Abstract
Acute respiratory failure occurs when the lungs fail to oxygenate arterial blood adequately and it is one of the commonest postoperative complications. The preoperative identification of risk factors for postoperative acute respiratory failure allows identification of those patients who may benefit from preoperative optimization and increased postoperative vigilance. Multiple postoperative pulmonary complications are associated with acute hypoxemic respiratory failure and this chapter discusses atelectasis, pulmonary embolism, aspiration, and acute respiratory distress syndrome in detail, as well as providing a unified clinical approach to the acutely hypoxemic perioperative patient.
Keywords: ARDS, atelectasis, hypoxemia, postoperative pulmonary complications, pulmonary embolism
Definition
Respiratory failure occurs when the lungs fail to oxygenate the arterial blood adequately and/or fail to prevent carbon dioxide retention. Although the definition does not contain any absolute values, an arterial O2 of less than 60 mmHg and an arterial CO2 of more than 50 mmHg are often regarded as of consequence. However, values should be considered in the context of an individual patient.
Hypoxemic Respiratory Failure
There are four main causes of hypoxemic respiratory failure:
-
1.
Hypoventilation
-
2.
Diffusion impairment
-
3.
Shunt
-
4.
Ventilation-perfusion (V/Q) mismatch
Of these, V/Q mismatch is the most frequently encountered.1, 2 Most of these abnormalities improve with supplemental oxygenation, except for a shunt. A “true shunt” develops when portions of the lung are perfused in total absence of ventilation. The most frequent causes of a shunt in the postoperative patient are consolidated pneumonia, lobar atelectasis, and the later phases of the acute respiratory distress syndrome (ARDS).3, 4 Other causes of hypoxemic respiratory failure in the postoperative population include pulmonary edema, chronic obstructive pulmonary disease (COPD), pneumothorax, pulmonary embolism, and pulmonary hypertension.3
Hypercapnic Respiratory Failure
The four basic mechanisms underlying hypercapnic respiratory failure are:
-
1.
Inability to sense increasing arterial CO2 (hypoventilation)
-
2.
Increased CO2 production
-
3.
Increased dead space
-
4.
Decreased tidal volume
The common causes of each in the postoperative patient are listed in Box 39.1 .2, 3, 5
Box 39.1. Common causes of type II respiratory failure in postoperative patients.
Inability to Sense an Increasing PaCO2
-
▪
Anesthetic agents
-
▪
Benzodiazepines
-
▪
Narcotics
Increased CO2 Production
-
▪Hypermetabolic states
-
▪Fever
-
▪Sepsis
-
▪Multiple organ failure
-
▪Burns
-
▪Trauma
-
▪
-
▪
Excessive carbohydrate intake
-
▪
Hyperthyroidism
Decreased Tidal Ventilation (VT)
-
▪
Post-traumatic flail chest
Increased Dead Space Ventilation (VD)
-
▪
Adult respiratory distress syndrome (ARDS)
Alt-text: Box 39.1
Acute Respiratory Failure in the Perioperative Patient
Identification of risk factors for postoperative acute respiratory failure is helpful in that it identifies those patients who may benefit from preoperative optimization and increased postoperative vigilance. Many studies have been undertaken to identify predictors of postoperative acute respiratory failure and other pulmonary complications. Nijbroek et al. reviewed 21 different studies attempting to derive predictive scores and concluded that only the ARISCAT score was adequately externally validated.6
The Assess Respiratory Risk in Surgical Patients in Catalonia (ARISCAT) investigators conducted a prospective multicenter observational random-sample cohort study of 2464 patients undergoing non-obstetric procedures under general, neuroaxial or regional anesthesia in southern Spain.7 The overall incidence of postoperative pulmonary complications (PPCs) was 5% and 30-day mortality was increased in those who developed PPCs compared with those who did not (19.5 versus 0.5%). Seven factors were found to be independently predictive of the development of PPCs: low preoperative arterial oxygen saturations when breathing room air and lying supine, acute respiratory infection associated with a fever and the need for antibiotic therapy during the preceding month, age, preoperative anemia, upper abdominal or intrathoracic surgery, a surgical duration longer than two hours, and emergency surgery. The derived ARISCAT score was able to classify patients as low (score < 26), intermediate (score 2–44) or high (score > 45) risk for PPCs. Although obesity and asthma did not emerge as independent predictors, other studies have shown that preexisting comorbidities are important contributors.8, 9 However, their importance may be lessened by preoperative optimization.
Subsequent investigators have validated the ARISCAT score for predicting the risk of developing PPCs, including a recent study of 1170 patients undergoing noncardiac surgery, which showed that patients with intermediate and high risk based on ARISCAT were found to have increased risk of PPCs.10
Some factors can be optimized prior to undertaking elective surgical procedures. Warner and coworkers documented that smoking cessation 8 weeks prior to elective surgery led to a decreased incidence of postoperative acute respiratory failure.11 Systematic review of the impact of preoperative smoking interventions by the Cochrane collaboration found that there was heterogeneity between intensive and brief behavioral interventions, with significant impact of intensive intervention on PPCs and wound complications.12
There are also data suggesting that the manner in which both emergency and elective surgical patients are mechanically ventilated during surgery can be associated with the development of PPCs. Several studies have shown that for patients receiving tidal volumes less than 8 mL/kg IBW (ideal body weight), increased driving pressure or peak inspiratory pressure are associated with increased development of PPCs.13, 14 These findings have also been reproduced in an individual patient meta-analysis of data from 2250 patients from 17 clinical trials.15
The association between intraoperative tidal volume and PPCs is less straightforward, but a meta-analysis of 2127 patients from 15 studies suggested that low tidal volume ventilation is associated with a decreased incidence of PPCs, but has no impact on mortality of length of hospital stay.16 However, this finding was not reproduced in more recent clinical studies.13, 14
Postoperative Factors
After surgery, all patients are at risk of acute respiratory failure. Some of the more common etiologies are atelectasis, bronchospasm, pulmonary aspiration, anesthetic effects, pulmonary edema, pulmonary embolism, and ARDS.
Atelectasis
The term atelectasis is derived from the Greek words ateles and ektasis, which mean incomplete expansion. Atelectasis is defined as alveolar collapse with reduced intrapulmonary air. It is the most common PPC, with radiographic evidence in up to 70% of patients undergoing a thoracotomy or a celiotomy.17 If left untreated, it can result in pulmonary gas exchange alterations leading to severe hypoxemia and acute respiratory failure. The mechanisms leading to atelectasis are multifactorial and include alterations in ventilatory mechanics, changes in the mechanical properties of the thoracic wall, stagnation of bronchial secretions, and airway obstruction.1
The alterations in ventilatory mechanics seen postoperatively include diminished vital capacity (VC), diminished VT, increased respiratory rate, and diminished functional residual capacity (FRC), resulting in atelectasis. The primary cause of these alterations is postoperative diaphragmatic dysfunction.1, 18 Stagnation of bronchial secretions is also a mechanism leading to atelectasis. This problem is normally prevented by mucociliary clearance and coughing. When these functions are inhibited, stagnation of bronchial secretions occurs, and atelectasis can develop.1
Mucociliary clearance is significantly diminished during mechanical ventilation.9 Coughing may be suppressed secondary to mechanical ventilation, opioids, diaphragmatic dysfunction, pain, altered mental status, and airway obstruction. A final mechanism of atelectasis is airway obstruction. In this case, atelectasis is either passive or absorptive. Passive atelectasis is secondary to external or internal compression of a lung segment (e.g., pneumothorax, hemothorax, abdominal distention). Absorptive atelectasis occurs when the inhaled gas is rich in oxygen and poor in nitrogen. In this instance, oxygen diffuses rapidly into venous blood, leading to alveolar collapse.9
Risk factors for atelectasis are shown in Box 39.2 .1 The type of surgical procedure performed has tremendous influence on the occurrence of postoperative atelectasis. Thoracic and upper abdominal surgeries pose a greater risk for atelectasis than do other procedures. Several studies have documented progressive deterioration of pulmonary gas exchange during the course of thoracic and abdominal surgeries.19, 20 Likewise, cardiopulmonary bypass surgery increases the risk of atelectasis more than other surgeries (including noncardiac thoracic surgeries).21, 22, 23 In addition, midline celiotomies have an increased risk of atelectasis relative to transverse or subcostal abdominal incisions.
