Abstract
Introduction/Objectives
To characterize the importance of musculoskeletal stiffness in a cohort of chikungunya patients with chronic joint symptoms.
Method
Eighty-two patients were followed up 3 years after chikungunya infection. Tender and swollen joint counts, a pain intensity scale, Health Assessment Questionnaire-Disability Index (HAQ-DI), and the EuroQol EQ-5D quality of life instrument were completed. A musculoskeletal stiffness questionnaire provided scores for overall stiffness and its components: stiffness severity, physical impact, and psychosocial impact.
Results
Patients had a mean age 51 ± 14 years. Sixty-seven patients were still experiencing chronic arthralgia. Musculoskeletal stiffness was reported by 43/67 patients with arthralgia and 3/15 patients without arthralgia. A physical impact of stiffness was reported by 87% patients and psychosocial impact by 71% patients. Mean tender joint count in patients reporting arthralgia was 6 ± 7, mean pain intensity 65 ± 20 out of 100, mean HAQ-DI was 0.54 ± 0.52, and mean EQ-VAS global health perception was 68 ± 62 out of 100. Stiffness severity was correlated with tender joint counts (ρ = 0.46) and pain intensity (ρ = 0.40). All three measures were equally well correlated with the EuroQol-VAS global health perception. Pain and tender joints were better correlated with the HAQ-DI (ρ = 0.68 and ρ = 0.63), but stiffness was more strongly correlated with several quality of life domains, including mobility. Swollen joints were a poor predictor of outcomes.
Conclusions
Musculoskeletal stiffness following chikungunya infection is distinct from arthralgia. It does not always occur in the same patients or with a corresponding intensity. Joint pain and stiffness may be independently associated with disability and quality of life assessments.
Keywords: Activities of daily living, Health assessment questionnaire, Outcomes
Introduction
Acute chikungunya virus infection is characterized by a rapid onset of fever with swollen and painful joints. Subsequently, rheumatic manifestations may persist for months or years in some patients [1, 2]. Arthralgia is considered to be the classic symptom of chronic chikungunya disease, but a range of other symptoms may follow chikungunya infection, of which musculoskeletal stiffness is one of the most frequent [3, 4]. Despite evidence that many chikungunya patients consider their stiffness to be important [5], there is little information on the severity and specific impact of stiffness on daily activities and quality of life in this population. This may be attributed in part to the lack of well-tested instruments for characterizing musculoskeletal stiffness.
Joint stiffness also presents a frequent problem in rheumatoid arthritis (RA), with which chronic chikungunya disease shares many features [6, 7]. A patient questionnaire for investigating joint stiffness in patients with RA is being developed [8–10], and a series of questions to characterize the severity, the physical impact, and the psychosocial impact of stiffness were tested and validated [11]. This resulted in a standardized questionnaire suitable for research purposes which has been subjected to further testing in RA and psoriatic arthritis patients [12].
The frequency and nature of post-chikungunya joint pain in the long-term follow-up of a cohort of patients from Atlántico Department in Colombia has recently been reported [13]. The objectives here are to describe the different dimensions of musculoskeletal stiffness in this cohort using a detailed questionnaire designed for RA, to determine how closely stiffness is associated with arthralgia, and lastly to investigate the relative importance of different symptoms to the patient.
Materials and methods
Subjects were drawn from a cohort of 485 patients in Colombia followed up by telephone after chikungunya infection [14]. Of the initial cohort, 82 subjects consented to attend a face-to-face medical examination approximately 3 years after infection and participate in this further investigation. These consisted of 67 subjects with continuing post-chikungunya arthralgia and 15 subjects whose arthralgia had resolved.
This study (IRB#121611, Trans#28283) was approved by the ethics committee of the Clinica de La Costa Ltda. and the George Washington University Committee on Human Research. A non-human subject determination was made by the George Washington University IRB for analysis of deidentified data. Written informed consent was obtained from all participants.
Demographic characteristics recorded included age, sex, and educational level, classified as none/primary, high school, college, or postgraduate. Twenty-eight joints were assessed by a physician for the presence of tenderness and swelling. Patients recorded pain intensity on a scale of 0–100. Patients also completed two patient outcome measures: the Health Assessment Questionnaire Disability Index (HAQ-DI), giving a score between 0 and 3 for the level of disability in daily activities [15], and the EuroQol (EQ-5D-5L) form assessing the five domains of mobility, self-care, usual activities, discomfort/pain, and anxiety/depression, plus the Global Health visual analogue scale (VAS). All patients recorded different dimensions of stiffness on a Musculoskeletal Stiffness Questionnaire (MSQ) (Online Resource 1), which gave separate scores for its three components: stiffness severity, physical impact, and psychosocial impact of stiffness, as well as an overall stiffness score.
