Abstract
The objective of this study is to investigate the magnitude of structural degradation of a monolithic translucent zirconia caused by clinically relevant grinding and polishing procedures, when associated or not with low temperature degradation (LTD), induced by accelerated hydrothermal aging using autoclave or thermocycling Ninety disks (Ø12 × 1 mm) were prepared from dental zirconia for monolithic restorations (Vipi Block Zirconn Translucent, Vipi). The specimens were divided into 3 groups (n = 30) according to surface treatment: As Sintered (untreated), Grind (diamond bur), Grind + Polish (diamond bur + polish); and then subdivided according to aging method (n = 10): Baseline (no aging), Autoclave (134°C, 2.2 kgf/cm2 pressure for 5 h), and Thermocycling (200,000 cycles, 5°C and 55°C, for 15 s each). Roughness, biaxial flexural strength and percentage of monoclinic phase were evaluated. Regarding surface treatment, the Grind group presented higher roughness and greater flexural strength compared to As Sintered group, while Grind + Polish showed intermediate roughness and flexural strength similar to Grind group. Aging had little effect on roughness, but yielded a significant reduction in flexural strength. Tetragonal to monoclinic phase transformation was observed in all groups, caused by both mechanical stresses (grinding and polishing) and LTD, which was similarly induced by the traditional autoclave method, as well as the thermocycling method The use of diamond burs to grind zirconia surface may result in deleterious effects on the surface quality of monolithic zirconia restorations, yet has a potential toughening effect by phase transformation. However, when zirconia is exposed to LTD, regardless of the surface treatment, degradation of the surface quality and strength are observed.
Keywords: A – Finishing, B – Surfaces, C - Mechanical properties, D – ZrO2
1. INTRODUCTION
Traditional dental zirconia, 3Y-TZP (3 mol% yttria-stabilized tetragonal zirconia polycrystal), contains alumina (Al2O3) as a promoter of densification, presenting high opacity and superior mechanical properties [1, 2]. The development of the zirconia for dental restorations followed a movement to increase the translucency and aesthetics of the final product This result can be obtained by various strategies that may or may not be combined: (i) reducing or eliminating alumina while increasing the density of zirconia, to reduce light scattering by pores and secondary phases; (ii) sintering at a temperature higher than that required for densification to increase the tetragonal grain size and / or increase the cubic phase content, which is more translucent than the tetragonal; and (iii) adding a greater amount of yttria, 4 mol% (4Y-PSZ, 4 mol% yttria partially stabilized zirconia) or 5 mol% (5Y-PSZ), to increase the cubic phase content All these strategies also influence the crystalline stability of zirconia and consequently its mechanical properties [1, 3–8].
Yttria stabilized zirconia has traditionally been used in single or multiple fixed prostheses as a coping material, which is subsequently coated with porcelain for better aesthetics using the layering technique However, such (layered) structures are prone to adhesive failures – between the infrastructure and the porcelain (delamination) – or cohesive failures, which occur within the porcelain (chipping) Chipping has been the most frequent type of complication reported in indirect restorations with zirconia infrastructure [9–14]. To reduce the chances of fracture (delamination and chipping), monolithic restorations have been introduced to the clinical practice [3, 15–17]. Monolithic zirconia restorations are made from more translucent zirconias obtained through the strategies described earlier.
However, during clinical use, monolithic zirconia is in constant contact with saliva and exposed to chewing loading and the person’s diet. Such environment makes zirconia susceptible to the phenomenon of low temperature degradation (LTD) [18, 19], which is characterized by the spontaneous transformation of the tetragonal phase into monoclinic when the material is exposed to moisture over time at low temperatures. LTD occurs primarily on the surface, which is originally composed of densely sintered tetragonal grains that undergo transformation to monoclinic grains, involving a 3–5% increase in grain volume, thereby creating micro-defects on the surface Water then penetrates into the intergranular defects causing phase transformation to occur progressively into the subsurface. In addition to an increase in surface micro-roughness, there happens a decrease in hardness; and, with the progression of LTD in depth, there is also the degradation of the mechanical strength of the material. The microstructure and chemical and crystalline composition of zirconia define its susceptibility to LTD: bigger tetragonal grains are critically susceptible to LTD, whereas cubic-containing zirconias are more stable [20–24].
Despite significant advances in the accuracy and external and internal adaptation of computer-aided design/computer-aided machining (CAD/CAM) systems, final adjustment of indirect restorations is still needed in order to improve the precise fitting and the occlusal contacts with the antagonist [25, 26]. These adjustments can be made with diamond burs, abrasive stones, and ideally should be followed by careful surface polishing with a sequence of diamond-impregnated rubber burs with decreasing abrasiveness. When the surface of the zirconia is ground during the testing and adjustment phases, surface defects are introduced; and some phase transformation (tetragonal → monoclinic) occurs, induced by mechanical stresses from the grinding and polishing procedures. The tetragonal and cubic phase fractions and the tetragonal grain sizes are key factors defining the susceptibility of the zirconia to phase transformation [1, 3–8]. The relationship between the depth of the transformed layer (consequently, the compressive stresses in such layer) and the size of the defects present on the zirconia surface can facilitate crack growth in the material, making it susceptible to premature failure at loads below the critical value [22, 25]. Furthermore, it is known that the polishing systems available on the market are not efficient in polishing sintered zirconia when it has an extremely rough surface produced by diamond burs [27].
Therefore, this study investigates the magnitude of degradation of a monolithic translucent zirconia caused by clinically relevant grinding and polishing procedures, associated or not with LTD. Two methods to induce LTD are also evaluated: (1) autoclave accelerated hydrothermal aging – traditionally used to evaluate zirconia phase transformation, but with limited clinical relevance; and (2) thermocycling, which is a widely used aging method for a clinically relevant evaluation of the degradation of various dental materials; yet little is known about its effect on the LTD of zirconia. The tested hypotheses are: i) the different grinding and polishing methods used influence the surface micro-morphology, phase transformation and biaxial flexural strength of a monolithic translucent zirconia; and ii) the different aging methods negatively influence the micro-morphology of the surface, phase transformation and biaxial flexural strength of a monolithic translucent zirconia.
2. MATERIALS AND METHODS
2.1. Specimen preparation
Ninety disk-shaped specimens were prepared from pre-sintered blocks of a monolithic translucent Y-TZP zirconia (Vipi Block Zirconn Translucent, Vipi, Brazil). This is an alumina-free 3 mol% yttria-stabilized zirconia, with high pre-sintered density. For standardization and removal of surface irregularities introduced by the cutting, the surface of the samples was finished with 1200-grit silicon carbide sandpaper and cleaned in an isopropyl alcohol ultrasound bath for 10 min.
The specimens were sintered at 1450°C for 2 h, with a heating rate of 8°C/min, according to manufacturer recommendations. After sintering specimens had the final dimensions of Ø12 mm × 1 mm (± 0.05 mm). The ninety specimens were then randomly distributed according to surface treatment and aging type.
2.2. Grinding and polishing methods
A group without any surface treatment after sintering (As Sintered) was used as reference.
The instruments used for grinding and polishing are described in Table 1. A single operator, trained in a pilot study, performed grinding and polishing on one side of each disc using diamond and rubber burs attached to a low-speed hand-piece using 8,000 to 10,000 rpm according to the manufacturer recommendations. Diamond bur were replaced after every five specimens. To standardize the grinding and polishing procedures, oscillatory movements were performed with diamond and rubber burs, simulating clinical grinding movements, introducing surface defects in all possible directions. To ensure stability, specimens were fixed with a double-sided tape to a stiff and flat base. The specimens were then marked with a permanent marker to standardize the thickness of grinding and ensure that the entire surface of the sample was treated Grinding and polishing were performed with oscillating movements and under gentle pressure (digital pressure) until the pen mark was completely eliminated.
