Abstract
Background
We assessed the safety, efficacy, and pharmacokinetics of the transforming growth factor beta (TGFβ) receptor inhibitor galunisertib co-administered with the anti-programmed death-ligand 1 (PD-L1) antibody durvalumab in recurrent/refractory metastatic pancreatic cancer previously treated with ≤2 systemic regimens.
Methods
This was a two-part, single-arm, multinational, phase Ib study. In a dose-finding phase, escalating oral doses of galunisertib were co-administered on days 1–14 with fixed-dose intravenous durvalumab 1500 mg on day 1 every 4 weeks (Q4W), followed by an expansion cohort phase.
Results
The galunisertib recommended phase II dose (RP2D) when co-administered with durvalumab 1500 mg Q4W was 150 mg two times per day. No dose-limiting toxicities were recorded. Among 32 patients treated with galunisertib RP2D, 1 patient had partial response, 7 had stable disease, 15 had objective progressive disease, and 9 were not evaluable. Disease control rate was 25.0%. Median overall survival and progression-free survival were 5.72 months (95% CI: 4.01 to 8.38) and 1.87 months (95% CI: 1.58 to 3.09), respectively. Pharmacokinetic profiles for combination therapy were comparable to those published for each drug. There was no association between potential biomarkers and treatment outcomes.
Conclusion
Galunisertib 150 mg two times per day co-administered with durvalumab 1500 mg Q4W was tolerable. Clinical activity was limited. Studying this combination in patients in an earlier line of treatment or selected for predictive biomarkers of TGFβ inhibition might be a more suitable approach.
Trial registration number
ClinicalTrials.gov identifier: NCT02734160.
Keywords: immunotherapy, tumor biomarkers, therapies, investigational, tumor microenvironment, clinical trials as topic
Background
Pancreatic cancer is one of the most lethal and poorly understood human malignancies. Nearly half a million people per year are diagnosed worldwide with pancreatic cancer, and approximately the same number die of this disease.1 2 As such, pancreatic cancer has been identified as a cancer of significant unmet need.3 The reasons why pancreatic cancer is difficult to treat are numerous but include: the stromalized nature of the tumor, causing an immunosuppressive microenvironment; the location of the tumor; and difficulties in achieving adequate drug delivery.4 5
The largest effort of integrated genomic analysis in understanding the molecular basis of pancreatic cancer has recently confirmed the transforming growth factor beta (TGFβ) to be a commonly dysregulated signal transduction pathway in this disease.6 The TGFβ signaling pathway has one of the most essential, but also complex and controversial, roles in cancer. TGFβ maintains homeostasis in normal tissue; however, cancer cells, being genetically unstable entities, have the capacity to corrupt the suppressive influence of TGFβ on tumors. Thus, dysregulation of TGFβ signaling promotes tumor growth, metastasis, and immune suppression.7 8
To date, immune checkpoint inhibitors—the monoclonal antibodies blocking cytotoxic T-lymphocyte-associated protein 4, programmed cell death protein-1 (PD-1), or programmed death-ligand 1 (PD-L1) that induce a CD8+ T-cell-dependent tumor regression in several neoplastic diseases9—have largely been ineffective in pancreatic cancer.10 11 An exception is a small subtype of patients with microsatellite instability-high/deficient mismatch repair (MSI-H/dMMR) tumors.12–14
Pancreatic cancer is characterized by a highly immunosuppressive tumor microenvironment that can actively suppress the functions of immune cells through a number of mechanisms, including overexpression of PD-L1 and secretion of immunosuppressive factors, such as TGFβ.15–17 High levels of TGFβ create an immunosuppressive milieu, which inhibits anti-tumor immunity by suppressing or altering activation, maturation, and differentiation of both innate and adaptive immune cells.18 To increase the sensitivity of pancreatic tumors to immune checkpoint inhibitors, it may therefore be necessary to overcome the immunosuppressive tumor microenvironment sustained by TGFβ.19 20
Galunisertib is an oral small-molecule inhibitor of the type I TGFβ receptor (TGFβ-RI) that specifically downregulates SMAD2 phosphorylation, abrogating activation of the TGFβ canonical pathway.21 A phase Ib/randomized phase II study (JBAJ) of galunisertib in combination with gemcitabine showed improved overall survival (OS) versus gemcitabine monotherapy in patients with unresectable pancreatic cancer.22 Exposure-response (defined as OS) analyses23 concluded that there was a flat daily exposure–OS relationship within the observed exposure range, once all significant baseline covariates were included. These published analyses suggested that 300 mg/day galunisertib administered as 150 mg two times per day for 14 days on/14 days off treatment was an appropriate dosing regimen for patients with pancreatic cancer.
Previous preclinical research on galunisertib in pancreatic cancer found that selective TGFβ inhibition in CD8+ T cells led to regression of neoplastic disease, but systemic blockade of TGFβ signaling failed to promote cytotoxicity due to compensatory upregulation of PD-L1 on the tumor cell.24 Dual targeting of TGFβ and PD-L1 receptors promoted T-cell-mediated clearance of pancreatic adenocarcinoma.24 25 On the basis of these findings, the combination of TGFβ and PD-L1 inhibition has the potential to act synergistically to induce immune restoration and improve anti-tumor responses in pancreatic cancer.
The purpose of this phase Ib study was to assess the safety, efficacy, and pharmacokinetics (PK) of galunisertib when combined with durvalumab, a human G1 immunoglobulin monoclonal antibody that blocks the interaction of PD-L1 with PD-1 in patients with recurrent or refractory metastatic pancreatic cancer. We also explored the relationship between potential biomarkers and treatment outcomes.
Methods
Study design and patients
This single-arm, multicenter, phase Ib study had a dose-finding phase (Part A) followed by an expansion cohort phase (Part B) (online supplemental figure S1). The study was conducted at 11 sites in France, Italy, Republic of Korea, Spain, and the USA. Patients were not involved in the design or conduct of this research.
jitc-2020-002068supp001.pdf (852.7KB, pdf)
Eligibility criteria included histologically or cytologically confirmed recurrent or refractory metastatic pancreatic adenocarcinoma, age ≥18 years, an Eastern Cooperative Oncology Group (ECOG) performance status ≤1, and ≤2 prior systemic regimens for locally advanced or metastatic pancreatic adenocarcinoma, which had to include one of the following: FOLFIRINOX, nab-paclitaxel/gemcitabine, TS-1 (tegafur-gimeracil-oteracil potassium), irinotecan/fluorouracil/leucovorin, or single-agent gemcitabine. Adjuvant lines of therapy were excluded. A current tumor biopsy or archived tumor tissue <3 years prior to enrollment for biomarker analysis was also required.
Key exclusion criteria were moderate or severe cardiovascular disease, or evidence of interstitial lung disease that was symptomatic or may have interfered with the detection or management of suspected drug-related pulmonary toxicity or active, non-infectious pneumonitis. Patients could not have been on immunosuppressive steroids or have autoimmune disease.
