Abstract
Background:
Although intensive blood pressure reduction has cardiovascular benefits, the absolute benefit is greater in those at higher cardiovascular disease (CVD) risk.
Objective:
We examined whether NT-proBNP helps identify individuals at higher risk for CVD events across systolic blood pressure (SBP), diastolic blood pressure (DBP) or pulse pressure (PP) categories.
Methods:
Participants from ARIC study visit 4 (1996–98) were grouped according to SBP, DBP or PP categories and further stratified by NT-proBNP categories. Cox regression models were used to estimate hazard ratios for incident CVD (CHD, ischemic stroke or HF hospitalization) and mortality across combined NT-proBNP/BP categories adjusting for CVD risk factors.
Results:
There were 9,309 participants (mean age 62.6 [SD 5.6] years, 58.3 % females) with 2,416 CVD events over a median follow-up of 16.7 years. Within each SBP, DBP or PP category, higher category of NT-proBNP (100-<300 or 3300, compared to NT-proBNP <100 pg/mL) was associated with graded increased risk for CVD events and mortality. Participants with SBP 130–139 mmHg but NT-proBNP ≥300 pg/mL had hazards ratio of 3.4 for CVD (95% CI 2.44–4.77) compared to NT-proBNP <100 pg/mL but SBP 140–149 mmHg.
Conclusion:
Elevated NT-proBNP is independently associated with CVD and mortality across SBP, DBP and PP categories and helps identify individuals at the highest risk. Individuals with “stage 1” hypertension but elevated NT-proBNP had greater cardiovascular risk compared to those with “stage 2” SBP but lower NT-proBNP. Future studies are needed to evaluate use of biomarkers-based strategies for CVD risk assessment to assist with initiation or intensification of BP treatment.
Keywords: NT-proBNP, blood pressure, cardiovascular risk assessment, cardiac biomarkers, cardiovascular disease
Condensed abstract:
Current hypertension guidelines recommend aggressive blood pressure (BP) targets for patients with higher baseline cardiovascular risk. Participants from visit 4 of ARIC study (n=9309) were grouped by systolic BP, diastolic BP and pulse pressure categories and further stratified by NT-proBNP. Compared to NT-proBNP <100 pg/mL, participants in higher category of NT-proBNP showed increased risk for CVD events, across all three BP variables. Participants with “stage 1” hypertension but elevated NT-proBNP had greater CVD risk compared to those with “stage 2” SBP but lower NT-proBNP. Future studies are needed to evaluate use of biomarkers for cardiovascular risk assessment for initiation or intensification of BP treatment.
Introduction
Large observational studies have shown a strong association between blood pressure (BP) and incident coronary heart disease (CHD), stroke, heart failure (HF) and overall cardiovascular (CV) mortality(1). The Systolic Blood Pressure Intervention Trial (SPRINT) demonstrated that intensive BP lowering to a target <120 mm Hg in high risk adults without diabetes significantly reduced the composite endpoint of incident CHD, stroke, HF and CV mortality. However, a higher risk of side-effects such as, hypotension, electrolyte abnormalities and hospitalizations for acute kidney injury were also seen in the intensively treated arm(2). Moreover, other clinical trials evaluating intensive BP control have failed to achieve similar reductions in cardiovascular outcomes in patients with diabetes(3), stroke(4) or intermediate risk adults (5).
The current American College of Cardiology/American Heart Association (ACC/AHA) guidelines recommend BP targets be individualized based on underlying cardiovascular risk rather than absolute BP values alone, with intensive BP control recommended for those at highest cardiovascular disease (CVD) risk (i.e. diabetes, chronic kidney disease, atherosclerotic CVD [ASCVD] or calculated 10-year ASCVD risk ≥10%)(6). However, given the higher incidence of side effects with intensive treatment, additional risk stratification to identify the highest risk groups could prove to be clinically valuable.
The potential value of troponin T [measured with a higher sensitivity assay (hs-cTnT)] as a marker to identify higher risk hypertensive individuals was described in the Atherosclerosis Risk In Communities (ARIC) study where increasing hs-cTnT levels were associated with increased hazards of incident CV events, HF and death across categories of systolic blood pressure (SBP)(7) and diastolic blood pressure (DBP)(8). In fact, individuals with SBP levels that were not well controlled (example 150–159 mmHg) but had undetectable hs-cTnT had lesser event rates than those with SBP which was relatively controlled but with detectable/elevated hs-cTnT(8).
Similar to hs-cTnT, NT-proB-type Natriuretic Peptide (NT-proBNP) is another well-established marker of elevated CV risk, especially HF(9). In a recent pooled analysis, which included data from the ARIC, Dallas Heart and Multi-Ethnic Study of Atherosclerosis studies, elevation of NT-proBNP or hs-cTnT levels identified individuals with higher CVD risk, among those individuals not on anti-hypertensive therapy(10). However, this study did not fully evaluate the value of NT-proBNP as it was evaluated only in combination with hs-cTnT, a single cut-point of NT-proBNP (i.e. >100 pg/ml) was used and only individuals not on anti-hypertensive therapy were included. Furthermore, the value of NT-proBNP with respect to diastolic blood pressure (DBP) and pulse pressure (PP) was not evaluated. Compared to high sensitivity troponins assays, NT-proBNP is more widely available and therefore has greater potential of clinical implementation.
The objective of our study was therefore to extend prior observations and comprehensively examine the association of NT-proBNP with incident CVD events (CHD, ischemic stroke and HF hospitalizations), CV and all-cause mortality across categories of SBP, DBP and PP in the ARIC Study.
Methods
Detailed methods are in the Supplemental Material.
Study Population
The ARIC Study is a prospective population-based study of CVD incidence that recruited 15,792 middle-aged men and women, ages 45 to 64 years from 4 US communities between 1987–1989. A detailed description of the design and objectives of the ARIC study has been published (11). The study protocol was approved by each field center’s institutional review board, and all participants provided written informed consent. Of 11,656 participants who attended ARIC visit 4 (1996–1998) we included 9,309 participants without CVD (Supplemental Figure 1).
Blood pressure measurement:
BP measurements were performed by certified technicians using a random-zero sphygmomanometer. An average of two BP readings measured in the sitting position after 5 minutes of rest was used. PP was calculated as the difference between SBP and DBP.
We used the following pre-specified categories of SBP: <120, 120–129, 130–139, 140–149, ≥150 mmHg and DBP: <60, 60–69, 70–79, 80–89, and ≥90 mmHg based on previous analyses from the ARIC study(7,8) while PP was categorized into <40, 40–49, 50–59, 60–69, and ≥70mmHg. For analyses involving numbers needed to treat (NNT) and stratification by use of hypertension therapy or ASCVD risk, SBP was categorized into only three groups (120–139, 140–159 and ≥160mmHg) consistent with groups identified in the 2017 ACC/AHA BP guidelines(6).
NT-proBNP quantification
NT-proBNP levels were measured with a high-sensitivity assay on a Cobas e411 analyzer using the Elecys proBNP II immunoassay (Roche Diagnostics, Indianapolis). The lower limit of detection for this assay is 5 pg/ml and the coefficient of variation is 3.5–4.7%(12). Based on prior analyses, NT-proBNP was categorized into prespecified levels of <100, 100-< 300, and ≥300 pg/ml(13).
Outcome measures
The primary outcomes included incident CHD, ischemic stroke, HF hospitalization, CVD (a composite of incident CHD, ischemic stroke, HF hospitalization), CV and all-cause mortality. Follow-up time ended when the participant had an outcome, was lost to follow-up, or survived from visit 4 until December 31st, 2014. Criteria for adjudicating CHD, ischemic stroke, HF events, CV and all-cause mortality in ARIC have been previously described(14–16); adjudication of HF hospitalization was done after 2005.
Statistical Analysis
Baseline characteristics are presented across 3 categories of NT-proBNP (<100, 100 to <300, ≥300 pg/mL). Using Cox proportional hazards models and after stratification into subgroups of 1) SBP, 2) DBP, or 3) PP categories we estimated the hazards ratio (HR) and 95% confidence intervals (CI) for the associations of NT-proBNP (modeled as a categorical or continuous variable) with cardiovascular outcomes. Models were adjusted for age, sex, race and pertinent clinical variables including use of antihypertensive drug, use of lipid lowering medication, estimated glomerular filtration rate (eGFR), diabetes mellitus, glucose, total cholesterol/high density lipoprotein cholesterol (HDL-C) ratio, body mass index (BMI) and smoking status. The p-value-for-interactions between categories of NT-proBNP and SBP, DBP or PP for association of cardiovascular outcomes were estimated using Wald chi-square test.
For SBP analysis two reference groups were used: (1) NT-proBNP <100 pg/ml and SBP <120 mmHg and (2) NT-proBNP <100 pg/ml and SBP 140–149 mmHg. The second reference group was created to evaluate how (with respect to clinical outcomes) individuals with higher levels of SBP (i.e. stage 2) but lower levels of biomarker (NT-proBNP) did when compared to those with elevated BP or stage 1 hypertension (SBP 120–139 mmHg) but higher levels of NT-proBNP. The reference group used for DBP was NT-proBNP <100 pg/ml and DBP 70–79 mmHg and for PP was NT-proBNP <100 pg/ml and PP <40 mmHg.
Analyses stratified by BMI category (<30kg/m2, ≥30 kg/m2), given that BMI has been shown to affect NT-proBNP levels (17), pooled cohort equation (PCE) risk (<10 or ≥ 10%) and baseline use of anti-hypertensive therapy were also performed.