Box 39.2. Risk factors for atelectasis.
-
▪
Very young age (infants and young children)
-
▪
Obesity
-
▪
Smoking
-
▪
Preexisting pulmonary disease
-
▪
Dehydration
-
▪
Anesthetic agents
-
▪
Mechanical ventilation
-
▪Types of surgery
-
▪Cardiopulmonary bypass surgery
-
▪Thoracic surgery
-
▪Upper abdominal surgery
-
▪Midline incisions
-
▪Prolonged anesthesia
-
▪
Alt-text: Box 39.2
Clinical Manifestations
Clinically, atelectasis ranges from asymptomatic to severe hypoxemia and acute respiratory failure. The variability in presentation depends on the rapidity of onset, the degree of lung involvement, and the presence of an underlying pulmonary infection. In the worst-case scenario with rapid onset, major airway collapse, and underlying infection, atelectasis presents with sudden dyspnea, chest pain, cyanosis, tachycardia, and an elevated temperature. On physical examination, the patient often exhibits diminished chest wall excursion, dullness to percussion, and diminished or absent breath sounds. In the less severe presentations, elevated temperature on the first postoperative day may be the only manifestation of atelectasis.24
Diagnosis
The diagnosis of atelectasis is generally made from radiographic findings of diminished lung volumes in the presence of the aforementioned clinical manifestations. On chest radiographs, findings indicative of atelectasis relate to volume loss and include displacement of the lobar fissure, retracted ribs, an elevated hemidiaphragm, mediastinal or tracheal deviation to the affected side, and over-inflation of the unaffected lung. The exact radiographic findings depend on which portion of the lung is involved and to what degree, in addition to how the surrounding structures compensate for the volume loss. On arterial blood gas (ABG) analysis, significant atelectasis results in hypoxemia. Atelectasis also may be identified by means of chest computed tomography (CT) or lung ultrasound.1, 24, 25
Treatment
For postoperative atelectasis, prevention is the key.26 Because tobacco use and underlying pulmonary disease processes are predictors of postoperative atelectasis, preoperative optimization is essential. Both smoking cessation and improved bronchial toilet preoperatively should be encouraged. During anesthesia induction, the use of positive end-expiratory pressure (PEEP) has been shown to be beneficial. Rusca and coworkers documented significantly decreased atelectasis and improved oxygenation by applying 6 cm H2O of positive end expiratory pressure (PEEP) on induction.27 In addition to this, long-acting anesthetics and those with significant post-anesthesia narcosis should be limited.1
During the postoperative period, a number of measures can be taken to prevent atelectasis (Fig. 39.1 ). Control of postoperative pain is critical. Insufficient analgesia results in pleural and parietal pain, causing inadequate coughing and expectoration. However, because narcotics depress the cough reflex, excessive doses should be avoided.1, 24, 25 The traditional intermittent dosing of narcotics at 3- to 4-hour intervals is insufficient. The patient cycles from overdosing after administration (over-sedation with resultant poor coughing and expectoration) to pain and anxiety before receiving the next dose. This cyclical pattern may be avoided by using patient-controlled analgesia (PCA). Another alternative is neuroaxial or regional analgesia, which is very effective. A meta-analysis supports the view that postoperative atelectasis is decreased when patients receive epidural opioids instead of systemic opioids.28
Fig. 39.1.
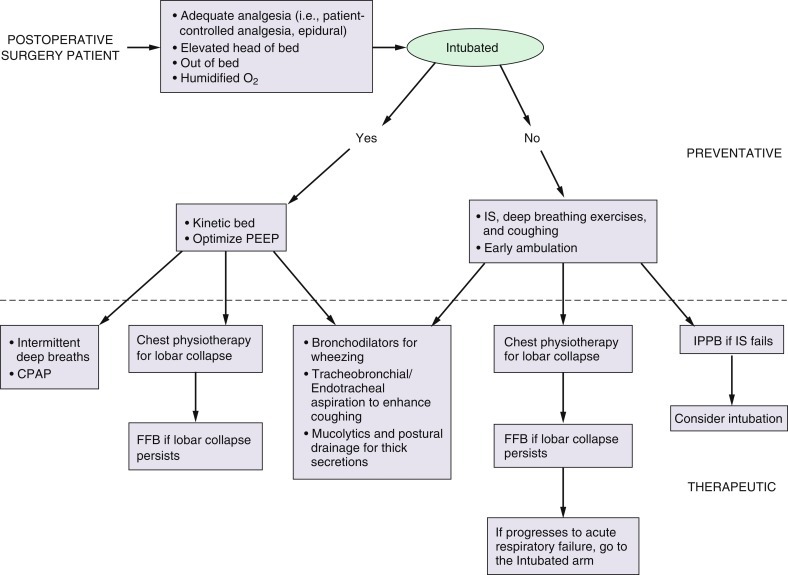
Prevention and treatment algorithm for postoperative atelectasis. CPAP, Continuous positive airway pressure; FFB, flexible fiberoptic bronchoscopy; IPPB, intermittent positive-pressure breathing; IS, incentive spirometry; PEEP, positive end-expiratory pressure.
Just as pain control is critical, so is meticulous nursing care. In non-intubated patients, several steps should be taken to prevent atelectasis. Early ambulation and techniques that encourage deep breathing are important.29, 30, 31
Incentive spirometry (IS) is the most widely used postoperative pulmonary therapy. Its purpose is to imitate the natural sighing or yawning that healthy individuals perform regularly. The simplicity of IS and its lack of required personnel account for its popularity. A meta-analysis suggests that IS, intermittent positive-pressure breathing (IPPB), and chest physiotherapy are all equally efficacious in decreasing PPCs after upper abdominal surgery.32 Chest physiotherapy encompasses deep breathing and coughing, postural drainage, and chest percussion.
Continuous positive airway pressure (CPAP) can be used as a last means in attempting to prevent intubation. In a randomized controlled trial, Squadrone and colleagues documented that CPAP decreases the incidence of PPCs (including endotracheal intubation) in patients who develop hypoxia after major elective abdominal surgery.33 If these maneuvers are unsuccessful and the patient continues to progress to acute respiratory failure, the patient should be intubated and consideration given to whether a flexible fiberoptic bronchoscopy may be of benefit.
