Abstract
Objective
The COVID-19 pandemic has placed health care workers under psychological stress. Previous reviews show a high prevalence of mental disorders among health care workers, but these need updating and inclusion of studies written in Chinese. The aim of this systematic review and meta-analysis was to provide updated prevalence estimates for depression, anxiety and post-traumatic stress disorder (PTSD) among health care workers during the COVID-19 pandemic, benefitting from the inclusion of studies published in Chinese.
Methods
Systematic search of EMBASE, MEDLINE, PsycINFO, Global Health, Web of Science, CINAHL, Google Scholar and the Chinese databases SinoMed, WanfangMed, CNKI and CQVIP, for studies conducted between December 2019 and August 2020 on the prevalence of depression, anxiety and PTSD in health care workers during the COVID-19 pandemic. Studies published in both English and Chinese were included.
Results
Data on the prevalence of moderate depression, anxiety and PTSD was pooled across 65 studies involving 97,333 health care workers across 21 countries. The pooled prevalence of depression was 21.7% (95% CI, 18.3%-25.2%), of anxiety 22.1% (95% CI, 18.2%-26.3%), and of PTSD 21.5% (95% CI, 10.5%-34.9%). Prevalence estimates are also provided for a mild classification of each disorder. Pooled prevalence estimates of depression and anxiety were highest in studies conducted in the Middle-East (34.6%; 28.9%). Subgroup and meta-regression analyses were conducted across covariates, including sampling method and outcome measure.
Conclusions
This systematic review and meta-analysis has identified a high prevalence of moderate depression, anxiety and PTSD among health care workers during the COVID-19 pandemic. Appropriate support is urgently needed. The response would benefit from additional research on which interventions are effective at mitigating these risks.
Introduction
In December 2019, China experienced the first outbreak of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), a highly infectious virus causing the coronavirus disease 2019 (COVID-19). In March 2020, the World Health Organization (WHO) declared this outbreak a global pandemic [1]. As of 21 December 2020, there have been over 76 million documented cases of COVID-19, and over 1.6 million deaths [2].
Coronaviruses are a family of viruses that typically cause serious and sometimes fatal respiratory tract infections, and compared to others, SARS-CoV-2 spreads quickly. The reproductive rate (i.e. number of infected generated by one infected individual, on average) for SARS-CoV-2 is estimated at 2.5, compared with 0.9 for the Middle-East respiratory syndrome coronavirus (MERS-CoV), and 1.5 for the influenza pandemic of 2009 [3]. With SARS-CoV-2 spreading rapidly, health systems across the globe have faced unprecedented challenges in resourcing a health care response [4]. Health care workers have reported inadequate training on infection prevention and control, and there are widespread shortages of personal protective equipment (PPE). These challenges resulted in high rates of COVID-19 among health care workers, especially in the early stages of the pandemic [5–7]. Fears for personal safety, high workload (particularly for those treating infected patients) and limited support may have contributed to fatigue, burnout and stress among health care workers [6]. Although separate constructs, burnout and stress are associated with co-morbid and future psychological outcomes, including common mental disorders, such as depression and anxiety, through various social and biological mechanisms [8–12].
Evidence from previous viral epidemics and initial findings from the COVID-19 pandemic highlight the psychological impact on health care workers [13–15]. The estimated prevalence of depression and anxiety among health care workers was 25% (95% CI, 17%-33%) and 26% (95% CI, 18%-34%), respectively, in a recent systematic review of 19 studies focussed on COVID-19 [16]. In another rapid systematic review, including 29 studies, the median prevalence of anxiety was 24%, and of depression 21% [13]. Comparing these estimates with those from the WHO on common mental disorders among the global population, at 4.4% for depression and 3.6% for anxiety disorders (including PTSD), highlights the substantial impact of the COVID-19 pandemic on the psychological wellbeing of health care workers [17].
Reliable, comprehensive estimates of mental health disorders among health care workers during the COVID-19 pandemic are needed to inform prevention and treatment initiatives. The existing estimates are important, but they need updating. Furthermore, substantial research has been conducted in China, as they were the first country to see an outbreak of COVID-19 and have an active academic community. However, much of this evidence is published in Chinese and stored on Chinese bibliographic databases, and is missed by existing reviews. As noted by Xiang et al., it is imperative that this language barrier does not impede dissemination of findings that will benefit of health professionals and policy makers during this pandemic [18].
In this systematic review and meta-analysis, we aimed to provide updated estimates of the prevalence of depression, anxiety and post-traumatic stress disorder (PTSD) among health care workers during the COVID-19 pandemic, including research published in Chinese.
Methods
This systematic review was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines [19]. The protocol for the review was registered in the PROSPERO International Prospective Register of Systematic Reviews in May 2020 (ID: CRD42020187314).
Search strategy
Articles were retrieved through a systematic search of EMBASE, MEDLINE, PsycINFO, Global Health, Web of Science, Google Scholar and CINAHL, as well as the Chinese databases SinoMed, WanfangMed, CNKI and CQVIP. The reference lists of included studies were searched for additional articles and previous meta-analyses were explored for studies not identified in our search.
Search terms combined items on mental health (depression, anxiety, PTSD), health care workers and COVID-19 (S1 Appendix).
Inclusion and exclusion criteria
Studies were included if they met the following criteria: (1) published in English or Chinese since the outbreak of COVID-19 in December 2019; (2) report on depression, anxiety or PTSD among health care workers (both clinical and support) in a country affected by COVID-19; (3) used an established assessment of depression, anxiety or PTSD, through either a self-report screening tool or diagnostic interview; (4) provided sufficient information to calculate prevalence of depression, anxiety or PTSD among health care workers (e.g. percentage or sample size and number). We excluded qualitative studies, study protocols and review articles. We did not limit our inclusion to peer-reviewed articles only, and included research letters, briefs and academic preprints stored on servers such as bioRxiv and medRxiv.
Study selection
The author YL screened all titles and abstracts against the selection criteria, of which 10% were independently screened by author HK. There was 97% agreement between reviewers. When the relevance of the title and abstract was unclear, reviewers consulted the full text. Full texts of selected studies were reviewed by YL and HK, and disagreements on inclusion were discussed until a consensus was reached.
Data extraction
The following data was extracted from included studies, with use of a standardised form: (1) Study details: country, setting, study design, sampling technique, sample size, response rate; (2) Participant characteristics: gender, age, occupation, proportion of health care workers in direct contact with patients infected with COVID-19; (3) Outcome: diagnostic method or screening tool used, reported prevalence of depression, anxiety and PTSD, prevalence estimates at different thresholds of symptom severity. Data was extracted by author YL and reviewed by NS.
Quality assessment
All included studies were cross-sectional, and were assessed for risk of bias using the tool from Agarwal et al. ‘Risk of Bias in Cross-Sectional Surveys of Attitudes and Practices’, developed as based on existing tools and response options for observational studies, and used widely [20]. Through this tool, risk of bias was assessed across five domains: (1) Is the source population representative of the population of interest? (2) Is the response rate adequate? (3) Is there little missing data? (4) Is the survey clinically sensible? (5) Is there any evidence for the reliability and validity of the survey instrument?
Each item is rated on a four-point scale from “definitely yes” (low risk of bias) to “definitely no” (high risk of bias). The instrument includes examples of study design that would lead to low risk of bias, higher risk of bias (“probably yes” or “probably no”) and high risk of bias.
