Abstract
Background:
Post-cancer work limitations may impact a substantial portion of patients and contribute to the “financial toxicity” of cancer treatment. The degree and nature of work limitations and employment outcomes are poorly understood for cancer patients, particularly in the immediate period of transition after active treatment. We prospectively examined employment, work ability, and work limitations during and following treatment.
Methods:
A sample of N=120 patients receiving curative therapy who were employed prior to diagnosis and intended to work during or after end-of-treatment (EOT) completed surveys at baseline (pre-chemotherapy), EOT, and 3-, 6-, and 12-months post EOT. Surveys included measures of employment, work ability, and work limitations. Descriptive statistics (frequencies, percentages, means with standard deviations) were calculated.
Results:
A total of 111 participants completed the baseline survey. On average, participants were 48 years old, and largely white (95%), female (82%) with a breast (69%) cancer diagnosis. Full time employment decreased during therapy (from 88% to 50%) and returned to near pre-diagnosis levels by 12-months follow-up (78%). Work-related productivity loss due to health was high during treatment.
Conclusions:
This study is the first to report the impact of curative-intent cancer therapy on employment, work ability and work limitations both during and after treatment. Perceived work ability was generally high overall 12-months after EOT, although a minority reported persistent difficulty. Analysis of factors (e.g., job type, education, symptoms) most associated with work limitations is underway to assist in prospectively identifying at-risk patients.
Keywords: return to work, cancer survivorship, cancer work limitations, working during cancer treatment
Precis:
Adjuvant therapy for cancer can negatively impact the ability to work, but the degree of work limitation due to cancer treatment has not been prospectively captured in a longitudinal fashion. This prospective study examines cancer patients receiving adjuvant chemotherapy who worked during cancer treatment and found that most eventually returned to the same level of work as pre-chemotherapy.
Introduction
The financial burden surrounding cancer treatment has been termed “financial toxicity” and is associated with treatment delay, discontinuation or lack of adherence as well as distress.[1–5] A potential contributor to cancer-related financial toxicity is the negative impact of cancer diagnosis and treatment on the ability to participate in employment activities (“work ability”). According to the US government, individuals are considered employed if they did any work at all for pay or profit.[6] Patients with cancer are more likely than individuals without a history of cancer to experience employment-related difficulties, such as inability to work or experiencing employment disability.[7–14] Prior research suggests that post-diagnosis unemployment may be partially driven by work limitations that arise as a result of cancer treatment.[15–18] Work limitations could range from a mild and transient impact (e.g. a 4-week surgical recovery) to persistent, long-term dysfunction (e.g. persistent neuropathy) that results in reduced work ability or productivity. At their most extreme, work limitations manifest as inability to work and/or unemployment. Work limitations following cancer diagnosis likely represent a significant and underappreciated cost to individuals, employers and society: cancer is a leading cause of disability claims, with workplace discrimination cited as a major concern by some, and with substantial possible economic burden from cancer survivorship.[19, 20]
Work ability reflects a complex interaction of individual and occupational factors.[21] Individual factors associated with employment outcomes may include education, income, marital status, race, rurality and age.[13, 16, 22–25] Occupational factors may include physical, cognitive, and interpersonal work demands, company size, co-worker support, and flexibility of work hours and work tasks.[26] These interactions may be further complicated by disease-specific factors, including stage/type/location of disease, cancer therapies, and related acute and chronic symptoms.[16, 25, 27] Work limitations related to cancer or treatments might result in employment instability (e.g. change in job or employer), under-employment (e.g. accepting less demanding or part-time positions), or non-employment (e.g. early retirement, loss of employment).[16, 25] However, the literature often focuses on employment as a simple dichotomous outcome (employed vs unemployed); the variations in employment laws by country may also confound outcomes.[21, 28] Furthermore, the published literature often assesses survivors in cross-sectional surveys: data suggests that difficulties seen at 6–12 months post-treatment predict difficulty at later time points [13] but the inclusion of those years removed from diagnosis may increase response bias.[17, 22, 23]
This study sought to address gaps in the literature by collecting data longitudinally: prior to chemotherapy, during treatment and for the 12-month period after completing cancer treatment. The purpose of this prospective survey study was to describe employment, work ability and work limitations experienced by patients with cancer during and after curative cancer treatment, when longer-term work limitations are likely to have emerged.
Methods
Participants and Setting.
We conducted a prospective longitudinal survey study. Patients were recruited from eight outpatient community and academic oncology practices through the Wisconsin Oncology Network (WON). Eligible patients were 18 years of age or older, diagnosed with a solid tumor malignancy or a lymphoma, for which they would receive curative-intent chemotherapy. Patients had to be working for pay at least 20 hours per week at the time of diagnosis, and had to intend to work during treatment or return to work within 3 months after completing treatment. Chemotherapy could be either neoadjuvant or adjuvant, but participants could not have received more than a single curative-intent cycle for their current diagnosis at the time of enrollment. All participants provided written informed consent and received a small financial incentive ($20) for completing surveys at the end of their participation.
