Highlights
-
•
Coronavirus Disease 2019 (COVID-19) affects almost all organ systems with very diverse clinical manifestations.
-
•
We present a very unique case of a patient presenting with vague abdominal pain from COVID-19 associated complication of Aortitis.
-
•
Our case of Aortitis in COVID-19 is the first of its kind in terms of COVID-19 presentation in the United States reported so far.
-
•
Aortitis can be life threatening and the diagnosis in the setting of COVID-19 presentation can be challenging.
-
•
Aortitis in COVID-19 is shown to respond to steroids with favorable outcomes if treated early.
Keywords: COVID-19, Aortitis, Large vessel vasculitis
Abstract
Corona Virus Disease of 2019 (COVID-19) pandemic has affected more than 67.9 million individuals world-wide and led to more than 15.5 million Deaths. In the initial studies from China, 88.7 % of the patient were noted to have fever, 67 % of the patient had cough and 56.4 % had ground glass changes on the chest imaging. With time, the presentation of patients has been found to be highly variable and unpredictable.
COVID-19 is reported to present with various complications, ranging from gastrointestinal (GI) manifestations, such as loss of sensation of taste, abdominal pain, diarrhea, vomiting, pancreatitis and hepatobiliary disease, to neurological manifestations of encephalitis and stroke, and cardiovascular manifestations like myocarditis, heart failure and arrythmia. We report a rare case of COVID-19 presenting with abdominal pain from aortitis.
Background
Corona Virus Disease of 2019 (COVID-19) pandemic has affected more than 67.9 million individuals world-wide and led to more than 15.5 million deaths [1]. In the initial studies from China, 88.7 % of the patient were noted to have fever, 67 % of the patient had cough and 56.4 % had ground glass changes on the chest imaging [2]. With time, the presentation of patients has been found to be highly variable and unpredictable. COVID-19 is reported to present with various complications, ranging from gastrointestinal(GI) manifestations, such as loss of sensation of taste, abdominal pain, diarrhea, vomiting, pancreatitis and hepatobiliary disease, to neurological manifestations of encephalitis and stroke, and cardiovascular manifestations like myocarditis, heart failure and arrythmia [[3], [4], [5]]. COVID –19 infection being a generalized inflammatory state, inflammation of aorta leading to aortitis is theoretically possible. Literature review revealed that only one case of COVID-19 associated aortitis has been reported so far, which was in Europe. To the best of our knowledge, our patient is the first reported case of COVID-19 associated aortitis in the United States.
Case presentation
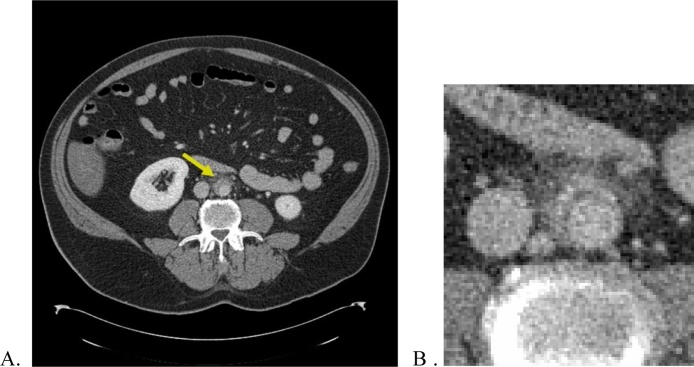
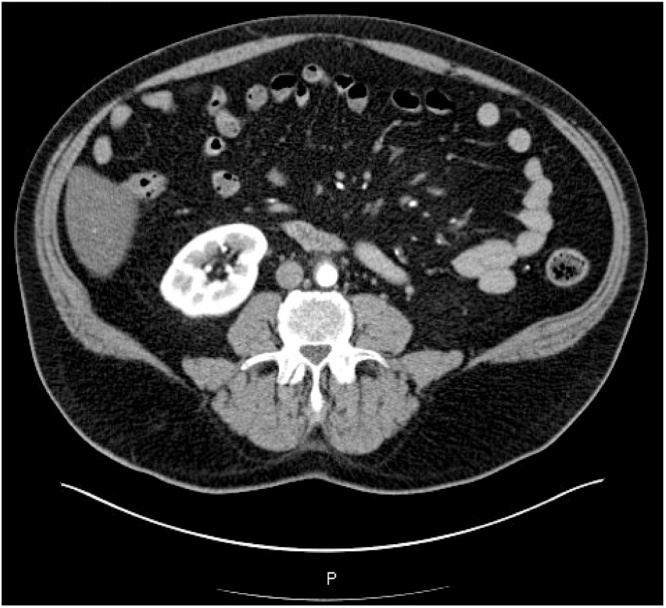
A 63-year-old male with past medical history of Parkinson disease, Asthma, Diabetes mellitus type 2, Hypertension, Obesity and Non-ischemic cardiomyopathy presented to the hospital with diffuse abdominal pain, dry cough, fatigue and generalized weakness for two days duration, not associated with shortness of breath, hypoxia, body rash, jaw claudication, joint pain. Patients was afebrile, hemodynamically stable and had O2 saturation of 98 % on room air. Physical examination was remarkable only for abdominal discomfort in peri-umbilical area upon palpation. Labs showed normal white blood cell count, liver function profile and renal function profile, as well as normal lipase and amylase levels. Computed tomography (CT) of abdomen/pelvis with intravenous contrast revealed patchy ground-glass opacities in the visualized portion of the lung and inflammatory changes involving a segment of the infra-renal aorta with small focal acute dissection (Fig. 1). Given the lung findings on CT abdomen, nasopharyngeal swab for SARS-COV-2 RNA was performed, which came back as positive. Subsequently, inflammatory markers were found to be elevated, with ESR at 57 mm/hr, CRP at 8.7 mg/dl and Interleukin-6 at 54.44 pg/mL. Immunologic work up including rheumatoid factor, cyclic citrullinated peptide antibody, antinuclear antibodyand anti-neutrophil cytoplasmic