Data analysis
Many studies used more than one cut-off score to report the prevalence of depression, anxiety and PTSD. For the purposes of this study, and for ease of interpretation, we calculated pooled prevalence estimates at two severity levels, classifying them as follows:
Moderate depression, anxiety or PTSD: the prevalence of health care workers scoring at or above the cut-off for moderate symptomology, or the cut-off defined by the author to be clinically relevant
Mild depression, anxiety or PTSD: the prevalence of health care workers scoring at or above the cut-off for mild symptomology, or the cut-off defined by the author to be clinically relevant
Pooled prevalence estimates of depression, anxiety and PTSD were calculated by pooling estimates from each study [21]. The Freeman-Tukey double arcsine transformation was applied to stabilise variance [22]. Pooled estimates were calculated using a random-effects model (DerSimonian and Laird method) to account for expected between-study heterogeneity arising from variations in study characteristics, such as country setting, sampling method and mental health screening tool used [23]. Heterogeneity across analyses was assessed using the I2 statistic; a value of 25%, 50% and 75% represents low, medium and high heterogeneity, respectively [24]. Risk of publication bias was assessed through visual inspection of Begg’s funnel plot and Egger’s test [25, 26].
Subgroup analyses were conducted across study characteristics; geographic region, sample size, sampling method, publication status (peer-reviewed vs preprint), proportion of female participations (≤ 50% <), proportion of participants in contact with patients infected with COVID-19 (≤ 50% <) and mental health screening tool. For this review, sampling method was categorised as either random (e.g. simple random sampling, cluster sampling) or non-random (e.g. convenience sampling, voluntary response/self-selection). In each subgroup analysis, Z-tests were used to calculate statistically significant inter-group differences in estimated prevalence. To further explore sources of heterogeneity, we conducted random-effects univariate meta-regression analyses for all variables [27]. Covariates significantly associated with heterogeneity were included in a multi-variate meta-regression model. From this model, we calculated the R2 index, in order to quantify the proportion of variance explained by the included covariates. Across analyses, p<0.05 indicated statistical significance.
All analyses were conducted using Stata version 16.1., using the metaprop and metareg commands.
Results
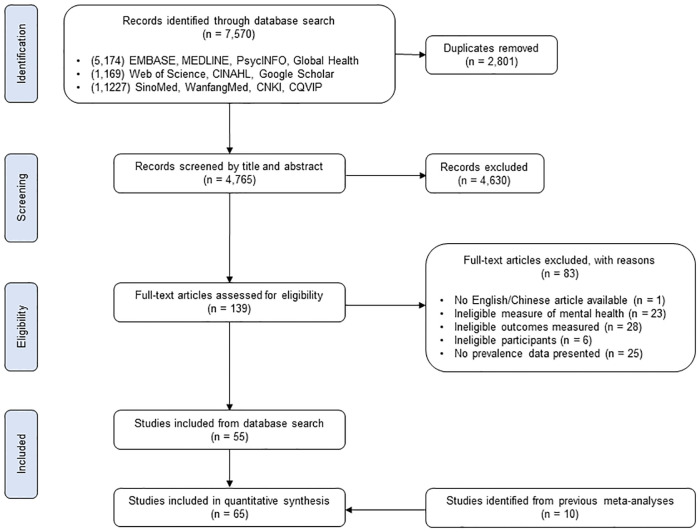
The literature search identified 7,570 articles published between 1st December 2019 and 1st August 2020, from which 2,801 duplicates were removed (Fig 1). After screening title and abstracts, 139 articles were eligible for full-text assessment, of which 55 were included [28–82]. An additional 10 articles were extracted from previous meta-analyses, which were not retrieved from the database search [83–92]. In total, 65 studies were included in the analysis. All articles were published in 2020.
Fig 1. PRISMA flowchart.
Study characteristics
97,333 health care workers across 21 countries participated in the 65 included studies (S2 Appendix). 46 of these studies were conducted in East Asia, seven in the Middle-East, five in Europe, three in South Asia, one in South America, two in North America and one in West Africa. 43 were conducted in China.
All included studies were cross-sectional in design. Five studies adopted random sampling techniques, whilst the other 60 used non-random methods (for example, self-selection through an online survey, or purposeful sampling). Studies with minimal information on sampling technique were deemed non-random.
70% of participants were female, when identified in 59 studies reporting gender demographics (involving 85,812 health care workers). 45% of participants across all studies were nurses, 27% were doctors, 11% were other medical workers (e.g. technicians, allied health professionals, pharmacists), 1% were administration and support staff, and 17% were health care workers with an undefined occupation. When reported (in 30 studies involving 37,983 participants) 37% of health care workers were in direct contact with patients infected with COVID-19.
All studies used valid self-report mental health screening tools designed to identify the presence of symptoms of common mental disorders. None of the included studies estimated prevalence via clinical diagnostic interview.
Prevalence data for each study is displayed in S3 Appendix, along with additional information on the screening tool and cut-off scores used to define symptom severity. The quality assessment, identifying risk of bias across five domains, is available in S4 Appendix.
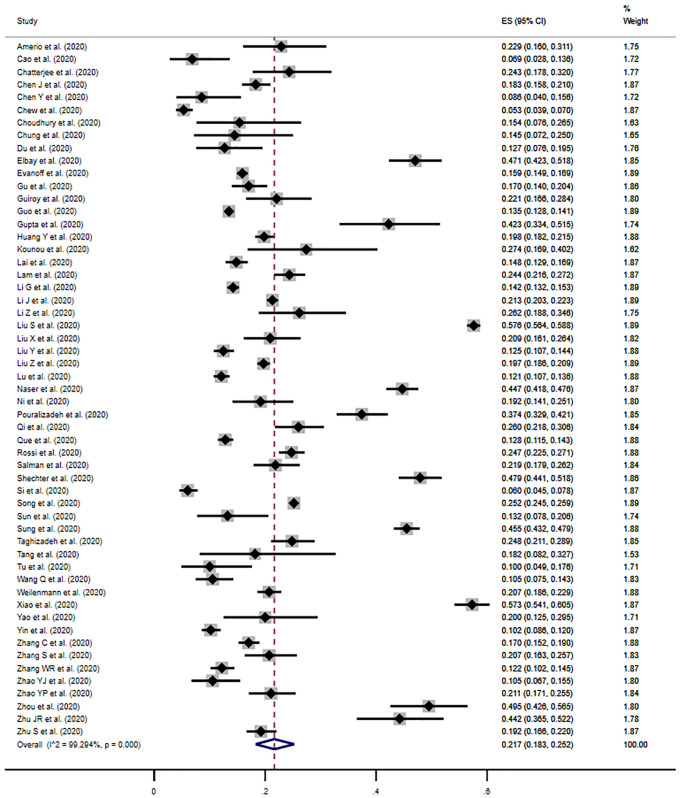
Prevalence of depression
The estimated pooled prevalence of moderate depression was 21.7% (95% CI, 18.3%-25.2%) across 55 studies, when defining depression as a score at or above the cut-off for moderate symptomology, or the cut-off deemed by the author to be clinically relevant (Fig 2). Individual study estimates ranged from 5.3% to 57.6% and there was evidence of high between-study heterogeneity (I2 = 99.3%, p<0.001). Although Begg’s funnel plot appeared slightly asymmetric, suggesting marginal bias, Egger’s test provided no evidence of publication bias (p = 0.90) (S5A Appendix).
Fig 2. Meta-analysis and pooled estimate of moderate depression in health care workers during the COVID-19 pandemic.
The pooled estimate of mild depression was 36.1% (95% CI, 31.3%-41.0%) when defining the presence of depressive symptoms as a score at or above the cut-off for mild symptomology, or that noted by the author to be clinically relevant (S5B Appendix).
Subgroup analysis and meta-regression: Depression
Prevalence estimates of moderate depression were compared between region: East Asia, South Asia, the Middle-East, Europe, North America, West Africa and South America (Table 1). The estimates of these regions significantly differed (p = 0.001). Pooled estimates were highest for studies conducted in the Middle-East (34.6%; 95% CI, 25.1%-44.9%), although relatively wide confidence intervals were present. Pooled estimates were lowest in North America (18.7%; 95% CI, 17.8%-19.7%) and East Asia (19.1%; 95% CI, 15.2%-23.4%). Pooling the estimates of the 37 studies from China only did not result in a substantially different estimate to that of all studies from East Asia.