Aspiration
Pulmonary aspiration of gastric contents is generally preventable with meticulous anesthesia technique and critical care. Despite this, the incidence varies from 1 in every 3900 elective surgical cases to 1 in every 895 emergent surgical cases. The number increases dramatically to 8% to 19% during emergent intubations without anesthesia.1
Aspiration of gastric contents results in chemical pneumonitis, which develops in four stages.1 Initially, the aspirate causes mechanical obstruction of the airways, with distal collapse. Obstruction alters ventilatory mechanics, leading to increased shunt, loss of FRC, and increased work of breathing. In the second stage, chemical injury occurs in response to the acidity of the aspirate. The pattern of injury includes mucosal edema, bronchorrhea, and bronchoconstriction, all resulting in an increased risk of bacterial infection. The third stage in the pathophysiology of aspiration is the inflammatory response. The release of tumor necrosis factor, interleukin 1, leukotrienes, and thromboxane A2 contribute to mucosal edema and bronchoconstriction resulting in lung inflammation. The final phase is progression to infection if appropriate interventions are not performed. Risk factors for pulmonary aspiration are shown in Table 39.1 .34, 35, 36
Table 39.1.
Risk factors for pulmonary aspiration.
| Risk factor | Clarification / Examples |
|---|---|
| Endotracheal intubation | The cuff does not prevent aspiration. |
| Decreased level of consciousness | GCS < 9, alcohol or drug overdose/withdrawal, excessive analgesics or sedatives, chemical paralysis |
| Neuromuscular disease and structural abnormalities of the aerodigestive tract | Diabetic gastroparesis, Parkinson’s disease, scleroderma, gastroesophageal reflux disease, esophageal cancer |
| Recent cerebrovascular accident | Within 4–6 weeks |
| Major intra-abdominal surgery | Less than 5 days postoperatively |
| Persistently high gastric residual volume (GRV) | GRV > 500 mL |
| Prolonger supine positioning | Spinal fractures |
| Persistent hyperglycemia | Blood glucose > 140 mg/dL |
Modified from Metheny NA. Risk factors for aspiration. JPEN J Parenter Enteral Nutr 2002;26(Suppl 6):S26-S31.
Clinical Manifestations
Hypoxemia is the most consistent finding in aspiration. In addition, patients present with increased temperature, tachypnea, tachycardia or bradycardia, cyanosis, and altered mental status. On physical examination, the pulmonary findings include crackles, rales, and decreased breath sounds. The extent of these manifestations depends on the degree of aspiration.1, 24
The outcome varies widely from asymptomatic to rapid death.1 Fortunately, many patients improve rapidly within several days without further treatment. A second subset of patients improves initially and then deteriorates over the following 2 to 5 days. These patients develop increased temperature, productive cough, and hypoxemia and progress from aspiration pneumonitis to aspiration pneumonia. The remaining patients do not improve from their initial pneumonitis and progress to diffuse pulmonary infiltrates, refractory hypoxemia, and ARDS.
Diagnosis
After a witnessed pulmonary aspiration, the diagnosis is clear. However, in other situations, the diagnosis of aspiration is based on the clinical symptoms and a high index of suspicion. On laboratory evaluation, significant aspiration results in hypoxemia and leukocytosis. Aspiration may also be identified by means of chest radiography. There are no pathognomonic radiologic features; however, infiltrates in gravity-dependent lung regions are the most consistent finding. The most common sites of infiltration are the superior segment of the right lower lobe and the right middle lobe. However, depending on the aspirate volume and the patient’s position during aspiration, left and bi-lobar aspiration is possible. Flexible fiberoptic bronchoscopy may also be used for diagnosing aspiration.1, 24
Treatment
As in atelectasis, prevention is the key. During the preoperative assessment by the anesthesiologist, patients at risk of aspiration need to be identified (Fig. 39.2 ). These include patients requiring emergency procedures, patients with diabetes mellitus, and pregnant patients. In these instances, an experienced anesthesiologist is required. If feasible, regional anesthesia should be entertained. The American Society of Anesthesiology have produced guidelines on the duration of preoperative fasting required under various circumstances (Table 39.2 ).37
Fig. 39.2.
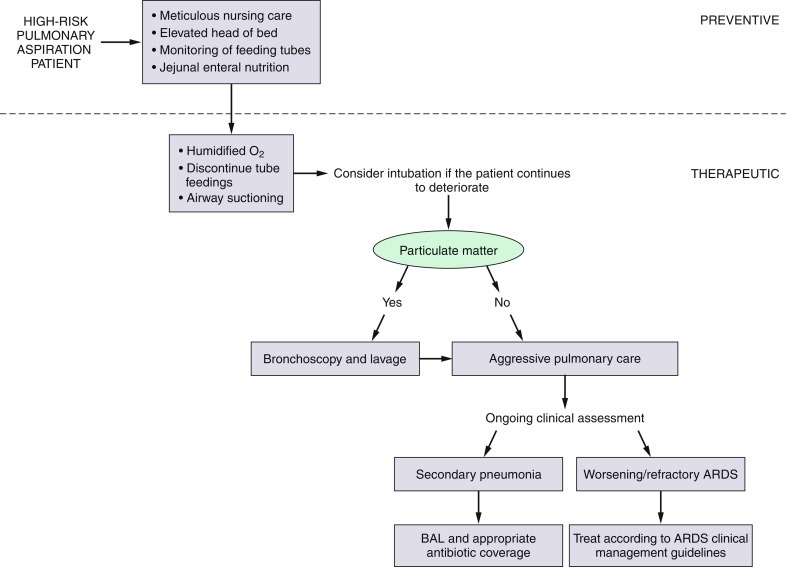
Prevention and treatment algorithm for pulmonary aspiration. ARDS, Acute respiratory distress syndrome; BAL, bronchoalveolar lavage.
Table 39.2.
Preoperative fasting recommendations of American Society of Anesthesiologists.
| Ingested material | Minimum fasting period |
|---|---|
| Clear liquids (water, fruit juices without pulp, carbonated drinks, tea and coffee without milk | 2 hours |
| Breast milk | 4 hours |
| Infant formula | 6 hours |
| Non-human milk | 6 hours |
| Light meal, e.g., toast and clear fluids | 6 hours |
| Fried foods, fatty foods or meat | Additional fasting time (e.g. 8 or more hours) may be needed |
Adapted from Practice guidelines for preoperative fasting and the use of pharmacologic agents to reduce the risk of pulmonary aspiration: application to healthy patients undergoing elective procedures: an updated report by the American Society of Anesthesiologists Task Force on preoperative fasting and the use of pharmacologic agents to reduce the risk of pulmonary aspiration. Anesthesiology 2017;127:376-393.
After the surgical procedure, meticulous nursing care is required.1 The head of the bed should be elevated to 30 degrees at a minimum; elevation to 45 degrees is better. In addition, particular attention should be paid to oral hygiene. Nasogastric and orogastric tubes should be monitored closely because they may become displaced during the course of hospitalization.
