Abstract
Background and aim of the work:
hypermobility of the first ray (FRH) began to be considered as a pathological entity from Morton’s studies and was associated as a primary cause of hallux valgus (HV). Currently, this relationship is in discussion, and various authors consider FRH as a consequence of the deformity. The purpose of this narrative review is to summarise the most influential publications relating to First Ray Mobility (FRM) to increase knowledge and promote its conventional assessment during clinical practice.
Methods:
papers of the last century were selected to obtain a homogeneous and up-to-date overview of I-MTCJ mobility and HV, as well as their relationship and management.
Results:
in recent years, FRH was studied from a biomechanical and pathophysiologic point of view. There is still not enough data regarding the aetiology of FRM. The higher rate of instability found in HV lacks an explanation of which is the cause and which is the effect. However, the Lapidus arthrodesis is still a valid method in cases of FRH and HV, even if is not rigorously indicated to treat both. When approaching FRH, radiographic or clinical findings are mandatory for the right diagnosis.
Conclusions:
FRM is an important factor that must be considered in routine clinical practice and prior and post HV surgery, as much as the conventional parameters assessed. Surgeons should consider performing I-MTCJ arthrodesis only if strictly necessary, also paying attention to soft tissue balancing. Improving the measurement of FRH could be useful to determine if it is a cause or effect of the HV deformity. (www.actabiomedica.it)
Keywords: hypermobility, hypermobility of first ray, first ray mobility, hallux valgus, Lapidus procedure, foot biomechanics
Introduction
Hypermobility of the first ray (FRH) has been described as a relatively increased arc of motion with respect to the second metatarsal bone (MB), and lacks a firm end point (1). In simple terms, it is an “abnormal and excessive mobility in dorsi-flexion of the first metatarsal head, due to instability of the First Metatarsal-Cuneiform Joint (I-MTCJ)” (2) not only in the sagittal plane, but also in the transverse one. Clinically, in normal conditions, applying a dorsiflexion force under the head of the first MB, its lower margin does not exceed the plane of the lesser metatarsal heads. In case of FRH, alterations of normal foot mechanics are present. While walking, for example, the vertical reaction force to the ground raises the first metatarsal head over the plane of the lesser metatarsal heads, moving the load onto the lesser metatarsals. This can lead to a collapse of the internal longitudinal arch of the foot, compromising the propulsive phase of the gait.
Historically, the first author to define the concept of I-MTCJ hypermobility was the anatomist of Columbia University, Dudley Morton (3) in 1928, who speculated that FRH may have been due to unusually free motion in the joint between the inner cuneiform and scaphoid bones, and between the inner and middle cuneiforms. He also defined a clinical method to assess FRH (Figure 1). However, hypermobility was defined as an arbitrarily excessive motion, without finding a way to quantify the examination. Then, in the 1930s, Lapidus (4-6) proposed an association between increased first ray mobility (FRM) and the development of hallux valgus (HV). However, neither Morton nor Lapidus were able to quantify the magnitude of FRM in any of their studies and based their findings on subjective clinical examination. In 1971, Courriades (7) was credited first with recognizing that FRH was a distinct clinical entity.
Figure 1.
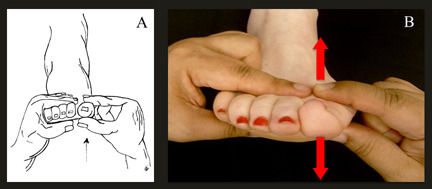
A and B: Manual examination to clinically assess FRM according to Morton. A dorsally directed forced is applied to the first ray with one hand, while other hand stabilises second to fifth metatarsals.
Rodgers and Cavanagh in 1986 (8) were the first researchers to measure dorsal motion of the first ray (FR) with a mechanical prototype device which was reengineered by Glasoe et al. in 1999. Measures of dorsal mobility with this new device have been judged valid and reliable by radiographic comparison. In 1990, Romash et al. demonstrated objective evidence of transverse hypermobility by performing a clinical squeeze test (9). Although an isolated transverse motion of the I-MTCJ is only a few degrees, the mobility can result in a large deviation of the distal metatarsal head.
In 1994, Klaue et al. introduced a non-invasive device to quantify dorsal I-MTCJ mobility with a numeric value (10). However, they were unable to selectively differentiate any of the joints of the medial column of the foot. This device has been used in several studies (11-15) and has been shown to be dependable, allowing the definition of FRH as a dorsal displacement of more than 8 to 10 mm to a lack of a firm endpoint (16). More recently, Singh et al. (17), using the same device, considered the measurement of FRM to be more adequate in a 45° dorso-medial direction (Figure 2), respecting the natural movement of the FR on the transverse plane during walking and defining it hypermobile at 10 mm displacement (Figures 3 and 4). Previously, Faber et al. (18) in 1999, observed that the relative contribution of first tarsometatarsal mobility to FRM is more pronounced in the transverse plane as opposed to the sagittal plane.
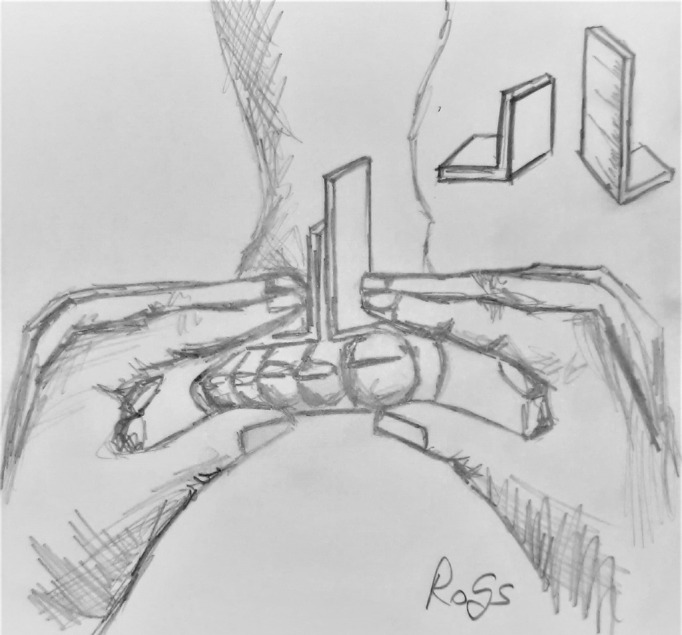
Figure 2.

A and B: Manual examination to clinically assess FRM by displacing the first metatarsal head at an angle of 45 degrees to the transverse plane.
Figure 3.

Correct position of foot for the measurement of FRM using the Klaue device: A) the foot is placed in the ankle orthosis with the ankle in neutral position and calf, ankle and midfoot are immobilised; B) the micrometre overlies the first metatarsal head in order to measure the mobility first in the sagittal plane.
Figure 4.

With one hand, the examiner immobilises second to fifth metatarsal bones, and with the other hand, exerts a force on the plantar side of the first metatarsal head, first A) in a purely dorsal direction; and then B) at a dorsomedial angle of 45 degrees to the transverse plane. Displacements were measured with the patient sitting in a non-weightbearing position, according to the method established by Klaue.
In 2006, normal dorsal mobility was reported by Glasoe and Coughlin (19) in a consensus statement to average 5 mm in normal adults, while pathologic mobility or hypermobility was defined as greater than 8 mm of sagittal translation to stress (1, 10, 12). However, in the literature there is no factual definition that exactly quantifies this overextension during walking of the FR with respect to the lesser ones. This lack of a precise definition may suggest a lack of understanding of the clinical results associated with FRM (20). Because of the intersegmental nature of foot motion, the measurement of dorsal FRM cannot be ascribed to only one specific joint as it involves more bones, and because the load imposed is not easily controlled, different methods yield different results.