Table 1. Subgroup analyses for studies on depression.
| Subgroup analysis | No. of studies | Prevalence % (95% CI) | I2 | Between-group difference | |
|---|---|---|---|---|---|
| Region | East Asia | 39 | 19.1 (15.2–23.4) | 99.4% | |
| Middle-East | 5 | 34.6 (25.1–44.9) | 96.6% | ||
| Europe | 4 | 22.0 (18.9–25.3) | 64.3% | ||
| South Asia | 3 | 28.8 (18.1–40.8) | -b | ||
| North America | 2a | 18.7 (17.8–19.7) | - | ||
| p = 0.001 | |||||
| Sampling method | Non-random | 51 | 22.1 (18.6–25.9) | 99.3% | |
| Random | 4 | 15.7 (10.7–21.3) | 76.0% | ||
| p = 0.06c | |||||
| Screening tool | PHQ-9 | 28 | 21.9 (16.2–28.2) | 99.4% | |
| SDS | 7 | 20.2 (15.5–25.3) | 96.9% | ||
| DASS-21 | 6 | 18.7 (9.6–30.0) | 98.8% | ||
| PHQ-2 | 3 | 25.1 (5.8–52.1) | - | ||
| HADS | 3 | 29.2 (6.3–60.2) | - | ||
| PHQ-4 | 2 | 20.8 (17.5–24.3) | - | ||
| CES-D | 2 | 24.4 (23.8–25.1) | - | ||
| p<0.001 | |||||
Abbreviation: CES-D = Center for Epidemiologic Studies Depression Scale; DASS = Depression Anxiety Stress Scales; HADS = Hospital Anxiety and Depression Scale; PHQ = Patient Health Questionnaire; SDS = Zung’s Self-Rating Depression Scale.
aOnly subgroups with two or more included studies are presented.
bI2 statistic provided for subgroups with four or more included studies.
cBorderline significance.
The pooled prevalence estimate of studies using random sampling techniques (15.7%; 95% CI, 10.7%-21.3%) was lower than those using non-random (22.1%; 95% CI, 18.6%-25.9%), although evidence of differential estimates was weak (p = 0.06).
28 of the included studies used the PHQ-9 to screen for depressive symptoms, and when estimates were pooled, these studies yielded a prevalence of 21.9% (95% CI, 16.2%-28.2%). The highest pooled prevalence estimate was calculated across the three studies using the HADS (29.2%; 95% CI, 16.3%-60.2%), with the lowest estimate from the six studies using the DASS-21 (18.7%; 95% CI 9.6%-30.0%), although it is worth noting the wide and overlapping confidence intervals, suggesting imprecise estimates. The subgroup analysis suggested evidence of differential prevalence estimates between screening tools (p<0.001).
There was no evidence of differential prevalence estimates across other subgroups: sample size (p = 0.81); publication status (p = 0.30); the proportion of female participants (p = 0.91); and the proportion of participants in contact with infected patients (p = 0.92). Moreover, none of the covariates included in the meta-regression model explained the presence of heterogeneity.
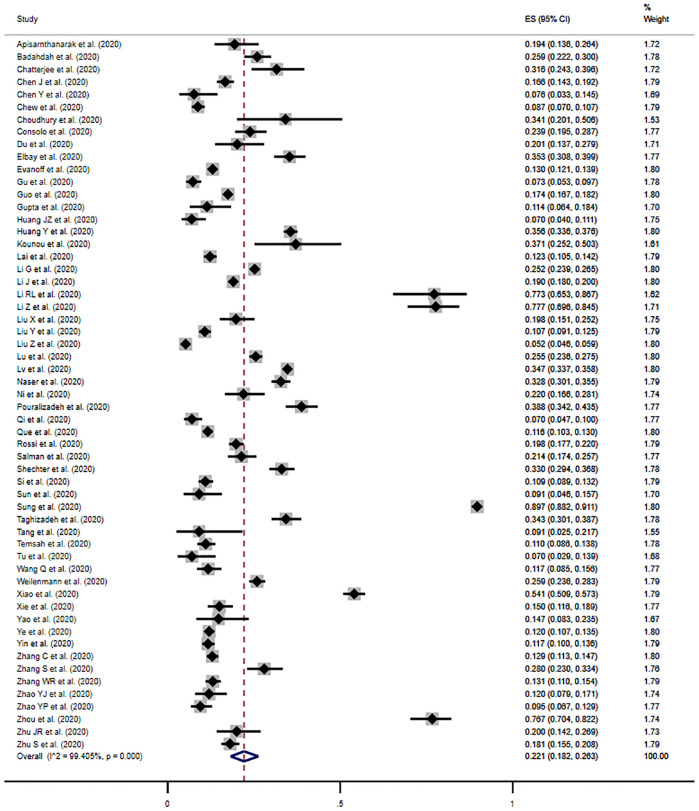
Prevalence of anxiety
The pooled prevalence of moderate anxiety was 22.1% (95% CI, 18.2%-26.3%) across 57 studies, when defining anxiety as a score at or above the cut-off for moderate symptomology, or the cut-off noted by the author to be clinically relevant (Fig 3). Individual study estimates ranged from 5.2% to 89.7%, and there was significant evidence of between-study heterogeneity (I2 = 99.4%, p<0.001). Although asymmetry in Begg’s funnel plot indicated a likelihood of publication bias, there was no evidence based on Egger’s test (p = 0.63) (S6A Appendix).
Fig 3. Meta-analysis and pooled estimate of moderate anxiety in health care workers during the COVID-19 pandemic.
The prevalence of mild anxiety was estimated at 38.3% (95% CI, 32.6%-44.3%) when defining the presence of anxiety symptoms as the cut-off for mild anxiety, or the cut-off for a clinically relevant score (S6B Appendix).
Subgroup analysis and meta-regression: Anxiety
As presented in Table 2, the prevalence estimates of moderate anxiety differed significantly across region (p<0.001). The studies from the Middle-East yielded the highest pooled prevalence estimate (28.9%; 95% CI, 21.6%-36.8%), and the lowest was calculated across the studies of North America (14.8%; 95% CI, 13.9%-15.7%). The 37 studies from China yielded a pooled prevalence (19.1%; 95% CI, 15.5%-23.0%) slightly lower than calculated across all studies from East Asia (20.5%; 95% CI, 15.7%-25.8), although the confidence intervals overlap, suggesting similar distribution of estimates.
Table 2. Subgroup analyses for studies on anxiety.
| Subgroup analysis | No. of studies | Prevalence % (95% CI) | I2 | Between-group difference | |
|---|---|---|---|---|---|
| Region | East Asia | 40 | 20.5 (15.7–25.8) | 99.6% | |
| Middle-East | 7 | 28.9 (21.6–36.8) | 96.4% | ||
| Europe | 4 | 23.9 (19.6–28.4) | 82.9% | ||
| South Asia | 3 | 21.0 (11.7–31.4) | -b | ||
| North America | 2a | 14.8 (13.9–15.7) | - | ||
| p<0.001 | |||||
| Sampling method | Non-random | 52 | 23.8 (19.7–28.1) | 99.4% | |
| Random | 5 | 7.9 (4.4–12.3) | 94.0% | ||
| p<0.001 | |||||
| Screening tool | GAD-7 | 29 | 20.8 (17.2–24.7) | 98.7% | |
| SAS | 9 | 10.1 (5.6–15.6) | 98.6% | ||
| DASS-21 | 6 | 27.0 (16.1–39.4) | 98.8% | ||
| HADS | 3 | 32.0 (10.8–58.1) | - | ||
| GAD-2 | 3 | 22.1 (10.1–37.2) | - | ||
| PHQ-4 | 2 | 24.1 (20.6–27.7) | - | ||
| HAMA | 2 | 26.8 (25.0–28.8) | - | ||
| p<0.001 | |||||
| Contact with infected patients | >50% | 15 | 25.7 (17.4–34.9) | 98.8% | |
| ≤50% | 12 | 17.4 (14.5–20.4) | 96.2% | ||
| p = 0.06c | |||||
Abbreviation: DASS = Depression Anxiety Stress Scales; GAD = Generalised Anxiety Disorder Assessment; HADS = Hospital Anxiety and Depression Scale; HAMA = Hamilton Anxiety Rating Scale; PHQ = Patient Health Questionnaire; SAS = Zung’s Self-Rating Anxiety Scale
aOnly subgroups with two or more included studies are presented
bI2 statistic provided for subgroups with four or more included studies
cBorderline significance
The prevalence estimate across studies adopting a random sampling methodology (7.9%; 95% CI, 4.4%-12.3%) was significantly lower (p<0.001) than the pooled estimate across studies using non-random methods (23.8%; 95% CI, 19.7%-28.1%), and was 14.2% lower than the overall pooled estimate.