Gastric feeding is a major risk factor for pulmonary aspiration and there appears to be no difference in risk between nasogastric/orogastric tubes and small-bore feeding tubes.38 To avoid this problem, many clinicians advocate postpyloric feeding. However, randomized controlled trials comparing gastric with postpyloric feeding have produced conflicting results,39, 40, 41, 42, 43, 44, 45 possibly because most postpyloric feeding tubes are too short to go beyond the ligament of Treitz. When the tube is too short, enteral nutrition is administered into the duodenum and there is a high incidence of duodenogastric reflux in patients at risk for aspiration.40 Heyland and coworkers documented an 80% rate of reflux into the stomach, 25% into the esophagus, and 4% into the lung when radioisotope-labeled enteral formulas were fed through postpyloric feeding tubes in mechanically ventilated patients in the intensive care unit.43 In postoperative patients, Tournadre and colleagues demonstrated gastroparesis and rapid uncoordinated duodenal contractions.46 These studies provide compelling evidence that duodenogastric reflux is present in postoperative and critically ill patients. Thus, with regard to aspiration risk, feeding into the duodenum is not significantly different from feeding into the stomach in these patients. In addition to these findings, there appears to be no difference in the rate of pulmonary aspiration between patients with nasogastric feeding tubes and percutaneous endoscopic gastrostomy (PEG) tubes.47
Once the diagnosis of aspiration is entertained, the resultant hypoxemia should be addressed. Supplemental oxygen via a nasal cannula or a face mask should be administered until the diagnosis is confirmed. In severe cases, patients may require intubation and positive-pressure mechanical ventilation. If tube feeding is ongoing, it should be discontinued. Suctioning should be performed to clear the upper airway of any residual aspirate. The role of bronchoscopy is limited to the retrieval of large particulate matter. The acidic aspirate is neutralized by pulmonary secretions within minutes of aspiration, therefore bronchoscopy and saline lavage are not required for the aspiration of nonparticulate matter. The use of empiric antibiotic coverage is not supported by current literature; however, if a subsequent aspiration pneumonia is identified, antibiotic coverage should be tailored according to the microbiological findings. Not only are empiric antibiotics not indicated in aspiration but they often select for resistant organisms.1
Pulmonary Embolism
In 1856, Virchow described a triad of conditions associated with the development of venous thromboembolism (VTE): vessel intimal injury, venous stasis, and hypercoagulability.48 Today, VTE remains a significant source of morbidity and mortality after surgical procedures. The most common and clinically significant forms of VTE are deep vein thrombosis (DVT) and pulmonary embolism (PE).49 PE is the most common preventable source of hospital mortality.50
Venous thromboembolic disorders vary in incidence depending on the type of surgical procedure being performed; the highest rates are reported in urologic and orthopedic procedures.51 Studies prior to 1984 documented a 15%–30% rate of DVT and a 0.2%–0.9% rate of fatal PE among general surgical patients not treated with VTE prophylaxis.52, 53, 54 The current risk of DVT and PE in general surgical procedures is unknown because trials devoid of prophylaxis are no longer ethical. The combination of individual predisposing factors and the specific type of surgery determine the risk of DVT and PE in surgical patients. Risk factors are shown in Box 39.3 .55, 56, 57, 58, 59, 60
Box 39.3. Risk factors for venous thromboembolism in general surgical patients.
Patient-Related Factors
-
▪
Genetic predisposition
-
▪
Increasing age
-
▪
Cancer
-
▪
Previous venous thromboembolism
-
▪
Obesity
-
▪
Smoking
-
▪
Varicose veins
-
▪
Estrogen-containing oral contraception or hormone replacement therapy
-
▪
Pregnancy
Type of Anesthesia
-
▪
General anesthesia
Postoperative Care
-
▪
Immobilization
-
▪
Central venous catheterization
-
▪
Fluid resuscitation
-
▪
Transfusion
Alt-text: Box 39.3
Clinical Manifestations
The clinical manifestations of pulmonary embolism are highly variable. The majority of emboli are asymptomatic. In those that are symptomatic, the most common complaint is dyspnea, which is sudden in onset. Additional findings include rales, pleuritic chest pain, and hemoptysis. Patients with massive pulmonary emboli often present with chest discomfort in addition to anxiety and a sense of impending doom. In the most severe form, massive embolic events involve complete circulatory collapse, characterized by shock and/or syncope.10 The physical examination is often unremarkable, the most common findings being tachypnea and tachycardia. Jugular vein distention, a parasternal heave, a pulsatile liver, and a loud S2 on cardiac can also be present.
Diagnosis
A high index of suspicion is critical for diagnosing a PE. A detailed history should be obtained specifically inquiring about a history of VTE, preexisting medical conditions, and other risk factors. On blood gas analysis, most patients are hypoxemic. On the electrocardiogram (ECG), the most common finding is sinus tachycardia. Other common abnormalities are anterior precordial T wave inversion, S1Q3T3 and precordial ST segment elevation.61 The chest radiograph is generally non-diagnostic; however, a wedge-shaped infiltrate (Hampton’s hump) should heighten suspicion of a PE. Additional findings can include a prominent pulmonary artery with decreased peripheral pulmonary vasculature (Westermark’s sign).61
Measuring circulating D-dimer levels as an aid in diagnosing DVT and PE has been recommended, but the role of this test remains uncertain in this setting. The main problem with this test is that D-dimer levels are elevated in multiple medical conditions, including routine recovery from operations. As such, the specificity and positive likelihood ratios are of little clinical value in diagnosing DVT or PE. Despite these limitations, if the D-dimer is not elevated, the patient does not have a PE.
More definitive diagnostic tools for PE include ventilation-perfusion (V/Q) scans and CT pulmonary angiography. The Prospective Investigation of Pulmonary Embolism Diagnosis (PIOPED) study reviewed V/Q scanning as a diagnostic modality for PE.62 Seventy-five percent of V/Q scans are in the indeterminate category. Thus, V/Q scanning alone is insufficient to either confirm or exclude the diagnosis of PE. The D-dimer test and Doppler ultrasound may be useful adjuncts in this situation.63, 64
Since the 1990s, CT scans have become a routine means of diagnosing PE. Advantages of the CT scan include its rapidity, widespread availability, and non-invasiveness. In 2005, Hayashino and colleagues performed a meta-analysis of the diagnostic performance of helical CT scanning in comparison to V/Q scanning in suspected PE.65 On the basis of a summary receiver operating characteristic (ROC) analysis, they determined that when the V/Q scan is normal or near-normal, the CT scan is superior in the diagnosis of PE. However, in situations of high probability, the V/Q scan is equivalent to CT scan for diagnosing PE.
Prophylaxis
Because of the inherent risk of DVT and PE in postoperative patients, numerous modalities have been developed for prophylaxis. Prophylactic measures are categorized by mechanism of action as pharmacologic or mechanical. The most commonly used pharmacologic measure is low molecular weight heparin (LMWH).66 In the past, low-dose unfractionated heparin was the pharmacologic standard of care for VTE prevention; however, a number of disadvantages have made it unattractive as a prophylactic agent. These include, but are not limited to, nonspecific binding, low bioavailability, anticoagulant and dose-response variability, resistance, and heparin-induced thrombocytopenia (HIT). LMWH overcomes the majority of these limitations with the exception of HIT.67
Mechanical measures include thromboembolism-deterrent stockings (TEDS) and intermittent pneumatic compression (IPC) devices, such as venous foot pumps (VFP) and sequential compression devices (SCD). In 1986, the National Institutes of Health Consensus Development Conference on the Prevention of Venous Thrombosis and Pulmonary Embolism endorsed IPC devices as an effective prophylactic measure68 and the American Society of Hematology 2019 guidelines for Management of Venous Thromboembolism: Prevention of venous thromboembolism in surgical hospitalized patients clinical guidelines69 recommended IPC devices over no prophylaxis rather than TEDS. In addition to the efficacy of IPCs, there are few associated complications. Only isolated case reports of pressure necrosis, peroneal nerve palsy, and compartment syndrome have been documented.70, 71 Mechanical measures should be considered in patients with a high bleeding potential. In addition, they should be considered in combination with chemical prophylaxis to improve efficacy in high-risk patients.69
The mechanism of action of intermittent pneumatic compression devices is twofold. The first is mechanical: the devices increase the velocity of venous return and decrease venous stasis. The second mechanism is the systemic activation of the fibrinolytic system. Compression results in the release of plasminogen activators, which are found in high concentrations in the vaso vasorum.
In multiple trauma patients, when neither chemical nor standard mechanical prophylaxis approaches are an option, placement of an inferior vena cava (IVC) filter may be considered.
