Abstract
Background
Pathologic tooth migration (PTM) is a common complication of mild to severe periodontitis and proper orthodontic treatment is helpful to alleviate periodontal diseases. The goal of this study is to explore an optimal orthodontic displacement of clear aligner using a three-dimensional (3D) finite element model (FEM).
Methods
The cone beam computed tomography (CBCT) data of a patient received invisible orthodontics without diabetes and other systemic diseases were collected. Based on the new classification scheme for periodontal diseases in 2017 (stage I: mild periodontitis, [M1]; stage II: moderate periodontitis, [M2]; stage III: severe periodontitis, [M3]), 3D-FEMs of mandible were established using MIMICS 10.0 and ABAQUS 6.5 softwares. The 3D stress distribution diagrams and stress value of the teeth (left lower incisor, left lower central incisor, right lower lateral incisor, and right lower central incisor) under three different periodontal conditions (M1, M2, and M3) with axial inclination 90° and 100° were obtained by ABAQUS 6.5.
Results
The stress of anterior teeth was concentrated in the teeth neck, and became greater when the periodontal condition was worse. The stress value of anterior teeth and the strain at the top of the alveolar crest are greater as the displacement increasing. The stress value of anterior teeth and the strain at the top of the alveolar crest in axial inclination 100° are relatively great compared to those of axial inclination 90°. For patients with excessively inclined anterior teeth (such as 100°), the optimal orthodontic displacement is 0.18 mm. In order to ensure that alveolar ridge crest is not deformed, the displacement is less than 0.18 mm (strain for 0.165 mm), 0.15 mm (strain for 0.167 mm) and 0.10 mm (strain for 0.117 mm) respectively when alveolar bone is normal, resorption 1/3 or 1/3–1/2.
Conclusions
The optimal orthodontic displacement for patients (M1, M2, and M3) with excessively inclined anterior teeth (axial inclination 100°) is 0.18 mm. To avoid the strain at the top of the alveolar crest, the optimal displacements for M1, M2 and M3 periodontal disease patients are less than 0.18 mm, 0.15 mm and 0.10 mm, respectively.
Keywords: Clear aligner, Anterior teeth, Alveolar ridge crest, Displacement
Background
Pathologic tooth migration (PTM) is a common complication of mild to severe periodontitis and manifests as the inclination, elongation and fan-out of the anterior teeth [1]. The incidence of periodontal diseases among adults is as high as 76%-92% [2]. In adult patients, the speed of alveolar bone resorption under pressure is greater than that of traction and hyperplasia [3]. The impedance center of the tooth moves to the root and the torque is increased, which further aggravates the destruction of periodontal tissues [4]. Therefore, adult patients with periodontitis should be treated with light force to maintain the health and stability of the periodontal environment [5]. A 12-year follow-up experiment has shown that orthodontic treatment is no longer a contraindication for severe periodontal diseases [6]. Therefore, a comprehensive and complete orthodontic treatment should be carried out, otherwise accelerating periodontal inflammation and bone destruction.
Recent years, more attentions have been paid to the effects of clear aligner on periodontal diseases due to its aesthetics and comfort on wearers [7]. As a new type of orthodontic treatment, clear aligner can cover all the teeth and keratinized gingiva without obvious damage to the periodontal tissues [8]. Besides, the use of removable orthodontic appliance is conducive to the maintenance of oral hygiene and minimizes the risk of periodontal complication [9, 10]. There are significant differences between the use of fixed appliance and clear aligner. The fixed appliance exerts continuous light force by bonding the brackets on the tooth surface and ligating the arch wire [11], while the clear aligner applies a kind of instantaneous stress, which is about 50 to 500 times than that of fixed orthodontic loading [11, 12]. However, whether the instantaneous higher-stress has a certain impact on the periodontal tissues, or whether there is a gap in the efficiency of tooth movement due to different periodontal conditions still need to be explored. Additionally, among the various types of movement of teeth such as intrusion, extrusion, rotation, tipping, and alignment movements, intrusion movement is easier to cause tooth loosening or root absorption [13]. Therefore, it is very crucial to investigate intrusion movement in the treatment of periodontal diseases [13, 14].
