Abstract
Background
Rates of thyroid cancer in patients with multinodular goitre (MNG) vary widely, from 3 per cent in older studies to 35 per cent in more recent studies. The purpose of the present study was to evaluate the prevalence of thyroid cancer in patients operated on for MNG, and to determine risk factors for incidental thyroid malignancy.
Methods
A prospectively developed database of all patients who underwent thyroidectomy for a benign MNG at the high-volume endocrine surgery unit of a tertiary referral university hospital was interrogated.
Results
A total of 3233 patients were analysed, separated into three groups according to their functional thyroid status (hypothyroid, hyperthyroid or euthyroid). There were 2788 women (86.2 per cent); the mean patient age was 56.4 years and mean preoperative disease duration was 106.2 months. Incidental thyroid cancer was identified in 1026 patients (31.7 per cent), of which 917 (89.4 per cent) were papillary cancers. Multivariable regression analysis identified functional thyroid status, younger age, male sex, smaller adenoma size, smaller thyroid glands, Hashimoto’s thyroiditis and chronic non-specific thyroiditis as independent risk factors for thyroid cancer.
Conclusion
MNG was associated with a considerable rate of incidental thyroid cancer, which has been underestimated. A variety of factors should be taken into account when considering the malignant potential of a presumed benign MNG.
A wide distribution of thyroid cancer rates has been demonstrated within a multinodular goitre. This study evaluated the incidence of and risk factors for thyroid cancer in patients operated on for benign multinodular goitre.
Resumen
Antecedentes
Las tasas de cáncer de tiroides en pacientes con bocio multinodular (multinodular goitre, MNG) varían ampliamente entre un 3% en estudios de hace años y un 35% en estudios más recientes. El objetivo de este estudio fue evaluar la prevalencia de cáncer de tiroides en pacientes operados de MNG y determinar los factores de riesgo de neoplasia tiroidea incidental.
Métodos
Se consultó una base de datos prospectiva de todos los pacientes sometidos a tiroidectomía por MNG benigno en una unidad de cirugía endocrina de alto volumen de un hospital terciario de referencia.
Resultados
Se analizaron un total de 3.233 pacientes pertenecientes a tres grupos de acuerdo con el estado funcional tiroideo (hipo-, hiper- o eutiroideo). Del total de pacientes, 2.788 fueron mujeres (86,2%) con una edad media de 56,4 años y una duración preoperatoria media de la enfermedad de 106,2 meses. Se identificó cáncer de tiroides incidental en 1.026 pacientes (31,7%), de los cuales un 89,4% fueron cánceres papilares. En el análisis de regresión multivariable, los factores de riesgo independientes de cáncer de tiroides identificados fueron el estado funcional de la glándula, la edad joven, el género masculino, un adenoma de menor tamaño, la glándula tiroidea de menor tamaño, la tiroiditis de Hashimoto y la tiroiditis crónica inespecífica.
Conclusión
El MNG se asoció con una tasa considerable de cáncer de tiroides incidental, que hasta ahora ha sido subestimada. Una variedad de factores debería tenerse presente cuando se considera el potencial maligno de un presunto MNG benigno.
Introduction
Thyroid nodules are common, discovered by palpation in at least 4 per cent of the population in iodine-sufficient areas and in more than half of patients by the use of ultrasonography1,2, with the majority being asymptomatic. They may be associated with local compressive symptoms, causing dysphagia and disordered thyroid hormone production as well as thyroid cancer1,3.
Published data regarding the prevalence of thyroid cancer within a multinodular goitre (MNG) have demonstrated a wide distribution of cancer rates, ranging from 3 to 35 per cent4–6. Although fine-needle aspiration (FNA) is the most accurate and cost-effective method of thyroid nodule evaluation, benign cytological diagnosis is associated with false-negative rates of up to 3 per cent7. Further complicating this topic, FNA cytology may be non-diagnostic in up to 25 per cent of patients with nodular thyroid disease8, and its performance in the setting of MNG presents other difficulties, including deeply located thyroid nodules that may be more challenging to aspirate as well as reliably evaluating all suspicious nodules9.
The purpose of the present study was to evaluate the prevalence of thyroid cancer in patients who had thyroidectomy for MNG, and analyse patient-related parameters to identify risk factors associated with incidental thyroid malignancy.
Methods
This was an observational study of a prospectively created database of all surgical patients from an iodine-sufficient area with a preoperative diagnosis of MNG who underwent thyroidectomy at a high-volume endocrine surgery unit in a tertiary referral university hospital, over a 10-year period between January 2009 and December 2018, with follow-up to the end of March 2020. All patient records were reviewed and parameters considered potentially important as risk factors for cancer development were extracted.
All patients had preoperative thyroid and cervical ultrasound imaging, and all hyperthyroid patients underwent preoperative thyroid scintigraphy. MNG was defined as enlargement of the thyroid gland, accompanied by the presence of two or more nodules in the thyroid parenchyma, on preoperative ultrasonography. The presence of two or more nodules within one thyroid lobe, with the contralateral lobe being normal on preoperative ultrasound imaging, was categorized as asymmetrical MNG, and these patients were included in the analysis. MNG was classified as cervical when less than 50 per cent of the total thyroid volume lay behind the sternum, or as substernal when 50 per cent or more of the gland lay in that location.
Patients were offered surgery, irrespective of their thyroid functional status, for associated compressive symptoms, nodule growth on follow-up, or nodule of 4 cm or more in size on ultrasound imaging. Exclusion criteria included patients with MNG and a preoperative FNA cytology result of atypia or follicular lesion of undetermined significance, follicular neoplasm or suspicion of a follicular neoplasm, suspicion of malignancy or malignancy (Bethesda diagnostic categories III–VI10). All patients with nodule growth and/or suspicious nodule characteristics on ultrasound imaging were evaluated before surgery by FNA of the respective nodule(s); only patients with benign cytology (Bethesda diagnostic category II10) were included in the analysis.