In the early 2000s, many authors including Ward Glasoe (19, 21) and Thomas Michaud (22-24) suggested that this overelevation and translation of the first MB relative to the second one in a sagittal plane, leads to overload of other MBs causing a wide range of disorders, such as HV synovitis, lesser metatarsal stress fractures, metatarsalgia and interdigital neuromas (19, 25, 26).
The clinical diagnosis of hypermobility in a sagittal plane is basically based on the drawer’s sign. Although several different methods have been proposed, all describe increased dorsal excursion with a soft end point (Figures 1-5), making the quantification in a clinical setting of what constitutes hypermobility in the sagittal plane difficult. Measurement of the FRH in the transverse plane can be documented both clinically and radiographically, manifested by an increased intermetatarsal angle (IMA), as showed by Singh and Romash (9, 17).
Figure 5.
Manual examination to clinically assess FRM using handheld rulers.
The controversy in the English literature about the association between HV and FRH regards whether hypermobility is a real pathology, or is a consequence of a deformity. The best strategies for management of FRH and HV are in question. It has been shown that there is also a significant relationship between radiographic malreduction of sesamoids and recurrence of HV deformities (27, 28), which is why their subluxation is normally measured in the most recent studies about HV deformity correction. Perhaps FRH should be among the parameters to be corrected if present during HV treatment. Its routine assessment pre- and post-operatively at different follow-up points as the other widespread known parameters used for HV correction evaluation should seem important. The purpose of this narrative review is to summarise the most influential publications relating to FRH to increase knowledge and promote its conventional assessment during the clinical practice and the pre- and post-operative evaluations of several HV surgical procedures.
Anatomy of the First Ray
The FR is defined as a single functional foot unit, whose bone components consist of the great toe phalanges, sesamoids, first MB and medial cuneiform bone. The various bones of the FR have a moderately defined space arrangement, and a variation in their relationships in the three planes of space can be a sign of foot pathologies such as HV. One of the most characteristic signs of the alteration of the normal anatomy of the FR is the variation of the space relationship between the sesamoid bones and the first MB. This alteration could have four progressive degrees of gravity on the transverse plane, and three degrees of gravity on the coronal plane. These pathognomonic signs can be investigated using 3D methods, which manage to represent in a single figure the space alteration of the relationships between the bones of the FR (29).
There are also other joints that are involved in FRM: between the medial cuneiform and the navicular bone, between the medial cuneiform and the intermediate cuneiform and the articulation between the medial cuneiform and the second metatarsal base (30-32). An important factor of anatomical potential instability of the FR is the absence of the intermetatarsal ligament. This structure is present among all the minor metatarsals; it is instead absent between the first and second rays (21). The absence of the intermetatarsal ligament between the first and second rays could be the reason why there can be no Morton neuroma in the first intermetatarsal space.
Anatomic structures serve as stabilisation factors of the FR. The dorsal and interosseus ligaments and above all, the plantar first MTC ligament are the most important stabilisers in the sagittal plane and in FR motion in general (26). Also the peroneus longus and flexor hallucis longus tendons contribute to minimise instability of the I-MTCJ during dorsi-flexion (33): they provide significant contribution to dorsal and medial stability with a larger role in the sagittal plane (34). Further, the role of the plantar fascia is crucial in foot stability (35), and Sarrafian specified the plantar aponeurosis as a critical component of FR stability (35). Grebing and Coughlin found an increased FRM when the ankle is plantarflexed and vice-versa when the ankle is dorsiflexed. These authors concluded that the plantar fascia is a key stabiliser of FR, but based on these findings, Doty et al. assessed that the alignment confers stability, rather than instability leading to malalignment (36, 37).
The Biomechanics of the I-MTC Joint and the First Ray
During walking, the forefoot has to be flexible to absorb ground reaction but also stiff to sustain the body weight and stressing activities (38). To support the arch of the foot, the human foot needs stability, especially at the I-MTCJ. This stability gives strength to the medial column (39), which is necessary and adapted for bipedal gait and propulsion (26, 40). Ideally, the human foot would have a rigid FR, to provide a long and rigid lever arm for the Achilles tendon during the heel rise phase of the gait cycle (26, 41).
Dullaert et al. supported the importance of peroneus longus function in maintaining medial longitudinal arch for the stability of the I-MTCJ (42). When the foot moves into the sagittal plane, the FR can spin around its axis. During the dorsiflexion of the foot, the FR inverts; during the plantarflexion of the foot, the FR everts. I-MTCJ has also mobility in the transversal plane. The biomechanical axis of the I-MTCJ motion is on a plane from 45° to 60° in a dorsomedial direction, thus allowing a movement of the first metatarsal head from a plantar-lateral to a dorso-medial position. The triplane movement of the first MB is inversion and adduction during dorsiflexion, and eversion and abduction during plantarflexion. This type of movement is commonly named “pronation of the FR” (21).
Because of these multi-plane movements, it is understandable how difficult it is to quantify FRM. Due to the number of joints which participate in the normal motion of the FR and the consequent intersegmental motion of foot, accurate measurement of hypermobility cannot be made only in the dorsal direction, considering only one joint movement and applying a load not precisely controlled (25). However, we must adopt a method to measure it in clinical sitting.
Initially Root et al. proposed that the normal FRM was 5 mm of dorsiflexion and 5 mm of plantarflexion in the sagittal plane (44), but lacked real scientific measurements. Later, various authors started to use different instruments to quantify the measurement (10, 45–47), even if not considering movement in the frontal plane of the FR. Klaue et al. reported that the dorsiflexion of the FR was normally 5.3 mm, and various authors have then used his device, obtaining diverse results from 4.4 mm to 7.2 mm (17, 36, 45, 48, 49). Dorsiflexion ranges from 3 to 8 mm in healthy adults, and one article authored in 2006 by Glasoe and Coughlin defined FRH when the value exceeds 8 mm (19).
While walking, the I-MTCJ has mobility in the sagittal plane. Some authors try to measure it ignoring the changes which take place in the frontal plane (14, 50) and have considered FRH as only a sagittal plane instability, not considering the relevance of motion in the transversal plane. The normal biomechanical axis of the I-MTCJ is a plane between 45° and 60°. For this reason, Singh et al. proposed considering FRH in the presence of a dorsal displacement more than 10 mm with FR pushed into the dorso-medial direction at an angle of 45° (17). According to these authors, the mean FRM in the 45° dorso-medial direction is 8.3 mm in patients with HV compared to a control group (Figures 2 and 4). In a recent study, gait analysis revealed a dynamic elevation of the FR at the level of I-MTCJ in the sagittal plane, but also a pronation and adduction of the first MB is apparent (51). Hence, I-MTCJ motion in the transversal plane is important and must be considered.
According to recently published literature, the average range of the FR is of about 6 mm of dorsiflexion and about 6 mm of plantarflexion, for a total range of motion of about 12 mm (45). Geng et al. assessed that movement of I-MTCJ during weightbearing is as follows: dorsiflexion, supination and internal rotation, suggesting that FRH occurs in multiple planes in patients with HV deformity (52).
Feet with low arches and real clinical flatfoot deformity have increased measures of FRM compared to those with high arches. This supports the concept of medial column laxity as a component in the development of flatfoot deformity (53). Other authors describe medial column hypermobility in planovalgus feet with tarsometatarsal arthritis. FR instability results in a loss of ability to resist the vertical ground reaction forces, and this leads to laterally displaced forces concentrating on the second and third MBs and midfoot structures, which leads to the development of tarsometatarsal osteoarthritis (54). However, Heng et al. have described no correlation between FRM and posterior tibial tendon dysfunction in flatfoot, although this relationship is still under discussion (55).
