Abstract
Background and aim of the work:
The long head of biceps (LHB) is one of the tendons of the rotator cuff that runs strictly close to the humeral head. In case of pathology, it can be responsible for pain and shoulder impairment: in such cases, surgical options include tenotomy or tenodesis. The management of LHB along with surgery of the rotator cuff or during shoulder prosthetic replacement has been widely discussed in the literature. Conversely, the possibility of acute impingement and incarceration of LHB in proximal humerus fractures, as well as its role in shoulder pain in outcomes of these fractures, has been poorly considered.
Methods:
The following aspects in the literature on LHB and proximal humerus fractures have been analysed: its management during fixation of fractures, the possibility of interference of the tendon with reduction of fractures or dislocations of the shoulder and its possible role in chronic pain after fixation of proximal humerus fractures.
Results:
LHB can be an obstacle in the reduction of fractures, dislocations and fracture-dislocations. Only a few papers take into account acute surgery to LHB (tenotomy or tenodesis); most of the studies on fixation of proximal humerus fractures simply ignore the problem of LHB. The tendon can be a source of pain and a cause of disability in sequelae of these fractures.
Conclusions:
LHB should be taken into consideration both in the acute phase of fractures of the proximal humerus and in the outcomes. Other studies are needed to better understand its optimal management during fracture surgery. (www.actabiomedica.it)
Keywords: long head of biceps, proximal humerus fracture, tenotomy, tenodesis
Introduction
When observing the anatomy of the proximal humerus, it is possible to schematically describe four bony parts connected by two “necks”, i.e. surgical and anatomical neck. The four parts are the metaphysis, the epiphysis (with the cartilage surface) and two tuberosities. The greater and the lesser tuberosities serve as an insertion of the rotator cuff and they are divided by the intertubercular groove. The long head of biceps (LHB) slides into this groove, surrounded by the synovial membrane and covered by the transverse humeral ligament (1, 2).
In 1970, based on this division, Neer made his classification of proximal humerus fractures (2), which is still used, although many new classifications have been formulated in recent decades. Neer classification divides the fracture into two, three or four parts, depending on the involvement of the surgical neck, greater and lesser tuberosity.
Proximal humerus fractures account for about 5–10% of all fractures in adults, the majority of which are attributable to osteoporosis and are caused by low-energy traumas; the incidence of such fractures is increasing worldwide as a result of an aging society, especially in females (3, 4).
Non-operative treatment, with early reprise of active movement, is a well approved solution for many of these fractures, particularly with undisplaced and stable or even in displaced fracture patterns in low-demand patients. Complex unstable fractures, displaced fractures and fracture-dislocation very often require surgical treatment, with open reduction and internal fixation (nearly 20% of all the cases). Anatomic or reverse shoulder arthroplasty is often suggested in the elderly, while in adults and young people every effort should be made to preserve the humeral head, with open reduction and internal fixation as treatment of choice (5, 6). Despite new advances in techniques and materials, the purchase of hardware remains challenging, especially in osteoporotic and/or comminuted bones. Even with fixed-angle devices and with the improvement of “soft tissue-friendly” techniques, several complications can occur (implant loosening, cut-out or cut-through of the screws in the humeral head, etc.); moreover, the rate of unsatisfactory clinical results (limited range of movement, painful joint, etc.) remains relatively high (7, 8).
Standard X-rays and computed tomography (CT) can be used to better evaluate the fracture, especially the head-splitting component, the extent of comminution and the fracture configuration of the tuberosities (5, 9).
Minor malunion of the proximal humerus without displacement is usually well tolerated; however, in some cases, after internal fixation of a humeral fracture, chronic and recurrent pain and limited range of motion can worsen shoulder girdle function. While in some cases the reasons for these bad results are evident (head necrosis, gross tuberosities malalignment, non-union, etc.), in other cases, despite X-rays showing a perfect restoration of the anatomy of the proximal humerus, the causes of poor outcomes remain unclear (10).
LHB: anatomy, pathology and treatment
LHB originates from the upper tubercle of the glenoid, runs laterally and anteriorly above the head of the humerus in its groove, where it is stabilized by a pulley (Figure 1a-b), and then runs vertically until its myotendinous junction.
Figure 1a – 1b.
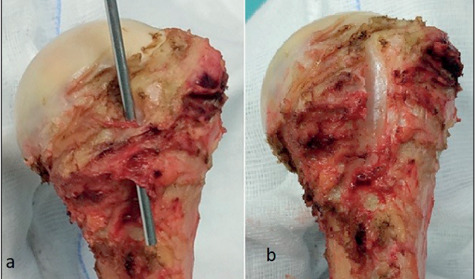
Left proximal humerus of anatomical specimen. Figure a: a probe is in the bicipital groove, closed by the pulley of LHB. Figure b: the pulley has been resected, revealing the intertubercular groove
Its main role is not clearly understood. Its contribution as a shoulder lifter is very poor; a role as a humerus head depressor was hypothesized, but clinical studies have not confirmed this. More recently, its possible involvement in shoulder stability has been considered. However, its main action takes place at the level of the forearm as a supinator and flexor of the elbow (11-14).
Disorders of LHB, both inflammatory and degenerative, play an important role in shoulder pain and in limitation of glenohumeral range of motion. Pathologies of LHB are very frequent, due to its peculiar intra-articular position and to the poor blood supply in this area.