Preoperative thyroid and parathyroid functional assessment was performed in all patients, measuring serum levels of thyroid-stimulating hormone (TSH), free thyroxine, tri-iodothyronine, thyroglobulin (Tg), antithyroid peroxidase antibodies (anti-TPO), antithyroid thyroglobulin antibodies (anti-Tg), intact parathyroid hormone, and calcium. Preoperative serum calcitonin levels were not measured routinely. Hashimoto’s thyroiditis (HT) was diagnosed biochemically by the presence of positive anti-TPO antibodies with or without positive anti-Tg antibodies, confirmed by pathological evidence of lymphocytic infiltration along with atrophy and eosinophilic changes in thyroid cells, as well as the presence of fibrosis11. Chronic non-specific thyroiditis (CNST) was defined as lymphocytic infiltration of thyroid cells without the presence of serum autoantibodies.
The surgical operation performed was total or near-total thyroidectomy. Patients with asymmetrical MNG underwent a hemithyroidectomy, defined as a unilateral lobectomy with excision of the thyroid isthmus.
The final diagnosis was determined by pathological analysis of the surgical specimen, performed by a single pathologist experienced in thyroid malignancy. Papillary microcarcinoma (PTMC) was defined as a papillary thyroid cancer (PTC) not exceeding 1 cm in size, whereas all papillary thyroid cancers greater than 1 cm in size were defined as clinical papillary thyroid cancers12.
Statistical analysis
Statistical analysis was performed using IBM SPSS® Statistics version 26.0 (IBM, Armonk, NY, USA). Continuous data are reported as mean(s.d.) values and analysed with Student’s t test for normally distributed data or ANOVA with Bonferroni post hoc pairwise comparisons. Univariable comparison of categorical variables was performed using Pearson’s χ2 test (or Fisher’s exact test for 2×2 tables). All parameters that demonstrated P <0.100 in univariable analysis were subsequently included in multivariable analysis. Logistic regression analysis for the identification of risk factors associated with thyroid cancer presence was performed for all types of thyroid cancer as well as for PTC, PTMC and Hürthle cell cancer (HCC), independently. Odds ratios (ORs) with 95 per cent c.i. are presented. The level of statistical significance was set at 5 per cent (α = 0.05).
Results
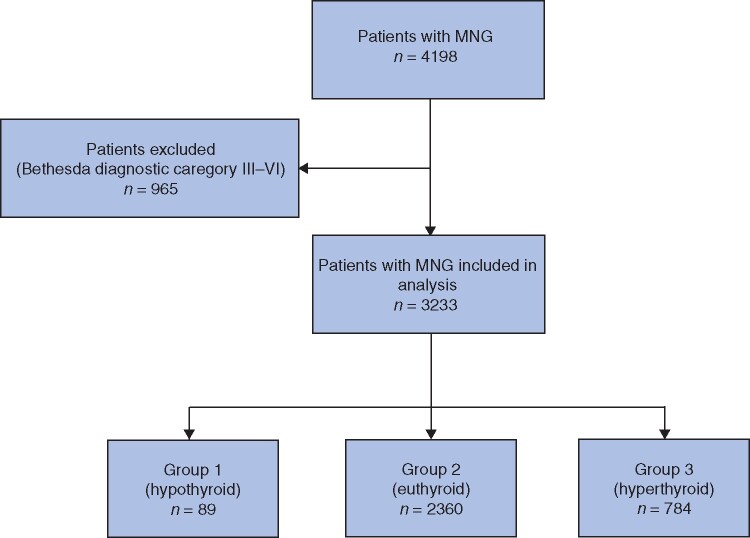
A total of 4198 patients were referred for surgical treatment of MNG during the study interval. After excluding 965 patients with a preoperative cytology result classified as Bethesda diagnostic category III–VI, a total of 3233 patients were included in the analysis. All enrolled patients were categorized according to their functional thyroid status as hypothyroid (group 1), euthyroid (group 2) or hyperthyroid (group 3) (Fig. 1).
Fig. 1.
Flow diagram showing inclusion of patients in the study
MCG, multinodular goitre.
The cohort contained 2788 women (86.2 per cent) and 445 men, with a mean age of 56.4 years and a mean preoperative disease duration of 106.2 months. Thyroid cancer was demonstrated in 1026 patients (31.7 per cent), with PTC (including PTMC) being the most frequent type (917 patients, 28.4 per cent), accounting for 89.4 per cent of the 1026 cancers. PTC was identified in 345 patients (10.7 per cent), with PTMC in 572 (17.7 per cent) (Table 1). According to the eighth AJCC classification12, PTC was classified as T1, T2 and T3 in 598 (65.2 per cent), 199 (21.7 per cent) and 120 (13.1 per cent) of the 917 patients respectively (P = 0.231). All 21 patients with incidental medullary thyroid carcinoma subsequently underwent bilateral central compartment neck dissection; their RET proto-oncogene status was not examined for the purposes of this study. All patients with PTC, follicular thyroid cancer, or HCC of T2 status or higher, as well as patients with an aggressive thyroid cancer histological subtype irrespective of T status (492 patients), were administered radioactive iodine after surgery; this represented 48.0 per cent of the entire cancer cohort (492 of 1026).
Table 1.
