Abstract
The knowledge and perceptions of cervical cancer among HIV negative and positive women, aged 25–49 years, from rural and urban locations in Zambia was systematically accessed in this study to determine any differences. Data were coded and analyzed using NVivo software. Compared to HIV negative women, HIV positive women had more accurate information about cervical cancer. They were more likely to cite male circumcision as the best approach to cervical cancer prevention. HPV infection was more commonly mentioned as a risk factor among HIV positive women. However, HIV positive women displayed little knowledge about HPV being the major cause of cervical cancer. Among HIV positive women, lack of time was the major screening barrier cited while HIV negative women mentioned being symptomatic as a determinant for early detection. Compared to rural residents, urban residents cited a wider range of cervical cancer information sources, including media and workplace although all of the participants who stated that they had no knowledge of cervical cancer were urban residents. Overall, knowledge and perceptions of cervical cancer among study participants was high, although differences exist between subgroups. Sharing accurate and standardized information on cervical cancer would improve participation in cervical cancer screening services.
Keywords: Cervical cancer, screening, HIV status, cervical cancer knowledge and perception, rural and urban location, Zambia
Résumé
Les connaissances et les perceptions du cancer du col utérin chez les femmes séropositives et les personnes séropositives, âgées de 25 à 49 ans originaires des milieux ruraux et urbains en Zambie, ont été systématiquement utilisées dans cette étude pour déterminer les différences. Les données ont été codées et analysées à l’aide du logiciel NVivo. Comparativement aux femmes séronégatives, les femmes séropositives avaient des informations plus précises sur le cancer du col utérin. Elles étaient plus susceptibles de citer la circoncision masculine comme la meilleure approche pour la prévention du cancer du col utérin. L’infection à VPH a été plus souvent mentionnée comme facteur de risque chez les femmes séropositives. Cependant, les femmes séropositives ont démontré peu de connaissances sur le fait que le VPH était la principale cause du cancer du col utérin. Chez les femmes séropositives, le principal obstacle au dépistage a été le manque de temps, tandis que les femmes séronégatives ont indiqué qu’elles étaient symptomatiques en tant que facteur déterminant du dépistage précoce. Comparés aux résidentes rurales, les citadines citent une gamme plus large de sources d’informations sur le cancer du col utérin, y compris les médias et le lieu de travail, alors que toutes les participantes qui ont déclaré qu’elles n’ont pas de connaissances à l’égard du cancer du col utérin étaient des résidentes urbaines. Dans l’ensemble, les connaissances et les perceptions du cancer du col utérin chez les participantes à l’étude étaient élevées, bien qu’il existe des différences entre les sous-groupes. Le partage d’informations précises et normalisées sur le cancer du col utérin améliorerait la participation aux services de dépistage du cancer du col utérin.
Mots-clés: Cancer du col utérin, dépistages, état du VIH, connaissance et perception du cancer du col utérin, milieu rural et urbain, Zambie
Introduction
Globally, an estimated 500,000 new cases of cervical cancer occur each year. Approximately 20% of those new cases occur in sub-Saharan Africa alone1. In 2015, an estimated 270,000 deaths from cervical cancer were reported across the globe, with 90% occurring in developing countries2. Zambia has one of the world’s highest cervical cancer incidence rates. The International Agency for Research on Cancer (IARC) estimates incidence rate in Zambia at 58.0 per 100,000 and mortality at 36.2 per 100,0003, with the disease mostly affecting women aged 15 to 44 years4.
In Zambia, the high incidence rate of cervical cancer has been attributed to the high prevalence of Human Papilloma Virus (HPV) types 16 and 18 (21.6% each), and the high national adult HIV prevalence of 16%5 with majority of those being women (15.1%)6. HIV infection has been associated with a higher incidence of precancerous cervical lesions and accelerated progression of these lesions to cervical cancer7 owing to immunosuppression8. Approximately 60% of all cervical cancer cases in sub-Saharan Africa are diagnosed in women living with HIV. A recent study conducted in Zambia among 309 HIV positive women, previously unscreened for cervical cancer, revealed that >50% of the study participants had evidence of precancer7.
Increasing awareness and knowledge among women and their communities is essential for changing attitudes and practices towards cervical cancer screening9. A study conducted in Kenya among HIV positive women demonstrated that high knowledge levels of the disease were associated with increased cervical cancer screening uptake10. This is in close agreement with an assessment conducted among female university students in Ethiopia which found that poor knowledge resulted in low screening uptake11.