The finite element model (FEM) is an engineering technique used to calculate stress and deformation developed on a geometric solid submitted to external forces [15–19]. Recent years, FEM has been widely applied in different dental fields, from fixtures to the simulation of dental movements to assess the stresses generated within the different tissue structures, such as alveolar bone, periodontal ligament, and teeth [20–23]. For instance, Crimi et al. used FEM to analyze the changes in the buccal cortical bone in patients undergoing orthodontics surgeries and indicated that there is no direct proportionality relationship between the extent of bone apposition/reabsorption and dental movement [24]. Interestingly, Cervino et al. introduced a new prosthodontic technology named Digital Smile Design, which is used in combination with FEM to improve the quality of the rehabilitations [25]. In addition, with the use of FEM, it is possible to determine loading and displacement patterns according to the appliance used [26, 27]. But relevant FEM researches on the optimal displacement of clear aligner under different periodontal-statuses are relatively rare.
In this study, we investigated the effects of anterior teeth intrusion on different periodontal conditions (stage I: mild periodontitis, [M1]; stage II: moderate periodontitis, [M2]; stage III: severe periodontitis, [M3]) using a 3D-FEM, and explored the optimal displacement of teeth when anterior teeth were intruded using clear aligner. This study is aimed to provide a direction for the use of clear aligner in clinic.
Methods
Establishment of mandible model
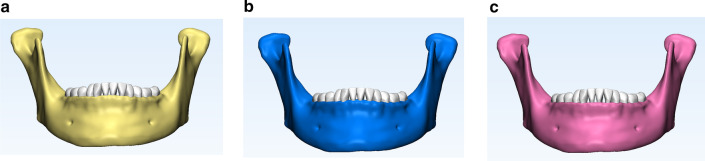
The Cone Beam Computed Tomography (CBCT) data (HiRes3D-Plus; Largev, Beijing, China) of a patient (female, 35 years old) with mild periodontitis received invisible orthodontics were collected. The exclusion criteria for the patient included diabetes and/or other systemic diseases that may cause progressive periodontal injury. Afterwards, based on the new classification scheme for periodontal diseases in 2017 (M1: stage I, normal alveolar bone with mild periodontitis; M2: stage II, alveolar bone resorption 1/3 with moderate periodontitis; M3: alveolar bone resorption 1/3–1/2 with severe periodontitis) [28, 29], 3D-FEMs of mandible (Fig. 1) were established using MIMICS 10.0 (Materi-alise, Leuven, Belgium) and ABAQUS 6.5 (ABAQUS. Inc, USA) softwares as previous studies described [17–19]. Though the finite element software ABAQUS 6.5, we calculated the stress of each part in the models, and obtained the 3D stress distribution diagrams and stress value of the teeth.
Fig. 1.
The 3D mandible models of three different periodontal conditions. a The 3D model of normal periodontal condition. b The 3D model of mild periodontal disease. c The 3D model of moderate periodontal disease
Simulation of anterior teeth intrusion
To simulate of anterior teeth intrusion (left lower incisor, left lower central incisor, right lower lateral incisor, and right lower central incisor), the displacement of the teeth (0.10 mm, 0.15 mm, 0.18 mm, 0.20 mm and 0.25 mm, respectively) was preseted [14] and was used to analyze the change of stress value with two different axial inclinations of anterior teeth (90° and 100°). The stress value of normal periodontal-condition was utilized as a control.
Structure parameters and calculation of stress
An elastic-lineal behavior and standard Young's modulus (alveolar bone: 1.40 × 103 MPa; tooth: 1.96 × 104 MPa; clear aligner: 528 MPa; vertical rectangular-attachment: 1.25 × 104 MPa) and Poisson's ratio (alveolar bone: 0.30; tooth: 0.30; clear aligner: 0.36; vertical rectangular-attachment: 0.36) of the model were considered for all calculations as the previous studies described [30, 31]. The Von Mises comprehensive equivalent stress was selected as the main indicator to measure the stress level. Though the finite element software ABAQUS 6.5, we calculated the stress of each part in the models, and obtained the 3D stress distribution diagrams and stress value of the teeth.
