Abstract
Agitation and delirium are common reasons for older adults to seek care in the emergency department (ED). Providing care for this population in the ED setting can be challenging for emergency physicians. There are several knowledge translation gaps in how to best screen older adults for these conditions and how to manage them. A working group of subject-matter experts convened to develop an easy-to-use, point-of-care tool to assist emergency physicians in the care of these patients. The tool is designed to serve as a resource to address the knowledge translation and implementation gaps that exist in the field. The purpose of this article is present and explain the Assess, Diagnose, Evaluate, Prevent, and Treat tool. Participants were identified with expertise in emergency medicine, geriatric emergency medicine, geriatrics, and psychiatry. Background literature reviews were performed before the in-person meeting in key areas: delirium, dementia, and agitation in older adults. Participants worked electronically before and after an in-person meeting to finalize development of the tool in 2017. Subsequent work was performed electronically in the following months and additional expert review sought. EDs are an important point of care for older adults. Behavioral changes in older adults can be a manifestation of underlying medical problems, mental health concerns, medication adverse effects, substance abuse, or dementia. Five core principles were identified by the group that can help ensure adequate and thorough care for older adults with agitation or delirium: assess, diagnose, evaluate, prevent, and treat. This article provides background for and explains the importance of these principles related to the care of older adults with agitation. It is important for emergency physicians to recognize the spectrum of underlying causes of behavioral changes and have the tools to screen older adults for those causes, and methods to treat the underlying causes and ameliorate their symptoms.
INTRODUCTION
Older adults, defined as aged 65 years and older, frequently present to the emergency department (ED) for or with agitation, confusion, or behavioral changes.1 The number of older patients who present to the ED is expected to increase as the population ages. In older patients presenting with behavioral changes, there is more often an underlying medical condition or trigger causing the acute change than in younger patients. It is rare for patients in this age group to present with a new-onset primary psychotic disorder or new-onset schizophrenia, so a medical cause should almost always be assumed until proven otherwise. Furthermore, the signs and symptoms of these patients’ presentation may be subtle or atypical, so the evaluation should be thorough. Management should focus on treatment of the underlying disorder, proactive measures to prevent worsening symptoms, and treatment of agitation, with a cautious awareness of the high risk of potential medication adverse effects. Delirium is frequently underrecognized in the ED2,3 and is an independent predictor of 6-month mortality.4
The care of agitated patients in the ED can be challenging. The presence of agitation or behavioral changes is often a clue to underlying delirium, but the diagnosis of delirium is often not formally made in the ED setting.5 Delirium is an acute change in mental status, with waxing and waning symptoms, that can present with hyperactive, hypoactive, or mixed symptoms. Its presentation can be subtle or can be confounded by other symptoms or disorders, such as strokes, sepsis, adverse drug reactions, or intoxication. A greater understanding and recognition of delirium may help clinicians better care for patients and prevent symptom progression. In addition, when patients are agitated or delirious, clinicians often use pharmacologic measures such as antipsychotics or benzodiazepines for symptom control. However, these medications have significant potential complications, so nonpharmacologic measures should be used first when possible.
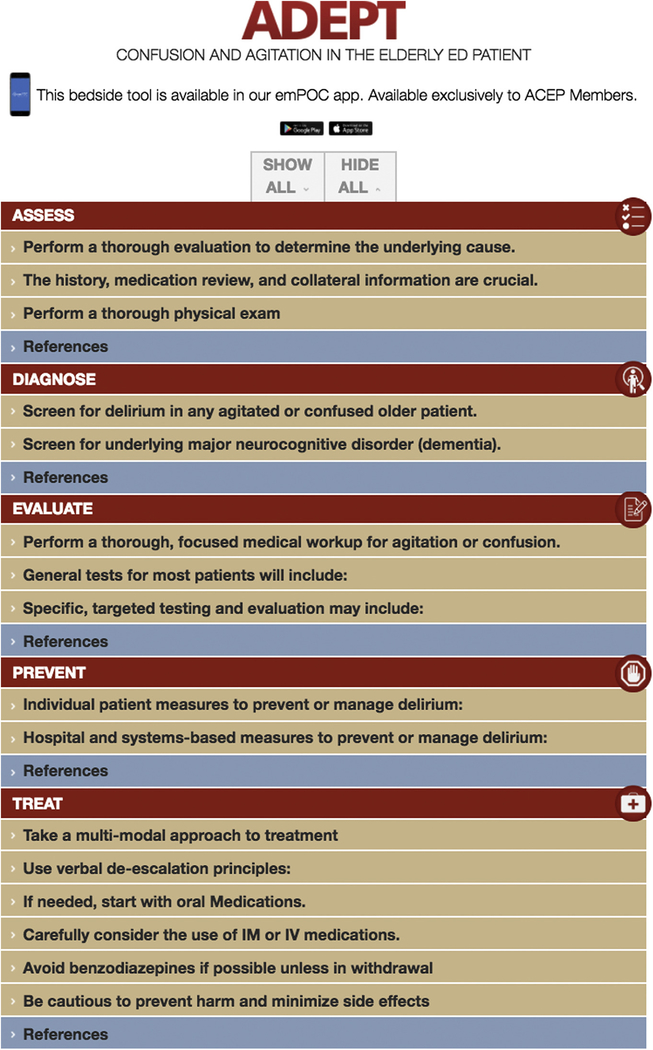
To address the knowledge translation and implementation gaps that exist in the field, the Coalition on Psychiatric Emergencies convened an expert panel on this topic in 2017. These experts were tasked with creating an easy-to-use reference tool for emergency physicians, the product of which was the Assess, Diagnose, Evaluate, Prevent, and Treat (ADEPT) tool (Figure 1).6 The ADEPT acronym stands for 5 core principles that can help ensure adequate and thorough care for older adults with agitation or delirium: assess, diagnose, evaluate, prevent, and treat. ADEPT is an open-access Web-based tool and is available on the American College of Emergency Physicians (ACEP) emPOC mobile device app intended for use by clinicians on shift. This article, by presenting the background and supporting evidence for each aspect of the ADEPT tool, will provide a recommended approach to the screening, diagnosis, and treatment of patients with agitation and delirium.