Routine use of VTE prophylaxis is recommended for at-risk surgical patients and the measures recommended vary depending on the nature of the surgical procedure and the bleeding versus thrombosis risk of individual patients.69
Treatment
Once the diagnosis of PE is seriously entertained, the treatment is supportive. Treatment includes the administration of oxygen, fluid resuscitation, and full anticoagulation. For medical patients, rapid anticoagulation before the definitive diagnosis is acceptable. However, this treatment strategy should be avoided in the surgical population, where the diagnostic uncertainty and bleeding potential are greater. Quinlan and coworkers performed a meta-analysis of randomized controlled trials comparing LMWH with intravenous unfractionated heparin in the treatment of PE.72 This meta-analysis revealed that fixed-dose LMWH is as effective and safe as intravenous unfractionated heparin for the treatment of sub-massive PE. In this study, the rate of bleeding, recurrent VTE, and mortality were not significantly different between the two treatment arms. Other modalities of PE treatment include thrombolytic therapy and IVC filters and specialist opinions should be sought if considered.
Acute Respiratory Distress Syndrome
Acute respiratory distress syndrome is characterized by the presence of refractory hypoxemic respiratory failure in the presence of bilateral pulmonary infiltrates on chest radiography. The diagnostic criteria were updated in the 2012 Berlin criteria and it is now sub-classified into mild, moderate, and severe depending on the degree of oxygenation deficit.73
Acute respiratory distress syndrome occurs in a bi-modal distribution in the postoperative period, with early cases occurring within 72 hours of the surgical procedure. Surgical procedures, such as pulmonary thromboendarterectomy, where pulmonary ischemia-reperfusion injury occurs are associated with the development of ARDS within 72 hours of the procedure. Similarly, procedures that involve the use of cardiopulmonary bypass, where the bypass circuit can induces a systemic inflammatory cascade, are also associated with an increased risk of ARDS in the early postoperative period.74
A second peak of acute respiratory distress syndrome in the postoperative patient occurs somewhat later and is a well-recognized postoperative pulmonary complication. Only two-thirds of ARDS occurring after esophagectomy surgery are within the first 72 hours.75 Interestingly, it has been observed that patients undergoing Ivor Lewis esophagectomy are more vulnerable to the development of ARDS between 1 and 10 days after the procedures than patients undergoing major pulmonary resection.76 The reported rates of pneumonia are also lower after major pulmonary resection than after Ivor Lewis esophagectomy. In this study, the intra-surgical blood loss, duration of one-lung ventilation, and the release of circulating biomarkers did not seem to explain the different rates of postoperative ARDS. The authors postulate that the site of the esophageal anastomosis and the risk of anastomotic leak may be causative factors, but this requires further study.
There is no licensed pharmacotherapy for ARDS anywhere in the world, despite several decades of clinical trials. The gold standard clinical management is supportive care with lung protective ventilation77 and conservative use of intravenous fluids,78 and does not significantly differ for the postoperative patient compared with ARDS from other etiologies.
Principles of Management
The most common clinical presentation of all types of acute respiratory failure is acute hypoxia.79 Early identification and appropriate management are critical in limiting adverse outcomes. In the non-intubated patient, evaluation includes a physical examination, a review of recent events, an inspection of any supplemental oxygen equipment, arterial blood analysis, chest radiography, and an electrocardiogram (selectively). Following this, management should be as indicated by the likely diagnosis.
In the intubated patient, the evaluation is more complex. An algorithm for the approach to the hypoxic intubated patient is found in Fig. 39.3 .80 In this scenario, hypoxia is defined as a 5% decrease in continuous pulse oximetry (SpO2) or a 10% decrease in mixed venous oximetry (SvO2). After identification of hypoxia, the supplemental oxygen should be enhanced. The patient should be disconnected from the mechanical ventilator and hand ventilated. If there is a cuff leak, the tube should be repaired or replaced. If there is difficulty bagging the patient, an attempt at passing a suction catheter should be made. Inability to do so confirms obstruction. If this cannot be reversed by altering the patient’s head position, checking the tube’s position, or deflating the cuff, the tube should be replaced. If there is no evidence of obstruction, despite bagging difficulty, a tension pneumothorax should be ruled out. Assuming that the patient is hand ventilated easily, the mechanical ventilator and its circuitry should be inspected to exclude a mechanical flaw. Additional workup at this time should include a physical examination, review of recent events, blood gas analysis, a portable anteroposterior chest radiograph, and an electrocardiogram. Further diagnostic studies should be guided by the findings in the algorithm of Fig. 39.3.
Fig. 39.3.
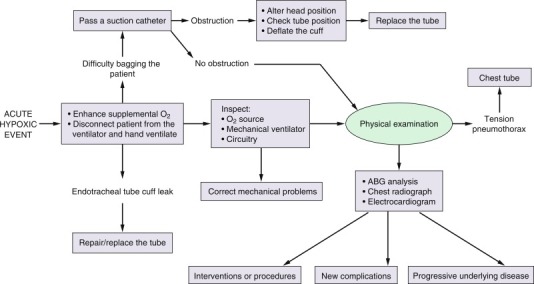
Treatment algorithm for acute hypoxia in the intubated patient. ABG, Arterial blood gas.
Summary
Throughout this chapter, we have focused on the clinically relevant issues regarding postoperative respiratory failure. Initially, we addressed the pathophysiology of the varying types of acute respiratory failure, then we identified the preoperative, intraoperative, and postoperative predictors of postoperative pulmonary complications including respiratory failure. We then took an in-depth look at the more common etiologies of acute respiratory failure: atelectasis, pulmonary aspiration, pulmonary embolism and the acute respiratory distress syndrome. Finally, we outlined a practice approach to the acutely hypoxemic perioperative patient, that is outlined in the algorithm shown in Fig. 39.4 .
Fig. 39.4.
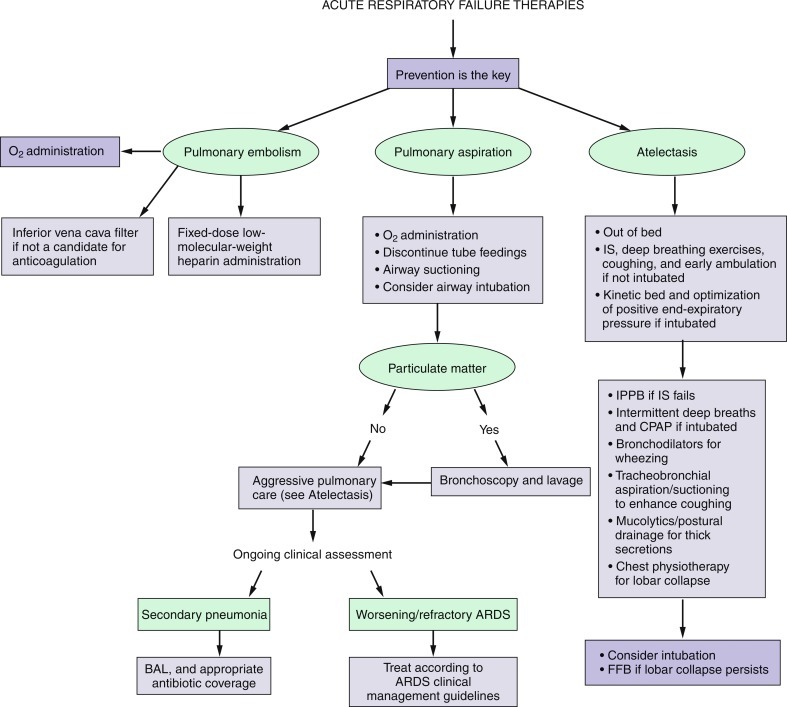
Overview algorithm for treatment of pulmonary embolism, pulmonary aspiration, and atelectasis. ARDS, Acute respiratory distress syndrome; BAL, bronchoalveolar lavage; CPAP, continuous positive airway pressure; FFB, flexible fiberoptic bronchoscopy; IS, incentive spirometry; IPPB, intermittent positive-pressure breathing.