The severity component of the MSQ consists of eight questions covering the periods of the day when stiffness occurs, the number of joints involved, the onset of stiffness after immobility, the overall severity, the impact and importance of stiffness for the patient’s life, and the presence, duration and severity of morning stiffness on the day of the assessment (Online Resource 1). Each question carried an equal weight in the severity component score. The stiffness severity component total is the average of the eight individual question scores, which are each expressed as a percentage.
The physical impact and psychosocial impact components of the MSQ consist respectively of eight and five questions (Online Resource 1). There are four possible answers to each question, grading the degree of impact of stiffness from no impact (0%) to maximum impact (100%). These two component scores are the average of the individual question scores in each component. Finally, an overall MSQ score was calculated as an average of the three component scores, also expressed as a percentage of the maximum possible score, such that each component has an equal weight in the final score. Patients not experiencing any stiffness scored zero for each component and for the overall MSQ score.
Average scores were expressed as means and standard deviations. Individual associations between the various symptom measures, disability score, and quality of life assessment were expressed using Spearman’s rank correlation coefficient with strength of association interpreted as proposed by [16]. Finally, multiple regression analysis was used to determine the most important predictors of the patient outcomes, the HAQ-DI and the EQ-VAS, considering p < 0.05 as statistically significant. Multiple regression analysis included stiffness, other measures of disease severity, and the patient characteristics of age, sex, and educational level.
Results
The 82 patients (12 male and 70 female) had a mean age 51 ± 14 years and were followed up an average of 40 months after chikungunya infection. The demographic characteristics of these patients did not differ substantially from the original cohort of 485 patients, except for having a larger proportion with a higher educational level (Online Resource 2). Sixty-seven patients (82%) reported persisting arthralgia and 46/82 (56%) experienced joint stiffness. Both symptoms were present in 43/82 (52%) while neither symptom was present in 12/82 (15%). Three out of the 15 patients with no arthralgia (20%) reported joint stiffness. All but five patients reporting arthralgia had tender joints on examination, mean tender joint count was 6 ± 7. Swollen joints were recorded in only 15 of the 67 patients with arthralgia. The mean pain intensity was 65 ± 20 out of 100, mean HAQ-DI was 0.54 ± 0.52 (representing mild difficulties to moderate disability), and mean EuroQol global health VAS score was 68 ± 62 out of 100.
Dimensions of stiffness severity
Forty-four of the 46 patients who experienced joint stiffness provided detailed data on different stiffness dimensions with a mean overall MSQ score of 32% ± 20. Although 24/44 (55%) patients experienced stiffness in the mornings, 35/44 (80%) patients reported stiffness after periods of immobility in general. More than three joints were affected in 20/44 (45%) patients. The MSQ severity component, including all eight questions on the presence, timing, and severity of stiffness, had a mean score of 26% ± 24 among the 67 patients reporting arthralgia and 41% ± 17 among only patients reporting stiffness. One item in the severity component asking for stiffness severity on a rating scale of zero (no stiffness) to 10 (extreme stiffness) resulted in a mean score of 6.0 ± 2.1. The different dimensions of stiffness recorded in the severity component generally correlated strongly with each other and with the overall severity component score (Table 1). The single exception was the duration of morning stiffness, which correlated poorly with other dimensions and with the overall severity component score.
Table 1.
Correlations between different dimensions of stiffness and with the overall severity component score, expressed by Spearman’s rank correlation coefficients, ρ
| No. of stiff joints | Stiffness after immobility | Severity | Impact | Importance | Morning stiffness duration | Severity component total | |
|---|---|---|---|---|---|---|---|
| 0.77 | 0.71 | 0.80 | 0.71 | 0.68 | 0.16 | 0.85 | Frequency |
| 0.73 | 0.86 | 0.85 | 0.83 | 0.26 | 0.88 | No. of stiff joints | |
| 0.83 | 0.74 | 0.72 | 0.10 | 0.82 | After immobility | ||
| 0.90 | 0.87 | 0.18 | 0.94 | Severity | |||
| 0.95 | 0.08 | 0.92 | Impact | ||||
| −0.08 | 0.90 | Importance | |||||
| 0.44 | Morning duration |
Physical and psychosocial impacts of stiffness
Between 30 and 73% of patients reported some impact of stiffness on each of the physical activities described in the physical impact component of the MSQ (Table 2). The most frequently impacted activity was “getting out of bed” and the least frequently impacted activity was “balancing.” Overall, 39 patients (89%) reported an impact on at least one activity, whereas five patients reporting stiffness (11%) considered that it had no impact on any of these physical activities.