Table 1:
Experimental design and description of surface treatments
| SURFACE TREATMENT | Aging Method (n = 90) |
|---|---|
| Without treatment (As Sintered) | Without aging (Baseline) (n = 10) |
| Autoclave (n = 10) | |
| Thermocycling (n = 10) | |
| Grinding (Grind) Sintered diamond bur (medium grain, D.5118.HP / E, Frank Dental, Germany) |
Without aging (Baseline) (n = 10) |
| Autoclave (n = 10) | |
| Thermocycling (n = 10) | |
| Grinding + Polish (Grind + Polish) Sintered diamond bur + Zr polishing rubbers [sequential diamond polishers, P.CEME8G.HP (coarse), P.CEME8M.HP (intermediate finish) and P.CEME8F.HP (final finish), Frank Dental, Germany] |
Without aging (Baseline) (n = 10) |
| Autoclave (n = 10) | |
| Thermocycling (n = 10) |
2.3. Aging methods
For groups undergoing accelerated hydrothermal aging (Autoclave), treatment was performed in an autoclave at 134°C under pressure of 2.2 kgf/cm2 for 5 h, corresponding to a clinical use of about 21 years at 37°C [18, 21].
Thermocycling (OMC200, Odeme, Brazil) groups underwent 200,000 cycles of 15 s each, at a temperature of 5°C and 55°C, corresponding to approximately 20 years of physiological aging in the oral cavity [28].
After aging, all specimens were carefully cleaned in an isopropyl alcohol ultrasonic bath for 10 min.
2.4. Roughness analysis (Ra)
For surface roughness analysis, the specimens were fixed to a glass plate and taken individually to the profilometer (1700 Surf-Corder, Kosaka, Japan), equipped with a 5 μm radius diamond tip). The specimens were carefully handled with plastic tweezers, avoiding contamination of the treated surface. Before the readings began, the device was calibrated according to the manufacturer’s recommendations. For each reading, the needle ran a 2.5 mm stretch on the surface, at a constant speed of 0.5 mm/s, with a cut-off length of 0.25 mm to maximize surface ripple filtration.
Three roughness measurements, 45° rotation apart, were taken on the specimen treated surface. The average of the three readings was used as the Ra value for each specimen.
2.5. Biaxial flexural strength
Biaxial flexural strength (n = 10) was investigated with a piston-on-three-ball test using a universal testing machine (EMIC DL 2000, São José dos Pinhais, Brazil). Each specimen was positioned with the treated surface under tension. The tests were performed with the device and specimens immersed in artificial saliva at 37°C (150 mmol/L KCl, 1.5 mmol/L CaCl2, and 0.9 mmol/LKH2PO4 in 0.1 mol/L buffer) CH3COONa, pH 7.0). A flat loading piston with a diameter of 1.7 mm was used and the test was performed at a speed of 1 mm/min until catastrophic fracture of the specimens The biaxial flexural strength (in MPa) was calculated using equations 1–3, defined in the ISO6872 [29]:
| (Eq. 1) |
| (Eq. 2) |
| (Eq. 3) |
where P is the maximum load at fracture (N), ν is the Poisson’s ratio of the ceramic, t is the specimen thickness (mm), a is the radius of the support ring (mm), c is the radius of the loaded area (mm), and R is the specimen radius (mm).
2.6. Phase transformation and X-ray diffraction
Phase transformation analysis was performed to elucidate the relative amount of monoclinic phase (Vm) present in each of the evaluated conditions. The analysis was performed using an X-ray diffractometer with a CuKα radiation, with 2θ scanning between 25° and 35°, with a 0.03° step and a speed of 1 s per step. The quantification of the volumetric fraction of the monoclinic phase was calculated from the intensities of the monoclinic peaks (111)m and the tetragonal peak (101 or 111)t, according to equations 4 and 5 [30, 31]:
| (Eq. 4) |
| (Eq. 5) |
where (111)m it is located at 2θ = 28°, (111)m at 2θ = 31.2°, (101 or 111)t at 2θ = 30°, and represent the intensity of the diffracted peaks in the monoclinic planes (111)m and (111)m and the tetragonal plane (101 or 111)t.
2.7. Scanning electron microscopy (SEM)
In order to evaluate surface modifications caused by grinding and polishing before and after aging, specimens were coated (BAL-TEC SC_RD 005, BAL-TEC AG, Balzers, Liechtenstein) with Au/Pd alloy. Then surface images were taken at 500, 1000 and 5000 times magnifications, with 5 to 10 kV energy using a high resolution field-emission scanning electron microscope (FE-SEM MIRA3 LM, Tescan, USA).
2.8. Statistical analysis
Flexural strength and roughness data were normal and homoscedastic. Therefore, two-way ANOVA (surface treatment and aging method) and Tukey test with significance level 0.05 were performed. The correlation between roughness and biaxial flexure was analyzed using Spearman’s correlation test.
3. RESULTS
For mean roughness (Ra), statistical significance was observed for factors surface treatment (p <0.001) and aging (p = 0.025), as well as for the double interaction surface treatment × aging (p <0.001) The results of the multiple pairwise comparisons are presented in Figure 1.
Figure 1:
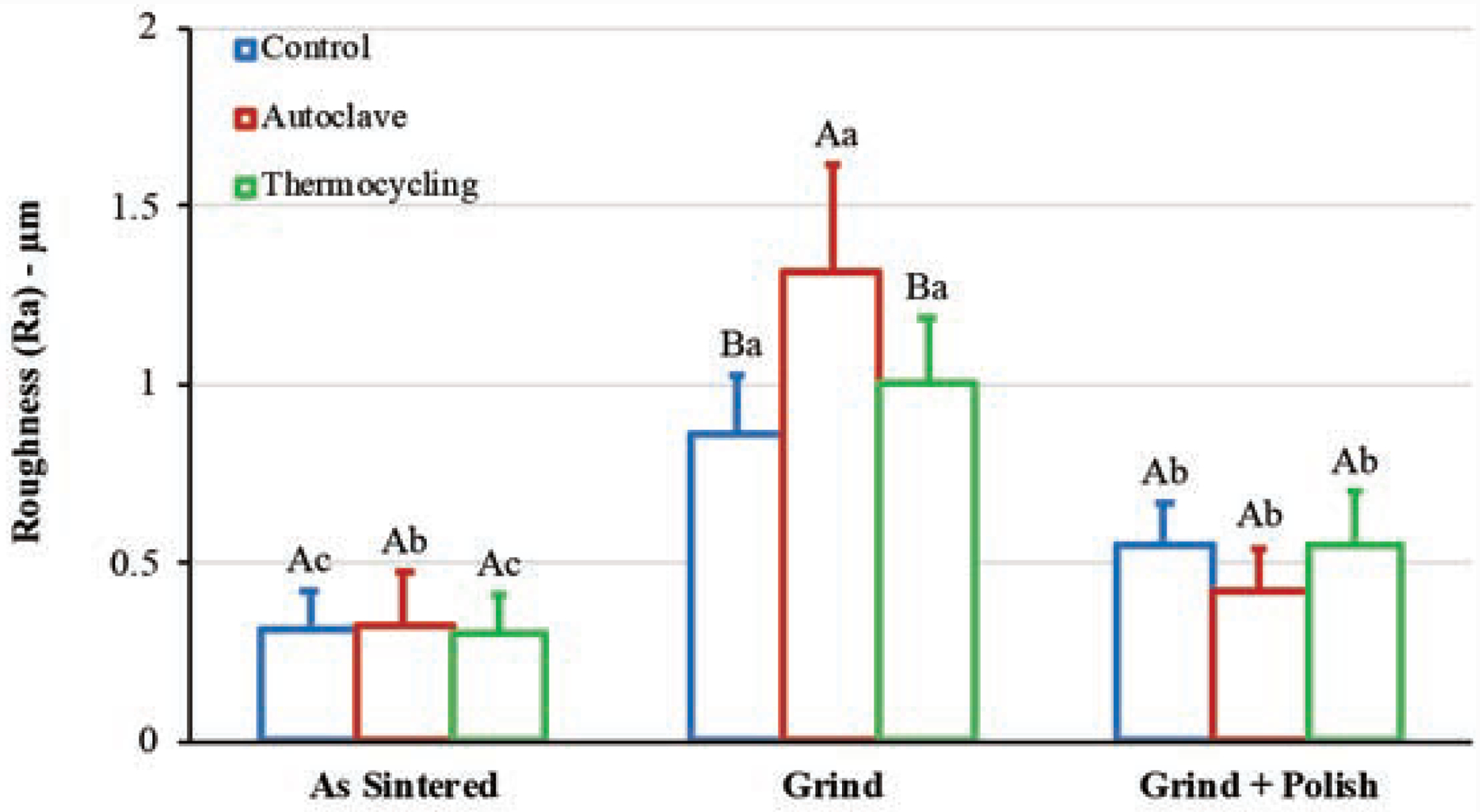
Mean and standard deviations of roughness (Ra, in μm) Distinct capital letters indicate statistically significant differences between aging methods for the same surface treatment. Distinct lowercase letters indicate statistically significant differences between surface treatments for the same aging method.
