Abstract
In the latest issues of Cell Host & Microbe and Cell, three articles describe new mutations in the SARS-CoV-2 Spike receptor binding domain that escape neutralizing responses. These highlight the importance of surveillance of SARS-CoV-2 evolution to anticipate and manage new variants that could impact reinfection, vaccine efficacy, and immunotherapies.
In the latest issues of Cell Host & Microbe and Cell, three articles describe new mutations in the SARS-CoV-2 Spike receptor binding domain that escape neutralizing responses. These highlight the importance of surveillance of SARS-CoV-2 evolution to anticipate and manage new variants that could impact reinfection, vaccine efficacy, and immunotherapies.
Main text
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) entry, mediated by the trimeric viral Spike glycoprotein, is the first step of the viral replication cycle. The mature SARS-CoV-2 Spike trimer is composed of the exterior S1 and transmembrane S2 subunits. The S1 subunit mediates attachment using its receptor-binding domain (RBD) to interact with the host protein angiotensin converting enzyme 2 (ACE2), while the S2 subunit governs the fusion between the viral and cellular membranes. Hence, Spike plays a central role in viral replication and is of particular interest due to its abundance at the surface of virions and infected cells and its high immunogenicity. Spike is considered the major target of the cellular and humoral responses against SARS-CoV-2 upon natural infection. Accordingly, the majority of current vaccine strategies (including mRNA-based and viral vector-based vaccines) are mostly focused on the elicitation of anti-Spike immunity. Similarly, interventional immunotherapies are largely directed against Spike with clinical trials testing the therapeutical benefits of convalescent plasma (or hyperimmune immunoglobulins) (NCT04381936, NCT04348656, NCT04362176, and NCT04546581), monoclonal antibodies (NCT04452318, NCT04497987, NCT04501978, and NCT04625972), and soluble ACE2 receptor decoy (NCT04335136). At the other end, the virus can mutate and generate new variants to escape different selective conditions. Given the relatively low mutation rate of Coronaviruses, emergence and selection for new Spike variants are most likely due to evading immune pressures that could otherwise compromise the favorable replication environment that it encounters in the human population.
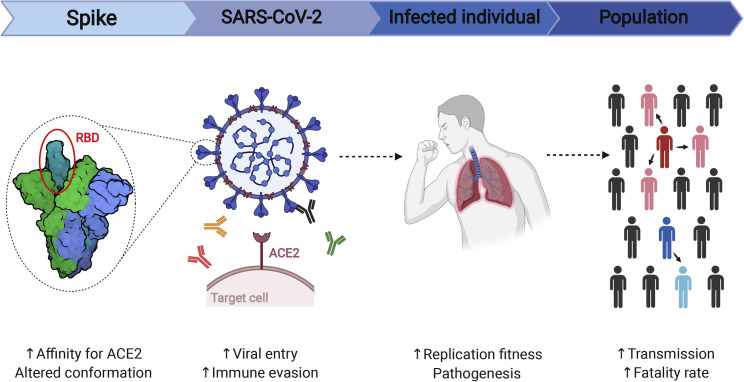
In vitro selection of SARS-CoV-2 escape variants by monoclonal neutralizing antibodies was initially performed using serial passages of replication-competent chimeric SARS-CoV-2 viruses (Weisblum et al., 2020) or by deep-mutational scanning using RBD libraries (Starr et al., 2021). Liu et al., Greaney et al., and Thomson et al. use complementary approaches to isolate and characterize preoccupying escape mutations that can evade polyclonal neutralizing responses from convalescent individuals (Greaney et al., 2021; Liu et al., 2021; Thomson et al., 2021). Using a traditional approach, Liu et al. generated escape variants in vitro by culturing a VSV-SARS-CoV-2 chimeric virus in presence of a panel of anti-RBD monoclonal neutralizing antibodies (Liu et al., 2021). Greaney et al. used a yeast surface display system to efficiently screen for RBD variants with reduced convalescent plasma binding (Greaney et al., 2021). Using epidemiological data, Thomson et al. identified in vivo-selected escape variants from circulating SARS-CoV-2 strains (Thomson et al., 2021). Strikingly, these three complementary approaches identified key mutations in the receptor-binding motif (RBM) of the Spike RBD negatively impacting convalescent plasma neutralizing activity (i.e., E484K and N439K). As pointed out by Thomson et al., the RBM represents a major sequence variation hotspot, consistent with its immunodominant nature as a primary target for neutralizing antibodies. Surveillance of recent arisen RBM mutations are of particular interest because of their apprehended effect on SARS-CoV-2 replication. As such, while evading immune pressure, in some cases RBM variants can increase viral entry by increasing the affinity for the ACE2 receptor or by altering the overall Spike conformation to favor fusion-competent states (Lu et al., 2020). This could result in a favorable intra-host viral replication fitness with enhanced SARS-CoV-2 inter-host transmissibility at a population level. Incidentally, selection of highly pathogenic strains might heighten disease severity and contribute to an increase in the infection fatality rate (see Figure 1 ).
