Abstract
Introduction
COVID-19 was declared a pandemic by the World Health Organization on the 11th of March 2020 with the NHS deferring all non-urgent activity from the 15th of April 2020. The aim of our study was to assess the impact of COVID-19 on Trauma and Orthopaedic trainees nationally.
Methods
Trauma and Orthopaedic (T&O) specialty trainees nationally were asked to complete an electronic survey specifically on the impact of COVID-19 on their training. This UK based survey was conducted between May 2020 and July 2020.
Results
A total of 185 out of 975 (19%) T&O specialty trainees completed the survey. Redeployment was experienced by 25% of trainees. 84% of respondents had experienced a fall in total operating numbers in comparison with the same time period in 2019. 89% experienced a fall in elective operating and 63% experienced a fall in trauma operating. The pandemic has also had an effect on the delivery of teaching, with face to face teaching being replaced by webinar-based teaching. 63% of training programmes delivered regular weekly teaching, whilst 19% provided infrequent sessions and 11% provided no teaching.
Conclusion
This study has objectively demonstrated the significant impact of the COVID-19 pandemic on all aspects of T&O training.
Keywords: COVID–19, Coronavirus, Pandemic, Trauma & orthopaedics, Education, Training
Introduction
Since being declared a pandemic on the 11th March 2020, COVID-19 has led to the urgent restructuring of healthcare delivery worldwide with the overall aim being to reduce associated morbidity and mortality.1 In the United Kingdom (UK), this has involved a nationwide response in the National Health Service (NHS) that has included cancellation of large volumes of elective surgery and the redeployment of healthcare professionals to frontline specialities and intensive care.2
The surgical colleges have released dynamic guidance to help the surgical workforce adapt to these rapid and unprecedented times as the impact of COVID-19 was realised. Priorities in order of importance included: maintaining emergency surgery provision; protecting the surgical workforce; fulfilling alternative surgical roles and fulfilling alternative non-surgical roles.3 In Trauma and Orthopaedics (T&O), the British Orthopaedic Association (BOA) have also responded by releasing a key document which has helped shape delivery of care in many departments across the country: “Management of patients with urgent orthopaedic conditions and trauma during the coronavirus pandemic”.4
Throughout the BOA guidelines, inevitable compromises to established patient care are discussed.4 They acknowledge “Surgeons and patients will have difficult choices to make about management options” to reduce demand on services and potential exposure to clinicians and patients. For example, offering hemiarthroplasty rather than total hip replacement, for fractured neck of femur, if suitable surgeons are not available and a focus on conservative treatment of upper limb injuries, with later reconstruction if required.4
In addition to changes to provision of trauma care and cessation of elective surgery, all non-essential face-to-face clinic appointments were cancelled.4 This led to the utilisation of remote consultations, particularly in elective practice. Significant work is required in order to ensure the clinical safety and patient satisfaction of these consultation methods when widening their scope.5 As well as redeployment to other specialties, consultant and junior rotas were redesigned. This included rostering shifts in dedicated minor injuries units or the Emergency Department. Further, a proportion of trainees were often requested to stay at home on ‘ghost rotas’ to ensure resilience with the threat of personnel loss.6
The impact of COVID-19 for all surgical trainees will be felt not only in the UK, but across the globe.7 In the UK, the extent and regional variability of loss of training remains unclear. Furthermore, the number of redeployed to other specialties, such as intensive care and internal medicine, is unknown. The above will have an inevitable impact on trainees ability to fulfill the criteria for the certificate of completion of training (CCT). The aim of this collaborative study was to assess the impact of the COVID-19 pandemic on T&O training nationally using a web-based retrospective survey.
Methods
A web-based survey using Google Forms was sent out to all T&O trainees throughout the UK from 1st May 2020. The link to the survey was sent via email to all orthopaedic Training Programme Directors and Regional Trainee Representatives to facilitate distribution to all trainees in the UK. Further circulation of the web-based survey occurred via social media. The survey consisted of 19 questions and was designed to collect data on different aspects of orthopaedic training during March and April 2020.