Treatments
Part A followed a modified 3+3 design in which patients were treated in sequential cohorts of escalating oral doses of galunisertib 50 mg one time per day (Cohort 1), 50 mg two times per day (Cohort 2), 80 mg two times per day (Cohort 3), or 150 mg two times per day on days 1–14 (Cohort 4). Galunisertib was self-administered in combination with a fixed dose of durvalumab 1500 mg delivered as an intravenous infusion over 60 min on day 1 every 4 weeks (Q4W). The criteria for dose escalation were based on dose-limiting toxicity (DLT) over 28 days or up to the completion of cycle 1. If no DLTs were observed in Cohort 1, three patients were treated at the higher-dose level (online supplemental figure S1). If one of the three patients experienced a DLT, the cohort would be expanded to six patients. Dose escalation could proceed if no further DLTs were observed. The maximum tolerated dose (MTD) was defined as the highest tested dose that had <33% probability of causing a DLT (ie, DLT in <2 of six patients). If the MTD was not identified, the recommended phase II dose (RP2D) of galunisertib was defined as the maximum study dose.
In Part B, the recommended galunisertib dose from Part A was given on days 1–14 of a ‘14 days on/14 days off’ treatment cycle in combination with a fixed dose of durvalumab 1500 mg delivered as an intravenous infusion over 60 min on day 1 Q4W. Patients were treated until progressive disease, unacceptable toxicity, protocol non-compliance, or withdrawal of consent. If a patient experienced an adverse event (AE) that required the patient to be discontinued from one study drug, the patient was discontinued from both drugs.
Objectives
The primary objective of Part A was to determine the MTD/RP2D of orally dosed galunisertib in combination with durvalumab, as measured by the number of patients with DLT in cycle 1. The primary objective of Part B was to evaluate the safety of galunisertib in combination with durvalumab in patients with metastatic pancreatic cancer at the RP2D.
Secondary objectives were to characterize the PK of galunisertib and durvalumab when co-administered and to characterize the immunogenicity of durvalumab when administered in combination with galunisertib. Additional secondary objectives were to assess the preliminary anti-tumor activity of the treatment combination by progression-free survival (PFS), OS, objective response rate (ORR), duration of response, disease control rate (DCR), and time to response. An exploratory objective was to examine biomarkers, which included pharmacodynamic markers and markers relevant to galunisertib, durvalumab, immune cells/immune functioning, other immune pathways, PD-L1 expression, and the advanced disease state, and to correlate these markers to clinical outcome.
Assessments
DLT was defined as one of the following AEs possibly related to either study drug during cycle 1: grade 4 hematological AEs (febrile neutropenia of any grade), grade 3 or grade 4 immune-related AEs (irAEs), or any grade 3 or grade 4 non-hematological AEs. Non-hematological toxicity must have resolved to grade 0, 1, or baseline level before treatment was resumed (with the exception of alopecia, fatigue, skin rash, constipation, electrolyte disturbances, and diarrhea), or grade 3 nausea, vomiting, or anorexia that could be controlled with treatment. Treatment-related failure to administer ≥75% of the planned total dose or delay in galunisertib administration >2 weeks because of any treatment-related toxicity was also considered a DLT. A full listing of DLT criteria and assessment details for AEs is available in the online supplemental material.
The pharmacokinetics of galunisertib were assessed in venous blood samples collected on day 1 (pre-dose and between 0.5 and 3 hours) and day 14 (pre-dose, between 0.5 and 2 hours, between 3.5 and 5 hours, and 24 hours post-dose) in cycles 1 and 2, followed by pre-dose samples in cycles 3, 4, and 7. Details on the pharmacokinetic methods used are provided in the online supplemental material and have been previously published.26 27
Tumor response was assessed radiographically according to Response Evaluation Criteria in Solid Tumours V.1.1. Disease assessment with CT and/or MRI, as appropriate, was performed at baseline and every 8 weeks until disease progression or until patients withdrew from the study. The assessment of biomarkers is described in the online supplemental material.
Statistical analyses
Approximately 12–24 patients were required to participate in the dose escalations and ≥28 were to be treated at the RP2D in Part B (≥3 in the dose escalation cohort and approximately 25 in the expansion cohort). All patients who received ≥1 dose of either galunisertib or durvalumab were evaluated for safety (safety population). For the purpose of this article, irAEs were analyzed post hoc and were defined as events considered to be related to treatment by the investigator that were treated with corticosteroids.
All patients who received ≥1 dose of either galunisertib or durvalumab at the RP2D of galunisertib in the dose escalation and expansion phases were combined for efficacy analyses (combined RP2D cohort). Statistical details for the efficacy endpoints, including censoring rules, are available in the online supplemental material.
Logistic regression analysis or Cox regression was performed to test the association between ‘clinical benefit’ and potential biomarkers (using the median value as the cut-off to dichotomize data as low vs high). For the purpose of the biomarker analysis, any patient who had a confirmed complete response, partial response (PR), or stable disease for ≥3 months was considered as having derived a clinical benefit from study treatment. Sixty biomarkers were evaluated in 32 patients. Multiplicity adjustment (Holm’s method) was applied. P values from a likelihood ratio test were obtained from logistic or Cox regression of clinical benefit as a function of a dichotomized marker. In the case of missing biomarker data for any patient, the patient was excluded from the relevant analysis.
Results
Patients
Between August 2016 and April 2018, 79 patients were enrolled in the study. Forty-two (53.2%) patients received study treatment; 28 (35.4%) patients were screen failures and did not receive study treatment, 4 patients withdrew consent, 4 did not participate owing to physician decision, and 1 experienced an AE that prevented participation. All 42 (53.2%) patients who received ≥1 dose of study drug discontinued study treatment. The primary reason for study discontinuation was progressive disease (35 (83.3%)). Three patients died during treatment (due to progressive disease; unrelated to treatment), two patients discontinued due to AEs, and one patient each discontinued due to protocol deviation and physician decision.
Of the 42 patients treated, the majority were women, <65 years of age, and white. Most had ≥1 previous surgery and two prior systemic therapies for pancreatic cancer in the advanced or metastatic setting (table 1).
Table 1.
Baseline demographics and treatment history
| Galunisertib 50 mg one time per day+durvalumab 1500 mg Q4W n=3 | Galunisertib 50 mg two times per day+durvalumab 1500 mg Q4W n=4 | Galunisertib 80 mg two times per day+durvalumab 1500 mg Q4W n=3 | Galunisertib 150 mg two times per day+durvalumab 1500 mg Q4W n=32 | Total N=42 |
|
| Male sex, n (%) | 1 (33.3) | 2 (50.0) | 0 | 14 (43.8) | 17 (40.5) |
| Age in years, median (range) | 54 (45–76) | 59 (51–63) | 50 (39–71) | 58 (38–81) | 57 (38–81) |
| <65, n (%) | 2 (66.7) | 4 (100) | 2 (66.7) | 26 (81.3) | 34 (81.0) |
| ≥65, n (%) | 1 (33.3) | 0 | 1 (33.3) | 6 (18.8) | 8 (19.0) |
| Race, n (%) | |||||
| White | 3 (100) | 4 (100) | 0 | 24 (75.0) | 31 (73.8) |
| Asian | 0 | 0 | 2 (66.6) | 4 (12.5) | 6 (14.3) |
| Missing* | 0 | 0 | 1 (33.3) | 4 (12.5) | 5 (11.9) |
| Prior surgery, n (%) | 1 (33.3) | 2 (50.0) | 2 (66.7) | 19 (59.4) | 24 (57.1) |
| Prior radiotherapy, n (%) | 1 (33.3) | 1 (25.0) | 2 (66.7) | 4 (12.5) | 8 (19.0) |
| Adjuvant | 0 | 0 | 1 (33.3) | 1 (3.1) | 2 (4.8) |
| Advanced or metastatic | 0 | 0 | 1 (33.3) | 2 (6.3) | 3 (7.1) |
| Neoadjuvant | 1 (33.3) | 1 (25.0) | 0 | 1 (3.1) | 3 (7.1) |
| Prior systemic therapy in the advanced setting, median | |||||
| One prior regimen, n (%) | 1 (33.3) | 1 (25.0) | 1 (33.3) | 9 (28.1) | 12 (28.6) |
| Two prior regimens, n (%) | 2 (66.7) | 3 (75.0) | 2 (66.7) | 21 (65.6) | 28 (66.7) |
*Racial data were not collected in France.