Results
The stress distribution and stress value of the lower anterior teeth with three different periodontal conditions
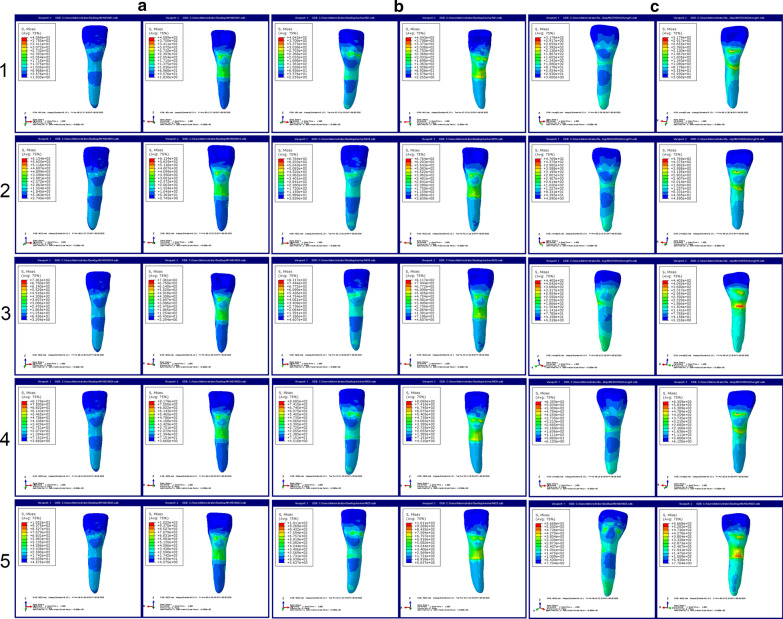
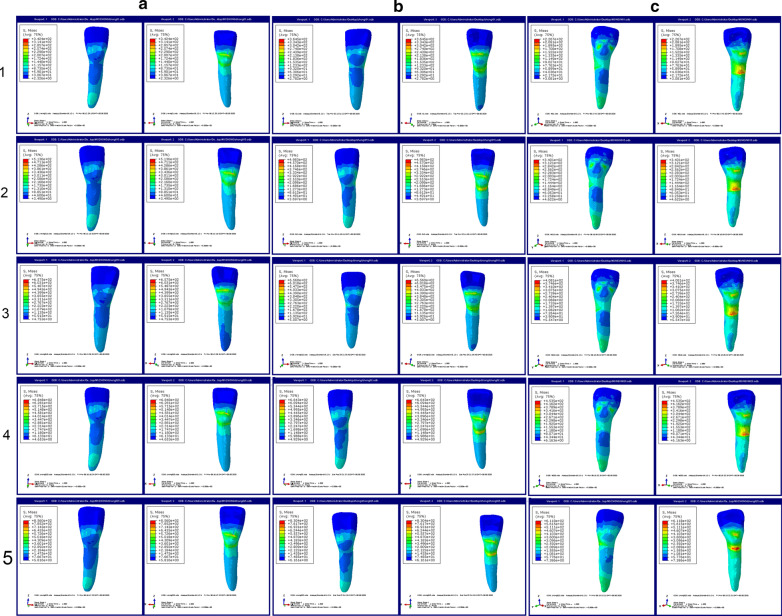
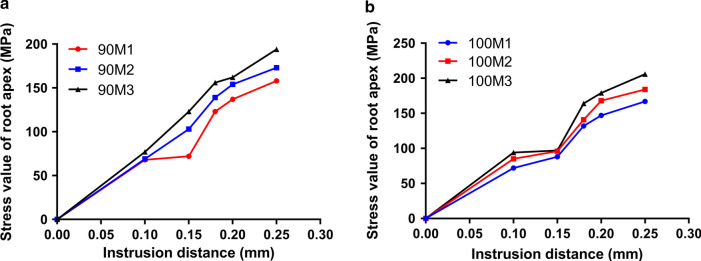
First, the stress distributions of the lower anterior teeth under three different periodontal conditions with two different axial inclinations of anterior teeth (90° and 100°) were observed (Figs. 2 and 3). We discovered that the stress of anterior teeth became stronger and was concentrated in the teeth neck when the periodontal condition was worse in the same axial inclination of anterior teeth (90° or 100°). Besides, as the displacement (0.10 mm, 0.15 mm, 0.18 mm, 0.20 mm and 0.25 mm, respectively) increasing, the stress was also more powerful. As illustrated in Fig. 4, we analyzed the stress values with quantification. The results demonstrated that the stress values (M1: 68 MPa, M2: 69 MPa, M3: 77 MPa) in 0.10 mm displacement were relatively low, whereas were increased greatly (M1: 72 MPa, M2: 103 MPa, M3: 123 MPa) starting from 0.15 mm displacement in the condition of axial inclination 90°. The stress values in 0.20 mm displacement were 137, 154, and 162 MPa (from M1 to M3), and were 158, 173, and 194 MPa (from M1 to M3) in 0.25 mm displacement (Fig. 4a). Interestingly, the stress values of anterior teeth in axial inclination 100° are relatively great compared to those of axial inclination 90°. In the condition of axial inclination 100°, the stress values of 0.10 mm were 72, 85, and 94 MPa (from M1 to M3), and next were 0.15 mm (M1: 88 MPa, M2: 96 MPa, M3: 97 MPa), 0.18 mm (M1: 132 MPa, M2: 141 MPa, M3: 164 MPa), 0.20 mm (M1: 147 MPa, M2: 168 MPa, M3: 179 MPa) and 0.25 mm (M1: 167 MPa, M2: 184 MPa, M3: 206 MPa).