This study was conducted to systematically assess knowledge levels and perceptions of cervical cancer among women in Zambia, stratified by HIV status and location of residence. These two key stratification factors were identified based on feedback received from key stakeholders in Zambia including cancer patients, providers, implementers, traditional healers and health ministry staff. The findings from this study will provide valuable information to tailor community-based interventions and enhance cervical cancer screening uptake.
Methods
Conceptual model
Figure 1 illustrates the conceptual pathways that lead to improvement in health outcomes through cervical cancer screening. The framework was used to identify the key target subgroups as well as the questions included in the interview guide. We began with social determinants of health which can impact mediating factors that are required for behavior change to take place. Mediating factors include knowledge and self-efficacy, family support and overall improvement in care seeking behavior. Interventions can be designed to influence these mediating factors and increase cancer screening. Moderating factors, such as rural versus urban residence and HIV status, can influence social determinants and mediating factors and thus also impact cervical cancer screening uptake.
Figure 1:
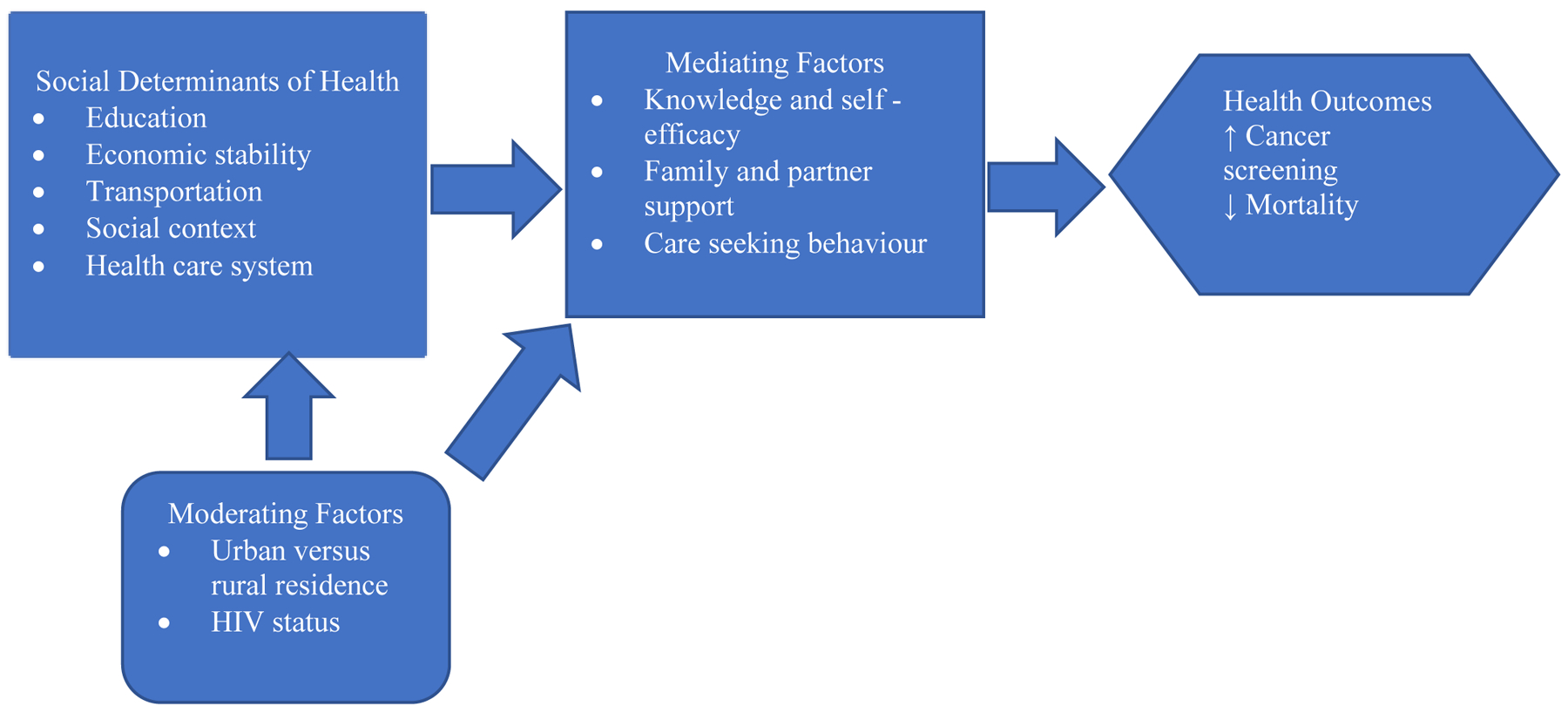
Conceptual model of factors influencing cervical cancer screening
Study design
A qualitative study using in-depth interviews (IDI) with men, HIV positive women and HIV negative women aged between 25 and 49 years was conducted. All respondents were recruited through the health facility and conveniently sampled from the patients who came to access health services. The urban and rural cohorts were recruited from Lusaka and Chongwe districts, respectively. The goal was to recruit 40 women and 20 men with equal distribution between urban and rural areas. A total of 59 interviews was completed.