Isolate disorders of LHB account for only 5% of the total; it is more common to observe LHB pathology along with rotator cuff injury or in sequelae of proximal humerus trauma.
Diagnosis is primarily made on clinical tests. Palpation of the tendon at the level of the bicipital groove can evoke pain; in the case of tendon dislocation, it is sometimes possible to perceive a “click” of the tendon during shoulder rotations. Speed and O’Brien tests are reliable in detecting LHB pathology, although they lack absolute specificity. In the case of acute complete rupture of LHB, the patient may report the sensation of a “snap” followed by diffuse ecchymosis. The anatomical profile of the arm will often be altered by the typical Popeye sign (15-17).
Ultrasound is a useful and inexpensive tool to analyse LHB; magnetic resonance imaging (MRI) – or, potentially, MRI arthrography – is the most accurate diagnostic exam to detect LHB lesions and, generally, shoulder disorders. Arthroscopy, as a diagnostic and therapeutic tool, can directly view the tendon in its intra-articular portion and near the pulley, while it cannot follow it distally.
General indications for surgical treatment are the following:
- complete lesion of the tendon in young and high-demand patients;
- partial, symptomatic lesions that exceed 25% of the tendon section;
- instability of the tendon at the level of the pulley;
- disabling chronic tendonitis not responsive to conservative therapy for more than six months (18).
In case of surgery on LHB, the operation should address the potential shoulder pathology associated.
The surgical options to treat LHB pathologies are tenodesis and tenotomy. In the tenotomy procedure, the tendon is cut near its glenoid insertion and a resection of the worn tendon can be associated. This is a fast and effective procedure, although with a high incidence of Popeye sign; some studies underline the possibility of supination and flexion deficits in high-demand patients. Tenodesis, on the other hand, reduces the risk of Popeye sign and strength deficit, but it is not free from potential risks (pain or soreness in the biceps muscle, stiffness, neurologic or vascular injury, proximal humerus fracture and reflex sympathetic dystrophy). The two techniques have been studied especially in association with repair of rotator cuff: they are both effective tools in reducing pain and improving joint function. The choice between tenodesis or tenotomy is often left to the surgeon and the literature has not clearly shown a superiority of one procedure over the other (19-22) (Fig. 2).
Figure 2.

Patient who underwent a right proximal humerus internal fixation with tenotomy of LHB compared to his healthy left side: only a slight Popeye sign can ben noted and no diffference of shoulder function (writing authors case)
LHB in fractures and dislocations of the shoulder
In the literature, there are case reports of axillary artery entrapment in proximal humerus fractures, but very few papers report the entrapment of LHB between fracture fragments. In some cases, the fracture was actually a fracture-dislocation of the shoulder (5).
Lucas et al. underwent a cadaveric study to investigate a potential LHB tendon impingement by a simulated proximal humeral fracture. A fracture at the level of the surgical neck of the humerus, immediately above the insertion of the pectoral, was performed. After manipulating the fracture in multiple directions, the LHB tendon did not become interposed into the fracture site at any point of the wide range of humeral motion. These findings can explain the rarity of entrapment of LHB in fractures, even in multifragmentary ones. In fracture-dislocations, the possibility of entrapment could be slightly more frequent due to a major dislocation of the fracture fragments (23).
Henderson (24) reported a case of fracture-dislocation of the shoulder in a patient treated with electro-convulsive therapy (this paper dates to 1952). LHB was entrapped between the humeral head and the greater tuberosity, thus preventing any possibility of the anatomic reduction of the tuberosity. Similar findings were reported by Pantazis in a fracture-dislocation of the shoulder (25).
Nour describes a 43-year-old male who sustained a multifragmentary fracture of the proximal humerus after a ski accident. The author performed a capsulotomy via a deltopectoral (DP) approach and he found LHB entrapped in the fracture of the humeral head (26).
The writing authors (unpublished data) observed entrapment of LHB in a fracture-dislocation of the shoulder. The humeral head was dislocated anteriorly and any attempt at its reduction with external manoeuvres was unsuccessful. The patient was operated in a beach chair position via a DP approach: LHB lay between the humeral head and the greater tuberosity (Figure 3). After tenotomy of LHB, the dislocation was reduced and the fracture fixed with a locked plate.
Figure 3.
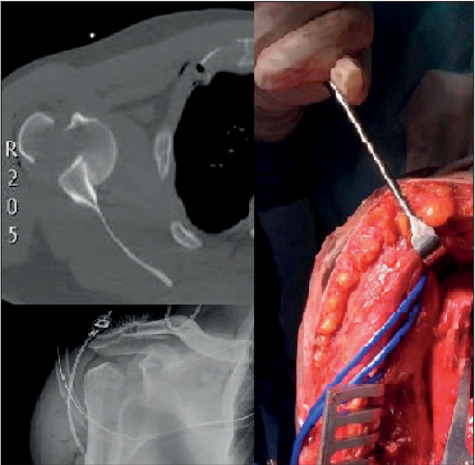
Fracture-dislocation of the right shoulder with interposition of LHB (white arrow) between head and Greater tuberosity
Some authors discussed the problem of LHB in proximal humeral fractures in the paediatric population: they recommend open reduction after failure of one or two attempts at close reduction of the fracture.