antibody were negative. IgG4 Immunoglobulin level was elevated at 187 mg/dl. Infectious vasculitis workup with syphilis serology, HIV antibodies, Hepatitis B, Hepatitis C, Q fever antibodies were all negative. Vascular Surgery team was consulted given concern for acute dissection on the imaging, who deemed it to be too small for any surgical intervention. Rheumatology team was consulted, who deemed the aortitis to be secondary to COVID-19 infection. Patient was started on oral prednisone 60 mg daily with gradual complete resolution of abdominal symptoms by day 9. Inflammatory markers were monitored which trended down gradually. Patient was discharged home with a gradual taper of prednisone over 1-month duration. Follow up imaging with CT abdomen/pelvis after completion of steroid therapy showed complete resolution of aortitis. (Fig. 2).
Fig. 1.
A: Aortic wall thickening, surrounding inflammation and possible dissection (yellow arrow). B: Magnified image of the aorta.
Fig. 2.
Follow up imaging post treatment showing resolution of aortic wall thickening and surrounding inflammation.
Discussion
Inflammation of aorta, termed as aortitis, can be due to infectious or non-infectious causes. Giant Cell Arteritis (GCA) and Takayasu Arteritis (TA) are the commonest cause of non-infectious aortitis. Infection with Treponema pallidum used to be commonest cause of infectious aortitis, which is recently surpassed by infection with gram positive (Staphylococcus aureus, enterococcus, Streptococcus pneumoniae) and gram negative organisms (Salmonella spp). Mycobacterial, Rickettsial (Q-fever) and fungal infection causing aortitis is rare but possible [6,7].
Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) gets access into the endothelial cells through angiotensin converting enzyme-2 receptor [8]. It then drives both T helper cells activating cell mediated immunity and humoral immunity ultimately causing endotheliitis and leukocytoclastic vasculitis in addition to type-3 hypersensitivity reaction leading to aortitis [[9], [10], [11]]. Depending on the site and extent of involvement, aortitis can manifest as non-specific symptoms like simple abdominal pain, fever and malaise to severe complications, such as claudication, neurological deficit and even life-threatening aortic aneurysm and dissection. Although no biomarker is diagnostic, acute phase reactants like ESR and CRP tends to be elevated [6]. In addition, increased Interleukin-6 level further supports the possibility of COVID-19 related aortitis. IgG4 in our patient was elevated to 187 mg/dl. In the absence of multi organ involvement mere elevation of IgG4 level is neither very sensitive nor specific for IgG4 related vasculopathy [12]. The rise in IgG4 level could be in the setting of COVID-19 infection.
Echocardiography, Ultrasonography, CT scan, Magnetic Resonance Imaging and Positron Emission Tomography scan are the imaging modalities routinely used to diagnose aortitis, which look at mural thickening, calcifications and other inflammatory changes [7]. If infectious causes are ruled out, inflammatory aortitis can be treated with steroids and immune modulators. Response to the treatment can be monitored with clinical response, down-trending of inflammatory markers and improvement in radiological findings [13].
COVID-19 associated inflammatory aortitis is unique. The first reported case of COVID-19 associated aortitis was in a 71-year-old male, who presented with symptoms of chest pain 2 months after resolution of a suspected COVID-19 infection, diagnosed later by the presence of IgG antibodies to COVID-19 on serology testing. Diffuse inflammation from subclavian artery to iliac artery was reported on CT scan of thorax, abdomen and pelvis.. They reported improvement in the clinical symptoms and radiological findings with steroids [14]. In contrast, our patient had aortitis in setting of acute COVID-19 infection with positive COVID-19 PCR at the time of presentation. Inflammatory changes in the infrarenal aorta responded to treatment with steroids, which was evident from clinical improvement and resolution of aortitis findings on repeat CT scan of abdomen and pelvis.