The survey contained questions on redeployment of orthopaedic trainees, clinic exposure, operative numbers in both trauma and elective settings during March and April of 2019 and 2020, the impact on fellowship exams, as well as the quality of regional teaching. A further follow up email to all participating trainees at the end of July 2020 enabled the recording of the trainees’ outcomes of their Annual Review of Competence Progression (ARCP) to assess the progression effect of the COVID-19 restructuring.
Statistical analysis was performed using IBM SPSS statistics (Version 26.0, IBM Corp, Armonk, NY, USA). Demographic data were presented descriptively. Categorical variables were described as proportions and continuous variables were presented as medians and interquartile ranges. The statistical relationship between categorical variables was assessed using a chi-squared test. The Shapiro-Wilk test was used to assess for data normality. For continuous data, the Student's t-test was used when the numerical values for the two independent groups were normally distributed, otherwise the Mann-Whitney U test was used when normal distribution was not achieved. Significance was set at a p-value < 0.05.
Results
Demographics
A total of 185 T&O specialty trainee level 1 to 8 (ST1-ST8) trainees from all training regions across the UK completed the online survey (Table 1 ). A freedom of information request in 2019 revealed that there were 975 ST3-ST8 T&O trainees across the UK. This gives a representative sample of approximately 18% when excluding the run-through ST1 and ST2 T&O trainees.
Table 1.
Demographics of respondents.
| Demographics | Number (%) |
|---|---|
| Year of Training | |
| ST1 & ST2 | 7 (3.8) |
| ST3 | 38 (20.5) |
| ST4 | 23 (12.4) |
| ST5 | 42 (22.7) |
| ST6 | 19 (10.3) |
| ST7 | 30 (16.2) |
| ST8 | 26 (14.1) |
| Training Region | |
| East of England | 8 (4.3) |
| East Midland | 10 (5.4) |
| North | 3 |
| South | 7 |
| Kent, Surrey & Sussex (KSS) | 4 (2.2) |
| Kent | 0 |
| Surrey | 3 |
| Sussex | 1 |
| North West | 60 (32.4) |
| Manchester | 20 |
| Mersey | 40 |
| North East | 15 (8.1) |
| London | 22 (11.9) |
| North East | 8 |
| North West | 9 |
| South East | 1 |
| South West | 4 |
| Northern Ireland | 5 (2.7) |
| Oxford | 4 (2.2) |
| Scotland | 5 (2.7) |
| East | 2 |
| North | 1 |
| South East | 1 |
| West | 1 |
| South West | 16 (8.6) |
| Peninsula | 2 |
| Severn | 14 |
| Wales | 4 (2.2) |
| Wessex | 17 (9.2) |
| West Midlands | 14 (7.6) |
| Warwick | 5 |
| Oswestry | 0 |
| Birmingham | 9 |
| Yorkshire & Humber | 1 (0.5) |
Trainee redeployment
During the surveyed period, 46 respondents (25%) experienced redeployment to either Intensive Care, Emergency Medicine or Internal Medicine. From this group, there were a slightly higher number of trainees redeployed to Intensive Care (18 out of 46; 39%) compared to Internal Medicine (14 out of 46; 30.5%) and Emergency Medicine (14 out of 46; 30.5%). However, the average length of redeployment was longest in Internal Medicine (50 days) compared to Emergency Medicine (38 days) and Intensive Care (30 days). The 53 respondents that worked in a major trauma centre were not less likely to be redeployed compared to those working in a district general hospital (X2 = 0.47 (1, N = 185), p = 0.49).