Bahrs et al. discussed 43 cases of proximal humeral fractures in children and adolescents concluding that a failed closed reduction should be interpreted as a possible soft tissue entrapment, most likely because of LHB (27).
Similar findings were reported by Visser in physeal injuries of the proximal humerus in children (all Salter-Harris type II), who underwent open reduction and internal fixation of severely displaced fracture fragments, finding interposition of both LHB and periosteum (28). Lucas reported four cases of LHB entrapment, treated only with external manipulation for reduction of the fracture, with good radiographic and clinical results (23).
Pandya reported ten children of a mean age of 14 years with proximal humerus fractures with severe displacement/angulation, impossible to reduce in a close manner. The cause of impossible close reduction interposition of the periosteum was found to be LHB, deltoid muscle and bone fragments. For this reason, the author deemed indicated open reduction of the fractures in such cases (29).
Shoulder dislocation affects young and old people alike; in the latter case, there is frequent association with rotator cuff tears (either concomitant or previous) and, in the case of involvement of the subscapularis, the pulley can be damaged, thus leading LHB to dislocate. In the event of surgical treatment after shoulder dislocation (Bankart lesion repair, Latarjet procedure, etc.), tenodesis or tenotomy of LHB are mandatory if rotator cuff is grossly torn (30, 31).
In the literature, there are also case reports of posterior incarceration of LHB in association with anterior dislocations of the shoulder. The cases described are consequent to high-energy traumas causing anterior dislocation of the humeral head, massive lesion of the rotator cuff, destruction of the pulley and posterolateral dislocation of LHB. The authors highlight the impossibility of close reduction of shoulder dislocation: the incarceration of LHB is finally detected with MRI. The treatment of choice is open reduction via a DP approach, followed by capsule-tendon reconstruction and LHB tenodesis (32-34).
LHB in rotator cuff and shoulder prosthetic replacement surgery
In many rotator cuff tears, because of great pressure and friction on the biceps tendon, LHB is affected by inflammatory, hypertrophic and degenerative processes or tendon sheet partial lesions. On the other hand, LHB rupture is highly correlated with the presence of rotator cuff disease, with the majority of patients presenting full-thickness tears of the supraspinatus (35). As mentioned earlier, during operation for rotator cuff pathology, tenotomy and tenodesis are validated techniques for the treatment of lesions of LHB.
Partial lesion of the tendon (>25% of its diameter), hypertrophy or massive inflammation are main indications for surgical treatment of LHB in association with repair of the rotator cuff involving the supraspinatus tendon. In the case of tear of subscapularis tendon, the involvement of the pulley is very frequent, with consequent instability of LHB, with medial dislocation. This is an absolute indication for tenodesis or tenotomy of LHB. Finally, massive rotator cuff tears are defined as tears involving the subscapularis, supra- and infraspinatus; an intact and macroscopically healthy LHB should be preserved in such cases. In case of instability of the tendon, this should be stabilized in its groove. Furthermore, LHB can provide a framework for the attachment of extrinsic musculotendinous transfers or be incorporated into intra-cuff transfers for greater strength in the repair (18, 36-39).
In elderly patients (>70 years), hemiarthroplasty (HA) or reverse shoulder arthroplasty (RSA) are well accepted options for the treatment of complex fractures of proximal humerus.
In case of HA, the anatomy of the shoulder is preserved and management of LHB must be considered. Preservation of LHB can cause residual pain and it contributes to impaired function of the shoulder, given that, by passing over the prosthetic head, it can impinge with it, especially in cases of bulky prosthetic domes. Tosounidis analysed histology and immunohistochemistry of LHB in shoulders treated with HA for humerus fracture with preservation of the tendon (fracture group). He compared the microscopic findings with tendons harvested from cadaveric shoulders (control group). Severe inflammatory and degenerative processes, even without previous LHB pathology, were noted in the fracture group. Based on the literature, there is strong indication to perform tenotomy or tenodesis of LHB along with the implant of HA of the shoulder (40-42).
RSA is gaining success for the treatment of fractures of the proximal humerus in the elderly, since it has been designed to obtain shoulder elevation even in the case of rotator cuff insufficiency. This is possible by changing the anatomy of the shoulder, which is obtained by distalisation and medialisation of the centre of rotation of the joint. Changing the anatomy of the shoulder means changing the biomechanics: for these reasons, tenodesis or tenotomy of LHB are necessary surgical steps during the operation (43-45).
LHB and approaches to proximal humerus: deltopectoral versus deltoid splitting
DP is the most common approach for plate fixation of proximal humeral fractures: it can be prolonged towards the arm when the fracture extends distally. Furthermore, this approach can be used in the case of immediate or later arthroplasty. It has been used for several years and it has always been considered the gold standard for treating these lesions. However, this approach has some limits: extensive soft tissue dissection and muscle retraction to gain adequate exposure to the lateral aspect of the humerus (especially greater tuberosity), difficulty to seat the plate in anatomic position, risk of injury to circumflex artery and consequent head necrosis. A lateral deltoid splitting (DS) approach (McKenzie and its variation) is a valid alternative to the DP approach and it is gaining more and more popularity. It allows for a direct approach to the greater tuberosity, minimising local soft tissue trauma and proper positioning of the plate (and thus of the screws) on the proximal humerus. The risk of this approach is a lesion to the axillary nerve and, with respect to the topic of the present paper, poor visualization of LHB (4, 8, 9).