References
- 1.Webb A.R., Shapiro M.J., Singer M., Suter P.M. Oxford University Press; New York: 1999. Oxford Textbook of Critical Care. [Google Scholar]
- 2.Parrillo J.E., Dellinger R.P. ed 2. Mosby; St. Louis: 2002. Critical Care Medicine: Principles of Diagnosis and Management in the Adult. [Google Scholar]
- 3.Tisi G.M. ed 2. Williams & Wilkins; Baltimore: 1983. Pulmonary Physiology in Clinical Medicine. [Google Scholar]
- 4.Cameron J.L. ed 5. Mosby; St. Louis: 1995. Current Surgical Therapy. [Google Scholar]
- 5.Neema P.K. Respiratory failure. Indian J Anaesth. 2003;47:360–366. [Google Scholar]
- 6.Nijbroek S.G., Schultz M.J., Hemmes S.N.T. Prediction of postoperative pulmonary complications. Curr Opin Anaesthesiol. 2019;32:443–451. doi: 10.1097/ACO.0000000000000730. [DOI] [PubMed] [Google Scholar]
- 7.Canet J., Gallart L., Gomar C., et al. Prediction of postoperative pulmonary complications in a population-based surgical cohort. Anesthesiology. 2010;113:1338–1350. doi: 10.1097/ALN.0b013e3181fc6e0a. [DOI] [PubMed] [Google Scholar]
- 8.Moulton M.J., Creswell L.L., Mackey M.E., et al. Obesity is not a risk factor for significant adverse outcomes after cardiac surgery. Circulation. 1996;94(Suppl II):II87–II92. [PubMed] [Google Scholar]
- 9.Pasulka P.S., Bistrian B.R., Benotti P.N., Blackburn G.L. The risks of surgery in obese patients. Ann Intern Med. 1986;104:540–546. doi: 10.7326/0003-4819-104-4-540. [DOI] [PubMed] [Google Scholar]
- 10.Gupta J., Fernandes R.J., Rao J.S., Dhanpal R. Perioperative risk factors for pulmonary complications after non-cardiac surgery. J Anaesthesiol Clin Pharmacol. 2020;36:88–93. doi: 10.4103/joacp.JOACP_54_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Warner M.A., Offord K.P., Warner M.E., et al. Role of preoperative cessation of smoking and other factors in postoperative pulmonary complications: a blinded prospective study of coronary artery bypass patients. Mayo Clin Proc. 1989;64:609–616. doi: 10.1016/s0025-6196(12)65337-3. [DOI] [PubMed] [Google Scholar]
- 12.Thomsen T., Villebro N., Møller A.M. Interventions for preoperative smoking cessation. Cochrane Database Syst Rev. 2014;3 doi: 10.1002/14651858.CD002294.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.LAS VEGAS investigators Epidemiology, practice of ventilation and outcome for patients at increased risk of postoperative pulmonary complications: LAS VEGAS – an observational study in 29 countries. Eur J Anaesthesiol. 2017;34:492–507. doi: 10.1097/EJA.0000000000000646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Watson X., Chereshneva M., Odor P.M., et al. Adoption of lung protective ventilation in patients undergoing emergency laparotomy: the ALPINE study. A prospective multicenter observational study. Br J Anaesth. 2018;121:909–917. doi: 10.1016/j.bja.2018.04.048. [DOI] [PubMed] [Google Scholar]
- 15.Neta A.S., Hemmes S.N.T., Barbas C.S.V., et al. Association between driving pressure and development of postoperative pulmonary complications in patients undergoing mechanical ventilation for general anaesthesia: a meta-analysis of individual patient data. Lancet Respir Med. 2016;4:272–280. doi: 10.1016/S2213-2600(16)00057-6. [DOI] [PubMed] [Google Scholar]
- 16.Neto A.S., Cardoso S.O., Manetta J.A., et al. Associations between use of lung-protective ventilation with lower tidal volumes and clinical outcomes among patients without acute respiratory distress syndrome. JAMA. 2012;308:1651–1659. doi: 10.1001/jama.2012.13730. [DOI] [PubMed] [Google Scholar]
- 17.Sabiston D.C., Lyerly H.K. ed 15. WB Saunders; Philadelphia: 1997. Textbook of Surgery: The Biological Basis of Modern Surgical Practice. [Google Scholar]
- 18.Duggan M., Kavanagh B.P. Pulmonary atelectasis: a pathogenic perioperative entity. Anesthesiology. 2005;102:838–854. doi: 10.1097/00000542-200504000-00021. [DOI] [PubMed] [Google Scholar]
- 19.Lundh R., Hedenstierna G. Ventilation-perfusion relationships during anesthesia and abdominal surgery. Acta Anaesthesiol Scand. 1983;27:167–173. doi: 10.1111/j.1399-6576.1983.tb01929.x. [DOI] [PubMed] [Google Scholar]
- 20.Jonmarker C., Nordstrom L., Werner O. Changes in functional residual capacity during surgery. Br J Anaesth. 1986;58:428–432. doi: 10.1093/bja/58.4.428. [DOI] [PubMed] [Google Scholar]
- 21.Magnusson L., Zemgulis V., Wicky S., et al. Atelectasis is a major cause of hypoxemia and shunt after cardiopulmonary bypass: an experimental study. Anesthesiology. 1997;87:1153–1163. doi: 10.1097/00000542-199711000-00020. [DOI] [PubMed] [Google Scholar]
- 22.Tenling A., Hachenberg T., Tyden H., et al. Atelectasis and gas exchange after cardiac surgery. Anesthesiology. 1998;89:371–378. doi: 10.1097/00000542-199808000-00013. [DOI] [PubMed] [Google Scholar]
- 23.Macnaughton P.D., Braude S., Hunter D.N., et al. Changes in lung function and pulmonary capillary permeability after cardiopulmonary bypass. Crit Care Med. 1992;20:1289–1294. doi: 10.1097/00003246-199209000-00016. [DOI] [PubMed] [Google Scholar]
- 24.Beers M.H., Berkow R. Merck; Whitehouse Station, NJ: 2005. Merck Manual of Diagnosis and Therapy. [Google Scholar]
- 25.Wilmore D.W., Cheung L.Y., Harken A.H., et al. WebMD Corporation; New York: 2002. American College of Surgeons ACS Surgery: Principles and Practice. [Google Scholar]
- 26.Warner D.O. Preventing postoperative pulmonary complications: the role of the anesthesiologist. Anesthesiology. 2000;92:1467–1472. doi: 10.1097/00000542-200005000-00037. [DOI] [PubMed] [Google Scholar]
- 27.Rusca M., Proietti S., Schnyder P., et al. Prevention of atelectasis formation during induction of general anesthesia. Anesth Analg. 2003;97:1835–1839. doi: 10.1213/01.ANE.0000087042.02266.F6. [DOI] [PubMed] [Google Scholar]
- 28.Ballantyne J.C., Carr D.B., deFerranti S., et al. The comparative effects of postoperative analgesic therapies on pulmonary outcome: cumulative meta-analysis of randomized, controlled trials. Anesth Analg. 1998;86:598–612. doi: 10.1097/00000539-199803000-00032. [DOI] [PubMed] [Google Scholar]
- 29.Dohi S., Gold M.I. Comparison of two methods of postoperative respiratory care. Chest. 1978;73:592–595. doi: 10.1378/chest.73.5.592. [DOI] [PubMed] [Google Scholar]