Figure 1.
ADEPT tool.
The Coalition on Psychiatric Emergencies includes more than a dozen professional organizations and patient advocacy groups. The organization was founded in December 2015 with the mission of unifying various nonprofit mental health advocacy groups in the United States. In partnership with the ACEP, the Coalition on Psychiatric Emergencies steering committee created a working group to design the geriatrics agitation tool. The working group was composed of 6 academic and community physicians with expertise in the areas of geriatric emergency medicine, delirium, agitation pharmacology, geriatrics, and critical care. Through an iterative process of literature review, development, review, revision, and consensus building, the working group created the ADEPT tool. An initial, broad literature review was performed on each of the aspects of the ADEPT tool. Individuals with expertise in each respective area were responsible for developing initial recommendations for each of the 5 components of ADEPT. As a group, their recommendations were reviewed, honed, and revised according to the literature. Feedback was also sought from the ACEP Emergency Medicine Clinical Practice Committee, members and leaders of the Academy of Geriatric Emergency Medicine, and an experienced ED pharmacist. The final recommendations were further edited into their succinct version that was then published online as the ADEPT tool.
Each part of the ADEPT tool is explained in further detail here. In older adults with undifferentiated agitation or confusion, it is important to recognize and establish that there has been a change, diagnose the condition, and determine the underlying causes if possible.7
ASSESS
First is “Assess.” Once life threats and immediately treatable conditions such as hypoxia, hypoglycemia, and ST-segment elevation myocardial infarction have been ruled out and patient and staff safety are ensured, the next step is to determine whether there has been a change from baseline and the time course.8 First establish the patient’s baseline mental status and the time course of any changes, a process that will typically require contacting a family member or caregiver.
Infections, neurologic disorders, and metabolic or electrolyte disorder are 3 of the most common causes of acute alterations in mental status among older patients.9 Adverse medication effects are another common cause. A list of medications that are high risk for causing confusion, altered mental status, or delirium is shown in Table 1.
Table 1.
Common and important precipitants of or contributors to delirium, agitation, confusion, or altered mental status.
| Category | Examples |
|---|---|
| Readily reversible causes | Hypoxia, hypercarbia, hypoglycemia, hyperglycemia, hyponatremia, hyperkalemia |
| Infection | Urinary tract infection, pneumonia, intra-abdominal infections, meningitis/encephalitis, sepsis from other source |
| Neurologic | Transient ischemic attack, stroke, intracranial hemorrhage, intracranial mass |
| Medication-induced adverse effects, intentional or unintentional overdose, supratherapeutic levels because of renal or liver disease | Anticholinergic medications (including tricyclic antidepressants, antihistamines, muscle relaxants, promethazine, typical antipsychotics, sedative hypnotics (benzodiazepines, zolpidem), corticosteroids, polypharmacy (considered ≥4 medications), salicylate toxicity |
| Toxicologic | Intoxication with alcohol or substance use, alcohol or benzodiazepine withdrawal |
| Metabolic | Hyper- or hypoglycemia, hyper- or hyponatremia, dehydration, acute kidney injury, uremia, diabetic ketoacidosis |
| Cardiopulmonary | Acute coronary syndrome, dissection, hypoxia, hypotension, anemia |
| Environmental factors | New or unfamiliar environment, lack of sleep, lack of hearing or vision aids |
| Other factors | Pain, urinary retention |
The patient should be given a gown to wear and examined for signs of trauma or infection, including checking for sacral ulcers. Bruising or abrasions could be a sign of accidental trauma from falls, but clinicians should also be aware of the physical signs of potential nonaccidental trauma or neglect, which are often underrecognized in older adults.10,11 The physical examination should assess for signs of stroke, intracranial hemorrhage, or subclinical seizures, all of which are less common but potentially life-threatening causes of agitation or altered mental status.
DIAGNOSE
Second is “Diagnose.” Delirium is a common syndrome that presents with confusion, agitation, or both in older patients. Older patients who present with hallucinations or altered sensorium are more likely to have delirium or, less commonly, dementia-related psychosis, rather than acute psychotic break. New-onset psychosis or schizophrenia is rare in this population.12
Despite delirium’s prevalence among geriatric ED patients, emergency clinicians formally diagnose it in less than 20% of delirious patients.2,3 Underrecognition of delirium may result in adverse outcomes, including higher mortality.4 Distinguishing between delirium, dementia, and primary psychiatric conditions can be challenging in older adults because neuropsychiatric symptoms, such as depression, agitation, and psychotic symptoms, are common in patients with dementia.13 In addition, patients with baseline dementia are at increased risk of developing superimposed delirium during an acute illness.
The hallmarks of delirium include acute onset, waxing and waning symptoms, inattention (eg, unable to recite the months of the year or days of the week backwards), change in cognition (new memory deficit, disorientation, perceptual disturbance, or disorganized thinking), or altered level of awareness (reduced orientation to environment such as somnolence or agitation).14
Delirium can be subcategorized into 3 main psychomotor types. Hyperactive delirium is characterized by agitation, increased psychomotor activity, and heightened level of arousal. It is the most recognizable type but accounts for less than 10% of delirium observed in the ED.15 Hypoactive delirium is by far the most common type, accounting for approximately 90%.1 It is characterized by somnolence and psychomotor retardation. It is more likely to be missed by the clinician because patients may be somnolent, quiet, and unlikely to draw attention to themselves. Hypoactive delirium is associated with the highest mortality rate.1 Finally, mixed delirium involves alternating hypoactive and hyperactive states. Risk factors for delirium include a history of neurocognitive disorder (dementia), previous episodes of delirium, increased age, vision or hearing impairment, previous stroke, impaired functional status, nursing facility residence, or home health aide for activities of daily living.
