Abstract
Background and aim of the work:
The total knee arthroplasty (TKA) revision is not a second time of primary implant surgery but is a very complex issue for orthopedic surgeon. When local conditions make necessary a greater visualization, medial para-patellar access with quadriceps snip (QS) or the osteotomy of the tibial tuberosity (TTO) can be the solutions. This work aims to compare the quadriceps snip and the detachment of the tibial tubercle, focusing on possible complications.
Materials and Methods:
At our institution, between January 2017 and February 2019 52 TKA revision for periprosthetic joint infection (PJI) or aseptic mobilization were performed. In 43 cases an extensive surgical approach was required: for patients with range of movement (ROM) < 60° was chosen TTO, while with ROM > 60° a QS was performed. Clinical and radiological follow-up was available for all the 43 cases.
Results:
The data about clinical outcome in our study show that both groups have a positive trend in KSS score over time with similar ROM results. Two partial avulsions of patellar tendon during revision surgery were reported. Clinical outcome in both groups has shown good results at the end of follow-up with no post-operative incidence of complications.
Conclusion:
We can assert that both QS and TTO are good approach for TKA revision. Future studies will be needed to understand if preparatory ROM is a good way to decide which surgical approach to use. (www.actabiomedica.it)
Keywords: Arthroplasty, Revision, Knee, Tibial Tuberosity Osteotomy, Quadriceps Snip, Complication
Introduction
The implant of a total knee arthroplasty (TKA) is an extremely common surgery nowadays. In Italy, according to RIAP data (1), the number of implants of TKA is approximately 25,000 per year. The results are satisfactory but there are complications that sometimes can lead to the need for revision surgery (2).
The TKA revision is not a second time of primary implant surgery, but is a very complex issue for orthopaedic surgeon (3-5). Of course, the pre-operative planning is mandatory: among the various aspects to be analyzed is very important the surgical approach. Surgical approach to the knee must ensure a wide view of the operating field and the capability to view all anatomical structures and protect the integrity of these, guarantee a complete soft tissue cover and favors an early mobilization and rehabilitation (6). This is not always possible: it is not uncommon to find a stiff knee, hypertrophic scar tissue or even less than non-optimal skin conditions. The usual approach used in our institution for primary knee arthroplasty is the medial para-patellar approach. When local conditions make necessary a greater visualization of the operative field or an easier eversion of the patella (7) an extended approach must be used: in literature are present many papers about this topic. Coonse and Adams described a quadriceps turn-down (8) subsequently modified with the addition of a medial para-patellar incision, the femoral peel (9), but we must not forget about the extensile medial para-patellar approach, which can be useful in the simplest cases.
In our institution the preferred approach is the medial para-patellar one with quadriceps snip (QS) (10) or the osteotomy of the tibial tuberosity (TTO) (11) when an extended approach is required. Both approaches have advantages and disadvantages. This work aims to compare the quadriceps snip and the detachment of the tibial tubercle, focusing on possible complications.
Material and Methods
This is prospective evaluation of a case series of 52 TKA revisions for periprosthetic joint infection (PJI) or aseptic mobilization performed at our institution, between January 2017 and February 2019. In 43 cases an extensive surgical approach was required to ensure correct visualization of the anatomical structures: TTO was performed in 23 cases and a QS in 20 cases.
The choice between the 2 extensive approach was based on the pre-operative range-of-motion (ROM) of the knee: for patients with ROM < 60° TTO was chosen, while QS was preferred with ROM > 60°. Surgical approach was performed in all cases by a single expert surgeon. After surgery, the rehabilitation protocol was the same in two groups: the only difference was the use of a post-operative hinged knee brace in TTO group and the prohibition of active extension for the first 2 weeks. The protocol allowed passive and active ROM (as tolerated) from first post-operative day. From second post-operative day assisted partial weight-bearing was allowed with crutches.
The following targets at 4 week were active ROM 0-90° and full weight-bearing with one crutch. From the 4th up to the 12th week, exercises aimed to recovery of muscle tropism and complete range-of-motion were recommended. In the TTO group, brace removal was allowed after radiological evaluation of bony union at 45 days.
