Abstract
This study examined the frequent clinical observation that toddlers with less expressive language have more severe temper tantrums. A representative sample of 2,001 mothers reported on their toddler’s expressive vocabulary and frequency of different temper tantrum behaviors, a prominent feature of irritability and an emergent marker of mental health risk. Results revealed that 12- to 38-month-olds with fewer spoken words demonstrated more severe (frequent and dysregulated) temper tantrums. Toddlers who were late talkers at 24–30 months also had more severe tantrums; their relative risk of having severe tantrums was 1.96 times greater than peers with typical language. These results are the first to show that language and temper tantrums are related, and that this relation is present in the second year of life. These findings point to the importance of assessing both language and mental health risk in order to promote earlier identification and intervention for early childhood disorders.
Keywords: temper tantrums, irritability, mental health, expressive language, language delay, early childhood
Temper tantrums are exceedingly common in early childhood (Wakschlag et al., 2012). Temper tantrums are expected and developmentally appropriate for many children; however, frequent and dysregulated tantrums not only disrupt daily life, but also are signs of clinically-concerning irritability, an indicator of transdiagnostic mental health risk in early childhood (Belden, Thomson, & Luby, 2008; Carlson, Danzig, Dougherty, Bufferd, & Klein, 2016; Wakschlag, et al., 2015, 2019). A common clinical observation is that toddlers with lower expressive language abilities have more tantrums (Daniels, Mandleco, & Luthy, 2012; Harrington, 2004; Mayo Clinic, 2015; Swanson, 2014). Although in older children there is a well-established association between language impairment and broad-band internalizing/externalizing mental health problems (Benasich, Curtiss, & Tallal, 1993; Benner, Nelson, & Epstein, 2002; Conti-Ramsden & Botting, 2008; Love & Thompson, 1988; Nicolson, et al., 2000; Toppelberg & Shapiro, 2000; Willinger et al., 2003), very little work has examined toddlerhood, and no study has specifically investigated associations between expressive language and temper tantrums. Explicating this association with developmentally-sensitive measures is important during this period in which there is substantial developmental variation and it is difficult to differentiate normative variation from cause for concern. Here, we investigated the relation between expressive language ability and temper tantrums using data from a large sample of mothers reporting about their toddlers’ behavior.
Typical and Atypical Patterns of Temper Tantrums and Language Development in Early Childhood
Temper tantrums, defined as behavioral outbursts reflecting dysregulated response to frustration, are exceedingly common in young children, present in up to 83% of toddlers in community samples (Potegal & Davidson, 2003; Wakschlag et al., 2012; Wakschlag et al., 2018). Some instances of temper tantrums are developmentally typical and appropriate (Wakschlag et al., 2007); such tantrums occur at expected times (e.g., when the child is tired or hungry), are relatively brief, and can be soothed or redirected (Wakschlag et al., 2012). However, severe tantrums, i.e., those that are frequent and dysregulated, are indicators of irritability, which is a risk factor for a variety of mental health problems, including internalizing (e.g., depression and anxiety) and externalizing (e.g., ADHD and disruptive behavior) disorders (Belden et al., 2008; Carlson et al., 2016; Wakschlag, et al., 2019; Wiggins et al., 2018). The identification of a transdiagnostic mental health risk in very young children is of high importance for elucidating the relation of language delays and mental health problems because it can be measured much earlier than frank mental health problems. Patterns of temper tantrums can be viewed along a continuum, from occasional normative tantrums that are responsive to redirection and occur in expectable contexts, to severe tantrums that are frequent, prolonged, intense, and/or seem to arise “out of the blue.” Severe tantrums not only indicate risk for later mental health problems, but are also impairing; they increase family stress and interfere with social and academic functioning (Campbell, Pierce, Moore, Marakovitz, & Newby, 1996; Wiggins et al., 2018).
Like temper tantrums, language development falls along a continuum from typical to concerning. Most toddlers achieve first spoken words by 12 months and acquire 50 spoken words and two-word utterances around 18 months (Tamis-LeMonda, Bornstein, & Baumwell, 2001). If a child is delayed in achieving these expressive vocabulary and word combination milestones, he or she is considered to have a language delay, often called “late talking” in toddlerhood. Late talking is common, with prevalence estimates ranging from approximately 10% to 15% of toddlers (Horwitz et al., 2003; Paul, 1996; Rescorla & Alley, 2001; Zubrick, Taylor, Rice, & Slegers, 2007). Among children who are late talkers at 24 months, 40% qualify for a diagnosis of language disorder or impairment at school age (Dale, Price, Bishop, & Plomin, 2003). For the other 60% of cases, children catch up, and their delayed language skills simply represent the low end of variation in the population (Dale et al., 2003). Importantly, although a diagnosis of developmental language disorder cannot be made in toddlerhood because many late talking children spontaneously remit and achieve typical language, late talking is a risk factor for developing a later language disorder (Dale et al., 2003; Reilly et al., 2010; Rescorla, 2011). In the case of both language and mental health, wide developmental variation makes it difficult to know which patterns are truly concerning or presaging later impairment.
Co-occurrence of Language Impairments and Mental Health Problems
A large body of literature has linked language impairments and mental health problems in school-age children at an age in which these disorders can be reliably identified. Similar patterns of co-occurrence have emerged both from studies that have focused on children with mental health problems and from studies of children with language impairments. First, among studies of children with mental health problems, frequent co-occurrence of expressive and receptive language impairments has been noted (Benner et al., 2002; Cohen et al., 1998; Javorsky, 1995; Love & Thompson, 1988; Nicolson, et al., 2000). Among these studies, the prevalence of language impairments among children with mental health problems ranges from 33% to 71%. A recent meta-analysis reports a significant, albeit small, negative correlation (effect size z = −.17, 95% CI = [−0.21, −0.13]) between externalizing mental health problems and language ability (Chow & Wehby, 2018).
Second, among studies of children with expressive/receptive language impairments, mental health problems are often present (Benasich et al., 1993; Cantwell & Baker, 1987; Conti-Ramsden & Botting, 2008; Redmond & Rice, 1998; Toppelberg & Shapiro, 2000; Willinger et al., 2003). School-age children with language impairments score higher on scales of internalizing and externalizing mental health problems (Benasich et al., 1993; Cantwell & Baker, 1987; Chow & Wehby, 2017; Conti-Ramsden & Botting, 2008; Redmond & Rice, 1998; Tervo, 2007; Van Daal, Verhoeven, & Van Balkom, 2007; Willinger et al., 2003). Specifically, children with language impairments tend to show more aggressive behavior (Chow & Wehby, 2017; Van Daal et al., 2007), problem behavior (Benasich et al., 1993; Cantwell & Baker, 1987), socio-emotional problems (Tervo, 2007; Willinger et al., 2003), and anxiety and depression (Conti-Ramsden & Botting, 2008; Willinger et al., 2003). These mental health problems appear to persist into or even worsen in later childhood (Benner et al., 2002). In one longitudinal study, 11% of children who had language impairments at 4 years showed mental health problems. Indeed, in that study, the number of children with co-occurring language impairments and mental health problems nearly tripled from age 4 to age 8 (Benasich et al., 1993). It is likely that the observed co-occurrence of language impairments and mental health problems is due to a variety of factors, including overlapping developmental processes (Tervo, 2007), causal influences (Redmond & Rice, 1998), and mediating factors (Horwitz et al., 2003; Mayes, Lockridge, & Tierney, 2017; Tomblin, Zhang, Buckwalter, & Catts, 2000; Vitiello & Williford, 2016; Zadeh, Im-Bolter, & Cohen, 2007).
The Relation Between Language Ability and Mental Health Indicators in Early Childhood
The link seen in older children between both expressive and receptive language abilities and various mental health indicators is also present in early childhood (Carson, Klee, Perry, Muskina, & Donaghy, 1998; Caulfield, Fischel, DeBarysche, & Whitehurst, 1989; Irwin, Carter, & Briggs-Gowan, 2002; Paul & James, 1990; Roben, Cole, & Armstrong, 2013; Tervo, 2007; Thurm, Farmer, Manwaring, & Swineford, 2017; Whitehouse, Robinson, & Zubrick, 2011). Young children with lower language ability are more likely to show internalizing mental health indicators such as anxiety, depression, and withdrawal and externalizing problems such as aggression and non-compliance (Carson et al., 1998; Caulfield et al., 1989; Horwitz et al., 2003; Irwin et al., 2002; Whitehouse et al., 2011). Our group has previously shown that in toddlers as young as 18 months, weaker overall (receptive and expressive) language skills are associated with greater disruptive behavior (Roberts et al., 2018). Evidence from a meta-analysis of interventions also suggests that improving language skills in young children with language delay leads to concomitant improvements in externalizing behaviors (Curtis, Kaiser, Estabrook, & Roberts, 2019).