Demographic, operative and histological data for the entire cohort
| No. of patients (n=3233) * | Benign MNG ‡ | Thyroid cancer § | P # | ||
|---|---|---|---|---|---|
| Age (years) † | 56.4(12.5) | 56.8(12.5) | 55.4(12.7) | 0.002** | |
| Sex | 0.030 | ||||
| F | 2788 (86.2) | 87.1 | 84.3 | ||
| M | 445 (13.8) | 12.9 | 15.7 | ||
| Smoking | 632 (19.5) | 19.6 | 19.4 | 0.881 | |
| Duration of disease (months) † | 106.2(116.7) | 114.2(121.3) | 90.5(105.4) | <0.001** | |
| Positive family history of thyroid cancer | 33 (1.0) | 1.0 | 1.0 | 0.859 | |
| History of head and neck irradiation ¶ | 9 (0.3) | 0.2 | 0.4 | 0.412 | |
| Substernal MNG | 124 (3.8) | 4.2 | 3.0 | 0.100 | |
| Functional thyroid status | <0.001 | ||||
| Hypothyroidism | 89 (2.8) | 2.4 | 3.6 | ||
| Euthyroidism | 2360 (73.0) | 70.0 | 79.3 | ||
| Hyperthyroidism | 784 (24.2) | 27.6 | 17.1 | ||
| Surgical operation | 0.432 | ||||
| Total or near-total thyroidectomy | 2843 (87.9) | 87.6 | 88.6 | ||
| Hemithyroidectomy | 390 (12.1) | 12.4 | 11.4 | ||
| MNG histological type | 0.010 | ||||
| Classical | 3033 (93.8) | 94.5 | 91.9 | ||
| Hyperplastic | 200 (6.2) | 5.5 | 8.1 | ||
| Hashimoto’s thyroiditis | 385 (11.9) | 9.2 | 17.8 | <0.001 | |
| Chronic non-specific thyroiditis | 284 (8.8) | 6.6 | 13.5 | <0.001 | |
| Histopathological diagnosis | 0.033 | ||||
| Follicular adenoma | 2525 (78.3) | 79.4 | 74.7 | ||
| Hyperplastic adenoma | 420 (13.0) | 12.5 | 14.1 | ||
| Hürthle adenoma | 181 (5.6) | 4.7 | 7.9 | ||
| Thyroid cyst | 65 (2.0) | 2.3 | 1.2 | ||
| C-cell hyperplasia | 42 (1.3) | 1.1 | 2.0 | ||
| Thyroid cancer | 1026 (31.7) | n.a. | |||
| Cancer histological type | n.a. | ||||
| Papillary cancer | 917 (28.4) | ||||
| Papillary microcarcinoma | 572 (17.7) | ||||
| Clinical papillary cancer | 345 (10.7) | ||||
| Follicular cancer | 17 (0.5) | ||||
| Hürthle cell cancer | 65 (2.0) | ||||
| Medullary cancer | 21 (0.6) | ||||
| Anaplastic cancer | 6 (0.2) | ||||
| TSH (munits/l) † | 1.30(1.50) | 1.19(1.54) | 1.51(1.38) | <0.001** | |
| Tg (ng/ml) † | 192.0(333.2) | 188.9(338.3) | 198.5(322.7) | 0.615** | |
| Anti-TPO (units/ml) † | 163.1(681.1) | 167.4(746.7) | 154.8(534.2) | 0.720** | |
| Anti-Tg (units/ml) † | 106.1(429.0) | 93.4(414.3) | 131.8(456.7) | 0.098** | |
| Largest adenoma (mm) † | 34.4(16.6) | 35.2(16.8) | 32.4(15.9) | 0.009** | |
| Second largest adenoma (mm) † | 25.2(12.4) | 25.4(13.0) | 24.4(10.3) | 0.663** | |
| Thyroid gland weight (g) † | 65.4(82.1) | 68.4(84.0) | 56.9(76.3) | 0.003** | |
*With percentages in parentheses unless indicated otherwise;
†values are mean(s.d.).
‡Percentage or mean(s.d.) value in patients without incidental thyroid cancer.
§Percentage or mean(s.d.) value in patients with incidental thyroid cancer.
¶Head and/or neck irradiation during childhood. MNG, multinodular goitre; n.a., not available; TSH, thyroid-stimulating hormone; Tg, thyroglobulin; TPO, thyroid peroxidase.
#χ2 test, except
**Bonferroni post hoc test for continuous variables.
Patients with thyroid cancer had a significantly higher mean(s.d.) preoperative TSH level than those with benign MNG (1.51(1.38 versus 1.19(1.54) munits/l respectively; P < 0.001), were more frequently men (161 (15.7 per cent) of 1026 versus 284 (12.9 per cent) of 2207; P = 0.030), were younger (mean(s.d.) 55.4(12.7) versus 56.8(12.5) years; P = 0.002), and had a shorter mean duration of disease (90.5(105.4) versus 114.2(121.3) months; P < 0.001) (Table 1). Some 2843 patients (87.9 per cent) underwent a total or near-total thyroidectomy, whereas the remaining 390 (12.1 per cent) had a hemithyroidectomy for asymmetrical MNG. A total of 124 patients (3.8 per cent) were operated on for a substernal MNG. HT was present more frequently in patients with thyroid cancer than in those with benign MBG (183 (17.8 per cent) of 1026 versus 202 (9.2 per cent) of 2207 respectively; P < 0.001), as was CNST (138 (13.5 per cent) of 1026 versus 146 (6.6 per cent) of 2207; P < 0.001). The mean size of the largest and second largest adenoma was 34.4 and 25.2 mm respectively. Smaller adenoma size (mean(s.d.) 32.4(15.9) mm versus 35.2(16.8) mm for benign MNG; P = 0.009) and smaller thyroid gland weight (mean(s.d.) 56.9(76.3) versus 68.4(84.0) g; P = 0.003) were correlated with an increased rate of incidental thyroid cancer (Table 1).