For the biaxial flexural test, there was statistical significance for factors surface treatment (p <0.001) and aging (p <0.001), while the double interaction surface treatment × aging (p = 0.239) was not statistically significant. Regarding surface treatment, pooled means of biaxial flexural strength (MPa) were: As Sintered = 775 (190)B; Grind = 1078 (235)A; Grind + Polish = 1129 (139)A. For the aging factor, pooled means of biaxial flexural strength (MPa) were: Baseline = 1149 (232)A; Autoclave = 939 (211)B; Thermocycling = 916 (230)B. Means and standard deviations of all groups are presented in Figure 2.
Figure 2:
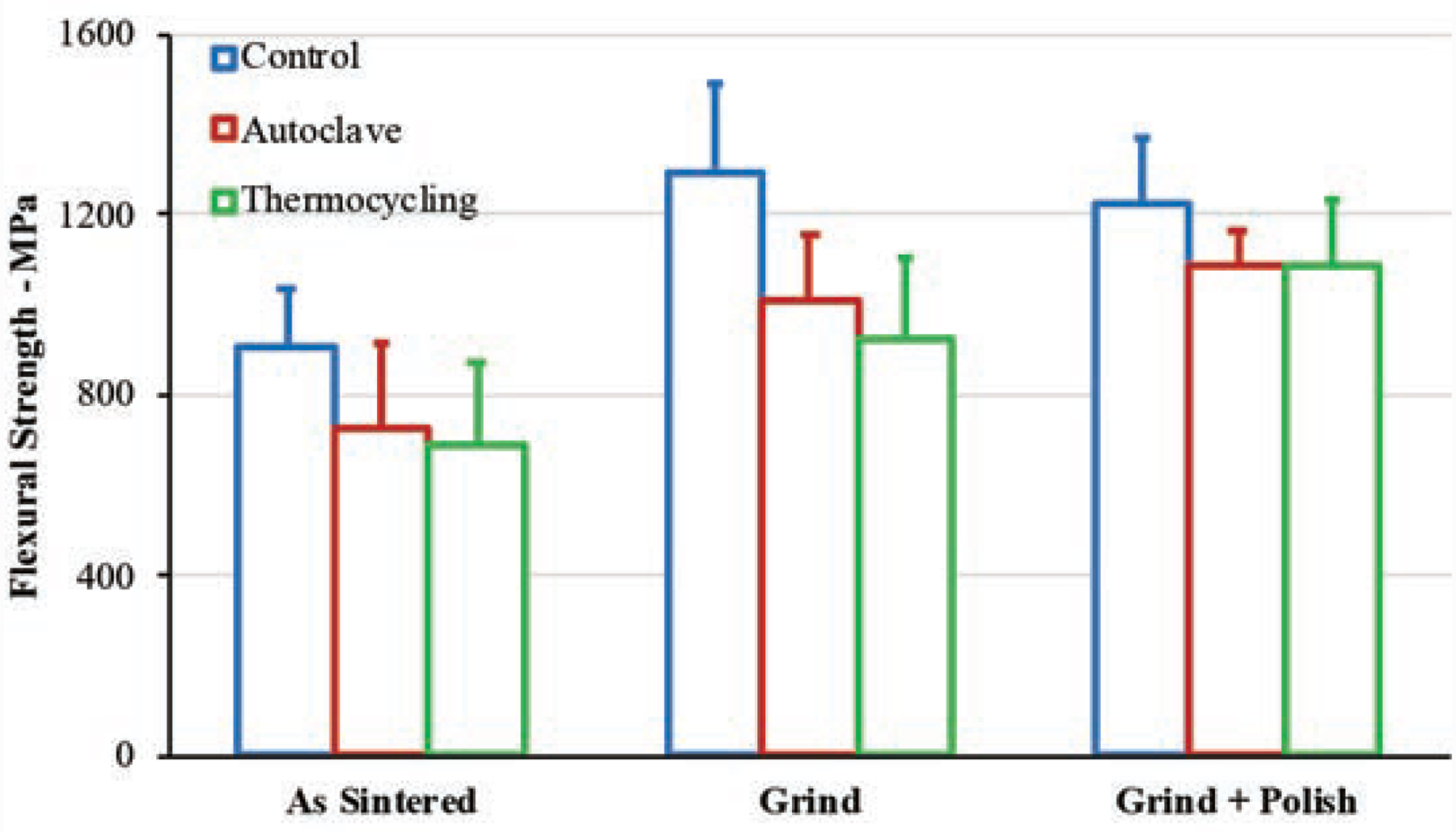
Means and standard deviations of biaxial flexural strength (MPa).
The results of the correlation analysis between flexural strength and roughness are presented in Figure 3. A weak positive correlation is observed when all groups are analyzed and a strong positive correlation when only the baseline groups (without aging) are analyzed However, none of the conditions had statistical significance (p >0.05), indicating the presence of confounding factors not considered in the analysis.