29 studies used the GAD-7, and the pooled prevalence estimate across these studies was 20.8% (95% CI, 17.2%-24.7%). The highest pooled prevalence was calculated from the studies using HADS (32.0%; 95% CI, 10.8%-58.1%), although this group included only three studies and the confidence intervals are wide. Those studies using the SAS yielded the lowest pooled estimate (10.1%; 95% CI, 5.6%-15.6%), although it should be noted that the confidence intervals overlap with those of the HADS. The pooled estimates of these subgroups differed significantly (p<0.001).
Data on the proportion of participants in contact with patients infected with COVID-19 was provided in 27 studies only. Studies in which more than 50% of participants were in contact with patients with COVID-19 demonstrated a higher prevalence of anxiety (25.7%; 95% CI, 17.4%-34.9%), compared to studies in which 50% or fewer participants were in contact (17.4%; 14.5%-20.4%), although evidence of this difference was of borderline significance (p = 0.06).
Prevalence estimates did not significantly differ based on sample size (p = 0.73); publication status (p = 0.13); and the proportion of female participants (p = 0.25). Based on the univariate meta-regression analyses, there was evidence that the following variables explained between-study heterogeneity: sampling method (p = 0.03); screening tool (p = 0.05); publication status (p = 0.03); and the proportion of participants in contact with infected patients (p = 0.04). The subsequent multi-variate meta-regression model suggested that these variables explained approximately 17% of the between-study variance (adjusted R2 = 17.4%).
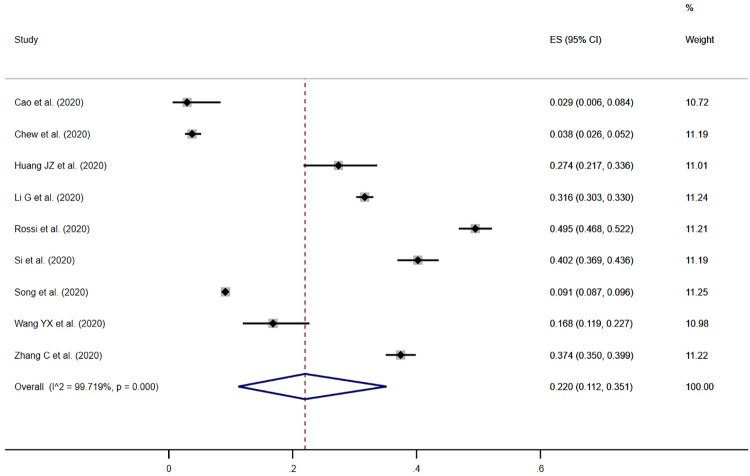
Prevalence of PTSD
Symptoms of PTSD in health care workers was measured in nine studies. The pooled prevalence estimate of moderate PTSD was 21.5% (95% CI, 10.5%-34.9%) when defined as a score at or above the cut-off for moderate symptomology, or the cut-off noted by the author to be clinically relevant (Fig 4). Individual study estimates ranged from 2.9% to 49.5%, and there was evidence of between-study heterogeneity (I2 = 99.7%, p<0.001).
Fig 4. Meta-analysis and pooled estimate of moderate PTSD in health care workers during the COVID-19 pandemic.
Seven of the nine studies reported the prevalence estimate of health care workers scoring at or above a single severity threshold, and we have not presented estimates of mild PTSD. Subgroup analyses and an assessment of publication bias were not undertaken because of the small number of studies (<10) reporting the prevalence of PTSD.
Discussion
This systematic review and meta-analysis of 65 studies involving 97,333 health care workers across 21 countries demonstrated high prevalence estimates of moderate depression (21.7%), anxiety (22.1%) and PTSD (21.5%) among health care workers during the COVID-19 pandemic, consistent with findings of previous reviews [13, 16].
Most of the studies in this review used non-random sampling methods, which may have led to selection bias and over-estimation of the prevalence of these disorders. This pattern is particularly notable in the prevalence estimates for anxiety, in which studies with random sampling yielded a pooled estimate of 7.9%, 14.2% lower than the summary estimate. Notwithstanding this concern, the estimates for depression, anxiety and PTSD are considerably higher than those expected among the general population in regular times (depression: 4.4%; anxiety, including PTSD: 3.6%), calling attention to the considerable psychological impact of the pandemic on health care workers [17]. The evidence is clear, those with mental disorders are more likely to experience excess morbidity and premature mortality, as well as negative impacts across work, education and community life [93, 94].
When interpreting the pooled prevalence estimates calculated in this review and meta-analysis, it is important to note that the percentage of variability (I2) in the prevalence estimates due to heterogeneity was very high. That said, the I2 is extremely sensitive when a large number of studies are included in meta-analyses, and a high I2 is often inevitable [95]. The I2 may therefore detect only a small amount of heterogeneity, which is not clinically important. Despite this, we explored heterogeneity based on subgroup and meta-regression analyses. Although the subgroup analyses suggested evidence of between-group differences in prevalence estimates across a number of variables (e.g. region, sampling method, screening tool), the meta-regression did not adequately explain the presence of heterogeneity. With regards to the pooled estimate of moderate anxiety, the included variables explained only 17.4% of between-study heterogeneity.
Nevertheless, observations across included studies suggest that health care workers are at risk of common mental disorders during the pandemic. We earlier compared the prevalence estimates of our meta-analysis with those from the WHO among the general population in regular times, to highlight the impact of the pandemic on mental health. With the estimates from the WHO and those presented in this paper generated through different methods, we did not think it appropriate to undertake statistical comparison, and have provided a narrative commentary. We were not able to source global estimates of common mental disorders among health care workers in regular times, but this would be a valuable comparison.
Our subgroup analyses identified a higher prevalence of anxiety in studies with a greater proportion of participants in direct contact with patients infected with COVID-19, although the evidence was weak. This finding is consistent with the association of anxiety and workplace fatigue, burnout and fear for one’s safety, likely higher in workers in direct contact with infected patients [6]. Not all studies provided information on the number of participants in contact with infected patients, and of those that did, none provided disaggregated prevalence data. Providing this information in future studies will aid further evidence syntheses and analyses. Similarly, disaggregated data by other variables (e.g. gender, occupation) would provide opportunity for more detailed analysis, and allow us to better understand the risk factors associated with common mental disorders, needed to inform an appropriate response. We encourage future research to identify risk factors present in different settings.
Although the prevalence estimates were imprecise (wide confidence intervals), it is suggested that health care workers in the Middle-East experience high prevalence of depression and anxiety, perhaps attributed to this region’s relatively high COVID-19 caseload [2]. Although China saw the first outbreak of COVID-19, the reported caseload is substantially lower than reported in other countries and regions, and this may be a factor in the relatively lower pooled estimates calculated for the country, and across the East Asia region. Variation in sampling methods is an alternative explanation. Most of the included literature adopted non-random sampling techniques, increasing the risk of bias in individual studies, and potentially resulting in overestimation of the prevalence of mental health disorders. Each study using random sampling was conducted in China, and this may also explain the lower prevalence estimates pooled across this country and East Asia.