Fig. 2.
The stress distributions of the lower anterior teeth under three different periodontal conditions with axial inclination 90°. a The stress distributions of the lower anterior teeth under normal periodontal condition with axial inclination 90°. b The stress distributions of the lower anterior teeth under mild periodontal disease with axial inclination 90°. c The stress distributions of the lower anterior teeth under moderate periodontal disease with axial inclination 90°. 1: 0.10 mm displacement; 2: 0.15 mm displacement; 3: 0.18 mm displacement; 4: 0.20 mm displacement; 5: 0.25 mm displacement
Fig. 3.
The stress distributions of the lower anterior teeth under three different periodontal conditions with axial inclination 100°. a The stress distributions of the lower anterior teeth under normal periodontal condition with axial inclination 100°. b The stress distributions of the lower anterior teeth under mild periodontal disease with axial inclination 100°. c The stress distributions of the lower anterior teeth under moderate periodontal disease with axial inclination 100°. 1: 0.10 mm displacement; 2: 0.15 mm displacement; 3: 0.18 mm displacement; 4: 0.20 mm displacement; 5: 0.25 mm displacement
Fig. 4.
The stress values of root apex in three periodontal conditions. a The stress values of the lower anterior teeth under three different periodontal conditions with axial inclination 90°. b The stress values of the lower anterior teeth under three different periodontal conditions with axial inclination 100°
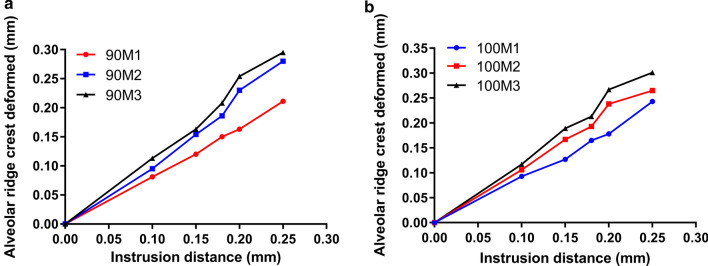
The correlation between the strain at the top of the alveolar crest and displacement
Subsequently, we analyzed the correlation between the strain at the top of the alveolar crest and displacement (0.10 mm, 0.15 mm, 0.18 mm, 0.20 mm and 0.25 mm, respectively) with two different axial inclinations of anterior teeth (90° and 100°) (Fig. 5). On the whole, we found that the alveolar ridge crest was deformed seriously as the displacement increasing in both two axial inclinations. In the terms of axial inclinations 90°, the ranges of strain at the top of the alveolar crest were 0.081–0.163 mm (0.1 mm displacement, M1: 0.081 mm, M2: 0.095 mm, M3: 0.113 mm; 0.15 mm displacement, M1: 0.120 mm, M2: 0.154 mm, M3: 0.163 mm) when the displacement was less than 0.15 mm. As the displacement increasing from 0.18 mm to 0.25 mm, the strain at the top of the alveolar crest was more visible, which ranged from 0.150 to 0.295 mm (0.18 mm displacement, M1: 0.150 mm, M2: 0.186 mm, M3: 0.208 mm; 0.2 mm displacement, M1: 0.163 mm, M2: 0.230 mm, M3: 0.254 mm; 0.25 mm displacement, M1: 0.211 mm, M2: 0.280 mm, M3: 0.295 mm) (Fig. 5a). The strain at the top of the alveolar crest was further elevated when axial inclinations changed to 100°. As shown in Fig. 5b, the ranges of the strain at the top of the alveolar crest were 0.093–0.117 (M1: 0.093 mm, M2: 0.106 mm, M3: 0.117 mm), 0.127–0.189 (M1: 0.127 mm, M2: 0.167 mm, M3: 0.189 mm), 0.165–0.213 (M1: 0.165 mm, M2: 0.193 mm, M3: 0.213 mm), 0.178–0.267 (M1: 0.178 mm, M2: 0.238 mm, M3: 0.267 mm), and 0.243–0.301 (M1: 0.243 mm, M2: 0.265 mm, M3: 0.301 mm) mm respectively when the displacement started from 0.10 to 0.25 mm.
Fig. 5.