All the 43 cases were re-evaluated by clinical assessments about 45 days after surgery, and subsequently at 3 months, 6 months and one year after surgery. Outcome were evaluated at 45 days, 6 months and one year after surgery by submitting the Knee Society Score (KSS) to all patients. Control radiographs (included full length weightbearing x-ray) were performed at each outpatient access: in particular, any changes in femoro-tibial alignment and pre and post-operative height of patella were assessed.
Complications, such as wound-related problems, mal-union or non-union, PJI, loss of hardware stability, fibrosis and joint stiffness were also assessed.
Surgical Technique
Quadriceps Snip: the technique is similar to a standard medial para-patellar with an anterior skin incision slightly extended proximally. The arthrotomy is performed through the medial part of quadriceps tendon with distal extension through medial patellar retinaculum and medial third o patellar tendon. Proximally the arthrotomy is extended to the apex of quadriceps tendon. At this point an oblique incision, in line with vastus lateralis fibers, is made through the quadriceps tendon. This allows a decrease of tension of tibial tubercle making possible, with tibial external rotation, patellar eversion.
Tibial Tubercule Osteotomy: this technique provides an anterior skin incision prolonged distally by 6-8 cm above the tibial tubercle. The arthrotomy is similarly extended distally trough the tibial tubercle and tibial anterior crest. The osteotomy is performed with an oscillating saw initially and then completed with an osteotome: a 8 cm long, 2 cm wide and 1,5 cm thick bony fragment is detached including the patellar tendon insertion. There are two methods for osteosynthesis: fixation with screws or with AO laces. We prefer fixation with AO laces, taking care to prepare the holes and to accommodate the necessary laces before implanting the tibial component. If you choose screws fixation, a tip may be pre-drilling 2 holes for screws before performing the osteotomy for the subsequent osteosynthesis. If it is necessary to raise patella in case of patella baja screws fixation is out treatment of choice.
Statistical analysis
Mean, SD and distribution of values were determined for each group. An independent-samples t-test was performed for comparison of the continuous variables between the QS and TTO groups. Proportions of categorical data were compared using chi-square tests. The level of significance was set at p-Value of < 0.05.
Results
Patients mean age was 70.6 years in the TTO group and 69.4 in the QS group. There where 9 male subjects in the TTO group and 7 males in the QS group.
In the TTO group, at the first control (45 post-operative day) only 1 patient not has achieved partial bone union. That patient has achieved complete bone healing at 90th post-operative day.
About post-operative clinical examination, at first assessment (45 day) the mean ROM in QS group were 76.2 ± 16.9 degree and in TTO group were 58.1 ± 9.7 degree. At subsequent assessment mean ROM in QS were 95.2 ± 16.8 degree at 3 months, 96.2 ± 16.9 degree at 6 months and 98.3 ± 17.3 degree at 1 year, meanwhile in TTO group were 84.1 ± 9.7 degree at 3 months, 96.3 ± 9.7 degree at 6 months and 99.1 ± 9.9 degree at 1 year. The KSS at 45 days in QS group were 64.4 ± 2.8, at 6 months were 81.3 ± 2.9 and at 1 year were 86.5 ± 2.8; instead in the TTO group the KSS at 45 days were 60.2 ± 3.2, at 6 months were 80.3 ± 3.5 and at 1 year were 86.4 ± 3.6.
Demographic data and clinical results are reported in Table 1.
Table 1.
Comparison pre- and post-operative data between two-groups (Mean±SD)
| Qadriceps snip (n 20) | Tibial tuberccle osteotomy | p-value | ||||||||||
| Gender | 7 | 14 | 9 | 14 | 0.50 | |||||||
| Age (year) | 69.5 ± 6.1 | 70.6 ± 6.4 | 0.55 | |||||||||
| BMI | 25.5 ± 2.3 | 25.8 ± 2.3 | 0.65 | |||||||||
| 45 d | 90 d | 180 d | 270 d | 45 d | 90 d | 180 d | 270 d | 45 d | 90 d | 180 d | 270 d | |
| ROM | 76.1 ± 16.9 | 95.1 ± 16.8 | 96.2 ± 16.9 | 98.3 ± 17.7 | 58.1 ± 9.7 | 84.1 ± 9.7 | 96.3 ± 9.8 | 99.1 ± 9.9 | 0.002 | 0.001 | 0.42 | 0.72 |
| KSS | 64.4 ± 2.8 | 81.3 ± 2.9 | 86.5 ± 2.8 | 60.2 ± 3.2 | 80.3 ± 3.5 | 86.4 ± 3.6 | 0.001 | 0.34 | 0.91 | |||
| Follow-up | 22.1± 12.4 | 21.5± 11.4 | 0.89 | |||||||||
Table 2.
