Abstract
In December 2019, coronavirus disease 2019 (COVID-19), which is caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), was reported in Wuhan, China. An 82-year-old woman presented to our hospital with high fever (39°C) and chest computed tomography revealed ground-glass opacities in the left lung apex. She was positive for SARS-CoV-2 based on a polymerase chain reaction test, and diagnosed with COVID-19 pneumonia. 6 months after treatment, chest CT showed a large bulla (47 mm × 29 mm) in the left lung apex, although pneumonia had partially resolved. Radiologic follow-up is needed after COVID-19 pneumonia, because patients may develop bullae after treatment.
Keywords: Bulla, COVID-19, Pneumonia, SARS-CoV-2, Coronavirus
Introduction
In December 2019, coronavirus disease 2019 (COVID-19), which is caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), was reported in Wuhan, China. It has spread rapidly all over the world.
Common symptoms include fever, cough, myalgia, fatigue, and olfactory or gustatory dysfunction [1,2]. In severely affected patients, disseminated intravascular coagulation, localized pulmonary thrombotic microangiography, and organ dysfunction can occur [3]. We herein report a case of bulla formation after treatment for COVID-19 pneumonia.
Case report
An 82-year-old woman presented to our hospital with high fever (39°C). Physical examination revealed percutaneous oxygen saturation of 94% while breathing ambient air, respiratory rate of 24 breaths/min, blood pressure of 97/54 mmHg, and pulse of 88 beats/min. She did not have cough or dyspnea. Chest X-ray showed a right pleural effusion, but no pneumonia (Fig. 1). Laboratory testing revealed an elevated level of C-reactive protein (9.23 mg/dL), but a normal white blood cell count (8600/µL) and a normal lactate dehydrogenase level (216U/L). Chest computed tomography (CT) revealed ground-glass opacities in the left lung apex (Fig. 2). Two days later, she was positive for SARS-CoV-2 based on a polymerase chain reaction (PCR) test. She was diagnosed with COVID-19 pneumonia. She was transferred to another hospital to be treated for pneumonia. After treatment, she had two negative PCR tests until being discharged home 18 days after symptom onset. After 6 months, chest CT was performed. Although pneumonia had partially resolved, a large bulla (47 mm × 29 mm) was observed in the left lung apex (Fig. 2). She had a medical history of right breast cancer and gastric cancer treated with endoscopic submucosal dissection. Thirteen years ago, she underwent surgery and adjuvant hormone therapy for pT1N1M0, Stage IIA breast cancer. Two years ago, breast cancer recurred (liver and bone metastasis) and she firstly received chemotherapy. One year ago, she discontinued chemotherapy because of neutropenia. Afterwards, she was administered hormone therapy. Six months ago, she developed a right pleural effusion secondary to breast cancer. She underwent pleurodesis on the right side.
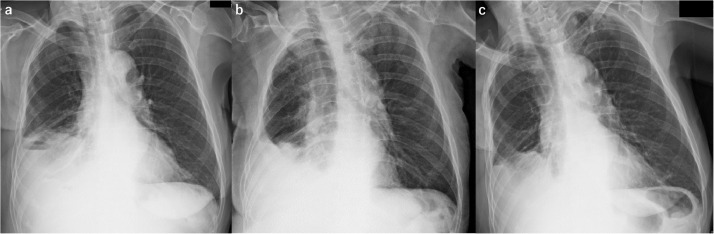
Fig. 1.
Chest X-ray. (A) Posteroanterior view, 1 month before onset. (B) Portable anteroposterior view, in the supine position at onset. (C) Posteroanterior view, 5 months after onset. Each chest X-ray showed right pleural effusion, but no pneumonia.
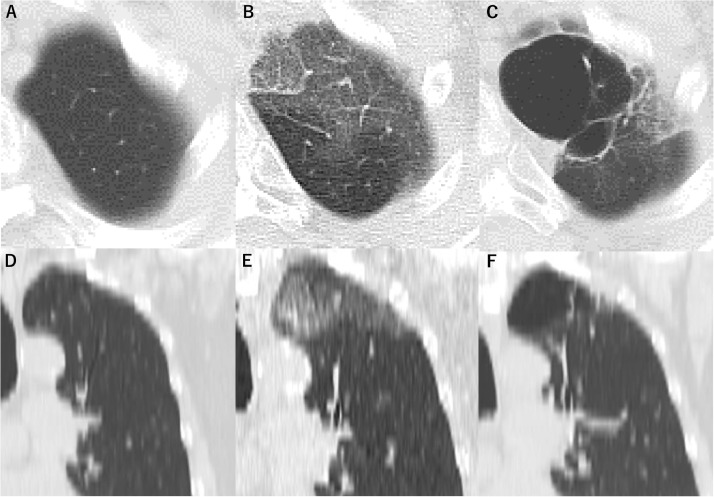
Fig. 2.
Chest computed tomography. (A) and (D) CT at 6 months before onset. (B) and (E) At onset, CT revealed ground-glass opacities in the left lung apex. (C) and (F) At 6 months after onset, although pneumonia had partially resolved, a large bulla (47 × 29 mm) was observed in the left lung apex. (A–C) axial and (D–F) coronal.
Discussion
A bulla is thought to be formed by the destruction of inter-alveolar walls caused by increased intra-alveolar pressure. This can result from a decrease in the size of a bronchiole lumen, but the exact cause is not known [4]. In this case, there was no lung metastasis, although liver and bone metastasis appeared. Because the bulla appeared at the same range of pneumonia (Fig. 2), we speculated that the bulla formation was associated with COVID-19 pneumonia rather than her cancer.