The strain at the top of the alveolar crest in three periodontal conditions. a the strain at the top of the alveolar crest in three periodontal conditions with axial inclination 90°. b The strain at the top of the alveolar crest in three periodontal conditions with axial inclination 100°
Discussion
The essence of clear aligner treatment is that teeth move under the force generated by the deformation of appliance [32]. This force is transmitted to the tooth root and periodontal tissues through the inner surface of the appliance, causing the tissues to remodel and move the tooth [32]. FEM is a widely used and effective method on orthodontic studies [16–19]. Geramy et al. and McGuinness et al. used FEM to analyze the stress components of maxillary central incisor and canine tooth respectively under different alveolar bone height [18, 19]. Tanne K et al. investigated the biomechanical effect of maxillary orthopedic forces on the craniofacial complex by use of FEM [17]. In the research conducted by Middleton et al. uncovered the stresses and strains within the periodontal ligament and surrounding bone, consequent to orthodontic loading of a tooth by application of a FEM [16]. Given the application of FEM in oral biomechanics and orthodontics, the optimal orthodontic displacement was explored through anterior teeth intrusion using a 3D-FEM in this study.
Stress is one of the most important factors affecting bone regeneration and absorption [14, 33, 34]. The teeth cannot move if the stress is too small, whereas too much stress may cause degeneration or even necrosis of the periodontal ligament [14, 33, 34]. Orthodontists should apply appropriate orthodontic force to achieve maximum tooth movement efficiency and minimum damage to root and periodontal tissues [13, 35]. This is especially true for invisible orthodontics, because the instantaneous force of the invisible orthodontic is much greater than that of the fixed orthodontic, and this instantaneous force may have a pathological reaction that is not conducive to tooth movement [36]. Tweed made a statistical study on Caucasians and found that under the conditions of facial coordination, stable dental arch and good masticatory function, the axial inclination is 90° [37]. The orthodontic treatment mainly depends on changing the position and inclination of the lower incisor. When the axial inclination is greater than 90° (such as 100°), the lower anterior teeth presents a status of lip inclination and the lower lip was protruding, which needs orthodontic treatment [37]. In this study, we found that as the periodontal conditions becoming worse (M1 to M3), the maximum stress values of the anterior teeth change accordingly. Meanwhile, the larger of the axial inclination, the greater of stress in anterior teeth is. We conjectured that the oversize axial inclination may increase the possibility of root damage. Besides, inadequate orthodontic treatment induces an injury of the periodontium that is clinically observed as root resorption and/or alveolar bone loss [38, 39].Therefore, it was necessary to reduce the displacement of tooth when designing tooth movement. Recent studies have demonstrated that in the process of invisible orthodontic, the displacement of each tooth is 0.20–0.40 mm [40, 41]. More importantly, the default displacement of different brands of clear aligners is usually 0.20–0.30 mm per step [40, 41]. Therefore, 0.20 mm displacement in axial inclination 90° was also considered as a control among the five displacements in this study. When the axial inclination was increased, the maximum stress value of anterior teeth should not exceed the stress value when the displacement was 0.20 mm. In axial inclination 100°, we discovered that the ranges of stress value in 0.18 mm are 132–164 MPa, which are similar to the stress value ranges of 0.20 mm in axial inclination 90° (137–162 MPa). Consequently, we inferred that for patients with excessively inclined anterior teeth (such as 100°), the optimal orthodontic displacement when using clear aligner is 0.18 mm.
We should also reasonably determine the displacement based on the strain of the alveolar bone or alveolar ridge crest. Peter et al. have analyzed the 3D-FEM of alveolar bone and revealed that in order to distribute the periodontal stress evenly, a combination of force reduction and increased moment-to-force (M/F) ratio is required [42]. A research conducted by Cobo et al. has been reported that the height of the alveolar bone can directly or indirectly affect the periodontal stress distribution, and the magnitude of the change is positively related to the degree of influence [43]. In this study, the strain at the top of the alveolar crest with different displacement (0.10 mm, 0.15 mm, 0.18 mm, 0.20 mm and 0.25 mm, respectively) under two different axial inclinations of anterior teeth (90° and 100°) was explored. Likewise, 0.20 mm in 90M1 was used as the control group and the strain at the top of the alveolar crest was 0.163 mm. We found that the displacement must be not exceeding 0.15 mm when alveolar bone resorption is 1/3 or 1/3–1/2. In axial inclination 100°, we discovered that in order to ensure that alveolar ridge crest is not deformed, the displacement is less than 0.18 mm (strain for 0.165 mm), 0.15 mm (strain for 0.167 mm) and 0.10 mm (strain for 0.117 mm) respectively when alveolar bone is normal, resorption 1/3 or 1/3–1/2. All the results implied that the stress on the teeth and the strain at the top of the alveolar crest should be taken into account at the same time when presetting displacement in orthodontic treatment.