Impact on operative and clinical sessions
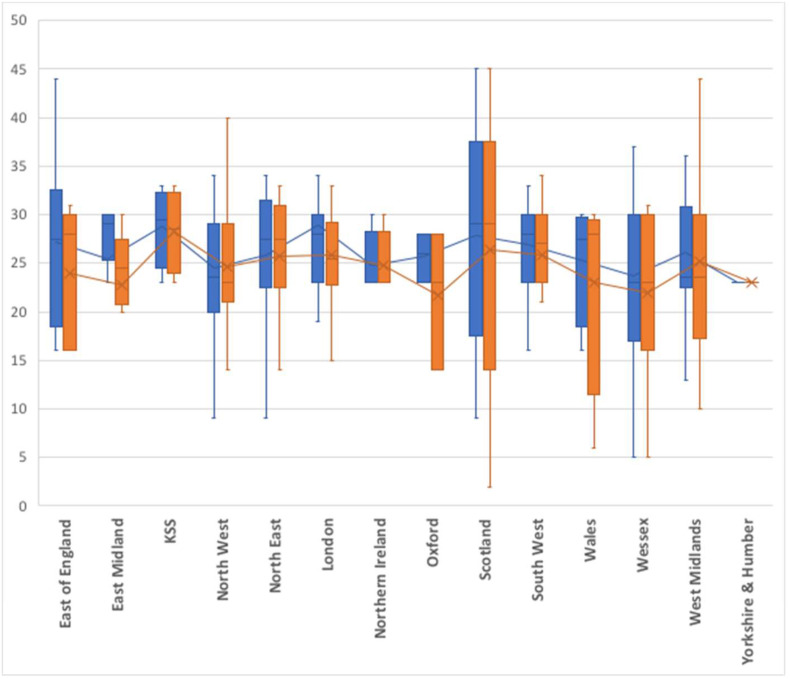
Although the government informed NHS hospitals to suspend all non-urgent elective work from the 15th April 2020,8 it is clear from the respondents that all trusts actually stopped elective activity well in advance of this date (Fig. 1 ). On average, elective operating and face-to-face elective clinics were stopped 26 days and 25 days before the 15th April respectively. There was no significant variation between the different regions. Considering elective activity only tentatively returned in July, trainees lost on average 44 elective theatre sessions and 29 face-to-face elective clinic sessions (up to 30th June).
Fig. 1.
Box and Whisker plot demonstrating the number of days when elective operating (blue) and face-to-face elective clinics (orange) were stopped in relation to the 15th April 2020.
The lack of operating has meant that 84% (146 out of 174) of respondents had a fall in the total number of recorded operative cases when compared to March–April 2019. More specifically, 89% (143 out of 160) and 63% (107 out of 169) of respondents had a fall in the number of recorded elective and trauma operative cases respectively. As shown in Table 2 , there was a 49%, 79% and 25% overall reduction in the median number of total, elective and trauma operative cases respectively compared to March–April 2019.
Table 2.
The impact on recorded operative cases.
| Total Operative Numbers | Elective Operative Numbers | Trauma Operative Numbers | |
|---|---|---|---|
| Number for Analysis | 174 | 160 | 169 |
| March & April 2019 Median (Interquartile range) | 53 (38–69) | 28 (19–40) | 24 (15–33) |
| March & April 2020 Median (Interquartile range) | 27 (14–38) | 6 (2–12) | 18 (9–27) |
| Significance - p value (Mann-Whitney U Test) | <0.001 | <0.001 | <0.001 |
Teaching
As with all other activity, conventional face-to-face teaching stopped in all regions around the time when national lockdown was announced. The majority of training programmes started to utilise webinar-based teaching with 63% (17 out of 27) establishing regular weekly sessions and 19% (5 out of 27) having infrequent sessions. The remaining 11% (3 out of 27) had no teaching provision with no data for 2 of the training programmes. This new teaching set-up was rated as very good or good by 76% (141 out of 185) of trainees, fair by 17% (31 out of 185), poor by 5% (10 out of 185) and very poor by 2% (3 out of 185).
Fellowship exams
The cancellation of fellowship exams directly impacted on surveyed ST7 and ST8 trainees. The cancelled part 1 exam in June affected 20% (11 out of 56) of the respondents, whilst the cancelled part 2 exam in May affected 16% (9 out of 56) of the respondents.