Clinical and Radiographic Measurements of First Ray Mobility
Morton was the first to describe a clinical method to define FRH with a provocative test which is still widely used (3). One hand of the examiner applies a dorsal force to the head of the first MB while stabilizing the lateral four MBs with the other hand. The test is positive when the first metatarsal head translates dorsally relative to the second metatarsal head in a coronal plane (Figure 1). This is a highly reproducible test, but it lacks a quantifying scale of severity, and it has many interobserver errors (56). According to Grebing et al., the magnitude of FRM at clinical examination varies with the position of ankle dorsiflexion/plantarflexion; hence, the provocative test has to be done in a neutral ankle position. This is due to the key stabilising effect of plantar fascia aponeurosis, whose tension is modified by ankle position (36, 41).
In the 1970s, Root at al. introduced an alternative clinical measurement: with one hand the examiner stabilises the lesser four MBs, and with the other hand applies alternately a dorsal force and a plantar force to the head of the first metatarsal. A hypermobile FR is defined when the dorsiflexion exceeds the plantarflexion. This is the difference from Morton’s manual examination. Other authors still suggest that the FR can be defined hypermobile if a dorsal stress force elevates the head of the first MB above the plane of the minor metatarsals (57).
Handheld rulers can assist in standardizing the measurement of FRM (Figure 5); three different rulers have been described in literature. The “Kilmartin Sagittal Raynger” rulers were described in 1990 by Wallace and Kilmartin. These two portable rulers are placed on the plantar surface of the foot. They are two side-to-side moving rulers that can measure the dorsal displacement of the FR, as the examiner applies a plantar force on it (58). Another type of ruler was described by Lee and Kim in 2008, naming it the “Euliji Medical Center (EMC) ruler”. This tool is composed of two small pieces of a metal ruler bent at right angles, marked in 1-mm gradations. The examiner applies a dorsiflexion force on the FR, and measurement of the FRM is made by balancing the ruler with the shorter limb on the dorsum of the first metatarsal head, and the ruler with the longer limb on the dorsum of lesser metatarsal head (47). Greisberg et al. ideated another handheld ruler in 2010, also used for another study in 2012 (26, 59). These rulers are a modification of the EMC one, with the first ruler placed on the plantar surface of the first metatarsal head, and the other on the plantar surface of the lesser metatarsal heads. As the FR is dorsiflexed, measurements are read directly off the ruler (26). Measurement by handheld rulers is burdened by the same reproducibility errors attributed to manual examination (26) even if they have a quantified scale. Using them, Greisberg et al. quantified first MB elevation compared with the second MB rather than total metatarsal translation. According to the authors, an increased first MB elevation would tend to transfer load to the lesser metatarsals during weightbearing, causing metatarsalgia and related problems (26, 59). However, manual testing for FR instability is unreliable compared to measurements made with mechanical devices. (Table 1)
Table 1.
Devices used to clinically assess the Hypermobility of the First Ray
| Authors | Device | Description |
| Rodgers and Cavanagh 1986 | Mechanical device with electronic sensor | This mechanical device applies a load beneath the first ray and then calculates its plantar displacement through an electronic sensor |
| Wallace and Kilmartin 1990 | Kilmartin Sagittal Raynger | Moveable rulers to measure the displacement as an examiner dorsiflexes the first ray |
| Klaue et al. 1994 | Klaue device | Modelled from an ankle foot orthosis with a suspended caliper on the first metatarsal that measures the dorsal displacement when the first ray is moved manually (figure 3 and 4) |
| Glasoe et al. 1998 | Glasoe device | Similar to Klaue device. This one stabilises the hindfoot, and the first ray is moved mechanically with a load |
| Lee and Kim 2008 | Eulji Medical Center (EMC) ruler | Two-piece plastic rulers that are placed on the dorsum of the first and second metatarsals with dorsiflexion of first ray (figure 5) |
| Greisberg et al. 2010 | Greisberg rulers | Two similar EMC rulers, but the authors measured metatarsal elevation and not translation, which was assessed with pressure placed under the first and the lesser metatarsals simultaneously. An increased first metatarsal elevation would tend to transfer load to the lesser metatarsals |
The first device described was created by Rodgers and Cavanagh in 1986. This mechanical device applied a load beneath the FR and then calculated its plantar displacement through an electronic sensor. It had a measurement error of approximately 3 mm given by the compression of the plantar fat pad during the loading process. For this reason, measurement error has been avoided by applying mechanical force on the dorsum of the FR (25, 60).
A device that most greatly influenced the method of measuring the FRH is the “Klaue device” (Figures 3 and 4). This device is composed of an ankle-foot orthosis, in which the ankle is placed in neutral position. The examiner with one hand dorsiflexes the FR until its maximum range of motion, and with the other hand blocks rays from second to fifth. A micrometre is suspended from the frame of the ankle-foot orthosis, fixed to the frame above the first metatarsal head with the ankle maintained in neutral position and in line with the FR in order to measure the mobility first in the sagittal plane. The micrometre records the full dorsiflexion range of motion of the FR. This device has variability due to the starting point of measurement and the force exerted by the examiner to dorsiflex the metatarsal head. To reduce variability, the measurement is repeated multiple times, with the average recorded for analysis (26). Additionally, since 25% of adults cannot attain a neutral ankle position with the knee extended, the knee should also be flexed (36).
The Glasoe device is similar to the one created by Klaue but has some technical expedients that reduce the variability of the measurement, having a mechanical piston able to measure the force produced. The lesser MBs are blocked by a separate platform, so the starting point of measurement of the dorsiflexion of the FR is reproducible in each measurement without variations (60). The device was improved in 2005 by connecting it to a computer, allowing the storage of the data for retrieval and time-based analysis (61). Both Klaue and Glasoe (Table 1) have a great potential in standardizing the measurement of FRH, but at present there are no commercial devices marketed on a large scale such as to allow widespread use (25).
Imaging exams can also be useful to standardize the measurement of FRM but are burdened by projection error. The modified Coleman block test is the most described x-ray exam (25). The protocol involves weightbearing lateral view radiographs of the foot. The dorsiflexion view of the FR is performed with hindfoot, midfoot and first MB stationary on a wooden block; hindfoot, midfoot and lesser metatarsals stationary on a wooden block give the plantarflexion view of the FR (62). The modified Coleman block test is widely known for measuring dorsal FRM. In 2018, Tavara-Vidalon et al. used it to measure both sagittal and frontal plane displacement on anteroposterior radiographs (45). Displacement of the FR can also be assessed in the transverse plane with the radiographic squeeze test, and measuring the FRM in 3 planes could be a valid help for surgical corrective procedure. Pressing or applying a tight bandage from first to fifth metatarsal-phalanges joints allows visualisation of significant differences in intermetatarsal angle in case of hypermobility in the transverse plane (63). Martin et al. evaluated FR dynamic motion using live fluoroscopy in 2012 taking lateral projections of radiographs during the stance phase of gait to evaluate the positional changes of the FR relative to the talus (64).
CT scan 3-dimensional (3D) evaluation of FR has also been investigated. A study of Geng and al., published in 2015, evaluated both feet of 10 females with healthy feet, and both feet of 10 females with HV. The evaluation was made with CT scan, comparing the position of the FR when the foot is in a non-weightbearing state versus when it is in a weightbearing state. Loading state was simulated by a custom-made device, that also blocked the ankle in a neutral position. The study observed that in loading conditions the I-MTCJ turns dorsiflexed, supinated, and internally rotated. These movements in multiple planes are wider in HV deformity (52).