Although a consistent overall relation between early language skills and problem behaviors has emerged, patterns are inconsistent particularly in relation to externalizing problems. For example, externalizing problems are related to language skills in some studies (Caulfield et al., 1989) but not in others (Carson et al., 1998). Further, language and mental health measures have varied widely among studies, which makes direct comparisons difficult (Carson et al., 1998; Irwin et al., 2002; Maggio et al., 2014; Paul & James, 1990; Tervo, 2007; Thurm et al., 2017). In addition, most of these studies have focused on children older than 24 months, and many have used small samples that are not representative. Assessing a large sample of children using sensitive markers of language and mental health could help to clarify these differences among studies and provide information on how early these associations can be detected.
The Relation Between Early Expressive Language Abilities and Temper Tantrums
It is a common clinical observation, stated on web pages for the American Academy of Pediatrics, Mayo Clinic, and others, that children with fewer words or lower expressive language ability have more temper tantrums (Daniels et al., 2012; Harrington, 2004; Mayo Clinic, 2015; Swanson, 2014). This observation is supported by the fact that temper tantrums peak around 2 years (Potegal & Davidson, 2003), an age when typically-developing toddlers are gaining greater independence. At the same time, toddlers are also rapidly acquiring new words, but they are only just beginning to combine these words into utterances in order communicate more complex thoughts and ideas (Tamis-LeMonda et al., 2001). As language and other skills such as social-emotional functioning and self-regulation increase (Röll, Koglin, & Petermann, 2012), children also show decreased frequency of temper tantrums (Potegal & Davidson, 2003).
Despite clinical impressions and understanding of broader developmental patterns, very few studies have directly examined how expressive language ability relates to temper tantrums. In studies which have measured early expressive language ability, a relation has been found with broader mental health indicators such as physical aggression (Dionne, Tremblay, Boivin, Laplante, & Perusse, 2003), social-emotional problems (Irwin et al., 2002; Tervo, 2007), depression/withdrawal (Irwin et al., 2002), decreased compliance (Irwin et al., 2002), and negative behavior (Caulfield et al., 1989). Expressive language ability appears related to early mental health behaviors even in children with typical receptive language and intellectual abilities (Caulfield et al., 1989; Irwin et al., 2002). Most of these studies, however, have not considered temper tantrums specifically, nor examined them in very young toddlers.
In two studies which did measure temper tantrums, an association between language (both expressive and receptive-expressive) and temper tantrums was found (Caulfield et al., 1989; Mattison, Cantwell, & Baker, 1980); however, because temper tantrums were not a central focus of these studies, they were not used as primary outcome measures. Instead, temper tantrums were only considered as part of a composite of broader behaviors (e.g., negative behavior) or as a single item on a developmental scale, which precludes direct clinical interpretation and does not consider the importance of both severity and frequency of tantrums.
Gaining a clearer picture of the relations between expressive language and temper tantrums is important for elucidating modifiable markers of risk that may increase the likelihood that delays in one area may lead to impairing problems subsequently, which may have important implications for accurate identification of atypicality in language and mental health. A recent consensus statement on language disorders recommends that clinicians consider children’s mental health problems in screening for language impairments (Bishop, Snowling, Thompson, Greenhalgh, & CATALISE consortium, 2016). A central premise of the current study is that temper tantrums, as easily-reportable, highly-salient, and early-emerging indicators of childhood irritability, which is a marker for broader mental health risk, are especially useful in this context. Parent report of temper tantrums is easily included in developmental screening and does not require extensive clinical assessment (Wakschlag, et al., 2019).
Current Study
The current study was designed to complement and extend our previous work in this sample, which demonstrated a relation between broad-band externalizing behaviors and receptive and expressive language skills starting in 18-month-olds (Roberts et al., 2018). Here, we focus on temper tantrums and expressive vocabulary specifically because medical providers and parents so frequently note severe temper tantrums in children with low expressive language ability (Daniels et al., 2012; Harrington, 2004; Mayo Clinic, 2015; Swanson, 2014), despite the lack of direct evidence for this association in the literature. We also examine this relation in younger children than have been examined previously, beginning at 12 months. Finally, we extend our approach to use clinically-translatable metrics by examining a dichotomized indicator of severe temper tantrums, to generate individual relative risk of tantrum severity based on language delay.
We examined the relation between expressive language ability and temper tantrums in a large, nationally-representative sample of toddlers using maternal report methods. First, we empirically tested the common clinical observation that toddlers with fewer spoken words have more frequent and dysregulated temper tantrums. We predicted that there would be a relation between parent-reported expressive vocabulary size and temper tantrums, such that toddlers with a lower expressive vocabulary size would demonstrate more frequent and dysregulated temper tantrums. Because of the rapid developmental change in this age range, we also examined whether this relation varies with age. We predicted that this relation would be present in this sample of 12–38-month-olds and the strength of this relation would increase with age. Next, we considered this association from a clinical risk standpoint, in order to determine whether late talking children (i.e., children with language delay after 24 months, who are thus at risk for language impairment) were more likely to have frequent and dysregulated temper tantrums, an emergent indicator of mental health risk. We predicted that late-talking children would have more frequent and severe tantrums.
Method
Procedure and Participants
Participants were drawn from a cross-sectional survey, which was part of a larger study focused on early identification of mental health risk (The When to Worry Study at Northwestern University, http://w2w.northwestern.edu). Although mental health risk was the main objective of the larger study, participants were also asked questions about related developmental domains, including language. The online panel survey sample included 2,001 mothers who had a toddler age 12 to 38 months; a larger proportion of 12-month-olds was included, in line with the objectives of the larger study. Mothers who reported at screening that their child had a diagnosis of developmental disability (e.g., autism spectrum disorder) were not included in the study.
The survey was conducted by Opinions 4 Good (Op4G), a company that uses a proprietary opt-in panel of over 200,000 US residents (approximately 31,000 of which have children) recruited primarily from non-profit organizations and web campaigns. Op4G selected mothers of toddlers in the study’s age band from its database and invited them to participate. All procedures were approved by the university’s Institutional Review Board and respondents provided informed consent online. Mothers were informed they would be participating in a research study investigating developmental patterns of behavior in toddlers and were asked questions about demographics, family composition, child behavior and functioning, and language. Participants received $9.00 compensation for completing the survey.
For our first analysis, data were analyzed from all surveys of the toddlers ages 12–38 months (n = 2,001). After excluding surveys with data that were outliers (as described in the section below), our final analytic sample contained 1,973 toddlers. For our second analysis, we focused only on toddlers ages 24–30 months (n = 435) in order to group children into late talker and not late talker groups. We focused on children 24–30 months because this is the typical age range in which children are identified as late talking; criteria for late talking was parent-reported expressive vocabulary of <50 spoken words and not yet producing 2-word utterances (American Speech-Language-Hearing Association).
Demographic characteristics of the full sample and late talker comparison subgroups are given in Table 1. The sample included approximately equal numbers of girls and boys, and participants were distributed across racial/ethnic groups roughly similarly to the U.S. population, per U.S. Census Bureau (2015) data. According to mothers’ reports, 24% of the sample had a family income that met federal poverty guidelines based on their household size (U.S. Department of Health & Human Services, 2017).
Table 1.
Demographic Characteristics of Toddlers in the Full Study Sample and Language Subgroups
| Demographic characteristics | Full sample | Subsample, age 24–30 months | |
|---|---|---|---|
| Late talkers | Not late talkers | ||
| Number of participants | 1,973 | 41 | 394 |
| Age in months (mean ± SD) | 23.1 ± 8.4 | 26.0 ± 1.9 | 27.0 ± 2.0 |
| Sex (% female) | 48.3% | 31.7%a | 47.2% |
| Family meets federal poverty criteria | 24.4% | 29.3%b | 24.1% |
| Race | |||
| Asian | 7.5% | 7.3% | 7.9% |
| Black/African American | 15.2% | 17.1% | 14.7% |
| Hispanic | 15.2% | 19.5% | 10.9% |
| Native American/Alaskan Native | 1.3% | 2.4% | 0.5% |
| Native Hawaiian/Pacific Islander | 0.9% | 0.0% | 0.8% |
| White/Caucasian | 56.9% | 53.7% | 61.2% |
| Other | 3.0% | 0.0% | 4.1% |
| Ethnicity | |||
| Hispanic/Latino | 20.3% | 26.8% | 15.5% |
| Not Hispanic/Latino | 79.7% | 73.2% | 84.5% |
Notes. Late talkers were defined as 24–30-months-olds with fewer than 50 words and no two-word utterances.