However, there are some limitations in this study. First, this study is focused on four of the anterior teeth, and posterior tooth movement remains unclear. Second, tooth movements are influenced by the patient’s age, periodontal support, root length, and bone density, and large sample size is necessary. Third, tooth movement is also affected by periodontal tissue remodeling, action time, strength attenuation, and oral and maxillofacial muscle occlusion. The results of preliminary finite element need to be used in clinical practice to verify its efficacy.
Conclusions
In summary, we explored the optimal orthodontic displacement to minimize the adverse effects of the clear aligner on periodontal tissues under laboratory conditions. However, the structure of oral cavity is extremely complex and there may be other factors to affect the treatment effect of clear aligner. Even so, we also hope our findings will improve orthodontic treatment with clear aligners.
Acknowledgements
Not applicable.
Abbreviations
- CBCT
cone beam computed tomography
- PTM
pathologic tooth migration
Authors' contributions
YNM: conception, design and analysis of data, performed the data analyses and wrote the manuscript; SL: contributed to the conception of the study and revised the manuscript; All authors have read and approved the manuscript.
Funding
Not applicable.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Ethics approval and consent to participate
This study was approved by the ethics committee of School of Stomatology, Capital Medical University. (No. CMUSH-IRB-KJ-PJ-2020-11) Written informed consent was obtained from all subjects.
Consent to publish
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Yanning Ma, Email: blueskyabc1007@163.com.
Song Li, Email: lisong325bk@163.com.
References
- 1.Zafar K, Nazeer MR, Ghafoor R. Interdisciplinary management of gingival recession and pathologic teeth migration-revisiting dental aesthetics. J Pak Med Assoc. 2019;69:1385–1389. [PubMed] [Google Scholar]
- 2.Brown LF, Ford PJ, Symons AL. Periodontal disease and the special needs patient. Periodontol. 2000;2017(74):182–193. doi: 10.1111/prd.12198. [DOI] [PubMed] [Google Scholar]
- 3.Gkantidis N, Christou P, Topouzelis N. The orthodontic-periodontic interrelationship in integrated treatment challenges: a systematic review. J Oral Rehabil. 2010;37:377–390. doi: 10.1111/j.1365-2842.2010.02068.x. [DOI] [PubMed] [Google Scholar]
- 4.Santosh TS, Srikanth K, Haritha D, Reddy ML, Parmar R. Need for speed in orthodontics: a review of noninvasive methods to accelerate the orthodontic tooth movement. Int J Oral Care Res. 2020;8:48. [Google Scholar]
- 5.Gyawali R, Bhattarai B. Orthodontic management in aggressive periodontitis. Int Sch Res Notices. 2017;2017:8098154. doi: 10.1155/2017/8098154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Re S, Corrente G, Abundo R, Cardaropoli D. Orthodontic treatment in periodontally compromised patients: 12-year report. Int J Periodontics Restorative Dent. 2000;20:31–39. [PubMed] [Google Scholar]
- 7.Tamer I, Oztas E, Marsan G. Orthodontic treatment with clear aligners and the scientific reality behind their marketing: a literature review. Turk J Orthod. 2019;32:241–246. doi: 10.5152/TurkJOrthod.2019.18083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Seo JH, Eghan-Acquah E, Kim MS, Lee JH, Jeong YH, Jung TG, et al. Comparative analysis of stress in the periodontal ligament and center of rotation in the tooth after orthodontic treatment depending on clear aligner thickness-finite element analysis study. Materials (Basel). 2021;14:324. doi: 10.3390/ma14020324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Levrini L, Mangano A, Montanari P, Margherini S, Caprioglio A, Abbate GM. Periodontal health status in patients treated with the Invisalign((R)) system and fixed orthodontic appliances: A 3 months clinical and microbiological evaluation. Eur J Dent. 2015;9:404–410. doi: 10.4103/1305-7456.163218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rossini G, Parrini S, Castroflorio T, Deregibus A, Debernardi CL. Periodontal health during clear aligners treatment: a systematic review. Eur J Orthod. 2015;37:539–543. doi: 10.1093/ejo/cju083. [DOI] [PubMed] [Google Scholar]