Figure 1.
Potential effects of emerging SARS-CoV-2 Spike variants
The Spike receptor binding domain (RBD) is facing strong selective pressure by neutralizing antibodies, particularly on its receptor binding motif (RBM), resulting in the emergence of Spike variants. Mutations in the RBM could increase Spike affinity for its host receptor or alter its conformational state, facilitating viral entry. Such modifications can affect Spike antigenicity, enabling immune evasion from humoral responses. In turn, this could enhance the viral replication fitness and potentially change viral pathogenesis. At the population level, this might lead to an increase in viral transmission and fatality rate.
Even though all three studies focused on the importance of RBD variants and their role in anti-SARS-CoV-2 neutralizing capacity, RBD is not the only Spike domain targeted by immune responses. With RBD being the main target of neutralizing antibodies, it is judicious to prioritize the surveillance of mutations located in the RBD, especially since some of them were shown to have a direct effect on receptor affinity. However, plasma from convalescent donors also generate escape mutations in the N-terminal domain (NTD), indicative of immune pressure (Weisblum et al., 2020). Accordingly, several neutralizing Abs targeting the NTD were isolated, featuring them as potential alternatives or complementary to RBD-directed Abs (Liu et al., 2020). Moreover, despite being comparatively understudied at the moment, the bulk of the antibody responses in infected patients is dominated by non-neutralizing antibodies directed toward the highly conserved S2 subunit (Shrock et al., 2020). Although current efforts are mostly focused on neutralization, increasing evidence argues for the importance of other antiviral properties of antibodies, including Fc-mediated effector functions, which have been shown to contribute to their protective efficacy against SARS-CoV-2 in animal models (Schäfer et al., 2021). Along with B cell immunity, recent studies showed that the Spike is also the major target for CD4+ and CD8+ T cell immunity (Tarke et al., 2021). The NTD and the S2 fusion peptide region were defined as immunodominant regions able to trigger CD4+ T cell responses, while CD8+ T cell responses were directed against equally distributed epitopes throughout the Spike polyprotein sequence.
The hazard caused by the emergence of single variants could potentially be contained by polyclonal antibody responses elicited by natural infection, vaccination, or using combinations of monoclonal antibodies in therapeutic interventions. However, the main problem resides in the emergence of new SARS-CoV-2 variants presenting an accumulation of mutations in different Spike domains, creating divergent strains able to evade polyclonal responses. This includes the B.1.1.7 lineage (also known as 501Y.V1 or VOC202012/01), which first emerged in the United Kingdom and has now spread worldwide. Other variants of concern include the B.1.351 lineage (501Y.V2) and the P.1 lineage (501Y.V3), which were first identified in South Africa and Brazil, respectively. These variants have cumulated at least nine non-synonymous mutations/deletions throughout the Spike coding region. Selected mutations were found in the RBM (up to three mutations), including the E484K mutation, identified in vitro in the Liu et al. and Greaney et al. studies. In these concerning variants, RBM modifications are often accompanied with numerous substitutions and/or deletions in the NTD region (up to seven), demonstrating a particular in vivo selective pressure on this site. At least one mutation was also found in the S2 subunit for all three new lineages, confirming the major immune pressure under which the Spike protein evolves. Additional variants are currently under high scrutiny because of the presence of key mutations in the RBM, including the 20A.EU2 variant (S477N), the CAL.20C variant (L452R), and the Danish mink cluster 5 (Y453F). The establishment of sequence monitoring initiatives by public health agencies like the coronavirus disease 2019 (COVID-19) Genomics UK Consortium (COG-UK) are critical to contain the rise of these preoccupying variants by informing and working hand in hand with governments, healthcare systems, and biopharmaceutical companies.
Hopes are now turned toward vaccines that are being deployed globally, which, in conjunction with public health measures, could stop the progression of the COVID-19 pandemic. The immune responses generated by mRNA and adenoviral vector-based vaccines are restricted to the Spike glycoprotein. Thus, their efficacy could be influenced by the emergence of new SARS-CoV-2 Spike variants presenting a major antigenic drift. Recent reports highlighted the deleterious effect of RBM mutations on the neutralization activity of vaccine-elicited antibodies (Wang et al., 2021). One advantage conferred by the mRNA platform is its adaptability and flexibility to rapidly generate new versions accounting for emerging variants. These variants could impact the long-term protective immunity that appears to be elicited by natural infection and vaccination. The emergence of new variants with the distinct capacity to evade polyclonal antibody responses could potentially lead to a growing number of reinfections. In this context, development of second-generation neutralizing antibody cocktails targeting more conserved regions in the RBD or the S2 subunit should be considered, although only a handful of these antibodies have been identified to date. Altogether, these studies shed light on the critical importance of monitoring SARS-CoV-2 sequence variation for a rapid identification of new variants that could require adjustments in vaccine strategies and therapeutic interventions.