Q4W, every 4 weeks.
Safety
The median durations of treatment with galunisertib ranged from 35 to 77 days, and from 47 to 91 days with durvalumab, across Cohorts 1–4. The study completed without observation of DLTs, and the combination of galunisertib 150 mg two times per day with durvalumab 1500 mg Q4W was considered tolerable. The majority of patients (41 (97.6%)) experienced treatment-emergent AEs. Overall, grade ≥3 treatment-emergent AEs occurred in 29 (69.0%) patients; only one of these was a grade 5 event (online supplemental table 1).
Twenty patients (47.6%) experienced treatment-related AEs (TRAEs), none of which were grade 5. The most common TRAEs were diarrhea (14.3%, all grade ≤2), fatigue (14.3%, all grade ≤2), elevated aspartate aminotransferase (AST; 11.9% (7.1% grade ≤2, 4.8% grade ≥3)), and elevated alanine aminotransferase (ALT; 11.9% (9.5% grade ≤2, 2.4% grade ≥3)). All other TRAEs occurred in ≤10% of patients (table 2). Four patients had immune-related TRAEs; these were diarrhea (n=2; grades 1 and 2), pneumonitis (n=1, grade 2), and elevated ALT (n=1, grades 1 and 2). None of the treatment-related irAEs were considered serious.
Table 2.
TRAEs in ≥5% of patients*
| TRAE, n (%)† | Galunisertib 50 mg one time per day+durvalumab 1500 mg Q4W n=3 | Galunisertib 50 mg two times per day+durvalumab 1500 mg Q4W n=4 | Galunisertib 80 mg two times per day+durvalumab 1500 mg Q4W n=3 | Galunisertib 150 mg two times per day+durvalumab 1500 mg Q4W n=32 | Total N=42 |
|||||
| All grades | Grade 3/4 | All grades | Grade 3/4 | All grades | Grade 3/4 | All grades | Grade 3/4 | All grades | Grade 3/4 | |
| ≥1 TRAE | 2 (66.7) | 0 | 2 (50.0) | 0 | 3 (100) | 0 | 13 (40.6) | 5 (15.6) | 20 (47.6) | 5 (11.9) |
| Diarrhea | 0 | 0 | 0 | 0 | 1 (33.3) | 0 | 5 (15.6) | 0 | 6 (14.3) | 0 |
| Fatigue | 0 | 0 | 0 | 0 | 2 (66.7) | 0 | 4 (12.5) | 0 | 6 (14.3) | 0 |
| Elevated AST | 0 | 0 | 0 | 0 | 1 (33.3) | 0 | 4 (12.5) | 2 (6.3) | 5 (11.9) | 2 (4.8) |
| Elevated ALT | 0 | 0 | 0 | 0 | 1 (33.3) | 0 | 4 (12.5) | 1 (3.1) | 5 (11.9) | 1 (2.4) |
| Nausea | 0 | 0 | 1 (25.0) | 0 | 0 | 0 | 3 (9.4) | 0 | 4 (9.5) | 0 |
| Vomiting | 0 | 0 | 0 | 0 | 1 (33.3) | 0 | 3 (9.4) | 0 | 4 (9.5) | 0 |
| Pruritus | 0 | 0 | 0 | 0 | 0 | 0 | 3 (9.4) | 0 | 3 (7.1) | 0 |
| Arthralgia | 0 | 0 | 0 | 0 | 0 | 0 | 3 (9.4) | 0 | 3 (7.1) | 0 |
*Includes all grade 1–4 TRAEs in the total population (N=42); patients may have had ≥1 TRAE.
†No grade 5 TRAEs occurred.
ALT, alanine aminotransferase; AST, aspartate aminotransferase; Q4W, every 4 weeks; TRAE, treatment-related adverse event.
Five of 32 patients (15.6%) in the galunisertib 150 mg two times per day group experienced a total of 10 grade 3 or grade 4 TRAEs. Of laboratory abnormalities, one patient had grade 3 elevated ALT and grade 3 AST (both also considered serious TRAEs), one patient had grade 3 elevated AST and two events of elevated gamma-glutamyl transferase (one grade 3 and one grade 4 event), and one had grade 3 elevated alkaline phosphatase and grade 3 elevated gamma-glutamyl transferase. Of the hematological events, one patient had grade 3 neutropenia and another had grade 3 anemia and grade 3 decreased lymphocyte count.
Two of 32 patients (6.3%) in the galunisertib 150 mg two times per day group discontinued study treatment prematurely due to AEs (treatment-related grade 2 arthralgia (n=1), treatment-unrelated pulmonary embolism (n=1)). A total of 31 of 42 (73.8%) patients died during the study. Of these, 11 (26.2%) died on therapy (n=3) or within 30 days of discontinuation (n=8), and 20 (47.6%) died after 30 days of treatment discontinuation. All deaths were due to progressive disease.
Pharmacokinetics
Following galunisertib administration at 50, 80, and 150 mg two times per day, the mean plasma concentration versus time profiles reached maximum concentration within 4 hours, with similar elimination rates across all doses (online supplemental figure S2). There was an increase in maximum concentration and exposure with dose increase across the cohorts (table 3). No anti-drug antibodies against durvalumab were detected in this study.
Table 3.
Steady-state galunisertib pharmacokinetic parameters following multiple doses
| Galunisertib 50 mg one time per day+durvalumab 1500 mg Q4W | Galunisertib 50 mg two times per day+durvalumab 1500 mg Q4W | Galunisertib 80 mg two times per day+durvalumab 1500 mg Q4W | Galunisertib 150 mg two times per day+durvalumab 1500 mg Q4W | |
| Patients per cohort | 3 | 4 | 3 | 32 |
| PK-evaluable patients* | 3 | 2 | 3 | 25 |
| PK profiles | 6 | 3 | 6 | 38 |
| Cycle 1 profiles | 3 | 2 | 3 | 24 |
| Cycle 2 profiles | 3 | 1 | 3 | 14 |
| tmax, hours, median (range) | 0.6 (0.5–3.9) | 0.5 (0.5–0.9) | 3.8 (0.5–4.0) | 2.7 (0.5–4.0) |
| Cmax, µmol/L | 424 (70) | 260† (71) | 612 (39) | 1070 (83) |
| AUC(0-tau), µg·h/L | 1630 (32) (tau=24 hours) |
813 (68) (tau=12 hours) |
3150 (63) (tau=12 hours) |
6120 (58) (tau=12 hours) |
All PK parameters at steady state are geometric mean (CV %) unless stated otherwise.