There was a marginally significant effect of more males in late talker group, χ2 = 3.60, Fisher’s exact test p = .07.
There was no significant difference between late talker vs. not late talker groups in terms of whether their family met poverty criteria, χ2 = 0.53, Fisher’s exact test p = .45.
Measures
Expressive language measurement.
Parent report is widely used to evaluate language development and late talking status (Rescorla & Alley, 2001). Information on toddlers’ expressive language ability was derived from two survey questions: (A) How many different words does your child say? with the answer choices, 0 = no words, 1 = 1–2 words, 2 = 3–10 words, 3 = 11–50 words, 4 = between 51 and 200 words, 5 = between 200 and 500 words, and 6 = more than 500 words and (B) Is your child combining words (for example, ‘more juice’, ‘want banana’)? with response options, 0 = no and 1 = yes.
Because the focus of the larger panel study was on early mental health risk rather than language skills, we were unable to include a more time-intensive, norm-referenced measure of expressive vocabulary, which often requires parents to complete a checklist of at least 100 words (Fenson, Marchman, Thal, Dale, & Reznick, 2007). Instead, our expressive language survey questions were developed to be brief, akin to screening questions a parent may be asked at their pediatrician’s office, and informative of major language milestones such as producing first words, using 50 spoken words, and combining words. We chose to capture vocabulary size (e.g., 1–2 words or 51–200 words) rather than asking parents for an exact number of words a child knows, to reference to these common milestones and increase likelihood of accurate parent report. Similar measures asking parents about their child’s vocabulary size via word bands or anchors have been used in questionnaires and screening measures that have demonstrated good reliability and validity (Allison et al., 2008; Bricker & Squires, 1999; Stott, Merricks, Bolton, & Goodyer, 2002). Our question about whether the child is combining words is similar to questions that have been shown to be valid and reliable in norm-referenced, parent-report assessments like the MacArthur-Bates Communicative Development Inventories (CDI): Words and Sentences form (Fenson et al., 2007). Parent report is a common and validated method for ascertaining late talking status (Rescorla & Alley, 2001).
Before analysis, we examined the data and excluded outliers on these language questions. We excluded extreme outliers with reported vocabulary sizes at least 5 times the vocabulary size of a child in the 90th percentile based on published norms from the CDI (Fenson et al., 2007). These included children who were 12- and 13-month-olds with 200 or more words or 14-month-olds with more than 500 words (n = 21). In addition, we excluded children who were reported to have no spoken words but to be combining words (n = 7). Together, these outliers represented less than 1.4% of the original sample.
Expressive language measurement.
For our first analysis, we investigated whether toddlers with lower parent-reported vocabulary size experienced more frequent and dysregulated temper tantrums on a continuous measure of tantrum severity. To measure expressive vocabulary size, we used the survey question: How many different words does your child say? Parent responses were analyzed using the ordinal scale from 0 to 6 (as corresponding to the ranges of words listed above, e.g., 1 = 1–2 words). For our second set of analyses, we were interested in evaluating emergent indicators of language and mental health risk. We categorized 24- to 30-month-old toddlers into late talker and not late talker groups based on their expressive language ability using both language survey questions: How many different words does your child say? and Is your child combining words (for example, ‘more juice’, ‘want banana’)? Groups were defined based on widely-used criteria for late talking: having fewer than 50 words and no two-word utterances by 24 months (American Speech-Language-Hearing Association; Paul, 1991). Among the 24- to 30-month-olds, 9.4% of toddlers met criteria for late talking, which is very similar to broader estimates of the prevalence of late talking (Horwitz et al., 2003; Zubrick et al., 2007). Distributions for the two language measures for all children included in the analyses are reported in Table 2.
Table 2.
Distribution of Language and Tantrum Measures in the Full Sample and Language Subgroups
| Full sample (n =1,973) | Toddlers age 24–30 months | ||
|---|---|---|---|
| Late talkers (n = 41) | Not late talkers (n = 394) | ||
| Expressive vocabulary size | |||
| No words | 67 | 0 | 0 |
| 1–2 words | 126 | 3 | 6 |
| 3–10 words | 436 | 13 | 34 |
| 11–50 words | 566 | 25 | 131 |
| Between 51 & 200 words | 439 | 0 | 119 |
| Between 200 & 500 words | 223 | 0 | 74 |
| More than 500 words | 116 | 0 | 30 |
| Word combinations | |||
| Yes | 1476 | 0 | 379 |
| No | 497 | 41 | 15 |
| Temper tantrum score (mean ± SD) | .04 ± 1.0 | .51 ± .90 | .02 ± .94 |
Note. Late talkers were defined as 24–30-months-olds with fewer than 50 words and no two-word utterances.
Temper tantrum measurement.
Temper tantrums were assessed as part of the panel survey using the Multidimensional Assessment of Profile of Disruptive Behavior, Infant-Toddler version (MAP-DB-IT; Wakschlag et al., 2018). The MAP-DB-IT includes a multidimensional scale of irritable behaviors and emotions (“Temper Loss”), which includes 21 questions that form a temper tantrum sub-scale. The MAP-DB was specifically designed to capture the typical to atypical spectrum of behavior with the goal of defining atypicality as deviation from normative patterns (Wakschlag et al., 2014). Parents were asked to rate the frequency of a variety of tantrum behaviors in different contexts; some behaviors are mild and normative (e.g., has tantrums when tired) whereas others are extreme and atypical (e.g., has temper tantrums until exhausted). The mothers indicated how often over the past month each behavior occurred for her child using the following scale: 0 = never, 1 = rarely (less than once per week), 2 = some days of the week (1–3 days), 3 = most days of the week (4–6 days), 4 = every day of the week, 5 = and many times each day. The MAP-DB has been extensively validated at preschool age (Wakschlag et al., 2012, 2014, 2015, 2018). Survey measures of socio-emotional problems via parent report have been shown to be reliable in infancy and early toddlerhood (Carter, Briggs-Gowan, Jones, & Little, 2003).
We used item response theory (IRT) to generate a dimensional scale of tantrum severity from the MAP-DB-IT tantrum items. In contrast to a simple sum of item scores, IRT has the advantage of scaling items based on severity in order to generate a normal-to-abnormal spectrum of behavior (Wakschlag et al., 2012). This approach takes frequency and qualitative intensity, into account, generating a score that indicates overall severity of tantrums. MAP-DB Temper Loss scores derived from IRT have been shown to predict mental health risk over time (Wakschlag, et al., 2015; Wiggins et al., 2018). The temper tantrum IRT score was computed using a graded response model (Samejima, 1997) fit to the 21 tantrum items. IRT scores are standardized, with a mean of 0 and a standard deviation of 1, similar to a z-score (an IRT scoreof 0 is equivalent to the sample mean, score of 1 = higher than 85% of the population, score of −2 = lower than 97.7%). From the graded response IRT models, coverage of tantrums was adequate, with item threshold parameter estimates ranging from −1.86 to 2.65 in the full sample and from −2.05 to 3.59 among the 24- to 30-month-old subsample. Item severity, as assessed by the average of the five thresholds for each item (ranging from never in past month to many times per day), ranged from 0.48 to 1.41 in the whole sample and from .38 to 1.78 among the 24- to 30-month-old subsample. Fit, as assessed by RMSEA, was good, with values of .03 for the full sample and values of .05 for 24- to 30-month-olds. Scores >95th percentile are considered above the severity threshold in IRT models, as validated in previous studies of preschool children (Wakshlag et al., 2014). From these models, a score of 1.43 fell at the 95th percentile for the full sample (−2.51 minimum, 2.77 maximum) and a score of 1.52 fell at the 95th percentile among 24–30-month-olds (−2.71 minimum, 2.21 maximum). Distributions for the MAP-DB IRT temper tantrum subscale scores are reported in Table 2. To aid in clinical interpretation, analyses with mean scores across tantrum items were also calculated so that their values could be mapped back on to the discrete frequency-based answer choices (see Supplemental Materials). IRT scores and mean scores were very strongly correlated (r = 0.98).
Finally, to generate a dichotomous categorization of severe tantrums, we created a severe tantrum variable based on IRT tantrum scores falling >1 standard deviation above the mean (coded as 0 = normative tantrums; 1 = severe tantrums). Of the 24- to 30-month-olds in the subsample, 16.3% (n = 71) were classified as having severe tantrums. This percentage is consistent with other estimates of severe tantrums and non-compliant behaviors in young toddlers (Carbonneau, Boivin, Brendgen, Nagin, & Tremblay, 2016).