Table 2.
Impact of stiffness on daily activities among patients reporting stiffness (n = 44). There were four possible answers to each question: not at all, a little, quite a lot or very much. Anything greater than “not at all” was considered a positive response
| MSQ items | No. of positive responses (%) |
|---|---|
| Physical component | |
| Has stiffness made it difficult to dress or undress yourself? | 30 (68) |
| Has stiffness made it difficult to wash yourself (for example, have a shower)? | 18 (41) |
| Has stiffness made it difficult to carry out your responsibilities or commitments? | 27 (61) |
| Has stiffness made it difficult to do your daily tasks or activities? | 31 (70) |
| Has stiffness made it difficult to get out of bed? | 32 (73) |
| Has stiffness made it difficult to do fine movements (for example, write with a pen)? | 21 (48) |
| Has stiffness made it difficult to grip or hold things? | 28 (64) |
| Has stiffness made it difficult to balance without physically supporting yourself? | 13 (30) |
| Psychosocial component | |
| Have you felt frustrated because of stiffness? | 24 (55) |
| Have you felt worried or concerned because of stiffness? | 29 (66) |
| Have you felt self-conscious because of stiffness? | 24 (55) |
| Have you had to change your plans or behavior because of stiffness? | 20 (45) |
| Have you had to work around your stiffness (or do things in a different way)? | 24 (55) |
Between 45 and 66% of patients expressed an impact of stiffness in each of the questions in the psychosocial impact component of the MSQ (Table 2). Overall, 32 patients (73%) reported at least one psychosocial impact, and the rest (27%) considered that it had no psychosocial impact at all.
The physical and psychological impacts of stiffness were strongly correlated with each other (ρ = 0.83) and also with the stiffness severity component (ρ = 0.86 and ρ = 0.73 respectively).
Association of stiffness with joint tenderness, swelling, and pain
The associations of the overall score on the MSQ and the MSQ stiffness severity component with tender and swollen joint counts and the pain intensity score were investigated (Table 3). The correlation coefficients for these associations ranged from very weak, for swollen joint counts, to moderate, for tender joint counts, and pain score (Table 3), suggesting that stiffness is not highly predictable from the other disease severity measures employed here.
Table 3.
Associations of musculoskeletal stiffness questionnaire components with other measures of disease severity, expressed by Spearman’s rank correlation coefficients, ρ
| Stiffness measures | Other disease severity measures |
||
|---|---|---|---|
| Tender joint count | Swollen joint count | Pain intensity | |
| Overall MSQ score | 0.47 | 0.13 | 0.46 |
| Severity component | 0.46 | 0.12 | 0.40 |
| Physical impact | 0.44 | 0.17 | 0.49 |
| Psychosocial impact | 0.36 | 0.10 | 0.41 |
Association of symptoms and disease severity with disability and quality of life
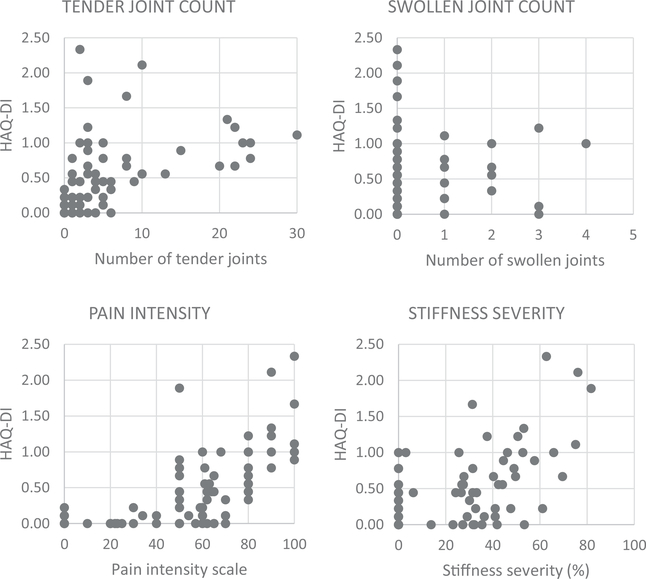
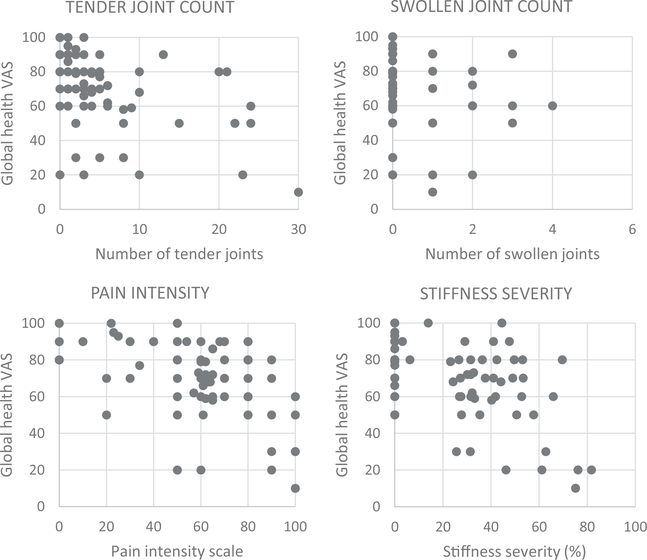