Data collection procedure
The IDIs were conducted between July 2017 and September 2017. Written consent was obtained from all the respondents. A structured questionnaire was used to conduct the interviews, which were carried out in the participant’s language of choice. The themes explored included knowledge and perceptions of women in relation to prevention and risk factors of cervical cancer and sources of information. The IDIs were conducted by the study coordinator in a private space and lasted 40 minutes. All IDIs were audio recorded and a research assistant took detailed notes of the conversation. To ensure confidentiality, the recordings were encrypted, and no identifiable information was collected from the interviewees.
Data analysis
All audio-recorded IDIs were simultaneously translated and transcribed from local languages into English. To ensure the accuracy and completeness of the translations and transcriptions, two research team members crosschecked each transcript against the audio-recordings and notes. Deductive and inductive qualitative content analyses were used to develop codes. The study coordinator read the transcripts to obtain an overall understanding of the data. Based on these readings, a codebook was developed and shared with the research team. The team agreed on the common themes used for the coding of all the transcripts. The coding of the transcripts was independently confirmed by two team members and the key themes that emerged were discussed with the study team to reach consensus. Using NVivo software, data was queried to establish differences in coded references between rural and urban respondents and between HIV negative and positive individuals to identify similarities and differences. Specific quotes from the interviewees in support of each of the key themes identified were reviewed.
Results
Socio-demographic characteristics of participants
Of the 59 participants, 40 were women and 19 were men. Nineteen of the women were HIV positive; 10 from Lusaka and 9 from Chongwe. Nineteen women were HIV negative; 8 from Lusaka and 11 from Chongwe. Two women from Lusaka were of unknown HIV status. Twenty –one of the women had been previously screened for cervical cancer (Table 1).
Table 1:
Characteristics of study participants in Lusaka and Chongwe, Zambia
| Characteristics | Female (n=40) | Male (n=19) |
|---|---|---|
| Lusaka | 20 (50%) | 10 (53%) |
| Chongwe | 20 (50%) | 9 (47%) |
| Age | ||
| 25 – 34 | 22 (55%) | 9 (47%) |
| 35 – 44 | 11(27.5%) | 7 (37%) |
| 45 – 49 | 7 (17.5%) | 3 (16%) |
| HIV Status | ||
| HIV Positive | 19 (47.5%) | N/A |
| HIV Negative | 19 (47.5%) | N/A |
| Cervical cancer screening status | ||
| Screened | 21 (52.5%) | N/A |
| Unscreened | 19 (47.5%) | N/A |
Importance of early detection of precancerous lesions was high among the participants
Most of the interviewees mentioned early detection and treatment as a preventive measure (Figure 2). Although, the interviewees did not make a clear distinction between precancerous lesions and cervical cancer, the majority indicated that cervical cancer can be prevented by seeking care early.
“When you go to the clinic earlier and they find the cancer. If they find the cancer, they can do something to prevent it from multiplying”.
(Lusaka, female, 33 years, HIV negative)
“Cervical cancer can be prevented if you go to the clinic early enough before the disease stays long in the body”.