Covariates and Analysis Plan
To address our first research question, we conducted a hierarchical linear regression to assess whether tantrum severity was related to parent-reported expressive vocabulary size, and whether this differed by age. Variables were centered before analysis. Child sex and family poverty status were also included in the model because of their documented association with temper tantrums (Wakschlag et al., 2012; Roberts et al., 2018) and language ability (Hoff, 2013).
Second, we conducted an analysis of covariance (ANCOVA) to examine whether late-talking toddlers, i.e., toddlers at risk for language disorder, had more frequent and dysregulated tantrums compared with typically-talking toddlers. We focused only on the subsample of 24- to 30-month-old toddlers in order to group children according to late-talking status. Child age, sex, and family poverty status were used as covariates. We also calculated relative risk statistics using the dichotomous severe tantrum indicator to determine whether being a late talker increased the likelihood of a child having severe tantrums.
Results
Relation Between Expressive Language Size and Temper Tantrums
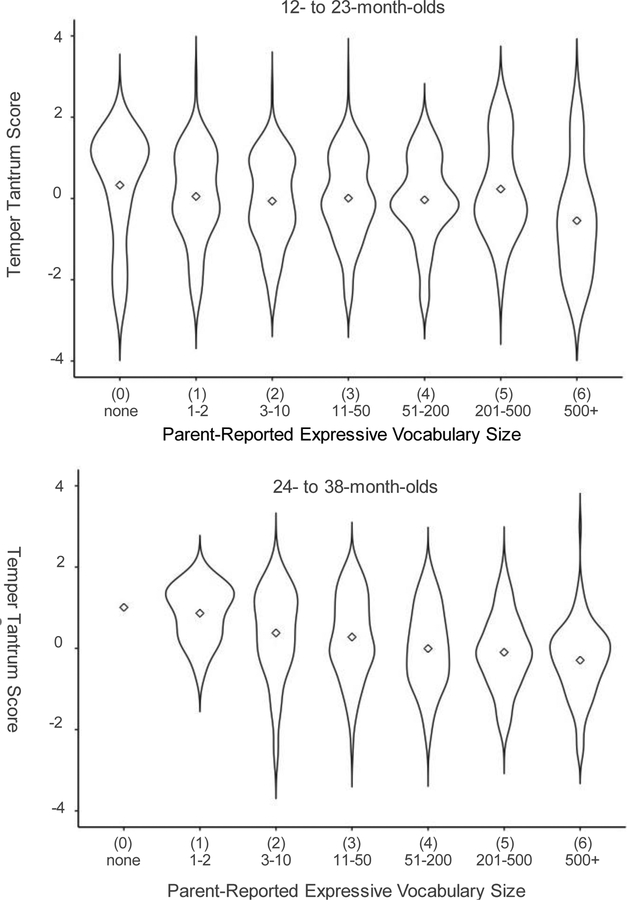
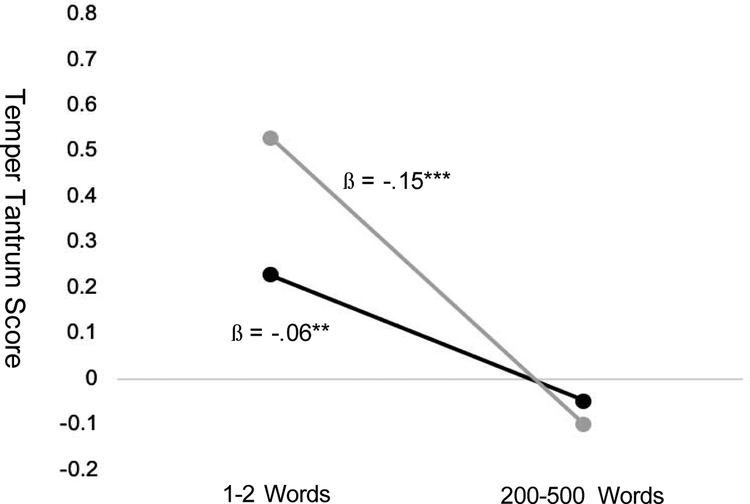
Figure 1 illustrates mean temper tantrum scores for toddlers in each expressive vocabulary size category, for 12- to 23-month-olds and 24- to 38-month-olds. A hierarchical linear regression was performed with the temper tantrum score as the dependent variable (see Table 3). In the first step, the independent variables of sex and poverty together explained significant variance in temper tantrum scores (R 2 = .027, p < .001). The regression coefficients indicated that children living in poverty had higher average tantrum severity scores than those not in poverty and that females had higher average tantrum severity scores than males (both p < .001). In the second step, age was added, but it was not significant (p > .05). In the third step, parent-reported expressive vocabulary size was added, which explained significant additional variance in temper tantrum scores (ΔR 2 = .013, p < .001). As predicted, lower reported expressive vocabulary was associated with higher tantrum scores. In the final step, the age*expressive vocabulary size interaction term was added, and it was also significant in explaining variance in tantrum scores (ΔR2 = .007, p < .001); toddlers with smaller vocabularies showed higher tantrum scores at older ages than at younger ages. To further investigate the interaction between age and expressive vocabulary size, we conducted a simple slopes analysis to test the relation between expressive vocabulary size and temper tantrum scores at prototypical “low” and “high” values of age; we chose to examine 18 months and 30 months as representative younger and older toddler ages in our sample. Values are evaluated at 0.5 for poverty and gender to control for these variables. Figure 2 illustrates the model-estimated temper tantrum score values for these younger and older toddlers. The simple slopes analysis revealed a significant non-zero slope, that is, a significant relation between vocabulary size and temper tantrum score at both the example ages of 18 months (ß = −.06, t = −2.59, p < .01) and 30 months (ß = −.15, t = −6.48, p < .001).
Figure 1.
Temper tantrum score means and distributions by parent-reported expressive vocabulary for (a) toddlers age 12–23 months and (b) toddlers age 24–38 months. Higher scores indicate more severe/frequent tantrums. These “violin” plots show width of the distribution as density of observations at that point, and a diamond indicates the mean. Note: One child in the 24–38-month-old group had 0 words; the diamond indicates that value.
Table 3.
Hierarchical Linear Regression with Temper Tantrum Score as Outcome (full sample)
| Steps and Variables | R2 | ΔR2 | ΔF (df1, df2) | Final B | SE B | Final β |
|---|---|---|---|---|---|---|
| Step 1 | .027 | 27.68 (2, 1970)*** | ||||
| Poverty | .293 | .054 | .120*** | |||
| Sex | .172 | .046 | .082*** | |||
| Step 2 | .027 | .001 | 1.53 (1, 1969) | |||
| Age | .013 | .003 | .104 | |||
| Step 3 | .040 | .013 | 26.32 (1, 1968)*** | |||
| Vocab. Size | −.099 | .020 | −.133*** | |||
| Step 4 | .047 | .007 | 13.69 (1, 1967)*** | |||
| Age*Vocab. Size | −.008 | .002 | −.082*** |
Notes. Betas are reported for the final model step. Poverty coding: 0 = not poverty, 1 = poverty; Sex coding: 0 = male, 1 = female.
p < .001.
Figure 2.
Plot displaying temper tantrum scores derived from the regression model for example ages of 18 and 30 months at vocabulary levels of 1–2 words and 200–500 words. The interaction observed in the regression indicates that the slope increases with age. Simple slopes analysis here revealed that both slopes are significantly different than zero, meaning that the association is present at both of these ages. Note: **p < .01, ***p < .001.