Figure 3:
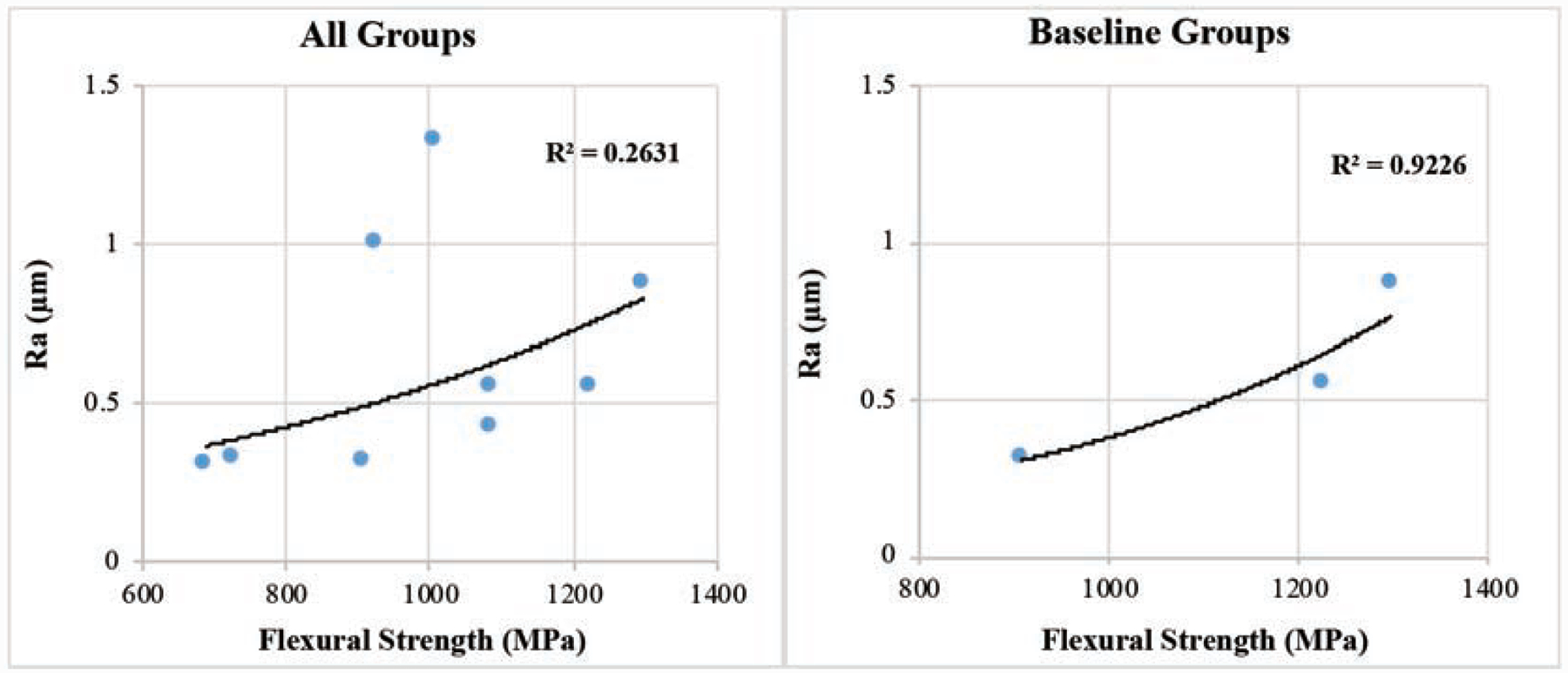
Exponential correlation between flexural strength and roughness for (A) all groups and (B) for Baseline groups only (no aging).
Table 2 shows the means and standard deviations for roughness and biaxial flexural strength for each group, as well as the monoclinic phase volumetric fraction associated with each condition (surface treatment / aging).
Table 2:
Mean (standard deviation) of roughness and biaxial flexural strength and percentage of monoclinic phase for each condition.
| Surface treatment | Aging | Ra (μm) | Biaxial strength (MPa) | Monoclinic phase (vol%) |
|---|---|---|---|---|
| As Sintered | Baseline | 0.32 (0.10) | 908 (131) | < 1 |
| Autoclave | 0.33 (0.15) | 724 (188) | ~8 | |
| Thermocycling | 0.31 (0.10) | 689 (185) | ~11 | |
| Grind | Baseline | 0.87 (0.16) | 1298 (194) | ~32 |
| Autoclave | 1.32 (0.30) | 1009 (147) | ~33 | |
| Thermocycling | 1.00 (0.19) | 926 (182) | ~31 | |
| Grind + Polish | Baseline | 0.55 (0.12) | 1224 (149) | ~28 |
| Autoclave | 0.43 (0.12) | 1085 (77) | ~27 | |
| Thermocycling | 0.55 (0.15) | 1086(144) | ~28 |
The X-ray diffraction spectra shown in Figure 4 demonstrate that both surface treatments and aging methods yielded crystallographic changes in the tested zirconia. Tetragonal to monoclinic phase transformation is visible in all treated groups by the presence of the monoclinic peak at 28° 2θ. This transformation occurred by two processes: (1) akin transformation-toughening, surface treatments introduce mechanical stresses that lead to phase transformation; and (2) both aging methods have yielded low temperature degradation (LTD), whereby, in the presence of moisture and heat, spontaneous transformation from tetragonal to monoclinic phase occurs. Moreover, an enlargement of the base of the tetragonal peak 30° 2θ is observed in the surface treated groups, indicating plastic deformation of the crystalline lattice due to the presence of stress.
Figure 4:
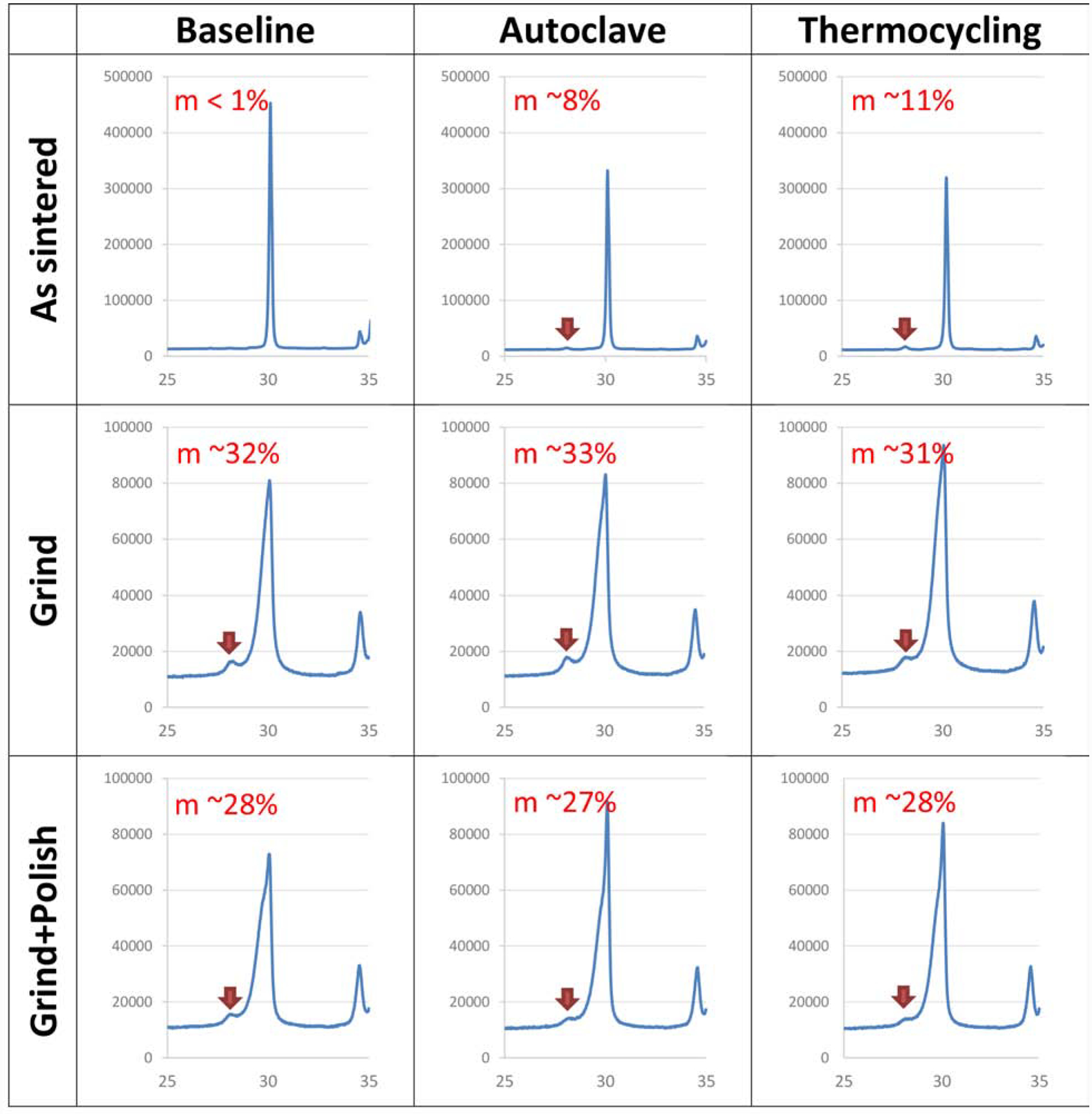
X-ray diffraction (XRD) spectra evaluating 2θ angles between 26° to 34° with relative intensity for all groups evaluated.