Range of Motion in QS group and TTO group (Mean ± SD)
 |
Table 3.
KSS in QS group and TTO group (Mean ± SD)
 |
Table 4.
Age distribution and mean in QS group and TTO group
 |
The mean surgical time (from skin incision to skin suture) in TTO group was 192 min and in the QS was 167 min.
In all cases the mechanical alignment was respected into the range ± 3° varus-valgus measured on full length weightbearing x-ray. In the TTO group, in 7 cases, a patella baja correction with an elevation of TTO during fixation was necessary. One case of reinfection was reported at 10 months after surgery and treated with DAIR (debridement, antibiotics and implant retention) (12).
In QS group 2 partial avulsion of the patellar tendon were reported during revision surgery.
Discussion
A wide-vision approach to the knee for TKA revision is the first step for a successful outcome (6,13). A great number of papers are present in literature about surgical approach in TKA revision (6, 14, 15).
The QS, described by Insall (10), is technically easy because provides a good exposure of the knee without specific instruments. An important characteristic of QS is that it do not need a specific rehabilitation protocol (16). Some studies shown similar outcome between QS and the more used medial para-patellar approach (10) but is mandatory to remind that the load in the extensor mechanism is higher proximally in the quadriceps tendon rather distally in the patellar tendon (17).
The TTO were described by Dolin (11) and afterword modified by Whiteside and Ohl (18). These technique have some advantages like the preservation of extensor mechanism and avoidance of patellar tendon avulsion (15) but the most important is the possibility to modify tibial tuberosity height and to perform realignment of extensor mechanism (19). According to literature, screws are the best method for bone fixation (20).
Figure 1.
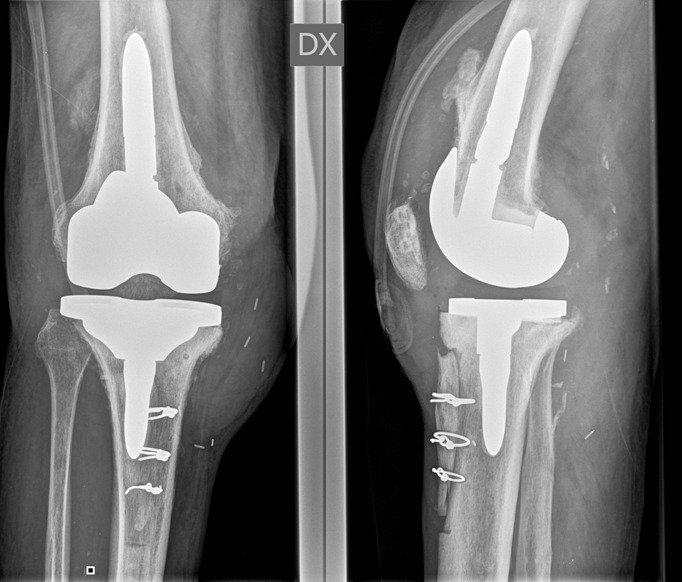
TKA revision with TTO approach and AO laces fixation.
Figure 2.