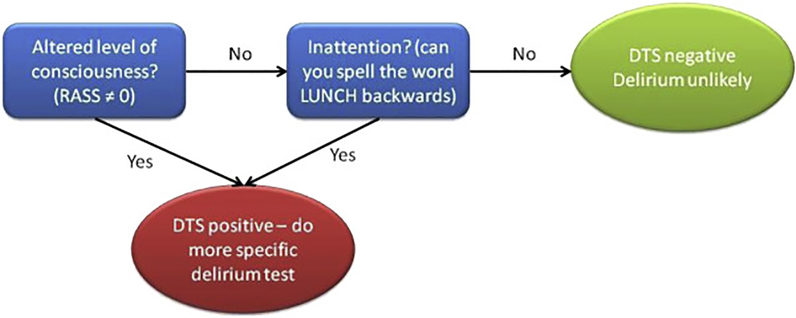
There are numerous brief tools that can be used to diagnose delirium in the ED. The Delirium Triage Screen (Figure 2) can be rapidly administered, does not require collateral information, and is very sensitive, so it functions well as a screening tool.16 It consists of a formal assessment of the level of arousal (normal, sedated, or agitated) and a test of attention. A positive Delirium Triage Screen result should trigger confirmation with a test that is more specific, such as the Confusion Assessment Method or Brief Confusion Assessment Method (Table 2).16–18 A patient is delirious if he or she has acute onset or fluctuating course, inattention, and either disorganized thinking or altered level of consciousness.
Figure 2.
Delirium Triage Screen.16 RASS, Richmond Agitation-Sedation Scale; DTS, Delirium Triage Screen.
Table 2.
Comparison of brief delirium assessment tools.
When family or caregivers are present, key questions to help differentiate between delirium, dementia, and a psychiatric condition include the following (Table 3):
Table 3.
Distinguishing features between delirium, dementia, and psychosis.
| Characteristic | Delirium | Dementia | Psychosis |
|---|---|---|---|
| Onset | Acute | Gradual | Variable |
| Course | Fluctuating | Progressive* | Chronic |
| Diminished level of consciousness | May be present (hypoactive/mixed delirium) | Absent | Absent |
| Orientation | Fluctuating | Impaired | Normal |
| Duration | Hours to months | Months to years | Months to years |
| Hallucinations | Common | Rare until end stage | Common |
| Attention | Impaired | Preserved until end stage | May be impaired |
| Sleep-wake pattern | Disrupted | Normal or fragmented | Variable |
Exception: fluctuations in cognition are present in Lewy body dementia.23
Previous diagnosis of dementia or psychiatric disease. In the absence of a preexisting diagnosis of dementia or psychiatric illness, hallucinations or behavioral disturbances should raise concern for delirium.
Presence of changes in the patient’s cognition or behavior. If changes are present, obtain information on the onset, duration, and fluctuations in symptoms. Delirium is characterized by acute onset. Fluctuations are a key feature of both delirium and Lewy body dementia.
Presence of hallucinations. With the exception of Lewy body dementia, hallucinations rarely occur in dementia until late stages of the disease.
Sleep/wake disturbances.
Patients with delirium or suspected delirium should undergo an evaluation to assess for underlying precipitating causes and receive nonpharmacologic measures to limit the duration and severity of delirium.
Nondelirious patients presenting with confusion, agitation, or hallucinations should be screened for dementia and depression. Although primary psychotic disorders are rare in older adults, with prevalence less than 1%,19 16% to 23% of older adults develop psychotic symptoms primarily related to advanced dementia.20 There are a number of brief screening tools that can be used to assess for underlying major cognitive disorder, such as the Mini-Cog,21 brief Alzheimer’s Screen, Short Blessed Test, Ottawa 3DY, and caregiver-completed AD8.17,22 Depressed older patients may present with symptoms mimicking delirium, including psychomotor retardation or agitation, decreased concentration, and sleep disturbances.23 Approximately 6% of older adults have major depressive disorder, but the prevalence is much higher in patients with comorbid medical conditions, including cognitive impairment. Older adults can be screened for depression with very brief screening tests, such as the Patient Health Questionnaire–2 or Emergency Department Depression Screening Instrument.24,25 A positive screen result for depression should prompt subsequent questions on suicidal thoughts and attempts because suicidal older patients are more likely to use lethal means.23
EVALUATE
Third is “Evaluate.” Although the “Diagnose” step focuses on determining whether delirium is present, the “Evaluate” step focuses on evaluation for underlying causes (Table 1).26 The evaluation should be directed by a focused history and careful physical examination.
Infections are the most common cause of delirium identified in ED studies, responsible for 30% to 40% of cases, followed by acute neurologic disorders such as ischemic stroke, intracranial hemorrhage, or intracranial mass.9,27 Adverse effects of medications commonly cause delirium and are estimated to be responsible for 12% to 39% of delirium across medical settings.28 Accordingly, it is critical that the emergency clinician perform a medication review to identify recent medication changes and use of medications at high risk of causing delirium (Table 1). Delirium is also frequently multifactorial.29 For example, a patient with a urinary tract infection may experience delirium from the infection, but other compounding factors such as dehydration, pain, new antibiotic medications, and change in environment can also contribute.
Although every evaluation should be tailored to the patient, most patients should receive an ECG, CBC count, metabolic panel, point-of-care glucose level test, and a urinalysis with culture. Although urinary tract infections are a common delirium precipitant, asymptomatic bacteriuria is also very common in geriatric populations. Among community-dwelling older adults, 5% of men and 6% to 10% of women have asymptomatic bacteriuria. The rates of asymptomatic bacteriuria are higher among institutionalized older adults, with 15% to 35% of men and 25% to 50% of women having asymptomatic bacteriuria.30 Pyuria with or without bacteriuria is also common in asymptomatic older adults, particularly those with chronic incontinence.30 Emergency clinicians should be wary of premature diagnostic closure, incorrectly attributing behavioral changes to a urinary tract infection when the evidence for this condition is sparse.