Acknowledgments
Work in the Finzi lab related to SARS-CoV-2 variants is supported by an Exceptional Fund COVID-19 from the Canada Foundation for Innovation (CFI) (no. 41027), by the Sentinelle COVID Quebec network led by the Laboratoire de Santé Publique du Quebec (LSPQ) in collaboration with Fonds de Recherche du Québec-Santé (FRQS) and Genome Canada – Génome Québec, and by the Ministère de la Santé et des Services Sociaux (MSSS) and the Ministère de l’Économie et Innovation (MEI). A.F. is the recipient of a Canada Research Chair on Retroviral Entry. J.P. is supported by a Canadian Institutes of Health Research (CIHR) doctoral fellowship. The figure was prepared using illustrations from BioRender.com. The authors declare no competing interests.
References
- Greaney A.J., Loes A.N., Crawford K.H.D., Starr T.N., Malone K.D., Chu H.Y., Bloom J.D. Comprehensive mapping of mutations in the SARS-CoV-2 receptor-binding domain that affect recognition by polyclonal human plasma antibodies. Cell Host Microbe. 2021;29 doi: 10.1016/j.chom.2021.02.003. this issue, 463–476.e6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Z., VanBlargan L.A., Bloyet L.-M., Rothlauf P.W., Chen R.E., Stumpf S., Zhao H., Errico J.M., Theel E.S., Liebeskind M.J., et al. Identification of SARS-CoV-2 spike mutations that attenuate monoclonal and serum antibody neutralization. Cell Host Microbe. 2021;29 doi: 10.1016/j.chom.2021.01.014. this issue, 477–488.e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu L., Wang P., Nair M.S., Yu J., Rapp M., Wang Q., Luo Y., Chan J.F., Sahi V., Figueroa A., et al. Potent neutralizing antibodies against multiple epitopes on SARS-CoV-2 spike. Nature. 2020;584:450–456. doi: 10.1038/s41586-020-2571-7. [DOI] [PubMed] [Google Scholar]
- Lu M., Uchil P.D., Li W., Zheng D., Terry D.S., Gorman J., Shi W., Zhang B., Zhou T., Ding S., et al. Real-Time Conformational Dynamics of SARS-CoV-2 Spikes on Virus Particles. Cell Host Microbe. 2020;28:880–891.e8. doi: 10.1016/j.chom.2020.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schäfer A., Muecksch F., Lorenzi J.C.C., Leist S.R., Cipolla M., Bournazos S., Schmidt F., Maison R.M., Gazumyan A., Martinez D.R., et al. Antibody potency, effector function, and combinations in protection and therapy for SARS-CoV-2 infection in vivo. J. Exp. Med. 2021;218:e20201993. doi: 10.1084/jem.20201993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shrock E., Fujimura E., Kula T., Timms R.T., Lee I.H., Leng Y., Robinson M.L., Sie B.M., Li M.Z., Chen Y., et al. MGH COVID-19 Collection & Processing Team Viral epitope profiling of COVID-19 patients reveals cross-reactivity and correlates of severity. Science. 2020;370:eabd4250. doi: 10.1126/science.abd4250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Starr T.N., Greaney A.J., Addetia A., Hannon W.W., Choudhary M.C., Dingens A.S., Li J.Z., Bloom J.D. Prospective mapping of viral mutations that escape antibodies used to treat COVID-19. Science. 2021;371:850–854. doi: 10.1126/science.abf9302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tarke A., Sidney J., Kidd C.K., Dan J.M., Ramirez S.I., Yu E.D., Mateus J., da Silva Antunes R., Moore E., Rubiro P., et al. Comprehensive analysis of T cell immunodominance and immunoprevalence of SARS-CoV-2 epitopes in COVID-19 cases. Cell Rep. Med. 2021;2:100204. doi: 10.1016/j.xcrm.2021.100204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomson E.C., Rosen L.E., Shepherd J.G., Spreafico R., da Silva Filipe A., Wojcechowskyj J.A., Davis C., Piccoli L., Pascall D.J., Dillen J., et al. Circulating SARS-CoV-2 spike N439K variants maintain fitness while evading antibody-mediated immunity. Cell. 2021;184 doi: 10.1016/j.cell.2021.01.037. 1171–1187.e20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Z., Schmidt F., Weisblum Y., Muecksch F., Barnes C.O., Finkin S., Schaefer-Babajew D., Cipolla M., Gaebler C., Lieberman J.A., et al. mRNA vaccine-elicited antibodies to SARS-CoV-2 and circulating variants. Nature. 2021 doi: 10.1038/s41586-021-03324-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weisblum Y., Schmidt F., Zhang F., DaSilva J., Poston D., Lorenzi J.C., Muecksch F., Rutkowska M., Hoffmann H.H., Michailidis E., et al. Escape from neutralizing antibodies by SARS-CoV-2 spike protein variants. eLife. 2020;9:e61312. doi: 10.7554/eLife.61312. [DOI] [PMC free article] [PubMed] [Google Scholar]