Our case of aortitis along with the other reported case in Europe is a rare manifestation of COVID-19 infection. Presentation can be related to COVID-19 symptoms or typical aortitis symptoms. Ruling out common infectious and non-infectious causes of vasculitis is necessary before establishing the diagnosis. Aortitis in COVID-19 do seem to respond to prednisone like other inflammatory aortitis, which is further supported by response to the recommended corticosteroid dosage for non-infectious aortitis with prednisone 40 mg–60 mg daily for four weeks, followed by gradual taper [15]. Given the short follow up period, long standing complications if any is unknown at this time.
Thus, we would like to emphasize the importance of maintaining vigilance and high level of clinical suspicion for the possibility of rare but life threatening complication of aortitis in patients with COVID-19, as early recognition and treatment can lead to favorable outcomes.
Conflicts of interest
None.
Funding
None.
Consent
Ethical approval: Not required.
Consent: Written consent is obtained from the patient and is available on request.
Author contribution
Dr. Pravash Dhakal: Writing, literature review.
Dr. Sushmita Khadka: Writing, literature review.
Dr. Jackie A. Clowes: Manuscript revision and proof reading.
Dr. Raja Chandra Chakinala: Study design, provided images, manuscript revision and proof.
Contributor Information
Pravash Dhakal, Email: Pravash.kd@gmail.com.
Sushmita Khadka, Email: Sushmita.khadka@guthrie.org.
Jackie A. Clowes, Email: Jackie.clowes@guthrie.org.
Raja Chandra Chakinala, Email: rajachandra@gmail.com.
References
- 1.COVID-19 situation update worldwide, as of 9 December 2020. https://www.ecdc.europa.eu/en/geographical-distribution-2019-ncov-cases. [Accessed 12 September 2020].
- 2.Guan W., Ni Z., Hu Y. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382(18):1708–1720. doi: 10.1056/nejmoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Patel K.P., Patel P.A., Vunnam R.R. Gastrointestinal, hepatobiliary, and pancreatic manifestations of COVID-19. J Clin Virol. 2020;128 doi: 10.1016/j.jcv.2020.104386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gavriatopoulou M., Korompoki E., Fotiou D. Organ-specific manifestations of COVID-19 infection. Clin Exp Med. 2020;20(4):493–506. doi: 10.1007/s10238-020-00648-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shafi A.M.A., Shaikh S.A., Shirke M.M., Iddawela S., Harky A. Cardiac manifestations in COVID-19 patients—a systematic review. J Card Surg. 2020;35(8):1988–2008. doi: 10.1111/jocs.14808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Benhuri B., ELJack A., Kahaleh B., Chakravarti R. Mechanism and biomarkers in aortitis––a review. J Mol Med. 2020;98(1):11–23. doi: 10.1007/s00109-019-01838-1. [DOI] [PubMed] [Google Scholar]
- 7.Bossone E., Pluchinotta F.R., Andreas M. Aortitis. Vascul Pharmacol. 2016;80:1–10. doi: 10.1016/j.vph.2015.11.084. [DOI] [PubMed] [Google Scholar]
- 8.Roncati L., Gallo G., Manenti A., Palmieri B. Renin-angiotensin system: the unexpected flaw inside the human immune system revealed by SARS-CoV-2. Med Hypotheses. 2020;140 doi: 10.1016/j.mehy.2020.109686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Roncati L., Ligabue G., Fabbiani L. Type 3 hypersensitivity in COVID-19 vasculitis. Clin Immunol. 2020;217 doi: 10.1016/j.clim.2020.108487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Manenti A., Farinetti A., Manco G., Mattioli A. Vasculitis and aortitis: COVID-19 challenging complications. J Vasc Surg. 2020;(September) doi: 10.1016/j.jvs.2020.08.029. S0741-5214(20)31913-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jung F., Krüger-Genge A., Franke R.P., Hufert F., Küpper J.H. COVID-19 and the endothelium. Clin Hemorheol Microcirc. 2020;75(1):107–119. doi: 10.3233/CH-209007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kamisawa T., Zen Y., Pillai S., Stone J.H. IgG4-related disease. Lancet. 2015;385(9976):1460–1471. doi: 10.1016/S0140-6736(14)60720-0. [DOI] [PubMed] [Google Scholar]
- 13.Deipolyi A.R., Czaplicki C.D., Oklu R. Inflammatory and infectious aortic diseases. Cardiovasc Diagn Ther. 2018;8(Suppl. 1):S61–S70. doi: 10.21037/cdt.2017.09.03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shergill S., Davies J., Bloomfield J. Florid aortitis following SARS-CoV-2 infection. Eur Heart J. 2020;(August) doi: 10.1093/eurheartj/ehaa635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mukhtyar C., Guillevin L., Cid M.C. EULAR recommendations for the management of large vessel vasculitis. Ann Rheum Dis. 2009;68(3):318–323. doi: 10.1136/ard.2008.088351. [DOI] [PubMed] [Google Scholar]