Relation Between Late Talking and Temper Tantrums
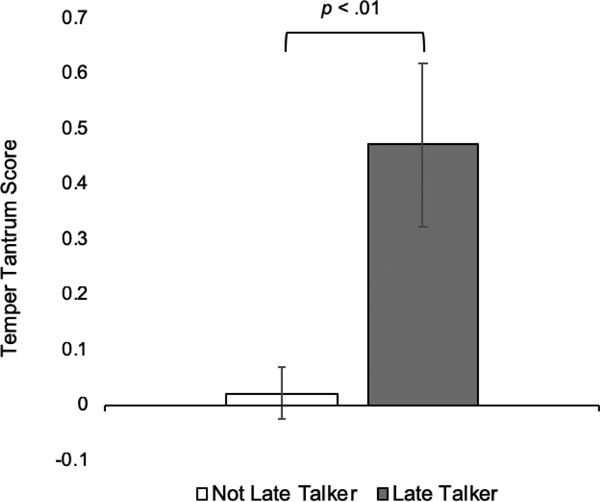
An ANCOVA was conducted to examine whether temper tantrum scores differed basedon late-talker status (coded as 0 = not late talker vs. 1 = late talker) in toddlers age 24–30-months. Covariates of poverty status, (coded 0 = not poverty, 1 = poverty), sex (coded 0 = male, 1 = female), and age (in months) were also included in the model. The data met assumptions for normality and homogeneity of variance; type-III sums of squares were used because they are robust to uneven group sizes (Lewsey, Gardiner, & Gettinby, 1997). The overall model was significant (F (4, 430) = 5.31, p < .001), with a significant main effect of late talking, such that late talkers had significantly higher tantrum scores than toddlers who were not late talkers (p = .004, partial η2 = .019, see Figure 3). The effect of poverty status was also significant (p = .008, partial η2 = .016, poverty associated with higher scores) but age (p = .118, partial η2 = .006) and sex (p = .396, partial η2 = .002) were not. Relative risk analyses revealed that late talkers were nearly twice as likely to have severe tantrums than peers who were not late talkers, a statistically significantly greater risk (relative risk = 1.96, 95% CI = [1.15–3.32], χ2 = 5.55, p = .018). Corresponding tantrum scores using the original item scale yielded similar results and are presented in Supplemental Figure 1.
Figure 3.
Temper tantrum scores (adjusted for covariates of sex and poverty status) for not late-talker and late-talker groups (24- to 30-month-olds). Error bars represent 1 SE.
Discussion
In this study, we explored the association between parent-reported expressive language ability and temper tantrums in a large community sample. To our knowledge, this is the first study to specifically examine the association between expressive language ability and temper tantrums, despite the frequently noted clinical observation. There was a significant relation between expressive vocabulary size and temper tantrum severity (indicated by frequent and dysregulated tantrum behaviors) in the sample of toddlers 12 to 38 months old, even when controlling for child age and sex, and family poverty status. These results are consistent with previous studies in older children which have shown that lower expressive language ability is associated with internalizing and externalizing problems (Carson et al., 1998; Irwin et al., 2002; Whitehouse et al., 2011). This work also expands our group’s previous work in the same sample, which showed an association between broader language ability and irritability in toddlers 18–36 months (Roberts et al., 2018).
The inclusion of a large sample of children across a broad age range from 12–38-months allowed us to examine how the association between temper tantrums and expressive vocabulary varies with age. We observed a significant main effect of expressive vocabulary size on temper tantrums; however, the interaction between age and expressive vocabulary indicated the strength of this association increased with age. In a practical sense, this indicates that having a reduced vocabulary size is a greater risk factor for older than younger children. In one other cross-sectional study with a relatively large sample (n = 1,189), 12- to 39-month-old toddlers with low expressive language ability (lowest 10% on the CDI) demonstrated varying patterns of externalizing and internalizing mental health problems across ages (Horwitz et al., 2003). In that study, toddlers 12–17 months with low language ability demonstrated lower prosocial peer relations than peers, but no associations were detected with internalizing or externalizing behaviors. Toddlers with low language at 18–23 months demonstrated poorer attention skills, whereas after 30 months, children with low language showed significantly higher rates of externalizing behavior. Rather than just in older toddlers, we saw that this pattern of weaker language associating with more frequent and severe temper tantrums was present even in younger, 18-month-old toddlers. In our study, we also considered temper tantrums, which are indicators of irritability and thus related to later internalizing and externalizing problems, and may be an explanatory pathway for the observed decrements in peer relations and attention. The focus on temper tantrums, which are both common and easily observable, may have helped to identify this pattern at an earlier age than prior work.
Our second analysis revealed that late talkers age 24–30 months had higher temper tantrum scores, and were nearly twice as likely to have severe temper tantrums, than typically-developing peers. These findings indicate an association between late talking status and mental health risk early in development, at ages before clinical diagnoses are typically made, suggesting an avenue for early neurodevelopmental risk identification. At this age, the smaller vocabulary size that characterizes late talking does not itself indicate a clinical disorder. It does, however, allow us to approximate risk for later disorder, as 40% of children who are late talkers in toddlerhood will go on to meet criteria for language disorder at school age (Dale et al., 2003).
Similarly, by measuring temper tantrum severity, we reflect on patterns of frequent and dysregulated temper tantrums that are indicators of childhood irritability. Irritability, of which tantrums are the most salient feature in young children, is a robust predictor of both internalizing and externalizing problems across the life span (Brotman, Kircanski, Stringaris, Pine, & Leibenluft, 2017; Wakschlag et al., 2015). Although the present study was cross-sectional, we theorize that the joint occurrence of delayed language and dysregulated tantrums will increase the likelihood of sustained and impairing language problems. A longitudinal study to test this hypothesis is currently underway.
The present findings are consistent with previous early childhood studies that have also demonstrated links between emergent language and mental health risk. For example, in one study, social-emotional skills were compared in 14 late-talking toddlers ages 21–31 months relative to 14 typically-developing peers (Irwin et al., 2002). Scales of dysregulated behavior and activity/impulsivity, similar constructs to our tantrum measure, showed the same patterns of greater severity in the late talker group and had similar effect sizes (η2 = .04−.07), but these did not reach significance in their smaller sample. In another study of 64 children ages 24–26 months, those with language delays scored significantly higher on scales of anxiety, depression, and internalizing/externalizing problems (Carson et al., 1998).
The vast influences on development led us to consider effects of poverty and child sex in our analyses. In this sample, late talkers were no more likely to be in poverty than non-late talkers, and there was only a marginal effect of late talking being more common in boys. Our finding that family poverty status was significantly associated with higher child tantrum severity scores is consistent with previous work showing that children from low-SES homes are more likely to demonstrate disruptive behavior than higher-income peers (Bertrand & Pan, 2013). However, we did not replicate previous findings in older children that boys demonstrate more disruptive behavior than girls (Wakschlag et al., 2012). In our regression analysis including the full sample, girls on average had higher tantrum scores than boys, and in our second analysis of 24- to 30-month-olds, sex was not significantly related with temper tantrums. Our group has previously found a moderating effect of sex on the relation between broader language and mental health indicators in this sample, such that at high levels of language ability, rates of irritable behavior are lower in girls than boys (Roberts et al., 2018).
There are multiple potential mechanisms for the observed relation between expressive language and temper tantrums. It is possible that there are multiple causal factors that are additive, or perhaps distinct profiles or subtypes, which are each explained by one or more of these hypotheses. Perhaps the simplest explanation is that children with poorer expressive language are unable to adequately express themselves verbally and instead resort to temper tantrums as a method of communication or out of frustration (Daniels et al., 2012; Harrington, 2004; Mayo Clinic, 2015; Swanson, 2014). This idea is supported by the fact that children with expressive language delays but average receptive language and intellectual abilities demonstrate reduced mental health (Caulfield et al., 1989; Irwin et al., 2002). A second explanation is that the relation is bidirectional. In this case, children with lower expressive skills are more frustrated and tantrum more; tantrums, in turn, reduce their participation in daily life and limit their language input and opportunities for language learning. A third possibility is that language and mental health disorders share biological underpinnings and that children with one risk factor are more likely to display the second. Further, a moderating factor, such as social-emotional skills or self-regulation abilities, may explain some of the relation between language and early mental health indicators (Horwitz et al., 2003; Mayes et al., 2017; Tomblin et al., 2000; Vitiello & Williford, 2016; Zadeh et al., 2007). In one longitudinal study, toddlers aged 18–24 months with better language skills and faster language development experienced less anger at 48 months; the relation was partially explained by use of regulation strategies (Roben et al., 2013). Future research aimed at identifying these profiles is crucial for the development of early meaningful indicators of risk for language and mental health problems and the development of appropriate treatment.
Notably, although we observed a statistically significant correlation between reduced expressive language and temper tantrums robust to sociodemographic indicators, the effect sizes for the association between language and temper tantrums are small. This further suggests that this association is multiply determined. Thus, although we examined family poverty status and child sex, other factors not examined here, such as parenting style, child cognitive abilities, or child nonverbal communication, also may influence these processes. Future research considering these overlapping developmental processes, causal influences, as well as moderating factors will be important to better understand the relation between expressive language and temper tantrums.