Kimura et al. carried out a similar study in 2017. They evaluated ten feet of 10 patients with hallux valgus and 10 feet of 10 healthy volunteers with no foot disorders using CT-scans. The evaluation was made both in non-weightbearing and weightbearing state, simulated by a custom-made device. This study demonstrated that, in patients who have HV, the weight-bearing state caused an increased FR mobility compared to the FR in normal feet (65).
Magnetic resonance (MR) imaging has been used to evaluate FRM. In the study of Swanson et al. in 2016, FR is scanned in a MR with the foot posed on a system of wedges to replicate the weightbearing phases of gait. Measures of hallux and FRM were made from 2D and 3D magnetic resonance scans, and the two measurement methods were compared with each other. This report found the study of FR sagittal mobility through 2D approach reliable, compared to 3D images (66).
Ultra-sound can also be used to ascertain FRH. In a study published in 2019, Stiglitz et al. asserted that ultra-sound could have good reproducibility for measures of I-MTCJ, but further studies are necessary to evaluate this procedure (67).
First Ray Hypermobility and Hallux Valgus
A complicated relationship
The aetiology of HV is complex and its connection with the instability of the FR is one of the most debated concepts in the current literature of foot and ankle disorders. Many other reports have claimed an association between increased I-MTCJ and HV valgus (10, 12, 68–70), nevertheless focusing only on mobility in the sagittal plate. Certainly, the tricky concept of the metatarsus primus varus, HV, hypermobility of the I-MTCJ and other different factors related to the HV deformity are well known, but most authors consider only a uniplanar evaluation of this multiplanar deformity (65).
Although HV deformity is estimated to be from 20 to 35% of the general population, FRH is not always and precisely assessed (65, 71, 72) often accompanied by significant functional disability and foot pain. Despite frequent mention in a diverse body of literature, a precise estimate of the prevalence of HV is difficult to ascertain. The purpose of this systematic review was to investigate prevalence of HV in the overall population and evaluate the influence of age and gender. METHODS Electronic databases (Medline, Embase, and CINAHL). Sigh et al. found 81% FR instability in patients with HV compared to 24% of FR instability in the control normal group (17). Some categories of athletes like ballet dancers seems to have higher FRH rates probably due to dancing technical errors (pronation) and intrinsic incorrect activity (72-74), meaning that altered biomechanics of the foot can be a risk factor.
As shown previously, many methods are available to measure FRM, of which the most common is manually moving the first MB in the dorsal and plantar directions (Figure 1). Although this technique can be readily used in a clinical setting without any special equipment, the validity and reliability can be questionable (19). Glasoe et al. (21) compared the interrater reliability of this manual measurement method with that of their mechanical measuring device. Their device is similar to Klaue’s in that the foot is constrained in an apparatus and the FRM is measured in a controlled environment. However, unlike the Klaue device, their device is capable of controlling the amount of pressure applied to the FR while measuring the dorsal displacement. Therefore, consistent pressure can be applied to all the subjects without relying on investigator consistency (74).
Coronal, Sagittal and Transverse: the 3 plains of Hallux Valgus Deformity
Some authors think HV is a transverse plane deformity involving HV with the sagittal plane hypermobility resulting secondarily and not acting as the primary deforming force (34, 76–79). Others claim those patients with higher motion in the sagittal plane are predisposed to the development of transverse plane malalignment and HV deformity (10, 68, 69, 80).
Recently, growing attention has been paid to the 3-dimensional changes in HV deformity (54, 65). Considering movement in multiple planes, measurement of FRH should be done in a 45° dorsomedial direction according to Singh et al. (17). In addition, it is important to consider first MB pronation in HV: by several HV surgical procedures is possible to obtain a good derotation of the first MB and a good reduction of subluxated sesamoids (54).
The association between the quantification of the HV angle (HVA) and IMA (70, 77) is well described in the current literature. Mobility of the I-MTCJ in a coronal plane causes the increase of both of these angles, but isolated sagittal plane MTC mobility has never been proven as a primary cause. With the development of HV, the dynamic restraints such as the plantar fascia, the sesamoids and the muscles around the foot become altered (70, 81). Hence, some authors propose that the increased FRM is due to loss of plantar aponeurosis alignment: it is secondary to the deformity, and the restoring of normal plantar fascia tension could resolve the instability (41).
Recently, Kimura et al. performed a comparison of intercuneiform 1-2 joint mobility between HV and normal feet using weightbearing computed tomography and 3-dimensional analysis. During their procedures, several patients with HV who had instability between the medial and middle cuneiform, in addition to the FR, were found. The results of this study showed that, relative to the medial cuneiform, the middle cuneiform was significantly displaced due to dorsiflexion and inversion under weightbearing conditions in patients with HV, suggesting that HV also involves hypermobility at the intercuneiform 1-2 joint. Because manual inspection was performed in their study, the force used might have been inconsistent among the patients. In addition, because HV deformities involve 3D factors, including rotation, and because the FRH is also 3D, it is ideal to assess the pathological condition 3-dimensionally instead of in one direction or one plane (65).
Hence, FRH in the sagittal plane is not the only indication for the Lapidus procedure because is important to consider the increased mobility in the transversal plane; I-MTCJ hypermobility occurred in both the sagittal and the transversal planes (82, 83).
Lapidus: a necessary procedure?
Lapidus was the first to propose fusing the first and second metatarsal bases with the medial cuneiforms, performing a surgical arthrodesis to reduce FRM. His technique was modified during the years by various surgeons, and it is still used above all for severe HV deformity correction or recurrent deformity (5,84,85). The procedure has been proven by various studies and in large systematic reviews of multiple techniques, reporting an IMA correction variable from 8.5 to 14.4 mm with different fixation techniques and an overall fusion rate of 4% (85, 86). According to Lapidus, many surgeons think that by correcting excess motion at the I-MTCJ by arthrodesis, this would then normalize FRM and would address the primary cause of the HV (5,6,43,80) deformity. However, there is some disagreement with prior indications for I-MTCJ arthrodesis. Studies have shown realignment procedures at the first metatarsophalangeal joint effect vectors of soft tissue support, which serve to stabilise the medial column without arthrodesis of the I-MTCJ. Currently, few studies report FRM values during the conventional evaluation of HV deformity and the outcomes of the different surgical techniques for its correction.
Ellington et al. (80) recommended MTCJ arthrodesis in case of HV recurrence and found that 96% had preoperatively clinical signs of FRH and 52% radiographic findings of instability (Table 2). Therefore, mobility of first MB should be always assessed when considering a Lapidus procedure. On the other hand, Kim and colleagues performed a series of proximal metatarsal Chevron osteotomies and distal soft tissue procedures for HV deformity without sacrificing the I-MTCJ, concluding that FRH is multifactorial and refuting Morton’s original theories (79).
Table 2.