Associations of disease severity measures with the HAQ disability index and quality of life domains were investigated (Table 4, Figs. 1 and 2). Pain intensity, tender joint count, and stiffness were all correlated with the HAQ disability index. Only stiffness severity was correlated to a moderate extent with both the mobility and self-care domains of the EQ-5D, whereas both stiffness and pain intensity were moderately correlated with the pain/discomfort domain. Tender and swollen joint counts showed weaker correlations with all EQ-5D domains. Tender joint count, pain intensity, and stiffness severity were all moderately and inversely correlated with global health perceptions on the EuroQol-VAS. The overall MSQ score, incorporating physical activity and psychosocial elements, showed moderate correlations with most of the disability and quality of life measures.
Table 4.
Correlations of HAQ-disability index and EuroQol EQ-5D scores with measures of disease severity, expressed by Spearman’s rank correlation coefficients, ρ
| Outcome measure | Tender joint count | Swollen joint count | Pain intensity | Stiffness severity | Overall MSQ score |
|---|---|---|---|---|---|
| HAQ-DI | 0.63 | 0.15 | 0.68 | 0.51 | 0.59 |
| EQ-5D domains: | |||||
| Mobility | 0.33 | 0.26 | 0.27 | 0.43 | 0.37 |
| Self-care | 0.35 | 0.12 | 0.37 | 0.40 | 0.51 |
| Usual activities | 0.25 | 0.10 | 0.33 | 0.34 | 0.43 |
| Pain/discomfort | 0.35 | 0.32 | 0.49 | 0.47 | 0.49 |
| Anxiety/depression | 0.13 | 0.01 | 0.20 | 0.25 | 0.31 |
| EQ global health VAS | −0.48 | −0.21 | −0.46 | −0.47 | −0.53 |
Fig. 1.
Association of the HAQ disability index with disease severity measures
Fig. 2.
Association of the EuroQol global health VAS with disease severity measures
A single question on stiffness severity with a rating of 0 to 10 was investigated as a substitute for the 8-item MSQ severity component. The single question on a severity rating was very strongly correlated with the overall severity component score at ρ = 0.94. However, the correlations with HAQ-DI, EuroQol mobility domain, and the global health VAS of ρ = 0.43, ρ = 0.36, and ρ = − 0.43, respectively, suggest that this was less informative for the overall patient status than the 8-item MSQ severity component as a whole.
Predictors of disability and global health perception
Multiple regression analysis identified tender joint count, pain intensity, and stiffness (MSQ score) as predictors for the HAQ disability index with beta values of 0.015 (p = 0.008), 0.005 (p = 0.0006), and 0.020 (p = 0.04), respectively. Thus, it was estimated that an increase of 10% in stiffness score would produce an increase of 0.20 (or 6.3%) in the HAQ disability index. However, the effect of stiffness was also modified by educational level. A model including these variables plus the interaction of stiffness and educational level explained 71% of the HAQ disability index. The EuroQol global health VAS was influenced by both tender and swollen joint counts in the final multiple regression model with beta values of − 0.69 (p = 0.007) and − 3.75 (p = 0.03). In addition, age and stiffness (modified by educational level) were significant predictors in the model, which overall accounted for 64% of variability in the global health score (Online Resource 3).