Most studies used online surveys and questionnaires to assess mental health status (examples of non-random self-selection). These would have been necessary during the COVID-19 pandemic, with many countries practicing self-isolation and social distancing measures, making face-to-face assessment challenging and dangerous. Evidence suggests that remote, online screening results in comparable estimates to face-to-face delivery, and these methods, in and of themselves, are not a concern [96, 97]. That being said, their use is associated with non-random sampling methodologies, and consequently increases the chance of selection bias. Future research should use face-to-face survey methodologies, where possible, to reduce the risk of bias.
Strengths and limitations
The primary strength of this study is its search of international and Chinese databases, and its inclusion of studies published in both English and Chinese. Adhering to PRISMA guidelines and systematic review methods provided methodological rigour.
This study has important limitations to consider. Not all studies were screened by two reviewers at title and abstract, and although evidence suggests that limited dual review processes remain an effective procedure, there may have been eligible studies missed [98, 99]. Additionally, it is possible we missed some relevant literature as only articles in English or Chinese were included, and some databases were not searched (e.g. Scopus). Further, we included preprint articles, not yet peer-reviewed, and results from these studies may change in the future and methodological biases may be present. That being said, results of our subgroup analyses did not indicate differential prevalence estimates between peer-reviewed and preprint papers. The majority of data were derived from studies using different sampling methods, study design, screening tools and diagnostic thresholds, and substantial heterogeneity was seen. We were unable to explain much of this variability in our meta-regression models, as we were restricted with the information on covariates available to us. Although visual inspection of Begg’s funnel plots suggested marginal publication bias, results of Egger’s tests did not; a less subjective methodology and reasonable to rely on, when a meta-analysis includes a relatively large number of studies, as is the case [100]. None of the studies used the gold standard diagnostic interview to identify mental health status, although they each used a validated self-report measure, common methodology in mental health research. Lastly, many studies were conducted with health care workers in a single setting, limiting insight into the generalisability of findings.
Conclusion
This systematic review and meta-analyses provide the most comprehensive information on the prevalence of depression, anxiety and PTSD among health care workers during the COVID-19 pandemic, to date. Health care workers are at risk of common mental disorders, and the results of this review should inform action in policy and practice, to support the psychological wellbeing of health care workers. Additional research should be conducted into the factors associated with poor mental health, and future prevalence studies must adopt random sampling methods to improve the precision of estimates.
Our findings present a concerning outlook for health care workers, a group continually needed at the forefront of action against COVID-19, and at continued risk of associated psychological stressors. The response from policy makers and service providers must be decisive and swift, addressing mental health concerns in in this group, before long-term health and social impacts are realised. Support initiatives developed during the pandemic can help inform and inspire ideas in service provision across different regions, as the global society combats this pandemic (for example, e-learning to support the psychological wellbeing of health care employees) [101]. There must now be more attention given to generating and assessing the effectiveness of different interventions and initiatives to support the mental health of health care workers during this pandemic.
Supporting information
(PDF)
(PDF)
(PDF)
(PDF)
(PDF)
(PDF)
(PDF)
Data Availability
All relevant data are within the paper and its Supporting information files.
Funding Statement
The author(s) received no specific funding for this work.
References
- 1.WHO Director-General’s opening remarks at the media briefing on COVID-19–11 March 2020. https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19—11-march-2020
- 2.COVID-19 Dashboard by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University (JHU). https://coronavirus.jhu.edu/map.html
- 3.Petersen E, Koopmans M, Go U, Hamer DH, Petrosillo N, Castelli F, et al. Comparing SARS-CoV-2 with SARS-CoV and influenza pandemics. The Lancet Infectious Diseases. 2020;20(9):e238–e44. 10.1016/S1473-3099(20)30484-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tanne JH, Hayasaki E, Zastrow M, Pulla P, Smith P, Rada AG. Covid-19: how doctors and healthcare systems are tackling coronavirus worldwide. BMJ. 2020;368:m1090. 10.1136/bmj.m1090 [DOI] [PubMed] [Google Scholar]
- 5.Chen W, Huang Y. To Protect Health Care Workers Better, To Save More Lives With COVID-19. Anesthesia & Analgesia. 2020;131(1). 10.1213/ANE.0000000000004834 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Giannis D, Geropoulos G, Matenoglou E, Moris D. Impact of coronavirus disease 2019 on healthcare workers: beyond the risk of exposure. Postgraduate Medical Journal. 2020:postgradmedj-2020-137988. 10.1136/postgradmedj-2020-137988 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nguyen LH, Drew DA, Graham MS, Joshi AD, Guo C-G, Ma W, et al. Risk of COVID-19 among front-line health-care workers and the general community: a prospective cohort study. The Lancet Public Health. 2020;5(9):e475–e83. 10.1016/S2468-2667(20)30164-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fisher M, Baum F. The social determinants of mental health: implications for research and health promotion. The Australian and New Zealand journal of psychiatry. 2010;44(12):1057–63. 10.3109/00048674.2010.509311 [DOI] [PubMed] [Google Scholar]
- 9.Garfin DR, Thompson RR, Holman EA. Acute stress and subsequent health outcomes: A systematic review. Journal of psychosomatic research. 2018;112:107–13. 10.1016/j.jpsychores.2018.05.017 [DOI] [PubMed] [Google Scholar]
- 10.Koutsimani P, Montgomery A, Georganta K. The Relationship Between Burnout, Depression, and Anxiety: A Systematic Review and Meta-Analysis. Frontiers in Psychology. 2019;10(284). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Salvagioni DAJ, Melanda FN, Mesas AE, González AD, Gabani FL, Andrade SMd. Physical, psychological and occupational consequences of job burnout: A systematic review of prospective studies. PLoS One. 2017;12(10):e0185781–e. 10.1371/journal.pone.0185781 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.van der Molen HF, Nieuwenhuijsen K, Frings-Dresen MHW, de Groene G. Work-related psychosocial risk factors for stress-related mental disorders: an updated systematic review and meta-analysis. BMJ Open. 2020;10(7):e034849. 10.1136/bmjopen-2019-034849 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Muller AE, Hafstad EV, Himmels JPW, Smedslund G, Flottorp S, Stensland SØ, et al. The mental health impact of the covid-19 pandemic on healthcare workers, and interventions to help them: A rapid systematic review. Psychiatry Research. 2020;293:113441. 10.1016/j.psychres.2020.113441 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shaukat N, Ali DM, Razzak J. Physical and mental health impacts of COVID-19 on healthcare workers: a scoping review. International Journal of Emergency Medicine. 2020;13(1):40. 10.1186/s12245-020-00299-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Stuijfzand S, Deforges C, Sandoz V, Sajin C-T, Jaques C, Elmers J, et al. Psychological impact of an epidemic/pandemic on the mental health of healthcare professionals: a rapid review. BMC Public Health. 2020;20(1):1230. 10.1186/s12889-020-09322-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Luo M, Guo L, Yu M, Jiang W, Wang H. The psychological and mental impact of coronavirus disease 2019 (COVID-19) on medical staff and general public—A systematic review and meta-analysis. Psychiatry research. 2020;291:113190-. 10.1016/j.psychres.2020.113190 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Depression and Other Common Mental Disorders: Global Health Estimates. Geneva: World Health Organization; 2017. [Google Scholar]