With the DP approach, LHB can be easily identified just lateral to the insertion of the subscapularis and followed to its insertion on the superior tubercle of the glenoid. Identification of LHB with the DS approach is more difficult, especially with MIPO technique. However, in three- and four-part fractures of the proximal humerus, which are the most hazardous lesions for the integrity of the tendon, mobilization of the broken tuberosities allow for direct visualization and possible treatment of the tendon. Furthermore, if the incision is carried out slightly more anteriorly (McKenzie approach), then handling of LHB can be easier (4, 8, 9, 46).
In the last few years, some studies have compared the two approaches: while some papers have sustained the superiority of DP, especially for four-part fractures and because of a reduced risk of axillary nerve lesions, some others support DS as a safe and effective surgical approach to treat these fractures, with an inferior head necrosis rate and shorter operation time. However, the majority of the studies and a recent meta-analysis, concluded that both approaches had similar results in functional outcomes, total complication, visual analogue scale and hospital stay (9, 47, 48).
LHB management in proximal humerus fracture fixation
Schai investigated arthroscopically 52 proximal humeral fractures pre-operatively, revealing a significant number of soft tissue lesions (labral, capsuloligamentous and rotator cuff). In 35% of those, there was an involvement of LHB tendon. Even though arthroscopy is not feasible in every proximal humerus fracture, the issue raised by the author is not to underestimate soft tissue lesions in such fractures (49).
In the literature, many surgical techniques to operate proximal humerus fracture are reported, with description of every step of surgery, from the approach to the final fixation (nail, plate and screws, K wire, etc.). Surprisingly, however, very few articles describe the management of LHB.
When treating proximal humerus fractures with plate and screws, some authors mention the management of LHB. Konrad and Khmelnitskaya describe how they identified the tendon of LHB and followed its course cranially using the DP approach. In the case of a fracture running in the intertubercular sulcus and/or if the tendon of LHB is damaged, a tenodesis or a tenotomy are performed after bone fixation. The authors describe their own personal surgical technique, rather than explaining the reasons for that peculiar management of LHB (6, 7).
At our knowledge, only two papers accurately describe and focus their attention on the treatment of LHB.
Kerschbaum et al. described a prospective study on 27 patients (average age 64.5 years) treated for proximal humerus fracture with locked plating. They performed the operation with a DP approach and, along with internal fixation, they pre-operatively opted for tenodesis (younger patients, with high functional and cosmetic demands) or tenotomy (older patients, with low functional and cosmetic demands) of LHB. At an average follow up of 25 months, they found no statistically significant differences between the two groups, neither in term of functionality of the joint, nor in subjective feeling and cosmetic appearance of the shoulder. It should be noted that in this study the authors did not compare the results of the two groups with a third (or a control) group, that could have included internal fixation without any treatment of LHB (50).
Greve et al. performed a retrospective study enrolling 56 patients treated with open reduction and internal fixation with locking plate, by a DP approach. Group 1 (26 patients) underwent LHB tenodesis; Group 2 (control group, 30 patients) was treated with internal fixation alone. The two groups contained similar patients regarding age, gender and fracture pattern. The average follow-up was 1.5 years; the patients were evaluated with the Munich Shoulder Questionnaire (MSQ), the Disability of Arm and Shoulder and Hand (DASH) score and the Shoulder Pain and Disability Index (SPADI). The Popeye sign and O’Brien test were also used to properly assess the status of LHB. Their results showed a better outcome when the patients had been treated with humerus fixation along with biceps tenodesis. The authors concluded that LHB tenodesis is a “promising adjunct” to ORIF of the proximal humerus (5).
LHB in outcomes of proximal humerus fractures
The involvement of the greater and, especially, of the lesser tuberosities in fractures of the proximal humerus can damage the restraints, i.e. transverse humeral ligament and expansions of the subscapularis and the supraspinatus, that stabilize LHB in the intertubercular groove. The damage to these restraints can lead to instability of LHB and, most frequently, to its medial dislocation. It should be noted that the fracture line between the tuberosities is often posterior to the bicipital groove; however, the proximity of LHB tendon to the fracture line and its possible instability can frequently compromise it even in such fractures (1, 51).
After a healed humerus fracture, even in the case of LHB perfectly seated in its groove, displacement of little fragments may cause potential disturbance of the gliding mechanism of the tendon. Thus, the tendon sheet can become frayed and worn and, consequently, be a source of severe pain. Furthermore, in case of malunion of the tuberosities, the intertubercular groove can be severely altered and tendinopathy of LHB can be chronic and disabling (1, 52).
After proximal humerus fixation, standard X-rays are usually done: antero-posterior, internal and external rotation and axillary views can show how accurate the reduction of the fracture has been. CT is rarely needed and MRI is performed exceptionally.