(Chongwe, female, 40 years, HIV positive)
Figure 2:
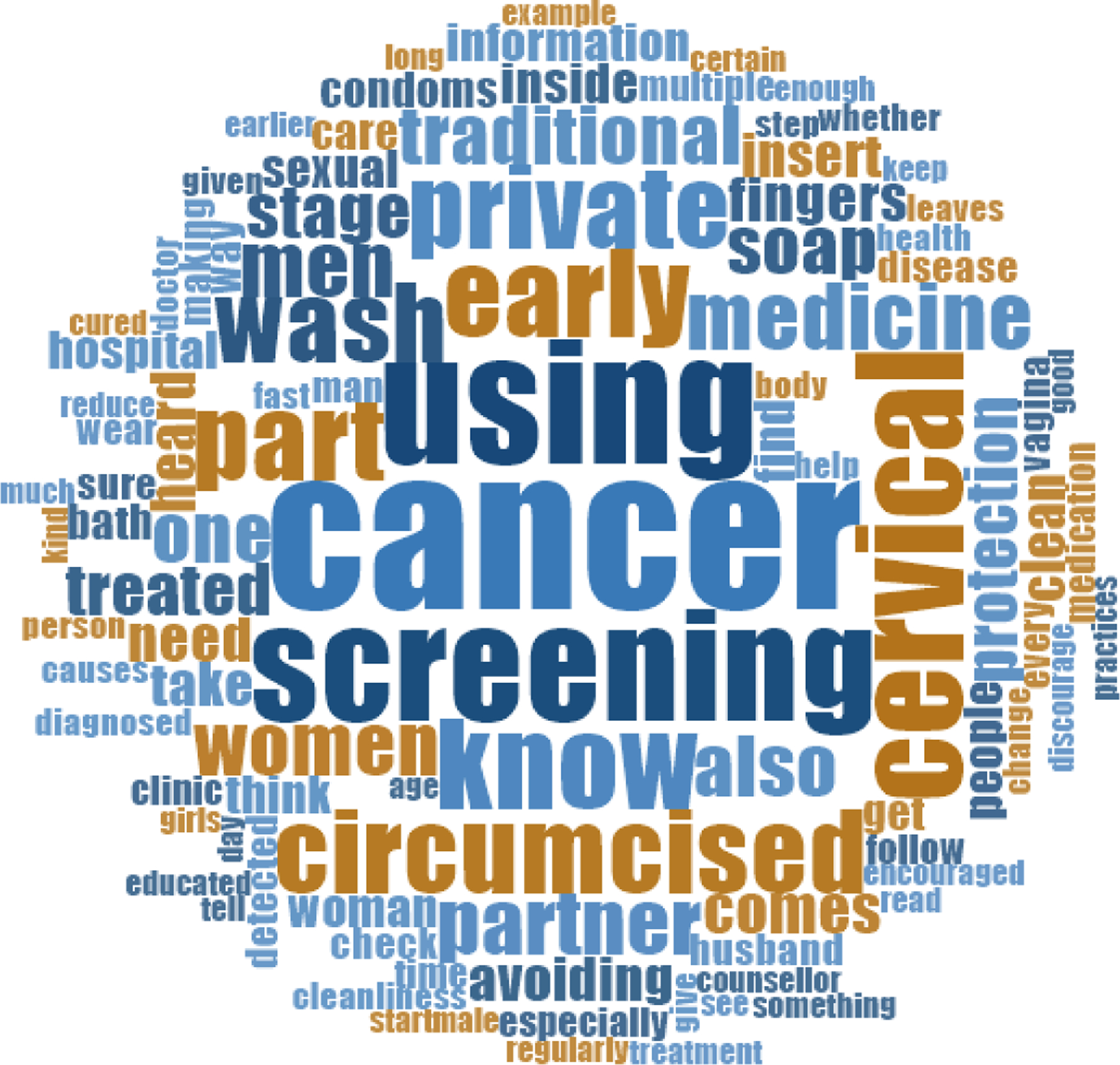
Word cloud showing how frequent early cervical cancer screening was mentioned
Knowledge about risk factors and approaches to prevent cervical cancer varied across subgroups of women
The most common causes of cervical cancer mentioned included not being circumcised, harmful traditional practices such as insertion of herbs in the vagina, HIV infection and multiple partners. There were several differences between subgroups in the knowledge about both risk factors and preventive approaches.
Circumcision was the most common preventive approach mentioned by HIV positive women
Most women who were HIV positive and generally those from the rural district mentioned circumcision as an important approach to reduce the risk of cervical cancer.
“Cancer is when a woman has a partner who is not circumcised. So, the men have dirt. When a woman gets that dirt, it can cause cervical cancer.”
(Chongwe, female, 34 years, HIV positive)
Women from Chongwe were more likely to mention hygiene and avoidance of traditional practices
Those from the rural district often mentioned traditional practices such as insertion of herbs, usage of snuff to tighten the orifice of the vagina and cleaning the inside of the vagina with soap as risk factors for cervical cancer.
“When you are bathing, and you have dirt in the nails and you clean the inside and that can affect the uterus. Don’t use washing soap to clean the private part and don’t insert fingers in the private part to clean the inside.”
(Chongwe, female, 42 years, HIV negative)
HIV positive women were more likely to mention HPV infection as a risk factor
A minority of women most of whom were HIV positive indicated they knew that persistent HPV infection can lead to cervical cancer and even among those who indicated that they had heard about HPV infection, the knowledge about the underlying processes was not always accurate.
“I have heard about it. Maybe it can also cause since it’s something which goes in the fallopian tube. I think it comes from men who are not circumcised.”
(Chongwe, female, 47 years, HIV positive)
“I heard that there is a virus that comes from the foreskin of a man which when it contacts the cervix, leads to cervical cancer.”