Additional tests may be warranted according to the history or physical examination and should be directed according to symptoms, history, and presentation. Routine computed tomography of the brain is low yield overall but should be performed for patients with focal neurologic deficits, fall, or head trauma, or decreased level of consciousness, and should be considered in patients receiving anticoagulation.31–33
PREVENT
The fourth is “Prevent.” Most EDs are busy, bright, noisy, and potentially deliriogenic environments, especially for older patients. However, there are measures that can be undertaken for individual patients to prevent the development of delirium, to prevent its progression, and to mitigate its symptoms.34,35 These include treating the underlying condition and managing pain,36 ideally with nonsedating, nonopioid medications if possible. Treatment of other bothersome symptoms such as nausea, vomiting, and constipation can be helpful. Unless contraindicated, a patient’s home medications should be administered on schedule to prevent exacerbation of baseline medical problems.
Medications that can cause delirium should be avoided (Table 1). Normalize the patient’s daily function by providing hydration, food (unless contraindicated), access and assistance to toileting, mobility assistance or aids, and hearing-assistive devices. Limit unnecessary disruptions. Unless medically necessary, things that tether the patient to the bed should be avoided, including blood pressure cuffs, monitor leads, continuous intravenous infusions, and bladder catheters. Greater numbers of restraints or tethers, immobilization, and use of bladder catheters are associated with higher rates of delirium.29,37
Although the measures just discussed can be accomplished in any ED, other measures require hospital- or systems-based organization and planning. Providing large-font clocks and other visual cues about the date and location can help self-orientation.38 In addition, promoting and creating a culture that encourages family members and caregivers who demonstrate a calming presence to remain at the bedside can be helpful.29 If feasible, volunteers can be trained to help redirect and calm patients.39 Patients with delirium are at higher risk for falls,40 so measures should be taken to help prevent injury while still promoting mobility, if possible. Some measures include low beds, getting out of bed to chairs, physical therapy, nonslip floors or socks, and 1:1 sitters.41,42
An ED length of stay of greater than 10 hours has been demonstrated to double the risk for incident delirium.43 Therefore, systems measures and protocols that reduce ED length of stay and avoid boarding patients in hallways should be considered for patients at risk of delirium. Prioritizing the transfer of older or frail patients to floor beds when they become available is one potential measure. In addition, it is important that the ED clinicians and nursing staff communicate the presence of delirium or agitation to the inpatient team. When the diagnosis of delirium is not made in the ED, it is also more likely to be missed by the inpatient teams,1 so it is important that the diagnosis be communicated explicitly.
TREAT
The fifth is “Treat.” The overall goal for treatment of delirium in the ED is to identify and address the underlying cause while avoiding actions or inactions that may worsen delirium. Following the preventive steps outlined in this review will assist with these goals. Some patients may require additional interventions or medications to successfully and safely manage their agitation.44
If the patient is agitated, it is imperative to calm and protect him or her and staff, and to allow the patient to participate in care to whatever extent is possible. Nonpharmacologic interventions such as verbal de-escalation, distraction, and reassurance can be used with assistance from sitters, family, or staff.45–47 Successful de-escalation helps the patient regain control without need for further treatment45,48 and may even be effective in patients with cognitive deficits such as dementia.49 A video recording message of family members can also help calm and de-escalate agitated older patients.50 Medications may be needed if the above measures fail. However, if at all possible, physical restraints should be avoided because they can lead to injuries.51
If nonpharmacologic management and verbal de-escalation are unsuccessful, pharmacologic interventions may be necessary. It is important to select medications carefully, dose them appropriately, and reassess their effects frequently. All available antipsychotics and benzodiazepines are listed as potentially inappropriate by the Beers criteria, and even at low doses, these medications may have increased adverse effects such as prolonged sedation or paradoxic agitation (with benzodiazepines) in older patients.52,53 In addition, all antipsychotics have a Food and Drug Administration black-box warning that they are not approved for dementia-related psychosis because of an increased mortality risk in older patients with dementia. Although it is unclear how these medications increase mortality in this population,54 antipsychotics should be used with caution in patients with a history of dementia. However, many patients are prescribed antipsychotics long term and may need them while in the ED.
When medications are used for agitated delirium in older patients, the goal should not be sedation, but rather sufficient treatment for safe symptom management.55,56 If medication is required, the recommendations are similar to those for nongeriatric patients, although lower doses should be used (Table 4). Although the few existing high-quality studies have not noted a difference between low-dose haloperidol, olanzapine, or risperidone for the pharmacologic treatment of delirium in hospitalized patients,57 the best current consensus evidence is for the use of low-dose olanzapine or risperidone.58,59 Olanzapine and risperidone have minimal effects on the QT interval, but can be associated with other adverse effects, such as orthostatic hypotension.60 Clinicians should be cautious in regard to geriatric patients who may be receiving multiple QT-interval-prolonging medications and should consider an ECG for QT-interval evaluation before administration. The oral route of administration is preferred because of fewer adverse effects.61 Although antipsychotics can help manage symptoms of delirium or agitation, meta-analyses do not demonstrate any benefit in terms of outcomes such as symptom duration, severity, hospital length of stay, disposition location, or mortality.29,62–66
Table 4.