- 11.Ke Y, Zhu Y, Zhu M. A comparison of treatment effectiveness between clear aligner and fixed appliance therapies. BMC Oral Health. 2019;19:24. doi: 10.1186/s12903-018-0695-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zheng M, Liu R, Ni Z, Yu Z. Efficiency, effectiveness and treatment stability of clear aligners: a systematic review and meta-analysis. Orthodontics Craniofacial Res. 2017;20:127–133. doi: 10.1111/ocr.12177. [DOI] [PubMed] [Google Scholar]
- 13.Rossini G, Parrini S, Castroflorio T, Deregibus A, Debernardi CL. Efficacy of clear aligners in controlling orthodontic tooth movement: a systematic review. Angle Orthod. 2015;85:881–889. doi: 10.2319/061614-436.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Liu Y, Hu W. Force changes associated with different intrusion strategies for deep-bite correction by clear aligners. Angle Orthod. 2018;88:771–778. doi: 10.2319/121717-864.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Korioth TW, Versluis A. Modeling the mechanical behavior of the jaws and their related structures by finite element (FE) analysis. Crit Rev Oral Biol Med. 1997;8:90–104. doi: 10.1177/10454411970080010501. [DOI] [PubMed] [Google Scholar]
- 16.Middleton J, Jones M, Wilson A. The role of the periodontal ligament in bone modeling: the initial development of a time-dependent finite element model. Am J Orthod Dentofacial Orthop. 1996;109:155–162. doi: 10.1016/s0889-5406(96)70176-2. [DOI] [PubMed] [Google Scholar]
- 17.Tanne K, Hiraga J, Kakiuchi K, Yamagata Y, Sakuda M. Biomechanical effect of anteriorly directed extraoral forces on the craniofacial complex: a study using the finite element method. Am J Orthod Dentofacial Orthop. 1989;95:200–207. doi: 10.1016/0889-5406(89)90050-4. [DOI] [PubMed] [Google Scholar]
- 18.McGuinness NJ, Wilson AN, Jones ML, Middleton J. A stress analysis of the periodontal ligament under various orthodontic loadings. Eur J Orthod. 1991;13:231–242. doi: 10.1093/ejo/13.3.231. [DOI] [PubMed] [Google Scholar]
- 19.Geramy A. Initial stress produced in the periodontal membrane by orthodontic loads in the presence of varying loss of alveolar bone: a three-dimensional finite element analysis. Eur J Orthod. 2002;24:21–33. doi: 10.1093/ejo/24.1.21. [DOI] [PubMed] [Google Scholar]
- 20.Hayashi K, Araki Y, Uechi J, Ohno H, Mizoguchi I. A novel method for the three-dimensional (3-D) analysis of orthodontic tooth movement-calculation of rotation about and translation along the finite helical axis. J Biomech. 2002;35:45–51. doi: 10.1016/s0021-9290(01)00166-x. [DOI] [PubMed] [Google Scholar]
- 21.Jones ML, Hickman J, Middleton J, Knox J, Volp C. A validated finite element method study of orthodontic tooth movement in the human subject. J Orthod. 2001;28:29–38. doi: 10.1093/ortho/28.1.29. [DOI] [PubMed] [Google Scholar]
- 22.Lauritano F, Runci M, Cervino G, Fiorillo L, Bramanti E, Cicciu M. Three-dimensional evaluation of different prosthesis retention systems using finite element analysis and the Von Mises stress test. Minerva Stomatol. 2016;65:353–367. [PubMed] [Google Scholar]
- 23.Cervino G, Romeo U, Lauritano F, Bramanti E, Fiorillo L, D'Amico C, et al. Fem and Von Mises analysis of OSSTEM ((R)) dental implant structural components: evaluation of different direction dynamic loads. Open Dent J. 2018;12:219–229. doi: 10.2174/1874210601812010219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Crimi S, Defila L, Nanni M, Cicciu M, Fiorillo L, Cervino G, et al. Three-dimensional evaluation on cortical bone during orthodontic surgical treatment. J Craniofac Surg. 2020;31:1637–1646. doi: 10.1097/SCS.0000000000006592. [DOI] [PubMed] [Google Scholar]
- 25.Cervino G, Fiorillo L, Arzukanyan AV, Spagnuolo G, Cicciu M. Dental restorative digital workflow: digital smile design from aesthetic to function. Dent J (Basel). 2019;7:30. doi: 10.3390/dj7020030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cattaneo PM, Dalstra M, Melsen B. The finite element method: a tool to study orthodontic tooth movement. J Dent Res. 2005;84:428–433. doi: 10.1177/154405910508400506. [DOI] [PubMed] [Google Scholar]