- 30.Bartlett R.H., Gazzaniga A.B., Geraghty T.R. Respiratory maneuvers to prevent postoperative pulmonary complications: a critical review. JAMA. 1973;224:1017–1021. [PubMed] [Google Scholar]
- 31.Hedstrand U., Liw M., Rooth G., Ogren C.H. Effect of respiratory physiotherapy on arterial oxygen tension. Acta Anaesthesiol Scand. 1978;22:349–352. doi: 10.1111/j.1399-6576.1978.tb01310.x. [DOI] [PubMed] [Google Scholar]
- 32.Thomas J.A., McIntosh J.M. Are incentive spirometry, intermittent positive pressure breathing, and deep breathing exercises effective in the prevention of postoperative pulmonary complications after upper abdominal surgery? A systematic overview and meta-analysis. Phys Ther. 1994;74:3–10. doi: 10.1093/ptj/74.1.3. [DOI] [PubMed] [Google Scholar]
- 33.Squadrone V., Coha M., Cerutti E., et al. Continuous positive airway pressure for treatment of postoperative hypoxia: a randomized controlled trial. JAMA. 2005;293:589–595. doi: 10.1001/jama.293.5.589. [DOI] [PubMed] [Google Scholar]
- 34.Marr A.B., McQuiggan M.M., Kozar R., Moore F.A. Gastric feeding as an extension of an established enteral nutrition protocol. Nutr Clin Pract. 2004;19:504–510. doi: 10.1177/0115426504019005504. [DOI] [PubMed] [Google Scholar]
- 35.McClave S.A., DeMeo M.T., DeLegge M.H., et al. North American Summit on Aspiration in the Critically Ill Patient: consensus statement. JPEN J Parenter Enteral Nutr. 2002;26(Suppl 6):S80–S85. doi: 10.1177/014860710202600613. [DOI] [PubMed] [Google Scholar]
- 36.Metheny N.A. Risk factors for aspiration. JPEN J Parenter Enteral Nutr. 2002;26(Suppl 6):S26–S31. doi: 10.1177/014860710202600605. [DOI] [PubMed] [Google Scholar]
- 37.Practice Guidelines for Preoperative Fasting and the Use of Pharmacologic Agents to Reduce the Risk of Pulmonary Aspiration Application to healthy patients undergoing elective procedures: an updated report by the American Society of Anesthesiologists Task Force on preoperative fasting and the use of pharmacologic agents to reduce the risk of pulmonary aspiration. Anesthesiology. 2017;127:376–393. doi: 10.1097/ALN.0000000000001452. [DOI] [PubMed] [Google Scholar]
- 38.Ferrer M., Bauer T.T., Torres A., et al. Effect of nasogastric tube size on gastroesophageal reflux and microaspiration in intubated patients. Ann Intern Med. 1999;130:991–994. doi: 10.7326/0003-4819-130-12-199906150-00007. [DOI] [PubMed] [Google Scholar]
- 39.Kearns P.J., Chin D., Mueller L., et al. The incidence of ventilator-associated pneumonia and success in nutrient delivery with gastric versus small intestinal feeding: a randomized clinical trial. Crit Care Med. 2000;28:1742–1746. doi: 10.1097/00003246-200006000-00007. [DOI] [PubMed] [Google Scholar]
- 40.Kortbeek J.B., Haigh P.I., Doig C. Duodenal versus gastric feeding in ventilated blunt trauma patients: a randomized controlled trial. J Trauma. 1999;46:992–996. doi: 10.1097/00005373-199906000-00002. [DOI] [PubMed] [Google Scholar]
- 41.Montejo J.C., Grau T., Acosta J., et al. Multicenter, prospective, randomized, single-blind study comparing the efficacy and gastrointestinal complications of early jejunal feeding with early gastric feeding in critically ill patients. Crit Care Med. 2002;30:796–800. doi: 10.1097/00003246-200204000-00013. [DOI] [PubMed] [Google Scholar]
- 42.Strong R.M., Condon S.C., Solinger M.R., et al. Equal aspiration rates from postpylorus and intragastric-placed small-bore nasoenteric feeding tubes: a randomized, prospective study. JPEN J Parenter Enteral Nutr. 1992;16:59–63. doi: 10.1177/014860719201600159. [DOI] [PubMed] [Google Scholar]
- 43.Heyland D.K., Drover J.W., MacDonald S., et al. Effect of postpyloric feeding on gastroesophageal regurgitation and pulmonary microaspiration: results of a randomized controlled trial. Crit Care Med. 2001;29:1495–1500. doi: 10.1097/00003246-200108000-00001. [DOI] [PubMed] [Google Scholar]
- 44.Davis A.R., Froomes P.R.A., French C.J., et al. Randomized comparison of nasojejunal and nasogastric feeding in critically ill patients. Crit Care Med. 2002;30:586–590. doi: 10.1097/00003246-200203000-00016. [DOI] [PubMed] [Google Scholar]
- 45.Montecalvo M.A., Steger K.A., Farber H.W., et al. Nutritional outcome and pneumonia in critical care patients randomized to gastric versus jejunal tube feedings. The Critical Care Research Team. Crit Care Med. 1992;20:1377–1387. doi: 10.1097/00003246-199210000-00004. [DOI] [PubMed] [Google Scholar]
- 46.Tournadre J.P., Barclay M., Fraser R., et al. Small intestinal motor patterns in critically ill patients after major abdominal surgery. Am J Gastroenterol. 2001;96:2418–2426. doi: 10.1111/j.1572-0241.2001.03951.x. [DOI] [PubMed] [Google Scholar]
- 47.Park R.H., Allison M.C., Lang J., et al. Randomised comparison of percutaneous endoscopic gastrostomy and nasogastric tube feeding in patients with persisting neurologic dysphagia. BMJ. 1992;304:1406–1409. doi: 10.1136/bmj.304.6839.1406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Knudson M.M., Lewis F.R., Clinton A., et al. Prevention of venous thromboembolism in trauma patients. J Trauma. 1994;37:480–487. doi: 10.1097/00005373-199409000-00025. [DOI] [PubMed] [Google Scholar]
- 49.Bell W.R., Simon T.L. Current status of pulmonary thromboembolism disease: pathophysiology, diagnosis, prevention, and treatment. Am Heart J. 1982;103:239–262. doi: 10.1016/0002-8703(82)90498-7. [DOI] [PubMed] [Google Scholar]
- 50.Anderson F.A., Wheeler H.B., Goldberg R.J., et al. A population-based perspective of the hospital incidence and case-fatality rates of deep vein thrombosis and pulmonary embolism: the Worcester DVT study. Arch Intern Med. 1991;151:933–938. [PubMed] [Google Scholar]
- 51.Geerts W.H., Pineo G.F., Heit J.A., et al. Prevention of venous thromboembolism: the Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest. 2004;126:338S–400S. doi: 10.1378/chest.126.3_suppl.338S. [DOI] [PubMed] [Google Scholar]
- 52.Mismetti P., Laporte S., Darmon J.Y., et al. Meta-analysis of low molecular weight heparin in the prevention of venous thromboembolism in general surgery. Br J Surg. 2001;88:913–930. doi: 10.1046/j.0007-1323.2001.01800.x. [DOI] [PubMed] [Google Scholar]