There are some other important considerations and limitations regarding this study, which also bring forward the need for future research. Although the cross-sectional survey design of our study allowed for collection of data from a large and representative sample, this method introduced several limitations. In both of our analyses, we used parent report to assess our constructs of interest, which can lead to shared method variance. Additionally, though our prevalence of late talking was consistent with the broader field, the categorical nature of the response choices to the vocabulary size question may have reduced meaningful variance. Further, it may have been difficult for parents to accurately estimate which answer best represents their child’s vocabulary if a child’s expressive vocabulary fell around one of the boundaries (e.g., is child’s vocabulary 45 or 55 words, near the 50-word boundary). Although we assessed temper tantrum severity using a multi-directional parent survey, we were unable to ask parents an extensive set of questions about their child’s language skills given the focus of the larger study on early mental health risk. This limitation should be considered in evaluating the findings of this study; however, we also suggest that a short language and temper tantrum screener could have useful clinical significance in identifying children at risk for either or both disorders. In addition, because of the panel demographics, we collected reports exclusively from mothers. Future analyses could compare reports from other parents or caregivers. Lastly, though we examined language and temper tantrums across a large band of toddlers, following young toddlers longitudinally would allow additional questions about how language development influences mental health and vice versa. Using performance-based measures of both language and temper tantrums will provide more in-depth understanding of their relation (Brotman et al., 2017; Petitclerc et al, 2015). Whereas we focused on expressive language here, delays in receptive language are important to consider in evaluating shared developmental profiles of language and mental health disorder. Assessment of receptive language could also help to answer questions about whether children with severe temper tantrums not only struggle to expressive themselves verbally, but may also be frustrated because of challenges understanding language.
Results from this study also have implications for clinical practice. Consistent with recommendations by Bishop and the CATALISE consortium (2016), identification of corollary red flags such as mental health and behavioral problems may allow developmental specialists to identify those young children with highest risk for language impairments earlier by specifying risk profiles that extend beyond language status alone. For example, early markers of mental health risk (i.e., severe temper tantrums) and language disorders (i.e., late talking) in tandem may increase probabilistic risk of functional impairment, in part because they jointly constrain environmental experience. Recognizing these patterns of vulnerability is important because developmental disorders often co-occur within children (Butterworth & Kovas, 2013; Caron & Rutter, 1991) and because many professional organizations recommend an interdisciplinary team approach to identification and intervention for children (e.g., American Academy of Pediatrics: Foy, Kelleher, & Laraque, 2010; American Speech-Language-Hearing Association: Paul-Brown & Ricker, 2003). Incorporating measurement of temper tantrums in particular is promising because it is quick, inexpensive, and scalable. Here, by using just parent-report questions as part of an online survey rather than more time-consuming or costly methods, we found results consistent with previous early childhood studies which have identified an association between mental health indicators and language delay using more extensive measures (Carson et al., 1998; Caulfield et al., 1989; Irwin et al., 2002; Paul & James, 1990; Roben et al., 2013; Tervo, 2007; Thurm et al., 2017; Whitehouse et al., 2011). Given their frequent co-occurrence, we also suggest that early intervention providers should consider mental health indicators, including severe temper tantrums, in the development of treatment plans for children with language delay. Effective intervention is especially important as co-occurring language and mental health disorders have long-term adverse consequences on child and family outcomes beyond the effect of either disorder alone (Nes et al., 2015). Intervention approaches may also consider that addressing one of these areas may impact the other; for example, targeting language skills in young children has been shown to reduce externalizing problems (Curtis et al., 2019). Of course, many toddlers with either or both of these early patterns of atypicality will go on to develop typically, but characterizing their emergence and relations will help us to better understand individual differences in how they portend typical and atypical development.
Supplementary Material
Highlights.
Expressive language is associated with temper tantrums in 12–38-month-olds
Late talkers, i.e., children with language delay, have more severe temper tantrums
Relative risk for severe tantrums is nearly 2x greater for late talkers
A relation between emergent language and mental health risk is evident
Acknowledgements
We thank Martha Neary for assistance with data collection and Camille Nuttall, Silvia Lam, Sean McWeeny, Emily Harriott, Emma Baime, Kamila Postolowicz, Winnie Liang, Olufemi Nyabingi, and Julia Nikolaeva for assistance with manuscript preparation. We gratefully acknowledge the contributions of our collaborators Ellen Leibenluft and Daniel Pine to the W2W Study. This work was supported by National Institute of Mental Health grant R01MH10765201 to Lauren Wakschlag, including support for Briggs-Gowan, Estabrook, Norton, Petitclerc, and Roberts.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Declarations of Interest: None.
References
- Allison C, Baron-Cohen S, Wheelwright S, Charman T, Richler J, Pasco G, & Brayne C (2008). The Q-CHAT (Quantitative Checklist for Autism in Toddlers): A normally distributed quantitative measure of autistic traits at 18–24 months of age: Preliminary report. Journal of Autism and Developmental Disorders, 38(8), 1414–1425. 10.1007/s10803-007-0509-7 [DOI] [PubMed] [Google Scholar]
- American Speech-Language Hearing Association (nd). Late language emergence Retrievedfrom https://www.asha.org/Practice-Portal/Clinical-Topics/Late-Language-Emergence/
- Belden AC, Thomson NR, & Luby JL (2008). Temper tantrums in healthy versus depressed and disruptive preschoolers: Defining tantrum behaviors associated with clinical problems. The Journal of Pediatrics, 152(1), 117–122. 10.1016/j.jpeds.2007.06.030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benasich AA, Curtiss S, & Tallal P (1993). Language, learning, and behavioral disturbances in childhood: A longitudinal perspective. Journal of the American Academy of Child & Adolescent Psychiatry, 32(3), 585–594. 10.1097/00004583-199305000-00015 [DOI] [PubMed] [Google Scholar]
- Benner GJ, Nelson JR, & Epstein MH (2002). Language skills of children with EBD: A literature review. Journal of Emotional and Behavioral Disorders, 10(1), 43–56. 10.1177/106342660201000105 [DOI] [Google Scholar]
- Bertrand M, & Pan J (2013). The trouble with boys: Social influences and the gender gap in disruptive behavior. American Economic Journal: Applied Economics, 5(1), 32–64. 10.1257/app.5.1.32 [DOI] [Google Scholar]
- Biedzio D, & Wakschlag L (2019). Developmental emergence of disruptive behaviors beginning in infancy: Delineating normal:abnormal boundaries to enhance early identification. In Zeenah C (Ed.), Handbook of Infant Mental Health, 4th ed. (pp.407–425). New York: Guilford. [Google Scholar]
- Bishop DVM, Snowling MJ, Thompson PA, Greenhalgh T, & CATALISE consortium. (2016). CATALISE: A multinational and multidisciplinary Delphi consensus study. Identifying language impairments in children. PLoS One, 11(7), e0158753. 10.1371/journal.pone.0158753 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bricker D, & Squires J (1999). Ages & Stages Questionnaires: A Parent-Completed, Child-Monitoring System 2nd ed. Baltimore, MD: Paul H. Brookes. [Google Scholar]
- Brotman MA, Kircanski K, Stringaris A, Pine DS, & Leibenluft E (2017). Irritability in youths: A translational model. American Journal of Psychiatry, 174(6), 520–532. 10.1176/appi.ajp.2016.16070839 [DOI] [PubMed] [Google Scholar]