*Patients with ≥1 profile of day 14 pre-dose sample, two post-dose samples, and 1 day 15 pre-dose (24-hour) sample.
†Should be interpreted with caution due to limited data (n=3). There is overlap between the observed Cmax ranges following galunisertib 50 mg one time per day and 50 mg two times per day administration (see online supplemental figure S2).
AUC(0-tau), area under the concentration versus time curve for the dosing interval; Cmax, maximum observed concentration; CV, coefficient of variation; PK, pharmacokinetics; Q4W, every 4 weeks; tmax, time of maximum observed concentration.
Efficacy outcomes
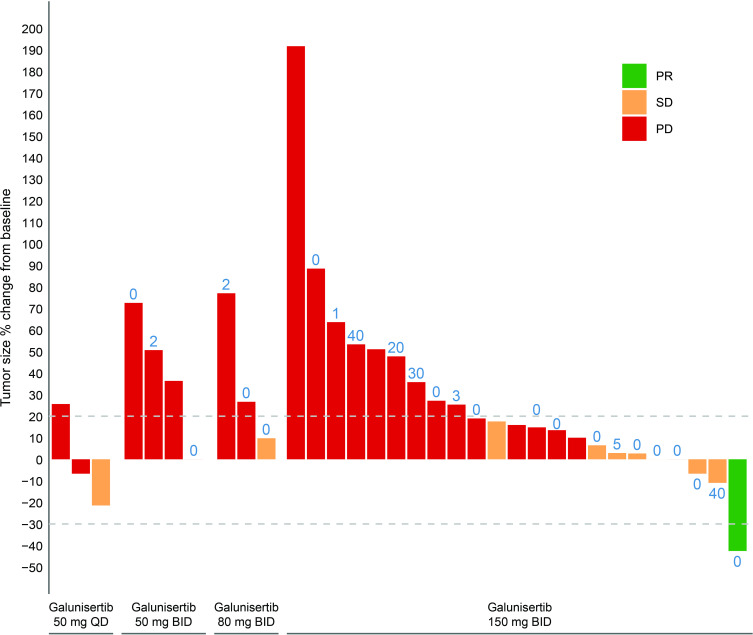
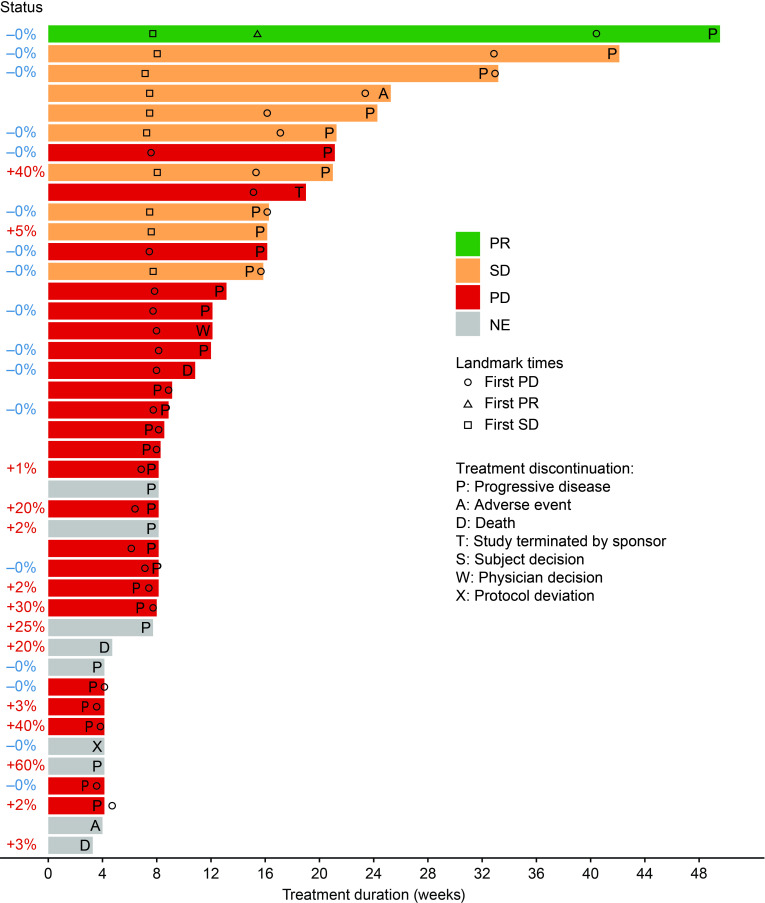
Among the 32 patients in the combined RP2D cohort, the confirmed ORR was 3.1% (n=1). One patient in the combined RP2D cohort had PR, 7 patients had stable disease, and 15 had objective progressive disease. Nine patients were not evaluable, largely because several patients experienced early symptomatic deterioration and discontinued due to progressive disease before the first post-baseline tumor assessment was performed; thus, these cases were not classified as objective progressive disease. The DCR was 25.0% (online supplemental table 2). Five patients had reductions in tumor size (figure 1). The time to response for the one patient who showed a PR was 15.4 weeks, and the duration of response was 25.0 weeks (figure 2).
Figure 1.
Best response by patient based on change in tumor size. All treated patients with best overall response (n=33). Blue number=percentage of tumor cells at baseline with positive PD-L1 membrane staining. Dashed lines at –30% and 20% represent the thresholds for SD; neither an increase in size of more than 20% nor a decrease in size of more than 30% since the initial baseline measurement. BID, two times per day; PD, progressive disease; PD-L1, programmed death-ligand 1; PR, partial response; QD, one time per day; SD, stable disease.
Figure 2.
Association between PD-L1 expression and clinical benefit. For the purpose of the biomarker analysis, any patient who had a CR, PR, or SD for ≥3 months was considered as having derived clinical benefit from study treatment. CR, complete response; NE, non-evaluable; PD, progressive disease; PD-L1, programmed death-ligand 1; PR, partial response; SD, stable disease.