Finally, we calculated a 10-year number needed to treat (NNT10) to prevent one CVD event for each combined SBP (120–139, 140–159 or ≥160 pg/mL) and NT-proBNP category, sub-stratified by PCE risk (low risk <10% or high risk ≥10%), assuming 25%, 22%, 41% and 24% relative risk reduction in CVD, CHD, ischemic stroke, and HF hospitalization, respectively, based on the treatment effect of intensive BP lowering to target SBP <120 mmHg shown in a meta-analysis (for CHD, stroke and HF)(18) or directly from SPRINT (for CVD)(2). For all presented tests were 2 tailed, and a P-value <0.05 was considered statistically significant.
Results
Baseline characteristics
The mean age of the study population was 62.6 years (SD 5.6), 41.7% were male and 21.5% were black. Subjects with higher baseline NT-proBNP were more likely to be older, females, white, smokers; have diabetes or hypertension, use antihypertensive medications, have higher HDL-C, high sensitivity c-reactive protein, hs-cTnT, galectin and left ventricular hypertrophy and lower BMI, total cholesterol, eGFR (Table 1).
Table 1.
Baseline Characteristics Across NT-proBNP Categories, ARIC Study (1996–1998, Visit 4)
| Risk factors | Overall | NT-proBNP (pg/mL) | P trend | ||
|---|---|---|---|---|---|
| <100 | 100-<300 | ≥300 | |||
| N (%) | 9309 | 6361 | 2470 | 478 | |
| Age | 62.6±5.6 | 61.7±5.4 | 64.0±5.7 | 66.0±5.4 | <0.001 |
| Male (%) | 41.7 | 47.7 | 27.8 | 33.7 | <0.001 |
| Black (%) | 21.5 | 24.8 | 14.3 | 15.3 | <0.001 |
| Hypertension (%) | 44.0 | 39.5 | 50.8 | 68.6 | <0.001 |
| Diabetes (%) | 14.7 | 15.9 | 11.5 | 16.1 | 0.001 |
| Current smoking (%) | 14.6 | 13.8 | 15.8 | 19.3 | <0.001 |
| Use of BP lowering meds (%) | 37.8 | 34.3 | 41.7 | 65.1 | <0.001 |
| Use of lipid-lowering meds (%) | 11.1 | 11.0 | 10.9 | 15.1 | 0.08 |
| Use of statins (%) | 8.5 | 8.5 | 7.8 | 12.4 | 0.22 |
| SBP (mmHg) | 127.0±18.8 | 124.8±17.2 | 130.4±20.1 | 138.2±24.6 | <0.001 |
| DBP (mmHg) | 71.1±10.1 | 71.3±9.7 | 70.4±10.7 | 71.5±12.4 | 0.004 |
| Pulse pressure (mmHg) | 55.9±15.7 | 53.5±14.2 | 60.0±16.4 | 66.7±20.6 | <0.001 |
| BMI (kg/m2) | 28.6±5.5 | 29.0±5.4 | 27.9±5.7 | 28.1±5.6 | <0.001 |
| Total cholesterol (mmol/L) | 5.2±0.94 | 5.2±1.0 | 5.2±0.9 | 5.06±0.94 | <0.001 |
| Triglycerides (mmol/L) | 1.4 (1.0, 1.9) | 1.4 (1.0, 2.0) | 1.3 (1.0, 1.9) | 1.4 (1.0, 1.9) | 0.03 |
| LDL-C (mmol/L) | 3.2±0.9 | 3.2±0.9 | 3.1±0.9 | 3.0±0.9 | <0.001 |
| HDL-C (mmol/L) | 1.3±0.43 | 1.3±0.4 | 1.4±0.5 | 1.4±0.5 | <0.001 |
| Cholesterol/HDL ratio | 4.3±1.5 | 4.5±1.5 | 4.1±1.4 | 4.1±1.5 | <0.001 |
| Fasting glucose (mmol/L) | 6.07 ± 2.019 | 6.20±2.172 | 5.75±1.572 | 5.93±1.764 | <0.001 |
| eGFR (mL/min/1.73m2) | 86.8±15.5 | 88.4±14.7 | 84.8±15.2 | 75.8±20.6 | <0.001 |
| LVH (%) | 3.0 | 1.9 | 4.2 | 11.5 | <0.001 |
| hs-TnT (ng/L) | 4 (1.5, 7) | 4 (1.5, 7) | 5 (1.5, 8) | 8 (4, 14) | <0.001 |
| Galactin-3 (ng/mL) | 14.1 (11.9, 16.7) | 13.8 (11.7, 16.2) | 14.5 (12.3, 17.4) | 16.0 (13.3, 19.2) | <0.001 |
| hs-cTnI (ng/L) | 2.1 (1.5, 3.3) | 2.0 (1.4, 3.0) | 2.3 (1.6, 3.6) | 4.1 (2.3, 8.3) | <0.001 |
| hs-CRP (mg/L) | 2.32 (1.05, 5.23) | 2.19 (1.02, 4.91) | 2.67 (1.13, 5.86) | 3.26 (1.16, 7.50) | <0.001 |
Data presented as mean±SD, median [25th, 75th percentiles], or percentage. P-values for linear trend were calculated by using trend test across ordered groups. p trend was calculated by non-parametric sum of rank test across ordered NT-proBNP groups. Abbreviations: DBP: diastolic blood pressure, eGFR: estimated glomerular filtration rate; HDL-C: high-density lipoprotein-cholesterol; hs-CRP: high sensitivity C-reactive protein; hs-cTnI: high sensitivity cardiac troponin I; hs-TnT: high sensitivity cardiac troponin T; LDL-C: low-density lipoprotein-cholesterol; SBP: systolic blood pressure.
Over a median follow-up of 16.3 (9.5–17.5) years, 25.9% of the study population experienced a cardiovascular event (n=2,416; 18.6 per 1000-person years). This included 1,359 incident CHD (10.2 per 1000 person-years), 500 incident ischemic stroke (3.6 per 1000 person-years) and 1,328 incident HF hospitalizations (9.7 per 1000 person-years). Approximately, 49% of CVD events occurred in individuals with SBP <130 mmHg (n=5601) and 59% in individuals with NT-proBNP <100 pg/mL (n=6361). On the other hand, 52% of those with baseline NT-proBNP ≥300 pg/mL (n=478) experienced a CVD event in follow up.
Systolic Blood Pressure, NT-proBNP and Cardiovascular Outcomes
Event rates for CVD were lowest for those with NT-proBNP <100 and SBP <120 mm Hg or 120–129 mm Hg. Increasing levels of NT-proBNP (≥100 pg/mL) were independently associated with higher hazards for CVD events, CV mortality and all-cause mortality across each SBP category (Table 2, Supplemental Figure 2). The associations were also seen for individual outcomes of incident CHD, ischemic stroke, and HF hospitalization (Online Figure 3), with the strongest numerical association for HF hospitalization (Table 2). Individuals with NT-proBNP ≥300 pg/mL in all SBP categories, had numerically higher hazards ratio for incident stroke, HF hospitalization, CVD, CV and all-cause mortality when compared to individuals in the highest SBP category (≥150 mmHg) but lower NT-proBNP (<300 pg/mL).
Table 2.