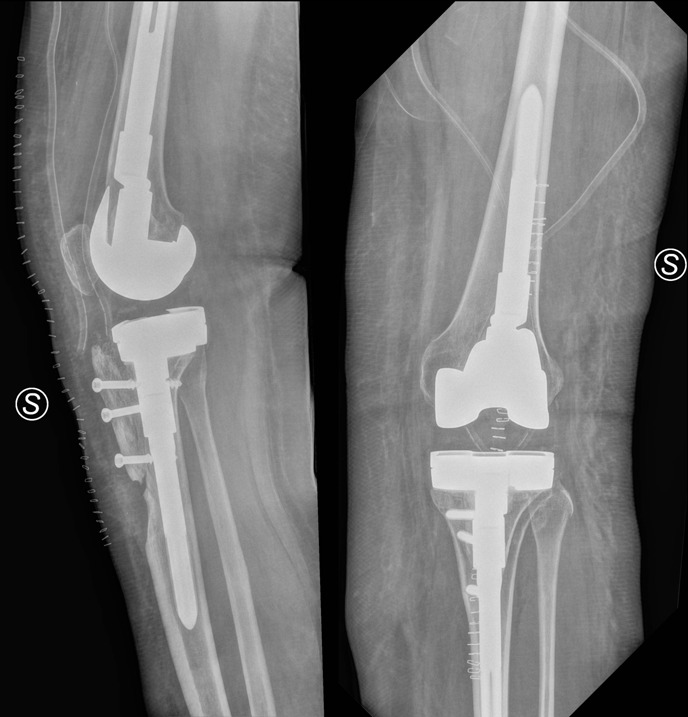
TKA revision with TTO approach and screws fixation.
From our results it seems that, when an extensive surgical approach is needed, there are no significant differences in terms of operating time between the QS and the TTO groups. The 25-minutes difference between the two groups is due to the fact that in the TTO group requires the osteotomy fixation. In addition, analyzing the data emerges as the most complex surgeries have been carried out through an approach with TTO. Comparing the operations that are temporally lasted less, it is clear that the operative time difference is more restricted, however always in favor of QS group.
The data about clinical outcome in our study show that both groups have a positive trend in KSS score over time that is comparable to previous studies (10). The initial gap in KSS in favor of QS group seen at 45 days is progressively reduced until the last assessment. Also the ROM shows a similar trend: at 45 days the ROM are 76.2 ± 16.9 degree and only 58.1 ± 9.7 degree for the QS and TTO group respectively, while after one year they are comparable (98.3 ± 17.7 degree and 99.1 ± 9.9 degree for the QS and TTO group respectively). The 45-days gaps are statistically significant either for KSS and ROM (also at 90-days), probably for the difference in the initial rehabilitation procotol with the TTO patients using a brace with a forbidden active extension for the first 2 weeks. (14). The only cases of intra-operative partial patellar tendon avulsion were reported in the QS group, thus highlighting that TTO approach is effective in reducing the risk for this complication in stiff knees (21).
Conclusion
Our study has many limitations: foremost is a retrospective study. All data were extrapolated from clinical records of our patients. The comparison between two groups not keep in mind difference in surgical cases complication: obviously the TTO approach were performed in most hard cases, with very important stiffness or after multiple surgeries. Conversely the QS approach were performed in mild difficult cases. Clinical outcome in both groups has shown good results at the end of follow-up with no incidence of complications. We can assert that both QS and TTO are good approach for TKA revision. Future studies will be needed to understand if pre-operative ROM may be the best factor to take into consideration to decide the more suitable surgical approach.