- 18.Xiang Y-T, Li W, Zhang Q, Jin Y, Rao W-W, Zeng L-N, et al. Timely research papers about COVID-19 in China. The Lancet. 2020;395(10225):684–5. 10.1016/S0140-6736(20)30375-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Moher D, Liberati A, Tetzlaff J, Altman DG, The PG. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLOS Medicine. 2009;6(7):e1000097. 10.1371/journal.pmed.1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Agarwal A, Guyatt G, Busse J. Methods Commentary: Risk of Bias in Cross-Sectional Surveys of Attitudes and Practices. https://www.evidencepartners.com/resources/methodological-resources/risk-of-bias-cross-sectional-surveys-of-attitudes-and-practices/
- 21.Nyaga VN, Arbyn M, Aerts M. Metaprop: a Stata command to perform meta-analysis of binomial data. Archives of Public Health. 2014;72(1):39. 10.1186/2049-3258-72-39 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Freeman MF, Tukey JW. Transformations Related to the Angular and the Square Root. Ann Math Statist. 1950;21(4):607–11. [Google Scholar]
- 23.Borenstein M, Hedges LV, Higgins JP, Rothstein HR. A basic introduction to fixed-effect and random-effects models for meta-analysis. Research synthesis methods. 2010;1(2):97–111. 10.1002/jrsm.12 [DOI] [PubMed] [Google Scholar]
- 24.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. Bmj. 2003;327(7414):557–60. 10.1136/bmj.327.7414.557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994;50(4):1088–101. [PubMed] [Google Scholar]
- 26.Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ (Clinical research ed). 1997;315(7109):629–34. 10.1136/bmj.315.7109.629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Harbord RM, Higgins JPT. Meta-Regression in Stata. The Stata Journal. 2008;8(4):493–519. [Google Scholar]
- 28.Amerio A, Bianchi D, Santi F, Costantini L, Odone A, Signorelli C, et al. Covid-19 pandemic impact on mental health: a web-based cross-sectional survey on a sample of Italian general practitioners. Acta Bio Medica Atenei Parmensis. 2020;91(2):83–8. 10.23750/abm.v91i2.9619 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Apisarnthanarak A, Apisarnthanarak P, Siripraparat C, Saengaram P, Leeprechanon N, Weber DJ. Impact of anxiety and fear for COVID-19 toward infection control practices among Thai healthcare workers. Infection control and hospital epidemiology. 2020;41(9):1093–4. 10.1017/ice.2020.280 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Badahdah A, Khamis F, Al Mahyijari N, Al Balushi M, Al Hatmi H, Al Salmi I, et al. The mental health of health care workers in Oman during the COVID-19 pandemic. International Journal of Social Psychiatry. 2020:0020764020939596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cao J, Duan Y, Wei J, Zhu H, Geng W, Fritzsche K, et al. The Sooner, the Better: Experience of Early-On Psychological Service to Medical Workers in Fever Clinic of a Tertiary General Hospital in Beijing During COVID-19 Outbreak. SSRN: https://ssrn.com/abstract=3588536 or 10.2139/ssrn.3588536. 2020. [DOI]
- 32.Chatterjee S, Bhattacharyya R, Bhattacharyya S, Gupta S, Das S, Banerjee B. Attitude, practice, behavior, and mental health impact of COVID-19 on doctors. Indian Journal of Psychiatry. 2020;62(3):257–65. 10.4103/psychiatry.IndianJPsychiatry_333_20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chen J, Liu X, Wang D, Jin Y, He M, Ma Y, et al. Risk factors for depression and anxiety in healthcare workers deployed during the COVID-19 outbreak in China. Social Psychiatry and Psychiatric Epidemiology. 2020. 10.1007/s00127-020-01954-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Chen Y, Zhou H, Zhou Y, Zhou F. Prevalence of self-reported depression and anxiety among pediatric medical staff members during the COVID-19 outbreak in Guiyang, China. Psychiatry Research. 2020;288:113005. 10.1016/j.psychres.2020.113005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Chew NWS, Lee GKH, Tan BYQ, Jing M, Goh Y, Ngiam NJH, et al. A multinational, multicentre study on the psychological outcomes and associated physical symptoms amongst healthcare workers during COVID-19 outbreak. Brain, Behavior, and Immunity. 2020;88:559–65. 10.1016/j.bbi.2020.04.049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Choudhury T, Debski M, Wiper A, Abdelrahman A, Wild S, Chalil S, et al. Covid-19 Pandemic: Looking after the Mental Health of our Healthcare Workers. Journal of occupational and environmental medicine. 2020. 10.1097/JOM.0000000000001907 [DOI] [PubMed] [Google Scholar]
- 37.Du J, Dong L, Wang T, Yuan C, Fu R, Zhang L, et al. Psychological symptoms among frontline healthcare workers during COVID-19 outbreak in Wuhan. General Hospital Psychiatry. 2020. 10.1016/j.genhosppsych.2020.03.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Elbay RY, Kurtulmuş A, Arpacıoğlu S, Karadere E. Depression, anxiety, stress levels of physicians and associated factors in Covid-19 pandemics. Psychiatry Research. 2020;290:113130. 10.1016/j.psychres.2020.113130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Evanoff BA, Strickland JR, Dale AM, Hayibor L, Page E, Duncan JG, et al. Work-related and Personal Factors Associated with Mental Well-being during COVID-19 Response: A Survey of Health Care and Other Workers. medRxiv. 2020:2020.06.09.20126722. 10.2196/21366 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Gu XW, Wen M, K HH. [The study on the relationship between the mental health status and social support of nurses in hospitals during the period of COVID-19]. Journal of Gannan Medical University. 2020;40(4):325–9. [Google Scholar]
- 41.Guiroy A, Gagliardi M, Coombes N, Landriel F, Zanardi C, Camino Willhuber G, et al. COVID-19 Impact Among Spine Surgeons in Latin America. Global Spine Journal. 2020:2192568220928032. 10.1177/2192568220928032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Gupta P, Rai P, Dang K. Acute stress disorder, generalized anxiety disorderand major depressive disorder during COVID-19 epidemic in India: online questionnaire-based cross-sectional survey. Journal of Dental and Medical Sciences. 2020;19(4):50–9. [Google Scholar]
- 43.Huang JZ, Han MF, Luo TD, Ren AK, Zhou XP. [Mental health survey of medical staff in a tertiary infectious disease hospital for COVID-19]. Zhonghua lao dong wei sheng zhi ye bing za zhi = Zhonghua laodong weisheng zhiyebing zazhi = Chinese journal of industrial hygiene and occupational diseases. 2020;38(3):192–5. 10.3760/cma.j.cn121094-20200219-00063 [DOI] [PubMed] [Google Scholar]
- 44.Huang Y, Zhao N. Mental health burden for the public affected by the COVID-19 outbreak in China: Who will be the high-risk group? Psychology, Health & Medicine. 2020:1–12. [DOI] [PubMed] [Google Scholar]
- 45.Kounou KB, Guédénon KM, Dogbe Foli AA, Gnassounou-Akpa E. Mental health of medical professionals during the COVID-19 pandemic in Togo. Psychiatry and Clinical Neurosciences. 2020;74(10):559–60. 10.1111/pcn.13108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lai J, Ma S, Wang Y, Cai Z, Hu J, Wei N, et al. Factors Associated With Mental Health Outcomes Among Health Care Workers Exposed to Coronavirus Disease 2019. JAMA Network Open. 2020;3(3):e203976–e. 10.1001/jamanetworkopen.2020.3976 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lam SC, Arora T, Grey I, Suen LKP, Huang EY, Li D, et al. Perceived Risk and Protection From Infection and Depressive Symptoms Among Healthcare Workers in Mainland China and Hong Kong During COVID-19. Frontiers in Psychiatry. 2020;11(686). 10.3389/fpsyt.2020.00686 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Li J, Xu J, Zhou H, You H, Wang X, Li Y, et al. Working condition and health status of 6,317 front line public health workers during the COVID-19 epidemic across 5 provinces in China: a cross-sectional study. BMC Public Health. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Li RL, Chen Y, Lv J, Liu L, Zong S, Li H, et al. Anxiety and related factors in frontline clinical nurses fighting COVID-19 in Wuhan. Medicine (Baltimore). 2020;99(30):e21413–e. 10.1097/MD.0000000000021413 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Li Z, Shi HR, Chen JF, Shi YF, Feng LH. [Investigation and Analysis on the Mental Health Status and Coping Style of First-line Nurses of Shanxi Province During the Outbreak of COVID-19]. Journal of Changzhi Medical College. 2020;34(2):87–91. [Google Scholar]
- 51.Liu S, Han W, Shen C. [The Prevalence and Influencing Factors for Depression Symptom Among Frontline Heathcare Workers from Emergency Department Fighting Against COVID-19: A National Cross-Sectional Survey in China] (Preprint). 2020.