- Butterworth B, & Kovas Y (2013). Understanding neurocognitive developmental disorders can improve education for all. Science, 340(6130), 300–305. 10.1126/science.1231022 [DOI] [PubMed] [Google Scholar]
- Campbell SB, Pierce EW, Moore G, Marakovitz S, & Newby K (1996). Boys’ externalizing problems at elementary school age: Pathways from early behavior problems, maternal control, and family stress. Development and Psychopathology, 8(4), 701–719. 10.1017/S0954579400007379 [DOI] [Google Scholar]
- Cantwell DP, & Baker L (1987). Prevalence and type of psychiatric disorder and developmental disorders in three speech and language groups. Journal of Communication Disorders, 20(2), 151–160. 10.1016/0021-9924(87)90006-2 [DOI] [PubMed] [Google Scholar]
- Carbonneau R, Boivin M, Brendgen M, Nagin D, & Tremblay RE (2016). Comorbid development of disruptive behaviors from age 1½ to 5 years in a population birth-cohort and association with school adjustment in first grade. Journal of Abnormal Child Psychology, 44(4), 677–690. 10.1007/s10802-015-0072-1 [DOI] [PubMed] [Google Scholar]
- Carlson GA, Danzig AP, Dougherty LR, Bufferd SJ, & Klein DN (2016). Loss of temper and irritability: The relationship to tantrums in a community and clinical sample. Journal of Child and Adolescent Psychopharmacology, 26(2), 114–122. 10.1089/cap.2015.0072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carson DK, Klee T, Perry CK, Muskina G, & Donaghy T (1998). Comparisons of children with delayed and normal language at 24 months of age on measures of behavioral difficulties, social and cognitive development. Infant Mental Health Journal, 19(1), 59–75. [DOI] [Google Scholar]
- Caron C, & Rutter M (1991). Comorbidity in child psychopathology: Concepts, issues and research strategies. Journal of Child Psychology and Psychiatry, 32(7), 1063–1080. 10.1111/j.1469-7610.1991.tb00350.x [DOI] [PubMed] [Google Scholar]
- Carter AS, Briggs-Gowan MJ, Jones SM, Little TD (2003). The Infant-Toddler Social and Emotional Assessment (ITSEA): Factor structure, reliability, and validity. Journal of Abnormal Child Psychology, 31(5),495–514. 10.1023/A:1025449031360 [DOI] [PubMed] [Google Scholar]
- Caulfield MB, Fischel JE, DeBaryshe BD, & Whitehurst GJ (1989). Behavioral correlates of developmental expressive language disorder. Journal of Abnormal Child Psychology, 17(2), 187–201. 10.1007/BF00913793 [DOI] [PubMed] [Google Scholar]
- Chow JC, & Wehby JH (2017). Profiles of problem behavior in children with varying language ability. Journal of Emotional and Behavioral Disorders, 27(2), 110–118. 10.1177/1063426617733714 [DOI] [Google Scholar]
- Chow JC, & Wehby JH (2018). Associations between language and problem behavior: A systematic review and correlational meta-analysis. Educational Psychology Review, 30(1), 61–82. 10.1007/s10648-016-9385-z [DOI] [Google Scholar]
- Cohen NJ, Menna R, Vallance DD, Barwick MA, Im N, & Horodezky NB (1998). Language, social cognitive processing, and behavioral characteristics of psychiatrically disturbed children with previously identified and unsuspected language impairments. Journal of Child Psychology and Psychiatry, 39(6), 853–864. 10.1111/1469-7610.00286 [DOI] [PubMed] [Google Scholar]
- Conti-Ramsden G, & Botting N (2008). Emotional health in adolescents with and without a history of specific language impairment (SLI). Journal of Child Psychology and Psychiatry, 49(5), 516–525. 10.1111/j.1469-7610.2007.01858.x [DOI] [PubMed] [Google Scholar]
- Curtis PR, Kaiser AP, Estabrook R, & Roberts MY (2019). The longitudinal effects of early language intervention on children’s problem behaviors. Child Development, 90(2), 576–592. 10.1111/cdev.12942 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dale PS, Price TS, Bishop DVM, & Plomin R (2003). Outcomes of early language delay: I. Predicting persistent and transient language difficulties at 3 and 4 years. Journal of Speech Language and Hearing Research, 46(3), 544–560. 10.1044/1092-4388(2003/044) [DOI] [PubMed] [Google Scholar]
- Daniels E, Mandleco B, & Luthy KE (2012). Assessment, management, and prevention of childhood temper tantrums. Journal of the American Association of Nurse Practitioners, 24(10), 569–573. 10.1111/j.1745-7599.2012.00755.x [DOI] [PubMed] [Google Scholar]
- Dionne G, Tremblay R, Boivin M, Laplante D, & Perusse D (2003). Physical aggression and expressive vocabulary in 19-month-old twins. Developmental Psychology, 39(2), 261–273. 10.1037/0012-1649.39.2.261 [DOI] [PubMed] [Google Scholar]
- Fenson L, Marchman VA, Thal DJ, Dale PS, & Reznick JS (2007). MacArthur-Bates Communicative Development Inventories. Baltimore, MD: Paul H. Brookes. [Google Scholar]
- Foy JM, Kelleher KJ, Laraque D, & American Academy of Pediatrics Task Force on Mental Health. (2010). Enhancing pediatric mental health care: strategies for preparing a primary care practice. Pediatrics, 125(Supplement 3), S87–S108. 10.1542/peds.2010-0788E [DOI] [PubMed] [Google Scholar]
- Harrington RG (2004). Temper tantrums: Guidelines for parents Retrieved 11/1/2018 from http://www.naspcenter.org/parents/tantrums_ho.html [Google Scholar]
- Hoff E (2013). Interpreting the early language trajectories of children from low-SES and language minority homes: Implications for closing achievement gaps. Developmental Psychology, 49(1), 4–14. 10.1037/a0027238 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horwitz SM, Irwin JR, Briggs-Gowan MJ, Heenan JMB, Mendoza J, & Carter AS (2003). Language delay in a community cohort of young children. Journal of the American Academy of Child & Adolescent Psychiatry, 42(8), 932–940. 10.1097/01.CHI.0000046889.27264.5E [DOI] [PubMed] [Google Scholar]
- Irwin JR, Carter AS, & Briggs-Gowan MJ (2002). The social-emotional development of “late-talking” toddlers. Journal of the American Academy of Child and Adolescent Psychiatry, 41(11), 1324–1332. 10.1097/00004583-200211000-00014 [DOI] [PubMed] [Google Scholar]
- Javorsky J (1995). An examination of language learning disabilities in youth with psychiatric disorders. Annals of Dyslexia, 45, 215–231. 10.1007/BF02648219 [DOI] [PubMed] [Google Scholar]
- Lewsey JD, Gardiner WP, & Gettinby G (1997). A study of simple unbalanced factorial designs that use type ii and type iii sums of squares. Communications in Statistics - Simulation and Computation, 26(4), 1315–1328. 10.1080/03610919708813442 [DOI] [Google Scholar]
- Love AJ, & Thompson MG (1988). Language disorders and attention deficit disorders in young children referred for psychiatric services: Analysis of prevalence and a conceptual synthesis. American Journal of Orthopsychiatry, 58(1), 52–64. 10.1111/j.1939-0025.1988.tb01566.x [DOI] [PubMed] [Google Scholar]
- Maggio V, Grañana NE, Richaudeau A, Torres S, Giannotti A, & Suburo AM (2014). Behavior problems in children with specific language impairment. Journal of Child Neurology, 29(2), 194–202. 10.1177/0883073813509886 [DOI] [PubMed] [Google Scholar]
- Mattison RE, Cantwell DP, & Baker L (1980). Behavior problems in children with speech and language retardation. Child Psychiatry and Human Development, 10(4), 246–257. 10.1007/BF01433684 [DOI] [PubMed] [Google Scholar]
- Mayes SD, Lockridge R, & Tierney CD (2017). Tantrums are not associated with speech or language deficits in preschool children with autism. Journal of Developmental and Physical Disabilities, 29(4), 587–596. 10.1007/s10882-017-9546-0 [DOI] [Google Scholar]
- Clinic Mayo (2015). Temper tantrums in toddlers: How to keep the peace Retrieved 11/1/2018 from https://www.mayoclinic.org/healthy-lifestyle/infant-and-toddler-health/in-depth/tantrum/art-20047845
- Nes RB, Hauge LJ, Kornstad T, Landolt MA, Irgens L, Eskedal L, … Vollrath ME (2015). Maternal work absence: A longitudinal study of language impairment and behavior problems in preschool children. Journal of Marriage and Family, 77, 1282–1298. 10.1111/jomf.12210 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nicolson R, Lenane M, Singaracharlu S, Malaspina D, Giedd JN, Hamburger SD, … Rapoport JL (2000). Premorbid speech and language impairments in childhood-onset schizophrenia: Association with risk factors. American Journal of Psychiatry, 157(5), 794–800. 10.1016/S0920-9964(00)90420-1 [DOI] [PubMed] [Google Scholar]
- Paul R (1991). Profiles of toddlers with slow expressive language development. Topics in Language Disorders, 11(4), 1–13. 10.1097/00011363-199111040-00003 [DOI] [Google Scholar]
- Paul R (1996). Clinical implications of the natural history of slow expressive language development. American Journal of Speech-Language Pathology, 5(2), 5–21. 10.1044/1058-0360.0502.05 [DOI] [Google Scholar]