In case of post-traumatic shoulder pain with persistent locking and catching, an MRI – or an MRI arthrogram – can be an option to further investigate the joint, as articular or peri-articular lesions can lead to persistent pain even after a perfect operation. Kattaghen (53) showed the results of shoulder arthroscopy in 46 shoulders after locked plating of proximal humeral fractures, before implant removal. He found that possible sources of pain include articular screw perforation, subacromial plate impingement or articular pathologies – especially of cartilage – LHB and rotator cuff tendons. Pathologies of LHB consist of full-thickness rupture, partial rupture, tendinitis, tendon capture and instability; the author treated these conditions with debridement or tenotomy. He observed that, in many cases, the pathologies of LHB were due to the perforation of the screws and direct damage to the tendon sheets, rather than to an alteration of the anatomy of the intertubercular groove.
Poroes reported a case of an intra-articular dislocation of an unusually long proximal biceps tendon stump. This was a consequence of extra-articular rupture of LHB, due to angular deformity and malunion of the proximal humerus. The patient was treated arthroscopically because of reported symptoms of pain, locking and catching (10).
Conclusions
Many papers describe how to treat – open or arthroscopically – pathologies of LHB, be they isolated or associated to rotator cuff lesions. The surgical options available are tenodesis or tenotomy of LHB, techniques that are equal in terms of clinical and functional outcomes. Even management of LHB along with prosthetic replacement of the shoulder has been described and debated, both in the case of traumatic (fracture) and non-traumatic (degenerative) conditions. Conversely, management of LHB during open reduction and internal fixation of proximal humerus fracture has not been considered in the majority of published papers; only two studies have focused on this topic so far.
Although rare, there is a possibility of acute incarceration of LHB between fragments of proximal humerus fractures or, more often, of fracture-dislocations. This possibility is relatively more frequent in children, especially in severely displaced physeal injuries. In such cases, open reduction, disengagement of the tendon and internal fixation are strongly recommended.
The treatment of LHB during internal fixation of proximal humerus fracture is scarcely debated. The management of the tendon is usually left to the surgeon’s personal technique and preference, without a real analysis of which the ideal treatment (tenodesis, tenotomy or simply ignoring LHB) would be.
There seems to be agreement in treating LHB when macroscopically damaged or when the fracture line runs along the intertubercular groove. The identification of LHB is much easier with the DP approach: the tendon can be followed from extra-articular to intra-articular course, after opening the rotator cuff interval. For this reason, it can be argued that the DP approach is superior to the DS approach when treating proximal humerus fractures. However, regardless of the possible treatment of LHB, the literature has shown that clinical and radiographic results obtained with the two approaches are substantially the same and no significant differences in terms of functional scale of the shoulder have been noted.
Long-term results and outcomes after surgically treated proximal humerus fractures are another matter of debate, in relation to the possibility of LHB as a source of pain and disability. This is the reason why patients can experience shoulder pain after these fractures, even when they look perfectly reduced and fixed. This could depend on LHB-related pain, due to its degeneration, impingement or instability, especially when the fracture has interested the intertubercular groove. However, some papers outline how LHB is very often damaged by protrusion of screws, rather than disturbed by fracture fragments.
In the case of bad outcomes, other radiologic exams should be suggested: CT, MRI (even with an arthrogram) to detect pathology or abnormal course of the tendon. Arthroscopy can be an option to effectively treat these patients.
At the moment, no recommendation can be made for the treatment of LHB along with internal fixation of proximal humerus fractures. In the case of acute impingement or severe damage to the tendon sheets, tenodesis or tenotomy are options to consider. In all the other cases, that are the vast majority, the surgical management of the tendon is guided by the personal experience of the surgeon.
The lack of studies on this topic in the literature could suggest the need for prospective studies comparing patients treated with tenodesis/tenotomy and patients treated only with bone fixation.