Adjusted Hazard Ratio of Cardiovascular Events Across Systolic Blood Pressure and NT-Pro-BNP Categories, ARIC Study (1996–1998, Visit 4)
| SBP, mmHg | NT-Pro-BNP | P-trend‡ | |||||
|---|---|---|---|---|---|---|---|
| <100 pg/mL | ≥100 to <300 pg/mL | ≥300 pg/mL | |||||
| n/N (event rate*) | HR (95% CI)† | n/N (event rate*) | HR (95% CI)† | n/N (event rate*) | HR (95% CI)† | ||
| Cardiovascular disease (CVD) | |||||||
| < 120 | 466/2602 (11.95) | Ref | 160/761 (14.82) | 1.47 (1.22–1.76) | 44/106 (37.27) | 3.01 (2.19–4.14) | <0.0001 |
| 120–129 | 332/1531 (14.96) | 1.08 (0.93–1.24) | 142/517 (20.21) | 1.56 (1.29–1.89) | 33/84 (34.02) | 2.59 (1.81–3.70) | <0.0001 |
| 130–139 | 288/1073 (19.06) | 1.23 (1.06–1.43) | 138/430 (24.30) | 1.91 (1.57–2.32) | 44/78 (59.84) | 4.15 (3.03–5.69) | <0.0001 |
| 140–149 | 170/611 (20.17) | 1.22 (1.02–1.46) | 113/336 (25.55) | 1.91 (1.54–2.35) | 38/70 (51.63) | 3.35 (2.39–4.70) | <0.0001 |
| ≥ 150 | 172/544 (23.13) | 1.36 (1.13–1.63) | 186/426 (35.73) | 2.49 (2.09–2.97) | 90/140 (72.33) | 4.59 (3.63–5.81) | <0.0001 |
| P trend | 0.002 | 0.0001 | 0.01 | ||||
| Heart failure hospitalization | |||||||
| < 120 | 198/2602 (4.84) | Ref | 107/761 (9.59) | 2.13 (1.68–2.71) | 34/106 (27.18) | 4.89 (3.38–7.09) | <0.0001 |
| 120–129 | 158/1531 (6.76) | 1.12 (0.91–1.39) | 84/517 (11.24) | 1.80 (1.38–2.33) | 23/84 (22.91) | 3.63 (2.34–5.62) | <0.0001 |
| 130–139 | 137/1073 (8.49) | 1.18 (0.94–1.47) | 90/430 (14.91) | 2.38 (1.85–3.08) | 34/78 (42.53) | 6.42 (4.44–9.31) | <0.0001 |
| 140–149 | 87/611 (9.66) | 1.20 (0.93–1.55) | 75/336 (16.07) | 2.40 (1.83–3.16) | 33/70 (42.80) | 5.53 (3.78–8.09) | <0.0001 |
| ≥ 150 | 95/544 (12.11) | 1.39 (1.08–1.79) | 109/426 (19.10) | 2.68 (2.10–3.42) | 64/140 (47.90) | 5.80 (4.32–7.78) | <0.0001 |
| P trend | 0.32 | 0.10 | 0.14 | ||||
| Coronary Heart Disease (CHD) | |||||||
| < 120 | 304/2602 (7.70) | Ref | 72/761 (6.49) | 1.07 (0.82–1.39) | 22/106 (17.46) | 2.08 (1.33–3.25) | 0.03 |
| 120–129 | 199/1531 (8.80) | 1.04 (0.87–1.25) | 81/517 (11.19) | 1.53 (1.19–1.96) | 13/84 (12.20) | 1.65 (0.94–2.89) | 0.01 |
| 130–139 | 172/1073 (11.19) | 1.22 (1.01–1.48) | 67/430 (11.28) | 1.56 (1.19–2.04) | 18/78 (21.78) | 2.26 (1.39–3.66) | 0.03 |
| 140–149 | 94/611 (10.93) | 1.16 (0.91–1.46) | 58/336 (12.62) | 1.74 (1.29–2.30) | 20/70 (25.05) | 2.67 (1.68–4.24) | 0.01 |
| ≥ 150 | 95/544 (12.41) | 1.34 (1.06–1.71) | 106/426 (19.35) | 2.44 (1.93–3.07) | 38/140 (26.84) | 2.90 (2.04–4.12) | <0.0001 |
| P trend | 0.05 | 0.0001 | 0.47 | ||||
| Ischemic stroke | |||||||
| < 120 | 68/2602 (1.64) | Ref | 24/761 (2.10) | 1.42 (0.89–2.28) | 9/106 (6.73) | 3.90 (1.93–7.92) | 0.004 |
| 120–129 | 67/1531 (2.84) | 1.52 (1.08–2.14) | 37/517 (4.81) | 2.58 (1.70–3.90) | 6/84 (5.41) | 2.84 (1.22–6.61) | 0.06 |
| 130–139 | 58/1073 (3.55) | 1.66 (1.16–2.37) | 26/430 (4.16) | 2.25 (1.42–3.57) | 10/78 (11.09) | 5.22 (2.65–10.27) | 0.005 |
| 140–149 | 38/611 (4.17) | 1.79 (1.19–2.68) | 27/336 (5.55) | 2.88 (1.82–4.54) | 8/70 (9.69) | 4.55 (2.15–9.60) | 0.04 |
| ≥ 150 | 44/544 (5.54) | 2.28 (1.54–3.38) | 46/426 (7.76) | 3.71 (2.52–5.46) | 32/140 (21.60) | 8.76 (5.63–13.64) | <0.0001 |
| P trend | 0.0004 | 0.02 | 0.008 | ||||
| CV mortality | |||||||
| < 120 | 160/2602 (3.84) | Ref | 85/761 (7.34) | 2.01 (1.54–2.63) | 34/106 (24.89) | 5.06 (3.45–7.42) | <0.0001 |
| 120–129 | 137/1531 (5.70) | 1.25 (0.99–1.58) | 74/517 (9.47) | 1.88 (1.42–2.49) | 23/84 (20.42) | 4.01 (2.57–6.25) | <0.0001 |
| 130–139 | 124/1073 (7.47) | 1.37 (1.08–1.73) | 73/430 (11.43) | 2.39 (1.80–3.18) | 28/78 (29.75) | 4.95 (3.28–7.46) | <0.0001 |
| 140–149 | 76/611 (8.16) | 1.35 (1.02–1.78) | 57/336 (11.41) | 2.26 (1.66–3.08) | 27/70 (30.61) | 5.00 (3.28–7.61) | <0.0001 |
| ≥ 150 | 87/544 (10.62) | 1.61 (1.22–2.11) | 102/426 (16.52) | 2.95 (2.28–3.81) | 67/140 (41.68) | 6.15 (4.56–8.29) | <0.0001 |
| P trend | 0.02 | 0.06 | 0.13 | ||||
| All-cause mortality | |||||||
| < 120 | 494/2602 (11.84) | Ref | 211/761 (18.22) | 1.49 (1.26–1.76) | 53/106 (38.79) | 2.67 (2.00–3.57) | <0.0001 |
| 120–129 | 362/1531 (15.07) | 1.12 (0.98–1.28) | 164/517 (20.99) | 1.37 (1.14–1.64) | 50/84 (44.39) | 2.80 (2.09–3.77) | <0.0001 |
| 130–139 | 283/1073 (17.06) | 1.13 (0.97–1.31) | 148/430 (23.18) | 1.59 (1.32–1.92) | 46/78 (48.87) | 2.75 (2.02–3.75) | <0.0001 |
| 140–149 | 187/611 (20.08) | 1.23 (1.04–1.47) | 121/336 (24.22) | 1.58 (1.29–1.94) | 39/70 (44.22) | 2.75 (1.97–3.83) | 0.0006 |
| ≥ 150 | 199/544 (24.29) | 1.40 (1.18–1.66) | 179/426 (29.00) | 1.75 (1.46–2.08) | 94/140 (58.48) | 3.15 (2.50–3.95) | <0.0001 |
| P trend | 0.007 | 0.36 | 0.43 | ||||
Significant values in bold.
Event rates per 1000 person years
Cox Model adjusted for: age, race, gender, body mass index, smoking status, hypertension medication use, use of cholesterol-lowering medication diagnosed diabetes, glucose, total cholesterol/ HDL-cholesterol ratio, estimated glomerular filtration rate in mL/min/1.73m2.
p trends for hazard ratios of proportional hazard regression models were calculated based on the results of Wald chi-square test on linearity hypothesis of ordered NT-proBNP or SBP categories.
Abbreviations: CI indicated confidence interval; CV=cardiovascular; HR: adjusted Hazard Ratio; SBP: systolic blood pressure; n: number of events, N: number of persons at risk.
Of note, adults with elevated or stage 1 SBP (i.e.120–139 mm Hg) and NT-proBNP ≥100 pg/ml had higher event rates and carried significantly higher risk for incident HF, CVD, CV and all-cause mortality compared to individuals with stage 2 SBP (140–149 mmHg) but NT-proBNP <100 pg/mL (Supplemental Table 2).
In analyses stratified by BMI (<30 or ≥ 30 kg/m2) or baseline antihypertensive treatment status, the associations between NT-proBNP and incident CVD across SBP categories were qualitatively similar as in the overall cohort (Online Table 3 and Table 4). When stratified by baseline PCE risk (<10 or ≥10%), the association of NT-proBNP with risk of incident CVD were consistent across all SBP categories for those with PCE risk ≥10%. However, for those with PCE risk <10%, NT-proBNP predicted increased risk of CVD events for SBP 120–139 mmHg subgroup only; albeit the numbers of individuals/events in the SBP 140–159 mmHg and ≥160 mmHg categories were very small (Supplemental Table 5).
In fact, within the SBP 120–139 mmHg category, the CVD event rate for those with low PCE risk (<10%) and elevated NT-proBNP (≥300 pg/mL; 24.2, 95% CI 14.6–40.1 per 1000 person-years) was comparable to those with high PCE risk (≥10%) but lower NT-proBNP levels (<100 pg/mL;18.0, 95% CI 15.9–20.4 per 1000 person-years) (Supplemental Table 5).
Individuals with SBP ≥130 mmHg (vs SBP <120 mmHg) demonstrated increased risk for incident CHD, ischemic strokes and CVD across NT-proBNP categories <100 and 100-<300 pg/mL. However, for individuals in NT-proBNP category ≥300 pg/mL, there was a J-shaped association between SBP and cardiovascular events where individuals with SBP 120–129 mmHg demonstrated the lowest risk for each cardiovascular events and those with lower or higher SBP demonstrating higher risk (Table 2).
The strongest numerical hazards for cardiovascular events were seen in individuals in the highest SBP (≥150 mmHg) and NT-proBNP category (≥300 pg/mL) (Table 2 and Figure 1). However, there was no significant interaction between SBP and NT-proBNP for risk of all cardiovascular events except for CV mortality (p-value-for-interaction=0.005) (Supplemental Table 1).
Figure 1. Forest Plot of Adjusted Hazard Ratio of Cardiovascular Disease (CVD) Events Across Systolic Blood Pressure (SBP) and NT-proBNP Categories.