Annual Review of Competency Progression (ARCP) outcomes
Follow up questions enquiring about ARCP outcomes, were answered by 63% (117 out of 185) of the initial list of respondents. However, 31% (36 out of 117) of these respondents had not had their end of year ARCP. Regarding the ST8 trainee group, 72% (13 out of 18) of the respondents received their outcome 6 (Table 3 ) for successful completion of training and 6% (1 out of 18) getting an outcome 10.2 with a 6-month training extension. Overall, 32% (37 out of 117) of the remaining respondents received an outcome 1, whilst 22% (26 out of 117) and 3% (4 out of 117) received an outcome 10.1 and 10.2 respectively. In addition to the 6% of respondents that received an extension to their training, 17% (6 out of 36) of those yet to have their end of year ARCP are expecting to get a 6-month training extension.
Table 3.
ARCP outcomes.
| Outcome 1 | Satisfactory Progress - achieving progress and the development of competences at the expected rate. This is subject to successful completion of the training period. |
| Outcome 2 | Development of specific competences required - additional training time not required. |
| Outcome 3 | Inadequate progress - additional training time required. |
| Outcome 4 | Released from training programme - with or without specified competences. |
| Outcome 5 | Incomplete evidence presented - additional training time may be required. |
| Outcome 6 | Gained all required competences - will be recommended as having completed the training programme and for award of a CCT or CESR/CEGPR. |
| Outcome 7.1 | Satisfactory progress in or completion of LAT placement. |
| Outcome 7.2 | Development of specific competences required - additional training time not required. |
| Outcome 7.3 | Inadequate progress by the trainee. |
| Outcome 7.4 | Incomplete evidence presented. |
| Outcome 8 | Out of programme for research, approved clinical training or a career break (OOPR/OOPT/OOPC). |
| Outcome 9 | Doctors undertaking top up training in a training post. |
| Outcome 10.1 | Progress is satisfactory but the acquisition of competences/capabilities by the trainee has been delayed by COVID-19 disruption. The trainee is not at a critical progression point in their programme and can progress to the next stage of their training. Any additional training time will be reviewed at the next ARCP. |
| Outcome 10.2 | Progress is satisfactory but the acquisition of competences/capabilities by the trainee has been delayed by COVID-19 disruption. The trainee is at a critical progression point in their programme and additional training time is required. |
Discussion
This study demonstrates objectively that there has been a significant impact on the training of T&O trainees across the country. Redeployment affected approximately a quarter of trainees across the country, however the loss of surgical training as compared to those not redeployed was mitigated by the significant fall in both elective and trauma operating. The effect of COVID-19 has also been acknowledged nationally across all specialities.9 The response from the training bodies has been to create a new outcome within the ARCP process (outcome 10). In the ARCP in July, trainees could now be given one of the new outcomes (either a 10.1 or 10.2).10 If a T&O trainee received an outcome 10.1, they are given the option of an extra 6 months of training, should they feel it to be necessary. This can be taken at any point during their training. If the trainee was awarded an outcome 10.2 this would mean that a 6-month extension would automatically be enforced by the ARCP panel. Studies in both the UK and in Europe have found similar reduction in case load and resources to our findings, highlighting similar changes to training may be required outside of the UK.11 , 12
There has been a smaller reduction observed in the number of trauma surgeries as many procedures have a worse outcome when treated conservatively. This is even in the presence of COVID 19, as published by Morelli et al. who found a mortality rate of 67% with conservative hip fracture management compared with 4% with operative management in COVID 19 positive patients.13
Elective orthopaedics has been planned to resume in a 3-phased manner, as recommended by the BOA.14 This will also have significant impact on T&O trainees, who are assessed annually based on the number of procedures they perform. It is impossible to predict when elective orthopaedics will return to the pre-COVID levels of activity, so this effect may carry on for a significant period. In May 2020, 84% of our respondents experienced a fall in operating numbers during the preceding 2 months when comparing total operative numbers during the same 2-month period in 2019. Further uncertainty will arise with local lockdowns in future waves of COVID-19 and the unequal effect this will have on trainees across the UK.