Summary of low-, intermediate-, and high-risk interventions, as well as risks or contraindications of certain medications, and interventions to avoid.
| Intervention Risk Category | Intervention Details |
|---|---|
| Low-risk interventions or activities: for all patients |
Treat underlying conditions and symptoms, restart home medications if possible. Follow prevention steps. Transfer to hospital-style bed or chair/recliner instead of gurney, which limits mobility/independence and may increase falls risk. Verbal de-escalation if actively agitated. |
| Medium-risk interventions: for moderate agitation or patient at risk of harming self or staff | Step 1: PO medications. If the patient is prescribed an antipsychotic at home, administer this. Other options include the following: Risperidone ≤1 mg. Caution in frail or volume-depleted patients; may cause orthostatic hypotension. Olanzapine 2.5–5 mg. Contraindications/risks: Caution in intoxicated or volume-depleted patients; may cause orthostatic hypotension or sedation. Quetiapine 25–50 mg at night. May cause orthostatic hypotension and somnolence. Haloperidol 1–2 mg PO. May have more extrapyramidal adverse effects than the atypical antipsychotics. |
| Step 2: IM or IV medications if patients are not cooperative with PO medications or are at risk of harming themselves or staff: Ziprasidone10–20 mg IM. Caution in uncontrolled heart failure or cardiac disease, intoxicated patients, or volume-depleted/orthostatic patients. Olanzapine 2.5–5 mg IM. Caution in intoxicated or volume-depleted patients; may cause orthostatic hypotension or sedation. Haloperidol 0.5–1 mg IM. Higher risk for extrapyramidal adverse effects than the atypical antipsychotics. Higher risk with IV, so IM is preferred. Can redose if needed, but avoid doses of 5–10 mg haloperidol because it may cause prolonged effects/sedation, EPS, or other adverse effects. Use caution or avoid IV haloperidol because of adverse effects. | |
| High-risk interventions | Benzodiazepines should be avoided if possible because they may cause prolonged sedation, paradoxic agitation, or worsening of delirium. If they are used, low doses such as 0.5 mg lorazepam should be given rather than the more common 2 mg used in younger patients. However, if a patient is receiving benzodiazepines long term, his or her home medication should be continued to prevent precipitating withdrawal. Physical restraints should be avoided if at all possible because patients can become injured, and their use precludes mobility. |
| Interventions to avoid | Diphenhydramine is appropriate for treatment of acute allergic reactions or anaphylaxis, but should not be used for agitation because of its sedative and anticholinergic properties. |
PO, Oral; IM, intramuscular; IV, intravenous.
If a patient has a history of long-term benzodiazepine use, do not stop these medications precipitately because it may lead to withdrawal and worsening delirium. Benzodiazepines should be avoided in individuals not already receiving them because there is increased risk of prolonged sedation, paradoxic agitation, and worsening delirium.52,57
Diphenhydramine should not be used for the treatment of older individuals. Its anticholinergic adverse effects can lead to worsening delirium and prolonged sedation.52 There is currently no evidence for or against subdissociative-dose ketamine for agitation in older adults. However, studies of subdissociative ketamine for pain in older adults found that it was effective but limited by adverse effects.67,68 More research is needed into the effects of low-dose ketamine in older adults before this medication can be recommended for routine use in the ED for agitation.
Most patients with delirium in the ED will require admission or observation unless there is a clear, easily reversible underlying cause, they have a caregiver who can monitor them closely, and their symptoms are improving.
In summary, the treatment of delirium and agitation in the ED should focus on identifying and reversing the underlying causes. Nonpharmacologic interventions are preferred because of their negligible risk. Pharmacologic interventions should be used only to preserve the safety of patients and staff. If pharmacologic interventions are necessary, then low doses should be used. Atypical antipsychotics may have a better profile of efficacy to adverse effects.
There are several areas in which current clinical controversies exist and further research is needed. One is the best timing and use of medications for delirium. Although medications such as antipsychotics may help manage symptoms, they do not provide any outcome benefit in terms of hospital or ICU length of stay, disposition, or mortality.29,62–66 Although many authors recommend avoiding antipsychotic medications in all but the most agitated delirious patients, most of the studies were performed on admitted patients, providing little evidence in regard to optimal ED treatment. Another outstanding question is what the minimum, routine evaluation should be for older patients who present with agitation. We have made suggestions here, but there is no widely recognized formal recommendation.
Further work is also needed to identify the best ways to prevent or manage delirium in the ED. There has been significant work done in the inpatient setting, in which interprofessional teams provide multicomponent interventions to help prevent delirium.63,69 To our knowledge, similar studies have not been performed in the ED.
Because of the high morbidity and mortality associated with delirium and because individuals with delirium may have an impaired ability to comprehend and adhere to discharge instructions,70 we recommend admission of most delirious patients to the hospital for continued medical treatment and monitoring. However, the environmental changes associated with hospital admission can precipitate delirium or contribute to its prolongation. Whether there are patients whose care would be optimized through alternatives to hospitalization remains unstudied. Further research is needed in this realm.
Finally, perhaps the largest controversy pertains to optimal delirium screening strategies; in particular, who should be screened and what screening methods should be used. Because delirium is underrecognized in ED patients,2,3 some individuals advocate ED-based screening of older patients for cognitive impairment.71 However, to our knowledge, to date there are no randomized controlled studies examining the effect of routine delirium screening in the ED setting. Benefits of screening include earlier diagnosis of delirium and potential avoidance of inappropriate discharge, which may be associated with increased mortality4; however, the potential risks include false-positive diagnoses, which may result in unnecessary resource use, including hospitalization and the potential for inappropriate treatment with antipsychotic medications.63,72
We have reviewed the ED screening, diagnosis, and treatment of older patients with alterations of mental status, using the ADEPT framework. A freely available electronic version of the tool is available for clinicians and trainees at http://www.acep.org/adept.6 It is designed to be succinct, easily accessible, and used during patient care. In the coming decades, older patients will make up an even greater portion of ED patients. They frequently present with or develop delirium or agitation in the ED. It is therefore important for hospitals to develop protocols and procedures to help reduce the development and severity of agitation and delirium, and for every clinician to be educated and prepared to care for patients with delirium.
Acknowledgments
The authors acknowledge the support of the Coalition on Psychiatric Emergencies as the convening body for the development of the tool and article.