Hallux Valgus and First Ray Hypermobility: the most recent literature
| Authors | Procedure (if present) | Results | Device |
| Coughlin and Jones 2007 | Proximal metatarsal osteotomy and distal soft tissue procedure alignment on hallux valgus patients (without MTC arthrodesis) | 27 months of average follow up. Reduction from 7.2 mm to 4.5 mm after the procedure. | Klaue device |
| Kim et al. 2008 | Proximal metatarsal Chevron osteotomy with distal soft tissue procedure in hallux valgus deformity correction with patient having first ray hypermobility | Mean dorsiflexion mobility of the first ray preoperatively was 6.8 mm and 1 year post-operatively was 3.2 mm. | Klaue device |
| Ellington et al. 2011 | Lapidus procedure in feet with recurrent hallux valgus | Preoperative evaluation revealed 96% of patients with clinical hypermobility and radiological finding of instability in 52% of patients. Lapidus procedure is recommended in case of HV recurrence. | Clinical and Radiographic Coleman block test (for sagittal motion) and radiographic squeeze test (for transverse motion) |
| Singh et al. 2016 | No intervention | First ray displacement in hallux valgus patients 11.0 in the 45° dorsal medial direction compared to 8.3 mm in control group. | Klaue device |
| Gent et al. 2015 | No intervention | During body weight-bearing conditions, the first MTC-J in HV feet dorsiflexed an average of 2.91°, versus 1.18° in controls; supinated 2.17° versus 0.98° in controls; and internally rotated 2.65° versus 0.96° in controls. Moreover, the joint in HV feet widened significantly compared with the controls and tended to translate more in the dorsal-plantar direction. | 3D models were reconstructed from CT scan in both unloaded and weight-bearing conditions |
| Stiglitz et al. 2019 | No intervention | Both inter- and intra-observer reliability was strong for all measured parameters. Dynamic ultrasound test is simple and reproducible to assess MTC gaping distance. | Dynamic ultrasound test |
Finally, procedures involving I-MTCJ fusion are technically demanding, and some investigators suggest fusion should be reserved for cases with MTCJ arthritis or more severe HV deformity cases in which the IMA cannot be improved by a metatarsal shaft osteotomy. Non-union, hardware removal and failure, metatarsalgia, and bone grafting are mentioned as factors leading to greater patient morbidity.
Hypermobility of First Ray: cause or effect of Hallux Valgus deformity?
The cause and effect between HV and FRH continue to be debated. To the clinician, it is a much more complicated matter, as the relationship between the deformity in the transverse plane and motion in the sagittal plane is more involved. It has been paralleled by some investigators to the philosophic debate: “Which came first, the chicken or the egg?”
Understanding the anatomic and radiographic examination of the I-MTCJ is critical to choosing an appropriate treatment algorithm for the surgical management of HV deformity. Many investigators think hypermobility arises secondarily from malalignment of the soft tissue constraints as the HV deformity progresses. Other investigators think hypermobility is a primary cause of the HV and have reported good results with surgical correction including a I-MTCJ arthrodesis.
According to a recent systematic review by Shibuya et al., there was a mean significant 3.62 mm increase of FR sagittal mobility in patients with HV compared with patients without it (75,83). Doty et al. demonstrate in a cadaveric study that dorsal motion using the Klaue device increased from 4.0 mm to 4.5 mm in specimens with mild to severe HV (48). However, it is still in discussion whether the FRM in patients with HV is the cause or the result of the deformity: in early reports, there was no consensus (41).
Regarding this dilemma, Coughlin and Jones (77) performed a prospective study on distal soft tissue reconstruction and proximal metatarsal osteotomy, showing a significant reduction of sagittal plane motion using a Klaue device. Correcting HV deformity and stabilizing sagittal plane motion without I-MTCJ arthrodesis, they concluded that FR instability is the result of the deformity and not the cause (41). The same conclusion was reached by Coughlin et al. (Table 2) using cadaver specimens, applying the identical procedure of the clinical prospective study (76).
Conclusions
From a clinical point of view, it is the belief of the authors that FRH should be assessed routinely in the clinical setting respecting both the triplane motion of FR and the 3-dimensional deformity of HV. To improve assessment, clinical practical tests without any sophisticated equipment, are necessary, even if their validity and reliability can be questionable. In the clinical context, manual tests and the use of a Klaue device or rulers are the easiest methods to implement FRM measures, better at 45° in the transverse plane to respect the FR biomechanics.
In relation to HV surgical correction, the original or modified Lapidus procedures are still valid to improve medial column stability. However, the historical theories seem to lack consensus in the recent literature regarding its exclusive role in correction of HV deformity and hypermobility, as also other more recent procedures seem to provide good outcomes for both.
Finally, only by implementing the measurement of FRM during clinical practice and its pre- and post-operative evaluations for the several HV techniques, will it be possible to come to the definitive conclusion whether FRH is the cause or consequence of the HV deformity. In the meantime, it remains academically controversial.
Authors’ contribution
All authors listed meet the authorship criteria according to the latest guidelines of the International Committee of Medical Journal Editors, and all authors are in agreement with the manuscript.
C.B., E.M., G.M.: study concept and design; writing/review/editing of manuscript;
E.M. and G.M.: literature research and data collection;
C.B. and J.T.: analysis, interpretation and discussion of literature research;
P.R.: final approval of the version to be published.
Funding:
This research received no external funding.
Conflict of interest:
The authors declare that they have no conflict of interest related to the publication of this manuscript, and they have not received benefits or financial funds in support of this study.
References