Discussion
The general frequency of chronic rheumatic symptoms in a large chikungunya patient cohort in Colombia has been described previously [13], but this more detailed investigation of a smaller sample permitted us to describe the relationship between symptoms, disease severity, and outcomes. These analyses showed that, independent of arthralgia, musculoskeletal stiffness as measured by a detailed questionnaire has a significant impact on the daily activities of patients after chikungunya infection and is relevant to their overall health perception. This finding is of importance as there are currently no evidence-based treatments for chikungunya-related arthritis, and specific, reliable, and valid metrics are needed to facilitate clinical trials for potential therapeutics. Our analysis suggests that stiffness measures may be an important element in the accurate measure of disease activity for chikungunya arthritis clinical trial endpoints.
Musculoskeletal symptoms persist in a significant proportion of patients following acute CHIKV infection. Joint pain is cited as the most typical symptom with a varying rate of persistence [17], depending on the outbreak in question and the time of follow-up. Although chronic musculoskeletal stiffness has often been reported following chikungunya infection [3, 4, 18–20], few data exist concerning its severity and importance. We identified a need to understand better the severity and impact of stiffness, but there was no specific instrument validated for measuring stiffness in chikungunya patients. Considering the many similarities between the symptoms reported by patients with rheumatoid arthritis (RA) and the chronic symptoms after chikungunya infection [7], it seemed appropriate to use a system already tested in RA for the measurement of stiffness and its impact. Simpler scales for stiffness severity, duration of stiffness, and interference with daily activities have been proposed for RA [21], but since our objective was to characterize chikungunya stiffness in detail, we selected this comprehensive 21-item musculoskeletal stiffness questionnaire (MSQ) [22].
The length of the stiffness questionnaire employed was less than ideal, but each question seemed to bring additional information. We considered whether a single question on stiffness severity could replace the overall 8-item severity component, but it was found to be less informative with respect to disability and the patient’s global health perception. However, future studies may explore the possibility of reducing the number of questions using an adaptive system based on item response theory [23]. As in RA, stiffness in chikungunya disease is frequently referred to as “morning stiffness.” In our cohort, stiffness was often a problem in the early morning, and getting out of bed was the physical activity most frequently affected, but a period of immobility in general was more often a trigger for stiffness and a range of physical activities were affected. Since the specific question on morning stiffness was poorly correlated with overall severity, this question might be considered of limited value and omitted in future studies of chikungunya disease.
Stiffness appears to be quite distinct from the other symptoms of chikungunya disease. Although previously reported as associated with joint pain [19], in the present study, it did not always coexist with arthralgia, and the stiffness scores correlated only moderately with pain and counts of involved joints. However, the stiffness score and its components were correlated with the HAQ disability index and quality of life parameters suggesting that they are measuring something important to the patient. Indeed, the stiffness score and its components correlated more strongly than the tender joint count and pain did with some EQ-5D domains, such as mobility. There is an acknowledged tendency for different patient self-report data to be more strongly correlated with each other than with objective or physician-derived measures in rheumatoid arthritis [24], so a similar phenomenon might be expected in chikungunya disease. Nonetheless, the association of stiffness with physical function replicates findings in RA [9, 25], thus supporting the construct validity of this questionnaire in the context of chikungunya.
The association of stiffness (characterized as present or absent) with some physical domains of health-related quality of life has been reported previously in post-CHIKV rheumatism [3]. The same study reported similar associations of joint pain with physical dimensions of QoL, but in contrast to our own findings, also found that presence of joint swelling was broadly associated with the QoL instruments tested. With more detailed information about stiffness, we were able to confirm the association with impairment of physical activities, but not the association of joint swelling with quality of life. In this respect, it may be a limitation of our study that we could only investigate these associations at the later time point of 40 months post-infection when the number of swollen joints was low. Time elapsing since infection may play a role considering the expected gradual resolution of symptoms over time [26].