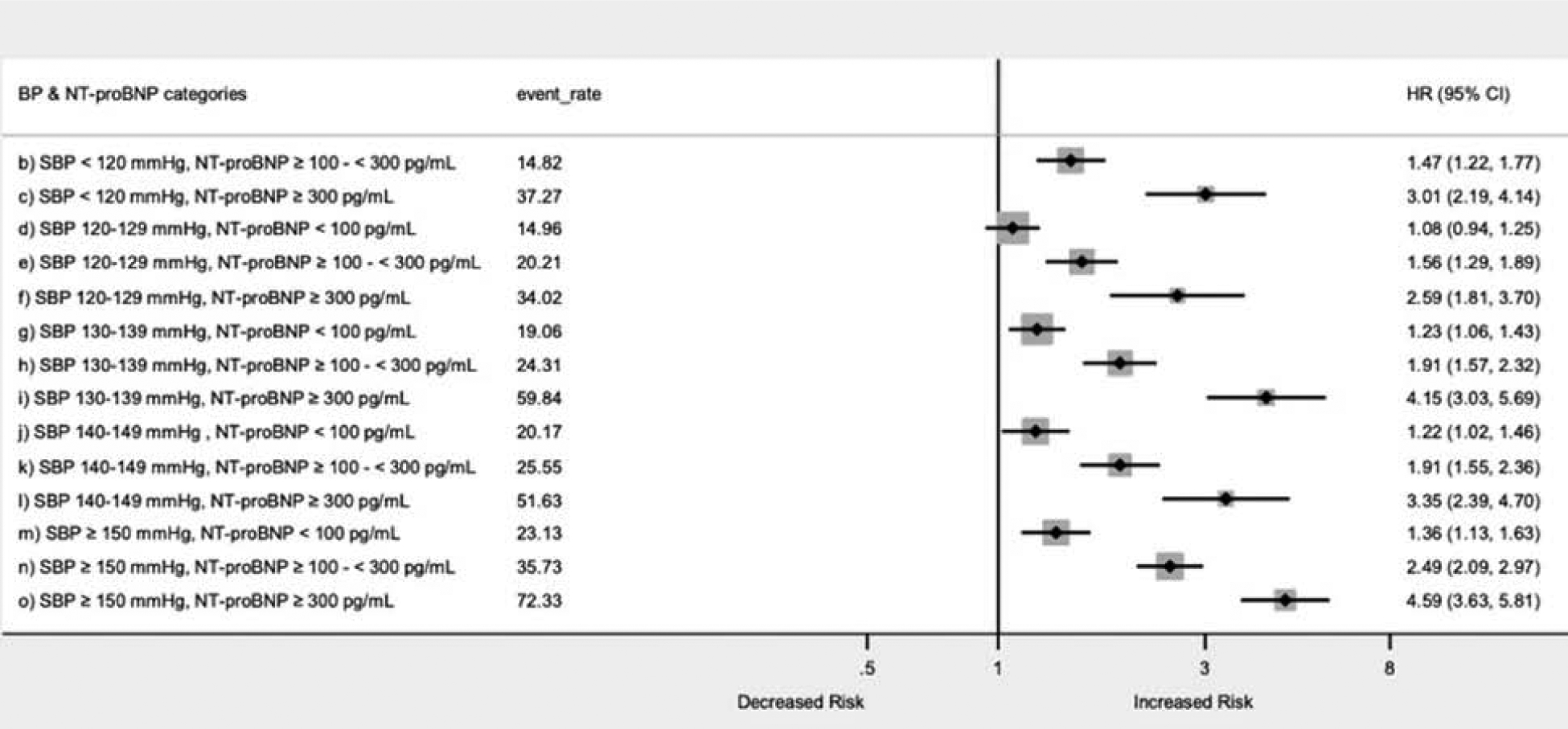
Forest plot represents the hazard’s ratio (HR) and 95% confidence interval (CI) for the association of NT-proBNP with CVD events stratified by SBP. HR calculated using Cox proportional hazards models adjusted for age, sex, race, use of antihypertensive drug, use of lipid lowering medication, estimated glomerular filtration rate, diabetes mellitus glucose, total cholesterol/ high density lipoprotein cholesterol ratio, body mass index and smoking status. Increasing levels of NT-proBNP (≥100 pg/mL) were independent associated with increased risk of CVD events across each SBP category
NT-proBNP, diastolic blood pressure and cardiovascular outcomes
Increasing NT-proBNP categories (100-<300 and ≥300 vs <100 pg/mL) demonstrated consistently higher event rates and significantly increased hazards for each cardiovascular event across DBP strata (Table 3, Supplemental Figure 4). DBP showed a J-shaped association with cardiovascular events; individuals with DBP between 60–79 mmHg had lower whereas those with DBP <60 mmHg or ≥90 mmHg had higher event rates (Supplemental Figure 4). There was a significant interaction between DBP and NT-proBNP categories for association with HF hospitalization (p-value-for-interaction=0.05) and CVD events (p-value-for-interaction=0.02) (Supplemental Table 1). DBP <60 mmHg (vs DBP 70–79 mmHg) was associated with an increased risk for incident HF hospitalization and CVD when NT-proBNP was <100 pg/mL. However, the association of low DBP (<60 mmHg) and CVD events were attenuated in higher NT-proBNP (≥100 pg/mL) categories (Table 3).
Table 3:
Adjusted Hazards Ratio of Cardiovascular Events Across Diastolic Blood Pressure and NT-proBNP Categories, ARIC Study (1996–1998, Visit 4)
| DBP, mmHg | NT-Pro-BNP | P trend‡ | |||||
|---|---|---|---|---|---|---|---|
| <100 pg/mL | ≥100 to <300 pg/mL | ≥300 pg/mL | |||||
| n/N (event rate*) | HR (95% CI)† | n/N (event rate*) | HR (95% CI)† | n/N (event rate*) | H (95% CI)† | ||
| Cardiovascular disease (CVD) | |||||||
| <60 | 173/654 (18.94) | 1.24 (1.04–1.47) | 104/353 (21.94) | 1.60 (1.28–1.98) | 36/72 (51.37) | 3.13 (2.21–4.43) | <0.0001 |
| 60–69 | 427/2061 (14.30) | 0.97 (0.85–1.10) | 216/816 (19.88) | 1.50 (1.27–1.77) | 77/148 (51.09) | 3.51 (2.75–4.49) | <0.0001 |
| 70–79 | 557/2441 (15.63) | Ref | 242/848 (20.74) | 1.54 (1.32–1.80) | 71/137 (47.23) | 3.24 (2.52–4.17) | <0.0001 |
| 80–89 | 221/1030 (14.72) | 0.93 (0.79–1.09) | 135/357 (29.30) | 2.02 (1.67–2.44) | 48/92 (53.38) | 3.16 (2.34–4.26) | <0.0001 |
| ≥90 | 50/175 (20.08) | 1.26 (0.94–1.69) | 42/96 (33.60) | 2.19 (1.60–3.01) | 17/29 (65.64) | 2.49 (1.52–4.07) | 0.009 |
| P trend | 0.02 | 0.06 | 0.95 | ||||
| Heart Failure hospitalization | |||||||
| <60 | 94/654 (9.74) | 1.39 (1.10–1.77) | 72/353 (14.51) | 2.04 (1.55–2.68) | 28/72 (38.73) | 4.83 (3.24–7.20) | <0.0001 |
| 60–69 | 198/2061 (6.28) | 0.96 (0.79–1.15) | 130/816 (11.31) | 1.80 (1.45–2.24) | 62/148 (38.43) | 5.13 (3.84–6.84) | <0.0001 |
| 70–79 | 270/2441 (7.18) | Ref | 154/848 (12.53) | 1.93 (1.57–2.37) | 55/137 (33.90) | 5.23 (3.88–7.05) | <0.0001 |
| 80–89 | 92/1030 (5.80) | 0.83 (0.65–1.06) | 82/357 (16.50) | 2.35 (1.83–3.01) | 31/92 (33.09) | 3.52 (2.41–5.13) | <0.0001 |
| ≥90 | 21/175 (7.92) | 1.01 (0.65–1.58) | 27/96 (20.34) | 2.67 (1.79–3.98) | 12/29 (45.13) | 4.21 (2.33–7.61) | <0.0001 |
| P-trend | 0.03 | 0.31 | 0.84 | ||||
| Coronary heart disease (CHD) | |||||||
| <60 | 103/654 (11.07) | 1.25 (1.00–1.57) | 49/353 (10.02) | 1.34 (0.98–1.83) | 17/72 (22.27) | 2.40 (1.44–4.00) | 0.08 |
| 60–69 | 273/2061 (8.99) | 1.03 (0.88–1.21) | 117/816 (10.40) | 1.42 (1.14–1.77) | 34/148 (20.21) | 2.20 (1.53–3.16) | <0.0001 |
| 70–79 | 328/2441 (9.05) | Ref | 126/848 (10.45) | 1.44 (1.17–1.78) | 33/137 (20.25) | 2.30 (1.60–3.31) | <0.0001 |
| 80–89 | 131/1030 (8.59) | 0.93 (0.76–1.14) | 74/357 (15.33) | 1.89 (1.46–2.43) | 20/92 (19.90) | 2.29 (1.45–3.61) | <0.0001 |
| ≥90 | 29/175 (11.40) | 1.31 (0.89–1.92) | 18/96 (13.60) | 1.63 (1.01–2.63) | 7/29 (24.54) | 1.35 (0.63–2.88) | 0.94 |
| P-trend | 0.15 | 0.57 | 0.80 | ||||
| Ischemic stroke | |||||||
| <60 | 31/654 (3.13) | 1.08 (0.72–1.62) | 20/353 (3.93) | 1.41 (0.86–2.31) | 7/72 (8.77) | 2.75 (1.26–5.99) | 0.17 |
| 60–69 | 71/2061 (2.22) | 0.83 (0.62–1.13) | 39/816 (3.27) | 1.24 (0.85–1.81) | 21/148 (11.83) | 3.95 (2.42–6.42) | <0.0001 |
| 70–79 | 107/2441 (2.81) | Ref | 57/848 (4.51) | 1.75 (1.26–2.44) | 13/137 (7.26) | 2.52 (1.40–4.54) | 0.0009 |
| 80–89 | 52/1030 (3.26) | 1.20 (0.86–1.67) | 35/357 (6.80) | 2.50 (1.70–3.67) | 17/92 (17.00) | 5.00 (2.97–8.44) | <0.0001 |
| ≥90 | 14/175 (5.31) | 1.86 (1.06–3.26) | 9/96 (6.47) | 2.10 (1.06–4.16) | 7/29 (24.13) | 5.00 (2.27–11.02) | 0.02 |
| P-trend | 0.06 | 0.11 | 0.11 | ||||
| CV Mortality | |||||||
| <60 | 88/654 (8.80) | 1.54 (1.20–1.99) | 62/353 (11.91) | 2.00 (1.49–2.68) | 28/72 (34.86) | 5.44 (3.60–8.21) | <0.0001 |
| 60–69 | 179/2061 (5.55) | 1.07 (0.88–1.31) | 118/816 (9.80) | 1.95 (1.54–2.45) | 56/148 (29.98) | 4.52 (3.33–6.15) | <0.0001 |
| 70–79 | 214/2441 (5.54) | Ref | 122/848 (9.43) | 1.80 (1.43–2.26) | 51/137 (27.55) | 4.69 (3.42–6.42) | <0.0001 |
| 80–89 | 81/1030 (4.99) | 0.92 (0.71–1.19) | 63/357 (11.81) | 2.15 (1.62–2.86) | 30/92 (27.58) | 3.69 (2.50–5.45) | <0.0001 |
| ≥90 | 22/175 (8.05) | 1.38 (0.89–2.15) | 26/96 (18.30) | 3.31 (2.20–5.00) | 14/29 (44.67) | 4.59 (2.64–7.96) | 0.0012 |
| P-trend | 0.0064 | 0.1560 | 0.8733 | ||||
| All-cause Mortality | |||||||
| <60 | 209/654 (20.90) | 1.37 (1.16–1.61) | 128/353 (24.59) | 1.49 (1.22–1.83) | 50/72 (62.25) | 3.63 (2.69–4.90) | <0.0001 |
| 60–69 | 505/2061 (15.65) | 1.15 (1.02–1.30) | 282/816 (23.41) | 1.65 (1.42–1.92) | 86/148 (46.05) | 2.81 (2.22–3.55) | <0.0001 |
| 70–79 | 525/2441 (13.60) | Ref | 248/848 (19.16) | 1.35 (1.16–1.58) | 78/137 (42.14) | 2.64 (2.07–3.37) | <0.0001 |
| 80–89 | 234/1030 (14.42) | 1.11 (0.95–1.30) | 125/357 (23.43) | 1.68 (1.38–2.05) | 49/92 (45.04) | 2.60 (1.94–3.50) | <0.0001 |
| ≥90 | 52/175 (19.03) | 1.54 (1.15–2.05) | 40/96 (28.15) | 2.11 (1.53–2.92) | 19/29 (60.62) | 3.15 (1.98–4.99) | 0.0380 |
| P-trend | 0.0007 | 0.0623 | 0.5453 | ||||
Significant values in bold.