- 1.Voellmicke KV, Deland JT. Manual examination technique to assess dorsal instability of the first ray. Foot ankle Int. 2002 Nov 17;23(11):1040–1. doi: 10.1177/107110070202301113. [DOI] [PubMed] [Google Scholar]
- 2.Glasoe WM, Allen MK, Saltzman CL, Ludewig PM, Sublett SH. Comparison of Two Methods Used to Assess First-Ray Mobility. Foot Ankle Int. 2002 Mar 28;23(3):248–52. doi: 10.1177/107110070202300310. [DOI] [PubMed] [Google Scholar]
- 3.Morton DJ. Hypermobility of the first metatarsal bone: the interlinking factor between metatarsalgia and longitudinal arch strains. JBJS. 1928;10(2):187–196. [Google Scholar]
- 4.Lapidus PW. The operative correction of the metatarsus primus varus in hallux valgus. Surg Gynecol Obs. 1934:183–91. [Google Scholar]
- 5.Lapidus PW. A quarter of a century of experience with the operative correction of the metatarsus varus primus in hallux valgus. Bull Hosp Joint Dis. 1956 Oct;17(2):404–21. [PubMed] [Google Scholar]
- 6.Lapidus PW. The author’s bunion operation from 1931 to 1959. Clin Orthop Relat Res. 1960;16:119–35. [PubMed] [Google Scholar]
- 7.Courriades H. L’ hypermobilite du premier rayon. Podologie. 1971;6:146–53. [Google Scholar]
- 8.Rodgers MM PC. A device for the measurement of first ray mobility. Proc North Am Congr Biomech. 1986 [Google Scholar]
- 9.Romash MM, Fugate D, Yanklowit B. Passive Motion of the First Metatarsal Cuneiform Joint: Preoperative Assessment. Foot Ankle. 1990 Jun 30;10(6):293–8. doi: 10.1177/107110079001000601. [DOI] [PubMed] [Google Scholar]
- 10.Klaue K, Hansen ST, Masquelet AC. Clinical, Quantitative Assessment of First Tarsometatarsal Mobility in the Sagittal Plane and Its Relation to Hallux Valgus Deformity. Foot Ankle Int. 1994 Jan 17;15(1):9–13. doi: 10.1177/107110079401500103. [DOI] [PubMed] [Google Scholar]
- 11.Faber FWM, Kleinrensink GJ, Mulder PGH, Verhaar JAN. Mobility of the First Tarsometatarsal Joint in Hallux Valgus Patients: A Radiographic Analysis. Foot Ankle Int. 2001 Dec 28;22(12):965–9. doi: 10.1177/107110070102201207. [DOI] [PubMed] [Google Scholar]
- 12.Faber FWM, Mulder PGH, Verhaar JAN. Role of First Ray Hypermobility in the Outcome of the Hohmann and the Lapidus Procedure. J Bone Jt Surg. 2004 Mar;86(3):486–95. doi: 10.2106/00004623-200403000-00005. [DOI] [PubMed] [Google Scholar]
- 13.Fraser JJ, Koldenhoven RM, Saliba SA, Hertel J. Reliability of ankle-foot morphology, mobility, strength and motor performance measures. Int J Sports Phys Ther. 2017 Dec;12(7):1134–49. doi: 10.26603/ijspt20171134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Geng X, Wang C, Ma X, Wang X, Huang J, Zhang C, et al. Mobility of the first metatarsal-cuneiform joint in patients with and without hallux valgus: in vivo three-dimensional analysis using computerized tomography scan. J Orthop Surg Res. 2015 Dec 15;10(1):140. doi: 10.1186/s13018-015-0289-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fraser JJ, Koldenhoven RM, Jaffri AH, Park JS, Saliba SF, Hart JM, et al. Foot impairments contribute to functional limitation in individuals with ankle sprain and chronic ankle instability. Knee Surgery, Sport Traumatol Arthrosc. 2020 May 6;28(5):1600–10. doi: 10.1007/s00167-018-5028-x. [DOI] [PubMed] [Google Scholar]
- 16.Glasoe WM, Yack J, Saltzman CL. The Reliability and Validity of a First Ray Measurement Device. Foot Ankle Int. 2000 Mar 28;21(3):240–6. doi: 10.1177/107110070002100310. [DOI] [PubMed] [Google Scholar]
- 17.Singh D, Biz C, Corradin M, Favero L. Comparison of dorsal and dorsomedial displacement in evaluation of first ray hypermobility in feet with and without hallux valgus. Foot Ankle Surg. 2016 Jun;22(2):120–4. doi: 10.1016/j.fas.2015.05.014. [DOI] [PubMed] [Google Scholar]
- 18.Faber FWM, Kleinrensink G-J, Verhoog MW, Vijn AH, Snijders CJ, Mulder PGH, et al. Mobility of the First Tarsometatarsal Joint in Relation to Hallux Valgus Deformity: Anatomical and Biomechanical Aspects. Foot Ankle Int. 1999 Oct 28;20(10):651–6. doi: 10.1177/107110079902001007. [DOI] [PubMed] [Google Scholar]
- 19.Glasoe WM, Coughlin MJ. A Critical Analysis of Dudley Morton’s Concept of Disordered Foot Function. J Foot Ankle Surg. 2006 May;45(3):147–55. doi: 10.1053/j.jfas.2006.02.008. [DOI] [PubMed] [Google Scholar]
- 20.Roukis TS, Landsman AS. Hypermobility of the first ray: a critical review of the literature. J Foot Ankle Surg. 2003 Nov;42(6):377–90. doi: 10.1053/j.jfas.2003.09.010. [DOI] [PubMed] [Google Scholar]
- 21.Glasoe WM, Yack HJ, Saltzman CL. Anatomy and biomechanics of the first ray. Phys Ther. 1999 Sep;79(9):854–9. [PubMed] [Google Scholar]
- 22.Michaud TC. Human locomotion : the conservative management of gait-related disorders. Newton Biomechanics. 2011:412. [Google Scholar]
- 23.Michaud TC, Nawoczenski DA. The Influence of Two Different Types of Foot Orthoses on First Metatarsophalangeal Joint Kinematics During Gait in a Single Subject. J Manipulative Physiol Ther. 2006 Jan;29(1):60–5. doi: 10.1016/j.jmpt.2005.11.009. [DOI] [PubMed] [Google Scholar]
- 24.Michaud TC. Baltimore: Williams & Wilkins; 1993. Foot orthoses and other forms of conservative foot care; p. 249. [Google Scholar]
- 25.Glasoe WM, Michaud TC. Measurement of Dorsal First Ray Mobility: A Topical Historical Review and Commentary. Foot Ankle Int. 2019 May 22;40(5):603–10. doi: 10.1177/1071100719839692. [DOI] [PubMed] [Google Scholar]
- 26.Greisberg J, Sperber L, Prince DE. Mobility of the First Ray in Various Foot Disorders. Foot ankle Int. 2012;33(1) doi: 10.3113/FAI.2012.0044. [DOI] [PubMed] [Google Scholar]
- 27.Seng C, Chunyin Ho D, Chong KW. Restoring Sesamoid Position in Scarf Osteotomy: A Learning Curve. J Foot Ankle Surg. 2015 Nov;54(6):1089–92. doi: 10.1053/j.jfas.2015.07.001. [DOI] [PubMed] [Google Scholar]
- 28.Chen JY, Rikhraj K, Gatot C, Lee JYY, Singh Rikhraj I. Tibial Sesamoid Position Influence on Functional Outcome and Satisfaction After Hallux Valgus Surgery. Foot Ankle Int. 2016 Nov 20;37(11):1178–82. doi: 10.1177/1071100716658456. [DOI] [PubMed] [Google Scholar]
- 29.de Cesar Netto C, Richter M. Use of Advanced Weightbearing Imaging in Evaluation of Hallux Valgus. Foot Ankle Clin. 2020 Mar;25(1):31–45. doi: 10.1016/j.fcl.2019.10.001. [DOI] [PubMed] [Google Scholar]
- 30.Kelso S, Richie D, Cohen I, Weed J, Root M. Direction and range of motion of the first ray. J Am Podiatr Med Assoc. 1982 Dec;72(12):600–5. doi: 10.7547/87507315-72-12-600. [DOI] [PubMed] [Google Scholar]