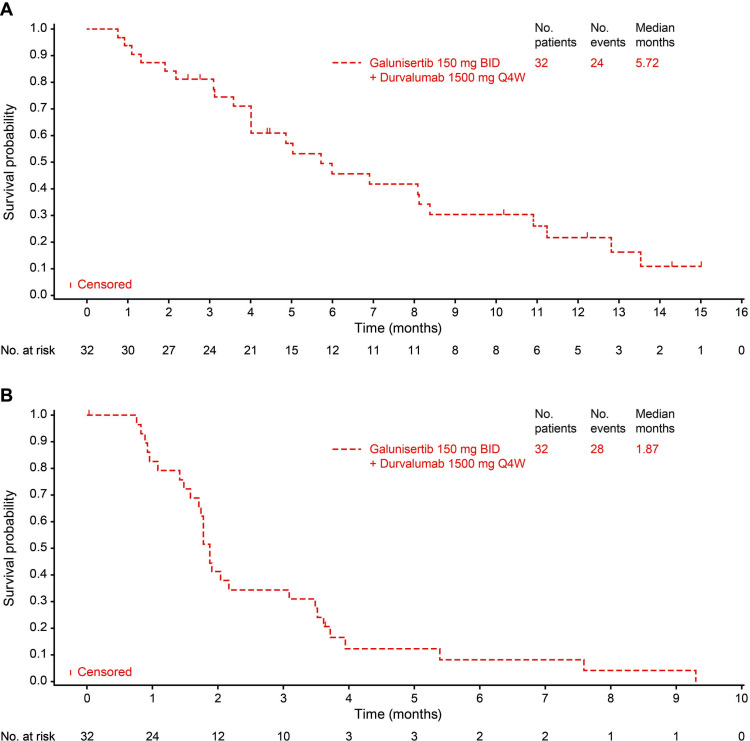
Median OS was 5.72 months in the galunisertib 150 mg group (95% CI: 4.01 to 8.38) (figure 3A). Eight patients were alive at data cut-off date (25.0%; figure 2). Median (95% CI) OS was 11.23 (1.31 to 13.54) months in patients who had received one prior therapy and 5.03 (3.12 to 6.90) months in patients with ≥2 prior therapies. The median PFS in the galunisertib 150 mg group was 1.87 months (95% CI: 1.58 to 3.09) (figure 3B). Median (95% CI) PFS was 1.58 (0.82 to 3.61) months in patients who had received one prior therapy and 1.89 (1.71 to 3.52) months in patients with ≥2 prior therapies.
Figure 3.
(A) Overall survival and (B) progression-free survival in the galunisertib 150 mg BID + durvalumab 1500 mg Q4W group. BID, two times a day; Q4W, every 4 weeks.
Biomarkers
PD-L1 immunohistochemistry scores evaluated as percentage of tumor cells at baseline with positive PD-L1 membrane staining were measured for 25 of 32 tumor samples from patients in the combined RP2D cohort. There was no statistically significant association between PD-L1 immunohistochemistry scores and clinical benefit as defined in this study.
Next-generation sequencing of 404 cancer-associated genes was performed on the subset of tumor samples with sufficient tissue (n=20, representing different galunisertib dose levels) (online supplemental table 3). As expected, the KRAS, TP53, CDKN2A, and SMAD4 genes had the greatest prevalence of genetic variants. Additionally, five (25.0%) tumors had ARID1A genetic variants. The clinical response and genetic data were too limited to observe any associations. Interestingly, tumors of the three patients with longest PFS and genetic data demonstrated a KRAS wild-type status.
No significant association between baseline serum proteins (n=73) and clinical benefit was detected after adjusting for multiplicity. However, we report the top five proteins each having p values of 0.02 or less: fibrinogen, interleukin-6, latency-associated peptide of TGFβ 1, interleukin-8, and interferon gamma-induced protein 10 (IP-10) (online supplemental table 4).
Discussion
To our knowledge, this is the first study to evaluate the combination treatment of an immune checkpoint inhibitor plus an inhibitor of TGFβ-RI in patients with pancreatic cancer. In this phase 1b study, no DLTs were observed, establishing galunisertib 150 mg two times per day plus durvalumab 1500 mg Q4W as the RP2D. No new safety issues were identified with galunisertib and durvalumab relative to either drug given as monotherapy, suggesting that this combination has an acceptable tolerability and safety profile.
The most common TRAEs observed with durvalumab monotherapy have previously been reported as fatigue, diarrhea, pruritus, and hypothyroidism.28 When durvalumab was combined with galunisertib, no increase in the frequency of these events was observed. In a previous study of galunisertib (300 mg/day) monotherapy, the most common TRAEs were nausea, fatigue, and hematological AEs.29 The combination of galunisertib with durvalumab in this study did not appear to increase the frequency of these events, and only 9.5% of patients had irAEs. In addition, cardiotoxicity, which can be associated with TGFβ modulation in preclinical models,27 30 was not observed.
Owing to the non-monitorable cardiac toxicity observed in preclinical species,27 an exposure threshold of 300 mg/day (administered as 150 mg two times per day) was determined for galunisertib using a PK/pharmacodynamic model.26 A dose of galunisertib 300 mg/day administered as 150 mg two times per day for 14 days on/14 days off treatment has been established in a phase II study as an appropriate dosing regimen for patients with pancreatic cancer.22 23 Galunisertib concentrations from this study were comparable with all observed concentration data from galunisertib completed trials,22 29 where the preclinically defined exposure threshold, sufficient in vivo target inhibition of pSMAD26 and flat exposure–OS relationship23 were achieved within the observed exposure range, following 150 mg two times per day dosing. These observations suggest that galunisertib concentrations are not affected by co-administration with durvalumab and that galunisertib dose could probably not be further increased without violating the toxicity defined exposure threshold. Durvalumab immunogenicity was not observed in this study, and likely did not contribute to the observed lack of efficacy. Durvalumab PK in this study were similar to previously reported concentrations.31
In this study, galunisertib in combination with durvalumab demonstrated a DCR of 25.0% and a confirmed ORR of 3.1%. We did not include any monotherapy arms in this study for determining contributions of each component, as checkpoint inhibitor treatment in pancreatic cancer has shown minimal response in previous studies. Based on the previously discussed preclinical data, we did not expect single-agent TGFβ inhibition to be adequate to generate a response due to tumor PD-L1 upregulation. However, the activity of this combination was similar to that observed in other recent studies in populations of patients treated with different combination strategies, including immune checkpoint inhibitors, following failure of gemcitabine-based chemotherapy.32–34 In a recent phase II randomized clinical trial of durvalumab with or without tremelimumab as second-line treatment for patients with metastatic pancreatic cancer, the ORR was 3.1% for patients receiving combination therapy and 0% for patients receiving monotherapy.32 In a phase II, multicenter, open-label, randomized clinical trial evaluating the Bruton tyrosine kinase inhibitor acalabrutinib as single-agent or with pembrolizumab in highly pre-treated patients with advanced pancreatic cancer, the ORR and DCR were 0% and 14.3% with monotherapy and 7.9% and 21.1% with combination therapy, respectively.33 A phase Ib single-arm study enrolled patients with pancreatic cancer who progressed after first-line treatment to receive pembrolizumab in combination with the oncolytic virus pelareorep and one chemotherapeutic agent among 5-fluorouracil, gemcitabine, or irinotecan. Even when including a registered chemotherapeutic agent, this combination strategy achieved an ORR of 9% and a DCR of 27%.34
This study also represents a large effort in exploring novel potential biomarkers. Consistent with previous studies in pancreatic cancer, tumor membrane PD-L1 expression was not associated with treatment response or PFS.10 Next-generation sequencing showed that a high proportion (25.0%) of samples analyzed lacked a KRAS mutation, indicating alternative genetic drivers for those tumors.35 Interestingly, three of the five samples with genetic data that lacked KRAS mutation were associated with longer PFS. KRAS mutation is a known negative prognostic factor in pancreatic cancer and may explain the longer PFS observed independent of any treatment effect.36 MSI-H/dMMR status has been proposed as a more robust predictive biomarker of immunotherapy efficacy than PD-L1 in pancreatic cancer.37 38 However, the one patient with a PR here had no known/likely functional mutations detected and only 14 mutations of unknown significance. The patient is therefore unlikely to be MSI-H because, on average, 11.5 mutations (known, likely functional, and unknown significance) were detected for all 20 tumor samples).