Event rates per 1000 person-years
Cox Model adjusted for: age, race, gender, body mass index, smoking status, hypertension medication use, use of cholesterol-lowering medication diagnosed diabetes, glucose, total cholesterol/ HDL-cholesterol ratio, estimated glomerular filtration rate in mL/min/1.73m2.
p trends for hazard ratios of proportional hazard regression models were calculated based on the results of Wald chi-square test on linearity hypothesis of ordered NT-proBNP or DBP categories.
Abbreviations: CI indicated confidence interval; CV=cardiovascular; HR: adjusted Hazard Ratio; SBP: systolic blood pressure; n: number of events, N: number of persons at risk
Pulse pressure, NT-proBNP and cardiovascular outcomes
Within each PP category, a higher category of NT-proBNP was associated with significantly increased risk for incident CHD, ischemic stroke, HF hospitalization events, CV and all-cause mortality (Table 4, Supplemental Figure 5). There was no significant interaction between NT-proBNP and PP categories and their association with cardiovascular events except for CV mortality (p-value-for-interaction <0.0001) (Supplemental Table 1).
Table 4.
Adjusted Hazards Ratio of Cardiovascular Events Across Pulse Pressure and NT-Pro-BNP Categories, ARIC Study (1996–1998, Visit 4)
| Pulse Pressure, mmHg | NT-Pro-BNP, pg/mL | P trend† | |||||
|---|---|---|---|---|---|---|---|
| <100 | ≥100 to <300 | ≥300 | |||||
| n/N (event rate) | HR (95% CI)* | n/N (event rate) | HR (95% CI)* | n/N (event rate) | HR (95% CI)* | ||
| Cardiovascular disease (CVD) | |||||||
| <40 | 144/909 (10.30) | Ref | 34/211 (10.87) | 1.30 (0.89-1.89) | 12/30 (33.56) | 2.77 (1.53–5.00) | 0.03 |
| 40–49 | 336/1902 (11.78) | 1.00 (0.82–1.21) | 102/485 (14.74) | 1.59 (1.23–2.05) | 22/58 (34.063) | 2.74 (1.73–4.34) | <0.0001 |
| 50–59 | 369/1688 (15.13) | 1.16 (0.95–1.41) | 184/610 (22.44) | 1.98 (1.58–2.48) | 49/107 (41.96) | 3.53 (2.53–4.91) | <0.0001 |
| 60–69 | 300/1051 (20.69) | 1.41 (1.15–1.73) | 158/520 (22.94) | 1.90 (1.51–2.41) | 45/95 (44.74) | 3.29 (2.33–4.63) | <0.0001 |
| ≥70 | 279/811 (35.90) | 1.63 (1.32–2.01) | 261/644 (32.63) | 2.58 (2.08–3.19) | 121/188 (71.64) | 5.46 (4.23–7.05) | <0.0001 |
| P trend† | <0.0001 | 0.0001 | 0.003 | ||||
| Heart Failure Hospitalization | |||||||
| <40 | 53/909 (3.62) | Ref | 22/211 (6.87) | 2.22 (1.35–3.67) | 10/30 (27.60) | 6.01 (3.04–11.85) | <0.0001 |
| 40–49 | 145/1902 (4.84) | 1.10 (0.81–1.51) | 62/485 (8.60) | 2.24 (1.55–3.25) | 14/58 (20.09) | 4.13 (2.28–7.47) | <0.0001 |
| 50–59 | 172/1688 (6.67) | 1.24 (0.91–1.70) | 124/610 (14.33) | 2.87 (2.07–3.99) | 39/107 (31.30) | 6.29 (4.12–9.60) | <0.0001 |
| 60–69 | 137/1051 (8.87) | 1.37 (0.99–1.90) | 90/520 (12.26) | 2.24 (1.58–3.18) | 32/95 (30.05) | 4.65 (2.96–7.29) | <0.0001 |
| ≥70 | 168/811 (14.65) | 1.97 (1.43–2.72) | 167/644 (19.35) | 3.24 (2.35–4.46) | 93/188 (51.90) | 8.15 (5.73–11.59) | <0.0001 |
| P-trend† | 0.0001 | 0.017 | 0.009 | ||||
| Coronary heart disease (CHD) | |||||||
| <40 | 93/909 (6.57) | Ref | 10/211 (3.12) | 0.63 (0.33–1.20) | 6/30 (15.17) | 1.93 (0.84–4.42) | 0.13 |
| 40–49 | 217/1902 (7.51) | 1.05 (0.82–1.34) | 56/485 (7.91) | 1.50 (1.07–2.10) | 10/58 (14.99) | 1.89 (0.95–3.76) | 0.03 |
| 50–59 | 230/1688 (9.31) | 1.25 (0.98–1.60) | 94/610 (11.01) | 1.76 (1.31–2.36) | 21/107 (16.21) | 2.20 (1.36–3.56) | 0.002 |
| 60–69 | 169/1051 (11.39) | 1.41 (1.09–1.83) | 83/520 (11.71) | 1.86 (1.37–2.53) | 22/95 (20.17) | 2.52 (1.57–4.06) | 0.02 |
| ≥70 | 155/811 (13.93) | 1.65 (1.26–2.16) | 141/644 (16.70) | 2.54 (1.93–3.35) | 52/188 (27.13) | 3.79 (2.65–5.42) | <0.0001 |
| P-trend† | <0.0001 | 0.0001 | 0.29 | ||||
| Ischemic Stroke | |||||||
| <40 | 18/909 (1.22) | Ref | 5/211(1.54) | 1.53 (0.57–4.14) | 3/30 (7.42) | 5.50 (1.61–18.76) | 0.12 |
| 40–49 | 53/1902 (1.75) | 1.29 (0.76–2.20) | 22/485 (2.97) | 2.60 (1.39–4.88) | 6/58 (8.36) | 6.34 (2.50–16.12) | 0.0008 |
| 50–59 | 73/1688 (2.81) | 1.83 (1.09–3.08) | 32/610 (3.56) | 2.57 (1.43–4.63) | 5/107 (3.62) | 2.40 (0.88–6.53) | 0.34 |
| 60–69 | 70/1051 (4.48) | 2.50 (1.48–4.24) | 41/520 (5.48) | 3.67 (2.07–6.49) | 12/95 (10.51) | 6.14 (2.90–12.97) | 0.002 |
| ≥70 | 61/811 (5.16) | 2.64 (1.54–4.55) | 60/644 (6.63) | 4.11 (2.38–7.09) | 39/188 (19.40) | 10.97 (6.13–19.65) | <0.0001 |
| P-trend† | <0.0001 | 0.15 | 0.009 | ||||
| CV Mortality | |||||||
| <40 | 42/909 (2.83) | Ref | 14/211 (4.26) | 1.70 (0.93–3.12) | 10/30 (24.31) | 6.62 (3.31–13.26) | 0.0002 |
| 40–49 | 101/1902 (3.31) | 0.95 (0.66–1.36) | 48/485 (6.40) | 2.14 (1.41–3.26) | 19/58 (25.64) | 5.85 (3.34–10.23) | <0.0001 |
| 50–59 | 158/1688 (5.99) | 1.51 (1.07–2.12) | 98/610 (10.74) | 2.76 (1.91–3.99) | 30/107 (21.37) | 5.07 (3.14–8.18) | <0.0001 |
| 60–69 | 133/1051 (8.34) | 1.69 (1.19–2.41) | 83/520 (10.85) | 2.61 (1.78–3.83) | 30/95 (24.92) | 4.53 (2.80–7.32) | <0.0001 |
| ≥70 | 150/811 (12.42) | 2.21 (1.55–3.15) | 148/644 (15.77) | 3.36 (2.36–4.79) | 90/188 (41.61) | 8.19 (5.59–12.01) | <0.0001 |
| P-trend† | <0.0001 | 0.0303 | 0.0101 | ||||
| All-cause Mortality | |||||||
| <40 | 137/909 (9.22) | Ref | 49/211 (14.91) | 1.65 (1.19–2.30) | 15/30 (36.46) | 3.01 (1.76–5.14) | 0.0002 |
| 40–49 | 333/1902 (10.90) | 1.01 (0.83–1.23) | 122/485 (16.26) | 1.57 (1.23–2.01) | 29/58 (39.14) | 3.09 (2.05–4.66) | <0.0001 |
| 50–59 | 407/1688 (15.42) | 1.26 (1.03–1.53) | 190/610 (20.82) | 1.61 (1.29–2.02) | 51/107 (36.32) | 2.65 (1.91–3.68) | <0.0001 |
| 60–69 | 340/1051 (21.31) | 1.43 (1.17–1.76) | 196/520 (25.62) | 1.89 (1.51–2.37) | 59/95 (49.00) | 3.02 (2.20–4.13) | <0.0001 |
| ≥70 | 308/811 (25.51) | 1.58 (1.28–1.94) | 266/644 (28.35) | 1.86 (1.50–2.31) | 128/188 (59.18) | 3.83 (2.97–4.92) | <0.0001 |
| P-trend† | <0.0001 | 0.2656 | 0.0763 | ||||
Significant values in bold.