Instruments.
The baseline survey obtained participants’ race, marital status, education, insurance status, annual household income, primary breadwinner status, number of dependents, and zip code. Data including cancer type, stage, treatment received, and dates of any recurrences or death were abstracted from participants’ medical records by research staff. The MD Anderson Symptom Inventory was used to assess symptom burden.[16, 25]
Employment was measured using a single item derived from the Eastern Cooperative Oncology Group’s (ECOG) “Symptom Outcomes Assessment Practice Patterns” study which asked, “What best describes your level of employment currently?”[16, 25] The single item Work Ability Score (WAS) from the Work Ability Index (WAI) was used to assess participants’ perceptions of how well they would be able to perform their work tasks, taking into consideration the demands of the work, their health status, and available resources. The WAS is a single item rating current work ability from 0 (completely unable) to 10 (work ability at its best).[29, 30] The Work Limitation Questionnaire (WLQ) was used to assess the degree to which health problems interfere with job performance and productivity. Participants rate how frequently in the past two weeks they have had difficulty with aspects of job performance using a 5-point Likert scale. A composite of weighted subscale scores is used to create the overall WLQ Productivity Loss score, reflecting the percentage loss in work productivity due to health (100% = complete loss of work productivity; 0% = no loss in work productivity).[31] The Job Content Questionnaire (JCQ) was used to assess social and psychological characteristics of participants’ jobs such as decision latitude, perceived stability, etc.[32]
Procedures.
The study was approved by the Health Sciences Institutional Review Board (IRB) at the University of Wisconsin-Madison and the IRBs of participating WON sites. At each site, a research staff member approached eligible patients, explained the study, and obtained written informed consent for participation. Following consent, participants were invited to complete the baseline survey online, either in clinic, using a computer or tablet provided by research staff, or outside clinic, using the participants’ own internet-connected device. Internet survey links were emailed to those participants completing the survey outside of the clinic setting. All survey data were collected and managed using the secure REDCap electronic data capture tools hosted at the University of Wisconsin-Madison, School of Medicine and Public Health.[33] The baseline survey included demographic data, the MDASI, the employment question, WAI, WLQ, JCQ, and additional work questions. Subsequent surveys included the same questionnaires, with the exception of demographic data and the JCQ (collected only at baseline). All surveys are available in Supplemental Material 1.
Post-baseline surveys were collected at multiple time points depending on the participant’s treatment plan – after completion of chemotherapy and before beginning the next primary treatment (e.g., radiation or surgery), after completing adjuvant radiation and/or surgery (if applicable), and at 3-, 6-, and 12-months after completion of all treatment. Differing sequences for chemotherapy, surgery and/or radiation were possible, so the “end-of-treatment (EOT)” was defined in our study as the last day of receiving any curative intent surgery, chemotherapy and radiation, though endocrine or other targeted therapies (e.g., trastuzumab) might still be ongoing.
Statistical Analyses.
Data were analyzed using SPSS, version 25 and R version 3.6.3. Summary statistics were calculated at baseline, end of treatment, and month 3, 6, and 12 post-EOT. Dichotomous variables were summarized as counts and percentages out of those completing the baseline survey, and continuous variables were summarized as means, standard deviations (SD), and ranges. P-values for longitudinal change were calculated using (generalized) linear mixed effects models with random subject effect and fixed, categorical timepoint effect. Sensitivity analyses were conducted in the cohort of subjects with complete data at all time points; no qualitative differences in results were noted.
Results
Sample characteristics (Table 1).
Table 1.