(Lusaka, female, 33 years, HIV positive)
Knowledge about HIV infection as a risk factor for cervical cancer was poor
Only a quarter of the women from both the urban and rural districts mentioned HIV infection as increasing the risk of developing cervical cancer.
“HIV+ people have a higher risk of getting infected with cervical cancer my aunt was asked to do a test when she had cervical cancer and she was found to be HIV +.”
(Lusaka, female, 27 years, HIV negative)
More women in Lusaka (urban) than Chongwe (rural) indicated that they did not have knowledge of cervical cancer risk factors and prevention
Although most women were able to mention at least one potential risk factor and approach to prevent cervical cancer, about one-sixth of the women, all of whom were from the urban district indicated that they did not know the risk factors for cervical cancer and whether it can be prevented.
“I don’t know if one can protect themselves because I don’t know how cervical cancer starts.”
(Lusaka, female, 34 years, HIV negative)
Men are generally knowledgeable about cervical cancer risk factors and prevention approaches
Men were knowledgeable about both risk factors and prevention of cervical cancer. The most commonly known risk factors among men were HPV and HIV infections and they cited circumcision and screening as important for prevention.
“I can say that with us men when meeting with a woman if you haven’t gone for male circumcision the dirt which is found on the man when the man has not washed properly will remain in the woman. The woman can get cervical cancer.”
(Chongwe, male 47 years)
“I think I’ve heard that if someone is HIV positive they are likely to get cervical cancer because those are some of the opportunistic infections that may come as a result of lower immunity levels”.
(Lusaka, male, 39 years)
“Yes, it can be prevented if you come to screen and they know. You will find help.”
(Lusaka, Male, 35 years)
Urban and rural respondents learned about cervical cancer from different sources
The dominant source of information for women and men in Chongwe (rural) was the health facility. Whereas in Lusaka (urban), there were multiple sources including the health facility, family and friend, media and the work place (Figure 3).
Figure 3:
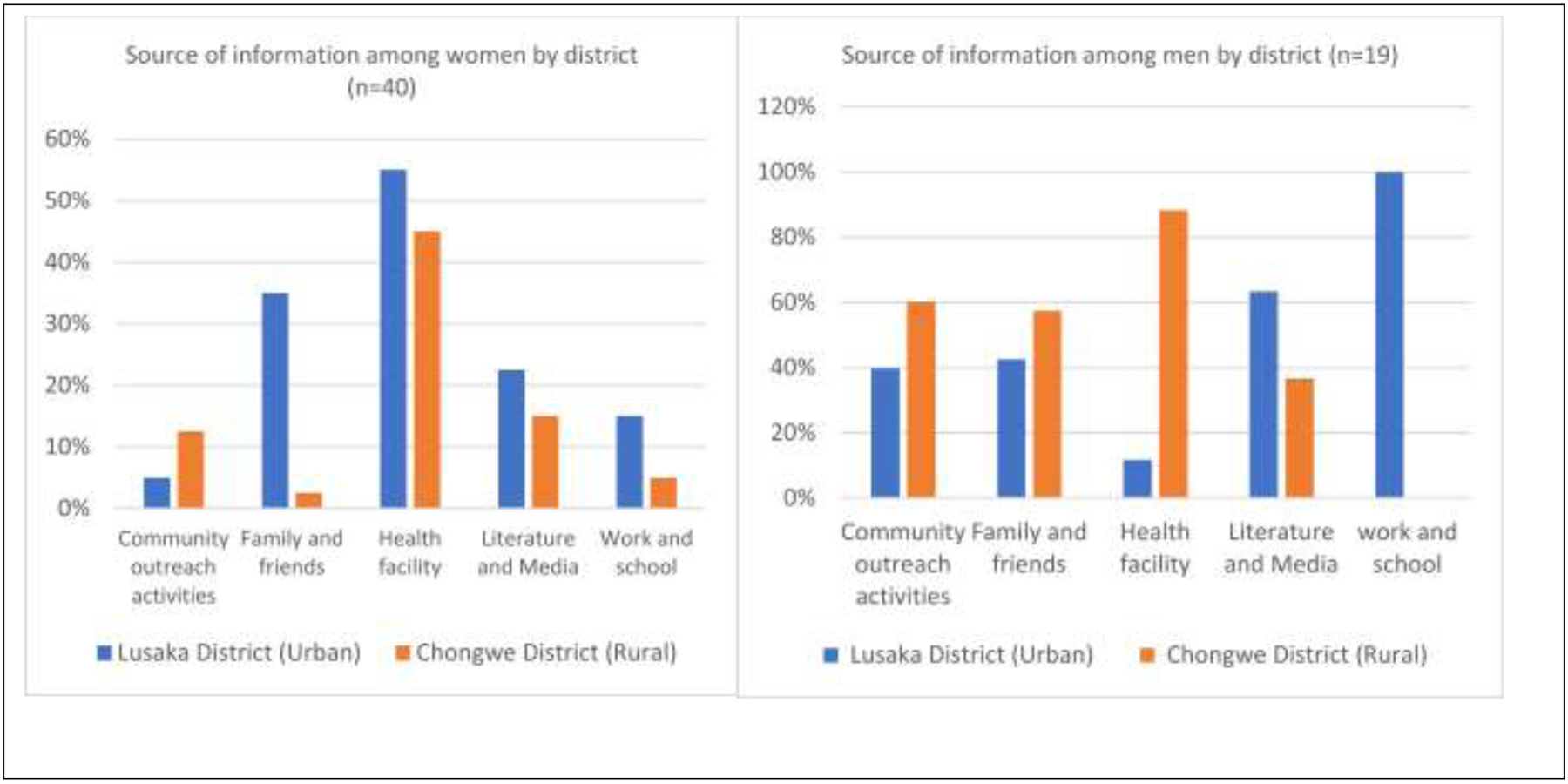
Source of cervical cancer information by district
Care seeking behavior is triggered by different factors among subgroups
Most of the respondents highlighted the desire to know one’s cervical cancer status as a reason for screening. More of the HIV negative women referenced being symptomatic as a reason to screen for cervical cancer compared to HIV positive women.
“Sometimes it’s getting sick which causes women to screen like, if you feel pain under your belly button, the doctor will advise you to go for screening.”
(Chongwe, female, 29 years, HIV negative)
The key themes emerging among unscreened women on reasons for not screening were fear of pain during screening, lack of time and reluctance. All the respondents who referenced lack of time were HIV positive whilst those who cited reluctance were HIV negative.
“I would have screened but I am afraid because of what other women say that the pain is similar to labour pains.”
(Chongwe, female, 29 years, HIV negative)
“There is no time. I think about the walking I have to do”