Conflict of interest:
Each author declares that he or she has no commercial associations (e.g. consultancies, stock ownership, equity interest, patent/licensing arrangement etc.) that might pose a conflict of interest in connection with the submitted article
References
- 1.Harrison JW, Howcroft DW, Warner JG, Hodgson SP. Internal fixation of proximal humeral fractures. Acta Orthop Belg. 2007 Feb;73(1):1–11. [PubMed] [Google Scholar]
- 2.Neer CS., 2nd Displaced proximal humeral fractures: I. Classification and evaluation. J Bone Joint Surg Am. 1970;52:1077–1089. [PubMed] [Google Scholar]
- 3.Tosounidis T, Hadjileontis C, Georgiadis M, Kafanas A, Kontakis G. The tendon of the long head of the biceps in complex proximal humerus fractures: a histological perspective. Injury. 2010 Mar;41(3):273–8. doi: 10.1016/j.injury.2009.09.015. [DOI] [PubMed] [Google Scholar]
- 4.Buecking B, Mohr J, Bockmann B, Zettl R, Ruchholtz S. Deltoid-split or deltopectoral approaches for the treatment of displaced proximal humeral fractures. Clin Orthop Relat Res. 2014 May;472(5):1576–85. doi: 10.1007/s11999-013-3415-7. doi: 10.1007/s11999-013-3415-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Greve F, Beirer M, Zyskowski M, Crönlein M, Müller M, Pesch S, et al. Prospective outcome analysis following tenodesis of the long head of the biceps tendon along with locking plate osteosynthesis for proximal humerus fractures. Injury. 2019 Mar;50(3):681–685. doi: 10.1016/j.injury.2019.02.003. doi: 10.1016/j.injury.2019.02.003. [DOI] [PubMed] [Google Scholar]
- 6.Khmelnitskaya E1, Lamont LE, Taylor SA, Lorich DG, Dines DM, Dines JS. Evaluation and management of proximal humerus fractures. Adv Orthop. 2012;2012 doi: 10.1155/2012/861598. 861598. doi: 10.1155/2012/861598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Konrad G, Bayer J, Hepp P, Voigt C, Oestern H, Kääb M, et al. Open reduction and internal fixation of proximal humeral fractures with use of the locking proximal humerus plate. Surgical technique. J Bone Joint Surg Am. 2010 Mar;92(Suppl 1 Pt 1):85–95. doi: 10.2106/JBJS.I.01462. doi: 10.2106/JBJS.I.01462. [DOI] [PubMed] [Google Scholar]
- 8.Laux CJ, Grubhofer F, Werner CML, Simmen HP, Osterhoff G. Current concepts in locking plate fixation of proximal humerus fractures. J Orthop Surg Res. 2017 Sep 25;12(1):137. doi: 10.1186/s13018-017-0639-3. doi: 10.1186/s13018-017-0639-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wu CH, Ma CH, Yeh JJ, Yen CY, Yu SW, Tu YK. Locked plating for proximal humeral fractures: differences between the deltopectoral and deltoid-splitting approaches. J Trauma. 2011 Nov;71(5):1364–70. doi: 10.1097/TA.0b013e31820d165d. doi: 10.1097/TA.0b013e31820d165d. [DOI] [PubMed] [Google Scholar]
- 10.Ramos Poroes F, Desmarchelier R, Bauer S. Atypical biceps-related complication of proximal humerus fracture leading to internal shoulder impingement due to tendon stump dislocation. BMJ Case Rep. 2020 Feb 9;13(2):pii: e232124. doi: 10.1136/bcr-2019-232124. doi: 10.1136/bcr-2019-232124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rodosky MW, Harner CD, Fu FH. The role of the long head of the biceps muscle and superior glenoid labrum in anterior stability of the shoulder. Am J Sports Med. 1994;22:121–30. doi: 10.1177/036354659402200119. [DOI] [PubMed] [Google Scholar]
- 12.Warner JJ, McMahon PJ. The role of the long head of the biceps brachii in superior stability of the glenohumeral joint. J Bone Joint Surg [Am] 1995;77-A:366–72. doi: 10.2106/00004623-199503000-00006. [DOI] [PubMed] [Google Scholar]
- 13.Kim SH, Ka KI, Kim HS, Kim SW. Electromyographic activity of the biceps brachii muscle in shoulders with anterior instability. Arthroscopy. 2001;17:864–8. doi: 10.1016/s0749-8063(01)90011-8. [DOI] [PubMed] [Google Scholar]
- 14.Ahrens PM, Boileau P. The long head of biceps and associated tendinopathy. J Bone Joint Surg [Br] AUGUST 2007;89-B(8) doi: 10.1302/0301-620X.89B8.19278. [DOI] [PubMed] [Google Scholar]
- 15.Favorito PJ, Harding WG, III, Heidt RS., Jr Complete arthroscopic examination of the long head of the biceps tendon. Arthroscopy. 2001;17:430–432. doi: 10.1053/jars.2001.22360. [DOI] [PubMed] [Google Scholar]
- 16.Crenshaw AH, Kilgore WE. Surgical treatment of bicipital tenosynovitis. J Bone Joint Surg Am. 1966 Dec;48(8):1496–502. [PubMed] [Google Scholar]
- 17.McFarland EG, Kim TK, Savino RM. Clinical assessment of three common tests for superior labral anterior-posterior lesions. Am J Sports Med. 2002 Nov-Dec;30(6):810–5. doi: 10.1177/03635465020300061001. [DOI] [PubMed] [Google Scholar]
- 18.Zhang Q, Zhou J, Ge H, Cheng B. Tenotomy or tenodesis for long head biceps lesions in shoulders with reparable rotator cuff tears: a prospective randomised trial. Knee Surg Sports Traumatol Arthrosc 2013. 2015 Feb;23(2):464–9. doi: 10.1007/s00167-013-2587-8. doi: 10.1007/s00167-013-2587-8. [DOI] [PubMed] [Google Scholar]