Although not initially developed and validated for chikungunya disease, the content of this stiffness questionnaire seems highly relevant to patients with chronic chikungunya symptoms. We were able to determine that stiffness is not always associated with arthralgia, and our results suggest that the assessment of musculoskeletal stiffness, as measured in this study, may be a meaningful parameter to include in the assessment of disease severity in chronic chikungunya disease. Importantly it may have as much impact as joint pain on the overall level of disability and the health perception of the patient.
Supplementary Material
Key Points.
Arthralgia is the classic symptom of chronic chikungunya rheumatism, associated with quality of life and disability.
Musculoskeletal stiffness was found to be distinct from arthralgia and equally important as a determinant of quality of life in this chronic chikungunya cohort.
Tender joint counts, but not swollen joint counts, were also a good predictor of disability in chikungunya disease.
Acknowledgments
The authors wish to acknowledge the contributions of Giulia Calusi to the statistical analysis of these data, and Serena Halls for kindly sharing and agreeing to our use of the questionnaire for assessment of musculoskeletal stiffness.
Funding information This work is supported by a Pilot award from the Rheumatology Research Foundation and the NIH (National Center for Advancing Translational Sciences grants UL1-TR-001876 and KL2-TR-001877).
Footnotes
Compliance with ethical standards
Disclosures None.
Ethical standards This study (IRB#121611, Trans#28283) was approved by the ethics committee of the Clinica de La Costa Ltda. and the George Washington University Committee on Human Research and has been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. All persons gave their informed consent prior to their inclusion in the study.
Disclaimer The views expressed herein are solely the responsibility of the authors and do not necessarily represent the official views of the Rheumatology Research Foundation or the NIH.
Electronic supplementary material The online version of this article (https://doi.org/10.1007/s10067-019-04919-1) contains supplementary material, which is available to authorized users.
References
- 1.Weaver SC, Lecuit M (2015) Chikungunya virus and the global spread of a mosquito-borne disease. New Engl J Med 372:1231–1239 [DOI] [PubMed] [Google Scholar]
- 2.Burt FJ, Rolph MS, Rulli NE, Mahalingram S, Heise MT (2012) Chikungunya a re-emerging virus. Lancet 9816:662–671 [DOI] [PubMed] [Google Scholar]
- 3.Couturier E, Guillemin F, Mura M, Leon L, Virion J-M, Letort M-J, de Valk H, Simon F, Vaillant V (2012) Impaired quality of life after chikungunya virus infection: a 2-year follow-up study. Rheumatology 51:1315–1322 [DOI] [PubMed] [Google Scholar]
- 4.Consuegra-Rodríguez MP, Hidalgo-Zambrano DM, Vasquez-Serna H, Jimenez-Canizales CE, Parra-Valencia E, Rodriguez-Morales AJ (2018) Post-chikungunya chronic inflammatory rheumatism: follow-up of cases after 1 year of infection in Tolima, Colombia. Travel Med Infect Dis 21:62–68 [DOI] [PubMed] [Google Scholar]
- 5.Marimoutou C, Vivier E, Oliver M, Boutin JP, Simon F (2012) Morbidity and impaired quality of life 30 months after chikungunya infection. Medicine 91:212–219 [DOI] [PubMed] [Google Scholar]
- 6.Chopra A, Anuradha V, Lagoo-Joshi V, Kunjir V, Salvi S, Saluja M (2008) Chikungunya virus aches and pains: an emerging challenge. Arthritis Rheum 58:2921–2922 [DOI] [PubMed] [Google Scholar]
- 7.Miner JJ, Yeang HXA, Fox JM, Taffner S, Malkova ON, Oh ST et al. (2015) Chikungunya viral arthritis in the United States. A mimic of seronegative rheumatoid arthritis. Arthritis Rheum 67: 1214–1220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Halls S, Dures E, Kirwan J, Pollock J, Baker G, Edmunds A, Hewlett S (2015) Stiffness is more than just duration and severity: a qualitative exploration in people with rheumatoid arthritis. Rheumatology 54:615–622 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Halls S, Sinnathurai P, Hewlett S, Mackie SL, March L, Bartlett SJ et al. (2017) Stiffness is the cardinal symptom of inflammatory musculoskeletal diseases, yet still variably measured: report from the OMERACT 2016 stiffness special interest group. J Rheumatol 44:1904–1910 [DOI] [PubMed] [Google Scholar]