Event rates per 1000 person-years
Cox Model adjusted for: age, race, gender, body mass index, smoking status, hypertension medication use, use of cholesterol-lowering medication diagnosed diabetes, glucose, total cholesterol/ HDL-cholesterol ratio, estimated glomerular filtration rate in mL/min/1.73m2.
p trends for hazard ratios of proportional hazard regression models were calculated based on the results of Wald chi-square test on linearity hypothesis of ordered NT-proBNP or pulse pressure categories.
Abbreviations: CI indicated confidence interval; CV=cardiovascular; HR: adjusted Hazard Ratio; n: number of events, N: number of persons at risk
Individuals with the highest PP (≥60 mmHg) and NT-proBNP (≥300 pg/ml) had the highest numerical hazards for CHD (HR: 3.79; 95% CI: 2.65–5.42), ischemic strokes (HR 10.97; 95% CI: 6.13–19.65) and HF hospitalizations (HR: 8.15; 95% CI: 5.73–11.59) when compared to individuals with PP <40 mmHg and NT-proBNP <100 pg/ml (Table 4).
Potential role of NT-proBNP in treatment decisions
Participants with NT-proBNP <100 pg/ml had lower CVD event rates and hence higher estimated NNT10 at all levels of baseline SBP and PCE risk. On the other hand, a low NNT10 to prevent CVD (between 3 and 20), was estimated for persons with SBP ≥160 mmHg irrespective of baseline NT-proBNP levels or estimated PCE risk (Central Illustration, Supplemental Table 6). Overall, NT-proBNP demonstrated the greatest value when NNT10 was considered in individuals with SBP 120–159 mmHg; for example among individuals with PCE <10% and, SBP 120–139 mmHg, those with NT-proBNP <100 pg/ml had a much higher NNT10 of 82 compared to those within same BP and PCE category but NT-proBNP ≥300 pg/ml (NNT10 of 21). Similar results were noted when incident CHD, ischemic stroke and HF hospitalization were assessed individually (Supplemental Table 6).
Central Illustration. Ten-year number needed to treat for prevention of an incident cardiovascular disease across systolic blood pressure categories stratified by NT-proBNP categories and sub-stratified by PCE risk group.
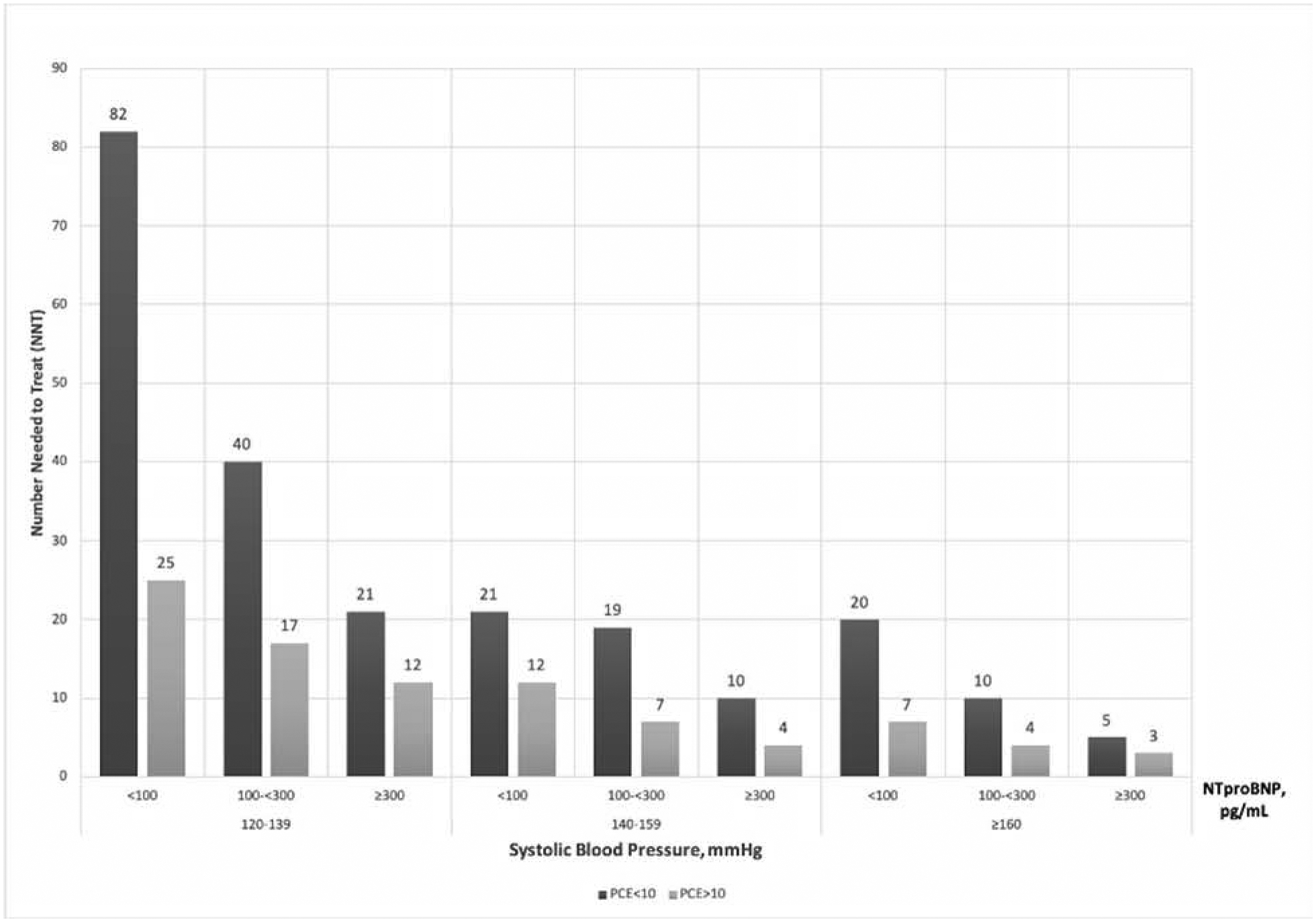
Number needed to treat (NNT10) to prevent one CVD event over 10 years with BP treatment initiation or intensification to SBP goal of 120 mmHg were calculated for each combined SBP and NT-proBNP category, sub-stratified by PCE risk (<10% or ≥10%). For each 10-mmHg reduction, we assumed a 25% relative risk reduction in CVD based on results from SPRINT(2). Individuals with increasing levels of NT-proBNP demonstrated lower NNT10 across SBP and pooled cohort equation (PCE) risk groups.
Individuals in the same BP category with low PCE risk (<10%) but higher NT-proBNP level (≥300 pg/ml) had comparable if not lower NNT10 to prevent CVD events as individuals with high PCE risk (≥10%) but lower NT-proBNP (<100 pg/ml). For example, among individuals with SBP 120–139 mmHg the NNT10 to prevent 1 CVD event in those with elevated NT-proBNP of ≥300 pg/ml and PCE risk <10%, was 21 when compared to an NNT10 of 25 for those with a PCE ≥10% and NT-proBNP of <100 pg/mL. Similarly, in individuals with SBP 140–159 mmHg the NNT10 was 10 for those with NT-proBNP ≥300 pg/ml and PCE risk <10%, vs NNT10 of 12 with PCE ≥10% and NT-proBNP of <100 pg/mL (Central Illustration).
Discussion
There has been a recent paradigm shift in the management of hypertension, with recommendations to move from a traditional approach of therapy based solely on BP values to one based on both BP and underlying CVD risk(6). Our results add to this emerging body of literature by demonstrating that NT-proBNP independently predicted increased risk for incident CVD events and individual outcomes of incident CHD, ischemic stroke, HF hospitalization, CV and all-cause mortality across narrow categories of SBP, DBP and PP in a large prospective cohort of adults without prevalent CVD. The associations were particularly strong for HF. Moreover, these associations persisted after stratification by BMI, anti-hypertensive treatment or PCE risk.