Regarding bulla formation after treatment for COVID-19 pneumonia, Yasukawa et al. reported a case of tension pneumothorax caused by rupture of a giant bulla 14 days after treatment for COVID-19 [5]. Sun et al. reported that follow-up CT revealed a giant bulla, mediastinal emphysema, and pneumothorax on day 15 of treatment for COVID-19 pneumonia [6]. Sato et al. described a patient with a bulla and hemoptysis more than 10 days after onset [7]. Our patient also developed a bulla after treatment for COVID-19 pneumonia. None of these four patients received mechanical ventilation, which rules out mechanical lung injury.
Radiologic studies have shown that patients with COVID-19 pneumonia can develop cystic changes in the lung during the course of SARS-CoV-2 infection [8]. Shi et al. reported that 10% of patients with COVID-19 pneumonia had cystic change in the lung [9], suggesting that cystic change including bullae in the lung may not be unusual.
Liu et al. speculated that ischemic parenchymal damage, lung fibrosis, and low lung compliance may lead to the formation of cysts and the development of pneumothorax [8]. In addition, acute respiratory distress syndrome may result in cyst formation in the lung [10].
Fan et al. reported that a patient with COVID-19 pneumonia developed spontaneous pneumothorax and bullae on day 21 from onset. At the 92-day follow-up, the pneumothorax and bullae had completely resolved. These complications were thought to be self-limiting [11].
Laboratory findings of severe COVID-19 can include increased concentrations of cytokines such as tumor necrosis factor α, interleukin (IL)-1, and IL-6 [1]. Inhibition of IL-6 with tocilizumab or siltuximab may be a novel treatment for the management of COVID-19 pneumonia [12]. In our patient, the inflammatory marker C-reactive protein was increased at 9.23 mg/dL, and IL-6 concentration was not evaluated.
Histological findings of COVID-19 pneumonia include bilateral diffuse alveolar damage with cellular fibromyxoid exudates [13]. More studies are needed to determine whether these findings are associated with cystic changes or bullae formation in the lung. Moreover, COVID-19 may cause a post-infectious inflammatory syndrome similar to Kawasaki disease in adults according to Sokolovsky et al. [14].
In conclusion, radiologic follow-up is needed after COVID-19 pneumonia, because patients may develop bullae and pneumothorax within approximately 1 month. It may be valid to confirm whether bullae have resolved by approximately 3 months after onset. The long-term prognosis of COVID-19 is unclear; we hope that more cases will be accumulated and examined.
Patient consent statement
Written informed consent was obtained from the patient for their anonymized information to be published in this article.
References
- 1.C. Huang, Y. Wang, X. Li, L. Ren, J. Zhao, Y. Hu. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Luers JC, Rokohl AC, Loreck N, Wawer Matos PA, Augustin M, Dewald F. Olfactory and gustatory dysfunction in coronavirus disease 2019 (COVID-19) Clin Infect Dis. 2020;71:2262–2264. doi: 10.1093/cid/ciaa525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Levi M, Thachil J, Iba T, Levy JH. Coagulation abnormalities and thrombosis in patients with COVID-19. Lancet Haematol. 2020;7:e438–e440. doi: 10.1016/S2352-3026(20)30145-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wiese ER. Bulla of the lung. Dis Chest. 1946;12:238–241. doi: 10.1378/chest.12.3.238. [DOI] [PubMed] [Google Scholar]
- 5.Yasukawa K, Vamadevan A, Rollins R. Bulla formation and tension pneumothorax in a patient with COVID-19. Am J Trop Med Hyg. 2020;103:943–944. doi: 10.4269/ajtmh.20-0736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sun R, Liu H, Wang X. Mediastinal emphysema, giant bulla, and pneumothorax developed during the course of COVID-19 pneumonia. Korean J Radiol. 2020;21:541–544. doi: 10.3348/kjr.2020.0180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sato L, Kinoshita N, Nakamoto T, Ohmagari N. Hemoptysis and a newly formed lung bulla in a case of convalescent COVID-19 pneumonia. Intern Med. 2021 doi: 10.2169/internalmedicine.5684-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Liu K, Zeng Y, Xie P, Ye X, Xu G, Liu J. COVID-19 with cystic features on computed tomography: a case report. Medicine (Baltimore) 2020;99:e20175. doi: 10.1097/MD.0000000000020175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shi H, Han X, Jiang N, Cao Y, Alwalid O, Gu J. Radiological findings from 81 patients with COVID-19 pneumonia in Wuhan, China: a descriptive study. Lancet Infect Dis. 2020;20:425–434. doi: 10.1016/S1473-3099(20)30086-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Joynt GM, Antonio GE, Lam P, Wong KT, Li T, Gomersall CD. Late-stage adult respiratory distress syndrome caused by severe acute respiratory syndrome: abnormal findings at thin-section CT. Radiology. 2004;230:339–346. doi: 10.1148/radiol.2303030894. [DOI] [PubMed] [Google Scholar]
- 11.Fan Q, Pan F, Yang L. Spontaneous pneumothorax and subpleural bullae in a patient with COVID-19: a 92-day observation. Eur J Cardiothorac Surg. 2020;58:858–860. doi: 10.1093/ejcts/ezaa305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Coomes EA, Haghbayan H. Interleukin-6 in COVID-19: a systematic review and meta-analysis. Rev Med Virol. 2020;30:1–9. doi: 10.1002/rmv.2141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Xu Z., Shi L., Wang Y., Zhang J., Huang L., Zhang C. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir Med. 2020;8:420–422. doi: 10.1016/S2213-2600(20)30076-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sokolovsky S, Soni P, Hoffman T, Kahn P, Scheers-Masters J. COVID-19 associated Kawasaki-like multisystem inflammatory disease in an adult. Am J Emerg Med. 2021;39:253 e1-e2. doi: 10.1016/j.ajem.2020.06.053. [DOI] [PMC free article] [PubMed] [Google Scholar]