Funding and support: By Annals policy, all authors are required to disclose any and all commercial, financial, and other relationships in any way related to the subject of this article as per ICMJE conflict of interest guidelines (see www.icmje.org). The authors have stated that no such relationships exist. This work was supported by the Allergan Foundation to the Emergency Medicine Foundation.
Footnotes
Supervising editor: David L. Schriger, MD, MPH. Specific detailed information about possible conflict of interest for individual editors is available at https://www.annemergmed.com/editors.
Contributor Information
Christina Shenvi, Department of Emergency Medicine, University of North Carolina, Chapel Hill, NC.
Maura Kennedy, Massachusetts General Hospital Department of Emergency Medicine and Harvard Medical School, Boston, MA.
Charles A. Austin, Department of Internal Medicine, Division of Pulmonary Diseases and Critical Care Medicine, University of North Carolina, Chapel Hill, NC.
Michael P. Wilson, University of Arkansas for Medical Sciences, Department of Emergency Medicine, Little Rock, AR.
Michael Gerardi, Department of Emergency Medicine, Morristown Medical Center, Morristown, NJ, and Coalition on Psychiatric Emergencies.
Sandy Schneider, American College of Emergency Physicians, Irving, TX; Department of Emergency Medicine, John Peter Smith Hospital, Fort Worth, TX; Hofstra Northwell School of Medicine, Hempstead, NY.
REFERENCES
- 1.Han JH, Zimmerman EE, Cutler N, et al. Delirium in older emergency department patients: recognition, risk factors, and psychomotor subtypes. Acad Emerg Med. 2009;16:193–200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hustey FM, Meldon SW. The prevalence and documentation of impaired mental status in elderly emergency department patients. Ann Emerg Med. 2002;39:248–253. [DOI] [PubMed] [Google Scholar]
- 3.LaMantia MA, Messina FC, Hobgood CD, et al. Screening for delirium in the emergency department: a systematic review. Ann Emerg Med. 2014;63:551–560.e2. [DOI] [PubMed] [Google Scholar]
- 4.Kakuma R, du Fort GG, Arsenault L, et al. Delirium in older emergency department patients discharged home: effect on survival. J Am Geriatr Soc. 2003;51:443–450. [DOI] [PubMed] [Google Scholar]
- 5.Barron EA, Holmes J. Delirium within the emergency care setting, occurrence and detection: a systematic review. Emerg Med J. 2013;30:263–268. [DOI] [PubMed] [Google Scholar]
- 6.Shenvi C, Kennedy M, Wilson MP, et al. The ADEPTool. Available at: https://www.acep.org/ADEPT. Published June 18, 2018. Accessed June 26, 2018.
- 7.Rosen T, Connors S, Clark S, et al. Assessment and management of delirium in older adults in the emergency department: literature review to inform development of a novel clinical protocol. Adv Emerg Nurs J. 2015;37:183–196; quiz E3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Brendel RW, Stern TA. Psychotic symptoms in the elderly. Prim Care Companion J Clin Psychiatry. 2005;7:238–241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Aslaner MA, Boz M, Çelik A, et al. Etiologies and delirium rates of elderly ED patients with acutely altered mental status: a multicenter prospective study. Am J Emerg Med. 2017;35:71–76. [DOI] [PubMed] [Google Scholar]
- 10.Wong NZ, Rosen T, Sanchez AM, et al. Imaging findings in elder abuse: a role for radiologists in detection. Can Assoc Radiol J. 2017;68:16–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rosen T, Bloemen EM, LoFaso VM, et al. Emergency department presentations for injuries in older adults independently known to be victims of elder abuse. J Emerg Med. 2016;50:518–526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Targum SD, Abbott JL. Psychoses in the elderly: a spectrum of disorders. J Clin Psychiatry. 1999;60(suppl 8):4–10. [PubMed] [Google Scholar]
- 13.Siafarikas N, Selbaek G, Fladby T, et al. Frequency and subgroups of neuropsychiatric symptoms in mild cognitive impairment and different stages of dementia in Alzheimer’s disease. Int Psychogeriatr. 2018;30:103–113. [DOI] [PubMed] [Google Scholar]
- 14.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-5. 5th ed. Washington, DC: American Psychiatric Association; 2013. [Google Scholar]
- 15.Han JH, Eden S, Shintani A, et al. Delirium in older emergency department patients is an independent predictor of hospital length of stay. Acad Emerg Med. 2011;18:451–457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Han JH, Wilson A, Vasilevskis EE, et al. Diagnosing delirium in older emergency department patients: validity and reliability of the delirium triage screen and the brief confusion assessment method. Ann Emerg Med. 2013;62:457–465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Borson S, Scanlan J, Brush M, et al. The Mini-Cog: a cognitive “vital signs” measure for dementia screening in multi-lingual elderly. Int J Geriatr Psychiatry. 2000;15:1021–1027. [DOI] [PubMed] [Google Scholar]
- 18.Inouye SK, van Dyck CH, Alessi CA, et al. Clarifying confusion: the confusion assessment method. A new method for detection of delirium. Ann Intern Med. 1990;113:941–948. [DOI] [PubMed] [Google Scholar]
- 19.Walsh PG, Currier G, Shah MN, et al. Psychiatric emergency services for the US elderly: 2008 and beyond. Am J Geriatr Psychiatry. 2008;16:706–717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Khouzam HR, Battista MA, Emes R, et al. Psychoses in late life: evaluation and management of disorders seen in primary care. Geriatrics. 2005;60:26–33. [PubMed] [Google Scholar]
- 21.Mini-Cog. Instructions for Administration & Scoring. Available at: http://mini-cog.com/wp-content/uploads/2015/12/Universal-MiniCog-Form-011916.pdf. Accessed June 26, 2018. [DOI] [PubMed]