Data has shown that although there is consistent relative risk reduction per unit decrease in SBP, individuals with higher baseline ASCVD risk derive greater absolute risk reduction and clinical benefit from BP treatment(19). This is particularly important as intensive BP control comes with increased risk for side effects especially in the elderly. Based on this concept, current guidelines recommend aggressive BP control (goal <130/80 mmHg) for individuals at the highest risk for CVD e.g. known CHD, diabetes or PCE risk ≥10%(6). Other groups have suggested higher threshold of 10-year ASCVD risk (~18%) based on a “benefit-to-harm” ratio for intensive BP treatment(20). In our study, NT-proBNP ≥300 pg/mL was associated with a 10-year CVD event rate >18% irrespective for SBP or PCE risk suggesting that it would clearly identify high-risk individuals by any criteria.
We also found that persons with stage 1 hypertension (SBP 120–139 mmHg) and NT-proBNP ≥100 pg/mL had significantly higher risk for CVD and mortality (primarily HF hospitalization and CV mortality) compared to those with stage 2 hypertension (SBP ≥140–149 mmHg) but NT-proBNP <100 pg/mL. This group is particularly important as decisions to initiate or escalate therapy to treat to intensive SBP targets of <130 mmHg (rather than 140 mmHg) are challenging in the context of results from SPRINT(2) and HOPE3(5). All participants with either SBP ≥150 mm Hg irrespective of NT-proBNP level or NT-proBNP ≥300 pg/mL irrespective of SBP had higher CVD event rates. However, individuals with elevation of both NT-proBNP and either SBP or PP demonstrated the highest risk for cardiovascular events.
Moreover, risk assessment using traditional risk factors (PCE) as suggested by current guidelines have limitations as they can underestimate risk in certain racial/ethnic groups, among those with lower socioeconomic status or with chronic inflammatory diseases while overestimating risk in certain contemporary cohorts(21). Another major issue is that events captured in PCE are atherosclerotic and does not assess HF outcomes or mortality. As seen in our analysis and clinical trials such as SPRINT, HF and CV mortality are important CV outcomes (and most frequent in the elderly). Hence, better tools to identify higher risk individuals are needed to guide BP treatment.
Low risk individuals (PCE risk <10%) with SBP 120–159 mmHg but NT-proBNP ≥300 pg/mL demonstrated higher 10-year CVD event rates with lower estimated NNT10 compared to those with lower NT-proBNP (<100 pg/mL) in the same BP and PCE risk category (Central Illustration) thereby identifying a higher risk group. Overall, we found NT-proBNP provided additive and incremental value to different BP parameters in identifying individuals with higher cardiovascular risk. Hence, more intensive BP targets may be considered when: 1) SBP ≥150 mmHg 2) estimated CVD risk based on traditional risk factors (PCE) was ≥ 10%, and most importantly 3) NT-proBNP ≥ 300 pg/mL irrespective of stage 1 or 2 hypertension or PCE risk.
NT-proBNP is a strong prognostic marker for predicting adverse cardiovascular outcomes in HF, CHD and diabetes mellitus(22,23) with a recent interest in its role in hypertension(24,25). Use of NT-proBNP to identify patients with diabetes for treatment with combined neuro-humoral therapy proved to be an effective strategy to prevent hospitalizations or CVD death in the PONTIAC study(26). Similarly, in the St Vincent’s Screening to Prevent Heart Failure (STOP-HF) clinical trial, BNP-based screening to identify individuals to refer to cardiologist reduced rates of combined systolic and diastolic dysfunction and HF(27). Increased NT-proBNP levels are indicative of increased wall stress and volume expansion, which may contribute to development of CVD events especially HF, even among those with BP in a normal range(28). This may also explain why individuals in our study with lower SBP but higher NT-proBNP levels had risk equivalent to if not higher than those with higher SBP (≥150 mmHg) but lower NT-proBNP levels.
A previous study from ARIC demonstrated that hs-cTnT predicted incident CVD across SBP categories(7). Similarly, our study provides a strong case for the use of NT-proBNP to identify higher risk individuals within narrow BP categories who could be expected to benefit more from more intensive BP goals. In a recent pooled cohort analysis from ARIC, Dallas Heart Study and Multiethnic Study of Atherosclerosis, combined elevation in NT-proBNP and hs-cTnT in participants with elevated BP or low-risk stage I hypertension, according to current BP guidelines, predicted a higher 10-year risk for incident ASCVD or HF (≥10%) and lower NNT compared to those with non-elevated biomarkers(10). Moving forward future prospective clinical trials should evaluate whether strategies as used in the STOP-HF and PONTIAC trials i.e., using a panel of biomarkers, such as NT-proBNP and hs-cTnT, to inform BP treatment goals result in net clinical benefit in CV prevention.
Another interesting finding in our study is that when considering stroke where traditionally SBP is a dominant risk factor, NT-proBNP predicted increased risk for incident stroke irrespective of SBP or DBP levels. On the other hand, the association of hs-cTnT with ischemic stroke in ARIC was found to be modest at best, especially at lower SBP categories(7). This parallels a previous study where NT-proBNP showed stronger association for cardioembolic and non-lacunar strokes than hs-cTnT(29).
Association of diastolic blood pressure and NT-proBNP with cardiovascular events
Low DBP (<60 mmHg) has been shown to be associated with prevalent and progressive myocardial damage (as evidenced by higher hs-cTnT levels), with a previous analysis from ARIC showing that low DBP had a significant interaction with elevated hs-cTnT in prediction of incident CHD(8). Our study echoes these findings as DBP<60 mmHg was associated higher rate of CVD, CV mortality and all-cause mortality compared to higher DBP values. Moreover, the association of DBP and CVD events showed a significant interaction with NT-proBNP, with the association being strongest for baseline NT-proBNP ≥300 pg/ml. Together, both studies, may provide a mechanistic link to explain why low DBP can result in adverse cardiovascular events. Low DBP (subclinical low perfusion pressures in the coronary arteries) may lead to myocardial damage (reflected by hs-cTnT) and neurohormonal activation with increased myocardial stiffness/fibrosis and adverse remodeling (reflected by NT-proBNP) which in turn may interact to increase the incidence of CVD. Thus, the presence of baseline elevation of hs-cTnT and NT-proBNP in an individual may call for careful follow-up of DBP levels when aggressive BP management is considered and may need to be evaluated in future studies.
Role of pulse pressure and NT-proBNP in cardiovascular risk assessment
In our study, we show that PP may play an important role in hypertension management. Despite recent evidence about benefits of intensive BP reduction in high risk patients, there is continued controversy about systolic and diastolic BP targets in clinical practice. Another approach could be to focus on PP which is a marker of arterial stiffness. With loss of aortic compliance, systolic pressures rise, and diastolic pressures decline resulting in an increase in pulse pressure. In our study, NT-proBNP showed the strongest association with cardiovascular events including CV and all-cause mortality in individuals with the widest pulse pressure. Individuals with wide PP will have an increased afterload (high SBP) along with decreased coronary perfusion (low DBP) which could result in greater subclinical myocardial damage and explain increased risk for cardiovascular events and mortality. McEvoy et al demonstrated that individuals with PP ≥60 mmHg and detectable hs-cTnT had the highest risk for CV events(8). BP control in this group will be the most challenging as benefit from reduction in SBP may be offset by increased myocardial injury from DBP lowering. Biomarkers such as NT-proBNP and troponin may therefore need to be evaluated not only to identify higher risk individuals but perhaps also to monitor intensity of therapy.
Limitations
Our study has some limitations. First, being an observational study, our inferences do not reflect direct causality and we must always recognize the potential for residual, uncontrolled confounding that may partly explain the associations. Second, while we can establish that NT-proBNP may help classify risk in lower BP categories, due to the observational nature of our study, prospective clinical trials are needed to establish whether aggressive BP management in these groups will improve cardiovascular outcomes and have similar NNT10 to our study. Moreover, the relative risk reduction used to estimate NNT10 is based on the assumption that a 10-mmHg reduction will have proportional effects in all BP groups which may not be the case. Third, despite a large sample size, certain subgroups (example NT-proBNP ≥300 pg/mL and SBP 130–139mmHg or 140–149mmHg) had relatively small numbers. Fourth the diagnosis of hypertension in clinical practice is based on at least 2 BP measurements ≥130/80 on two separate occasions. In our study, hypertension was defined as use of antihypertensive medications or blood pressure of ≥140/90 and participants were categorized into blood pressure groups based on two BP readings 5 minutes apart at the same visit. Lastly, although we performed stratified analysis to exclude participants who were taking antihypertensive medication before baseline visit, some may have been initiated on anti-hypertensive medications on follow-up. Antihypertensive medication initiation would be expected to lower incident CV event rates and may therefore result in underestimation of CV risk in the present analysis.
Conclusion
Measurement of NT-proBNP, in in ambulatory patients without baseline CVD, can provide incremental and independent prognostic value in identifying individuals at higher cardiovascular risk and allow for personalized BP management. From a clinical perspective, our study suggests that individuals with higher concentrations of NT-proBNP across a range of mildly elevated BPs (120–149 mmHg) could identify those at higher risk for CHD, HF, ischemic stroke, CV and all-cause mortality who may benefit from intensive BP goals. Future trials should consider validation of a biomarker-assisted approach to guide risk-based decisions for BP treatment initiation or titration.
Supplementary Material
Clinical Perspectives.
Competency in Medical Knowledge:
Increased blood levels of NT-proBNP are associated with an increased risk of cardiovascular events across categories of systolic and diastolic blood pressure and pulse pressure.
Translational Outlook:
Future studies should examine whether elevated levels of NT-proBNP identifies adults who benefit from more intensive blood pressure lowering.
Acknowledgements:
The authors thank the staff and participants of the ARIC study for their important contributions. Roche supplied reagents for hs-cTnT and NT-proBNP.
