apparently good LARS integration (Figure 4).
Figure 4.
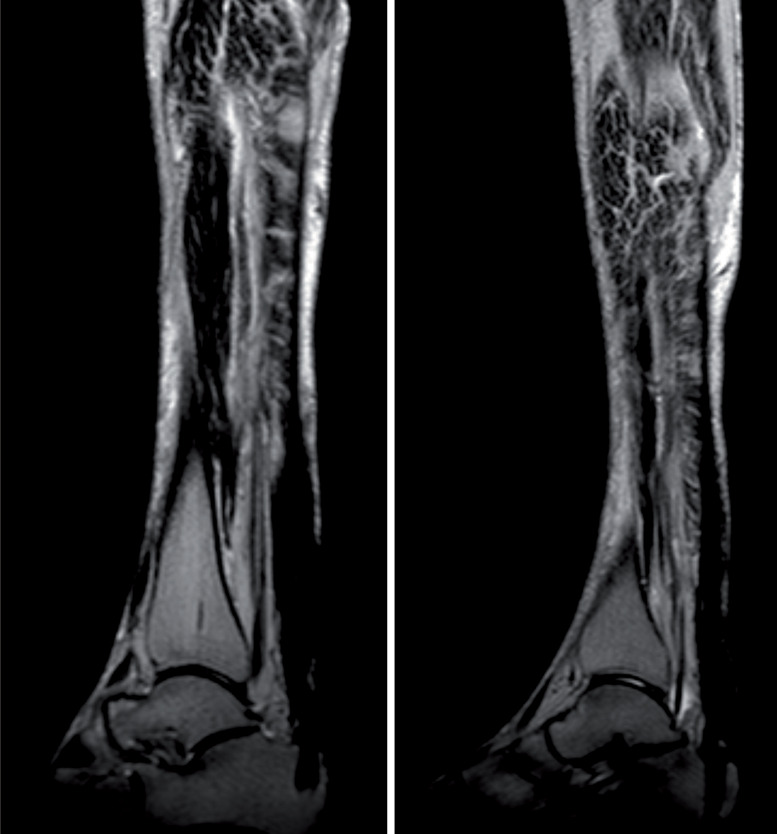
Two sagittal postoperative MRI view showing LARS integration in the calcaneus tunnel and fatty degeneration of calf muscles
Twelve months after the procedure, the patient gained a good autonomy level in walking and in daily life activities, being satisfied about the functional recovery and the surgery outcome (Figure 5).
Figure 5.

Postoperative active standing on forefoot
Interestingly however, persisted a subjective feeling of gait instability, referred by the patient as a sensation of “walking in the dark”, or “blinded”, especially on uneven grounds, needing a walking stick not to weight bear rather as a way to feel the ground. To investigate this disequilibrium we prescribed a new neurologic consult and a head CT, to rule out central or peripheral nervous degenerative disorders, obtaining a negative result.
Analyzing this condition, and starting from the knowledge that an Achilles tendon rupture produces a deficit in ankle proprioception (14) the most likely hypothesis was that we were in presence of a quite complete loss of proprioception previously conveyed by the Achilles tendons, now substituted by the synthetic ligaments.
In relation to this hypothesis therefore, we prescribed an intensive program of proprioceptive exercises, partially improving the symptoms.
Discussion and conclusions
The bilateral simultaneous Achilles tendon reconstruction with LARS allowed us to restore an anatomical entity by then degenerated, with a very short surgical time, avoiding large surgical dissection of soft tissues to harvest autologous tendons and complications related to surgical wounds healing, ensuring a hight primary weight bearing resistance (15,16).
All of these factors surely contributed to a good recovery, in a short time related to the pathology and the little patient ability to follow complex postoperative rehabilitation protocols, with a hight level of patient and surgeon satisfaction, avoiding dangerous postoperative complications.
LARS reconstruction could be an effective method in selected patients to avoid some intraoperative issues related to patient comorbidities and ability to follow complex postoperative rehabilitation protocols.
Anyway further studies should investigate the relationship between the use of synthetic ligaments in chronic Achilles tendon reconstruction and their influence on ankle proprioception.