Demographic Characteristics of Participants at Baseline (n=111)
| Characteristic | Mean (SD) |
|---|---|
| Age | 48.2 (8.9) |
| Number of dependent children | 1.9 (1.1) |
| Symptom severity (0–10) | 1.8 (1.5) |
| Symptom distress (0–10) | 2.0 (2.0) |
| n (%)* | |
| Race | |
| White | 106 (95%) |
| Non-White | 3 (3%) |
| Gender | |
| Female | 91 (82%) |
| Male | 18 (16%) |
| Education | |
| High school or less | 27 (24%) |
| Some college | 29 (26%) |
| ≥ 4 yrs college | 54 (49%) |
| Marital Status | |
| Married / partnered | 82 (74%) |
| Widowed, Divorced, Single | 29 (26%) |
| Insured | |
| Yes | 109 (98%) |
| No | 2 (2%) |
| Primary Breadwinner | |
| Yes | 52 (47%) |
| No | 53 (48%) |
| Prefer not to answer | 5 (5%) |
| Living with Dependents (child or adult) | |
| Yes | 52 (47%) |
| No | 59 (53%) |
| Total Household Income | |
| < $50,000/year | 28 (25%) |
| $50,000–75,000/ year | 22 (20%) |
| $75,000–150,000/ year | 37 (33%) |
| >$150,000/ year | 16 (14%) |
| Employment Status | |
| Working, Full-Time (>35 hours/week) | 61 (55%) |
| Working, Part-Time (1–35 hours/week) | 18 (16%) |
| Employed, but Not Working | 31 (28%) |
| Looking for Work | 0 (0%) |
| Not in workforce | 1 (1%) |
| Place of Residence | |
| Urban | 75 (68%) |
| Rural | 31 (28%) |
Some percentages do not sum to 100% due to missing data and/or because participants indicated “I prefer not to answer”.
We consented 120 participants between May 2013 and October 2015. Five participants were determined ineligible following enrollment, and 4 participants did not complete a baseline survey. Of the 111 participants with a baseline survey, 95 completed the EOT survey (86%), 96 completed the 3-month follow-up (86%), 79 completed the 6-month follow-up (71%), and 73 completed the 12-month follow-up survey (66%). When possible, we captured cancer progression and/or death (2 and 2 participants respectively; progressing participants did not receive further surveys). The majority of participants (n=86, 77%) were White, non-Hispanic females, but they did span a range of educational attainment and total annual household income. With regards to cancer type, 77 participants (69%) had breast cancer, 15 (14%) had colorectal cancer, and 17 (15%) had other cancers including lymphoma, lung, testicular, or head and neck cancers. Two participants (2%) were missing this medical record information. With regards to treatment modalities, 49 participants (44%) received chemotherapy, surgery and radiation, 31 (28%) received chemotherapy and surgery, 8 (7%) received chemotherapy and radiation, and 13 (12%) received chemotherapy alone. Ten participants (9%) were missing full medical record data.
Job Characteristics (Table 2).
Table 2.
Participant Job Characteristics at Baseline (n=111) from Job Content Questionnaire (JCQ)
| Job Characteristic | n (%)* |
|---|---|
| Job Type | |
| Professional | 40 (36%) |
| Management / Administration | 19 (17%) |
| Technical | 9 (8%) |
| Clerical | 12 (11%) |
| Service | 8 (7%) |
| Other | 22 (20%) |
| Years in current job | |
| < 1 year | 4 (4%) |
| 1–5 years | 30 (27%) |
| 5–14 years | 42 (38%) |
| 15–24 years | 20 (18%) |
| 25–39 years | 15 (14%) |
| Size of company | |
| < 15 people | 22 (20%) |
| 15–100 people | 22 (20%) |
| 101–500 people | 22 (20%) |
| 501–1000 people | 13 (12%) |
| > 1000 people | 31 (28%) |
| Size of work group/unit | |
| Work alone | 10 (9%) |
| 2–5 people | 32 (29%) |
| 6–10 people | 29 (26%) |
| 10–20 people | 21 (19%) |
| 20 or more people | 18 (16%) |
| Difficulty changing hours | |
| Very difficult to change hours | 23 (21%) |
| Changes approved for special situations | 33 (30%) |
| Schedule is already flexible | 54 (49%) |
| Level of skill required | |
| Junior high school education | 3 (3%) |
| High school graduate | 28 (25%) |
| Some college education | 29 (26%) |
| College graduate | 42 (38%) |
| Graduate school | 8 (7%) |
| JCQ Subscale Scores (possible range) | Mean (SD) |
| Decision Latitude (24–96) | 73.8 (13.6) |
| Psychological job demands (12–48) | 32.8 (5.4) |
| Physical job demands (5–20) | 9.6 (3.7) |
| Coworker support (4–16) | 13.1 (2.1) |
| Supervisor support (4–16) | 12.2 (2.7) |
| Job insecurity (3–12) | 4.8 (1.5) |
Some percentages do not sum to 100% due to missing data.
Participants were required to be working for pay at diagnosis, but were not required to be working at enrollment. As such, roughly one-third (n=32, 29%) reported not working or not being in the workforce on the baseline survey, likely reflecting leave taken following diagnosis to permit healthcare visits, testing and/or surgery. The majority of participants were working in professional, managerial, or administrative jobs and perceived a moderate-to-high degree of decision latitude in their work (mean 78.8, SD=13.6, range 24–96), had more psychological (mean 32.8, SD=5.4, range 12–48) than physical (mean 9.6, SD=3.7, range 5–20) job demands, and perceived a moderate-to-high degree of supervisor (mean 12.2, SD=2.7, range 4–16) and co-worker (mean 13.1, SD=2.1, range 4–16) support as assessed by the JCQ. Their overall sense of job insecurity was low (mean 4.8, SD=1.5, range 3–12). Of note, non-respondents to the 12 months survey were more likely to report “other” for job type at baseline than respondents (48% vs 13%, p=0.04).