- 22.Carpenter CR, Bassett ER, Fischer GM, et al. Four sensitive screening tools to detect cognitive dysfunction in geriatric emergency department patients: brief Alzheimer’s Screen, Short Blessed Test, Ottawa 3DY, and the caregiver-completed AD8. Acad Emerg Med. 2011;18:374–384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Piechniczek-Buczek J Psychiatric emergencies in the elderly population. Emerg Med Clin North Am. 2006;24:467–490, viii. [DOI] [PubMed] [Google Scholar]
- 24.Li C, Friedman B, Conwell Y, et al. Validity of the Patient Health Questionnaire 2 (PHQ-2) in identifying major depression in older people. J Am Geriatr Soc. 2007;55:596–602. [DOI] [PubMed] [Google Scholar]
- 25.Fabacher DA, Raccio-Robak N, McErlean MA, et al. Validation of a brief screening tool to detect depression in elderly ED patients. Am J Emerg Med. 2002;20:99–102. [DOI] [PubMed] [Google Scholar]
- 26.Gower L, Gatewood M, Kang C. Emergency department management of delirium in the elderly. West J Emerg Med. 2012;13:194–201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kennedy M, Enander RA, Tadiri SP, et al. Delirium risk prediction, healthcare use and mortality of elderly adults in the emergency department. J Am Geriatr Soc. 2014;62:462–469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Alagiakrishnan K, Wiens CA. An approach to drug induced delirium in the elderly. Postgrad Med J. 2004;80:388–393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Inouye SK, Westendorp RG, Saczynski JS. Delirium in elderly people. Lancet. 2014;383:911–922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rowe TA, Juthani-Mehta M. Diagnosis and management of urinary tract infection in older adults. Infect Dis Clin North Am. 2014;28:75–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lai MMY, Wong Tin Niam DM. Intracranial cause of delirium: computed tomography yield and predictive factors. Intern Med J. 2012;42:422–427. [DOI] [PubMed] [Google Scholar]
- 32.Hardy JE, Brennan N. Computerized tomography of the brain for elderly patients presenting to the emergency department with acute confusion. Emerg Med Australas. 2008;20:420–424. [DOI] [PubMed] [Google Scholar]
- 33.Naughton BJ, Moran M, Ghaly Y, et al. Computed tomography scanning and delirium in elder patients. Acad Emerg Med. 1997;4:1107–1110. [DOI] [PubMed] [Google Scholar]
- 34.Carpenter CR, Bromley M, Caterino JM, et al. Optimal older adult emergency care: introducing multidisciplinary geriatric emergency department guidelines from the American College of Emergency Physicians, American Geriatrics Society, Emergency Nurses Association, and Society for Academic Emergency Me. Acad Emerg Med. 2014;21:806–809. [DOI] [PubMed] [Google Scholar]
- 35.Siddiqi N, Harrison JK, Clegg A, et al. Interventions for preventing delirium in hospitalised non-ICU patients. Cochrane Database Syst Rev. 2016;3:CD005563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Husebo BS, Ballard C, Sandvik R, et al. Efficacy of treating pain to reduce behavioural disturbances in residents of nursing homes with dementia: cluster randomized clinical trial. BMJ. 2011;15:d4065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Inouye SK, Charpentier PA. Precipitating factors for delirium in hospitalized elderly persons. Predictive model and interrelationship with baseline vulnerability. JAMA. 1996;275:852–857. [PubMed] [Google Scholar]
- 38.Kostas T, Zimmerman K, Rudolph J. Improving delirium care: prevention, monitoring, and assessment. Neurohospitalist. 2013;3:194–202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sanon M, Baumlin KM, Kaplan SS, et al. Care and Respect for Elders in Emergencies program: a preliminary report of a volunteer approach to enhance care in the emergency department. J Am Geriatr Soc. 2014;62:365–370. [DOI] [PubMed] [Google Scholar]
- 40.Mazur K, Wilczyński K, Szewieczek J. Geriatric falls in the context of a hospital fall prevention program: delirium, low body mass index, and other risk factors. Clin Interv Aging. 2016;11:1253–1261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hshieh TT, Yue J, Oh E, et al. Effectiveness of multicomponent nonpharmacological delirium interventions: a meta-analysis. JAMA Intern Med. 2015;175:512–520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hshieh TT, Yang T, Gartaganis SL, et al. Hospital Elder Life Program: systematic review and meta-analysis of effectiveness. Am J Geriatr Psychiatry. 2018;26:1015–1033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Bo M, Bonetto M, Bottignole G, et al. Length of stay in the emergency department and occurrence of delirium in older medical patients. J Am Geriatr Soc. 2016;64:1114–1119. [DOI] [PubMed] [Google Scholar]
- 44.Wilson MP, Nordstrom K, Vilke GM. The agitated patient in the emergency department. Curr Emerg Hosp Med Rep. 2015;3:188–194. [Google Scholar]
- 45.Coons HW, Klorman R, Borgstedt AD. Effects of methylphenidate on adolescents with a childhood history of attention deficit disorder: II. Information processing. J Am Acad Child Adolesc Psychiatry. 1987;26:368–374. [DOI] [PubMed] [Google Scholar]
- 46.Allen MH, Currier GW, Carpenter D, et al. ; 2005 Expert Consensus Panel for Behavioral Emergencies. The expert consensus guideline series. Treatment of behavioral emergencies 2005. J Psychiatr Pract. 2005;11(suppl 1):2–5. [DOI] [PubMed] [Google Scholar]
- 47.Richmond JS, Berlin JS, Fishkind AB, et al. Verbal de-escalation of the agitated patient: consensus statement of the American Association for Emergency Psychiatry Project BETA De-escalation Workgroup. West J Emerg Med. 2012;13:17–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Stevenson S Heading off violence with verbal de-escalation. J Psychosoc Nurs Ment Health Serv. 1991;29:6–10. [DOI] [PubMed] [Google Scholar]