Patients were also not selected on the basis of the most promising circulating biomarkers for TGFβ inhibition, giving rise to a more heterogeneous population. In the previous randomized JBAJ study in patients with newly diagnosed advanced pancreatic cancer, IP-10 and macrophage inflammatory protein-1 alpha (MIP-1α; also known as CCL3) were identified as negative prognostic factors for the placebo plus gemcitabine cohort.39 In the same study, galunisertib combination treatment reversed this aggressiveness such that high IP-10 or MIP-1α was a positive predictive marker. In the present study, baseline serum IP-10 and MIP-1α were measured and were not statistically associated with better clinical benefit, as defined; however, at a median cut-point, high IP-10 trended with better clinical benefit (p=0.019, adjusted p=1.0; online supplemental table 4).
A potential limitation of our analyses is the relatively small sample size. Nonetheless, we might speculate that there may be a subpopulation of patients with pancreatic cancer who have an increased macrophage infiltration in the tumor microenvironment, causing an immune suppressed nature, poor prognostic outcome, and non-response to cytotoxic treatment. Owing to the aggressiveness of their disease, these patients may not be fit after completing first-line cytotoxic chemotherapy to receive further second-line or third-line treatment. It is reasonable to conceive that patients enrolled in the present trial were selected for their better prognosis as most of them progressed under a median of two prior systemic therapies while maintaining a good ECOG performance status score ≤1. Thus, the patient population who may have benefited most from this combination treatment may have been under-represented in this study. It may therefore be of particular interest to explore this therapeutic strategy in patients in an early line of treatment and selected for higher levels of macrophage-enriching cytokines such as IP-10 and MIP-1α. Furthermore, an immunogenic subtype of patients with enriched CD4+ and CD8+ T cell signaling, tumor-specific antigen presentation and, importantly, cytotoxic T-lymphocyte-associated protein 4 and PD-1 signaling have improved survival and may be more likely to respond to immunotherapies.6 40 41 Two recent studies provide preclinical evidence that combining TGFβ inhibition with immune checkpoint blockade may increase tumor CD8+ T-cell infiltration and induce complete and durable responses in models of immune-excluded urothelial and colon cancer.42 43
Heterogeneity of immune cell composition in the tumor microenvironment might also help to explain the failure to elicit an inflammatory response via TGFβ inhibition. Infiltrating FoxP3+ regulatory T cells (Tregs) in tumor tissues are considered a major obstacle to clinical efficacy of tumor immunotherapy and associated with a poor prognosis.44 45 The ability of galunisertib to block the suppressive activity of human Tregs has been demonstrated in vitro46 but has not yet been observed clinically. Additional studies examining tumor microenvironment characteristics may be warranted to increase the efficiency of PD-1 immunotherapy and improve the prognosis of pancreatic cancer.47
In conclusion, this study established galunisertib 150 mg two times per day on days 1–14 of a 28-day cycle plus durvalumab 1500 mg Q4W as the RP2D for future clinical exploration. No unexpected safety signals were observed with the use of combination therapy. The combination of galunisertib with durvalumab showed a clinical activity in line with other recent studies in similar populations of patients with different combination strategies, including immune checkpoint inhibitors. Given the aggressive nature of pancreatic cancer, and the advanced stages of the study population, studying this novel immunotherapy combination in patients in an early line of treatment and selected for higher levels of macrophage-enriching cytokines may be a more suitable approach. The tolerability of galunisertib in combination with durvalumab could also lend itself to combination of with other treatments in future trials.
Acknowledgments
Medical writing assistance was provided by Samantha Forster of ProScribe - Envision Pharma Group and was funded by Eli Lilly and Company. ProScribe’s services complied with international guidelines for Good Publication Practice (GPP3). The authors would also like to thank Shuaicheng (Freeman) Wang of BioStat Solutions Inc for his help with the data analysis for this study. Work in the unit of DM was partially supported by the Associazione Italiana per la Ricerca sul Cancro (AIRC) Investigator Grant n°23719 and 5x1000 Grant n°12182, by the Italian Ministry of Health Ricerca Finalizzata 2016 GR-2016- 02361134 grant, and by the patients' associations 'Nastro Viola' and 'Voglio il Massimo' donations.
Footnotes
Contributors: AMV, KAB, and MCL were involved in the study design. Authors DM, AH, EC, AMV, EB, KAB, and EA were involved in the analysis and interpretation of data, and all authors critically revised the manuscript. All authors agree to be responsible for all aspects of the work and read and approved the final manuscript to be published.
Funding: This study was funded by Eli Lilly and Company.
Competing interests: DM has received research funding from Celgene, Incyte, and Shire, and has a consulting role with Baxter, Eli Lilly and Company, Incyte, and Shire. D-YO has received research funding from Array, AstraZeneca, Eli Lilly and Company, and Novartis, and has a consulting/advisory role with ASLAN, AstraZeneca, Bayer, Celgene, Genentech/Roche, Halozyme, Merck Serono, Novartis, Taiho, and Zymeworks. AH has received travel and accommodation expenses from Eli Lilly and Company. EC has received research funding from AbbVie, Amcure, Amgen, AstraZeneca, BeiGene, BMS, Boehringer-Ingelheim, CytomX, Eli Lilly and Company, H3, Incyte, Kura, LOXO, Macrogenics, Menarini, Merck, Merck Serono, Merus, Millennium Pharmaceuticals, Nanobiotix Janssen, Nektar, Novartis, Pfizer, PharmaMar, Principia Bayer, PsiOxus Therapeutics, PUMA, Rigontec, Roche/Genentech, Sanofi, Tahio, Tesaro; has a consulting/advisory role with AbbVie, Amcure, AstraZeneca, Boehringer-Ingelheim, Celgene, Cerulean Pharma, EUSA, GLG, Guidepoint Global, Janssen-Cilag, Nanobiotix Janssen, Novartis, Pfizer, Pierre Pharma, PsiOxus Therapeutics, Roche/Genentech, Seattle Genetics, Servier; is employed by HM Hospitals Group and START; has shares in HM Hospitals Group, International Cancer Consultants, Oncoart Associated, and START; and is president and founder of NPO Foundation Intheos (Investigational Therapeutics in Oncological Sciences). AMV has participated in clinical trials funded by Bristol Myers Squibb, Eli Lilly and Company, GlaxoSmithKline, Silenseed, and Verastem. EB has received honoraria for consultancy from Corcept Therapeutics and Invitae, is on the speaker bureau for Ipsen, and his institution has received research funding from Biontech, Bristol-Myers Squibb, Daiichi Sankyo, Eli Lilly and Company, Helix, Mabvax, Merck, Minneamrita Therapeutics, Pharmacyclics, and Samumed. TM has received honoraria for consultancy from Baxalta, Baxter, Celgene, Genzyme, Roche, Sanofi, Shire Pharmaceuticals, Tesaro, and QED Therapeutics, and has received travel/accommodation compensation from Bayer, H3 Biomedicine, Merck, and Sanofi. VM and CZ have no conflicts of interest to disclose. YZ, IG, MM, LG, STE, and EA are employees and stock holders of Eli Lilly and Company. KAB was an employee of Eli Lilly and Company at the time this research was conducted and is a stock holder of Eli Lilly and Company and a current employee of Taiho Oncology. MCL is a current employee and stock holder of AstraZeneca. SCG was an employee of Eli Lilly and Company at the time this research was conducted and is a stock holder of Eli Lilly and Company. RG-C declares having provided scientific advice and/or received honoraria from AAA, Advanz Pharma, Amgen, Bayer, BMS, Eli Lilly and Company, HMP, Ipsen, Merck, Midatech Pharma, MSD, Novartis, PharmaMar, Pfizer, Roche, and Sanofi, and has received research support from Pfizer and BMS. Work in the unit of DM was partially supported by the Associazione Italiana per la Ricerca sul Cancro (AIRC) Investigator Grant n°23719 and 5x1000 Grant n°12182, by the Italian Ministry of Health Ricerca Finalizzata 2016 GR-2016- 02361134 grant, and by the patients associations 'Nastro Viola' and 'Voglio il Massimo' donations.