Employment, Hours Worked and Missed Work During and After Cancer Treatment (Table 3).
Table 3.
Employment, Hours Worked, and Missed Work by Study Time Point
| Employment | Before Diagnosis | Baseline | EOT | 3-month | 6-month | 12-month |
|---|---|---|---|---|---|---|
| Level of employment,1 n (%) | ||||||
| Working, Full-Time (>35 hrs per week) | 98 (88%) | 61 (55%) | 55 (58%) | 67 (70%) | 59 (75%) | 57 (78%) |
| Working, Part-Time (1–35 hrs per week) | 12 (11%) | 18 (16%) | 25 (26%) | 17 (18%) | 16 (20%) | 11 (15%) |
| Not in the workforce (e.g., retired, disabled) | 0 (0%) | 1 (1%) | 1 (1%) | 1 (1%) | 2 (3%) | 3 (4%) |
| Employed but not working (e.g., on leave) | 0 (0%) | 31 (28%) | 14 (15%) | 9 (9%) | 0 (0%) | 1 (1%) |
| Not in the workforce but looking for work | 0 (0%) | 0 (0%) | 0 (0%) | 2 (2%) | 2 (3%) | 1 (1%) |
| Time Worked, Mean (SD) | ||||||
| Average number of hours worked / week2 | 42.05 (7.04) | -- | 33.0 (17.0) | 36.8 (18.7) | 38.1 (13.8) | 38.2 (14.6) |
| Number of FULL work days missed3 | -- | -- | 1.8 (3.3) | 1.1 (3.0) | 0.6 (1.9) | 0.5 (1.9) |
| Number of PARTIAL work days missed4 | -- | -- | 2.0 (3.4) | 1.1 (2.5) | 0.6 (1.1) | 0.7 (2.3) |
Abbreviations: SD= standard deviation; EOT= end of treatment
Baseline survey asked: “What best describes your level of employment BEFORE being told about the cancer? And What best describes your level of employment CURRENTLY?”
Baseline survey asked: “On average, how many hours per week did you work BEFORE being told about the cancer?; Follow-up surveys asked: Over the past 2 weeks, how many hours per week did you work?”
Follow-up surveys asked: “In the past 2 weeks, how many FULL WORKDAYS did you miss because of your health or medical care?”
Follow-up surveys asked: “In the past 2 weeks, what was the total number of days on which you missed PART OF A WORKDAY because of your health or medical care (for example, you came in late or left early)?”
The percentage of participants working full-time changed significantly over the period of observation (p<0.001), decreasing during cancer treatment, from 88% before diagnosis to approximately 50% during treatment, and then gradually increasing during follow-up to 78% at 12 months post-treatment. The percentage of persons working part-time did not change significantly over time (p=0.10), though there was a trend towards the opposite pattern with a small increase from 11% before diagnosis to 26% at the end of treatment and decrease over the follow-up period to 15% at 12 months post-treatment. Nearly one-third of patients described themselves as “employed but not working” during the period of cancer treatment. However, those numbers quickly decreased (p<0.001), with 9% “employed but not working” at 3 months, and only 1% at 12 months post-treatment. The number of hours worked also changed significantly (p<0.001), declining from a mean of 42 reported hours/week pre-diagnosis to 33 hours/week at EOT, and returned to near baseline by 12 months post-treatment (38 hours/week). While receiving treatment, participants missed approximately 2 full and 2 partial work days in the 2 weeks prior to reporting. Both numbers were halved at 3-months post-treatment (1 full and 1 partial day missed) and decreased further at 6- and 12-months post-treatment to an average of 0.5 days.
Work Ability and Limitations.