- 49.Cohen-Mansfield J, Werner P. Management of verbally disruptive behaviors in nursing home residents. J Gerontol A Biol Sci Med Sci. 1997;52:M369–M377. [DOI] [PubMed] [Google Scholar]
- 50.Waszynski CM, Milner KA, Staff I, et al. Using simulated family presence to decrease agitation in older hospitalized delirious patients: a randomized controlled trial. Int J Nurs Stud. 2018;77:154–161. [DOI] [PubMed] [Google Scholar]
- 51.Annas GJ. The last resort—the use of physical restraints in medical emergencies. N Engl J Med. 1999;341:1408–1412. [DOI] [PubMed] [Google Scholar]
- 52.American Geriatrics Society 2015 Beers Criteria Update Expert Panel. American Geriatrics Society 2015 updated Beers criteria for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2015;63:2227–2246. [DOI] [PubMed] [Google Scholar]
- 53.Wilson MP, Nordstrom K, Hopper A, et al. Risperidone in the emergency setting is associated with more hypotension in elderly patients. J Emerg Med. 2017;53:735–739. [DOI] [PubMed] [Google Scholar]
- 54.Girard TD, Pandharipande PP, Carson SS, et al. Feasibility, efficacy, and safety of antipsychotics for intensive care unit delirium: the MIND randomized, placebo-controlled trial. Crit Care Med. 2010;38:428–437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Zun L, Wilson MP, Nordstrom K. Treatment goal for agitation: sedation or calming. Ann Emerg Med. 2017;70:751–752. [DOI] [PubMed] [Google Scholar]
- 56.Wilson MP, Zeller SL. Reconsidering psychiatry in the emergency department. J Emerg Med. 2012;43:771–772. [DOI] [PubMed] [Google Scholar]
- 57.Lonergan E, Luxenberg J, Areosa Sastre A. Benzodiazepines for delirium. Cochrane Database Syst Rev. 2009;4:CD006379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Aupperle P Management of aggression, agitation, and psychosis in dementia: focus on atypical antipsychotics. Am J Alzheimers Dis Other Demen. 2006;21:101–108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Wilson MP, Pepper D, Currier GW, et al. The psychopharmacology of agitation: consensus statement of the American Association for Emergency Psychiatry Project BETA Psychopharmacology Workgroup. West J Emerg Med. 2012;13:26–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Harrigan EP, Miceli JJ, Anziano R, et al. A randomized evaluation of the effects of six antipsychotic agents on QTc, in the absence and presence of metabolic inhibition. J Clin Psychopharmacol. 2004;24:62–69. [DOI] [PubMed] [Google Scholar]
- 61.Mullinax S, Shokraneh F, Wilson MP, et al. Oral medication for agitation of psychiatric origin: a scoping review of randomized controlled trials. J Emerg Med. 2017;53:524–529. [DOI] [PubMed] [Google Scholar]
- 62.Neufeld KJ, Yue J, Robinson TN, et al. Antipsychotic medication for prevention and treatment of delirium in hospitalized adults: a systematic review and meta-analysis. J Am Geriatr Soc. 2016;64: 705–714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Inouye SK, Marcantonio ER, Metzger ED. Doing damage in delirium: the hazards of antipsychotic treatment in elderly people. Lancet Psychiatry. 2014;1:312–315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Santos E, Cardoso D, Neves H, et al. Effectiveness of haloperidol prophylaxis in critically ill patients with a high risk of delirium: a systematic review. JBI Database System Rev Implement Rep. 2017;15:1440–1472. [DOI] [PubMed] [Google Scholar]
- 65.Burry L, Mehta S, Perreault MM, et al. Antipsychotics for treatment of delirium in hospitalised non-ICU patients. Cochrane Database Syst Rev. 2018;6:CD005594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Kishi T, Hirota T, Matsunaga S, et al. Antipsychotic medications for the treatment of delirium: a systematic review and meta-analysis of randomised controlled trials. J Neurol Neurosurg Psychiatry. 2016;87:767–774. [DOI] [PubMed] [Google Scholar]
- 67.Bennett CC. A healthier future for all Australians: an overview of the final report of the National Health and Hospitals Reform Commission. Med J Aust. 2009;191:383–387. [DOI] [PubMed] [Google Scholar]
- 68.Erstad BL, Patanwala AE. Ketamine for analgosedation in critically ill patients. J Crit Care. 2016;35:145–149. [DOI] [PubMed] [Google Scholar]
- 69.Inouye SK, Bogardus ST, Charpentier PA, et al. A multicomponent intervention to prevent delirium in hospitalized older patients. N Engl J Med. 1999;340:669–676. [DOI] [PubMed] [Google Scholar]
- 70.Han JH, Bryce SN, Ely EW, et al. The effect of cognitive impairment on the accuracy of the presenting complaint and discharge instruction comprehension in older emergency department patients. Ann Emerg Med. 2011;57:662–671.e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Terrell KM, Hustey FM, Hwang U, et al. Quality indicators for geriatric emergency care. Acad Emerg Med. 2009;16:441–449. [DOI] [PubMed] [Google Scholar]
- 72.Inouye SK, Robinson T, Blaum C, et al. ; American Geriatrics Society Expert Panel on Postoperative Delirium in Older Adults. Postoperative delirium in older adults: best practice statement from the American Geriatrics Society. J Am Coll Surg. 2015;220:136–148.e1. [DOI] [PubMed] [Google Scholar]
- 73.Reich DL, Konstadt SN, Thys DM, et al. Effects of doxacurium chloride on biventricular cardiac function in patients with cardiac disease. Br J Anaesth. 1989;63:675–681. [DOI] [PubMed] [Google Scholar]
- 74.Wei LA, Fearing MA, Sternberg EJ, et al. The Confusion Assessment Method: a systematic review of current usage. J Am Geriatr Soc. 2008;56:823–830. [DOI] [PMC free article] [PubMed] [Google Scholar]