Conflict of interest:
Each author declares that he or she has no commercial associations (e.g. consultancies, stock ownership, equity interest, patent/licensing arrangement etc.) that might pose a conflict of interest in connection with the submitted article
References
- 1.Hess G.W. Achilles tendon rupture: a review of etiology, population, anatomy, risk factors, and injury prevention. Foot ankle spec. 2010;3(1):29–32. doi: 10.1177/1938640009355191. [DOI] [PubMed] [Google Scholar]
- 2.Matsumoto K, Hukuda S, Nishioka J, Asajima S. Rupture of the Achilles tendon in rheumatoid arthritis with histologic evidence of enthesitis. A case report. Clin. Orthop. Relat. Res. 1992;280:235–240. [PubMed] [Google Scholar]
- 3.Vosseller J.T, Ellis S.J, Levine D.S, et al. Achilles tendon rupture in women. Foot Ankle int. 2013;34(1):49–53. doi: 10.1177/1071100712460223. [DOI] [PubMed] [Google Scholar]
- 4.Soroceanu A, Sidhwa F, Aarabi S, Kaufman A, Glazebrook M. Surgical versus nonsurgical treatment of acute Achilles tendon rupture: a meta-analysis of randomized trials. J Bone and Jt. Surg. American volume. 2012;94(23):2136. doi: 10.2106/JBJS.K.00917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cary D.V. How to diagnose and manage an acute Achilles tendon rupture. JAAPA-J AM ACAD PHYS. 2009;22(8):39–43. doi: 10.1097/01720610-200908000-00010. [DOI] [PubMed] [Google Scholar]
- 6.Chalmers J. Treatment of Achilles tendon ruptures. J Orthop Surg Res. 2000;8(1):97–99. doi: 10.1177/230949900000800118. [DOI] [PubMed] [Google Scholar]
- 7.Habusta S.F. Bilateral simultaneous rupture of the Achilles tendon. A rare traumatic injury. Clin. Orthop. Relat. Res. 1995;320:231–234. [PubMed] [Google Scholar]
- 8.Gabel S, Manoli A. Neglected rupture of the Achilles tendon. Foot Ankle Int. 1994;15(9):512–517. doi: 10.1177/107110079401500912. [DOI] [PubMed] [Google Scholar]
- 9.Dhillon M.S, Chauhan D, Kumar V, Saini U.C. Reconstruction of bilateral spontaneous chronic idiopathic Achilles tendon rupture using LARS ligament: case report. The Foot. 2010;20(4):154–157. doi: 10.1016/j.foot.2010.09.008. [DOI] [PubMed] [Google Scholar]
- 10.Wegrzyn J, Luciani J.F, Philippot R, Brunet-Guedj E, Moyen B, Besse J.L. Chronic Achilles tendon rupture reconstruction using a modified flexor hallucis longus transfer. Int. Orthop. 2010;34(8):1187–1192. doi: 10.1007/s00264-009-0859-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sarzaeem M.M, Lemraski M.M.B, Safdari F. Chronic Achilles tendon rupture reconstruction using a free semitendinosus tendon graft transfer. Knee Surg. Sports Traumatol. Arthrosc. 2012;20(7):1386–1391. doi: 10.1007/s00167-011-1703-x. [DOI] [PubMed] [Google Scholar]
- 12.Us A.K, Bilgin S.S, Aydin T, Mergen E. Repair of neglected Achilles tendon ruptures: procedures and functional results. Arch. Orthop. Trauma Surg. 1997;116(6-7):408–411. doi: 10.1007/BF00434001. [DOI] [PubMed] [Google Scholar]
- 13.Mendicino S.S, Reed T.S. Repair of neglected Achilles tendon ruptures with a triceps surae muscle tendon advancement. J Foot Ankle Surg. 1996;35(1):13–18. doi: 10.1016/s1067-2516(96)80006-8. [DOI] [PubMed] [Google Scholar]
- 14.Bressel E, Larsen B.T, McNair P.J, Cronin J. Ankle joint proprioception and passive mechanical properties of the calf muscles after an Achilles tendon rupture: a comparison with matched controls. CLIN BIOMECH. 2004;19(3):284–291. doi: 10.1016/j.clinbiomech.2003.12.008. [DOI] [PubMed] [Google Scholar]
- 15.Chen J, Xu J, Wang A, Zheng M. Scaffolds for tendon and ligament repair: review of the efficacy of commercial products. Expert Rev Med Devices. 2009;6(1):61–73. doi: 10.1586/17434440.6.1.61. [DOI] [PubMed] [Google Scholar]
- 16.Ibrahim S.A.R. Surgical treatment of chronic Achilles tendon rupture. J Foot Ankle Surg. 2009;48(3):340–346. doi: 10.1053/j.jfas.2009.02.007. [DOI] [PubMed] [Google Scholar]