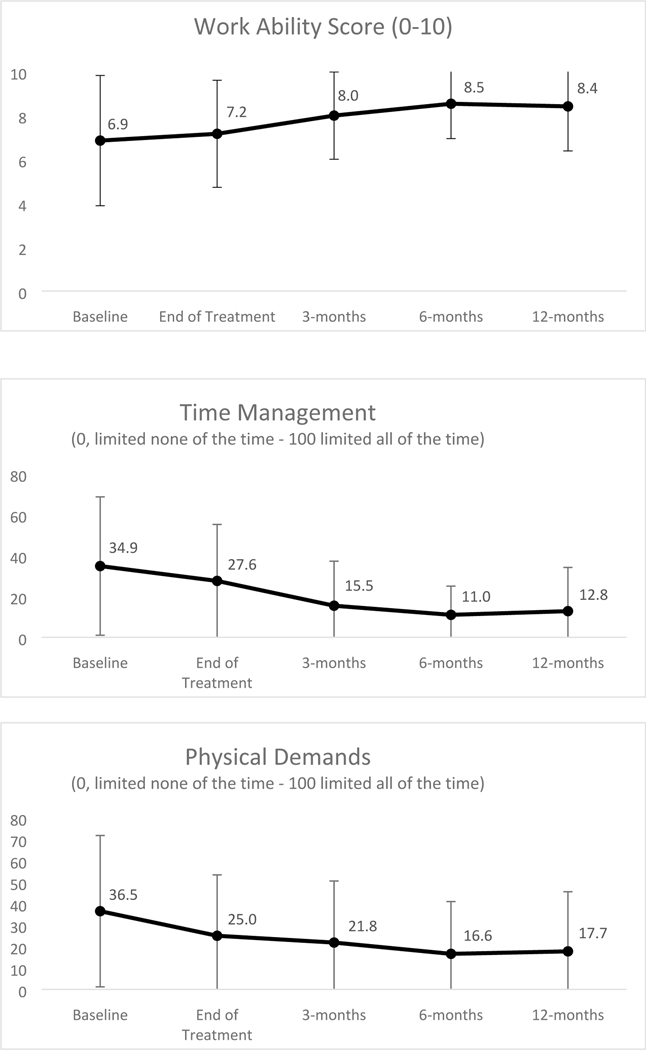
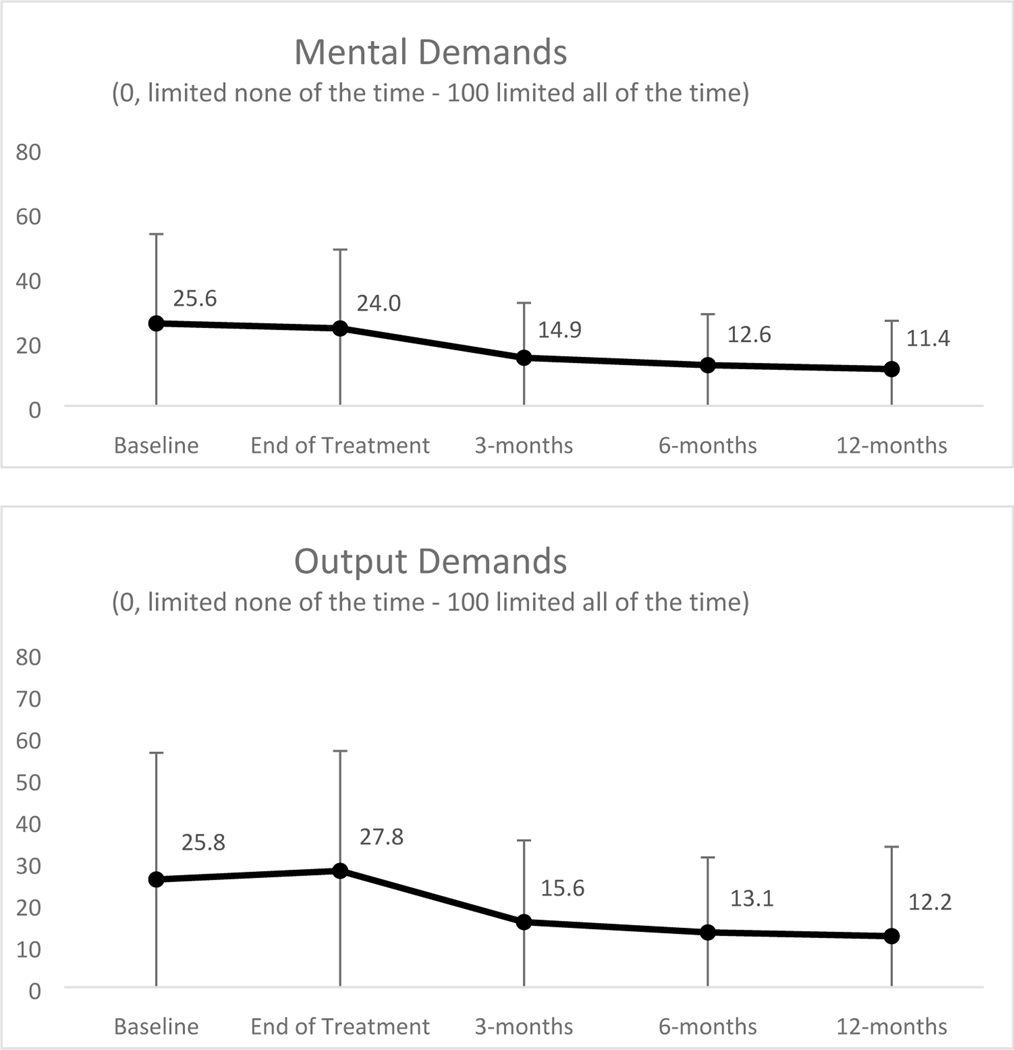
Participants’ self-reported work ability score (WAS; range 0 = completely unable to work, 10 = work ability at its best) was moderate at baseline (mean 6.9, SD=3.0) and EOT (mean 7.2, SD=2.5), but showed improvement over time (p<0.001, see Figure 1). Work-related productivity loss due to health changed significantly (p<0.001) as well. It was high during treatment, with the highest losses at baseline (mean 91%) and at EOT (mean 86%), and gradually improved, but remained impacted at 3-months (mean 75%), 6-months (mean 68%), and 12-months (mean 65%) post-treatment. Similar trends demonstrating decreasing but persistent limitations in time and scheduling demands, physical demands, mental-interpersonal demands, and output demands (WLQ subscales) are depicted in Figure 1.