- 31.D’Amico JC, Schuster RO. Motion of the first ray: clarification through investigation. J Am Podiatry Assoc. 1979 Jan 1;69(1):17–23. doi: 10.7547/87507315-69-1-17. [DOI] [PubMed] [Google Scholar]
- 32.Hicks JH. The mechanics of the foot. I. The joints. J Anat. 1953 Oct;87(4):345–57. [PMC free article] [PubMed] [Google Scholar]
- 33.Mizel MS. The role of the plantar first metatarsal first cuneiform ligament in weightbearing on the first metatarsal. Foot Ankle. 1993 Feb 17;14(2):82–4. doi: 10.1177/107110079301400205. [DOI] [PubMed] [Google Scholar]
- 34.Doty JF, Harris WT. Hallux Valgus Deformity and Treatment. Foot Ankle Clin. 2018 Jun;23(2):271–80. doi: 10.1016/j.fcl.2018.01.007. [DOI] [PubMed] [Google Scholar]
- 35.Sarrafian SK. Functional Characteristics of the Foot and Plantar Aponeurosis under Tibiotalar Loading. Foot Ankle. 1987 Aug 30;8(1):4–18. doi: 10.1177/107110078700800103. [DOI] [PubMed] [Google Scholar]
- 36.Grebing BR, Coughlin MJ. The Effect of Ankle Position on the Exam for First Ray Mobility. Foot Ankle Int. 2004 Jul 28;25(7):467–75. doi: 10.1177/107110070402500705. [DOI] [PubMed] [Google Scholar]
- 37.Doty JF, Coughlin MJ. Hallux valgus and hypermobility of the first ray: facts and fiction. Int Orthop. 2013 Sep;37(9):1655–60. doi: 10.1007/s00264-013-1977-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Alfieri Montrasio U, Corbo V, Mangiavini L, Palmucci M. Is it still current to talk about first ray hypermobility? Acta Bio Medica Atenei Parm. 2019;90(Suppl 1):32. doi: 10.23750/abm.v90i1-S.8009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.DiGiovanni CW, Greisberg J. Foot and ankle : core knowledge in orthopaedics. Elsevier Mosby; 2007. p. 394. [Google Scholar]
- 40.Rolian C, Lieberman DE, Hallgrímsson B. The Coevolution of Human Hands and Feet. Evolution (N Y) 2010 Jun 1;64(6):1558–68. doi: 10.1111/j.1558-5646.2010.00944.x. [DOI] [PubMed] [Google Scholar]
- 41.Van Beek C, Greisberg J. Mobility of the First Ray: Review Article. Foot Ankle Int. 2011 Sep;32(9):917–22. doi: 10.3113/FAI.2011.0917. [DOI] [PubMed] [Google Scholar]
- 42.Dullaert K, Hagen J, Klos K, Gueorguiev B, Lenz M, Richards RG, et al. The influence of the Peroneus Longus muscle on the foot under axial loading: A CT evaluated dynamic cadaveric model study. Clin Biomech (Bristol, Avon) 2016 May;34:7–11. doi: 10.1016/j.clinbiomech.2016.03.001. [DOI] [PubMed] [Google Scholar]
- 43.Wanivenhaus A, Pretterklieber M. First Tarsometatarsal Joint: Anatomical Biomechanical Study. Foot Ankle. 1989 Feb;9(4):153–7. doi: 10.1177/107110078900900401. [DOI] [PubMed] [Google Scholar]
- 44.Merton L, Root, John H, Weed WPO. Normal and Abnormal Function of the Foot - Clinical Biomechanics Volume II -. Clinical Biomechanics Corp: Los Angeles, CA U, editor. 1977 [Google Scholar]
- 45.Tavara-Vidalón SP, Monge-Vera MÁ, Lafuente-Sotillos G, Domínguez-Maldonado G, Munuera-Martínez P V. Static Range of Motion of the First Metatarsal in the Sagittal and Frontal Planes. J Clin Med. 2018 Nov 21;7(11) doi: 10.3390/jcm7110456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Glasoe WM, Allen MK, Saltzman CL. First Ray Dorsal Monility in Relation to Hallux Vlagus Deformity and First Intermetatarsal Angle. Foot Ankle Int. 2001 Feb 14;22(2):98–101. doi: 10.1177/107110070102200203. [DOI] [PubMed] [Google Scholar]
- 47.Kim J-Y, Hwang SK, Lee KT, Young K won, Jung JS. A Simpler Device for Measuring the Mobility of the First Ray of the Foot. Foot Ankle Int. 2008 Feb;29(2):213–8. doi: 10.3113/FAI.2008.0213. [DOI] [PubMed] [Google Scholar]
- 48.Doty JF, Coughlin MJ, Hirose C, Stevens F, Schutt S, Kennedy M, et al. First Metatarsocuneiform Joint Mobility. Foot Ankle Int. 2014 May 21;35(5):504–11. doi: 10.1177/1071100714524556. [DOI] [PubMed] [Google Scholar]
- 49.Coughlin MJ, Shurnas PS. Hallux Valgus in Men Part II: First Ray Mobility after Bunionectomy and Factors Associated with Hallux Valgus Deformity. Foot Ankle Int. 2003 Jan 28;24(1):73–8. doi: 10.1177/107110070302400112. [DOI] [PubMed] [Google Scholar]
- 50.Roling BA, Christensen JC, Johnson CH. Biomechanics of the first ray. Part IV: The effect of selected medial column arthrodeses. A three-dimensional kinematic analysis in a cadaver model. J Foot Ankle Surg. 2002 Sep;41(5):278–85. doi: 10.1016/s1067-2516(02)80045-x. [DOI] [PubMed] [Google Scholar]
- 51.Kawakami W, Takahashi M, Iwamoto Y, Shinakoda K. Coordination Among Shank, Rearfoot, Midfoot, and Forefoot Kinematic Movement During Gait in Individuals With Hallux Valgus. J Appl Biomech. 2019 Feb;35(1):44–51. doi: 10.1123/jab.2017-0319. [DOI] [PubMed] [Google Scholar]
- 52.Geng X, Wang C, Ma X, Wang X, Huang J, Zhang C, et al. Mobility of the first metatarsal-cuneiform joint in patients with and without hallux valgus: in vivo three-dimensional analysis using computerized tomography scan. J Orthop Surg Res. 2015 Sep 15;10(1):140. doi: 10.1186/s13018-015-0289-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Greisberg J, Assal M, Hansen ST, Sangeorzan BJ. Isolated Medial Column Stabilization Improves Alignment in Adult-acquired Flatfoot. Clin Orthop Relat Res. 2005 Jun;NA(435):197–202. doi: 10.1097/01.blo.0000157658.17056.46. [DOI] [PubMed] [Google Scholar]
- 54.Cowie S, Parsons S, Scammell B, McKenzie J. Hypermobility of the first ray in patients with planovalgus feet and tarsometatarsal osteoarthritis. Foot Ankle Surg. 2012 Dec;18(4):237–40. doi: 10.1016/j.fas.2012.01.004. [DOI] [PubMed] [Google Scholar]
- 55.Heng ML, Krishnasamy P, Kong PW. First ray mobility and posterior tibial tendon dysfunction (PTTD) in persons with flatfoot: A case control study. Foot. 2018 Dec;37:57–60. doi: 10.1016/j.foot.2018.08.001. [DOI] [PubMed] [Google Scholar]
- 56.Cornwall MW, Fishco WD, McPoil TG, Lane CR, O’Donnell D, Hunt L. Reliability and validity of clinically assessing first-ray mobility of the foot. J Am Podiatr Med Assoc. 2004;94(5):470–6. doi: 10.7547/0940470. [DOI] [PubMed] [Google Scholar]
- 57.Tavara-Vidalón SP, Monge-Vera MÁ, Lafuente-Sotillos G, Domínguez-Maldonado G, Munuera-Martínez P V. Static Range of Motion of the First Metatarsal in the Sagittal and Frontal Planes. J Clin Med. 2018;7(11) doi: 10.3390/jcm7110456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.TE K, WA W. First metatarsal head shape in juvenile hallux abducto valgus. J Foot Surg. 1991 Sep 1;30(5):506–8. [PubMed] [Google Scholar]
- 59.Greisberg J, Prince D, Sperber L. First Ray Mobility Increase in Patients With Metatarsalgia. Foot Ankle Int. 2010 Nov;31(11):954–8. doi: 10.3113/FAI.2010.0954. [DOI] [PubMed] [Google Scholar]