- 52.Liu Y, Liu X, Gao B, Chengzhong L, Xuesong L. Mental distress among frontline healthcare workers outside the central epidemic area during the novel coronavirus disease (COVID-19) outbreak in China:A cross-sectional study. Health Economics & Outcomes Research. 2020. [Google Scholar]
- 53.Lu W, Wang H, Lin Y, Li L. Psychological status of medical workforce during the COVID-19 pandemic: A cross-sectional study. Psychiatry Research. 2020;288:112936. 10.1016/j.psychres.2020.112936 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Naser AY, Dahmash EZ, Al-Rousan R, Alwafi H, Alrawashdeh HM, Ghoul I, et al. Mental health status of the general population, healthcare professionals, and university students during 2019 coronavirus disease outbreak in Jordan: A cross-sectional study. Brain and Behavior. 2020;10(8):e01730. 10.1002/brb3.1730 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Zhou P, Du N, Ouyang Y. Investigation on the Mental Health of Healthcare Workers for Aid in Hu Bei Province During the Outbreak of Covid-19 Based on the Network Survey. Research Square. 2020. [Google Scholar]
- 56.Pouralizadeh M, Bostani Z, Maroufizadeh S, Ghanbari A, Khoshbakht M, Alavi SA, et al. Anxiety and depression and the related factors in nurses of Guilan University of Medical Sciences hospitals during COVID-19: A web-based cross-sectional study. International Journal of Africa Nursing Sciences. 2020;13:100233. 10.1016/j.ijans.2020.100233 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Qi JJ L L.M., Li WT, Xu YH, Shan X. 临床护士面对新型冠状病毒肺炎的心理状况调查与分析. Chinese General Practice Nursing. 2020;18(6). [Google Scholar]
- 58.Que J, Shi L, Deng J, Liu J, Zhang L, Wu S, et al. Psychological impact of the COVID-19 pandemic on healthcare workers: a cross-sectional study in China. General Psychiatry. 2020;33(3):e100259. 10.1136/gpsych-2020-100259 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Rossi R, Socci V, Pacitti F, Di Lorenzo G, Di Marco A, Siracusano A, et al. Mental Health Outcomes Among Frontline and Second-Line Health Care Workers During the Coronavirus Disease 2019 (COVID-19) Pandemic in Italy. JAMA Network Open. 2020;3(5):e2010185–e. 10.1001/jamanetworkopen.2020.10185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Salman M, Raza MH, Mustafa ZU, Khan TM, Asif N, Tahir H, et al. The psychological effects of COVID-19 on frontline healthcare workers and how they are coping: a web-based, cross-sectional study from Pakistan. medRxiv. 2020:2020.06.03.20119867. [Google Scholar]
- 61.Shechter A, Diaz F, Moise N, Anstey DE, Ye S, Agarwal S, et al. Psychological distress, coping behaviors, and preferences for support among New York healthcare workers during the COVID-19 pandemic. General Hospital Psychiatry. 2020;66:1–8. 10.1016/j.genhosppsych.2020.06.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Si MY, Su XY, Jiang Y, Wang WJ, Gu XF, Ma L, et al. The Psychological Impact of COVID-19 on Medical Care Workers in China. SSRN: https://ssrn.com/abstract=3592642 or 10.2139/ssrn.3592642. 2020. [DOI] [PMC free article] [PubMed]
- 63.Song X, Fu W, Liu X, Luo Z, Wang R, Zhou N, et al. Mental health status of medical staff in emergency departments during the Coronavirus disease 2019 epidemic in China. Brain, Behavior, and Immunity. 2020;88:60–5. 10.1016/j.bbi.2020.06.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Sun ZX, Yu XF. Anxiety and depression symptoms and related factors of medical staff in closed-door psychiatric ward during COVID-19 outbreak. Sichuan Mental Health. 2020;33(2):102–6. [Google Scholar]
- 65.Sung CW, Chen CH, Fan CY, Su FY, Chang JH, Hung CC, et al. Burnout in Medical Staffs During a Coronavirus Disease (COVID-19) Pandemic. SSRN: https://ssrn.com/abstract=3594567 or 10.2139/ssrn.3594567. 2020. [DOI]
- 66.Taghizadeh F, Hassannia L, Moosazadeh M, Zarghami M, Taghizadeh H, Fathi Dooki A, et al. Anxiety and Depression in Health Workers and General Population During COVID-19 Epidemic in IRAN: A Web-Based Cross-Sectional Study. medRxiv. 2020:2020.05.05.20089292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Tang HH, Lu XY, Cai SX. [Investigation and analysis on mental health status of frontline nurses in Wuhan during COVID-19 epidemic]. Int Infect Dis. 2020;9(2):296–7. [Google Scholar]
- 68.Temsah M-H, Al-Sohime F, Alamro N, Al-Eyadhy A, Al-Hasan K, Jamal A, et al. The psychological impact of COVID-19 pandemic on health care workers in a MERS-CoV endemic country. Journal of Infection and Public Health. 2020;13(6):877–82. 10.1016/j.jiph.2020.05.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Tu ZH, He JW, Zhou N. Sleep quality and mood symptoms in conscripted frontline nurse in Wuhan, China during COVID-19 outbreak: A cross-sectional study. Medicine (Baltimore). 2020;99(26):e20769. 10.1097/MD.0000000000020769 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Wang Q, Dong L, Guo X, Fan Y, Zhang X, Nie Y. [Investigation on mental health status of nurses who participated in COVID-19 prevention and control in Zhongshan City]. Nursing of Integrated Traditional Chinese and Western Medicine. 2020;6(3):14–6. [Google Scholar]
- 71.Wang YX, Guo HT, Du XW, Song W, Lu C, Hao WN. Factors associated with post-traumatic stress disorder of nurses exposed to corona virus disease 2019 in China. Medicine (Baltimore). 2020;99(26):e20965. 10.1097/MD.0000000000020965 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Weilenmann S, Ernst J, Petry H, Sazpinar O, Pfaltz MC, Gehrke S, et al. Health Care WorkersMental Health During the First Weeks of the SARS-CoV-2 Pandemic in Switzerland: A Cross-Sectional Study. medRxiv. 2020:2020.05.04.20088625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Xiao X, Zhu X, Fu S, Hu Y, Li X, Xiao J. Psychological impact of healthcare workers in China during COVID-19 pneumonia epidemic: A multi-center cross-sectional survey investigation. Journal of Affective Disorders. 2020;274:405–10. 10.1016/j.jad.2020.05.081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Xie ZY, Zhang P, Xie Q, Chen YQ, Chen ZW. [Correlation study between mental health and coping style of medical staff during COVID-19 epidemic]. Journal of Hubei Minzu University. 2020;37(2). [Google Scholar]
- 75.Yao L, Kong W, Deng Z, Dong H, Sun L. [Psychological problems and interventions of front-line medical staff in COVID-19 isolation ward]. Journal of Xinjiang Medical University. 2020;43(4):386–90. [Google Scholar]
- 76.Ye JR, Xia ZC, Xiao AX, Li SY, Lin JK. [Investigation on nurses’ anxiety status and influencing factors during the outbreak of COVID-19]. 2020;33(1):11–4. [Google Scholar]
- 77.Yin J, Wu X, Ma W, Xu J, Wei P. [Psychological investigation and analysis on medical care personnel in designated hospitals of coronavirus disease 2019]. Medicine and Philosophy. 2020;41(8):38–67. [Google Scholar]