Qualitative analysis of surface topography by SEM imaging (Figure 5) showed that grinding with diamond burs changed the zirconia topographic pattern by introducing marked surface defects, following a major direction with some lateral projections. After the rubber polishing sequence, it was observed that the surface defects were significantly reduced, both in length and depth, showing a smoother surface than that obtained after using only diamond burs. Aging in both autoclave and thermocycling caused no noticeable surface change, regardless of surface treatment.
Figure 5:
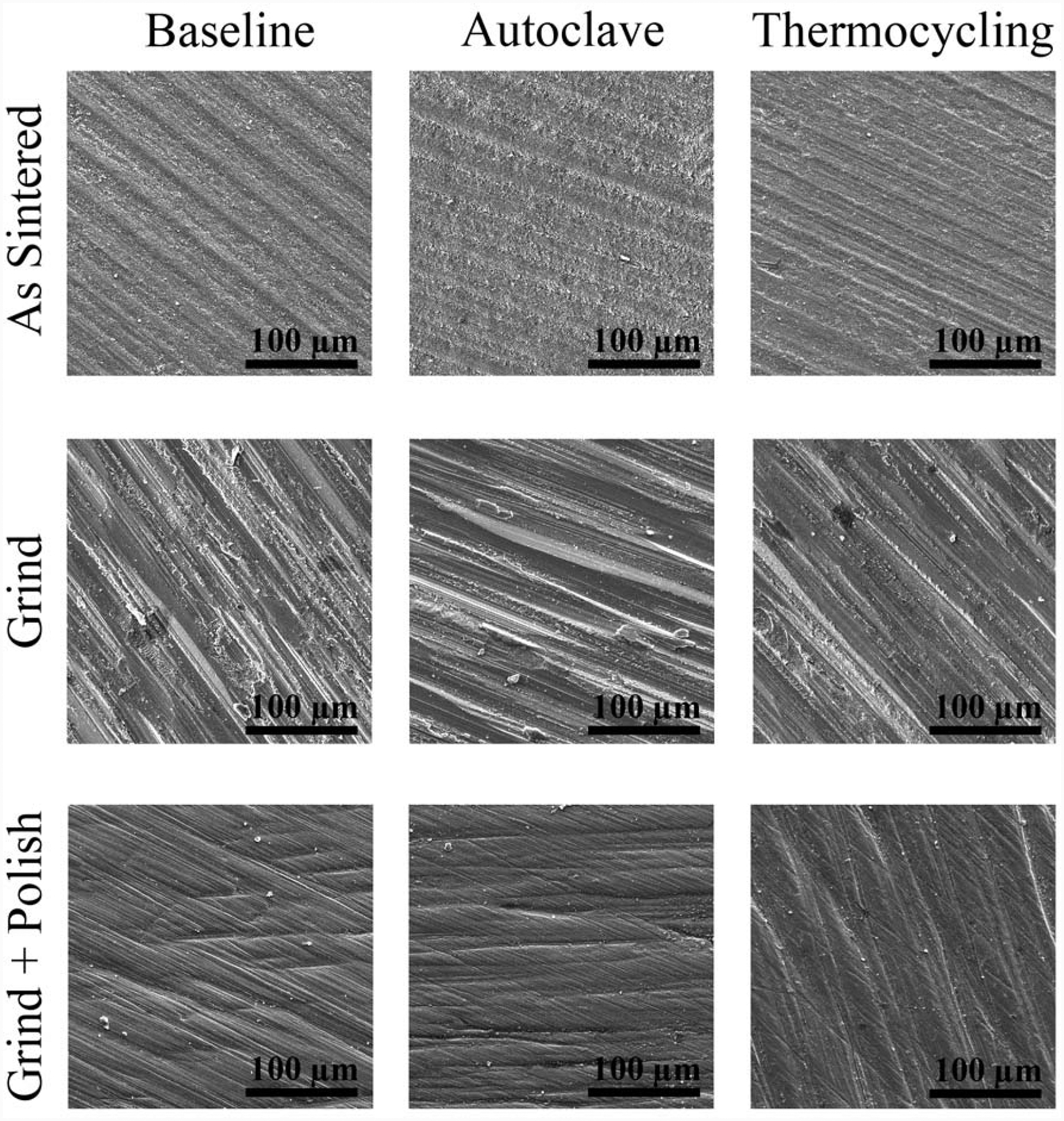
SEM images (1000 times magnification), showing the surface characteristics and topography of the evaluated groups, as a function of surface treatment and aging method.
Figure 6 shows two representative fields of the As Sintered group, without aging, showing the microstructural characteristics of the evaluated zirconia. It can be seen that the material presents densely sintered grains with evenly distributed grain size.