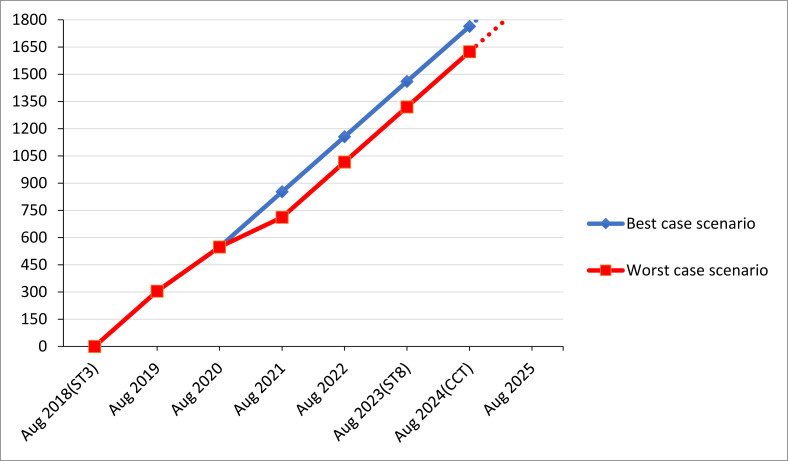
All orthopaedic trainees in the UK are required to achieve certain set targets in order to be awarded the Certificate of Completion of Training (CCT). This includes performing or taking part in a total of 1800 surgical cases over the six year period of higher surgical training.15 The significant drop in recorded operative numbers for trainees, as demonstrated in our study, is a great cause for concern. The uncertainty around the variable pace of re-establishment of elective activity across different NHS trusts, makes it difficult to predict whether trainees will be able to achieve this total number during their orthopaedic training. We used the results from this study to build a predictive model to determine whether trainees would be able to achieve this target within their expected CCT date. We considered resuming full elective activities in August 2020 as the best-case scenario, while the worst-case scenario was resuming full elective activities in August 2021. Based on this model, it is anticipated that trainees will not be able to achieve the 1800 operative cases in their 6 years of training. Moreover, they are likely to be short of 150 cases if full elective activity were only resumed in August 2021 (Fig. 2 ). This worst-case scenario indicates that trainees are likely to require an extra 6 month of training to achieve their target of 1800 surgical cases. Therefore, the new ARCP outcomes created by the UK training committees appear to be correct at this time.
Fig. 2.
Prediction of the effect of COVID-19 on surgical operative numbers for a trainee starting in August 2018. Prediction was based on full surgical activities resuming in August 2020 (best case scenario) and August 2021 (worst case scenario).
Teaching is an important and essential part of T&O training with training programmes across the country delivering weekly teaching. In order to reduce face to face interactions and adhere to social distancing regulations, training programmes nationally have tried to continue teaching with 63% of them delivering regular weekly webinar-based sessions. The quality of this teaching was rated as very good and good by 76% of the respondents. A number of authors have suggested that remote learning is likely to remain in the post-COVID era, due to benefits such as reduced cost, reduced need for travel (as trainees are spread over a wide area) and the opportunity to record lectures.16 , 17 This effect been seen Worldwide where it has created new opportunities for learning delivery and professional growth and demonstrates how quickly the Orthopaedic community adapted to these rapid unprecedented changes caused by the pandemic18
The Fellowship of the Royal College of Surgeons in Trauma and Orthopaedics is normally taken during the penultimate years of training and comprises of a written paper and a clinical/viva section. A policy issued by the Presidents of the four surgical Royal Colleges of Great Britain and Ireland in response to the COVID–19 pandemic, postponed all examinations from the 16th March 2020.19 The consequence of this is the creation of a bottleneck of trainees, which in turn may create problems with work force planning. Larger number of trainees than usual may emerge onto the Consultant job market as a single cohort. With trainees also spending a longer time within the training programme, there could be difficulties for training programme directors to accommodate new trainees joining at the ST3 level.