(Lusaka, female, 35 years, HIV positive)
“The situation would still be the same. It’s not that there is only one day when the screening is offered, women just feel lazy.”
(Chongwe, female, 27 years, HIV negative)
Discussion
The differences in knowledge and perceptions on cervical cancer between HIV positive and HIV negative women from a rural and an urban district was examined. It was observed that knowledge about the role of screening in preventing cervical cancer is generally good in our study population. This is consistent with the findings of a study which was carried out to assess the level of knowledge on cervical cancer and uptake of screening among HIV infected women in Gondar, northwest Ethiopia were early detection, diagnosis and treatment were the most commonly mentioned approach to cervical cancer prevention12.
This study showed however, that there is less consistency in terms of specific knowledge about risk factors and other prevention approaches and this varied by HIV status and by location of residence. HIV positive women seemed to have more accurate knowledge compared to HIV negative women. For example, they mentioned HIV and HPV infection as cervical cancer risk factors and circumcision as a preventive measure, which are all in agreement with the World Health Organization’s guidelines and recommendations. Our findings are consistent with the results of a study conducted among Rwandese women to assess their knowledge about cervical cancer prevention. It was found that women who had ever had an HIV test were more likely to know more about cervical cancer compared to those who had not tested for HIV13. HIV positive women visit the health facilities more often and therefore may have access to information on various health concerns including cervical cancer through interaction with clinic staff.
We found differences in knowledge of the respondents between the two districts. Rural women were more likely to identify risk factors related to hygiene and traditional practices than those living in urban areas. Respondents from the urban district had access to more institutionalized sources of information which were more likely to have much accurate information, for example, media, schools and place of work. Respondents from the rural districts were more likely to get information through friends, family and community outreach activities. They were also more likely to receive messaging that emphasizes harmful traditional practices. Although this knowledge is important, rural women could benefit from having a broader understanding of risk factors so that they understand they can still develop cervical cancer even if they avoid traditional practices.
The most important risk factor for cervical cancer is HPV infection14. We found that only a minority of women were able to accurately indicate why this is a risk factor for cervical cancer. This is similar to the findings of the study conducted in Gondor, Ethiopia were only 53% of the respondents mentioned HPV infection as a risk factor12. This implies that there is need for more education on the link between HPV infection and cervical cancer, especially as plans for introducing the HPV vaccine are underway in Zambia. A lack of understanding on the link between HPV infection and cervical cancer may negatively affect acceptability of the HPV vaccine.