Patient consent for publication: Not required.
Ethics approval: The study was conducted in compliance with the Declaration of Helsinki, International Council for Harmonisation Guidelines for Good Clinical Practice, and applicable local regulations. The protocol was approved by the ethics committees of all participating centers, and all patients provided written informed consent before study entry.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: Data are available upon reasonable request. Lilly provides access to all individual participant data collected during the trial, after anonymization, with the exception of pharmacokinetic or genetic data. Data are available to request 6 months after the indication studied has been approved in the USA and EU and after primary publication acceptance, whichever is later. No expiration date of data requests is currently set once data are made available. Access is provided after a proposal has been approved by an independent review committee identified for this purpose and after receipt of a signed data sharing agreement. Data and documents, including the study protocol, statistical analysis plan, clinical study report, blank or annotated case report forms, will be provided in a secure data sharing environment. For details on submitting a request, see the instructions provided at www.vivli.org.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
References
- 1.Siegel RL, Miller KD, Jemal A. Cancer statistics, 2020. CA Cancer J Clin 2020;70:7–30. 10.3322/caac.21590 [DOI] [PubMed] [Google Scholar]
- 2.Rawla P, Sunkara T, Gaduputi V. Epidemiology of pancreatic cancer: global trends, etiology and risk factors. World J Oncol 2019;10:10–27. 10.14740/wjon1166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Macdonald S, Mair F. Tackling cancers of unmet need: the pancreatic cancer pathway. Lancet Gastroenterol Hepatol 2016;1:266–7. 10.1016/S2468-1253(16)30113-3 [DOI] [PubMed] [Google Scholar]
- 4.Hilmi M, Bartholin L, Neuzillet C. Immune therapies in pancreatic ductal adenocarcinoma: where are we now? World J Gastroenterol 2018;24:2137–51. 10.3748/wjg.v24.i20.2137 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Oberstein PE, Olive KP. Pancreatic cancer: why is it so hard to treat? Therap Adv Gastroenterol 2013;6:321–37. 10.1177/1756283X13478680 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bailey P, Chang DK, Nones K, et al. Genomic analyses identify molecular subtypes of pancreatic cancer. Nature 2016;531:47–52. 10.1038/nature16965 [DOI] [PubMed] [Google Scholar]
- 7.Massagué J. TGFβ signalling in context. Nat Rev Mol Cell Biol 2012;13:616–30. 10.1038/nrm3434 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pickup M, Novitskiy S, Moses HL. The roles of TGFβ in the tumour microenvironment. Nat Rev Cancer 2013;13:788–99. 10.1038/nrc3603 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Topalian SL, Drake CG, Pardoll DM. Immune checkpoint blockade: a common denominator approach to cancer therapy. Cancer Cell 2015;27:450–61. 10.1016/j.ccell.2015.03.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Henriksen A, Dyhl-Polk A, Chen I, et al. Checkpoint inhibitors in pancreatic cancer. Cancer Treat Rev 2019;78:17–30. 10.1016/j.ctrv.2019.06.005 [DOI] [PubMed] [Google Scholar]
- 11.Royal RE, Levy C, Turner K, et al. Phase 2 trial of single agent ipilimumab (anti-CTLA-4) for locally advanced or metastatic pancreatic adenocarcinoma. J Immunother 2010;33:828–33. 10.1097/CJI.0b013e3181eec14c [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Eso Y, Shimizu T, Takeda H, et al. Microsatellite instability and immune checkpoint inhibitors: toward precision medicine against gastrointestinal and hepatobiliary cancers. J Gastroenterol 2020;55:15–26. 10.1007/s00535-019-01620-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lee V, Murphy A, Le DT, et al. Mismatch repair deficiency and response to immune checkpoint blockade. Oncologist 2016;21:1200–11. 10.1634/theoncologist.2016-0046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Prasad V, Kaestner V, Mailankody S. Cancer drugs approved based on biomarkers and not tumor type-FDA approval of pembrolizumab for mismatch repair-deficient solid cancers. JAMA Oncol 2018;4:157–8. 10.1001/jamaoncol.2017.4182 [DOI] [PubMed] [Google Scholar]
- 15.Bazzichetto C, Conciatori F, Luchini C, et al. From genetic alterations to tumor microenvironment: the Ariadne’s string in pancreatic cancer. Cells 2020;9:309. 10.3390/cells9020309 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sideras K, Braat H, Kwekkeboom J, et al. Role of the immune system in pancreatic cancer progression and immune modulating treatment strategies. Cancer Treat Rev 2014;40:513–22. 10.1016/j.ctrv.2013.11.005 [DOI] [PubMed] [Google Scholar]
- 17.Martinez-Bosch N, Vinaixa J, Navarro P. Immune evasion in pancreatic cancer: from mechanisms to therapy. Cancers (Basel) 2018;10:6. 10.3390/cancers10010006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Principe DR, DeCant B, Mascariñas E, et al. TGFβ signaling in the pancreatic tumor microenvironment promotes fibrosis and immune evasion to facilitate tumorigenesis. Cancer Res 2016;76:2525–39. 10.1158/0008-5472.CAN-15-1293 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kabacaoglu D, Ciecielski KJ, Ruess DA, et al. Immune checkpoint inhibition for pancreatic ductal adenocarcinoma: current limitations and future options. Front Immunol 2018;9:1878. 10.3389/fimmu.2018.01878 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kowal J, Kornete M, Joyce JA. Re-education of macrophages as a therapeutic strategy in cancer. Immunotherapy 2019;11:677–89. 10.2217/imt-2018-0156 [DOI] [PubMed] [Google Scholar]
- 21.Herbertz S, Sawyer JS, Stauber AJ, et al. Clinical development of galunisertib (LY2157299 monohydrate), a small molecule inhibitor of transforming growth factor-beta signaling pathway. Drug Des Devel Ther 2015;9:4479–99. 10.2147/DDDT.S86621 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Melisi D, Garcia-Carbonero R, Macarulla T, et al. Galunisertib plus gemcitabine vs. gemcitabine for first-line treatment of patients with unresectable pancreatic cancer. Br J Cancer 2018;119:1208–14. 10.1038/s41416-018-0246-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gueorguieva I, Tabernero J, Melisi D, et al. Population pharmacokinetics and exposure-overall survival analysis of the transforming growth factor-β inhibitor galunisertib in patients with pancreatic cancer. Cancer Chemother Pharmacol 2019;84:1003–15. 10.1007/s00280-019-03931-1 [DOI] [PubMed] [Google Scholar]