Figure 1.
a. Mean Work Ability Score with Standard Deviation by Study Time Point b-e. Mean WLQ Subscale Scores with Standard Deviation by Study Time Point
Participant perceptions of work related to treatment.
The majority of participants reported that they continued working because they needed or wanted to (86–91% depending on timepoint of survey). The majority of participants were satisfied with the amount of time off they had received, but one-quarter to one-third would have liked more time off before chemotherapy, during radiation, and at each of the post-treatment follow-up points. Use of benefits was most frequent at baseline and during chemotherapy, with 40–48% using sick leave, 25–32% using short-term disability, and 14–20% using unpaid time off. At baseline, only 35% used no benefits, and after chemotherapy, only 22% had used no benefits. After radiation, and at the 3-, 6-, and 12-month follow-ups, > 50% used no benefits. Participants were generally satisfied with how things were going at work since cancer and treatment (M=3.96–4.23 on 1–5 scale). Supervisors and co-workers knew of the diagnosis for the vast majority (≥ 90%) of participants.
Discussion
We conducted this prospective survey study to better understand the impact of curative-intent cancer therapy on employment, work limitations and work ability. Our results demonstrate that cancer survivors can be accrued and retained to employment and financial toxicity survey trials during active cancer treatment, at least when accrued through medical oncology clinics. However, we did need to amend the protocol early on to permit receipt of a single cycle of chemotherapy, as the local research teams reported that potentially eligible patients felt overwhelmed and unable to add “one more thing” as they contemplated starting chemotherapy. Not unexpectedly, the baseline and EOT timepoints therefore revealed the highest degree of cancer-related work limitations. The significant impact on work ability seen in the baseline scores also likely reflects the fact that many of these participants would have spent the preceding few weeks undergoing diagnostic testing with the associated anxiety and/or stress, as well as the fact that participants could have already undergone surgery and received up to 1 cycle of chemotherapy.
In this Midwestern population, participant self-reported work ability and self-reported work limitation remained relatively diminished but without deterioration despite ongoing therapy from baseline to EOT. Our inclusion criteria required that participants intend to work either during or following treatment, which while a reasonable requirement given the purpose of the study, may have selected participants for whom work was more central to their self-identity. Common free-text responses reflected that participants strongly enjoyed their work, felt like work was part of their identity, or felt responsible for work (business owner, self-employed, need to keep up, others dependent). Work ability and the degree of work limitation then steadily improved starting at 3 months and extending over the 12-month post-treatment timeframe. While many patients changed employment from full-time to part-time or took a leave from work during treatment, most reported being back to pre-diagnosis work hours by 6 months post-treatment. This rate of returning to work is higher than that seen in other prospective studies such as the CANTO study, where 21% of breast cancer patients had not returned to work 2 years following diagnosis despite the fact that only about half received chemotherapy.[28] Despite our findings, participant-perceived productivity loss was high and did remain elevated at 12 months post-treatment. This could reflect the fact that our baseline surveys do not capture “pre-diagnosis” work ability, as well as the fact that sustaining pre-diagnosis work ability may require more effort post-treatment.