Male circumcision is recommended as a primary prevention method against cervical cancer2, and it was consistently mentioned as such by the participants especially among HIV positive women. This is in agreement with findings from a study carried out on HIV positive women in Zimbabwe which found that circumcision was one of the methods commonly mentioned as a prevention method15. Behavior change messages in Zambia have incorporated male circumcision for both HIV and HPV prevention. However, caution should accompany this information as male circumcision does not completely protect women from acquiring HPV. Our results indicate that some women think that they do not need to screen for cervical cancer because their partner is circumcised. Behavior change messages need to convey that there is a risk of acquiring cervical cancer even with a circumcised partner. One of the positive findings from this study is that men in general were aware of cervical cancer and approaches to prevent the disease. They were also willing to support their female relatives to undergo regular screening to detect cervical cancer at an early stage when treatments are more effective.
Despite understanding the risk factors for cervical cancer, HIV positive women do not consistently access cervical cancer screening. The study conducted in Gondor, Ethiopia also showed that only 71% of the HIV positive women in the study had ever been screened for cervical cancer12. A primary barrier mentioned by respondents in our study was the lack of time, reflecting long travel times to clinics and long waiting times at clinics to undergo screening. A study conducted in Ethiopia showed that most of the participants were unwilling to take the screening test due to the assumption that the test was time consuming16. A key recommendation to increase screening uptake is to reduce waiting time at clinics and make the screening more accessible so that women do not need to travel long distances.
Early detection of precancerous lesions is universally recognised as an effective method of preventing cervical cancer8. In this study, women had the knowledge that cervical cancer can be prevented through early screening and treatment but the drive to know one’s cervical cancer status was largely due to the presence of perceived symptoms of cervical cancer. In its early stages, cervical cancer does not typically exhibit symptoms. Many women are diagnosed with invasive cervical cancer because they do not go early enough or regularly to screen regardless of whether they are symptomatic. This is consistent with the findings of a qualitative study conducted in Malaysia in which unscreened women were asked about barriers to cervical cancer screening. Majority of the women believed that the test was not necessary for them as they did not have any reproductive health problems. They felt that they would only need a screening test if they developed symptoms of pelvic infection or abnormal bleeding17. Similarly, a study carried out in Lao PDR reports that, of the one-third of the women in the study, about half of whom were HIV positive, mentioned the absence of symptoms as a reason for not screening for cervical cancer8. These findings indicate that there is need to educate and motivate women to seek screening prior to experiencing symptoms as this will offer the highest likelihood of identifying precancerous lesions that can be treated to prevent cervical cancer.
There are some limitations to our analysis which need to be highlighted. Firstly, we only used one methodological approach to elicit information from women and men who participated in this study. Using multiple approaches, including mixed-methods, may have revealed a richer set of themes. Secondly, we had a limited sample size and therefore focused on key stratifying factors related to location of residence and HIV status. Other aspects such as education and socio-economics can also play a role and should be explored in future studies. Finally, our findings are limited to the feedback received from those interviewed and potentially, an ethnographic focused research which could include observation and interactions with the subjects could have yielded additional actionable findings on facilitators and barriers to cervical cancer screening.
Conclusion
The study established that generally, the level of knowledge and perception of cervical cancer screening among women is high. A few gaps and differences in knowledge and perceptions between subgroups exist. HIV positive women have more accurate information on cervical cancer. They are also more likely to mention HPV infection as a risk factor. However, there are individual and service delivery level barriers that were revealed which hinder them from accessing screening services. More women in the urban district than the rural district indicated that they did not have knowledge of cervical cancer risk factors and prevention approaches and overall a minority of women acknowledged HIV as a risk factor for developing cervical cancer. There is need to standardize information on cervical cancer. Accurate information on cervical cancer risk factors and prevention approaches may help improve access to cervical cancer screening. Improving efficiency of the screening process by eliminating long waiting times and travel time to clinics can also motivate more women to seek regular screening. HPV vaccination is an essential approach to decrease the incidence of cervical cancer in future cohorts of women in Zambia, and better understanding of the link between HPV infection and cervical cancer can help women advocate to have their daughters to seek HPV vaccination. The findings from this study can assist the Zambian Ministry of Health in the ongoing efforts to scale-up cervical cancer screening and introduce HPV vaccination.
Acknowledgement
We would like to thank Dr. Hector Chiboola for his assistance in data collection as well as Ms. Patricia Kantumoya and Ms. Rhoda Chabaputa for their assistance in data collection and transcription of audio recorded interviews.
Funding
This study was funded by a grant from the US National Cancer Institute (1R01CA200845-01A1).
Footnotes
Ethics Approval and Consent to Participate
This study was approved by the Zambia Biomedical Research Ethics Committee, National Health Research Authority and the Institutional Review Board at RTI International. Permission was sought from the Provincial and District Medical Offices and the facility in-charges and superintendents were informed about the study objectives and procedures of the data collection. Informed consent was obtained from all participants.