- 78.Zhang SX, Liu J, Afshar Jahanshahi A, Nawaser K, Yousefi A, Li J, et al. At the height of the storm: Healthcare staff’s health conditions and job satisfaction and their associated predictors during the epidemic peak of COVID-19. Brain, Behavior, and Immunity. 2020;87:144–6. 10.1016/j.bbi.2020.05.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Zhang WR, Wang K, Yin L, Zhao W, Xue Q, Peng M, et al. Mental Health and Psychosocial Problems of Medical Health Workers during the COVID-19 Epidemic in China. Psychotherapy and Psychosomatics. 2020;89(4):242–50. 10.1159/000507639 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Zhao YP, Zhang XJ, Peng JX, Fang P. Status and Influencing Factors of Depression of Nurses from High-risk Departments during COVID-19 Pandemic Period. Chinese Journal of Medicinal Guide. 2020;22(5):294–300. [Google Scholar]
- 81.Zhao YJ, Zhang FY, Gong JZ, Li RR, Wu DM. [Survey on the difficulties, requirements and psychological status of general practitioners in community-based prevention and control of the COVID-19 epidemic]. Clinical Education of General Practice. 2020;18(3):240–4. [Google Scholar]
- 82.Zhu J, Sun L, Zhang L, Wang H, Fan A, Yang B, et al. Prevalence and Influencing Factors of Anxiety and Depression Symptoms in the First-Line Medical Staff Fighting Against COVID-19 in Gansu. Frontiers in psychiatry. 2020;11:386-. 10.3389/fpsyt.2020.00386 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Chung JPY, Yeung WS. Staff Mental Health Self-Assessment During the COVID-19 Outbreak. East Asian archives of psychiatry: official journal of the Hong Kong College of Psychiatrists = Dong Ya jing shen ke xue zhi: Xianggang jing shen ke yi xue yuan qi kan. 2020;30(1):34. 10.12809/eaap2014 [DOI] [PubMed] [Google Scholar]
- 84.Consolo U, Bellini P, Bencivenni D, Iani C, Checchi V. Epidemiological Aspects and Psychological Reactions to COVID-19 of Dental Practitioners in the Northern Italy Districts of Modena and Reggio Emilia. Int J Environ Res Public Health. 2020;17(10):3459. 10.3390/ijerph17103459 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Guo J, Liao L, Wang B, Li X, Tong Z, Guan Q, et al. Psychological Effects of COVID-19 on Hospital Staff: A National Cross-Sectional Survey of China Mainland. SSRN Electronic Journal. 2020. [Google Scholar]
- 86.Li G, Miao J, Wang H, Xu S, Sun W, Fan Y, et al. Psychological impact on women health workers involved in COVID-19 outbreak in Wuhan: a cross-sectional study. Journal of neurology, neurosurgery, and psychiatry. 2020;91(8):895–7. 10.1136/jnnp-2020-323134 [DOI] [PubMed] [Google Scholar]
- 87.Liu X, Shao L, Zhang R, Wei Y, Li J, Wang C, et al. Perceived Social Support and Its Impact on Psychological Status and Quality of Life of Medical Staffs After Outbreak of SARS-CoV-2 Pneumonia: A Cross-Sectional Study. SSRN: https://ssrncom/abstract=3541127. 202.
- 88.Liu Z, Han B, Jiang R, Huang Y, Ma C, Wen J, et al. Mental Health Status of Doctors and Nurses During COVID-19 Epidemic in China. SSRN: https://ssrncom/abstract=3551329. 2020.
- 89.Lv Y, Zhang Z, Zeng W, Li J, Wang X, Luo G. Anxiety and Depression Survey of Chinese Medical Staff Before and During COVID-19 Defense. SSRN: https://ssrncom/abstract=3551350. 2020.
- 90.Ni MY, Yang L, Leung CMC, Li N, Yao XI, Wang Y, et al. Mental Health, Risk Factors, and Social Media Use During the COVID-19 Epidemic and Cordon Sanitaire Among the Community and Health Professionals in Wuhan, China: Cross-Sectional Survey. JMIR mental health. 2020;7(5):e19009. 10.2196/19009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Zhang C, Yang L, Liu S, Ma S, Wang Y, Cai Z, et al. Survey of Insomnia and Related Social Psychological Factors Among Medical Staff Involved in the 2019 Novel Coronavirus Disease Outbreak. Frontiers in psychiatry. 2020;11:306-. 10.3389/fpsyt.2020.00306 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Zhu S, Wu Y, Zhu C-Y, Hong W-C, Yu Z-X, Chen Z-K, et al. The immediate mental health impacts of the COVID-19 pandemic among people with or without quarantine managements. Brain, behavior, and immunity. 2020;87:56–8. 10.1016/j.bbi.2020.04.045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Saxena S. Excess mortality among people with mental disorders: a public health priority. The Lancet Public Health. 2018;3(6):e264–e5. 10.1016/S2468-2667(18)30099-9 [DOI] [PubMed] [Google Scholar]
- 94.Walker ER, McGee RE, Druss BG. Mortality in mental disorders and global disease burden implications: a systematic review and meta-analysis. JAMA Psychiatry. 2015;72(4):334–41. 10.1001/jamapsychiatry.2014.2502 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Borges Migliavaca C, Stein C, Colpani V, Barker TH, Munn Z, Falavigna M, et al. How are systematic reviews of prevalence conducted? A methodological study. BMC Med Res Methodol. 2020;20(96). 10.1186/s12874-020-00975-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Ballester L, Alayo I, Vilagut G, Almenara J, Cebrià AI, Echeburúa E, et al. Accuracy of online survey assessment of mental disorders and suicidal thoughts and behaviors in Spanish university students. Results of the WHO World Mental Health- International College Student initiative. PLoS One. 2019;14(9):e0221529–e. 10.1371/journal.pone.0221529 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Cronly J, Duff AJ, Riekert KA, Perry IJ, Fitzgerald AP, Horgan A, et al. Online versus paper-based screening for depression and anxiety in adults with cystic fibrosis in Ireland: a cross-sectional exploratory study. BMJ Open. 2018;8(1):e019305. 10.1136/bmjopen-2017-019305 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Taylor-Phillips S, Geppert J, Stinton C, Freeman K, Johnson S, Fraser H, et al. Comparison of a full systematic review versus rapid review approaches to assess a newborn screening test for tyrosinemia type 1. Research synthesis methods. 2017;8(4):475–84. 10.1002/jrsm.1255 [DOI] [PubMed] [Google Scholar]
- 99.Waffenschmidt S, Knelangen M, Sieben W, Bühn S, Pieper D. Single screening versus conventional double screening for study selection in systematic reviews: a methodological systematic review. BMC medical research methodology. 2019;19(1):132. 10.1186/s12874-019-0782-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Rothstein HR, Sutton AJ, Borenstein M. Publication Bias in Meta-Analysis: Prevention, Assessment and Adjustments. Chichester: Wiley; 2005. [Google Scholar]
- 101.Blake H, Bermingham F, Johnson G, Tabner A. Mitigating the Psychological Impact of COVID-19 on Healthcare Workers: A Digital Learning Package. Int J Environ Res Public Health. 2020;17(9):2997. 10.3390/ijerph17092997 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF)
(PDF)
(PDF)
(PDF)
(PDF)
(PDF)
(PDF)
Data Availability Statement
All relevant data are within the paper and its Supporting information files.