- 53.Clagett G.P., Reisch J.S. Prevention of venous thromboembolism in general surgical patients: results of a meta-analysis. Ann Surg. 1988;208:227–240. doi: 10.1097/00000658-198808000-00016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Pezzuoli G., Neri Serneri C.G., Settembrini P., et al. Prophylaxis of fatal pulmonary embolism in general surgery using low-molecular-weight heparin Cy 216: a multicentre, double-blinded, randomized, controlled, clinical trial versus placebo (STEP) Int Surg. 1989;74:205–210. [PubMed] [Google Scholar]
- 55.Goldhaber S.Z. Medical progress: pulmonary embolism. N Engl J Med. 1998;339:93–104. doi: 10.1056/NEJM199807093390207. [DOI] [PubMed] [Google Scholar]
- 56.Nicolaides A., Irving D., Pretzell M., et al. The risk of deep-vein thrombosis in surgical patients. Br J Surg. 1973;60:312. [PubMed] [Google Scholar]
- 57.Wille-Jorgensen P., Ott P. Predicting failure of low-dose heparin in general surgical procedures. Surg Gynecol Obstet. 1990;171:126–130. [PubMed] [Google Scholar]
- 58.Huber O., Bounameaux H., Borst F., et al. Postoperative pulmonary embolism after hospital discharge: an underestimated risk. Arch Surg. 1992;127:310–313. doi: 10.1001/archsurg.1992.01420030076014. [DOI] [PubMed] [Google Scholar]
- 59.Flordal P.A., Berggvist D., Burmark U.S., et al. Risk factors for major thromboembolism and bleeding tendency after elective general surgical operations. Eur J Surg. 1996;162:783–789. [PubMed] [Google Scholar]
- 60.Hendolin H., Mattila M.A.K., Poikolainen E. The effect of lumbar epidural analgesia on the development of deep vein thrombosis of the legs after open prostatectomy. Acta Chir Scand. 1981;147:425–429. [PubMed] [Google Scholar]
- 61.Bernal AG, Fanola C, Bartos A, American College of Cardiology. Management of PE guidelines. https://www.acc.org/latest-in-cardiology/articles/2020/01/27/07/42/management-of-pe
- 62.PIOPED Investigators. Value of the ventilation/perfusion scan in acute pulmonary embolism: results of the prospective investigation of pulmonary embolism diagnosis (PIOPED) JAMA. 1990;263:2753–2759. doi: 10.1001/jama.1990.03440200057023. [DOI] [PubMed] [Google Scholar]
- 63.Stein P.D., Hull R.D., Raskob G.E. Withholding treatment in patients with acute pulmonary embolism who have a high risk of bleeding and negative serial noninvasive leg tests. Am J Med. 2000;109:301–306. doi: 10.1016/s0002-9343(00)00508-8. [DOI] [PubMed] [Google Scholar]
- 64.Righini M., Goehring C., Bounameaux H., Perrier A. Effects of age on the performance of common diagnostic tests for pulmonary embolism. Am J Med. 2000;109:357–361. doi: 10.1016/s0002-9343(00)00493-9. [DOI] [PubMed] [Google Scholar]
- 65.Hayashino Y., Goto M., Noguchi Y., Fukui T. Ventilation-perfusion scanning and helical CT in suspected pulmonary embolism: meta-analysis of diagnostic performance. Radiology. 2005;234:740–748. doi: 10.1148/radiol.2343031009. [DOI] [PubMed] [Google Scholar]
- 66.Rogers F.B. Venous thromboembolism in trauma patients. Surg Clin North Am. 1995;75:279–291. doi: 10.1016/s0039-6109(16)46588-6. [DOI] [PubMed] [Google Scholar]
- 67.Fiorica J.V. Prophylaxis and treatment of venous thromboembolism. Surg Rounds. 2001:6–9. S. [Google Scholar]
- 68.National Institutes of Health Consensus Development Conference Prevention of venous thrombosis and pulmonary embolism. JAMA. 1986;256:744–749. [PubMed] [Google Scholar]
- 69.Anderson D.R., Morgano G.P., Bennett C., et al. American Society of Hematology 2019 guidelines for management of venous thromboembolism: prevention of venous thromboembolism in surgical hospitalized patients. Blood Adv. 2019;3:3898–3944. doi: 10.1182/bloodadvances.2019000975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Parra R.O., Farber R., Feigel A. Pressure necrosis from intermittent pneumatic compression stockings. N Engl J Med. 1989;321:1615. doi: 10.1056/NEJM198912073212316. [DOI] [PubMed] [Google Scholar]
- 71.Pittman G.R. Peroneal nerve palsy following sequential pneumatic compression. JAMA. 1989;261:2201–2202. doi: 10.1001/jama.1989.03420150051030. [DOI] [PubMed] [Google Scholar]
- 72.Quinlan D.J., McQuillan A., Eikelboom J.W. Low-molecular-weight heparin compared with intravenous unfractionated heparin for the treatment of pulmonary embolism: a meta-analysis of randomized, controlled trials. Ann Intern Med. 2004;140:175–183. doi: 10.7326/0003-4819-140-3-200402030-00008. [DOI] [PubMed] [Google Scholar]
- 73.ARDS Definition Task Force, Ranieri V.M., Rubenfeld G.D., et al. Acute respiratory distress syndrome: the Berlin Definition. JAMA. 2012;307:2526–2533. doi: 10.1001/jama.2012.5669. [DOI] [PubMed] [Google Scholar]
- 74.Stephens R.S., Shah A.S., Whitman G.J.R. Lung injury and acute respiratory distress syndrome after cardiac surgery. Ann Thorac Surg. 2013;95:1122–1129. doi: 10.1016/j.athoracsur.2012.10.024. [DOI] [PubMed] [Google Scholar]
- 75.Howells P., Thickett D., Knox C., et al. The impact of the acute respiratory distress syndrome on outcome after oesophagectomy. Br J Anaesth. 2016;117:375–381. doi: 10.1093/bja/aew178. [DOI] [PubMed] [Google Scholar]
- 76.Reichert M., Schistek M., Uhle F., et al. Ivor Lewis esophagectomy patients are particularly vulnerable to respiratory impairment – a comparison to major lung resection. Sci Rep. 2019;9:11856. doi: 10.1038/s41598-019-48234-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Fan E., Del Sorbo L., Goligher E.C., et al. An Official American Thoracic Society / European Society of Intensive Care Medicine / Society of Critical Care Medicine Clinical Practice Guideline: mechanical ventilation in adult patients with acute respiratory distress syndrome. Am J Respir Crit Care Med. 2017;195:1253–1263. doi: 10.1164/rccm.201703-0548ST. [DOI] [PubMed] [Google Scholar]
- 78.The National Heart National Heart, Lung, and Blood Institute Acute Respiratory Distress Syndrome (ARDS) Clinical Trials Network, Wiedemann HP, Wheeler AP, et al. Comparison of two fluid-management strategies in acute lung injury. N Engl J Med. 2006;354:2564–2575. doi: 10.1056/NEJMoa062200. [DOI] [PubMed] [Google Scholar]
- 79.Barcroft J.T. Anoxemia. Lancet. 1920;2:485–489. [Google Scholar]
- 80.Moore F.A., Haenel J.B., Moore E.E., Abernathy C.M. Hypoxic events in the surgical intensive care unit. Am J Surg. 1990;160:647–651. doi: 10.1016/s0002-9610(05)80766-4. [DOI] [PubMed] [Google Scholar]