Consent for Publication
Not applicable.
Availability of Data and Materials
The data is available with corresponding author on reasonable request.
Competing Interests
The authors declare that they have no competing interests.
References
- 1.Makuza JD, Nsanzimana S, Muhimpundu MA, Pace LE, Ntaganira J and Riedel DJ. Prevalence and risk factors for cervical cancer and pre-cancerous lesions in Rwanda. Pan Afr Med J 2015, 22:26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.UNAIDS. HPV, HIV and cervical cancer Leveraging synergies to save women’s lives. 2016.
- 3.Ferlay JS I and Ervik M GLOBOCAN 2012 v1.0, Cancer Incidence and Mortality Worldwide: IARC CancerBase No. 10 [Internet] 2012.
- 4.Bruni L, Barrionuevo-Rosas L, Albero G, Serrano B, Mena M, Gómez D, Muñoz J, Bosch FX and de Sanjosé S. Human Papillomavirus and Related Diseases Report-ZAMBIA. 2017.
- 5.Kalima M, Lishimpi K, Meza JL, Watanabe-Galloway S, Msadabwe SC, Mwaba CK, Shibemba AL, Banda L, Wood C and Chamberlain RM. Observed and expected incidence of cervical cancer in lusaka and the southern and Western provinces of Zambia, 2007 to 2012. Int J Gynecol Cancer 2015, 25(1):98–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Central Statistical Office (CSO) and Ministry of Health (MOH). 2013–14 ZDHS. 2015.
- 7.Bateman AC, Katundu K, Mwanahamuntu MH, Kapambwe S, Sahasrabuddhe VV, Hicks ML, Chi BH, Stringer JS, Parham GP and Chibwesha CJ. The burden of cervical pre-cancer and cancer in HIV positive women in Zambia: a modeling study. BMC Cancer 2015, 15:541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sichanh C, Quet F, Chanthavilay P, Diendere J, Latthaphasavang V, Longuet C and Buisson Y. Knowledge, awareness and attitudes about cervical cancer among women attending or not an HIV treatment center in Lao PDR. BMC Cancer 2014, 14:161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Aweke YH, Ayanto SY and Ersado TL. Knowledge, attitude and practice for cervical cancer prevention and control among women of childbearing age in Hossana Town, Hadiya zone, Southern Ethiopia: Community-based cross-sectional study. PLoS One 2017, 12(7): e0181415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lukorito J, Wanyoro A and Kimani H. Uptake of Cervical Cancer Screening among HIV Positive Women in Comrehensive Care Centres in Nairobi, Kenya. Research in Obstetrics and Gynecology 2017, 5(1):1–6. [Google Scholar]
- 11.Mulatu K, Motma A, Seid M and Tadesse M. Assessment of Knowledge, Attitude and Pratice on Cervical Cancer Screening among Female Students of Mizan Tepi University, Ethiopia. iMedPub Journals 2017, 1(1). [Google Scholar]
- 12.Erku DA, Netere AK, Mersha AG, Abebe SA, Mekuria AB and Belachew SA. Comprehensive knowledge and uptake of cervical cancer screening is low among women living with HIV/AIDS in Northwest Ethiopia. Gynecol Oncol Res Pract 2017, 4:20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mukama T, Ndejjo R, Musabyimana A, Halage AA and Musoke D. Women’s knowledge and attitudes towards cervical cancer prevention: a cross sectional study in Eastern Uganda. BMC Womens Health 2017, 17(1):9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Human papillomavirus (HPV) and cervical cancer [http://www.who.int/mediacentre/factsheets/fs380/en/].
- 15.Matangaidze O, Ramalivhana NJ, Mbambo-Kekana NP, Ndaimani A and Maxwel M. Knowledge, Attitudes and Practices of HIV-Infected Women on Cervical Cancer Screening at a Church-affiliated Hospital. IOSR Journal of Dental and Medical Sciences 2016, Volume 15(Issue 4):PP 119–126. [Google Scholar]
- 16.Belete N, Tsige Y and Mellie H. Willingness and acceptability of cervical cancer screening among women living with HIV/AIDS in Addis Ababa, Ethiopia: a cross sectional study. Gynecol Oncol Res Pract 2015, 2:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wong LP, Wong YL, Low WY, Khoo EM and Shuib R. Cervical Cance Screening Attitudes and Beliefs of Malaysian Women who have Never had a Pap Smear: A Qualitative Study. International Journal of Behavioral Medicine 2008, 15: 289–292. [DOI] [PubMed] [Google Scholar]