Mean follow-up for the entire cohort was 29 months; at last follow-up there were no detected recurrences or deaths.
Univariable analysis based on functional thyroid status
Patient age was significantly higher in group 3 than in group 2 (mean(s.d.) 57.8(12.3) versus 55.8(12.5) years respectively; P < 0.001), as was preoperative disease duration (132.3(131.9) versus 97.2(109.7) months; P < 0.001) Significantly higher serum anti-TPO (472.1(782.4), (160.2(700.3) and 127.4(590.1) units/ml in groups 1, 2 and 3 respectively) and anti-Tg (378.9(870.1), 104.3(437.7) and 69.9(254.4) units/ml) levels were observed in patients with hypothyroid MNG than in the other groups. HT was significantly more common in group 1 than in the other groups (36 (40 per cent) of 89 versus 310 (13.1 per cent) of 2360 in group 2 and 39 (5.0 per cent) of 784 in group 3; P < 0.001). Total thyroidectomy was performed more frequently in group 3 (711 of 784, 90.7 per cent) compared with group 2 (2056 of 2360, 87.1 per cent) and group 1 (76 of 89, 85 per cent) (P = 0.022). Moreover, adenoma size showed no correlation with functional thyroid status (Tables S1 and S2).
The incidence of thyroid cancer in groups 1, 2 and 3 was 42 per cent (37 of 89 patients), 34.5 per cent (814 of 2360) and 22.3 per cent (175 of 784) respectively (P < 0.001). The same pattern was also observed regarding the incidence of PTC in the three groups (32 (36 per cent), 717 (30.4 per cent) and 168 (21.4 per cent) patients respectively; P < 0.001). Rates of PTMC, although most common in group 1, showed no significant difference between the groups (18 (20 per cent), 437 (18.5 per cent) and 117 (14.9 per cent) patients respectively; P = 0.060). HCC (2 (2 per cent), 59 (2.5 per cent) and 4 (0.5 per cent) patients in groups 1, 2 and 3 respectively; P = 0.003) and medullary thyroid cancer (0 (0 per cent), 21 (0.9 per cent) and 0 (0 per cent) patients respectively; P = 0.020) were significantly more common in group 2, whereas anaplastic thyroid cancer was more common in group 1 (2 (2 per cent) versus 3 (0.1 per cent) in group 2 and 1 (0.1 per cent) in group 3; P < 0.001) (Tables S1 and S2).
Risk factors for incidental thyroid cancer
All histological types
Although MNG histological type, histopathological diagnosis and preoperative disease duration were identified as significant risk factors for thyroid cancer in univariable analysis (Table 1), they failed to reach statistical significance in multivariable regression analysis.
Increasing thyroid functional status was associated with a decreasing cancer rate (OR 0.68, 95 per cent c.i. 0.59 to 0.80; P < 0.001), with hyperthyroidism demonstrating the lowest risk of cancer (22.3 per cent), followed by euthyroidism (34.5 per cent); the highest risk was observed in hypothyroid patients (42 per cent). Older age was correlated significantly with a decreased cancer rate (OR 1.00, 0.99 to 1.00; P = 0.023), as was female sex (OR 0.73, 0.60 to 0.88; P = 0.001), with men demonstrating a 27.5 per cent increased risk of cancer. HT (OR 2.31, 1.85 to 2.89; P < 0.001) and CNST (OR 2.54, 1.97 to 3.26; P < 0.001) were also strongly associated with thyroid cancer. In addition, larger size adenomas were correlated with a decreased rate of cancer, compared with smaller adenomas (OR 0.99, 0.98 to 1.00; P = 0.012) (Table 2). The multivariable analysis for each group of patients is depicted in Table 3.
Table 2.
Multivariable logistic regression analysis of parameters significantly associated with all histological types of thyroid cancer, papillary thyroid cancers, papillary thyroid microcarcinoma and Hürthle cell thyroid cancer
| All thyroid cancers |
All papillary thyroid cancers* |
Papillary thyroid microcarcinoma |
Hürthle cell cancer |
|||||
|---|---|---|---|---|---|---|---|---|
| OR | P | OR | P | OR | P | OR | P | |
| Age | 1.00 (0.99, 1.00) | 0.023 | 0.99 (0.99, 0.99) | <0.001 | 0.99 (0.99, 1.00) | 0.036 | 1.03 (1.01, 1.06) | 0.005 |
| Sex | 0.73 (0.60, 0.88) | 0.001 | 0.72 (0.59, 0.88) | 0.001 | 0.410 | 0.245 | ||
| Functional thyroid status | 0.68 (0.59, 0.80) | <0.001 | 0.77 (0.66, 0.90) | 0.001 | 0.101 | 0.37 (0.21, 0.65) | 0.001 | |
| Largest adenoma | 0.99 (0.98, 1.00) | 0.012 | 0.388 | 0.302 | 0.506 | |||
| Hashimoto’s thyroiditis | 2.31 (1.85, 2.89) | <0.001 | 2.42 (1.93, 3.04) | <0.001 | 2.49 (1.92, 3.23) | <0.001 | 0.335 | |
| Chronic non-specific thyroiditis | 2.54 (1.97, 3.26) | <0.001 | 2.88 (2.24, 3.71) | <0.001 | 2.78 (2.07, 3.72) | <0.001 | 0.229 | |
Values in parentheses are 95 per cent confidence intervals. *Includes papillary microcarcinoma and clinical papillary cancer. OR. odds ratio.
Table 3.