- 10.Orbai A-M, Bingham CO (2015) Patient reported outcomes in rheumatoid arthritis clinical trials. Curr Rheumatol Rep 17:28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Halls S, Dures E, Kirwan J, Pollock J, Baker G, Edmunds A, Hewlett S (2018) Development and testing of candidate items for inclusion in a new rheumatoid arthritis stiffness patient-reported outcome measure. Rheumatology 57:263–272 [DOI] [PubMed] [Google Scholar]
- 12.Craig ET, Orbai AM, Mackie S, Bartlett SJ, COB Ill, Goodman S et al. (2019) Advancing stiffness measurement in rheumatic disease: report from the stiffness special interest group at OMERACT 2018. J Rheumatol 46:1374–1378 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tritsch SR, Encinales L, Pacheco N, Cadena A, Cure C, McMahon E, et al. (2019) Chronic joint pain 3 years after chikungunya virus infection is largely characterized by relapsing-remitting symptoms. J Rheumatol July 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chang AY, Encinales L, Porras A, Pacheco N, Reid SP, Martins KAO et al. (2018) Frequency of chronic joint pain following chikungunya virus infection: a Colombian cohort study. Arthritis Rheum 70:578–584 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wolfe F, Michaud K, Pincus T (2004) Development and validation of the health assessment questionnaire II: a revised version of the health assessment questionnaire. Arthritis Rheum 50:3296–3305 [DOI] [PubMed] [Google Scholar]
- 16.Evans JD (1996) Straightforward statistics for the behavioral sciences. Brooks/Cole publishing, Pacific grove, Calif [Google Scholar]
- 17.Edington F, Varjão D, Melo P (2018) Incidence of articular pain and arthritis after chikungunya fever in the Americas: a systematic review of the literature and meta-analysis. Joint Bone Spine 85:669–678 [DOI] [PubMed] [Google Scholar]
- 18.Brighton SW, Prozesky OW, de la Harpe AL (1983) Chikungunya virus infection. A retrospective study of 107 cases. S Afr Med J 63: 313–315 [PubMed] [Google Scholar]
- 19.Sissoko D, Malvy D, Ezzedine K, Renault P, Moscetti F, Ledrans M et al. (2009) Post-epidemic chikungunya disease on Reunion Island: course of rheumatic manifestations and associated factors over a 15-month period. PLoS Negl Trop Dis 3:e389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Elsinga J, Grobusch MP, Tami A, Gerstenbluth I, Bailey A (2017) Health-related impact on quality of life and coping strategies for chikungunya: a qualitative study in Curacao. PLoS Negl Trop Dis 11:e0005987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Craig ET, COB Ill, Bartlett SJ, Haque U, Leong A, Orbai A-M (2018) Construct validity and responsiveness of three stiffness items in rheumatoid arthritis: an application of the OMERACT filter 2.1. Ann Rheum Dis 77(suppl 2):849 [Google Scholar]
- 22.Halls S, Dures E, Kirwan J, Pollock J, Baker G, Edmunds A et al. (2016) Construct validity testing of RAST, a new RA stiffness patient reported outcome measure (PROM). Ann Rheum Dis 75 (suppl 2):1317. [DOI] [PubMed] [Google Scholar]
- 23.Khanna D, Krishnan E, Dewitt EM, Khanna PP, Spiegel B, Hays RD (2011) The future of measuring patient-reported outcomes in rheumatology: patient-reported outcomes measurement information system (PROMIS). Arthritis Care Res 63(Suppl 11):S486–S490 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pincus T, Callahan LF, Brooks RH, Fuchs HA, Olsen NJ, Kaye JJ (1989) Self-report questionnaire scores in rheumatoid arthritis compared with traditional physical, radiographic, and laboratory measures. Ann Intern Med 110:259–266 [DOI] [PubMed] [Google Scholar]
- 25.Sinnathura P, Bartlett SJ, Halls S, Hewlett S, Orbai AM, Buchbinder R, et al. (2019) Investigating dimensions of stiffness in rheumatoid and psoriatic arthritis: the Australian Rheumatology Association Database Registry and OMERACT collaboration. J Rheumatol 46:1462–1469 [DOI] [PubMed] [Google Scholar]
- 26.Yaseen HM, Simon F, Deparis X, Marimoutou C (2012) Estimation of lasting impact of a chikungunya outbreak in Reunion Island. Epidemiology S:2 [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.