The study does have limitations. Whilst 19% is one of the largest representations of T&O training in a UK based study, data collection was done in March and April 2020, which was only a snapshot view of the impact of the COVID-19 pandemic during the first peak. As the situation with clinical services continues to evolve, the exact long-term impact on training will be difficult to predict.
Conclusions
This trainee led collaborative project has shown that the COVID-19 pandemic has had a significant effect on T&O training in the UK. With the second wave upon us and winter pressures around the corner it remains to be seen what further impact there will be on the NHS as a whole and T&O specifically.
The ever-changing dynamic nature of this virus has meant as a service we have had to adapt. As a specialty we will also have to adapt to the new training needs of the future T&O surgical workforce. While the COVID-19 10.1 and 10.2 ARCP outcomes have been a good temporary solution to the problem, further remedial measures will be required should the impact on training continue into 2021. The long term effects remains to be seen on these trainees consultants careers and there are a lot of unanswered questions related to the effect of this disruption as there is no historic president with which to model it on.
Acknowledgments
The authors would like to thank Fayez Almari, William Aspinall, Ruaraidh Collins, Andrew Crone, Tom Fleming, Abdullah Gabr, Rachael Grupping, Borna Guevel, Ryan P C Higgin, Ibrahim Ahmed Khalil Ibrahim, Efstathios Kostopoulos, Christopher Manning, Mark McMullan, Lorraine Murphy, Mohamed Altayeb Mussa, Richard W Myatt, Ciaran Nolan, Hammad Parwaiz, Pail Rai, Parisah Seyed-Safi, Manpreet Singh Sidhu, Mazen Soufi and Howard C Tribe for providing data for the study by completing the electronic survey.
Contributor Information
COVI-ORTH UK:
Samir Abdalla, Jamie A'Court, Jack Allport, Stefanie Andrew, Thomas Ankers, James E. Archer, Rebecka AM. Asp, Lambros Athanatos, Morgan Bailey, Joe JT. Barrett-Lee, Ian Baxter, Oliver Beaumont, Harry Benjamin-Laing, Usman N. Bhatty, Sabri Bleibleh, Jessica Blong, Basil Budair, Joseph Carter, Thomas Cash, Govind S. Chauhan, Nameer Choudhry, Rachael Clegg, Thomas Collins, Georgina Crate, George WV. Cross, Sebastien CR. Crosswell, Ian Crowther, Rory Cuthbert, Mark A. Dahill, Rishi Das, Peter Samuel Edward Davies, Daniel Dawson, Anil Dhadwal, Edward Dickenson, Richard AC. Dimock, Huan Dong, Thomas Donnelly, Sara Dorman, Cameron Dott, Prashanth D'sa, Leanne Dupley, Alexander Durst, Nicholas Eastley, Darren Ebreo, Anthony Egglestone, Douglas Evans, Mohamed Fagir, Christopher Fenner, David Ferguson, Oliver Flannery, Hossam Fraig, Surya Gandham, Catherine Gibson, Matthew Gillespie, Robin Gordon, Selina Graham, Michael J. Grant, Rhodri Gwyn, Alexandra Haddon, Zaid Hamoodi, Luke Harris, William D. Harrison, David H. Hawkes, David Hillier, Ryan Hillier-Smith, John Timothy Hirst, Ghazal Hodhody, David Holmes, James Houston, Michael Hughes, Helen Ingoe, Mark D. Jones, Stevan Jordan, Hean Wu Kang, Luliana Kanya, Benjamin Kapur, Edward Karam, Angus Kaye, James Kennedy, Mohsin Khan, Shoaib Khan, Anthony Kinnair, Thomas D. Knapper, Alastair Konarski, Karadi Hari Sunil Kumar, Langhit Kurar, Tariq Kwaees, Hannah Lennox-Warburton, Frank Liaw, Ignatius Liew, Richard Limb, Zoe Lin, Thomas