- 60.Glasoe WM, Allen MK, Yack HJ. Measurement of Dorsal Mobility in the First Ray: Elimination of Fat Pad Compression as a Variable. Foot Ankle Int. 1998 Aug 17;19(8) doi: 10.1177/107110079801900807. [DOI] [PubMed] [Google Scholar]
- 61.Glasoe WM, Getsoian S, Myers M, Komnick M, Kolkebeck D, Oswald W, et al. Criterion-Related Validity of a Clinical Measure of Dorsal First Ray Mobility. J Orthop Sport Phys Ther. 2005 Sep;35(9):589–93. doi: 10.2519/jospt.2005.35.9.589. [DOI] [PubMed] [Google Scholar]
- 62.Fritz GR, Prieskorn D. First Metatarsocuneiform Motion: A Radiographic and Statistical Analysis. Foot Ankle Int. 1995 Mar 28;16(3):117–23. doi: 10.1177/107110079501600302. [DOI] [PubMed] [Google Scholar]
- 63.Cruz FD. Literature Review of Hypermobile First Ray. North Ohio Foot Ankle J. 2016;3(3) [Google Scholar]
- 64.Martin H, Bahlke U, Dietze A, Zschorlich V, Schmitz K-P, Mittlmeier T. Investigation of first ray mobility during gait by kinematic fluoroscopic imaging-a novel method. BMC Musculoskelet Disord. 2012 Dec 9;13(1):14. doi: 10.1186/1471-2474-13-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Kimura T, Kubota M, Suzuki N, Hattori A, Marumo K. Comparison of Intercuneiform 1-2 Joint Mobility Between Hallux Valgus and Normal Feet Using Weightbearing Computed Tomography and 3-Dimensional Analysis. Foot Ankle Int. 2018 Mar 4;39(3):355–60. doi: 10.1177/1071100717744174. [DOI] [PubMed] [Google Scholar]
- 66.Swanson JE, Stoltman MG, Oyen CR, Mohrbacher JA, Orandi A, Olson JM, et al. Comparison of 2D-3D Measurements of Hallux and First Ray Sagittal Motion in Patients With and Without Hallux Valgus. Foot Ankle Int. 2016 Feb 8;37(2):227–32. doi: 10.1177/1071100715604238. [DOI] [PubMed] [Google Scholar]
- 67.Stiglitz Y, Cazeau C, Klouche S, Bauer T. Reliability of a new dynamic ultrasound test for quantifying first-ray mobility. Orthop Traumatol Surg Res. 2019 Oct;105(6):1131–6. doi: 10.1016/j.otsr.2019.02.016. [DOI] [PubMed] [Google Scholar]
- 68.Bednarz PA, Manoli A. Modified Lapidus Procedure for the Treatment of Hypermobile Hallux Valgus. Foot Ankle Int. 2000 Oct 26;21(10):816–21. doi: 10.1177/107110070002101004. [DOI] [PubMed] [Google Scholar]
- 69.Lee KT, Young K. Measurement of first-ray mobility in normal vs. hallux valgus patients. Foot ankle Int. 2001 Dec 28;22(12):960–4. doi: 10.1177/107110070102201206. [DOI] [PubMed] [Google Scholar]
- 70.Smith BW, Coughlin MJ. The first metatarsocuneiform joint, hypermobility, and hallux valgus: What does it all mean. Foot Ankle Surg. 2008 Jan;14(3):138–41. doi: 10.1016/j.fas.2008.05.006. [DOI] [PubMed] [Google Scholar]
- 71.Nix S, Smith M, Vicenzino B. Prevalence of hallux valgus in the general population: a systematic review and meta-analysis. J Foot Ankle Res. 2010 Dec 27;3(1):21. doi: 10.1186/1757-1146-3-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Mansur NSB, de Souza Nery CA. Hypermobility in Hallux Valgus. Foot Ankle Clin. 2020 Mar;25(1):1–17. doi: 10.1016/j.fcl.2019.10.004. [DOI] [PubMed] [Google Scholar]
- 73.Davenport KL, Simmel L, Kadel N. Hallux Valgus in Dancers: A Closer Look at Dance Technique and Its Impact on Dancers’ Feet. J Danc Med Sci. 2014 Jun 15;18(2):86–92. doi: 10.12678/1089-313X.18.2.86. [DOI] [PubMed] [Google Scholar]
- 74.Biz C, Favero L, Stecco C, Aldegheri R. Hypermobility of the first ray in ballet dancer. Muscles Ligaments Tendons J. 2012 Oct;2(4):282–8. [PMC free article] [PubMed] [Google Scholar]
- 75.Shibuya N, Roukis TS, Jupiter DC. Mobility of the First Ray in Patients With or Without Hallux Valgus Deformity: Systematic Review and Meta-Analysis. J Foot Ankle Surg. 2017 Sep;56(5) doi: 10.1053/j.jfas.2017.05.021. [DOI] [PubMed] [Google Scholar]
- 76.Coughlin MJ, Jones CP, Viladot R, Glanó P, Grebing BR, Kennedy MJ, et al. Hallux Valgus and First Ray Mobility: A Cadaveric Study. Foot Ankle Int. 2004 Aug;25(8):537–44. doi: 10.1177/107110070402500805. [DOI] [PubMed] [Google Scholar]
- 77.Coughlin MJ, Jones CP. Hallux Valgus and First Ray Mobility. A prospective study. J Bone Jt Surg. 2007 Sep;89(9):1887–98. doi: 10.2106/JBJS.F.01139. [DOI] [PubMed] [Google Scholar]
- 78.Coughlin MJ, Grebing BR, Jones CP. Arthrodesis of the First Metatarsophalangeal Joint for Idiopathic Hallux Valgus: Intermediate Results. Foot Ankle Int. 2005 Oct 28;26(10):783–92. doi: 10.1177/107110070502601001. [DOI] [PubMed] [Google Scholar]
- 79.Kim J-Y, Park JS, Hwang SK, Young KW, Sung IH. Mobility changes of the first ray after hallux valgus surgery: clinical results after proximal metatarsal chevron osteotomy and distal soft tissue procedure. Foot ankle Int. 2008 May;29(5):468–72. doi: 10.3113/fai.2008.0468. [DOI] [PubMed] [Google Scholar]
- 80.Ellington JK, Myerson MS, Coetzee JC, Stone RM. The Use of the Lapidus Procedure for Recurrent Hallux Valgus. Foot Ankle Int. 2011 Jul;32(7):674–80. doi: 10.3113/FAI.2011.0674. [DOI] [PubMed] [Google Scholar]
- 81.Rush SM, Christensen JC, Johnson CH. Biomechanics of the first ray. Part II: Metatarsus primus varus as a cause of hypermobility. A three-dimensional kinematic analysis in a cadaver model. J Foot Ankle Surg. 2000 Mar;39(2):68–77. doi: 10.1016/s1067-2516(00)80030-7. [DOI] [PubMed] [Google Scholar]
- 82.Myerson M, Kadakia AR, Myerson M. 3rd edition. Elsevier; 2018. Reconstructive foot and ankle surgery : management of complications; pp. 13–26. [Google Scholar]
- 83.Li S, Myerson MS. Evolution of Thinking of the Lapidus Procedure and Fixation. Foot Ankle Clin. 2020 Mar;25(1):109–26. doi: 10.1016/j.fcl.2019.11.001. [DOI] [PubMed] [Google Scholar]
- 84.Galli MM, McAlister JE, Berlet GC, Hyer CF. Enhanced Lapidus Arthrodesis: Crossed Screw Technique With Middle Cuneiform Fixation Further Reduces Sagittal Mobility. J Foot Ankle Surg. 2015 May;54(3):437–40. doi: 10.1053/j.jfas.2014.10.008. [DOI] [PubMed] [Google Scholar]
- 85.Blackwood S, Gossett L. Hallux Valgus/Medial Column Instability and Their Relationship with Posterior Tibial Tendon Dysfunction. Foot Ankle Clin. 2018 Jun;23(2):297–313. doi: 10.1016/j.fcl.2018.02.003. [DOI] [PubMed] [Google Scholar]
- 86.Willegger M, Holinka J, Ristl R, Wanivenhaus AH, Windhager R, Schuh R. Correction power and complications of first tarsometatarsal joint arthrodesis for hallux valgus deformity. Int Orthop. 2015 Mar 28;39(3):467–76. doi: 10.1007/s00264-014-2601-x. [DOI] [PubMed] [Google Scholar]