- 19.Ahmad CS, DiSipio C, Lester J, Gardner TR, Levine WN, Bigliani LU. Factors affecting dropped biceps deformity after tenotomy of the long head of the biceps tendon. Arthroscopy. 23(5):537–541. doi: 10.1016/j.arthro.2006.12.030. [DOI] [PubMed] [Google Scholar]
- 20.Checchia SL, Doneux PS, Miyazaki AN, Silva LA, Fregoneze M, Ossada A, et al. Biceps tenodesis associated with arthroscopic repair of rotator cuff tears. J Shoulder Elbow Surg. 14(2):138–144. doi: 10.1016/j.jse.2004.07.013. [DOI] [PubMed] [Google Scholar]
- 21.Franceschi F, Longo UG, Ruzzini L, Papalia R, Rizzello G, Denaro V. To detach the long head of the biceps tendon after tenodesis or not: outcome analysis at the 4-year follow-up of two different techniques. Int Orthop. 31(4):537–545. doi: 10.1007/s00264-006-0206-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Frost A, Zafar MS, Maffulli N. Tenotomy versus tenodesis in the management of pathologic lesions of the tendon of the long head of the biceps brachii. Am J Sports Med. 37(4):828–833. doi: 10.1177/0363546508322179. [DOI] [PubMed] [Google Scholar]
- 23.Lucas JC, Mehlman CT, Laor T. The location of the biceps tendon in completely displaced proximal humerus fractures in children: a report of four cases with magnetic resonance imaging and cadaveric correlation. J Pediatr Orthop. 2004 May-Jun;24(3):249–53. [PubMed] [Google Scholar]
- 24.Henderson SR. Fracture-dislocation of the shoulder with interposition of long head of biceps. J Bone Joint Surg Br. 1952 May;34-B(2):240–1. doi: 10.1302/0301-620X.34B2.240. [DOI] [PubMed] [Google Scholar]
- 25.Pantazis K, Panagopoulos A, Tatani I, Daskalopoulos B, Iliopoulos I, Minos Tyllianakis. Irreducible Anterior Shoulder Dislocation with Interposition of the Long Head of the Biceps and Greater Tuberosity Fracture: A Case Report and Review of the Literature. Open Orthop J. 2017;11:327–334. doi: 10.2174/1874325001711010327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Abdel Nour HG, Joukhadar N, Maalouly J, Ayoubi RA, Aouad DK, El Rassi GS. Entrapment of the Long Head of the Biceps in a Multi-Fragmentary Proximal Humeral Fracture: A Case Report. J Physiother Res. 2(10) [Google Scholar]
- 27.Bahrs C, Zipplies S, Ochs BG, Rether J, Oehm J, Eingartner C, et al. Proximal humeral fractures in children and adolescents. J Pediatr Orthop. 2009 Apr-May;29(3):238–42. doi: 10.1097/BPO.0b013e31819bd9a7. doi: 10.1097/BPO.0b013e31819bd9a7. [DOI] [PubMed] [Google Scholar]
- 28.Visser JD, Rietberg M. Interposition of the tendon of the long head of biceps in fracture separation of the proximal humeral epiphysis. Neth J Surg. 1980;32(1):12–5. [PubMed] [Google Scholar]
- 29.Pandya NK, Behrends D, Hosalkar HS. Open reduction of proximal humerus fractures in the adolescent population. J Child Orthop. 2012 Jun;6(2):111–8. doi: 10.1007/s11832-012-0398-y. doi: 10.1007/s11832-012-0398-y. Epub 2012 Mar 29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.White AE, Patel NK, Hadley CJ, Dodson CC. An algorithmic approach to the management of shoulder instability. J Am Acad Orthop Surg Glob Res Rev. 2019 Dec 23;3(12) doi: 10.5435/JAAOSGlobal-D-19-00168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cibulas A, Leyva A, Cibulas G, 2nd, Foss M, Boron A, Dennison J, et al. Acute Shoulder Injury. Radiol Clin North Am. 2019 Sep;57(5):883–896. doi: 10.1016/j.rcl.2019.03.004. [DOI] [PubMed] [Google Scholar]
- 32.Wortley P, Omar L, Robertson W, Moore D, Sims GC, Omar H. Nonreducible Shoulder Due to Acute Posterior Dislocation of the Long Head of the Biceps Tendon: A Case Report and Review of the Literature. JBJS Case Connect. 2014 Mar 12;4(1 Suppl 8):e261–4. doi: 10.2106/JBJS.CC.M.00032. [DOI] [PubMed] [Google Scholar]
- 33.Seo JB, Yoon SH, Yang JH, Yoo JS. Irreducible posterior fracture and dislocation of shoulder with massive rotator cuff tear due to incarceration of biceps tendon: A case report. J Orthop. 2020 Feb 4;21:6–9. doi: 10.1016/j.jor.2020.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.McArthur C, Welsh F, Campbell C. Posterior dislocation of long head of biceps tendon following traumatic anterior shoulder dislocation: imaging and intra-operative findings. J Radiol Case Rep. 2013 Sep 1;7(9):19–26. doi: 10.3941/jrcr.v7i9.1516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Vestermark GL, Van Doren BA, Connor PM, Fleischli JE, Piasecki DP, Hamid N. The prevalence of rotator cuff pathology in the setting of acute proximal biceps tendon rupture. Shoulder Elbow Surg. 2018 Jul;27(7):1258–1262. doi: 10.1016/j.jse.2018.01.006. doi: 10.1016/j.jse.2018.01.006. Epub 2018 Feb 22. [DOI] [PubMed] [Google Scholar]