Multivariable logistic regression analysis of regarding parameters significantly associated with all histological types of thyroid cancer, papillary thyroid cancers and papillary thyroid microcarcinoma in each of the three thyroid status groups
| All thyroid cancers |
All papillary thyroid cancers† |
Papillary thyroid microcarcinoma |
|||||||
|---|---|---|---|---|---|---|---|---|---|
|
P
*
|
P
*
|
P
*
|
|||||||
| Group 1 | Group 2 | Group 3 | Group 1 | Group 2 | Group 3 | Group 1 | Group 2 | Group 3 | |
| Age | 0.231 |
0.005
(0.99 (0.98, 1.00)) |
0.451 | 0.286 |
<0.001
(0.99 (0.98, 0.99)) |
0.443 | 0.308 | 0.376 | 0.398 |
| Sex | 0.342 |
0.001
(0.66 (0.51, 0.84)) |
0.390 | 0.305 |
0.004
(0.68 (0.53, 0.88)) |
0.501 | 0.225 | 0.289 | 0.402 |
| Hashimoto’s thyroiditis | 0.097 |
<0.001
(2.25 (1.76, 2.88)) |
0.008
(2.48 (1.27, 4.86)) |
0.119 |
<0.001
(2.41 (1.87, 3.10)) |
0.005
(2.62 (1.34, 5.14)) |
0.035
(3.59 (1.09, 11.81)) |
<0.001
(2.34 (1.74, 3.14)) |
0.017
(2.56 (1.18, 5.52)) |
| Chronic non-specific thyroiditis | 0.091 |
<0.001
(2.45 (1.85, 3.25)) |
0.002
(2.53 (1.42, 4.50)) |
0.145 |
<0.001
(2.89 (2.18, 3.85)) |
0.002
(2.47 (1.38, 4.43)) |
0.102 |
<0.001
(2.72 (1.95, 3.80)) |
0.001
(2.89 (1.53, 5.44)) |
*With odds ratio (95 per cent c.i.) in parentheses when P value was significant. †Includes papillary microcarcinoma and clinical papillary cancer.
Papillary thyroid cancer
As for all cancer histological types, increasing thyroid functional activity was associated with a decreasing cancer rate (OR 0.77, 95 per cent c.i. 0.66 to 0.90; P = 0.001), with hyperthyroidism demonstrating the lowest risk of cancer (21.4 per cent), followed by euthyroidism (30.4 per cent), with the highest risk observed in hypothyroid patients (36 per cent). Older age was significantly correlated with a decreased cancer rate (OR 0.99, 0.99 to 0.99; P < 0.001), as was female sex (OR 0.72, 0.59 to 0.88; P = 0.001). HT (OR 2.42, 1.93 to 3.04; P < 0.001) and CNST (OR 2.88, 2.24 to 3.71; P < 0.001) demonstrated significant associations with PTC, with a 2.4- and 2.9-fold increased risk of PTC development respectively (Table 2). The multivariable analysis for each group of patients is depicted in Table 3.
Papillary thyroid microcarcinoma
The occurrence of PTMC was independent of thyroid functional status (P = 0.101) and sex (P = 0.410). Older age was significantly associated with a decreased cancer rate (OR 0.99, 95 per cent c.i. 0.99 to 1.00; P = 0.036). HT (OR 2.49, 1.92 to 3.23; P < 0.001) and CNST (OR 2.78, 2.07 to 3.72; P < 0.001) were significant factors predisposing to PTMC development (Table 2). Multivariable analysis for each group of patients is depicted in Table 3.
Hürthle cell cancer
Increasing thyroid functional activity was associated with a decreasing HCC rate (OR 0.37, 95 per cent c.i. 0.21 to 0.65; P = 0.001). Unlike for other histological types, older age was a significant risk factor for HCC (OR 1.03, 1.01 to 1.06; P = 0.005) (Table 2).
Total or near-total thyroidectomy
Thyroid gland weight was inversely associated with cancer incidence, with larger thyroid glands demonstrating a decreased cancer rate compared with smaller glands (OR 1.00, 95 per cent c.i. 1.00 to 1.00; P = 0.007) (Table 4).
Table 4.
Multivariable logistic regression analysis of parameters significantly associated with all histological types of thyroid cancer, papillary thyroid cancers, papillary thyroid microcarcinoma and Hürthle cell thyroid cancer in 2843 patients who had total or near-total thyroidectomy
| All thyroid cancers |
All papillary thyroid cancers* |
Papillary thyroid microcarcinoma |
Hürthle cell cancer |
|||||
|---|---|---|---|---|---|---|---|---|
| OR | P | OR | P | OR | P | OR | P | |
| Age | 0.100 | 0.99 (0.99, 1.00) | 0.026 | 0.262 | 1.03 (1.01, 1.05) | 0.017 | ||
| Sex | 0.53 (0.42, 0.66) | < 0.0001 | 0.53 (0.41, 0.69) | <0.001 | 0.178 | 0.265 | ||
| Functional thyroid status | 0.66 (0.56, 0.78) | <0.001 | 0.75 (0.61, 0.91) | 0.004 | 0.151 | 0.38 (0.21, 0.68) | 0.001 | |
| Hashimoto’s thyroiditis | 2.16 (1.64, 2.86) | <0.001 | 2.32 (1.74, 3.10) | <0.001 | 1.93 (1.38, 2.69) | <0.001 | 0.374 | |
| Chronic non-Specific thyroiditis | 2.78 (2.00, 3.87) | <0.001 | 3.08 (2.21, 4.30) | <0.001 | 2.56 (1.76, 3.73) | <0.001 | 0.283 | |
| Thyroid gland weight | 1.00 (1.00, 1.00) | 0.007 | 1.00 (1.00, 1.00) | 0.026 | 0.402 | 0.655 | ||
Values in parentheses are 95 per cent confidence intervals. *Includes papillary microcarcinoma and clinical papillary cancer. OR. odds ratio.