- Paul R, & James DF (1990). Language delay and parental perceptions. Journal of the American Academy of Child & Adolescent Psychiatry, 29(4), 669–670. 10.1097/00004583-199007000-00030 [DOI] [PubMed] [Google Scholar]
- Paul-Brown D, & Ricker JH (2003). American Speech-Language-Hearing Association: Evaluating and treating communication and cognitive disorders: Approaches to referral and collaboration for speech-language pathology and clinical neuropsychology [Technical Report] 10.1044/policy.TR2003-00137 [DOI]
- Petitclerc A, Briggs-Gowan MJ, Estabrook R, Burns JL, Anderson EL, McCarthy KJ, & Wakschlag LS (2015). Contextual variation in young children’s observed disruptive behavior on the DB-DOS: Implications for early identification. Journal of Child Psychology and Psychiatry, 56(9), 1008–1016. 10.1111/jcpp.12430 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Potegal M, & Davidson RJ (2003). Temper tantrums in young children: 1. Behavioral composition. Journal of Developmental and Behavioral Pediatrics, 24(3), 140–147. 10.1097/00004703-200306000-00002 [DOI] [PubMed] [Google Scholar]
- Redmond SM, & Rice ML (1998). The socioemotional behaviors of children with SLI: Social adaptation or social deviance. Journal of Speech, Language, and Hearing Research, 41(3), 688–700. 10.1044/jslhr.4103.688 [DOI] [PubMed] [Google Scholar]
- Reilly S, Wake M, Ukoumunne OC, Bavin E, Prior M, Cini E, … Bretherton L (2010). Predicting language outcomes at 4 years of age: findings from Early Language in Victoria Study. Pediatrics, 126(6), e1530–e1537. https://doi.org10.1542/peds.2010-0254 [DOI] [PubMed] [Google Scholar]
- Rescorla L (2011). Late talkers: Do good predictors of outcome exist? Developmental Disabilities Research Reviews, 17(2), 141–150. 10.1002/ddrr.1108 [DOI] [PubMed] [Google Scholar]
- Rescorla L, & Alley A (2001). Validation of the Language Development Survey (LDS): A parent report tool for identifying language delay in toddlers. Journal of Speech, Language, and Hearing Research, 44(2), 434–445. 10.1044/1092-4388(2001/035) [DOI] [PubMed] [Google Scholar]
- Roben CK, Cole PM, & Armstrong LM (2013). Longitudinal relations among language skills, anger expression, and regulatory strategies in early childhood. Child Development, 84(3), 891–905. 10.1111/cdev.12027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Röll J, Koglin U, & Petermann F (2012). Emotion regulation and childhood aggression: Longitudinal associations. Child Psychiatry & Human Development, 43(6), 909–923. 10.1007/s10578-012-0303-4 [DOI] [PubMed] [Google Scholar]
- Samejima F (1997). The graded response model. In van der Linden WJ & Hambleton RK (Eds.), Handbook of modern item response theory (pp. 85–100). New York: Springer. [Google Scholar]
- Stott CM, Merricks MJ, Bolton PF, & Goodyer IM (2002). Screening for speech and language disorders: The reliability, validity and accuracy of the General Language Screen. International Journal of Language and Communication Disorders, 37(2), 133–151. 10.1080/13682820110116785 [DOI] [PubMed] [Google Scholar]
- Swanson WS (2014). Top tips for surviving tantrums Retrieved 11/1/2018 from https://www.healthychildren.org/English/family-life/family-dynamics/communication-discipline/Pages/Temper-Tantrums.aspx
- Tamis-LeMonda CS, Bornstein MH, & Baumwell L (2001). Maternal responsiveness and children’s achievement of language milestones. Child Development, 72(3), 748–767. 10.1111/1467-8624.00313 [DOI] [PubMed] [Google Scholar]
- Tervo RC (2007). Language proficiency, development, and behavioral difficulties intoddlers. Clinical Pediatrics, 46(6), 530–539. 10.1177/0009922806299154 [DOI] [PubMed] [Google Scholar]
- Thurm A, Farmer CA, Manwaring S, & Swineford L (2017). Social-emotional and behavioral problems in toddlers with language delay. Journal of the American Academy of Child & Adolescent Psychiatry, 56(10), S155. 10.1016/j.jaac.2017.09.024 [DOI] [Google Scholar]
- Tomblin JB, Zhang X, Buckwalter P, & Catts H (2000). The association of reading disability, behavioral disorders, and language impairment among second-grade children. Journal of Child Psychology and Psychiatry, 41(4), 473–482. 10.1111/1469-7610.00632 [DOI] [PubMed] [Google Scholar]
- Toppelberg CO, & Shapiro T (2000). Language disorders: A 10-year research update review. Journal of the American Academy of Child & Adolescent Psychiatry, 39(2), 143–152. 10.1097/00004583-200002000-00011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Census Bureau (2015). QuickFacts: United States Retrieved 11/1/2018 from https://www.census.gov/quickfacts/table/PST045216/00
- U.S. Department of Health and Human Services (2017). U.S. federal poverty guidelines used to determine financial eligibility for certain federal programs Retrieved 11/1/2018 from https://aspe.hhs.gov/poverty-guidelines [Google Scholar]
- Van Daal J, Verhoeven L, & Van Balkom H (2007). Behaviour problems in children with language impairment. Journal of Child Psychology and Psychiatry, 48(11), 1139–1147. 10.1111/j.1469-7610.2007.01790.x [DOI] [PubMed] [Google Scholar]
- Vitiello V, & Williford AP (2016). Relations between social skills and language and literacy outcomes among disruptive preschoolers: Task engagement as a mediator. Early Childhood Research Quarterly, 36, 136–144. 10.1016/j.ecresq.2015.12.011 [DOI] [Google Scholar]
- Wakschlag LS, Briggs-Gowan MJ, Carter AS, Hill C, Danis B, Keenan K, … Leventhal BL (2007). A developmental framework for distinguishing disruptive behavior from normative misbehavior in preschool children. Journal of Child Psychology and Psychiatry, 48(10), 976–987. 10.1111/j.1469-7610.2007.01786.x [DOI] [PubMed] [Google Scholar]
- Wakschlag LS, Briggs-Gowan MJ, Choi SW, Nichols SR, Kestler J, Burns JL, … Henry D (2014). Advancing a multidimensional, developmental spectrum approach to preschool disruptive behavior. Journal of the American Academy of Child & Adolescent Psychiatry, 53(1), 82–96. 10.1016/j.jaac.2013.10.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wakschlag LS, Choi SW, Carter AS, Hullsiek H, Burns J, McCarthy K, … Briggs-Gowan MJ (2012). Defining the developmental parameters of temper loss in early childhood: Implications for developmental psychopathology. Journal of Child Psychology and Psychiatry, 53(11), 1099–1108. 10.1111/j.1469-7610.2012.02595.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wakschlag LS, Estabrook R, Petitclerc A, Henry D, Burns J, Perlman S, … Briggs-Gowan M (2015). Clinical implications of a dimensional approach: The normal:abnormal spectrum of early irritability. Journal of the American Academy of Child & Adolescent Psychiatry, 54, 626–634. 10.1016/j.jaac.2015.05.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wakschlag LS, Perlman SB, Blair RJ, Leibenluft E, Briggs-Gowan M, & Pine DS (2018). The neurodevelopmental basis of early childhood disruptive behavior: Irritable and callous phenotypes as exemplars. American Journal of Psychiatry, 175(2), 114–130. 10.1176/appi.ajp.2017.17010045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wakschlag L, Roberts M, Flynn R, Smith JD, Krogh-Jespersen S, Gray L, … Davis MM (2019). Future directions for advancing early identification and prevention of mental disorders: A roadmap to mental health, earlier. Journal of Clinical Child and Adolescent Psychiatry, 48(3), 539–554. 10.1080/15374416.2018.1561296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wiggins JL, Briggs-Gowan MJ, Estabrook R, Brotman MA, Pine DS, Leibenluft E, & Wakschlag LS (2018). Identifying clinically significant irritability in early childhood. Journal of the American Academy of Child & Adolescent Psychiatry, 57(3), 191–199. 10.1016/j.jaac.2017.12.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Willinger U, Brunner E, Diendorfer-Radner G, Sams J, Sirsch U, & Eisenwort B (2003). Behaviour in children with language development disorders. The Canadian Journal of Psychiatry, 48(9), 607–614. 10.1177/070674370304800907 [DOI] [PubMed] [Google Scholar]
- Whitehouse AJ, Robinson M, & Zubrick SR (2011). Late talking and the risk for psychosocial problems during childhood and adolescence. Pediatrics, 128(2), e324–e332. 10.1542/peds.2010-2782 [DOI] [PubMed] [Google Scholar]
- Zadeh ZY, Im-Bolter N, & Cohen NJ (2007). Social cognition and externalizing psychopathology: An investigation of the mediating role of language. Journal of Abnormal Child Psychology, 35(2), 141–152. 10.1007/s10802-006-9052-9 [DOI] [PubMed] [Google Scholar]
- Zubrick SR, Taylor CL, Rice ML, & Slegers DW (2007). Late language emergence at 24 months: An epidemiological study of prevalence, predictors, and covariates. Journal of Speech Language and Hearing Research, 50(6), 1562–1592. 10.1044/1092-4388(2007/106) [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.