Funding
The Atherosclerosis Risk in Communities study has been funded in whole or in part with federal funds from the National Heart, Lung, and Blood Institute, National Institutes of Health, Department of Health and Human Services, under Contract nos. (HHSN268201700001I, HHSN268201700002I, HHSN268201700003I, HHSN268201700005I, HHSN268201700004I). Dr. Selvin is supported by National Institutes of Health grants K24-DK106414 and R01-DK089174. Drs. Selvin and Ballantyne are supported by National Institutes of Health grant R01-HL134320. Dr Virani has research support/grant from Department of Veterans Affairs and World Heart Federation. Dr. Shah was supported by NIH R01-HL135008, R01-HL143224, R01-HL150342, and K24-HL152008. Dr. Nambi is supported by a VA MERIT grant 1I01CX001112-01. Roche Diagnostics provided reagents and loan of an instrument to conduct the highly sensitive cTnT and NT-proBNP assays.
Disclosures:
Dr. Hussain, Ms. Sun, Dr Deswal, Dr McEvoy, Dr. Matsushita, Dr. Aguilar, Dr. Bozkurt, Dr. Ndumule declare that they have no conflict of interest or relationship relevant to the contents of this paper to disclose. Dr. de Lemos receives grant support and consulting income from Roche Diagnostics and Abbott Diagnostics, consulting income from Ortho Clinical Diagnostics and Quidel Cardiovascular, Inc. Dr. Hoogeveen has received research grants (to his institution) from Denka Seiken and is a consultant for Denka Seiken. Dr. Virani receives honorarium from American College of Cardiology (Associate editor for Innovations acc.org) and is part of Steering Committee member: PALM registry at Duke Clinical Research Institute (no financial remuneration). Dr Shah has research support (significant; paid to institution, not individual) from Novartis, and is a consultant (modest) for Philips Ultrasound. Dr. Selvin has received honoraria from Novo Nordisk. Dr. Ballantyne has received National Institutes of Health grant R01HL134320; has received grants or research support (to his institution) from Abbott Diagnostic, Akcea, Amgen, Esperion, Novartis, Regeneron, and Roche Diagnostic and is a consultant for Abbott Diagnostics, Akcea, Amarin, Amgen, AstraZeneca, Boehringer Ingelheim, Corvidia, Denka Seiken, Esperion, Intercept, Janssen, Matinas BioPharma Inc., Merck, Novartis, Novo Nordisk, Regeneron, Roche Diagnostic, and Sanofi-Synthelabo. Dr. Ballantyne and Dr. Nambi are named on provisional patent no. 61721475 “Biomarkers to Improve Prediction of Heart Failure Risk” filed by Baylor College of Medicine and Roche. Dr. Nambi is site principal investigator for a study sponsored by Merck and Amgen.
Abbreviations:
- ARIC
Atherosclerosis Risk in Communities Study
- NT-proBNP
N-terminal pro–B-type natriuretic peptide
- CVD
cardiovascular disease
- CHD
coronary heart disease
- HF
heart failure
- SBP
systolic blood pressure
- DBP
diastolic blood pressure
- PP
pulse pressure
- PCE
pooled cohort equation
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Lewington S, Clarke R, Qizilbash N, Peto R, Collins R, Prospective Studies Collaboration. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies 2002;360:1903–1913. [DOI] [PubMed] [Google Scholar]
- 2.SPRINT Research Group, Wright JT Jr, Williamson JD, et al. Randomized Trial of Intensive versus Standard Blood-Pressure Control. N Engl J Med. 2015;373:2103–2116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.ACCORD Study Group, Cushman WC, Evans GW, et al. Effects of intensive blood‐pressure control in type 2 diabetes mellitus. N Engl J Med. 2010;362:1575–1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.SPS3 Study Group, Benavente OR, Coffey CS, et al. Blood-pressure targets in patients with recent lacunar stroke: the SPS3 randomized trial. Lancet. 2013;382:507–515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lonn EM, Bosch J, López-Jaramillo P, et al. Blood-pressure lowering in intermediate-risk persons without cardiovascular disease. N Engl J Med. 2016;374:2009–20 [DOI] [PubMed] [Google Scholar]
- 6.Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: Executive summary: A report of the american college of cardiology/american heart association task force on clinical practice guidelines. J Am Coll Cardiol. 2018. May 15;71(19):2199–2269.29146533 [Google Scholar]
- 7.Pokharel Y, Sun W, de Lemos JA, et al. High-sensitivity troponin T and cardiovascular events in systolic blood pressure categories: Atherosclerosis risk in communities study. Hypertension. 2015;65:78–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.McEvoy JW, Chen Y, Rawlings A, et al. Diastolic Blood Pressure, Subclinical Myocardial Damage, and Cardiac Events: Implications for Blood Pressure Control. J Am Coll Cardiol. 2016;68:1713–1722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nambi V, Liu X, Chambless LE, et al. Troponin T and N-terminal pro-B-type natriuretic peptide: A biomarker approach to predict heart failure risk--the atherosclerosis risk in communities study. Clin Chem. 2013;59:1802–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pandey A, Patel KV, Vongpatanasin W, et al. Incorporation of biomarkers into risk assessment for allocation of antihypertensive medication according to the 2017 ACC/AHA high blood pressure guideline: A pooled cohort analysis. Circulation. 2019;140:2076–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.The ARIC Investigators, The Atherosclerosis Risk in Communities (ARIC) study: design and objectives Am J Epidemiol. 1989;129:687–702. [PubMed] [Google Scholar]
- 12.Apple FS, Panteghini M, Ravkilde J, et al. Quality specifications for B-type natriuretic peptide assays. Clin Chem. 2005;51:486–93. [DOI] [PubMed] [Google Scholar]
- 13.Januzzi JL, van Kimmenade R, Lainchbury J, et al. NT-proBNP testing for diagnosis and short-term prognosis in acute destabilized heart failure: An international pooled analysis of 1256 patients: The international collaborative of NT-proBNP study. Eur Heart J. 2006;27:330–7. [DOI] [PubMed] [Google Scholar]
- 14.White AD, Folsom AR, Chambless LE, et al. Community surveillance of coronary heart disease in the atherosclerosis risk in communities (ARIC) study: Methods and initial two years’ experience. J Clin Epidemiol. 1996;49:223–33. [DOI] [PubMed] [Google Scholar]
- 15.Rosamond WD, Folsom AR, Chambless LE, et al. Stroke incidence and survival among middle-aged adults: 9-year follow-up of the atherosclerosis risk in communities (ARIC) cohort. Stroke. 1999;30:736–43. [DOI] [PubMed] [Google Scholar]
- 16.Rosamond WD, Chang PP, Baggett C, et al. Classification of heart failure in the atherosclerosis risk in communities (ARIC) study: A comparison of diagnostic criteria. Circ Heart Fail. 2012;5:152–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ndumele CE, Matsushita K, Sang Y, et al. N-terminal pro-brain natriuretic peptide and heart failure risk among individuals with and without obesity: The atherosclerosis risk in communities (ARIC) study. Circulation. 2016;133:631–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Law MR, Morris JK, Wald NJ. Use of blood pressure lowering drugs in the prevention of cardiovascular disease: meta-analysis of 147 randomised trials in the context of expectations from prospective epidemiological studies. BMJ. 2009; 338: b1665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Blood Pressure Lowering Treatment Trialists’ Collaboration. Blood pressure-lowering treatment based on cardiovascular risk: A meta-analysis of individual patient data. Lancet. 2014;384:591–8. [DOI] [PubMed] [Google Scholar]
- 20.Phillips RA, Xu J, Peterson LE, et al. Impact of cardiovascular risk on the relative benefit and harm of intensive treatment of hypertension. J Am Coll Cardiol 2018; 71:1601–1610. [DOI] [PubMed] [Google Scholar]
- 21.DeFilippis AP, Young R, Carrubba CJ, et al. An analysis of calibration and discrimination among multiple cardiovascular risk scores in a modern multiethnic cohort. Ann Intern Med. 2015;162:266–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Doust JA, Pietrzak E, Dobson A, Glasziou P. How well does B-type natriuretic peptide predict death and cardiac events in patients with heart failure: Systematic review. BMJ. 2005;330:625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Magnusson M, Melander O, Israelsson B, Grubb A, Groop L, Jovinge S. Elevated plasma levels of NT-proBNP in patients with type 2 diabetes without overt cardiovascular disease. Diabetes Care. 2004;27:1929–35. [DOI] [PubMed] [Google Scholar]
- 24.Pedersen F, Raymond I, Kistorp C, Sandgaard N, Jacobsen P, Hildebrandt P. N-terminal pro-brain natriuretic peptide in arterial hypertension: A valuable prognostic marker of cardiovascular events. J Card Fail. 2005;11:70. [DOI] [PubMed] [Google Scholar]
- 25.Paget V, Legedz L, Gaudebout N, et al. N-terminal pro-brain natriuretic peptide: A powerful predictor of mortality in hypertension. Hypertension. 2011;57:702–9. [DOI] [PubMed] [Google Scholar]
- 26.Huelsmann M, Neuhold S, Resl M, et al. PONTIAC (NT-proBNP selected prevention of cardiac events in a population of diabetic patients without a history of cardiac disease): A prospective randomized controlled trial. J Am Coll Cardiol. 2013;62:1365–72. [DOI] [PubMed] [Google Scholar]
- 27.Ledwidge M, Gallagher J, Conlon C, et al. Natriuretic peptide-based screening and collaborative care for heart failure: the STOP-HF randomized trial. JAMA. 2013;310(1):66–74. [DOI] [PubMed] [Google Scholar]
- 28.Levin ER, Gardner DG, Samson WK. Natriuretic peptides. N Engl J Med. 1998;339:321–8. [DOI] [PubMed] [Google Scholar]
- 29.Folsom AR, Nambi V, Bell EJ, et al. Troponin T, N-terminal pro-B-type natriuretic peptide, and incidence of stroke: The atherosclerosis risk in communities study. Stroke. 2013;44:961–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