- 36.Barber FA, Field LD, Ryu RK. Biceps tendon and superior labrum injuries: decision making. Instr Course Lect. 2008;57:527–538. [PubMed] [Google Scholar]
- 37.Al-Hakim W, Noorani A, Lambert S. Assessment and treatment strategies for rotator cuff tears. Shoulder Elbow. 2015 Apr;7(2):76–84. doi: 10.1177/1758573214557143. doi: 10.1177/1758573214557143. Epub 2014 Oct 31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Godenèche A, Nove-Josserand L, Audebert S, Toussaint B, Denard PJ, Lädermann A. Relationship between subscapularis tears and injuries to the biceps pulley. Knee Surg Sports Traumatol Arthrosc. 2017;25:2114–2120. doi: 10.1007/s00167-016-4374-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Boileau P, Baqué F, Valerio L, Ahrens P, Chuinard C, Trojani C. Isolated arthroscopic biceps tenotomy or tenodesis improves symptoms in patients with massive irreparable rotator cuff tears. J Bone Joint Surg Am. 2007 Apr;89(4):747–57. doi: 10.2106/JBJS.E.01097. [DOI] [PubMed] [Google Scholar]
- 40.Pietu G, Deluzarches P, Goin F, Letenneur J. Complex injuries of the proximal humerus treated with humeral head prosthesis: apropos of 21 cases review after a median follow-up of 4 years. Acta Orthopaedica Belgica. 1992;58:159–69. [PubMed] [Google Scholar]
- 41.Moeckel BH, Dines DM, Warren RF, Altchek DW. Modular hemiarthroplasty for fractures of the proximal part of the humerus. Journal of Bone and Joint Surgery - American Volume. 1992;74-A:884–9. [PubMed] [Google Scholar]
- 42.Green A, Barnard WL, Limbird RS, Providence RI. Humeral head replacement for acute, four-part proximal humerus fractures. Journal of Shoulder and Elbow Surgery. 1993;2:249–54. doi: 10.1016/S1058-2746(09)80084-0. [DOI] [PubMed] [Google Scholar]
- 43.Hawkins RJ, Switlyk P. Acute prosthetic replacement for severe fractures of the proximal humerus. Clinical Orthopaedics. 1993;289:156–60. [PubMed] [Google Scholar]
- 44.Goldman RT, Koval KJ, Cuomo MA, Zuckerman JD. Functional outcome after humeral head replacement for acute three- and four-part proximal humeral fractures. Journal of Shoulder and Elbow Surgery. 1995;4:81–6. doi: 10.1016/s1058-2746(05)80059-x. [DOI] [PubMed] [Google Scholar]
- 45.Omar A, Soliman A, Wael MT. Proximal humeral fractures treated with hemiarthroplasty: Does tenodesis of the long head of the biceps improve results. Injury, Int. J. Care Injured. 2013;44:461–464. doi: 10.1016/j.injury.2012.09.012. [DOI] [PubMed] [Google Scholar]
- 46.Borer J, Schwarz J, Potthast S, Jakob M, Lenzlinger P, Zingg U. Mid-term results of minimally invasive deltoid-split versus standard open deltopectoral approach for PHILOS™ (proximal humeral internal locking system) osteosynthesis in proximal humeral fractures. Eur J Trauma Emerg Surg. 2019 Jan 14 doi: 10.1007/s00068-019-01076-7. doi: 10.1007/s00068-019-01076-7. [DOI] [PubMed] [Google Scholar]
- 47.Mouraria GG, Zoppi A, Kikuta FK, Moratelli L, Cruz MA, Etchebehere M. Anterolateral approaches for proximal humeral osteosynthesis: a systematic review. Acta Ortop Bras. 2019 May-Jun;27(3):178–182. doi: 10.1590/1413-785220192703215572. doi: 10.1590/1413-785220192703215572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Xie L, Zhang Y, Chen C, Zheng W, Chen H, Cai L. Deltoid-split approach versus deltopectoral approach for proximal humerus fractures: A systematic review and meta-analysis. Orthop Traumatol Surg Res. 2019 Apr;105(2):307–316. doi: 10.1016/j.otsr.2018.12.004. doi: 10.1016/j.otsr.2018.12.004. Epub 2019 Mar 14. [DOI] [PubMed] [Google Scholar]
- 49.Schai PA1, Hintermann B, Koris MJ. Preoperative arthroscopic assessment of fractures about the shoulder. Arthroscopy. 1999 Nov-Dec;15(8):827–35. doi: 10.1053/ar.1999.v15.015082. [DOI] [PubMed] [Google Scholar]
- 50.Kerschbaum M, Werth M, Gerhardt C, Scheibel M. Simultaneous surgical treatment of the long head of the biceps tendon during operative treatment of proximal humeral fractures. Unfallchirurg. 2017 Oct;120(10):865–872. doi: 10.1007/s00113-016-0279-9. doi: 10.1007/s00113-016-0279-9. [DOI] [PubMed] [Google Scholar]
- 51.Ahovuo J, Paavolainen P, Björkenheim JM. Fractures of the proximal humerus involving the intertubercular groove. Acta Radiol. 1989 Jul-Aug;30(4):373–4. [PubMed] [Google Scholar]
- 52.Duparc F. Malunion of the proximal humerus. Orthop Traumatol Surg Res. 2013 Feb;99(1 Suppl):S1–11. doi: 10.1016/j.otsr.2012.11.006. doi: 10.1016/j.otsr.2012.11.006. Epub 2013 Jan 16. [DOI] [PubMed] [Google Scholar]
- 53.Katthagen JC, Hennecke D, Jensen G, Ellwein A, Voigt C, Lill H. Arthroscopy after locked plating of proximal humeral fractures: implant removal, capsular release, and intra-articular findings. Arthroscopy. 2014 Sep;30(9):1061–7. doi: 10.1016/j.arthro.2014.04.092. doi: 10.1016/j.arthro.2014.04.092. Epub 2014 Jun 14. [DOI] [PubMed] [Google Scholar]