Figure 6:
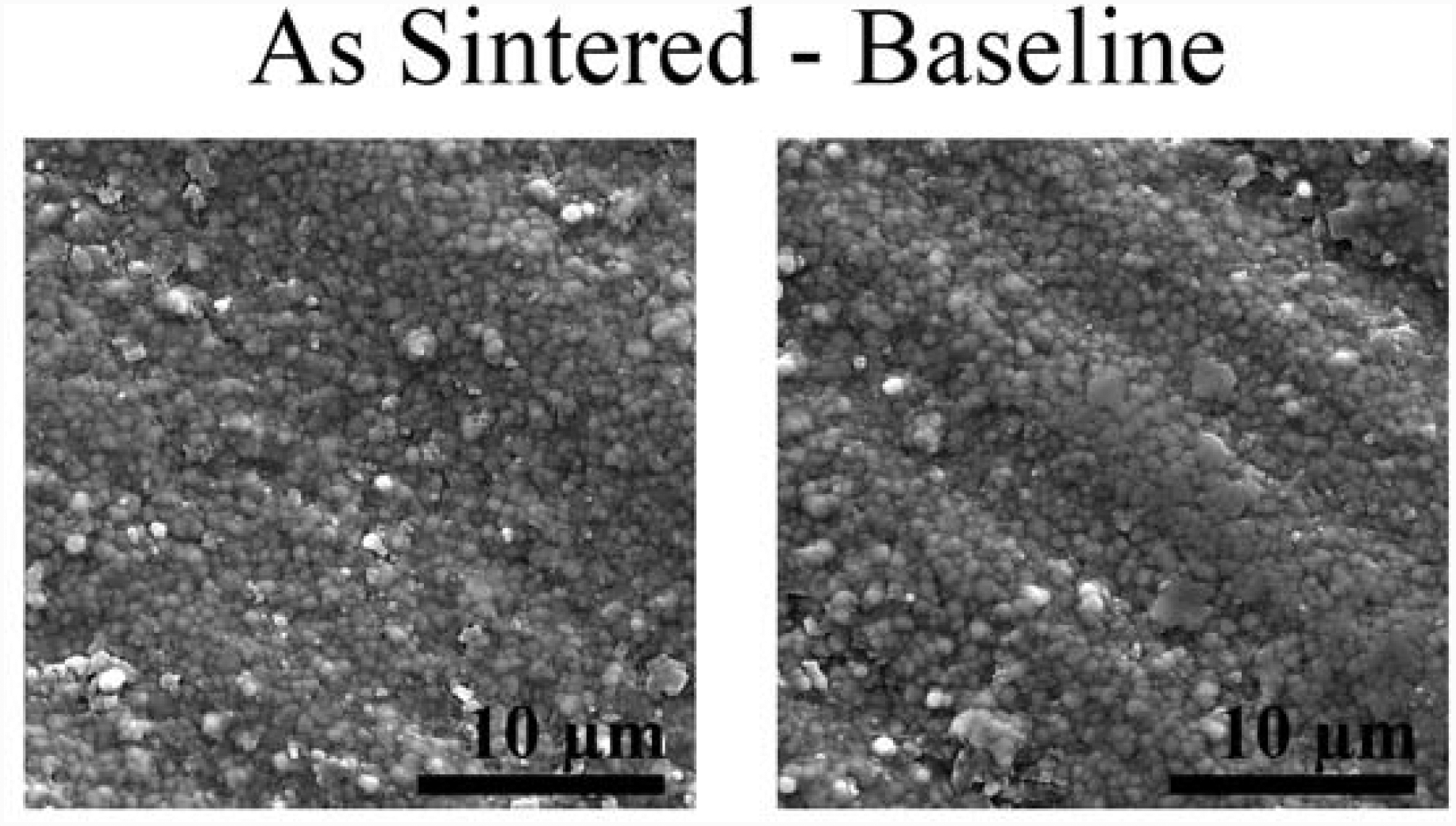
SEM images (5000 times magnification) of As Sintered Baseline specimens (without aging), showing the evaluated zirconia microstructure.
4. DISCUSSION
Zirconia is the most versatile ceramic material for use in indirect dental restorations, as it has a variety of levels of mechanical strength and translucency [5, 6, 8], allowing it to be used for applications from infrastructures to aesthetic monolithic restorations [1, 2]. Similar to other dental ceramics, zirconia is sensitive to surface defects that can be introduced at various stages of the rehabilitation process [22, 24]. These aspects motivate the present study, which demonstrates that the mechanical strength of a monolithic zirconia results from a complex balance between surface defect population and modifications on surface crystalline structure introduced by grinding and polishing procedures and low temperature degradation. This is particularly important in zirconias with similar composition to the one used herein, an alumina-free 3 mol% yttria-stabilized zirconia, with high pre-sintered density. The predominant tetragonal crystalline structure makes the material susceptible to tetragonal to monoclinic phase transformation and the discussed consequences of that. Distinctively, the cubic-containing translucent zirconias are generally more stable, meaning: neither very capable of undergoing transformation toughening, nor very susceptible to LTD [1, 3–8].
The first hypothesis of this study, that different clinically relevant methods for zirconia grinding and polishing influence the structural integrity of this material, was accepted. Significant effects were observed on both roughness (Fig 1) and on the flexural strength (Fig 2) of the specimens that went through grinding (Grind) and grinding + polishing (Grind + Polish). The use of diamond burs in the superficial grinding of zirconia restorations is required for adjustments of the piece at the internal, proximal, and emergence profile areas during the fitting tests, as well as for occlusal adjustments after the restoration is cemented. High roughness in these areas can lead to poor clinical performance, namely: (i) patient discomfort due to roughness; (ii) biofilm accumulation in the cervical region, which increases the risk of caries and periodontal disease; (iii) cervical margin fractures due to the presence of hoop stresses in this region; (iv) radial fracture at the intaglio surface of the restoration due to the occurrence of occlusal loading induced flexural stresses; (v) excessive wear of antagonist enamel; and (vi) crack propagation caused by repetitive contact fatigue in chewing function [10, 16, 32–37].
It is therefore crucial to emphasize that the use of fine and extra fine diamond burs should be preferred by dentists and dental technicians, as the present study shows that the surface defects introduced by medium grain diamond burs used under low-speed were not completely removed after standard polishing (Fig 4). Surface roughness (Fig 1) was reduced by polishing but did not reach the same level of initial smoothness (As Sintered). It is known that the coarser the diamond bur used to grind the ceramic surface, the greater the resulting surface roughness [22, 24]. A systematic review of the literature [25] assessing the effect of grinding on Y-TZP mechanical properties, structural stability and surface characteristics, showed that grinding generally decreased the flexural strength and increased roughness of Y-TZP ceramic. However, the use of equipment that allows better grinding accuracy (low-speed + fine grained burs) seem to be the major factors in reducing the introduction of defects and allowing the occurrence of toughening mechanism, minimizing the occurrence of degradation of the mechanical properties of zirconia. In addition, compared to other surface finish forms such as glaze, polishing is the most appropriate surface treatment for zirconia and is considered mandatory [38]. In this sense, there is still much room for the development of new polishing systems with greater efficiency in zirconia [27].
Surface roughness plays a crucial role in ceramic strength, and generally has a significant negative correlation with flexural strength; the greater the roughness, the larger the surface defects and, consequently, the lower the fracture strength of the ceramic [16]. However, when the material in question is zirconia, the interpretation of the effect of surface roughness is not as simple, as observed in the correlation analysis between roughness and fracture strength in this study: a strong positive correlation was observed between these properties in the Baseline groups (without aging). Zirconia, when subjected to mechanical stresses, such as crack propagation or grinding and polishing, undergoes transformation from tetragonal to monoclinic phase, which is accompanied by a volumetric expansion of the grains of 3 to 5%, generating compressive stresses in the transformed area. These compressive stresses hinder crack propagation, absorbing part of the energy required for crack growth and, consequently, increasing the fracture toughness of zirconia [39–41]. Such effect is corroborated by the X-ray diffraction results of this study, which showed, in addition to the monoclinic peak (28° 2θ), the widening of the tetragonal peak (30° 2θ) for the surface treated groups, indicating plastic deformation of the crystal lattice of zirconia. When a balance is reached between the depth of surface defects introduced by grinding / polishing and the compressive stresses generated by zirconia phase transformation, the material has high fracture resistance, as observed in this study. At baseline, surface treatments yielded phase transformation that resulted in surface compressive stresses and, consequently, resulting in greater flexural strength compared to the As Sintered group, despite the also greater roughness yielded by surface treatments. Similar results with increased biaxial flexural strength for groups with higher roughness have been reported in the literature [24].