Discussion
Although thyroid nodules within a MNG were traditionally regarded less likely to harbour thyroid cancer compared with solitary nodules, recent studies have questioned this belief. It has been reported13 that the probability of thyroid cancer does not depend on the number of thyroid nodules within a MNG, but that the likelihood of cancer within a nodule decreases as the total number of thyroid nodules increases. Although a recent meta-analysis14 suggested that patients with MNG were less likely to harbour thyroid cancer compared with those with a solitary thyroid nodule, subgroup analysis revealed an equal risk of incidental thyroid cancer in the two groups of patients. The present study indicated that nearly one-third of patients operated on for MNG have unsuspected thyroid cancer.
Ultrasound guidance in FNA of suspicious nodules within a MNG is used widely for the evaluation of thyroid nodules 1 cm or more in greatest diameter with sonographic features of intermediate or highsuspicion7. Several studies have shown that preoperative ultrasonography and FNA have an 84 per cent15 to 88 per cent9 negative predictive value for excluding thyroid cancer in patients who undergo thyroidectomy for MNG. However, a more recent study16 reported that FNA was able to detect only 46 per cent of the total thyroid cancers discovered at pathological evaluation of the surgical specimen, even though nearly half of the cancers missed by FNA were more than 1 cm in size.
The present study results are broadly in line with these findings. Some 31.7 per cent of patients with MNG and a benign preoperative FNA cytology result (Bethesda diagnostic category II10) were found to have an incidental thyroid cancer at pathological evaluation of the specimen. Approximately 44 per cent of these incidental cancers were either PTC of greater than 1cm in size or other more aggressive histological cancer types.
The observed rate of incidental cancer in the present study is higher than that in most series investigating similar subjects17–19. Considering that the incidence of PTC is increasing, for both PTMC and PTC greater than 1cm in size20–22, a plausible explanation of this increased rate may be that it reflects the global trend of increasing incidence of PTC. Studies17,23 have shown that variable rates of incidental thyroid cancer may reflect the standard of examination of the surgical specimen. This may be a factor in the present study related to the scrupulous dissection and evaluation of the surgical specimen by a pathologist experienced in thyroid malignancy.
Historically, hyperthyroidism has been regarded as a protective factor against the development of thyroid cancer24, with low cancer rates of 3–5 per cent18,25,26. Other studies27–29 have questioned these low cancer rates, demonstrating thyroid cancer rates of 12–21 per cent. In the present study, incidental thyroid cancer was discovered in 22.3 per cent of hyperthyroid patients with MNG, highlighting the assumption that the incidence of thyroid cancer in these patients was underestimated in the past28,29. Lower TSH levels may still act protectively against thyroid cancer development in hyperthyroid patients, considering the significantly higher cancer rates in euthyroid as well as hypothyroid patients in the present study.
HT is the most common cause of hypothyroidism in areas where dietary iodine intake is adequate30. Its association with PTC was first described in 195531, with recent studies indicating a causative relationship between HT and PTC development32. The present study confirmed a significant association between the development of HT and PTC within a MNG, with an observed OR of 2.42 for PTC development in the presence of HT. This finding was also identified by a recent systematic review33, which demonstrated an OR of 2.36 for PTC development in the presence of HT.
Various studies have identified patient age, sex and thyroid nodule size as independent risk factors for thyroid cancer development16,34. The present study indicated that younger age was an independent risk factor for all histological types of thyroid cancer, except for HCC, the incidence of which has been shown to increase with advancing age35–37. Regarding sex, the present study demonstrated that men were at greater risk of having an incidental PTC. Smaller thyroid nodule size was also found to be significantly associated with higher thyroid cancer rates.
The incidence of thyroid cancer within a substernal MNG has been a subject of debate for several years. It has been proposed38,39 that substernal MNGs may be at an increased risk of harbouring incidental thyroid cancer where FNA of suspicious nodules can be extremely difficult or impossible. The reported incidence of thyroid cancer in substernal goitres ranged from 3.4 per cent in earlier studies40 to 21 per cent in later reports41. Although 25.0 per cent of all substernal MNGs in the present study (31 of 124) were found to contain an incidental thyroid cancer, this rate was lower than the overall rate among all MNGs analysed. Considering these findings, it seems that substernal MNGs may not be at increased risk of harbouring thyroid malignancy, compared with their cervical counterparts.
Thyroid gland weight has been implicated as a potential risk factor for incidental thyroid cancer within a MNG2. The present study demonstrated a significantly increased incidental thyroid cancer rate in a MNG of smaller weight, especially regarding the likelihood of PTC. A plausible explanation may be that smaller MNGs facilitate more scrupulous preoperative evaluation by ultrasound imaging and FNA biopsy of suspicious nodule(s), compared with larger MNGs.
A natural limitation to this study is that it was based on patients operated on at a single centre. Despite the size of this patient series, it would be interesting to see whether similar results might exist in the context of an international multicentre study.
Disclosure: The authors declare no conflict of interest.
Supplementary material
Supplementary material is available at BJS Open online.
Supplementary Material
Contributor Information
K Apostolou, Centre for Endocrine Surgery, Clinical Centre of Serbia, Belgrade, Serbia.
V Zivaljevic, Centre for Endocrine Surgery, Clinical Centre of Serbia, Belgrade, Serbia; Faculty of Medicine, University of Belgrade, Belgrade, Serbia.