This study is unique in that it was designed to prospectively capture the work experiences of patients with cancer as they moved from diagnosis through curative-intent therapy in a U.S.-based cohort. Similar to the French CANTO study, we deliberately tailored survey timepoints to follow treatment schedules rather than being cross-sectional calendar timepoints.[28] While this added to the heterogeneity of the actually timing of the surveys, it means that for surveys completed after the EOT, participants were all at similar time-frames out from treatment. Furthermore, this study recruited largely from community oncology practices (86%), and included a significant proportion of rural participants and a distribution of income and educational attainment (Table 1). Rural breast cancer patients may be more likely to report employment effects, including reduced household income.[23]
Limitations include that our participants are largely White despite inclusion of a site serving a predominantly African-American population. Studies conducted in racial or ethnic minority and/or rural populations have reported more financial implications or employment difficulties following cancer.[13, 14, 23] Studies may also be confounded by lack of information on educational attainment, income, job types and job flexibility.[26] For instance, low job flexibility has been linked to poorer post-cancer employment outcomes[26], and survivors engaged in manual work are less likely to have flexibility with reducing hours or accommodating employers.[34][26] Although diverse from an educational and income perspective, many of our study participants were in professional positions with relative job flexibility. It is possible that participants with high job demands or little flexibility were less able or less inclined to participate. The difference in baseline job types between responders and non-responders at 12 months suggests that this might have been an issue. Thus, our study may under-represent the work limitations and over-represent the work ability that would occur in other populations. An additional limitation is the relative over-participation for breast cancer patients (our initial goal was to recruit more equal numbers of breast, colon and “other” patients by holding spots specifically for non-breast patients), which adds potential confounding with regards to differential impacts on work and employment based on gender. Finally, we did not accrue most patients before any treatment had been rendered (e.g. many patients had had at least 1 dose of chemotherapy and/or a surgery).
This novel study examined the impact of curative-intent therapy on work limitations and ability, as well as on employment in a US-based cohort. Ongoing analyses are exploring differences among sub-populations with different patterns of employment, work ability and work limitations as well as the association between symptom burden and work limitations. Ultimately, we hope to design an intervention that can be embedded within oncology clinics to help address work ability and off-set contributions to financial toxicity.
Supplementary Material
Acknowledgements:
The authors thank the patients, participating healthcare professionals, members of the UW Breast Disease Oriented Team (DOT) and the UWCCC Survivorship Program.
Funding: This work was supported by the NCI Cancer Center Support Grant P30 CA014520. AJT and MES received support from the Clinical and Translational Science Award (CTSA) program via NIH National Center for Advancing Translational Sciences (NCATS), grants UL1TR000427and KL2TR000428.
Footnotes
Disclosures: The authors report no conflicts of interest and no disclosures.
References
- 1.Zafar SY and Abernethy AP, Financial toxicity, Part II: how can we help with the burden of treatment-related costs? Oncology (Williston Park), 2013. 27(4): p. 253–4, 256. [PubMed] [Google Scholar]
- 2.Zafar SY and Abernethy AP, Financial toxicity, Part I: a new name for a growing problem. Oncology (Williston Park), 2013. 27(2): p. 80–1, 149. [PMC free article] [PubMed] [Google Scholar]
- 3.Zafar SY, et al. , The financial toxicity of cancer treatment: a pilot study assessing out-of-pocket expenses and the insured cancer patient’s experience. Oncologist, 2013. 18(4): p. 381–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Carrera PM, Kantarjian HM, and Blinder VS, The financial burden and distress of patients with cancer: Understanding and stepping-up action on the financial toxicity of cancer treatment. CA Cancer J Clin, 2018. 68(2): p. 153–165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Board., P.A.T.E., Financial Toxicity and Cancer Treatment (PDQ®): Health Professional Version. PDQ Cancer Information Summaries [Internet]. Bethesda (MD): National Cancer Institute (US); Available from: https://www.ncbi.nlm.nih.gov/books/NBK384502, 2019. September 18. [Google Scholar]
- 6.statistics, U.S.B.o.L. https://www.bls.gov/ [cited 2020 March 31]. [Google Scholar]
- 7.Yabroff KR, et al. , Financial Hardship Associated With Cancer in the United States: Findings From a Population-Based Sample of Adult Cancer Survivors. J Clin Oncol, 2016. 34(3): p. 259–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Steiner JF, et al. , Assessing the impact of cancer on work outcomes: what are the research needs? Cancer, 2004. 101(8): p. 1703–11. [DOI] [PubMed] [Google Scholar]