Lloyd, Joann Lum, Weisang Luo, John M. Lynch, John T. Machin, Tim Maheswaran, Fahd Mahmood, Ihsan Mahmood, Samer SS. Mahmoud, Rebecca Martin, Gulraj S. Matharu, George Matheron, Raymond McKenna, Kathryn McLoughlin, Nisarg Mehta, James Miller, Mohamed Mohamed, Mathias Nagy, Devaraj M. Navaratnam, Michael Newman, Ashley Newton, Jimmy Ng, Albert Wee Tun Ngu, Tobenna Oputa, Neal Ormsby, Piers RJ. Page, Andreas C. Panagiotopoulos, Chang Park, Rebekah J. Parkes, Jack Pearce, Jared Quarcoopome, Ashok Ramasamy, Fatima Rashid, Damir Rasidovic, Parag Raval, Pradyumna Raval, Gautam Reddy, Mohammed abbas Remtulla, Luke Render, Charlotte Richardson, Peter Riddlestone, James Riley, Sophie Rogers, Lebur Rohman, Neil Segaren, Abhinav Singh, Rohit Singhal, Adam Smith, Gregory FW. Stamp, Michael Thomas Stoddart, Adam CS. Stoneham, Rebecca Stoner, Kasia Studnicka, Muaaz Tahir, Gajendiran Thiruchandran, Xenia Tonge, Richard Mark Unsworth, Karen A. Vejsbjerg, Abdus Samee Wasim, Robert DJ. Whitham, William Wynell-Mayow, Jonathan Yates, Nasri Zreik, and Matthew Chan
References
- 1.Massey P.A., McClary K., Zhang A.S., Savoie F.H., Barton R.S. Orthopaedic surgical selection and inpatient paradigms during the coronavirus (COVID-19) pandemic. J Am Acad Orthop Surg. 2020;28(11):436–450. doi: 10.5435/JAAOS-D-20-00360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Haddad F.S. COVID-19 and orthopaedic and trauma surgery. Bone Jt J. 2020;B102(5):545–546. doi: 10.1302/0301-620X.102B5.BJJ-2020-0552. [DOI] [PubMed] [Google Scholar]
- 3.Royal College of Surgeons . 2020 March. Guidance for surgeons working during the COVID-19 pandemic from the surgical royal colleges of the United Kingdom and Ireland; pp. 3–4. [Google Scholar]
- 4.British Orthopaedic Association . 2020 March. Emergency BOAST: management of patients with urgent orthopaedic conditions and trauma during the coronavirus pandemic; pp. 1–6.https://www.boa.ac.uk/resources/covid-19-boasts-combined.html Available from: [Google Scholar]
- 5.Richards, T (Cardiff and Vale Orthopaedic Centre University Hospital Llandough, Cardiff) Mohanty, K (Cardiff and Vale Orthopaedic Centre, University Hospital Llandough C. Virtual follow-up for first appointment after hip and knee arthroplasty surgery is acceptable during the COVID-19 pandemic but not for routine practice. Trans J. 2020 https://www.boa.ac.uk/resources/knowledge-hub/virtual-follow-up-for-first-appointment-after-hip-and-knee-arthroplasty-surgery-is-acceptable-during-the-covid-19-pandemic-but-not-for.html [Internet] Available from: [Google Scholar]
- 6.Pearce O., Yeomans D., Kelly M. The impact of a global pandemic on orthopaedic services: the collaborative approach in a UK major trauma centre. Trans J. 2020 https://www.boa.ac.uk/resources/knowledge-hub/the-impact-of-a-global-pandemic-on-orthopaedic-services-the-collaborative-approach-in-a-uk-major-trauma-centre.html [Internet] Available from: [Google Scholar]
- 7.Kogan M., Klein S.E., Hannon C.P., Nolte M.T. Orthopaedic education during the COVID-19 pandemic. J Am Acad Orthop Surg. 2020;28(11):e456–e464. doi: 10.5435/JAAOS-D-20-00292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Iacobucci G. Covid-19: all non-urgent elective surgery is suspended for at least three months in England. BMJ. 2020;368:m1106. doi: 10.1136/bmj.m1106. [Internet] Available from: [DOI] [PubMed] [Google Scholar]