K Tausanovic, Centre for Endocrine Surgery, Clinical Centre of Serbia, Belgrade, Serbia; Faculty of Medicine, University of Belgrade, Belgrade, Serbia.
G Zoric, Centre for Endocrine Surgery, Clinical Centre of Serbia, Belgrade, Serbia.
G Chelidonis, National Actuarial Authority, Athens, Greece.
N Slijepcevic, Centre for Endocrine Surgery, Clinical Centre of Serbia, Belgrade, Serbia; Faculty of Medicine, University of Belgrade, Belgrade, Serbia.
M Jovanovic, Centre for Endocrine Surgery, Clinical Centre of Serbia, Belgrade, Serbia.
I Paunovic, Centre for Endocrine Surgery, Clinical Centre of Serbia, Belgrade, Serbia; Faculty of Medicine, University of Belgrade, Belgrade, Serbia.
References
- 1. Polyzos SA, Kita M, Avramidis A. Thyroid nodules—stepwise diagnosis and management. Hormones (Athens) 2007;6:101–119 [DOI] [PubMed] [Google Scholar]
- 2. Erbil Y, Barbaros U, Salmaslioglu A, Mete O, Issever H, Ozarmagan S et al. Effect of thyroid gland volume in preoperative detection of suspected malignant thyroid nodules in a multinodular goiter. Arch Surg 2008;143:558–563 [DOI] [PubMed] [Google Scholar]
- 3. Pelizzo MR, Merante Boschin I, Toniato A, Sorgato N, Marzola MC, Rubello D. Surgical therapeutic planning options in nodular goiter. Minerva Endocrinol 2010;35:173–185 [PubMed] [Google Scholar]
- 4. Marqusee E, Benson CB, Frates MC, Doubilet PM, Larsen PR, Cibas ES et al. Usefulness of ultrasonography in the management of nodular thyroid disease. Ann Intern Med 2000;133:696–700 [DOI] [PubMed] [Google Scholar]
- 5. Nixon IJ, Simo R. The neoplastic goitre. Curr Opin Otolaryngol Head Neck Surg 2013;21:143–149 [DOI] [PubMed] [Google Scholar]
- 6. Gandolfi PP, Frisina A, Raffa M, Renda F, Rocchetti O, Ruggeri C et al. The incidence of thyroid carcinoma in multinodular goiter: retrospective analysis. Acta Biomed 2004;75:114–117 [PubMed] [Google Scholar]
- 7. Haugen BR, Alexander EK, Bible KC, Doherty GM, Mandel SJ, Nikiforov YE et al. 2015 American Thyroid Association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: the American Thyroid Association guidelines task force on thyroid nodules and differentiated thyroid cancer. Thyroid 2016;26:1–133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Rago T, Fiore E, Scutari M, Santini F, Di Coscio G, Romani R et al. Male sex, single nodularity, and young age are associated with the risk of finding a papillary thyroid cancer on fine-needle aspiration cytology in a large series of patients with nodular thyroid disease. Eur J Endocrinol 2010;162:763–770 [DOI] [PubMed] [Google Scholar]
- 9. Rios A, Rodriguez JM, Galindo PJ,, Montoya M, Tebar FJ, Sola J et al. Utility of fine-needle aspiration for diagnosis of carcinoma associated with multinodular goitre. Clin Endocrinol (Oxf) 2004;61:732–737 [DOI] [PubMed] [Google Scholar]
- 10. Ali SZ, Cibas ES. The Bethesda system for reporting thyroid cytopathology II. Acta Cytol 2016;60:397–398 [DOI] [PubMed] [Google Scholar]
- 11. Costa A, Torchio B, Zoppetti G, Feyless E. What is meant today by Hashimoto’s thyroiditis? J Endocrinol Invest 1989;12:355–356 [DOI] [PubMed] [Google Scholar]
- 12. American Joint Committee on Cancer. AJCC Cancer Staging Manual (8th edn). New York: Springer International Publishing, 2018 [Google Scholar]
- 13. Frates MC,, Benson CB, Doubilet PM, Kunreuther E, Contreras M,, Cibas ES et al. Prevalence and distribution of carcinoma in patients with solitary and multiple thyroid nodules on sonography. J Clin Endocrinol Metab 2006;91:3411–3417 [DOI] [PubMed] [Google Scholar]
- 14. Brito JP, Yarur AJ,, Prokop LJ, McIver B, Murad MH, Montori VM. Prevalence of thyroid cancer in multinodular goiter versus single nodule: a systematic review and meta-analysis. Thyroid 2013;23:449–455 [DOI] [PubMed] [Google Scholar]
- 15. Al-Yaarubi S, Farhan H, Al-Futaisi A, Al-Qassabi S, Al-Rasadi K, Al-Riyami S et al. Accuracy of ultrasound-guided fine-needle aspiration cytology for diagnosis of carcinoma in patients with multinodular goiter. Indian J Endocrinol Metab 2011;15(Suppl 2):S132–S135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Luo J, McManus C, Chen H, Sippel RS. Are there predictors of malignancy in patients with multinodular goiter? J Surg Res 2012;174:207–210 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Bradly DP, Reddy V, Prinz RA, Gattuso P. Incidental papillary carcinoma in patients treated surgically for benign thyroid diseases. Surgery 2009;146:1099–1104 [DOI] [PubMed] [Google Scholar]
- 18. Cerci C, Cerci SS, Eroglu E, Dede M, Kapucuoglu N, Yildiz M et al. Thyroid cancer in toxic and non-toxic multinodular goiter. J Postgrad Med 2007;53:157–160 [DOI] [PubMed] [Google Scholar]