In addition to surface treatments, the effect of two aging methods on the structural stability of zirconia was investigated. The second hypothesis that aging would result in structural degradation of zirconia was also accepted. Autoclave aging yielded higher roughness than baseline (without aging), while fracture resistance was compromised by both aging methods compared to baseline. One of the main limitations of zirconia is known to be its susceptibility to low temperature degradation (LTD). This phenomenon occurs when the material is exposed to moisture and heat for long periods of time, leading to progressive transformation from tetragonal to monoclinic phase and consequent introduction of microcracks in the transformed area, which results in increased roughness and decreased mechanical properties [20–24]. The literature, however, presents conflicting results regarding the effect of hydrothermal aging on fracture resistance and other properties of zirconia. This phenomenon seems to be material dependent, since Flinn et al (2017) [42] report that fracture resistance decreased markedly or remained unchanged depending on the brand of zirconia used. Other studies have not shown deleterious effects of hydrothermal aging on the flexural strength of zirconia [43, 44]. In this study, the fraction of monoclinic phase on the surface increased after aging for the As Sintered group, while remained similarly high for surface treated groups before and after aging. It is important to highlight that XRD has limited surface penetration, thus the in-depth transformation, which explains the strength degradation, was not accounted for in the phase fraction analyses. As discussed earlier, the effect of phase transformation on the mechanical properties of zirconia depends on the balance between the depth of surface defects and compressive stresses introduced by phase transformation – from both mechanical stresses and LTD.
Another interesting result of the present study is the similar aging effect observed by autoclave and thermocycling. The authors acknowledge that thermocycling is far more time consuming than autoclave, which still is the best accelerated hydrothermal aging method to evaluate zirconia phase transformation. However, thermocycling is the preferred artificial aging method used in studies about bonding properties of zirconia [45, 46]. The explicit results of the present study, along with a previous study [46], showing LTD of zirconia caused by thermocycling indicate the formation of micro-defects that grow progressively into the subsurface of the material. Therefore, one must notice there is a poorly explored research question here: How the surface degradation yielded by LTD affect the zirconia bonding properties over time?
Finally, it should be emphasized that it is essential that dentists and technicians be thoughtful when working with zirconia restorations, as surface treatment during the fitting and adjustment phases, before and after cementation, may affect zirconia’s monoclinic phase content, roughness, mechanical properties and wear of antagonist enamel. The use of zirconia with better optical properties and greater resistance to hydrothermal aging may also improve long-term clinical performance of monolithic zirconia restorations.
5. CONCLUSION
Clinically relevant grinding and polishing procedures can potentially be deleterious to the surface quality of monolithic zirconia restorations, while introducing crystalline phase transformation that may result in a toughening effect. Nonetheless, when zirconia is exposed to hydrothermal aging at low temperatures, which can be similarly induced by the traditional autoclave method or by thermocycling method, further degradation of surface quality may result in a compromise of its mechanical properties.
ACKNOWLEDGMENTS
The authors would like to thank Camila Rodrigues for the help with the XRD analyses; Cibele Almeida Kintopp and José Alexandre de Campos for the help with the preparation of the specimens. This work was partially supported by the National Institutes of Health/National Institute of Dental and Craniofacial Research (grants R01DE026772, R01DE026279, and R01DE017925). The authors declare no potential conflicts of interest with respect to the authorship and/or publication of this article.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Declaration of interests
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
REFERENCES
- [1].Zhang Y, Lawn BR, Novel Zirconia Materials in Dentistry, Journal of dental research, 97 (2018) 140–147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Zhang Y, Kelly JR, Dental Ceramics for Restoration and Metal Veneering, Dent Clin North Am, 61 (2017) 797–819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Zhang Y, Lee JJ, Srikanth R, Lawn BR, Edge chipping and flexural resistance of monolithic ceramics, Dental materials : official publication of the Academy of Dental Materials, 29 (2013) 1201–1208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Zhang Y, Lawn BR, Evaluating dental zirconia, Dental materials : official publication of the Academy of Dental Materials, 35 (2019) 15–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Yan J, Kaizer MR, Zhang Y, Load-bearing capacity of lithium disilicate and ultra-translucent zirconias, Journal of the mechanical behavior of biomedical materials, 88 (2018) 170–175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Tong H, Tanaka CB, Kaizer MR, Zhang Y, Characterization of three commercial Y-TZP ceramics produced for their high-translucency, high-strength and high-surface area, Ceram Int, 42 (2016) 1077–1085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Kaizer MR, Kolakarnprasert N, Rodrigues C, Chai H, Zhang Y, Probing the interfacial strength of novel multi-layer zirconias, Dental materials : official publication of the Academy of Dental Materials, 36 (2020) 60–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Kolakarnprasert N, Kaizer MR, Kim DK, Zhang Y, New multi-layered zirconias: Composition, microstructure and translucency, Dental materials : official publication of the Academy of Dental Materials, 35 (2019) 797–806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Koenig V, Vanheusden AJ, Le Goff SO, Mainjot AK, Clinical risk factors related to failures with zirconia-based restorations: an up to 9-year retrospective study, Journal of dentistry, 41 (2013) 1164–1174. [DOI] [PubMed] [Google Scholar]
- [10].Pang Z, Chughtai A, Sailer I, Zhang Y, A fractographic study of clinically retrieved zirconia-ceramic and metal-ceramic fixed dental prostheses, Dental materials : official publication of the Academy of Dental Materials, 31 (2015) 1198–1206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Pjetursson BE, Sailer I, Zwahlen M, Hammerle CH, A systematic review of the survival and complication rates of all-ceramic and metal-ceramic reconstructions after an observation period of at least 3 years Part I: Single crowns, Clin Oral Implants Res, 18 Suppl 3 (2007) 73–85. [DOI] [PubMed] [Google Scholar]
- [12].Sailer I, Pjetursson BE, Zwahlen M, Hammerle CH, A systematic review of the survival and complication rates of all-ceramic and metal-ceramic reconstructions after an observation period of at least 3 years Part II: Fixed dental prostheses, Clin Oral Implants Res, 18 Suppl 3 (2007) 86–96. [DOI] [PubMed] [Google Scholar]
- [13].Sailer I, Makarov NA, Thoma DS, Zwahlen M, Pjetursson BE, All-ceramic or metal-ceramic tooth-supported fixed dental prostheses (FDPs)? A systematic review of the survival and complication rates Part I: Single crowns (SCs), Dental materials : official publication of the Academy of Dental Materials, 31 (2015) 603–623. [DOI] [PubMed] [Google Scholar]