- 9.British Medical Association . 2020. The hidden impact of COVID-19 on patient care in the NHS in England.https://www.bma.org.uk/media/2840/the-hidden-impact-of-covid_web-pdf.pdf [Internet] Available from: [Google Scholar]
- 10.Statutory T., Bodies E., Sebs T., Colleges M.R., Arcps P., Outcomes A. 2020. Supporting the COVID-19 Response : enabling progression at ARCP introduction changes to ARCPs in 2020.https://www.hee.nhs.uk/sites/default/files/documents/Enabling Progression at ARCP - 20-04-20.pdf [Internet] Available from: [Google Scholar]
- 11.Megaloikonomos P.D., Thaler M., Igoumenou V.G., Bonanzinga T., Ostojic M., Couto A.F., et al. Impact of the COVID-19 pandemic on orthopaedic and trauma surgery training in Europe. Int Orthop. 2020;44(9):1611–1619. doi: 10.1007/s00264-020-04742-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Khan H., Williamson M., Trompeter A. The impact of the COVID-19 pandemic on orthopaedic services and training in the UK. Eur J Orthop Surg Traumatol. 2020 doi: 10.1007/s00590-020-02748-6. [Internet] Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Morelli I., Luceri F., Giorgino R., Accetta R., Perazzo P., Mangiavini L., et al. COVID-19: not a contraindication for surgery in patients with proximal femur fragility fractures. J Orthop Surg Res BioMed Centr. 2020;15 doi: 10.1186/s13018-020-01800-9. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7385330/ [Internet] [cited 2021 Jan 13]. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Radha S., Afzal I. Evidence based suggestions for the return to elective orthopaedic surgery following the COVID-19 pandemic. Trans J. 2020 https://www.boa.ac.uk/resources/knowledge-hub/evidence-based-suggestions-for-the-return-to-elective-orthopaedic-surgery-following-the-covid-19-pandemic.html [Google Scholar]
- 15.JCST . 2020. Updated guidance to the certification guidelines for trauma & orthopaedic surgery for trainees with a certification date of 5 August 2020 or later.https://www.jcst.org/quality-assurance/certification-guidelines-and-checklists/ [Internet] Available from: [Google Scholar]
- 16.Scarlat M.M., Sun J., Fucs P.M.B., Giannoudis P., Mavrogenis A.F., Benzakour T., et al. Maintaining education, research and innovation in orthopaedic surgery during the COVID-19 pandemic. The role of virtual platforms. From presential to virtual, front and side effects of the pandemic. Int Orthop Springer Sci Busin Media Deutschland GmbH. 2020;44 doi: 10.1007/s00264-020-04848-8. [Internet] [cited 2020 Nov 4]. p. 2197–202. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Afshan G., Ahmed A. Distance learning is here to stay: shall we reorganize ourselves for the post-covid-19 world? Anaesthesia. Pain Intens Care. 2020 Oct 6;24(5):487–489. http://apicareonline.com/index.php/APIC/article/view/1353 [Internet] Available from: [Google Scholar]
- 18.Giordano L., Cipollaro L., Migliorini F., Maffulli N. Impact of Covid-19 on undergraduate and residency training. Surgeon. 2020 Nov 12 doi: 10.1016/j.surge.2020.09.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Alderson D., Taylor J., Griffin M.,S., Mealy K. 2020. Joint policy statement on COVID-19 from the royal surgical colleges.https://www.rcsed.ac.uk/news-public-affairs/news/2020/march/joint-policy-statement-on-covid-19-from-the-royal-surgical-colleges [Internet] Available from: [Google Scholar]