Conflict of interest:
Each author declares that he or she has no commercial associations (e.g. consultancies, stock ownership, equity interest, patent/licensing arrangement etc.) that might pose a conflict of interest in connection with the submitted article
References
- 1.Registro Italiano ArtroProtesi - Annual Report. 2018, Istituto Superirore di Sanità [Google Scholar]
- 2.Fehring T.K, et al. Early failures in total knee arthroplasty. Clin Orthop Relat Res. 2001;(392):315–8. doi: 10.1097/00003086-200111000-00041. [DOI] [PubMed] [Google Scholar]
- 3.Delanois R.E, et al. Current Epidemiology of Revision Total Knee Arthroplasty in the United States. J Arthroplasty. 2017;32(9):2663–2668. doi: 10.1016/j.arth.2017.03.066. [DOI] [PubMed] [Google Scholar]
- 4.Di Benedetto P, et al. Two-stage revision after total knee arthroplasty. Acta Biomed. 2017;88(2S):92–97. doi: 10.23750/abm.v88i2-S.6519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mancuso F, et al. Management of metaphyseal bone loss in revision knee arthroplasty. Acta Biomed. 2017;88(2S):98–111. doi: 10.23750/abm.v88i2-S.6520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Della Valle C.J, Berger R.A, Rosenberg A.G. Surgical exposures in revision total knee arthroplasty. Clin Orthop Relat Res. 2006;446:59–68. doi: 10.1097/01.blo.0000214434.64774.d5. [DOI] [PubMed] [Google Scholar]
- 7.Ryan J.A, et al. Failure of the Patellar Tendon with the Patella Everted versus Noneverted in a Matched-Pair Cadaver Model. HSS J. 2010;6(2):134–7. doi: 10.1007/s11420-009-9149-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Coonse KD, A.J. A new operative approach to the knee joint. Surg Gynecol Obstet. 1943;77:344. [Google Scholar]
- 9.Lavernia C, Contreras J.S, Alcerro J.C. The peel in total knee revision: exposure in the difficult knee. Clin Orthop Relat Res. 2011;469(1):146–53. doi: 10.1007/s11999-010-1431-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Garvin K.L, Scuderi G, Insall J.N. Evolution of the quadriceps snip. Clin Orthop Relat Res. 1995;321:131–7. [PubMed] [Google Scholar]
- 11.Dolin M.G. Osteotomy of the tibial tubercle in total knee replacement. A technical note. J Bone Joint Surg Am. 1983;65(5):704–6. [PubMed] [Google Scholar]
- 12.Di Benedetto P, et al. Acute periprosthetic knee infection: is there still a role for DAIR. Acta Biomed. 2017;88(2S):84–91. doi: 10.23750/abm.v88i2-S.6518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Vaienti E, Scita G, Ceccarelli F, Pogliacomi F. Understanding the human knee and its relationship to total knee replacement. Acta Biomed. 2017 Jun 7;88(2-S):6–16. doi: 10.23750/abm.v88i2-S.6507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Barrack R.L. Specialized surgical exposure for revision total knee: quadriceps snip and patellar turndown. Instr Course Lect. 1999;48:149–52. [PubMed] [Google Scholar]
- 15.Mendes M.W, Caldwell P, Jiranek W.A. The results of tibial tubercle osteotomy for revision total knee arthroplasty. J Arthroplasty. 2004;19(2):167–74. doi: 10.1016/j.arth.2003.08.013. [DOI] [PubMed] [Google Scholar]
- 16.Rand J.A, et al. Intraoperative assessment in revision total knee arthroplasty. J Bone Joint Surg Am. 2003;85-A(Suppl 1):S26–37. doi: 10.2106/00004623-200300001-00007. [DOI] [PubMed] [Google Scholar]
- 17.Denham R.A, Bishop R.E. Mechanics of the knee and problems in reconstructive surgery. J Bone Joint Surg Br. 1978;60-B(3):345–52. doi: 10.1302/0301-620X.60B3.355258. [DOI] [PubMed] [Google Scholar]
- 18.Whiteside L.A, Ohl M.D. Tibial tubercle osteotomy for exposure of the difficult total knee arthroplasty. Clin Orthop Relat Res. 1990;260:6–9. [PubMed] [Google Scholar]
- 19.Bruni D, et al. Tibial tubercle osteotomy or quadriceps snip in two-stage revision for prosthetic knee infection? A randomized prospective study. Clin Orthop Relat Res. 2013;471(4):1305–18. doi: 10.1007/s11999-012-2763-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Caldwell P.E, et al. Dynamic confirmation of fixation techniques of the tibial tubercle osteotomy. Clin Orthop Relat Res. 2004;424:173–9. doi: 10.1097/01.blo.0000130205.57095.a2. [DOI] [PubMed] [Google Scholar]
- 21.Anand S, et al. Management of Patellar Tendon Rupture after Total Knee Arthroplasty using Hamstring graft: A Case Report. J Orthop Case Rep. 2018;8(2):57–60. doi: 10.13107/jocr.2250-0685.1050. [DOI] [PMC free article] [PubMed] [Google Scholar]