- 19. Ito Y, Higashiyama T, Takamura Y, Miya A, Kobayashi K, Matsuzuka F et al. Prognosis of patients with benign thyroid diseases accompanied by incidental papillary carcinoma undetectable on preoperative imaging tests. World J Surg 2007;31:1672–1676 [DOI] [PubMed] [Google Scholar]
- 20. Enewold L, Zhu K, Ron E, Marrogi AJ, Stojadinovic A, Peoples GE et al. Rising thyroid cancer incidence in the United States by demographic and tumor characteristics, 1980–2005. Cancer Epidemiol Biomarkers Prev 2009;18:784–791 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Davies L, Welch HG. Increasing incidence of thyroid cancer in the United States, 1973–2002. JAMA 2006;295:2164–2167 [DOI] [PubMed] [Google Scholar]
- 22. Verkooijen HM, Fioretta G, Pache JC, Franceschi S, Raymond L, Schubert H et al. Diagnostic changes as a reason for the increase in papillary thyroid cancer incidence in Geneva, Switzerland. Cancer Causes Control 2003;14:13–17 [DOI] [PubMed] [Google Scholar]
- 23. Bisi H, Fernandes VS, de Camargo RY, Koch L, Abdo AH, de Brito T. The prevalence of unsuspected thyroid pathology in 300 sequential autopsies, with special reference to the incidental carcinoma. Cancer 1989;64:1888–1893 [DOI] [PubMed] [Google Scholar]
- 24. Sokal JE. Incidence of malignancy in toxic and nontoxic nodular goiter. J Am Med Assoc 1954;154:1321–1325 [DOI] [PubMed] [Google Scholar]
- 25. Kang AS, Grant CS, Thompson GB, van Heerden JA. Current treatment of nodular goiter with hyperthyroidism (Plummer’s disease): surgery versus radioiodine. Surgery 2002;132:916–923 [DOI] [PubMed] [Google Scholar]
- 26. Gelmini R, Franzoni C, Pavesi E, Cabry F, Saviano M. Incidental thyroid carcinoma (ITC): a retrospective study in a series of 737 patients treated for benign disease. Ann Ital Chir 2010;81:421–427 [PubMed] [Google Scholar]
- 27. Calo PG, Tatti A, Farris S, Malloci A, Nicolosi A. [Differentiated thyroid carcinoma and hyperthyroidism: a frequent association?] Chir Ital 2005;57:193–197 [PubMed] [Google Scholar]
- 28. Senyurek Giles Y, Tunca F, Boztepe H, Kapran Y, Terzioglu T, Tezelman S. The risk factors for malignancy in surgically treated patients for Graves’ disease, toxic multinodular goiter, and toxic adenoma. Surgery 2008;144:1028–1036 [DOI] [PubMed] [Google Scholar]
- 29. Smith JJ, Chen X, Schneider DF, Nookala R, Broome JT, Sippel RS et al. Toxic nodular goiter and cancer: a compelling case for thyroidectomy. Ann Surg Oncol 2013;20:1336–1340 [DOI] [PubMed] [Google Scholar]
- 30. Campos LA, Picado SM, Guimaraes AV, Ribeiro DA, Dedivitis RA. Thyroid papillary carcinoma associated to Hashimoto’s thyroiditis. Braz J Otorhinolaryngol 2012;78:77–80 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Dailey ME, Lindsay S, Skahen R. Relation of thyroid neoplasms to Hashimoto disease of the thyroid gland. AMA Arch Surg 1955;70:291–297 [DOI] [PubMed] [Google Scholar]
- 32. Uhliarova B, Hajtman A. Hashimoto’s thyroiditis—an independent risk factor for papillary carcinoma. Braz J Otorhinolaryngol 2018;84:729–735 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Resende de Paiva C, Gronhoj C, Feldt-Rasmussen U, von Buchwald C. Association between Hashimoto’s thyroiditis and thyroid cancer in 64 628 patients. Front Oncol 2017;7:53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Campbell MJ, Seib CD, Candell L, Gosnell JE, Duh QY, Clark OH et al. The underestimated risk of cancer in patients with multinodular goiters after a benign fine needle aspiration. World J Surg 2015;39:695–700 [DOI] [PubMed] [Google Scholar]
- 35. Carcangiu ML, Bianchi S, Savino D, Voynick IM, Rosai J. Follicular Hurthle cell tumors of the thyroid gland. Cancer 1991;68:1944–1953 [DOI] [PubMed] [Google Scholar]
- 36. Zhang YW, Greenblatt DY, Repplinger D, Bargren A, Adler JT, Sippel RS et al. Older age and larger tumor size predict malignancy in Hurthle cell neoplasms of the thyroid. Ann Surg Oncol 2008;15:2842–2846 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Goffredo P, Roman SA, Sosa JA. Hurthle cell carcinoma: a population-level analysis of 3311 patients. Cancer 2013;119:504–511 [DOI] [PubMed] [Google Scholar]
- 38. Netterville JL, Coleman SC, Smith JC, Smith MM, Day TA, Burkey BB. Management of substernal goiter. Laryngoscope 1998;108:1611–1617 [DOI] [PubMed] [Google Scholar]
- 39. Nervi M, Iacconi P, Spinelli C, Janni A, Miccoli P. Thyroid carcinoma in intrathoracic goiter. Langenbecks Arch Surg 1998;383:337–339 [DOI] [PubMed] [Google Scholar]
- 40. Lamke LO, Bergdahl L, Lamke B. Intrathoracic goitre: a review of 29 cases. Acta Chir Scand 1979;145:83–86 [PubMed] [Google Scholar]
- 41. Sanders LE, Rossi RL, Shahian DM, Williamson WA. Mediastinal goiters. The need for an aggressive approach. Arch Surg 1992;127:609–613 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.