- [14].Swain MV, Unstable cracking (chipping) of veneering porcelain on all-ceramic dental crowns and fixed partial dentures, Acta biomaterialia, 5 (2009) 1668–1677. [DOI] [PubMed] [Google Scholar]
- [15].Kaizer MR, Gierthmuehlen PC, Dos Santos MB, Cava SS, Zhang Y, Speed sintering translucent zirconia for chairside one-visit dental restorations: Optical, mechanical, and wear characteristics, Ceram Int, 43 (2017) 10999–11005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Lohbauer U, Reich S, Antagonist wear of monolithic zirconia crowns after 2 years, Clin Oral Investig, 21 (2017) 1165–1172. [DOI] [PubMed] [Google Scholar]
- [17].Yuan K, Wang F, Gao J, Sun X, Deng ZX, Wang H, Jin L, Chen JH, Effect of zircon-based tricolor pigments on the color, microstructure, flexural strength and translucency of a novel dental lithium disilicate glass-ceramic, J Biomed Mater Res B Appl Biomater, 102 (2014) 98–107. [DOI] [PubMed] [Google Scholar]
- [18].Chevalier J, What future for zirconia as a biomaterial?, Biomaterials, 27 (2006) 535–543 [DOI] [PubMed] [Google Scholar]
- [19].J Chevalier B Cales, J M Drouin, Low-temperature aging of Y-TZP ceramics, J Am Ceram Soc, 82 (1999) 2150–2154. [Google Scholar]
- [20].K Kobayashi H Kuwajima, T Masaki, Phase-Change and Mechanical-Properties of Zro2-Y2o3 Solid Electrolyte after Aging, Solid State Ionics, 3–4 (1981) 489–493. [Google Scholar]
- [21].Pereira GKR, Venturini AB, Silvestri T, Dapieve KS, Montagner AF, Soares FZM, Valandro LF, Low-temperature degradation of Y-TZP ceramics: A systematic review and meta-analysis, Journal of the mechanical behavior of biomedical materials, 55 (2015) 151–163. [DOI] [PubMed] [Google Scholar]
- [22].Pereira GK, Silvestri T, Camargo R, Rippe MP, Amaral M, Kleverlaan CJ, Valandro LF, Mechanical behavior of a Y-TZP ceramic for monolithic restorations: effect of grinding and low-temperature aging, Mater Sci Eng C Mater Biol Appl, 63 (2016) 70–77. [DOI] [PubMed] [Google Scholar]
- [23].Pereira GKR, Muller C, Wandscher VF, Rippe MP, Kleverlaan CJ, Valandro LF, Comparison of different low-temperature aging protocols: its effects on the mechanical behavior of Y-TZP ceramics, Journal of the mechanical behavior of biomedical materials, 60 (2016) 324–330 [DOI] [PubMed] [Google Scholar]
- [24].Guilardi LF, Pereira GKR, Gundel A, Rippe MP, Valandro LF, Surface micro-morphology, phase transformation, and mechanical reliability of ground and aged monolithic zirconia ceramic, Journal of the mechanical behavior of biomedical materials, 65 (2017) 849–856. [DOI] [PubMed] [Google Scholar]
- [25].Pereira GKR, Fraga S, Montagner AF, Soares FZM, Kleverlaan CJ, Valandro LF, The effect of grinding on the mechanical behavior of Y-TZP ceramics: A systematic review and meta-analyses, Journal of the mechanical behavior of biomedical materials, 63 (2016) 417–442. [DOI] [PubMed] [Google Scholar]
- [26].Preis V, Grumser K, Schneider-Feyrer S, Behr M, Rosentritt M, The effectiveness of polishing kits: influence on surface roughness of zirconia, The International journal of prosthodontics, 28 (2015) 149–151. [DOI] [PubMed] [Google Scholar]
- [27].Al-Haj Husain N, Camilleri J, Ozcan M, Effect of polishing instruments and polishing regimens on surface topography and phase transformation of monolithic zirconia: An evaluation with XPS and XRD analysis, Journal of the mechanical behavior of biomedical materials, 64 (2016) 104–112. [DOI] [PubMed] [Google Scholar]
- [28].Gale MS, Darvell BW, Thermal cycling procedures for laboratory testing of dental restorations, Journal of dentistry, 27 (1999) 89–99. [DOI] [PubMed] [Google Scholar]
- [29].ISO 6872, Dentistry -- Ceramic materials, International Organization for Standardization; (2015), pp 1–28, (2015). [Google Scholar]
- [30].Garvie RC, Nicholson PS, Phase Analysis in Zirconia Systems, J Am Ceram Soc, 55 (1972) 303–305. [Google Scholar]
- [31].Toraya YMH, Somiya S, Calibration curve for quatitative analysis of monoclinic-tetragonal ZrO2 systems, Journal of American Ceramic Society 1984;67:C199–221. [Google Scholar]
- [32].Bollen CM, Lambrechts P, Quirynen M, Comparison of surface roughness of oral hard materials to the threshold surface roughness for bacterial plaque retention: a review of the literature, Dental materials : official publication of the Academy of Dental Materials, 13 (1997) 258–269. [DOI] [PubMed] [Google Scholar]
- [33].Esquivel-Upshaw JF, Rose WF Jr, Barrett AA, Oliveira ER, Yang MC, Clark AE, Anusavice KJ, Three years in vivo wear: core-ceramic, veneers, and enamel antagonists, Dental materials : official publication of the Academy of Dental Materials, 28 (2012) 615–621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Jones CS, Billington RW, Pearson GJ, The in vivo perception of roughness of restorations, Br Dent J, 196 (2004) 42–45; discussion 31. [DOI] [PubMed] [Google Scholar]
- [35].Oilo M, Quinn GD, Fracture origins in twenty-two dental alumina crowns, Journal of the mechanical behavior of biomedical materials, 53 (2016) 93–103. [DOI] [PubMed] [Google Scholar]
- [36].Ren L, Zhang Y, Sliding contact fracture of dental ceramics: Principles and validation, Acta biomaterialia, 10 (2014) 3243–3253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Zhang Y, Sailer I, Lawn BR, Fatigue of dental ceramics, Journal of dentistry, 41 (2013) 1135–1147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Zucuni CP, Guilardi LF, Rippe MP, Pereira GKR, Valandro LF, Polishing of Ground Y-TZP Ceramic is Mandatory for Improving the Mechanical Behavior, Brazilian dental journal, 29 (2018) 483–491 [DOI] [PubMed] [Google Scholar]
- [39].Flury S, Peutzfeldt A, Lussi A, The effect of polymerization procedure on Vickers hardness of dual-curing resin cements, Am J Dent, 24 (2011) 226–232. [PubMed] [Google Scholar]
- [40].Guazzato M, Albakry M, Ringer SP, Swain MV, Strength, fracture toughness and microstructure of a selection of all-ceramic materials Part II Zirconia-based dental ceramics, Dental materials : official publication of the Academy of Dental Materials, 20 (2004) 449–456. [DOI] [PubMed] [Google Scholar]
- [41].Kelly JR, Dental ceramics: current thinking and trends, Dent Clin North Am, 48 (2004) viii, 513–530. [DOI] [PubMed] [Google Scholar]
- [42].Flinn BD, Raigrodski AJ, Mancl LA, Toivola R, Kuykendall T, Influence of aging on flexural strength of translucent zirconia for monolithic restorations, J Prosthet Dent, 117 (2017) 303–309. [DOI] [PubMed] [Google Scholar]
- [43].De Souza GM, Zykus A, Ghahnavyeh RR, Lawrence SK, Bahr DF, Effect of accelerated aging on dental zirconia-based materials, Journal of the mechanical behavior of biomedical materials, 65 (2017) 256–263. [DOI] [PubMed] [Google Scholar]
- [44].Nam MG, Park MG, Changes in the flexural strength of translucent zirconia due to glazing and low-temperature degradation, J Prosthet Dent, 120 (2018) 969 e961–969 e966. [DOI] [PubMed] [Google Scholar]
- [45].Chai H, Kaizer M, Chughtai A, Tong H, Tanaka C, Zhang Y, On the interfacial fracture resistance of resin-bonded zirconia and glass-infiltrated graded zirconia, Dental materials : official publication of the Academy of Dental Materials, 31 (2015) 1304–1311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [46].Ramos NC, Kaizer MR, Campos TMB, Kim J, Zhang Y, Melo RM, Silica-Based Infiltrations for Enhanced Zirconia-Resin Interface Toughness, Journal of dental research, 98 (2019) 423–429. [DOI] [PMC free article] [PubMed] [Google Scholar]