- 24.Principe DR, Park A, Dorman MJ, et al. TGFβ blockade augments PD-1 inhibition to promote T-cell-mediated regression of pancreatic cancer. Mol Cancer Ther 2019;18:613–20. 10.1158/1535-7163.MCT-18-0850 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sow HS, Ren J, Camps M, et al. Combined inhibition of TGF-β signaling and the PD-L1 immune checkpoint is differentially effective in tumor models. Cells 2019;8:320. 10.3390/cells8040320 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gueorguieva I, Cleverly AL, Stauber A, et al. Defining a therapeutic window for the novel TGF-β inhibitor LY2157299 monohydrate based on a pharmacokinetic/pharmacodynamic model. Br J Clin Pharmacol 2014;77:796–807. 10.1111/bcp.12256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Stauber A, Credille K, Truex L. Nonclinical safety evaluation of a transforming growth factor β receptor I kinase inhibitor in Fischer 344 rats and beagle dogs. J Clin Pract 2014;4:196. [Google Scholar]
- 28.Siu LL, Even C, Mesía R, et al. Safety and efficacy of durvalumab with or without tremelimumab in patients with PD-L1-low/negative recurrent or metastatic HNSCC: the phase 2 CONDOR randomized clinical trial. JAMA Oncol 2019;5:195–203. 10.1001/jamaoncol.2018.4628 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Brandes AA, Carpentier AF, Kesari S, et al. A phase II randomized study of galunisertib monotherapy or galunisertib plus lomustine compared with lomustine monotherapy in patients with recurrent glioblastoma. Neuro Oncol 2016;18:1146–56. 10.1093/neuonc/now009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kovacs RJ, Maldonado G, Azaro A, et al. Cardiac safety of TGF-β receptor I kinase inhibitor LY2157299 monohydrate in cancer patients in a first-in-human dose study. Cardiovasc Toxicol 2015;15:309–23. 10.1007/s12012-014-9297-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Baverel PG, Dubois VFS, Jin CY, et al. Population pharmacokinetics of durvalumab in cancer patients and association with longitudinal biomarkers of disease status. Clin Pharmacol Ther 2018;103:631–42. 10.1002/cpt.982 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.O’Reilly EM, D-Y O, Dhani N, et al. Durvalumab with or without tremelimumab for patients with metastatic pancreatic ductal adenocarcinoma: a phase 2 randomized clinical trial. JAMA Oncol 2019;5:1431–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Overman M, Javle M, Davis RE, et al. Randomized phase II study of the Bruton tyrosine kinase inhibitor acalabrutinib, alone or with pembrolizumab in patients with advanced pancreatic cancer. J Immunother Cancer 2020;8:e000587. 10.1136/jitc-2020-000587 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mahalingam D, Wilkinson GA, Eng KH, et al. Pembrolizumab in combination with the oncolytic virus pelareorep and chemotherapy in patients with advanced pancreatic adenocarcinoma: a phase Ib study. Clin Cancer Res 2020;26:71–81. 10.1158/1078-0432.CCR-19-2078 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Singhi AD, George B, Greenbowe JR, et al. Real-time targeted genome profile analysis of pancreatic ductal adenocarcinomas identifies genetic alterations that might be targeted with existing drugs or used as biomarkers. Gastroenterology 2019;156:2242–53. 10.1053/j.gastro.2019.02.037 [DOI] [PubMed] [Google Scholar]
- 36.Bernard V, Kim DU, San Lucas FA, et al. Circulating nucleic acids are associated with outcomes of patients with pancreatic cancer. Gastroenterology 2019;156:108–18. 10.1053/j.gastro.2018.09.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Macherla S, Laks S, Naqash AR, et al. Emerging role of immune checkpoint blockade in pancreatic cancer. Int J Mol Sci 2018;19:3505. 10.3390/ijms19113505 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Signorelli D, Giannatempo P, Grazia G, et al. Patients selection for immunotherapy in solid tumors: overcome the naïve vision of a single biomarker. Biomed Res Int 2019;2019. 10.1155/2019/9056417 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Melisi D, Garcia-Carbonero R, Macarulla T, et al. TGFβ receptor inhibitor galunisertib is linked to inflammation- and remodeling-related proteins in patients with pancreatic cancer. Cancer Chemother Pharmacol 2019;83:975–91. 10.1007/s00280-019-03807-4 [DOI] [PubMed] [Google Scholar]
- 40.Carstens JL, Correa de Sampaio P, Yang D, et al. Spatial computation of intratumoral T cells correlates with survival of patients with pancreatic cancer. Nat Commun 2017;8:15095. 10.1038/ncomms15095 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Knudsen ES, Vail P, Balaji U, et al. Stratification of pancreatic ductal adenocarcinoma: combinatorial genetic, stromal, and immunologic markers. Clin Cancer Res 2017;23:4429–40. 10.1158/1078-0432.CCR-17-0162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Mariathasan S, Turley SJ, Nickles D, et al. TGFβ attenuates tumour response to PD-L1 blockade by contributing to exclusion of T cells. Nature 2018;554:544–8. 10.1038/nature25501 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Tauriello DVF, Palomo-Ponce S, Stork D, et al. TGFβ drives immune evasion in genetically reconstituted colon cancer metastasis. Nature 2018;554:538–43. 10.1038/nature25492 [DOI] [PubMed] [Google Scholar]
- 44.Pu N, Zhao G, Yin H, et al. CD25 and TGF-β blockade based on predictive integrated immune ratio inhibits tumor growth in pancreatic cancer. J Transl Med 2018;16:294. 10.1186/s12967-018-1673-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ohue Y, Nishikawa H. Regulatory T (Treg) cells in cancer: can Treg cells be a new therapeutic target? Cancer Sci 2019;110:2080–9. 10.1111/cas.14069 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Holmgaard RB, Schaer DA, Li Y, et al. Targeting the TGFβ pathway with galunisertib, a TGFβRI small molecule inhibitor, promotes anti-tumor immunity leading to durable, complete responses, as monotherapy and in combination with checkpoint blockade. J Immunother Cancer 2018;6:47. 10.1186/s40425-018-0356-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Pu N, Lou W, Yu J. PD-1 immunotherapy in pancreatic cancer: current status. J Pancreatol 2019;2:6–10. 10.1097/JP9.0000000000000010 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
jitc-2020-002068supp001.pdf (852.7KB, pdf)