- 9.Finkelstein EA, et al. , The personal financial burden of cancer for the working-aged population. Am J Manag Care, 2009. 15(11): p. 801–6. [PubMed] [Google Scholar]
- 10.Guy GP Jr., et al. , Economic burden of cancer survivorship among adults in the United States. J Clin Oncol, 2013. 31(30): p. 3749–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Moran JR, Short PF, and Hollenbeak CS, Long-term employment effects of surviving cancer. J Health Econ, 2011. 30(3): p. 505–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bouknight RR, Bradley CJ, and Luo Z, Correlates of return to work for breast cancer survivors. J Clin Oncol, 2006. 24(3): p. 345–53. [DOI] [PubMed] [Google Scholar]
- 13.Jagsi R, et al. , Impact of adjuvant chemotherapy on long-term employment of survivors of early-stage breast cancer. Cancer, 2014. 120(12): p. 1854–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jagsi R, et al. , Long-term financial burden of breast cancer: experiences of a diverse cohort of survivors identified through population-based registries. J Clin Oncol, 2014. 32(12): p. 1269–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sun W, et al. , Work-related barriers, facilitators, and strategies of breast cancer survivors working during curative treatment. Work, 2016. 55(4): p. 783–795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tevaarwerk AJ, et al. , Employment outcomes among survivors of common cancers: the Symptom Outcomes and Practice Patterns (SOAPP) study. J Cancer Surviv, 2013. 7(2): p. 191–202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hansen JA, et al. , Breast cancer survivors at work. J Occup Environ Med, 2008. 50(7): p. 777–84. [DOI] [PubMed] [Google Scholar]
- 18.Sesto ME, et al. , Employment and retirement status of older cancer survivors compared to non-cancer siblings. Work, 2013. 46(4): p. 445–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ekwueme DU, et al. , Medical costs and productivity losses of cancer survivors--United States, 2008–2011. MMWR Morb Mortal Wkly Rep, 2014. 63(23): p. 505–10. [PMC free article] [PubMed] [Google Scholar]
- 20.Feuerstein M, et al. , Pattern of workplace disputes in cancer survivors: a population study of ADA claims. J Cancer Surviv, 2007. 1(3): p. 185–92. [DOI] [PubMed] [Google Scholar]
- 21.Mehnert A, de Boer A, and Feuerstein M, Employment challenges for cancer survivors. Cancer, 2013. 119 Suppl 11: p. 2151–9. [DOI] [PubMed] [Google Scholar]
- 22.Tangka FKL, et al. , Insurance Coverage, Employment Status, and Financial WellBeing of Young Women Diagnosed with Breast Cancer. Cancer Epidemiol Biomarkers Prev, 2020. 29(3): p. 616–624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Spencer JC, et al. , Employment changes following breast cancer diagnosis: the effects of race and place. J Natl Cancer Inst, 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wheeler SB, et al. , Financial Impact of Breast Cancer in Black Versus White Women. J Clin Oncol, 2018. 36(17): p. 1695–1701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tevaarwerk AJ, et al. , Working after a metastatic cancer diagnosis: Factors affecting employment in the metastatic setting from ECOG-ACRIN’s Symptom Outcomes and Practice Patterns study. Cancer, 2016. 122(3): p. 438–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Blinder V, et al. , Women With Breast Cancer Who Work For Accommodating Employers More Likely To Retain Jobs After Treatment. Health Aff (Millwood), 2017. 36(2): p. 274–281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rotter J, Spencer JC, and Wheeler SB, Financial Toxicity in Advanced and Metastatic Cancer: Overburdened and Underprepared. J Oncol Pract, 2019. 15(4): p. e300–e307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Dumas A, et al. , Impact of Breast Cancer Treatment on Employment: Results of a Multicenter Prospective Cohort Study (CANTO). J Clin Oncol, 2020. 38(7): p. 734–743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ahlstrom L, et al. , The work ability index and single-item question: associations with sick leave, symptoms, and health--a prospective study of women on long-term sick leave. Scand J Work Environ Health, 2010. 36(5): p. 404–12. [DOI] [PubMed] [Google Scholar]
- 30.Schouten LS, et al. , Shortened version of the work ability index to identify workers at risk of long-term sickness absence. Eur J Public Health, 2016. 26(2): p. 301–5. [DOI] [PubMed] [Google Scholar]
- 31.Tang K, et al. , Measures of work disability and productivity: Rheumatoid Arthritis Specific Work Productivity Survey (WPS-RA), Workplace Activity Limitations Scale (WALS), Work Instability Scale for Rheumatoid Arthritis (RA-WIS), Work Limitations Questionnaire (WLQ), and Work Productivity and Activity Impairment Questionnaire (WPAI). Arthritis Care Res (Hoboken), 2011. 63 Suppl 11: p. S337–49. [DOI] [PubMed] [Google Scholar]
- 32.Karasek R, et al. , The Job Content Questionnaire (JCQ): an instrument for internationally comparative assessments of psychosocial job characteristics. J Occup Health Psychol, 1998. 3(4): p. 322–55. [DOI] [PubMed] [Google Scholar]
- 33.Harris PA, et al. , Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform, 2009. 42(2): p. 377–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ekenga CC, et al. , Long-Term Employment Outcomes among Female Cancer Survivors. Int J Environ Res Public Health, 2020. 17(8). [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.