- 27.McGuinness N, Wilson AN, Jones M, Middleton J, Robertson NR. Stresses induced by edgewise appliances in the periodontal ligament—a finite element study. Angle Orthod. 1992;62:15–22. doi: 10.1043/0003-3219(1992)062<0015:SIBEAI>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 28.Highfield J. Diagnosis and classification of periodontal disease. Aust Dent J. 2009;54(Suppl 1):S11–26. doi: 10.1111/j.1834-7819.2009.01140.x. [DOI] [PubMed] [Google Scholar]
- 29.Caton JG, Armitage G, Berglundh T, Chapple ILC, Jepsen S, Kornman KS, et al. A new classification scheme for periodontal and peri-implant diseases and conditions—introduction and key changes from the 1999 classification. J Clin Periodontol. 2018;45(Suppl 20):S1–S8. doi: 10.1111/jcpe.12935. [DOI] [PubMed] [Google Scholar]
- 30.Gomez JP, Pena FM, Martinez V, Giraldo DC, Cardona CI. Initial force systems during bodily tooth movement with plastic aligners and composite attachments: a three-dimensional finite element analysis. Angle Orthod. 2015;85:454–460. doi: 10.2319/050714-330.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Liu YF, Wang R, Baur DA, Jiang XF. A finite element analysis of the stress distribution to the mandible from impact forces with various orientations of third molars. J Zhejiang Univ Sci B. 2018;19:38–48. doi: 10.1631/jzus.B1600552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wolfram H, Antonia Z, Henning D, Julia FF, Susanne FZ, Rudolf G, et al. Torquing an upper central incisor with aligners–acting forces and biomechanical principles. Eur J Orthod. 2010;32:607–613. doi: 10.1093/ejo/cjq007. [DOI] [PubMed] [Google Scholar]
- 33.Singh A, Gill G, Kaur H, Amhmed M, Jakhu H. Role of osteopontin in bone remodeling and orthodontic tooth movement: a review. Prog Orthod. 2018;19:18. doi: 10.1186/s40510-018-0216-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cortona A, Rossini G, Parrini S, Deregibus A, Castroflorio T. Clear aligner orthodontic therapy of rotated mandibular round-shaped teeth: a finite element study. Angle Orthod. 2020;90:247–254. doi: 10.2319/020719-86.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hennessy J, Al-Awadhi EA. Clear aligners generations and orthodontic tooth movement. J Orthod. 2016;43:68–76. doi: 10.1179/1465313315Y.0000000004. [DOI] [PubMed] [Google Scholar]
- 36.Li X, Ren C, Wang Z, Zhao P, Wang H, Bai Y. Changes in force associated with the amount of aligner activation and lingual bodily movement of the maxillary central incisor. Korean J Orthod. 2016;46:65–72. doi: 10.4041/kjod.2016.46.2.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Tweed CH. Clinical orthodontics. Clin. Orthodontics. 1966;1:940.
- 38.Hollender L, Ronnerman A, Thilander B. Root resorption, marginal bone support and clinical crown length in orthodontically treated patients. Eur J Orthod. 1980;2:197–205. doi: 10.1093/ejo/2.4.197-a. [DOI] [PubMed] [Google Scholar]
- 39.Reed BE, Polson AM, Subtelny JD. Long-term periodontal status of teeth moved into extraction sites. Am J Orthod. 1985;88:203–208. doi: 10.1016/s0002-9416(85)90215-5. [DOI] [PubMed] [Google Scholar]
- 40.Kravitz ND, Kusnoto B, BeGole E, Obrez A, Agran B. How well does Invisalign work? A prospective clinical study evaluating the efficacy of tooth movement with Invisalign. Am J Orthod Dentofacial Orthop. 2009;135:27–35. doi: 10.1016/j.ajodo.2007.05.018. [DOI] [PubMed] [Google Scholar]
- 41.Boyd RL, Miller RJ, Vlaskalic V. The Invisalign system in adult orthodontics: mild crowding and space closure cases. J Clin Orthod. 2000;34:203–212. [Google Scholar]
- 42.Jeon PD, Turley PK, Ting K. Three-dimensional finite element analysis of stress in the periodontal ligament of the maxillary first molar with simulated bone loss. Am J Orthod Dentofacial Orthop. 2001;119:498–504. doi: 10.1067/mod.2001.112999. [DOI] [PubMed] [Google Scholar]
- 43.Cobo J, Arguelles J, Puente M, Vijande M. Dentoalveolar stress from bodily tooth movement at different levels of bone loss. Am J Orthod Dentofacial Orthop. 1996;110:256–262. doi: 10.1016/s0889-5406(96)80008-4. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.